Molecular Pro-Apoptotic Activities of Flavanone Derivatives in Cyclodextrin Complexes: New Implications for Anticancer Therapy
Abstract
1. Introduction
2. Results and Discussion
2.1. Biological Assay
2.1.1. Determination of Cytotoxicity of Chromanone Analogues Condensed with Pyrazolines by Metabolic Microplate Spectrophotometric Assay with MTT
2.1.2. Determination of Cytotoxicity of Chromanone Analogues Condensed with Pyrazolines Incorporated in Cyclodextrins by Metabolic Microplate Spectrophotometric Assay with MTT
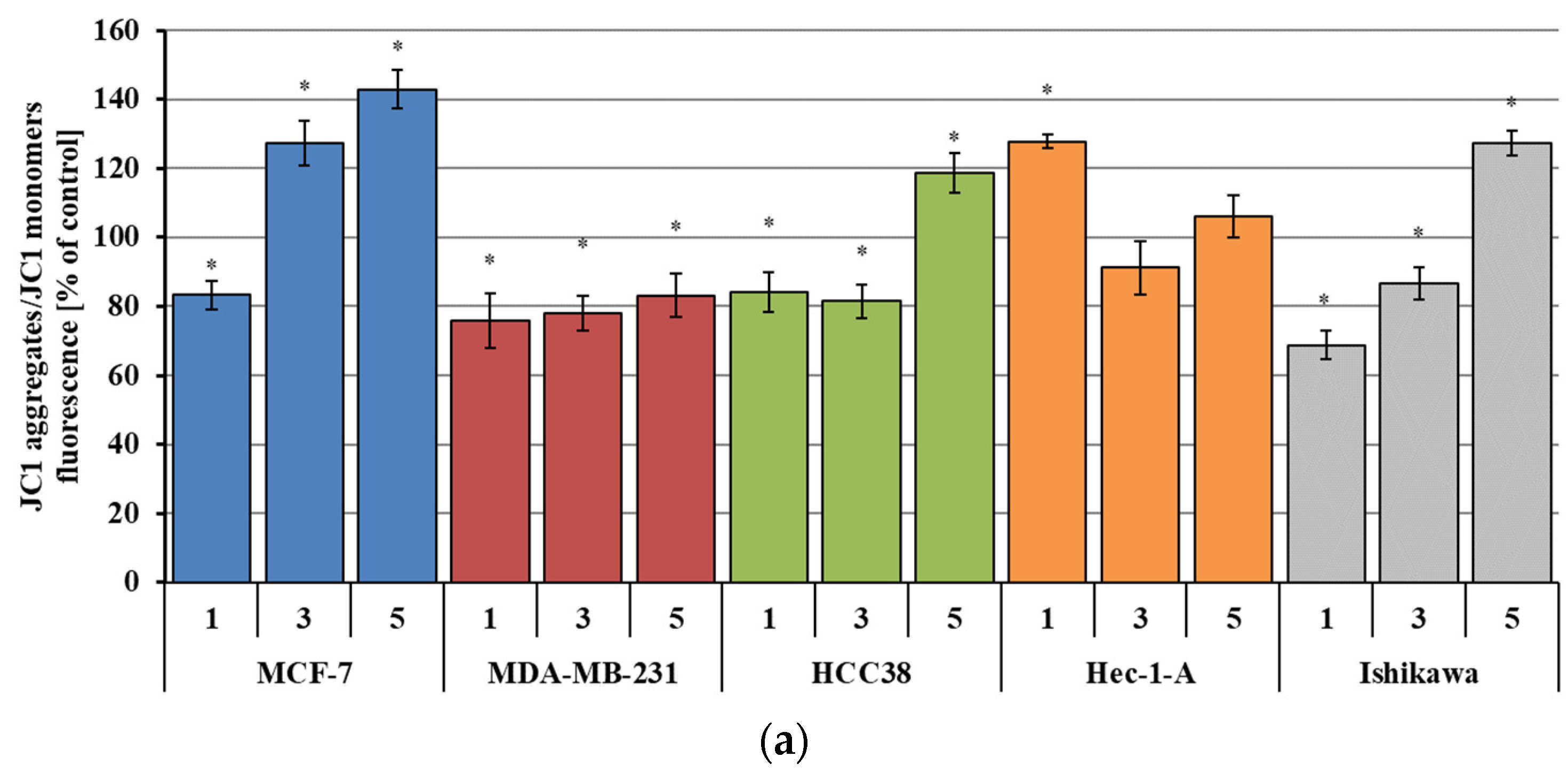
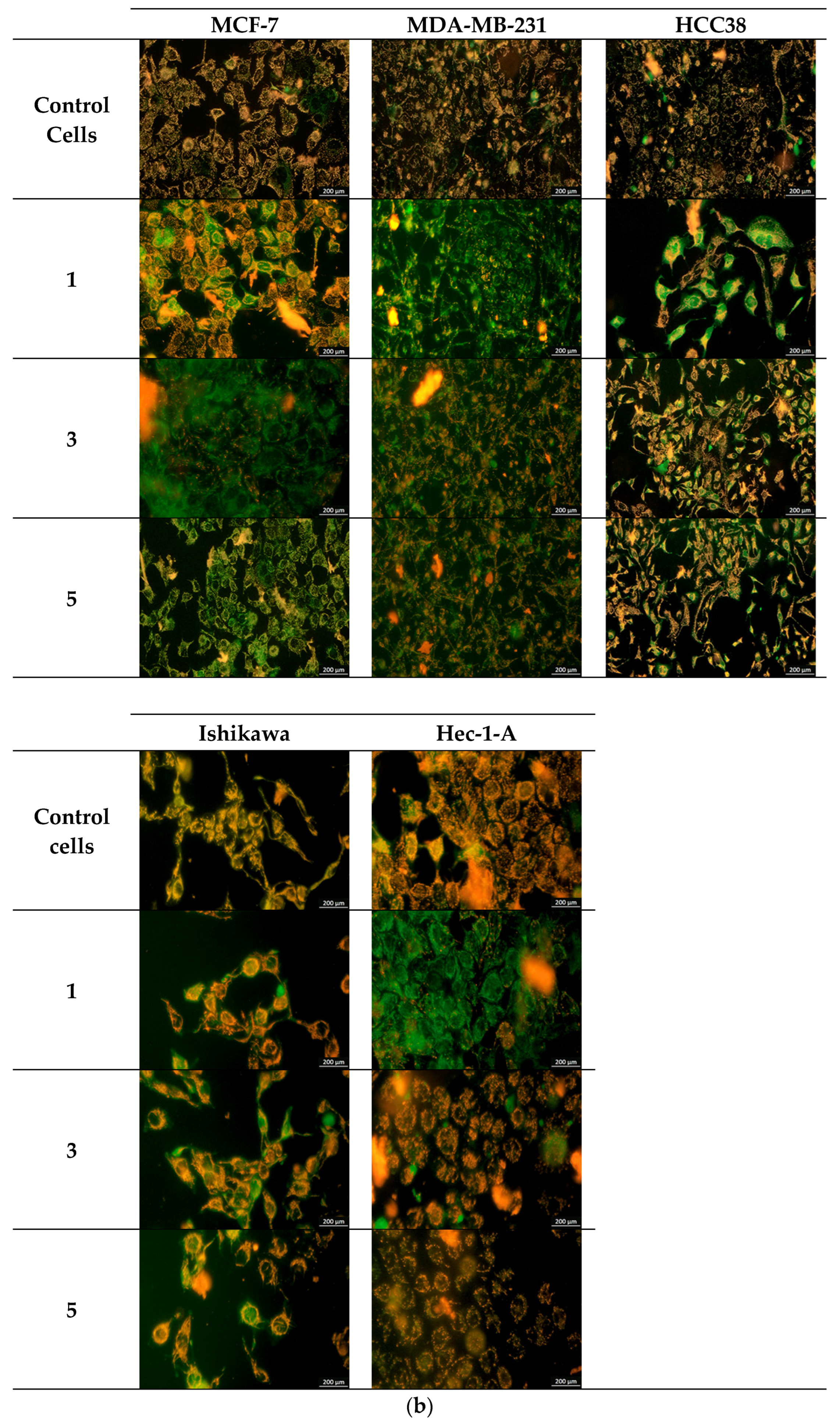
2.1.3. Analysis of Changes in Transmembrane Mitochondrial Potential (ΔΨm)—JC-1 Method
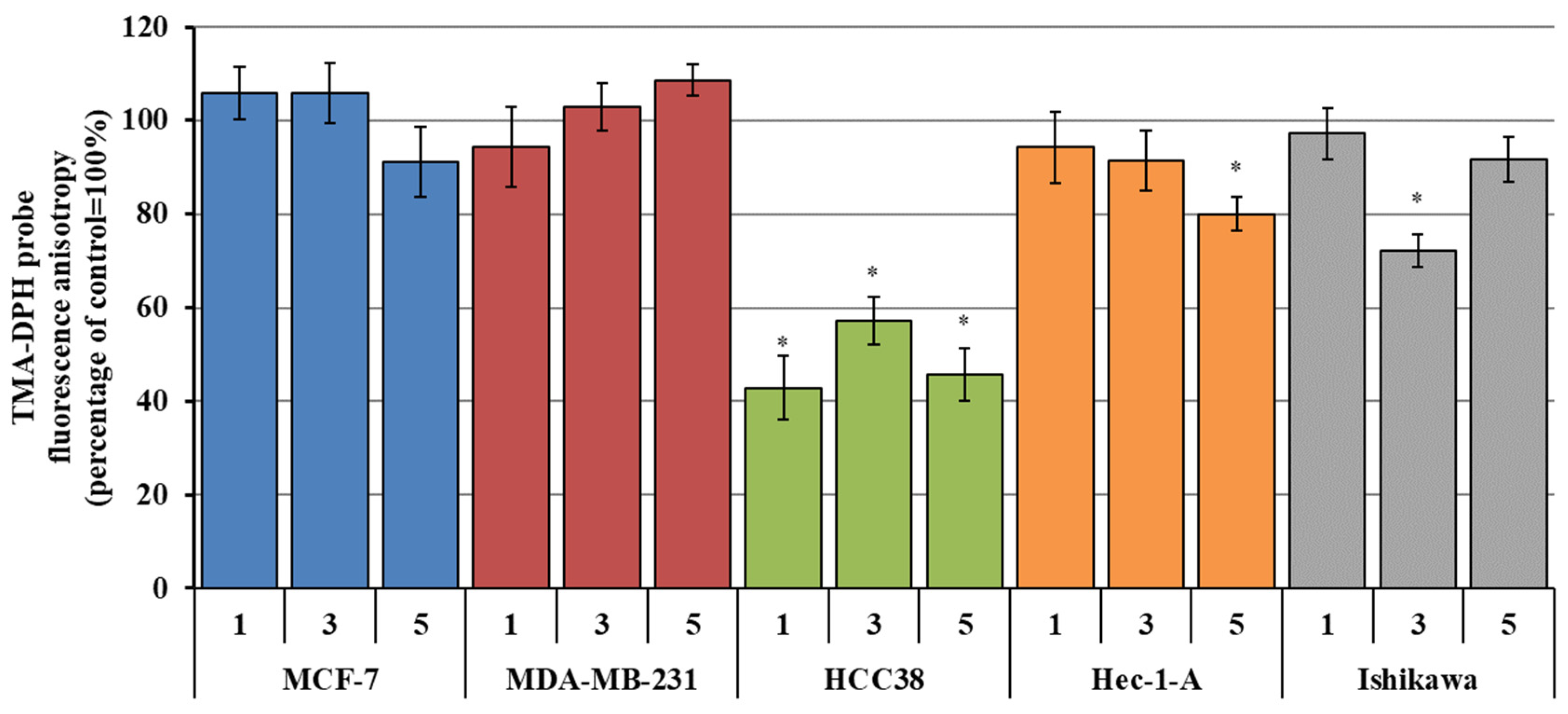
2.1.4. Changes in Plasma Membrane Fluidity (Measurement of TMA-DPH and DAUDA Fluorescence Anisotropy)—Lipid Peroxidation
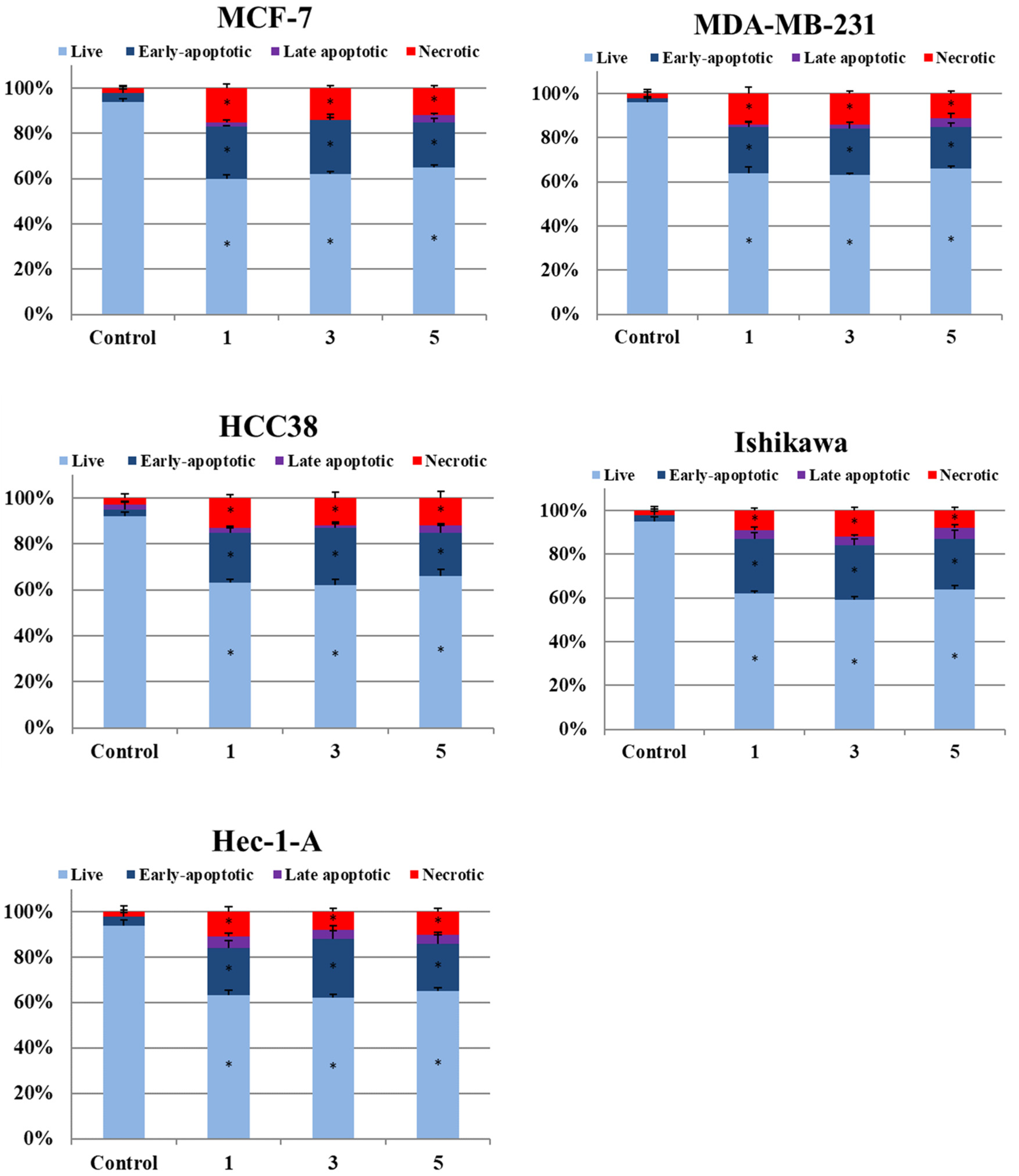
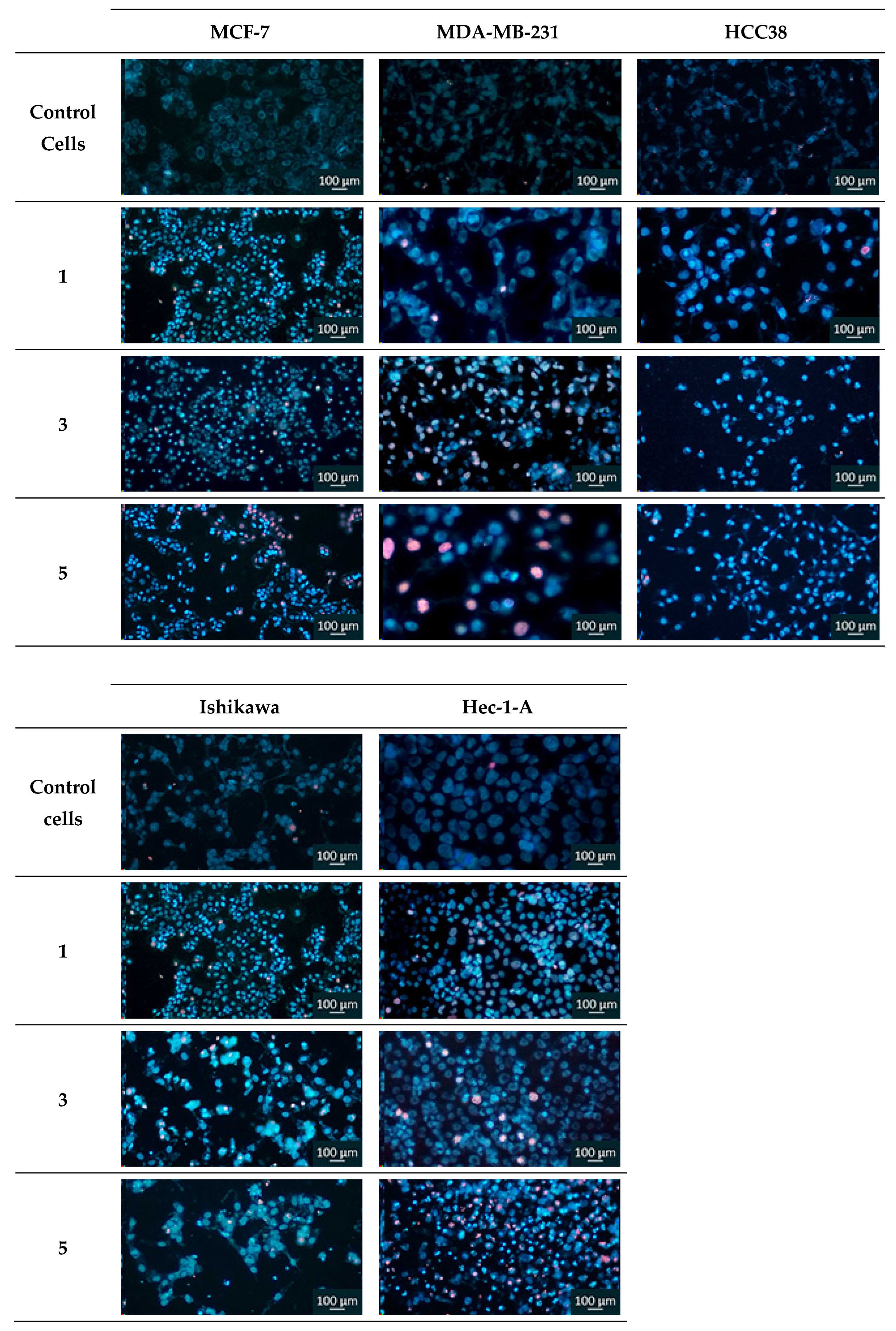
2.1.5. Determination of the Fraction of Apoptotic and Necrotic Cells by Fluorescence Microscopy (Double Staining of Cells with Hoechst 33258 and Propidium Iodide Fluorescent Dyes
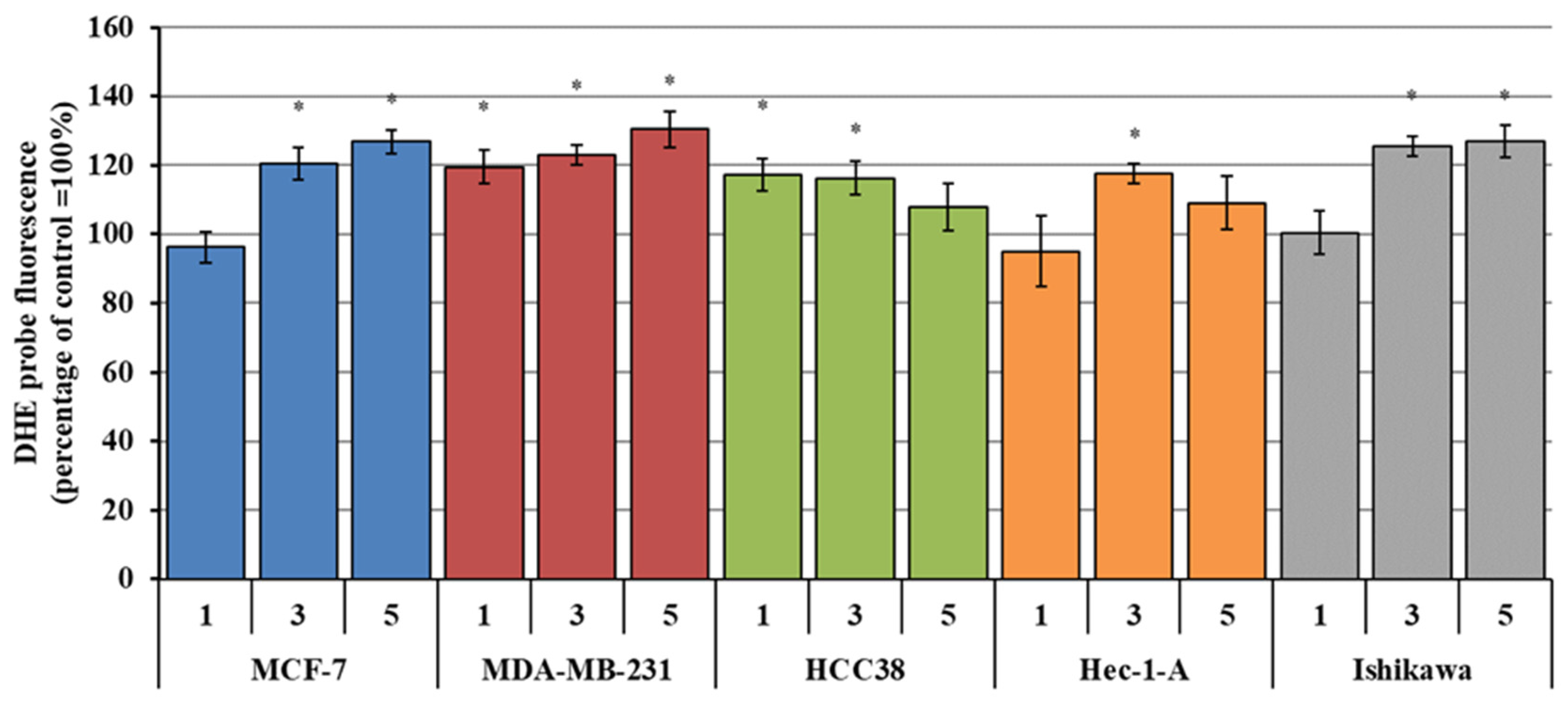
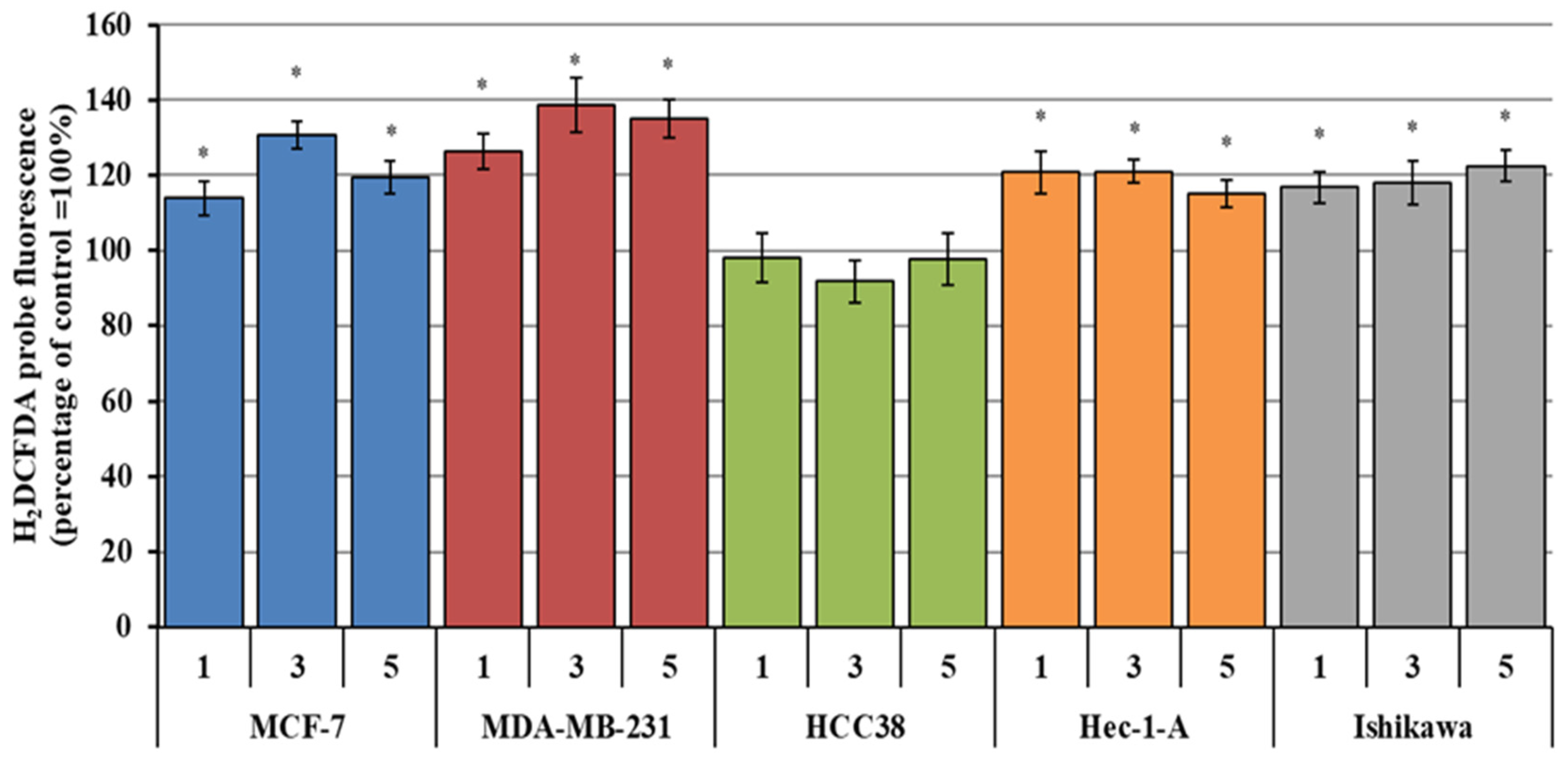
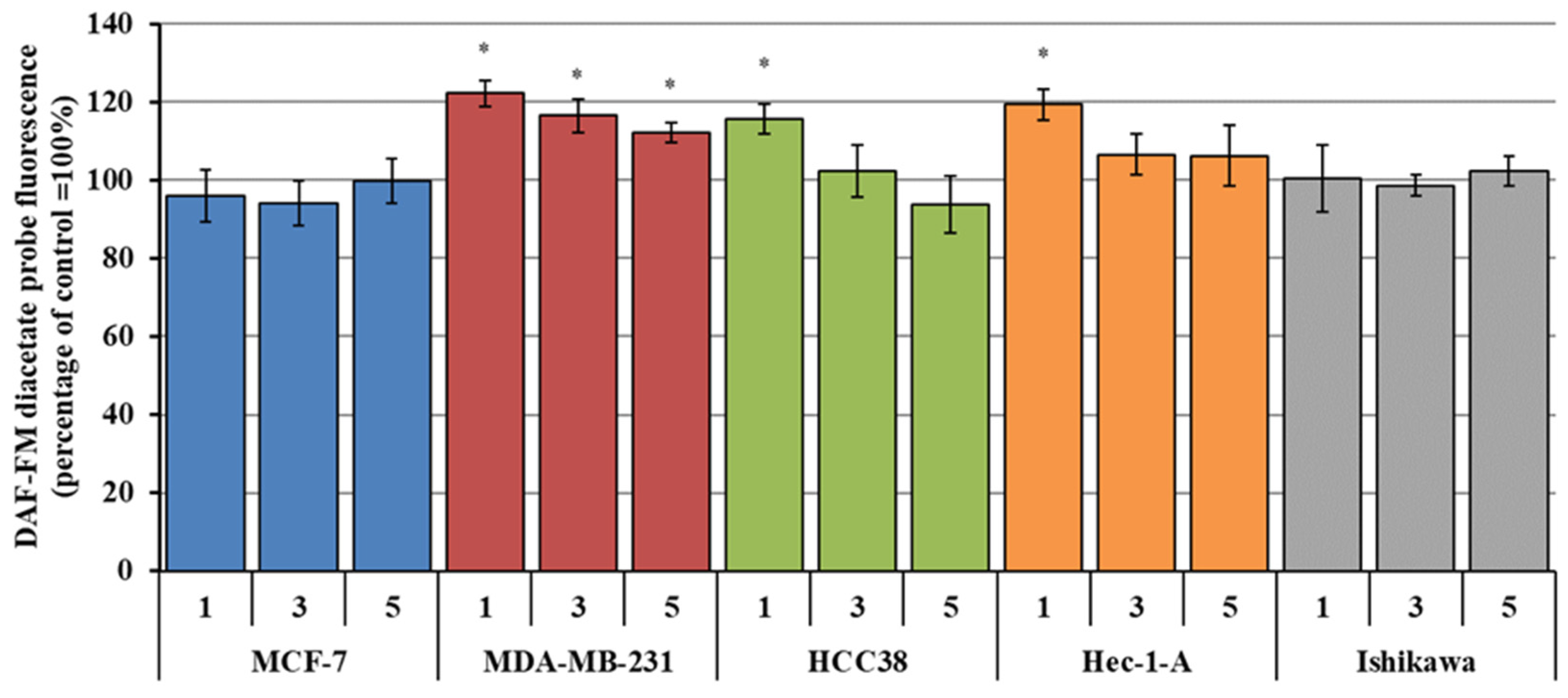
2.1.6. Analysis of the Generation of Reactive Oxygen Species (ROS) and Reactive Nitrogen Species (RNS)
2.1.7. Assessment of the Contribution of Reactive Oxygen Species to the Cytotoxicity of the Cytotoxic Activity of Chromanone Derivatives
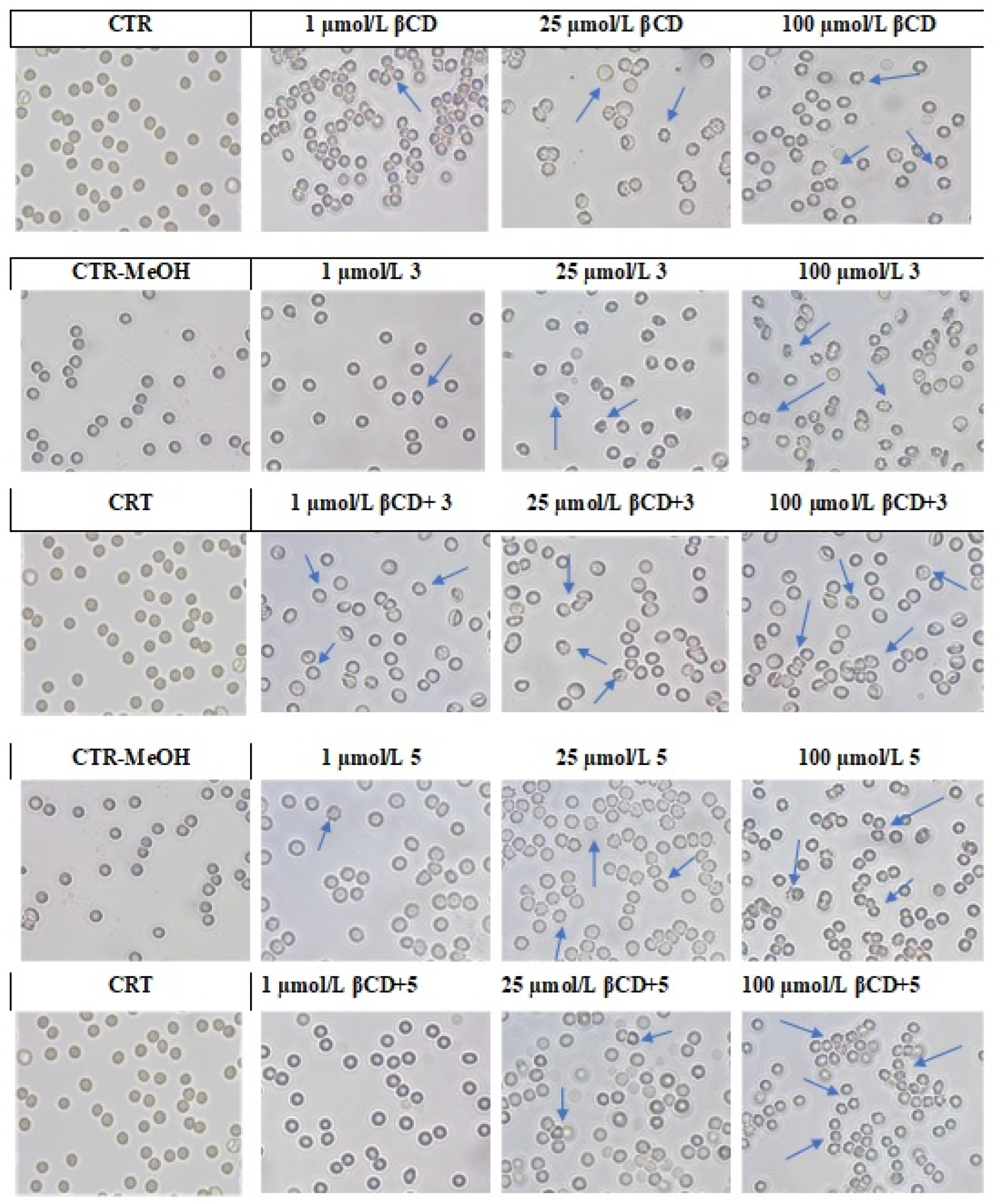
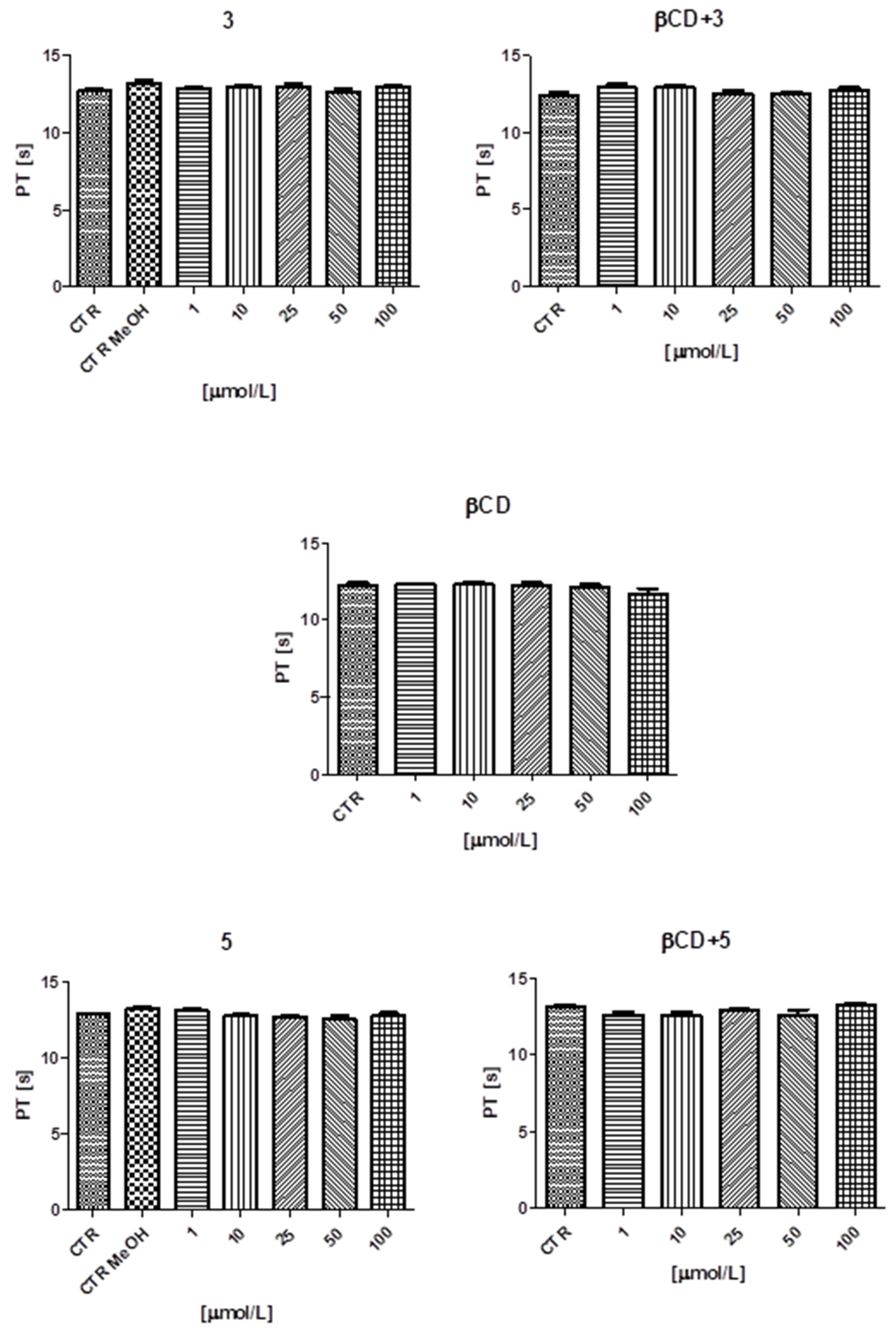
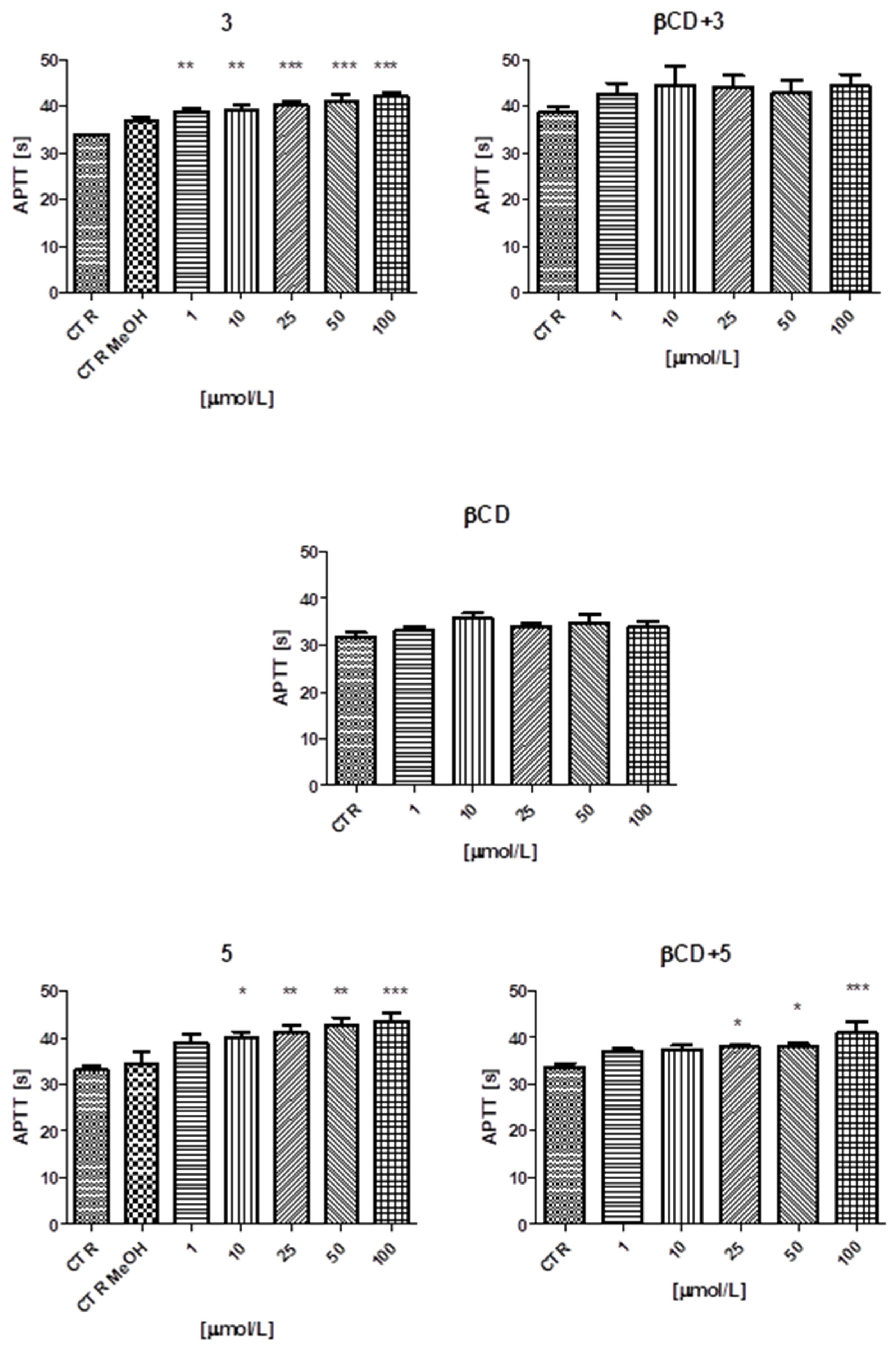
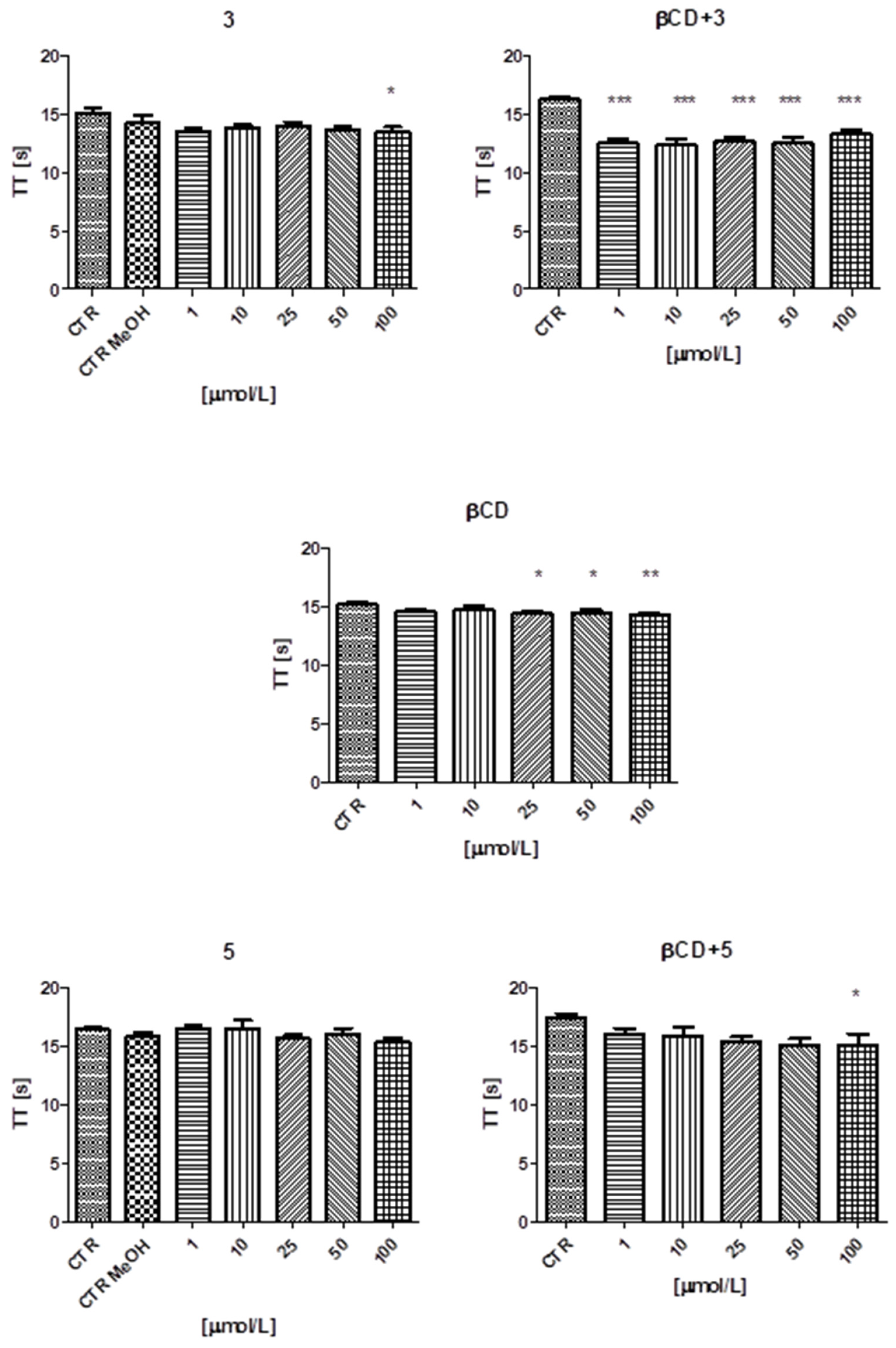
2.1.8. The Results of the Biocompatibility Assessments
2.2. Studies of Physicochemical Measurements
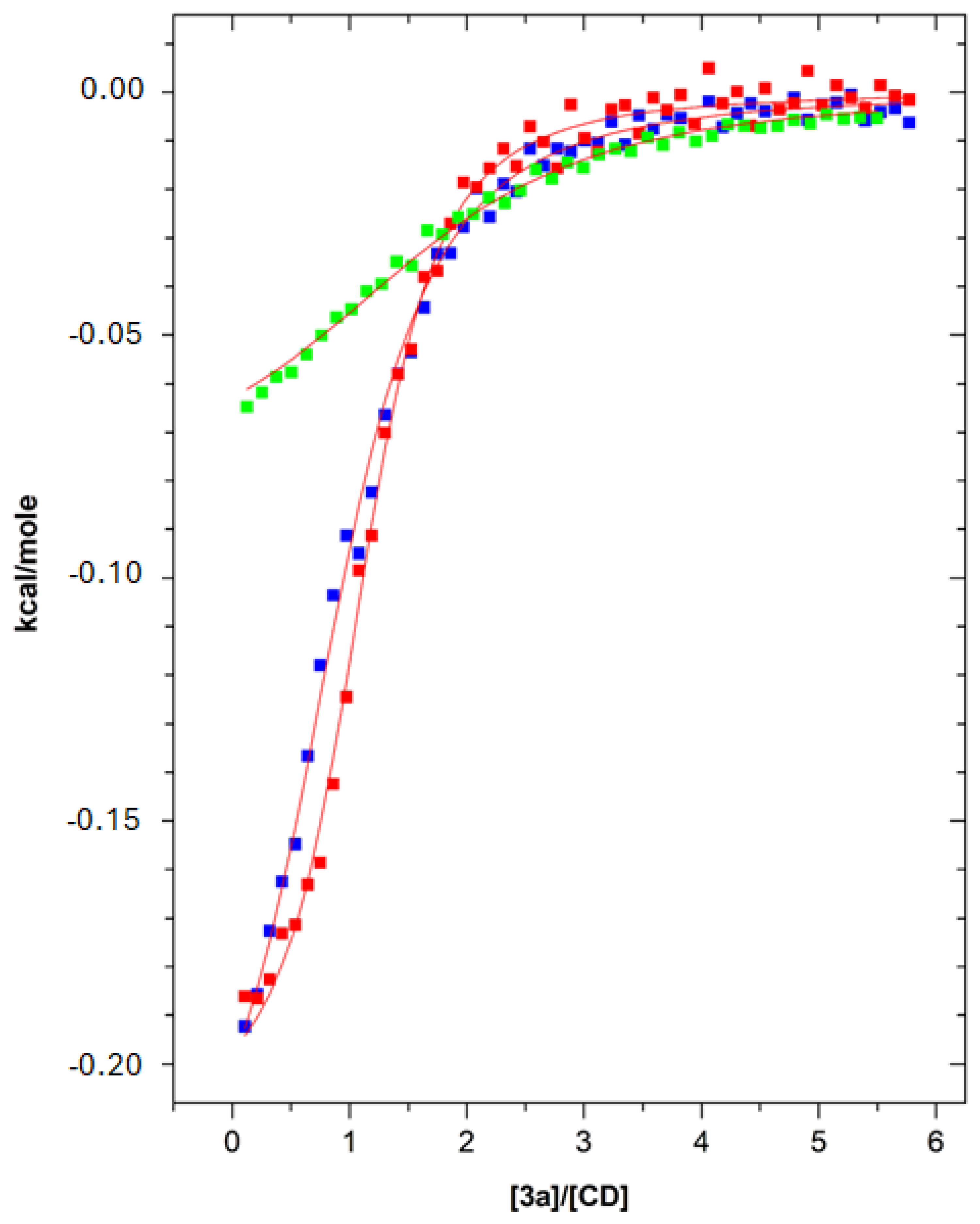
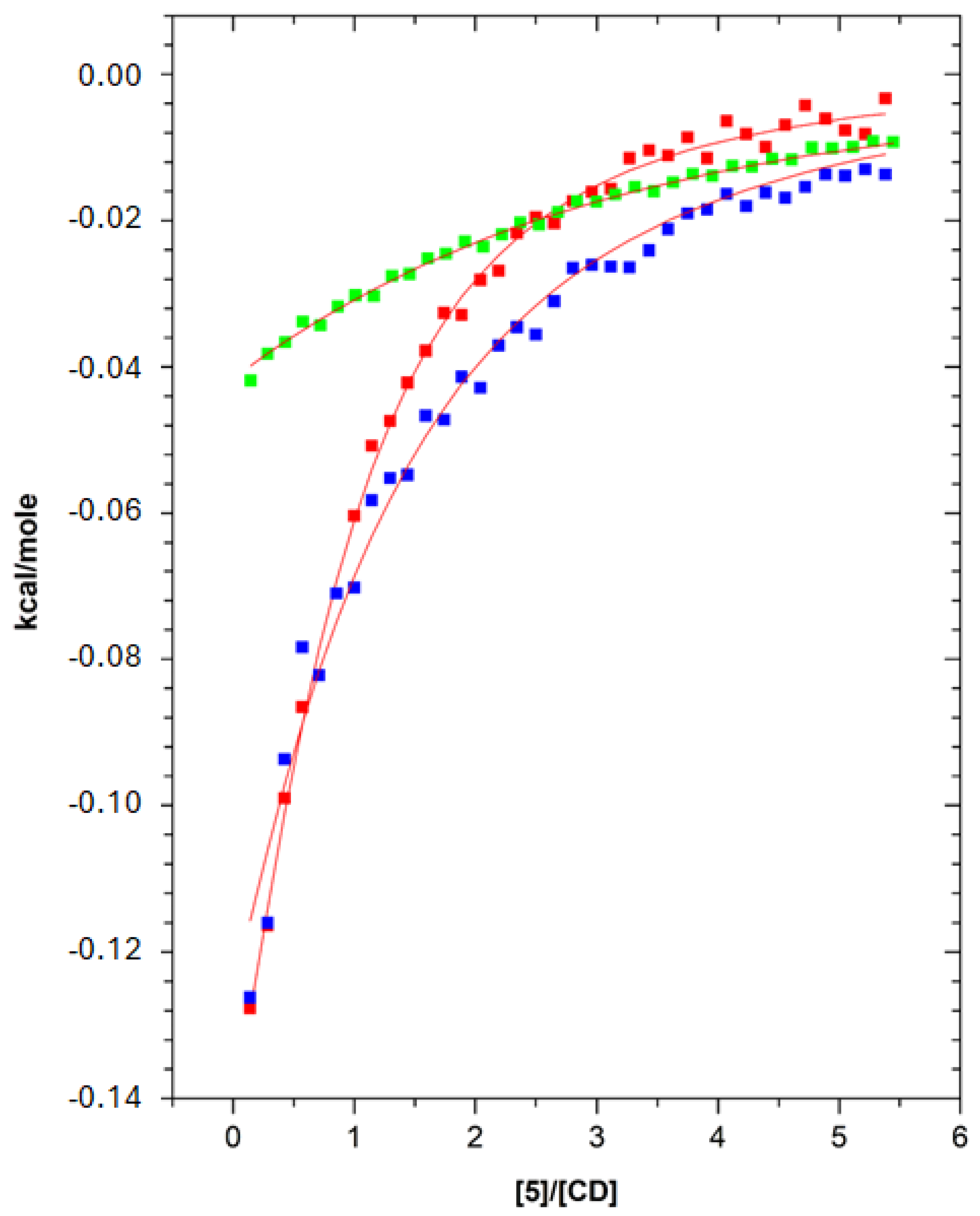
2.2.1. ITC
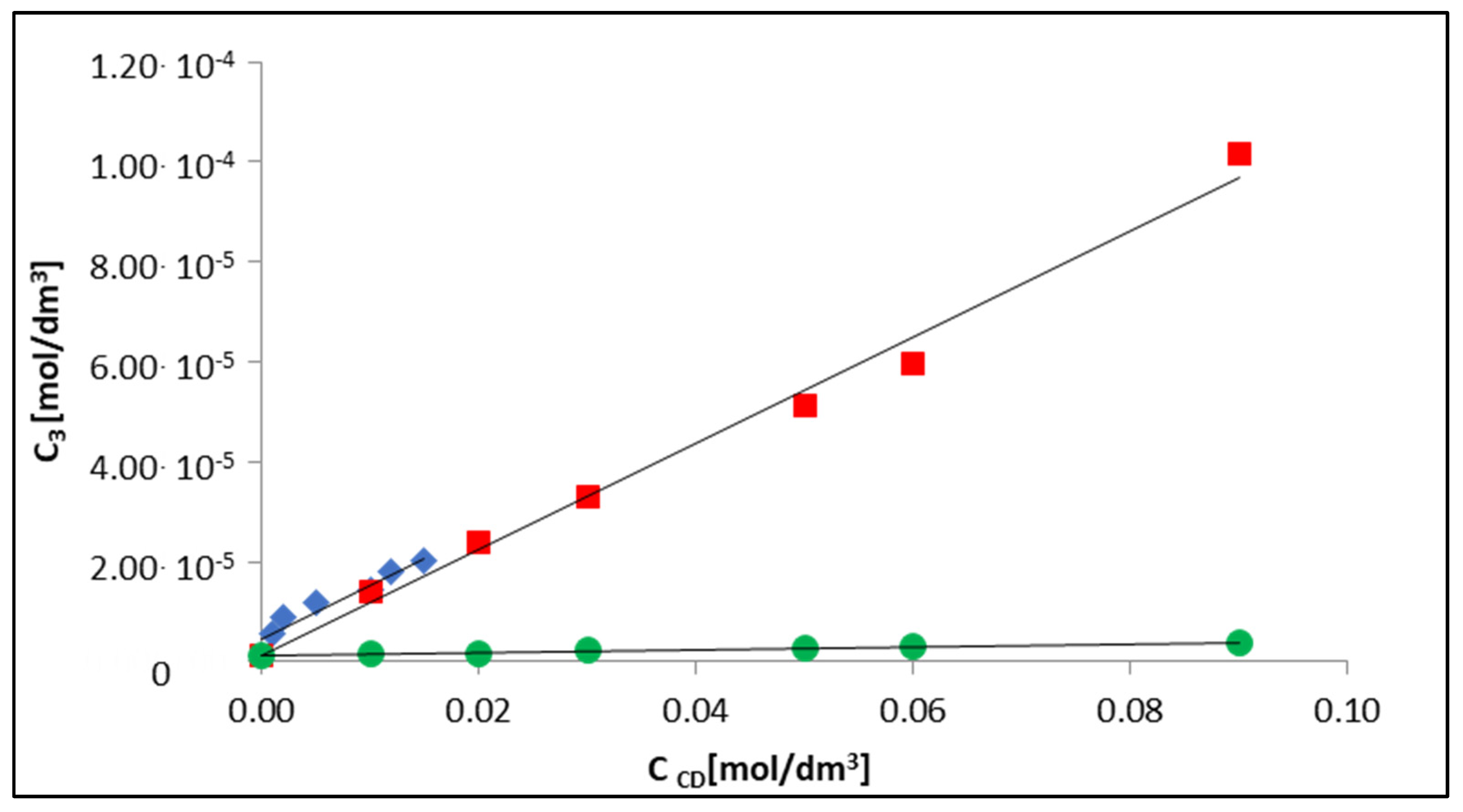
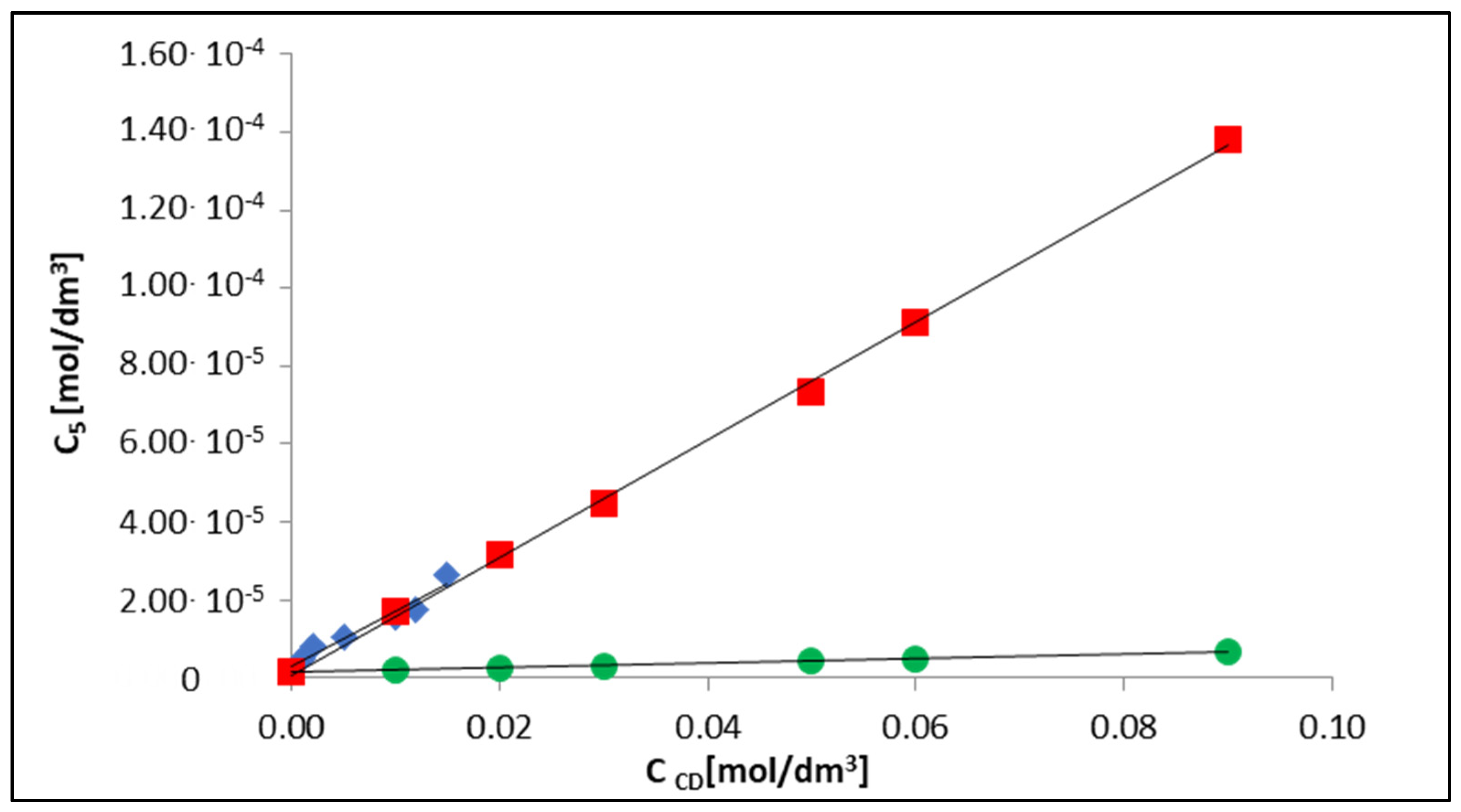
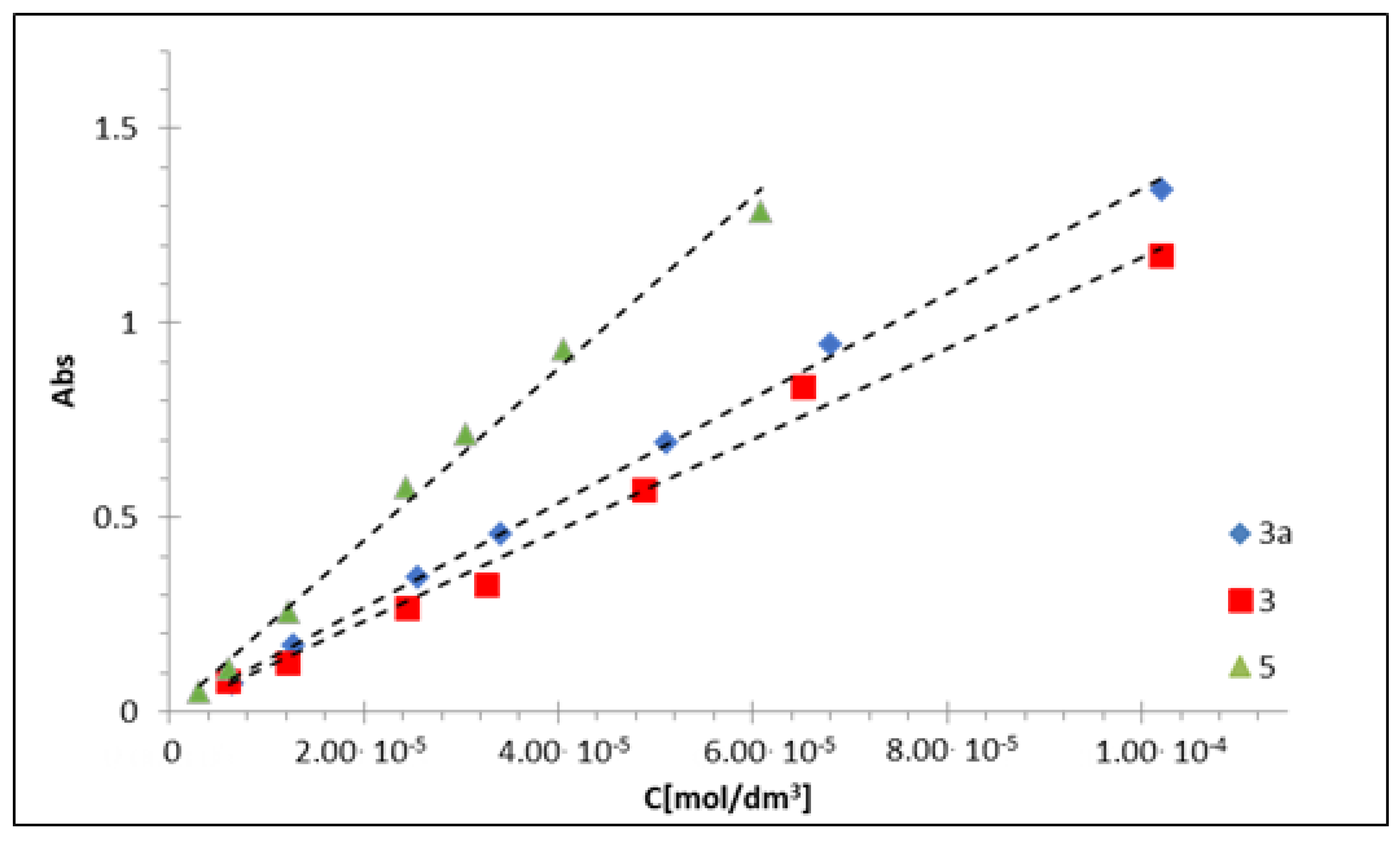
2.2.2. UV–Vis
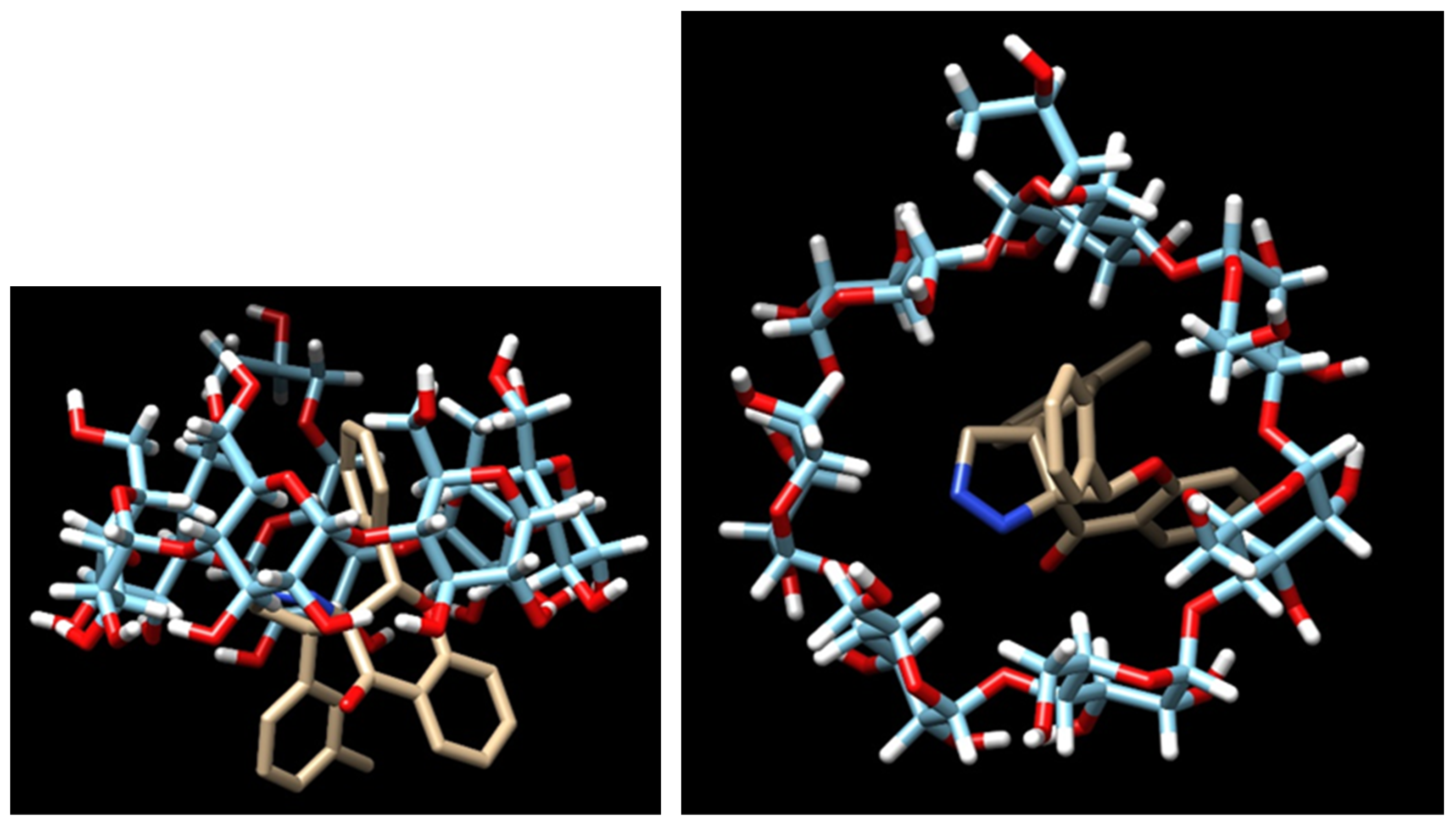
2.3. Docking Studies
3. Materials and Methods
3.1. Biological Assay
3.1.1. Biological Material, Culture and Passage of Cells
3.1.2. Determination of Cell Viability by Metabolic Microplate Spectrophotometric Assay with MTT
3.1.3. Changes in Plasma Membrane Fluidity (Measurement of TMA-DPH and DAUDA Fluorescence Anisotropy)—Lipid Peroxidation
3.1.4. Analysis of the Generation of Reactive Oxygen Species—Measurement of Superoxide Anion
3.1.5. Analysis of the Generation of Reactive Oxygen Species—Measurement of Hydrogen Peroxide
3.1.6. Analysis of the Generation of Reactive Nitrogen Species—Measurement of Nitric Oxide
3.1.7. Assessment of the Contribution of Reactive Oxygen Species to the Cytotoxic Activity of Pyrazoline Derivatives
3.1.8. Analysis of Changes in Transmembrane Mitochondrial Potential (ΔΨm)—JC-1 Method
3.1.9. Determination of the Fraction of Apoptotic and Necrotic Cells by Fluorescence Microscopy (Double-Staining of Cells with Hoechst 33258 and Propidium Iodide Fluorescent Dyes)
3.2. Biocompatibility Assessment
3.2.1. Preparation of Solutions of Tested Compounds to Assess Biocompatibility
3.2.2. Red Blood Cells Lysis Assay
3.2.3. Basic Coagulation Tests: PT, INR, APTT, TT
3.3. Studies of Physicochemical Measurements
3.3.1. Isothermal Titration Calorimetry (ITC)
3.3.2. UV–Vis Spectroscopy
3.4. Molecular Docking Calculation
4. Conclusions and Future Direction
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siegel, R.L.; Giaquinto, A.N.; Jemal, A. Cancer Statistics, 2024. CA Cancer J. Clin. 2024, 74, 12–49. [Google Scholar] [CrossRef] [PubMed]
- Wéber, A.; Vignat, J.; Shah, R.; Morgan, E.; Laversanne, M.; Nagy, P.; Kenessey, I.; Znaor, A. Global Burden of Bladder Cancer Mortality in 2020 and 2040 According to GLOBOCAN Estimates. World J. Urol. 2024, 42, 237. [Google Scholar] [CrossRef] [PubMed]
- Kerru, N.; Gummidi, L.; Maddila, S.; Gangu, K.K.; Jonnalagadda, S.B. A Review on Recent Advances in Nitrogen-Containing Molecules and Their Biological Applications. Molecules 2020, 25, 1909. [Google Scholar] [CrossRef]
- Sidhu, J.S.; Singla, R.; Mayank; Jaitak, V. Indole Derivatives as Anticancer Agents for Breast Cancer Therapy: A Review. Anti-Cancer Agents Med. Chem. 2015, 16, 160–173. [Google Scholar] [CrossRef]
- Jicsinszky, L.; Fenyvesi, E.; Hashimoto, H.; Ueno, A. Chapter 4. Cyclodextrin derivatives. Cyclodextrins. In Comprehensive Supramolecular Chemistry; Szejtli, J., Osa, T., Eds.; Pergamon: Oxford, UK, 1996; pp. 57–188. [Google Scholar]
- Loftsson, T.; Duchêne, D. Cyclodextrins and Their Pharmaceutical Applications. Int. J. Pharm. 2007, 329, 1–11. [Google Scholar] [CrossRef]
- Crini, G. The Contribution of Franz Schardinger to Cyclodextrins: A Tribute on the Occasion of the Centenary of His Death. J. Incl. Phenom. Macrocycl. Chem. 2020, 97, 19–28. [Google Scholar] [CrossRef]
- French, D.; Pulley, A.O.; Effenberger, J.A.; Rougvie, M.A.; Abdullah, M. Studies on the Schardinger Dextrins: XII. The Molecular Size and Structure of the δ-, ϵ-, ζ-, and η-Dextrins. Arch. Biochem. Biophys. 1965, 111, 153–160. [Google Scholar] [CrossRef]
- Freudenberg, K.; Cramer, F. Notizen: Die Konstitution Der Schardinger-Dextrine α, β Und γ. Z. Naturforschung B 1948, 3, 464–466. [Google Scholar] [CrossRef]
- Ueda, H. Physicochemical Properties and Complex Formation Abilities of Large-Ring Cyclodextrins. J. Incl. Phenom. 2002, 44, 53–56. [Google Scholar] [CrossRef]
- Sherje, A.P.; Dravyakar, B.R.; Kadam, D.; Jadhav, M. Cyclodextrin-Based Nanosponges: A Critical Review. Carbohydr. Polym. 2017, 173, 37–49. [Google Scholar] [CrossRef]
- Jambhekar, S.S.; Breen, P. Cyclodextrins in Pharmaceutical Formulations I: Structure and Physicochemical Properties, Formation of Complexes, and Types of Complex. Drug Discov. Today 2016, 21, 356–362. [Google Scholar] [CrossRef] [PubMed]
- Rassu, G.; Sorrenti, M.; Catenacci, L.; Pavan, B.; Ferraro, L.; Gavini, E.; Bonferoni, M.C.; Giunchedi, P.; Dalpiaz, A. Versatile Nasal Application of Cyclodextrins: Excipients and/or Actives? Pharmaceutics 2021, 13, 1180. [Google Scholar] [CrossRef]
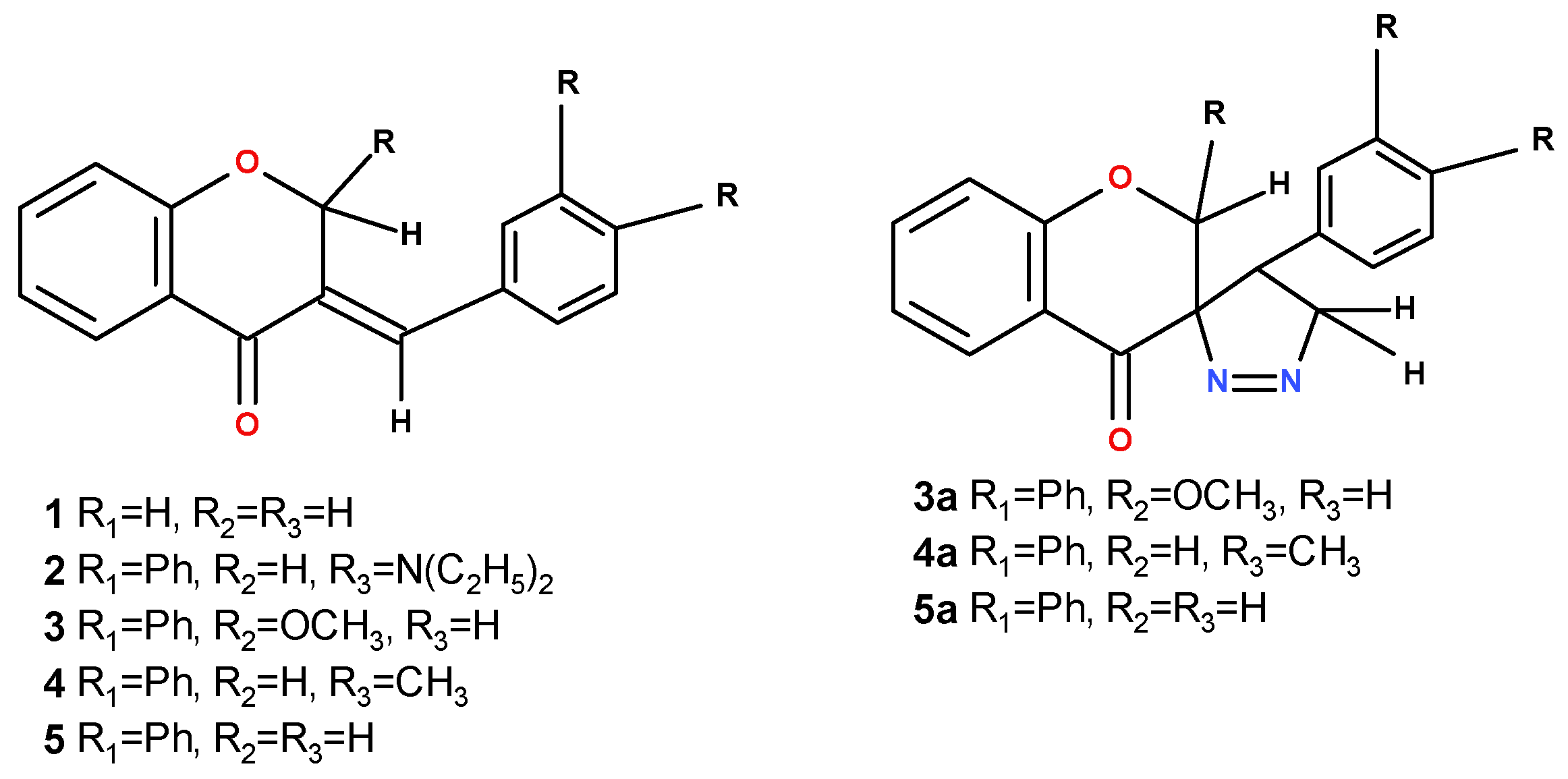
- Budzisz, E.; Paneth, P.; Geromino, I.; Muzioł, T.; Rozalski, M.; Krajewska, U.; Pipiak, P.; Ponczek, M.B.; Małecka, M.; Kupcewicz, B. The Cytotoxic Effect of Spiroflavanone Derivatives, Their Binding Ability to Human Serum Albumin (HSA) and a DFT Study on the Mechanism of Their Synthesis. J. Mol. Struct. 2017, 1137, 267–276. [Google Scholar] [CrossRef]
- Lévai, A.; Simon, A.; Jenei, A.; Kálmán, G.; Jekõ, J.; Tóth, G. Synthesis of Spiro-1-Pyrazolines by the Reaction of Exocyclic α,β,γ,δ-Unsaturated Ketones with Diazomethane. Arkivoc 2009, 2009, 161–172. [Google Scholar] [CrossRef]
- Adamus-Grabicka, A.A.; Markowicz-Piasecka, M.; Cieślak, M.; Królewska-Golińska, K.; Hikisz, P.; Kusz, J.; Małecka, M.; Budzisz, E. Biological Evaluation of 3-Benzylidenechromanones and Their Spiropyrazolines-Based Analogues. Molecules 2020, 25, 1613. [Google Scholar] [CrossRef]
- Adamus-Grabicka, A.A.; Markowicz-Piasecka, M.; Ponczek, M.B.; Kusz, J.; Małecka, M.; Krajewska, U.; Budzisz, E. Interaction of Arylidenechromanone/Flavanone Derivatives with Biological Macromolecules Studied as Human Serum Albumin Binding, Cytotoxic Effect, Biocompatibility Towards Red Blood Cells. Molecules 2018, 23, 3172. [Google Scholar] [CrossRef]
- Lévai, A. Synthesis of Pyrazolines by the Reactions Ofα,β-Enones with Diazomethane and Hydrazines (Review). Chem. Heterocycl. Compd. 1997, 33, 647–659. [Google Scholar] [CrossRef]
- Kupcewicz, B.; Małecka, M.; Zapadka, M.; Krajewska, U.; Rozalski, M.; Budzisz, E. Quantitative Relationships between Structure and Cytotoxic Activity of Flavonoid Derivatives. An Application of Hirshfeld Surface Derived Descriptors. Bioorg. Med. Chem. Lett. 2016, 26, 3336–3341. [Google Scholar] [CrossRef] [PubMed]
- Adamus-Grabicka, A.; Daśko, M.; Hikisz, P.; Kusz, J.; Małecka, M.; Budzisz, E. Biochemical, Structural Analysis, and Docking Studies of Spiropyrazoline Derivatives. Int. J. Mol. Sci. 2022, 23, 6061. [Google Scholar] [CrossRef]
- Chiang, F.-F.; Huang, S.-C.; Yu, P.-T.; Chao, T.-H.; Huang, Y.-C. Oxidative Stress Induced by Chemotherapy: Evaluation of Glutathione and Its Related Antioxidant Enzyme Dynamics in Patients with Colorectal Cancer. Nutrients 2023, 15, 5104. [Google Scholar] [CrossRef]
- Kasapović, J.; Pejić, S.; Stojiljković, V.; Todorović, A.; Radošević-Jelić, L.; Saičić, Z.S.; Pajović, S.B. Antioxidant Status and Lipid Peroxidation in the Blood of Breast Cancer Patients of Different Ages after Chemotherapy with 5-Fluorouracil, Doxorubicin and Cyclophosphamide. Clin. Biochem. 2010, 43, 1287–1293. [Google Scholar] [CrossRef]
- Evaluation of Malondialdehyde, Homocysteine and Antioxidant Influence Chemotherapy in Breast Cancer Patients|Semantic Scholar. Available online: https://www.semanticscholar.org/paper/EVALUATION-OF-MALONDIALDEHYDE%2C-HOMOCYSTEINE-AND-Hamza-Muhsin/802d46a66fe8aadc2eb526d7bfc62e7d684f93d5 (accessed on 23 July 2024).
- Xiong, Y.; Xiao, C.; Li, Z.; Yang, X. Engineering Nanomedicine for Glutathione Depletion-Augmented Cancer Therapy. Chem. Soc. Rev. 2021, 50, 6013–6041. [Google Scholar] [CrossRef]
- Tormos, C.; Javierchaves, F.; Garcia, M.; Garrido, F.; Jover, R.; Oconnor, J.; Iradi, A.; Oltra, A.; Oliva, M.; Saez, G. Role of Glutathione in the Induction of Apoptosis and C-Fos and c-Jun mRNAs by Oxidative Stress in Tumor Cells. Cancer Lett. 2004, 208, 103–113. [Google Scholar] [CrossRef]
- Gana, C.C.; Hanssen, K.M.; Yu, D.M.T.; Flemming, C.L.; Wheatley, M.S.; Conseil, G.; Cole, S.P.C.; Norris, M.D.; Haber, M.; Fletcher, J.I. MRP1 Modulators Synergize with Buthionine Sulfoximine to Exploit Collateral Sensitivity and Selectively Kill MRP1-Expressing Cancer Cells. Biochem. Pharmacol. 2019, 168, 237–248. [Google Scholar] [CrossRef] [PubMed]
- Khan, H.Y.; Zubair, H.; Ullah, M.F.; Ahmad, A.; Hadi, S.M. A Prooxidant Mechanism for the Anticancer and Chemopreventive Properties of Plant Polyphenols. Curr. Drug Targets 2012, 13, 1738–1749. [Google Scholar] [CrossRef]
- Rice-Evans, C.; Miller, N.; Paganga, G. Antioxidant Properties of Phenolic Compounds. Trends Plant Sci. 1997, 2, 152–159. [Google Scholar] [CrossRef]
- Podsiedlik, M.; Markowicz-Piasecka, M.; Sikora, J. Erythrocytes as Model Cells for Biocompatibility Assessment, Cytotoxicity Screening of Xenobiotics and Drug Delivery. Chem.-Biol. Interact. 2020, 332, 109305. [Google Scholar] [CrossRef] [PubMed]
- Biernacka, M.; Ilyich, T.; Zavodnik, I.; Pałecz, B.; Stepniak, A. Studies of the Formation and Stability of Ezetimibe-Cyclodextrin Inclusion Complexes. Int. J. Mol. Sci. 2021, 23, 455. [Google Scholar] [CrossRef]
- Belica-Pacha, S.; Małecka, M.; Daśko, M.; Miłowska, K.; Bryszewska, M.; Budryn, G.; Oracz, J.; Pałecz, B. The Interaction of Heptakis (2,6-Di-O-Methyl)-β-Cyclodextrin with Mianserin Hydrochloride and Its Influence on the Drug Toxicity. Int. J. Mol. Sci. 2021, 22, 9419. [Google Scholar] [CrossRef]
- Belica-Pacha, S.; Daśko, M.; Buko, V.; Zavodnik, I.; Miłowska, K.; Bryszewska, M. Thermodynamic Studies of Interactions between Sertraline Hydrochloride and Randomly Methylated β-Cyclodextrin Molecules Supported by Circular Dichroism Spectroscopy and Molecular Docking Results. Int. J. Mol. Sci. 2021, 22, 12357. [Google Scholar] [CrossRef]
- Wszelaka-Rylik, M.; Gierycz, P. Isothermal Titration Calorimetry (ITC) Study of Natural Cyclodextrins Inclusion Complexes with Tropane Alkaloids. J. Therm. Anal. Calorim. 2015, 121, 1359–1364. [Google Scholar] [CrossRef]
- Mercader-Ros, M.T.; Lucas-Abellán, C.; Fortea, M.I.; Gabaldón, J.A.; Núñez-Delicado, E. Effect of HP-β-Cyclodextrins Complexation on the Antioxidant Activity of Flavonols. Food Chem. 2010, 118, 769–773. [Google Scholar] [CrossRef]
- Higuchi, T.; Connors, A. Phase Solubility Techniques. Adv. Anal. Chem. Instrum. 1965, 4, 117–212. [Google Scholar]
- Tao, Y.; Han, Y.; Dong, S.; Fan, X.; Wang, T.; Yan, X. Preparation, Solubilization and In Vitro Anti-Tumour Effect of Water-Soluble Betulinic Acid/Oligo(Polylvinylamino) Bridged Bis(β-Cyclodextrin)s Complexes. Chem. Sci. Int. J. 2017, 21, 1–15. [Google Scholar] [CrossRef]
- Harata, K.; Rao, C.T.; Pitha, J. Crystal Structure of 6-O-[(R)-2-Hydroxypropyl]Cyclomaltoheptaose and 6-O-[(S)-2-Hydroxypropyl]Cyclomaltoheptaose. Carbohydr. Res. 1993, 247, 83–98. [Google Scholar] [CrossRef]
- Chacko, K.K.; Saenger, W. Topography of Cyclodextrin Inclusion Complexes. 15. Crystal and Molecular Structure of the Cyclohexaamylose-7.57 Water Complex, Form III. Four- and Six-Membered Circular Hydrogen Bonds. J. Am. Chem. Soc. 1981, 103, 1708–1715. [Google Scholar] [CrossRef]
- Steiner, T.; Koellner, G. Crystalline. Beta.-Cyclodextrin Hydrate at Various Humidities: Fast, Continuous, and Reversible Dehydration Studied by X-ray Diffraction. J. Am. Chem. Soc. 1994, 116, 5122–5128. [Google Scholar] [CrossRef]
- Harata, K.; Rao, C.T.; Pitha, J.; Fukunaga, K.; Uekama, K. Crystal Structure of 2-O-[(S)-2-Hydroxypropyl]Cyclomaltoheptaose. Carbohydr. Res. 1991, 222, 37–45. [Google Scholar] [CrossRef]
- Benov, L.; Sztejnberg, L.; Fridovich, I. Critical Evaluation of the Use of Hydroethidine as a Measure of Superoxide Anion Radical. Free Radic. Biol. Med. 1998, 25, 826–831. [Google Scholar] [CrossRef]
- McLennan, H.R.; Esposti, M.D. The Contribution of Mitochondrial Respiratory Complexes to the Production of Reactive Oxygen Species. J. Bioenerg. Biomembr. 2000, 32, 153–162. [Google Scholar] [CrossRef]
- Balcerczyk, A.; Soszynski, M.; Bartosz, G. On the Specificity of 4-Amino-5-Methylamino-2′,7′-Difluorofluorescein as a Probe for Nitric Oxide. Free Radic. Biol. Med. 2005, 39, 327–335. [Google Scholar] [CrossRef] [PubMed]
- Sakamuru, S.; Li, X.; Attene-Ramos, M.S.; Huang, R.; Lu, J.; Shou, L.; Shen, M.; Tice, R.R.; Austin, C.P.; Xia, M. Application of a Homogenous Membrane Potential Assay to Assess Mitochondrial Function. Physiol. Genom. 2012, 44, 495–503. Available online: https://journals.physiology.org/doi/epdf/10.1152/physiolgenomics.00161.2011 (accessed on 21 May 2024). [CrossRef] [PubMed]
- Markowicz-Piasecka, M.; Huttunen, K.M.; Mikiciuk-Olasik, E.; Sikora, J. Biocompatible Sulfenamide and Sulfonamide Derivatives of Metformin Can Exert Beneficial Effects on Plasma Haemostasis. Chem. Biol. Interact. 2018, 280, 15–27. [Google Scholar] [CrossRef]
- Markowicz-Piasecka, M.; Sadkowska, A.; Podsiedlik, M.; Mikiciuk-Olasik, E.; Sikora, J. Generation 2 (G2)–Generation 4 (G4) PAMAM Dendrimers Disrupt Key Plasma Coagulation Parameters. Toxicol. Vitr. 2019, 59, 87–99. [Google Scholar] [CrossRef] [PubMed]
- Origin(Pro), Version 7. OriginLab Corporation, Northampton, MA, USA. Available online: https://structbio.vanderbilt.edu/wetlab/private/ITC_Data_Analysis_in_Origin_Tutorial_Guide.pdf (accessed on 10 June 2024).
- Eberhardt, J.; Santos-Martins, D.; Tillack, A.F.; Forli, S. AutoDock Vina 1.2.0: New Docking Methods, Expanded Force Field, and Python Bindings. J. Chem. Inf. Model 2021, 61, 3891–3898. [Google Scholar] [CrossRef]
- Goddard, T.D.; Huang, C.C.; Meng, E.C.; Pettersen, E.F.; Couch, G.S.; Morris, J.H.; Ferrin, T.E. UCSF ChimeraX: Meeting Modern Challenges in Visualization and Analysis. Protein Sci. 2018, 27, 14–25. [Google Scholar] [CrossRef]
- Wang, J.; Wang, W.; Kollman, P.A.; Case, D.A. Automatic Atom Type and Bond Type Perception in Molecular Mechanical Calculations. J. Mol. Graph. Model. 2006, 25, 247–260. [Google Scholar] [CrossRef]
- Dutra, J.D.L.; Filho, M.A.M.; Rocha, G.B.; Simas, A.M.; Freire, R.O. RM1 Semiempirical Quantum Chemistry: Parameters for Trivalent Lanthanum, Cerium and Praseodymium. PLoS ONE 2015, 10, e0124372. [Google Scholar] [CrossRef]
- Gaussian 16|Gaussian.Com. Available online: https://gaussian.com/gaussian16/ (accessed on 22 May 2024).
- Dhurve, P.; Tripathi, A.; Gidwani, B.; Vyas, A. Investigating the Phase-Solubility and Compatibility Study of Anticancer Drug Complexed with β-Cyclodextrin and HP–β-Cyclodextrin. Int. J. Adv. Pharm. Sci. 2018, 9, 69–74. [Google Scholar] [CrossRef][Green Version]




| Cell Line | Cytotoxic Effect of Chromanone Analogues Condensed with Pyrazolines and Reference Compounds Cisplatin, IC50 (µM) | ||||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 3a | 4 | 5 | Cisplatin | |
| MCF-7 | 10.2 ± 0.9 | 121.5 ± 6.7 | 16.4 ± 2.3 | 84.2 ± 2.2 | 53.4 ± 4.1 | 25.1 ± 4.2 | 8.1 ± 1.8 |
| MDA-MB-231 | 12.6 ± 1.1 | >200 | 15.2 ± 3.1 | >120 | >120 | 23.3 ± 1.4 | 19.2 ± 1.3 |
| HCC38 | 15.7 ± 0.8 | >200 | 20.9 ± 1.5 | >120 | 93.2 ± 2.8 | 25.6 ± 0.9 | 3.4 ± 0.8 |
| Ishikawa | 10.2 ± 1.8 | >200 | 15.2 ± 1.6 | 68.5 ± 4.6 | 48.9 ± 6.1 | 18.6 ± 4.4 | 14.0 ± 1.4 |
| Hec-1-A | 18.5 ± 1.2 | >200 | 26.9 ± 2.3 | 67.2 ± 2.5 | 44.6 ± 4.5 | 35.9 ± 2.4 | 67.5 ± 5.9 |
| HMEC-1 | 21.2 ± 3.1 | - | 24.1 ± 1.3 | - | - | 19.7 ± 3.7 | 1.7 ± 1.2 |
| Cell Line | Cytotoxic Effect of Chromanone Analogues Condensed with Pyrazolines Incorporated in Cyclodextrins and Reference Compounds Cyclodextrin, IC50 (µM) | |||
|---|---|---|---|---|
| 3 + β-CD | 3a + β-CD | 5 + β-CD | β-CD | |
| MCF-7 | 118.9 ± 7.1 | >120 | 115.6 ± 4.7 | >120 |
| MDA-MB-231 | >120 | >120 | >120 | >120 |
| HCC38 | 101 ± 2.8 | 104 ± 3.9 | 109 ± 1.8 | >120 |
| Ishikawa | 116.1 ± 0.9 | 118.9 ± 4.6 | 111.5 ± 6.8 | >120 |
| Hec-1-A | >120 | >120 | >120 | >120 |
| HMEC-1 | 111.5 ± 4.3 | >120 | 109.9 ± 5.5 | >120 |
| Cell line | Cytotoxic Effect of Chromanone Analogues Condensed with Pyrazolines and Reference Compounds Cisplatin, IC50 (µM) | |||||
|---|---|---|---|---|---|---|
| 1 + NAC | 1 + Trolox | 3 + NAC | 3 + Trolox | 5 +NAC | 5 + Trolox | |
| MCF-7 | 116.3 ± 1.9 | 62.2 ± 4.9 | 61.9 ± 4.7 | 67.7 ± 2.4 | 30.1 ± 5.2 | 92.7 ± 6.3 |
| MDA-MB-231 | 119.6 ± 4.2 | 41.3 ± 1.4 | 108.5 ± 6.5 | 116.9 ± 4.9 | 46.9 ± 4.8 | 99.3 ± 6.7 |
| HCC38 | 54.3 ± 2.7 | 31.1 ± 5.9 | 31.9 ± 1.9 | 41.1 ± 1.2 | 31.8 ± 4.1 | 49.9 ± 2.2 |
| Ishikawa | 83.0 ± 1.4 | 49.6 ± 4.1 | 25.8 ± 2.5 | 52.2 ± 2.9 | 25.5 ± 1.1 | 54.4 ± 2.2 |
| Hec-1-A | 81.5 ± 0.9 | 41.1 ± 2.5 | 113.9 ± 2.3 | 110.1 ± 6.9 | 50.0 ± 7.1 | 97.9 ± 1.9 |
| 3 | ΔH [J mol−1] | ΔG [J mol−1] | ΔS [J mol−1K−1] | n | K |
|---|---|---|---|---|---|
| α-cyclodextrin | −385 ± 46 | −19,188.6 | 63.1 | 0.90 ± 0.13 | 2.30 × 103 ± 180 |
| β-cyclodextrin | −1036 ± 88 | −20,353.7 | 64.8 | 0.99 ± 0.11 | 3.68 × 103 ± 230 |
| HP-β-cyclodextrin | −983 ± 80 | −21,902.2 | 70.2 | 1.03 ± 0.10 | 6.88 × 103 ± 430 |
| 3a | ΔH [J mol−1] | ΔG [J mol−1] | ΔS [J mol−1K−1] | n | K |
|---|---|---|---|---|---|
| α-cyclodextrin | −280 ± 88 | −18,145.5 | 59.9 | 0.85 ± 0.13 | 1.51 × 103 ± 130 |
| β-cyclodextrin | −846 ± 71 | −19,385.4 | 62.2 | 0.92 ± 0.11 | 2.49 × 103 ± 200 |
| HP-β-cyclodextrin | −773 ± 59 | −21,420.7 | 69.3 | 0.98 ± 0.09 | 5.66 × 103 ± 390 |
| 5 | ΔH [J mol−1] | ΔG [J mol−1] | ΔS [J mol−1K−1] | n | K |
|---|---|---|---|---|---|
| α-cyclodextrin | −205 ± 31 | −17,940.2 | 59.5 | 0.83 ± 0.17 | 1.39 × 103 ± 120 |
| β-cyclodextrin | −172 ± 50 | −20,328.0 | 62.5 | 0.93 ± 0.11 | 2.32 × 103 ± 220 |
| HP-β-cyclodextrin | −496 ± 63 | −21,172.4 | 69.3 | 0.93 ± 0.10 | 5.12 × 103 ± 410 |
| Solubility in H2O [mol/dm3] | α-CD | β-CD | HP-β-CD | |
|---|---|---|---|---|
| 3 | 1.29 × 10−6 | 2.8 | 15.6 | 132.2 |
| 3a | 1.55 × 10−6 | 3.1 | 6.2 | 28.4 |
| 5 | 1.50 × 10−6 | 4.5 | 17.5 | 92.2 |
| α-CD (Refocode: BANXUJ [38]) | β-CD (Refocode: BCDEXD05 [39]) | KOYYUS [40] | LEDROB [38] | LEDRUH [38] | |
|---|---|---|---|---|---|
| 3 | −4.7 | −6.5 | −6.7 | −6.8 | −6.9 |
| 4 | −4.7 | −6.4 | −6.6 | −6.3 | −6.7 |
| 5 | −4.7 | −6.4 | −6.5 | −6.6 | −6.7 |
| 3a | −5.3 | −6.9 | −6.9 | −7.0 | −7.0 |
| 4a | −5.2 | −7.0 | −7.1 | −7.2 | −7.1 |
| 5a | −5.2 | −6.8 | −6.9 | −7.0 | −7.0 |
| Ligand | λMax (nm) | ε | R2 |
|---|---|---|---|
| 3 | 257 | 11,976 | 0.9968 |
| 3a | 262.8 | 13,446 | 0.9983 |
| 5 | 303.4 | 22,147 | 0.9975 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adamus-Grabicka, A.A.; Hikisz, P.; Stepniak, A.; Malecka, M.; Paneth, P.; Sikora, J.; Budzisz, E. Molecular Pro-Apoptotic Activities of Flavanone Derivatives in Cyclodextrin Complexes: New Implications for Anticancer Therapy. Int. J. Mol. Sci. 2024, 25, 8488. https://doi.org/10.3390/ijms25158488
Adamus-Grabicka AA, Hikisz P, Stepniak A, Malecka M, Paneth P, Sikora J, Budzisz E. Molecular Pro-Apoptotic Activities of Flavanone Derivatives in Cyclodextrin Complexes: New Implications for Anticancer Therapy. International Journal of Molecular Sciences. 2024; 25(15):8488. https://doi.org/10.3390/ijms25158488
Chicago/Turabian StyleAdamus-Grabicka, Angelika A., Pawel Hikisz, Artur Stepniak, Magdalena Malecka, Piotr Paneth, Joanna Sikora, and Elzbieta Budzisz. 2024. "Molecular Pro-Apoptotic Activities of Flavanone Derivatives in Cyclodextrin Complexes: New Implications for Anticancer Therapy" International Journal of Molecular Sciences 25, no. 15: 8488. https://doi.org/10.3390/ijms25158488
APA StyleAdamus-Grabicka, A. A., Hikisz, P., Stepniak, A., Malecka, M., Paneth, P., Sikora, J., & Budzisz, E. (2024). Molecular Pro-Apoptotic Activities of Flavanone Derivatives in Cyclodextrin Complexes: New Implications for Anticancer Therapy. International Journal of Molecular Sciences, 25(15), 8488. https://doi.org/10.3390/ijms25158488








