Loss of Heterozygosity and Mutations in the RAS-ERK Pathway Genes in Tumor Cells of Various Loci in Multiple Myeloma
Abstract
:1. Introduction
2. Results
3. Discussion
4. Materials and Methods
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bolli, N.; Avet-Loiseau, H.; Wedge, D.C.; Van Loo, P.; Alexandrov, L.B.; Martincorena, I.; Dawson, K.J.; Iorio, F.; Nik-Zainal, S.; Bignell, G.R.; et al. Heterogeneity of genomic evolution and mutational profiles in multiple myeloma. Nat. Commun. 2014, 5, 2997. [Google Scholar] [CrossRef]
- Melchor, L.; Jones, J.R.; Lenive, O.; Peterson, E.A.; Brioli, A.; Murison, A.; Wardell, C.P.; Kaiser, M.F.; Proszek, P.; Boyle, E.M.; et al. Spatiotemporal Analysis of Intraclonal Heterogeneity in Multiple Myeloma: Unravelling the Impact of Treatment and the Propagating Capacity of Subclones Using Whole Exome Sequencing. Blood 2015, 126, 371. [Google Scholar] [CrossRef]
- Rasche, L.; Chavan, S.S.; Stephens, O.W.; Patel, P.H.; Tytarenko, R.; Ashby, C.; Bauer, M.; Stein, C.; Deshpande, S.; Wardell, C.; et al. Spatial genomic heterogeneity in multiple myeloma revealed by multi-region sequencing. Nat. Commun. 2017, 8, 268. [Google Scholar] [CrossRef]
- Soloveva, M.; Solovev, M.; Nikulina, E.; Risinskaya, N.; Biderman, B.; Yakutik, I.; Obukhova, T.; Mendeleeva, L. Loss of Heterozygosity in the Circulating Tumor DNA and CD138+ Bone Marrow Cells in Multiple Myeloma. Genes 2023, 14, 351. [Google Scholar] [CrossRef] [PubMed]
- Anwer, F.; Gee, K.M.; Iftikhar, A.; Baig, M.; Russ, A.D.; Saeed, S.; Abu Zar, M.; Razzaq, F.; Carew, J.; Nawrocki, S.; et al. Future of Personalized Therapy Targeting Aberrant Signaling Pathways in Multiple Myeloma. Clin. Lymphoma Myeloma Leuk. 2019, 19, 397–405. [Google Scholar] [CrossRef]
- A Dimopoulos, M.; Swern, A.S.; Li, J.S.; Hussein, M.; Weiss, L.; Nagarwala, Y.; Baz, R. Efficacy and safety of long-term treatment with lenalidomide and dexamethasone in patients with relapsed/refractory multiple myeloma. Blood Cancer J. 2014, 4, e257. [Google Scholar] [CrossRef]
- Richardson, P.G.; Sonneveld, P.; Schuster, M.W.; Irwin, D.; Stadtmauer, E.A.; Facon, T.; Harousseau, J.-L.; Ben-Yehuda, D.; Lonial, S.; Goldschmidt, H.; et al. Bortezomib or high-dose dexamethasone for relapsed multiple myeloma. N. Engl. J. Med. 2005, 352, 2487–2498. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.K.; Lee, J.H.; Lahuerta, J.J.; Morgan, G.; Richardson, P.G.; Crowley, J.; Haessler, J.; Feather, J.; Hoering, A.; Moreau, P.; et al. Risk of progression and survival in multiple myeloma relapsing after therapy with IMiDs and bortezomib: A multicenter international myeloma working group study. Leukemia 2012, 26, 149–157. [Google Scholar] [CrossRef]
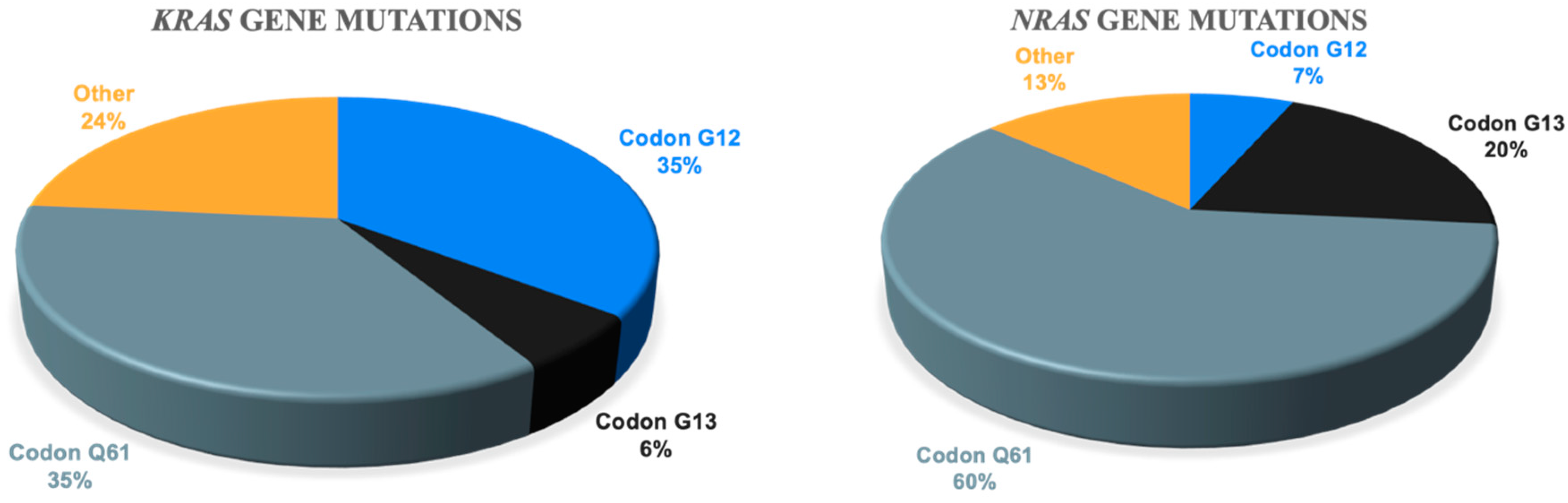
- Pasca, S.; Tomuleasa, C.; Teodorescu, P.; Ghiaur, G.; Dima, D.; Moisoiu, V.; Berce, C.; Stefan, C.; Ciechanover, A.; Einsele, H. KRAS/NRAS/BRAF Mutations as Potential Targets in Multiple Myeloma. Front. Oncol. 2019, 9, 1137. [Google Scholar] [CrossRef]
- Mey, U.J.M.; Renner, C.; Von Moos, R. Vemurafenib in combination with cobimetinib in relapsed and refractory extramedullary multiple myeloma harboring the BRAF V600E mutation. Hematol. Oncol. 2017, 35, 890–893. [Google Scholar] [CrossRef]
- Raje, N.; Chau, I.; Hyman, D.M.; Ribrag, V.; Blay, J.-Y.; Tabernero, J.; Elez, E.; Wolf, J.; Yee, A.J.; Kaiser, M.; et al. Vemurafenib in Patients With Relapsed Refractory Multiple Myeloma Harboring BRAFV600 Mutations: A Cohort of the Histology-Independent VE-BASKET Study. JCO Precis. Oncol. 2018, 2, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Giesen, N.; Chatterjee, M.; Scheid, C.; Poos, A.M.; Besemer, B.; Miah, K.; Benner, A.; Becker, N.; Moehler, T.; Metzler, I.; et al. A phase 2 clinical trial of combined BRAF/MEK inhibition for BRAFV600E-mutated multiple myeloma. Blood 2023, 141, 1685–1690. [Google Scholar] [CrossRef] [PubMed]
- Waldschmidt, J.M.; Kloeber, J.A.; Anand, P.; Frede, J.; Kokkalis, A.; Dimitrova, V.; Potdar, S.; Nair, M.S.; Vijaykumar, T.; Im, N.G.; et al. Single-Cell Profiling Reveals Metabolic Reprogramming as a Resistance Mechanism inBRAF-Mutated Multiple Myeloma. Clin. Cancer Res. 2021, 27, 6432–6444. [Google Scholar] [CrossRef] [PubMed]
- Walker, B.A.; Mavrommatis, K.; Wardell, C.P.; Ashby, T.C.; Bauer, M.; Davies, F.E.; Rosenthal, A.; Wang, H.; Qu, P.; Hoering, A.; et al. Identification of novel mutational drivers reveals oncogene dependencies in multiple myeloma. Blood 2018, 132, 587–597. [Google Scholar] [CrossRef]
- Gupta, N.; Sharma, A. Emerging biomarkers in Multiple Myeloma: A review. Clin. Chim. Acta 2019, 503, 45–53. [Google Scholar] [CrossRef]
- Mazzotti, C.; Buisson, L.; Maheo, S.; Perrot, A.; Chretien, M.-L.; Leleu, X.; Hulin, C.; Manier, S.; Hébraud, B.; Roussel, M.; et al. Myeloma MRD by deep sequencing from circulating tumor DNA does not correlate with results obtained in the bone marrow. Blood Adv. 2018, 2, 2811–2813. [Google Scholar] [CrossRef]
- Kis, O.; Kaedbey, R.; Chow, S.; Danesh, A.; Dowar, M.; Li, T.; Li, Z.; Liu, J.; Mansour, M.; Masih-Khan, E.; et al. Circulating tumour DNA sequence analysis as an alternative to multiple myeloma bone marrow aspirates. Nat. Commun. 2017, 8, 15086. [Google Scholar] [CrossRef]
- Mithraprabhu, S.; Khong, T.; Ramachandran, M.; Chow, A.; Klarica, D.; Mai, L.; Walsh, S.; Broemeling, D.; Marziali, A.; Wiggin, M.; et al. Circulating tumour DNA analysis demonstrates spatial mutational heterogeneity that coincides with disease relapse in myeloma. Leukemia 2016, 31, 1695–1705. [Google Scholar] [CrossRef]
- Rajkumar, S.V.; Dimopoulos, M.A.; Palumbo, A.; Blade, J.; Merlini, G.; Mateos, M.-V.; Kumar, S.; Hillengass, J.; Kastritis, E.; Richardson, P.; et al. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol. 2014, 15, e538–e548. [Google Scholar] [CrossRef]
- Usmani, S.Z.; Heuck, C.; Mitchell, A.; Szymonifka, J.; Nair, B.; Hoering, A.; Alsayed, Y.; Waheed, S.; Haider, S.; Restrepo, A.; et al. Extramedullary disease portends poor prognosis in multiple myeloma and is over-represented in high-risk disease even in the era of novel agents. Haematologica 2012, 97, 1761–1767. [Google Scholar] [CrossRef]
- Varettoni, M.; Corso, A.; Pica, G.; Mangiacavalli, S.; Pascutto, C.; Lazzarino, M. Incidence, presenting features and outcome of extramedullary disease in multiple myeloma: A longitudinal study on 1003 consecutive patients. Ann. Oncol. 2010, 21, 325–330. [Google Scholar] [CrossRef] [PubMed]
- Bladé, J.; de Larrea, C.F.; Rosiñol, L.; Cibeira, M.T.; Jiménez, R.; Powles, R. Soft-Tissue Plasmacytomas in Multiple Myeloma: Incidence, Mechanisms of Extramedullary Spread, and Treatment Approach. J. Clin. Oncol. 2011, 29, 3805–3812. [Google Scholar] [CrossRef]
- Weinstock, M.; Ghobrial, I.M. Extramedullary multiple myeloma. Leuk. Lymphoma 2012, 54, 1135–1141. [Google Scholar] [CrossRef] [PubMed]
- Rasche, L.; Bernard, C.; Topp, M.S.; Kapp, M.; Duell, J.; Wesemeier, C.; Haralambieva, E.; Maeder, U.; Einsele, H.; Knop, S. Features of extramedullary myeloma relapse: High proliferation, minimal marrow involvement, adverse cytogenetics: A retrospective single-center study of 24 cases. Ann. Hematol. 2012, 91, 1031–1037. [Google Scholar] [CrossRef]
- Rosiñol, L.; Beksac, M.; Zamagni, E.; Van de Donk, N.W.C.J.; Anderson, K.C.; Badros, A.; Caers, J.; Cavo, M.; Dimopoulos, M.; Dispenzieri, A.; et al. Expert review on soft-tissue plasmacytomas in multiple myeloma: Definition, disease assessment and treatment considerations. Br. J. Haematol. 2021, 194, 496–507. [Google Scholar] [CrossRef] [PubMed]
- McAvera, R.; Quinn, J.; Murphy, P.; Glavey, S. Genetic Abnormalities in Extramedullary Multiple Myeloma. Int. J. Mol. Sci. 2023, 24, 11259. [Google Scholar] [CrossRef]
- Dahl, I.M.S.; Rasmussen, T.; Kauric, G.; Husebekk, A. Differential expression of CD56 and CD44 in the evolution of extramedullary myeloma. Br. J. Haematol. 2002, 116, 273–277. [Google Scholar] [CrossRef]
- Firsova, M.V.; Mendeleeva, L.P.; Kovrigina, A.M.; Solovev, M.V.; Savchenko, V.G. Plasmacytoma in patients with multiple myeloma: Morphology and immunohistochemistry. BMC Cancer 2020, 20, 346. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Jelloul, F.; Zhang, Y.; Bhavsar, T.; Ho, C.; Rao, M.B.; Lewis, N.E.; Cimera, R.B.; Baik, J.B.; Sigler, A.B.; et al. Genetic Basis of Extramedullary Plasmablastic Transformation of Multiple Myeloma. Am. J. Surg. Pathol. 2020, 44, 838–848. [Google Scholar] [CrossRef]
- Weinstock, M.; Aljawai, Y.; Morgan, E.A.; Laubach, J.; Gannon, M.; Roccaro, A.M.; Varga, C.; Mitsiades, C.S.; Paba-Prada, C.; Schlossman, R.; et al. Incidence and clinical features of extramedullary multiple myeloma in patients who underwent stem cell transplantation. Br. J. Haematol. 2015, 169, 851–858. [Google Scholar] [CrossRef]
- Firsova, M.V.; Risinskaya, N.V.; Solovev, M.V.; Obukhova, T.N.; Kislitsyna, M.A.; Nikulina, E.E.; Yakutik, I.A.; Abramova, T.V.; Sudarikov, A.B.; Kovrigina, A.M.; et al. Multiple myeloma with extramedullary plasmacytoma: Pathogenesis and clinical case. Oncohematology 2022, 17, 67–80. [Google Scholar] [CrossRef]
- Risinskaya, N.; Kozhevnikova, Y.; Gavrilina, O.; Chabaeva, J.; Kotova, E.; Yushkova, A.; Isinova, G.; Zarubina, K.; Obukhova, T.; Kulikov, S.; et al. Loss of Heterozygosity in the Tumor DNA of De Novo Diagnosed Patients Is Associated with Poor Outcome for B-ALL but Not for T-ALL. Genes 2022, 13, 398. [Google Scholar] [CrossRef]
- Risinskaya, N.; Mangasarova, Y.; Nikulina, E.; Kozhevnikova, Y.; Chabaeva, J.; Yushkova, A.; Magomedova, A.; Kulikov, S.; Julhakyan, H.; Kravchenko, S.; et al. STR Profiling Reveals Tumor Genome Instability in Primary Mediastinal B-Cell Lymphoma. Curr. Oncol. 2022, 29, 3449–3459. [Google Scholar] [CrossRef]
- Long, X.; Xu, Q.; Lou, Y.; Li, C.; Gu, J.; Cai, H.; Wang, D.; Xu, J.; Li, T.; Zhou, X.; et al. The utility of non-invasive liquid biopsy for mutational analysis and minimal residual disease assessment in extramedullary multiple myeloma. Br. J. Haematol. 2020, 189, e45–e48. [Google Scholar] [CrossRef]
- Walker, B.A.; Boyle, E.M.; Wardell, C.P.; Murison, A.; Begum, D.B.; Dahir, N.M.; Proszek, P.Z.; Johnson, D.C.; Kaiser, M.F.; Melchor, L.; et al. Mutational Spectrum, Copy Number Changes, and Outcome: Results of a Sequencing Study of Patients With Newly Diagnosed Myeloma. J. Clin. Oncol. 2015, 33, 3911–3920. [Google Scholar] [CrossRef]
- Chapman, P.B.; Hauschild, A.; Robert, C.; Haanen, J.B.; Ascierto, P.; Larkin, J.; Dummer, R.; Garbe, C.; Testori, A.; Maio, M.; et al. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N. Engl. J. Med. 2011, 364, 2507–2516. [Google Scholar] [CrossRef]
- Heidorn, S.J.; Milagre, C.; Whittaker, S.; Nourry, A.; Niculescu-Duvas, I.; Dhomen, N.; Hussain, J.; Reis-Filho, J.S.; Springer, C.J.; Pritchard, C.; et al. Kinase-Dead BRAF and Oncogenic RAS Cooperate to Drive Tumor Progression through CRAF. Cell 2010, 140, 209–221. [Google Scholar] [CrossRef]
- Manier, S.; Park, J.; Capelletti, M.; Bustoros, M.; Freeman, S.S.; Ha, G.; Rhoades, J.; Liu, C.J.; Huynh, D.; Reed, S.C.; et al. Whole-exome sequencing of cell-free DNA and circulating tumor cells in multiple myeloma. Nat. Commun. 2018, 9, 1691. [Google Scholar] [CrossRef]
- Grisedale, K.S.; van Daal, A. Comparison of STR profiling from low template DNA extracts with and without the consensus profiling method. Investig. Genet. 2012, 3, 14. [Google Scholar] [CrossRef]
- Vij, R.; Mazumder, A.; Klinger, M.; O’Dea, D.; Paasch, J.; Martin, T.; Weng, L.; Park, J.; Fiala, M.; Faham, M.; et al. Deep Sequencing Reveals Myeloma Cells in Peripheral Blood in Majority of Multiple Myeloma Patients. Clin. Lymphoma Myeloma Leuk. 2014, 14, 131–139.e1. [Google Scholar] [CrossRef]
- Gozzetti, A.; Bocchia, M. Liquid biopsy and blood-based minimal residual disease evaluation in multiple myeloma. Oncol. Res. Featur. Preclin. Clin. Cancer Ther. 2023, 31, 271–274. [Google Scholar] [CrossRef]
- Sidorova, J.V.; Sorokina, T.V.; Biderman, B.V.; Nikulina, E.E.; Kisilichina, D.G.; Naumova, E.V.; Pochtar’, M.E.; Lugovskaia, S.A.; Ivanova, V.L.; Kovaleva, L.G.; et al. The detection of minimal residual disease in patients with chronic B-cell lymphatic leukemia using patient-specified polymerase chain reaction. Klin. Lab. Diagn. 2011, 12, 22–24. (In Russian) [Google Scholar]
- Sidorova, J.V.; Biderman, B.V.; Nikulina, E.E.; Sudarikov, A.B. A simple and efficient method for DNA extraction from skin and paraffin-embedded tissues applicable to T-cell clonality assays. Exp. Dermatol. 2011, 21, 57–60. [Google Scholar] [CrossRef]
- Bolger, A.M.; Lohse, M.; Usadel, B. Trimmomatic: A flexible trimmer for Illumina sequence data. Bioinformatics 2014, 30, 2114–2120. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Durbin, R. Fast and accurate long-read alignment with Burrows–Wheeler transform. Bioinformatics 2010, 26, 589–595. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Handsaker, B.; Wysoker, A.; Fennell, T.; Ruan, J.; Homer, N.; Marth, G.; Abecasis, G.; Durbin, R.; 1000 Genome Project Data Processing Subgroup. The Sequence Alignment/Map format and SAMtools. Bioinformatics 2009, 25, 2078–2079. [Google Scholar] [CrossRef]
- Lai, Z.; Markovets, A.; Ahdesmaki, M.; Chapman, B.; Hofmann, O.; McEwen, R.; Johnson, J.; Dougherty, B.; Barrett, J.C.; Dry, J.R. VarDict: A novel and versatile variant caller for next-generation sequencing in cancer research. Nucleic Acids Res. 2016, 44, e108. [Google Scholar] [CrossRef]
- Wang, K.; Li, M.; Hakonarson, H. ANNOVAR: Functional annotation of genetic variants from high-throughput sequencing data. Nucleic Acids Res. 2010, 38, e164. [Google Scholar] [CrossRef] [PubMed]
- Yakutik, I.A.; Al-Radi, L.S.; Biderman, B.V.; Nikitin, E.A. Detection of BRAF V600E mutation in patients with hairy cell leukemia by allele-specific RT-PCR. Hematol. Transfusiology 2014, 59, 16–19. (In Russian) [Google Scholar]

| Parameters | Patients with MM (n = 97) |
|---|---|
| Age, years, median and range | 55 (29–83) |
| Males/females | 43/54 |
| Type of secretion | |
| G | 59 (61%) |
| A | 19 (20%) |
| BJ | 15 (15%) |
| D | 4 (4%) |
| Type of FLC | |
| κ | 58 (60%) |
| λ | 39 (40%) |
| D-S stage | |
| IA | 5 (5%) |
| IB | 2 (2%) |
| IIA | 16 (17%) |
| IIIA | 58 (60%) |
| IIIB | 15 (15%) |
| Not available | 1 (1%) |
| ISS stage | |
| I | 29 (30%) |
| II | 20 (21%) |
| III | 17(17%) |
| Not available | 31 (32%) |
| Hemoglobin (g/L), median and range | 109 (66–156) |
| LDH (U/L), median and range | 170 (65–694) |
| % plasma cells in bone marrow aspiration, median and range | 16 (2.4–92) |
| FISH | |
| Standard risk | 45 (46%) |
| High risk | 49 (51%) |
| Not available | 3 (3%) |
| Plasmacytomas | |
| Yes | 57 (59%) |
| No | 40 (41%) |
| n = 57 | |
| bone | 51 (90%) |
| extramedullary | 2 (3%) |
| bone and extramedullary | 4 (7%) |
| # | Mutations in CD138+ Bone Marrow Cells | Mutations in ctDNA | Disease Features |
|---|---|---|---|
| 1 | none | KRAS c.286 delT | High LDH; ISS stage III; double-HIT: del17p13, 1q21; amyloidosis; Relapse/refractory |
| 2 | none | NRAS L95P | 1q21; only partial remission after HSCT |
| 3 | none | KRAS G12V | High LDH; 1q21; relapse/refractory |
| 4 | KRAS G12S | KRASV29A | T (4;14); only partial remission after 2 rounds of HSCT |
| 5 | NRAS Y64N | none | Plasma cell leukemia; high LDH; 1q21; extramedullary plasmacytomas; D-myeloma; death in induction |
| 6 | KRAS A59G | none | only partial remission after HSCT |
| 7 | KRAS L19F | none | ISS stage III; double HIT: t(14;16), 1q21; relapse/refractory; death in induction |
| # | LOH Loci in Bone Marrow | Mutations in Bone Marrow | LOH Loci in ctDNA | Mutations in ctDNA | DNA Concentration (ng/mL) |
|---|---|---|---|---|---|
| 1 | 2 | KRAS | 0 | none | 17.5 |
| 2 | 2 | BRAF | 0 | none | 11 |
| 3 | 6 | 2 KRAS | 0 | none | 22 |
| 4 | 0 | NRAS | 0 | none | 13.5 |
| 5 | 2 | KRAS | 0 | none | 17 |
| 6 | 0 | - | 3 | KRAS | 45.75 |
| 7 | 3 | KRAS | 4 (shared 1) | none | 46.5 |
| 8 | 0 | KRAS | 6 | none | 32 |
| 9 | 8 | NRAS | 7 (shared 2) | none | 8 |
| 10 | 0 | KRAS | 1 | none | 10 |
| 11 | 0 | NRAS | 1 | none | 17 |
| 12 | 2 | KRAS | 5 (shared 1) | none | 20 |
| 13 | 2 | - | 3 (shared 1) | NRAS | 77 |
| 14 | 5 | KRAS G12S | 3 (shared 2) | KRAS V29A | 17 |
| 15 | 2 | BRAF | 4 (shared none) | none | 30 |
| 16 | 6 | NRAS BRAF | 3 (shared 2) | none | 17 |
| 17 | 0 | - | 4 | KRAS | 50 |
| 18 | 5 | NRAS | 2 (shared none) | none | 5 |
| 19 | 1 | BRAF | 1 (shared none) | none | 10 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Soloveva, M.; Solovev, M.; Risinskaya, N.; Nikulina, E.; Yakutik, I.; Biderman, B.; Obukhova, T.; Chabaeva, Y.; Kulikov, S.; Sudarikov, A.; et al. Loss of Heterozygosity and Mutations in the RAS-ERK Pathway Genes in Tumor Cells of Various Loci in Multiple Myeloma. Int. J. Mol. Sci. 2024, 25, 9426. https://doi.org/10.3390/ijms25179426
Soloveva M, Solovev M, Risinskaya N, Nikulina E, Yakutik I, Biderman B, Obukhova T, Chabaeva Y, Kulikov S, Sudarikov A, et al. Loss of Heterozygosity and Mutations in the RAS-ERK Pathway Genes in Tumor Cells of Various Loci in Multiple Myeloma. International Journal of Molecular Sciences. 2024; 25(17):9426. https://doi.org/10.3390/ijms25179426
Chicago/Turabian StyleSoloveva, Maiia, Maksim Solovev, Natalya Risinskaya, Elena Nikulina, Igor Yakutik, Bella Biderman, Tatiana Obukhova, Yulia Chabaeva, Sergej Kulikov, Andrey Sudarikov, and et al. 2024. "Loss of Heterozygosity and Mutations in the RAS-ERK Pathway Genes in Tumor Cells of Various Loci in Multiple Myeloma" International Journal of Molecular Sciences 25, no. 17: 9426. https://doi.org/10.3390/ijms25179426





