A Comprehensive Review of Molecular Mechanisms, Pharmacokinetics, Toxicology and Plant Sources of Juglanin: Current Landscape and Future Perspectives
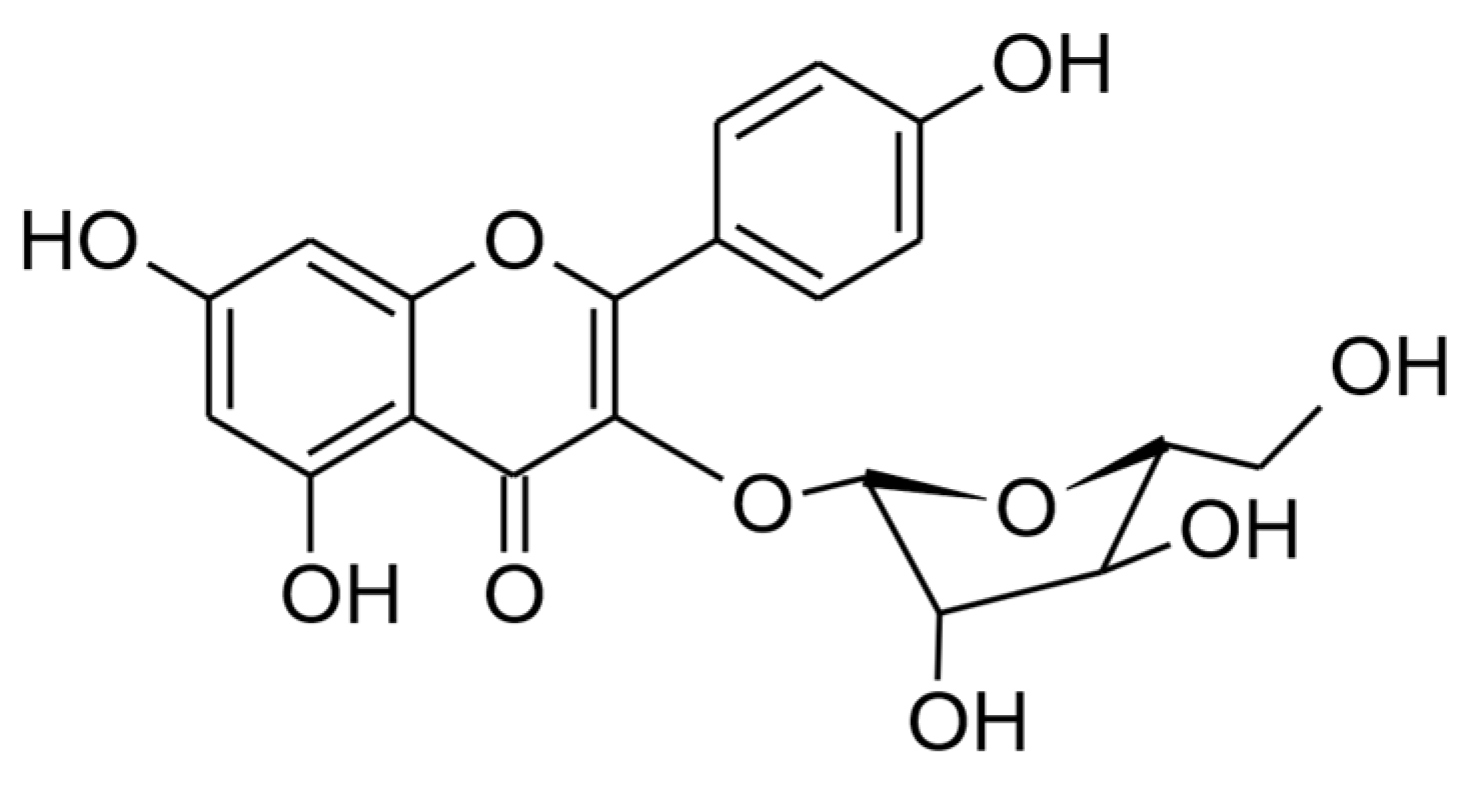
Abstract
1. Introduction
2. Juglanin Occurrence in Plant Species
3. Pharmacokinetic Properties
3.1. Absorption, Distribution, Metabolism, and Excretion Based on the ADMETlab Webserver
3.2. Bioavailability Assessment Based on Experimental Studies
4. Safety of Use
4.1. The Toxicology Study Based on the ADMETlab Webserver
4.2. The Cellular Safety Studies
4.3. Safety of Use Based on Animal Models
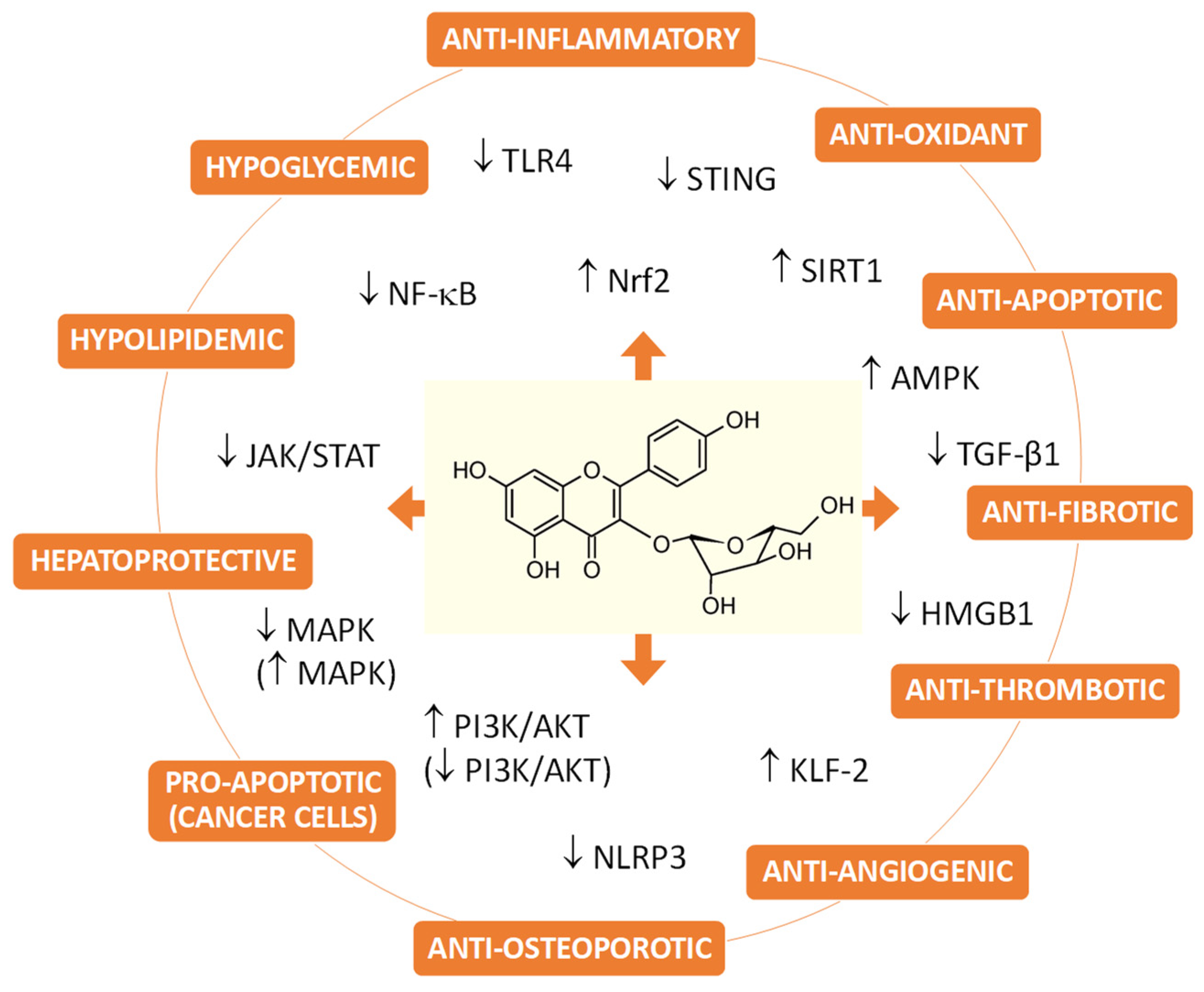
5. Biological Activity
5.1. Juglanin and Fibrosis Treatment
5.2. Juglanin and Metabolic Syndrome Therapy
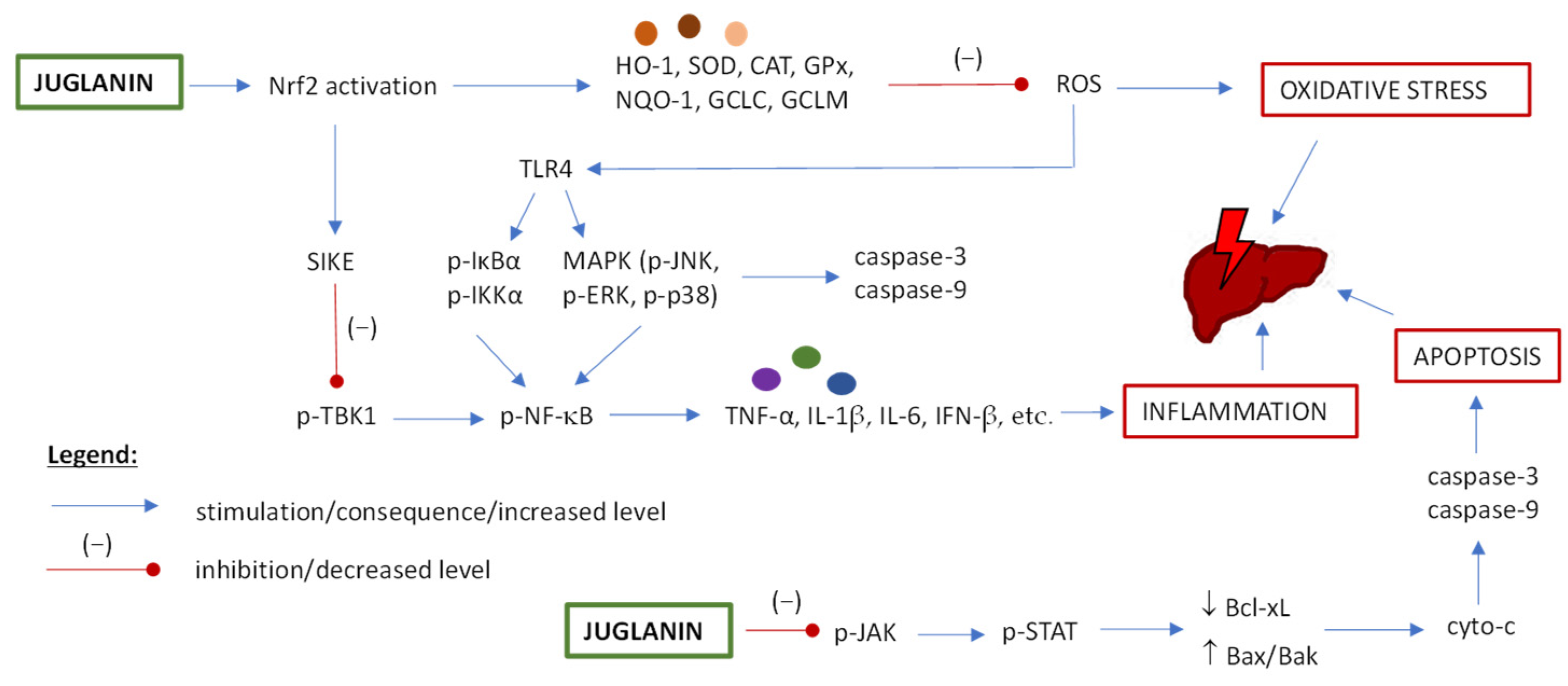
5.3. Hepatoprotective Potential of Juglanin
5.4. Effects of Juglanin on UVB-Induced Skin Injury, Wound Healing and Cellular Senescence
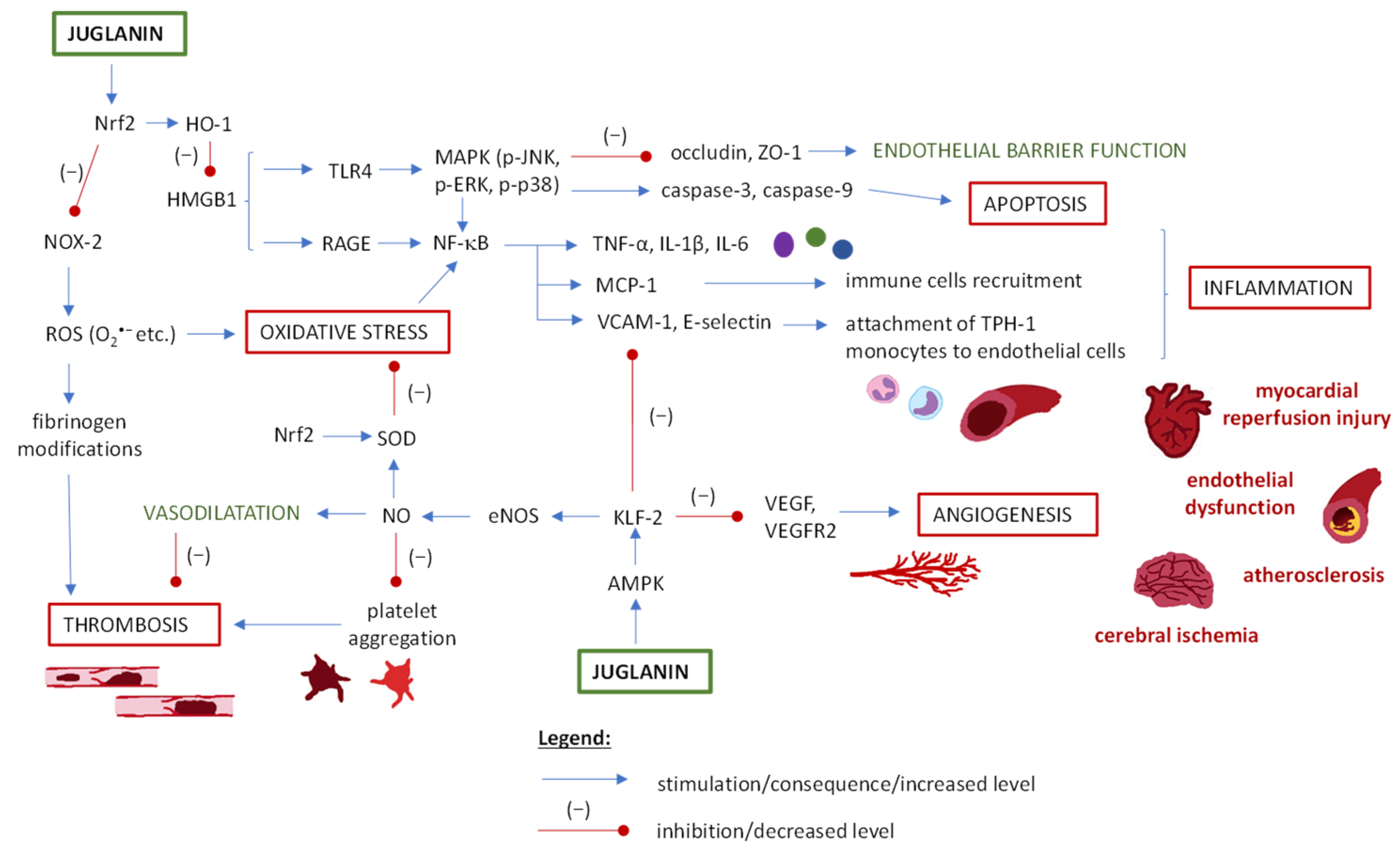
5.5. Juglanin and Cardiovascular Disorders
5.6. Juglanin and Central Nervous System Disorders
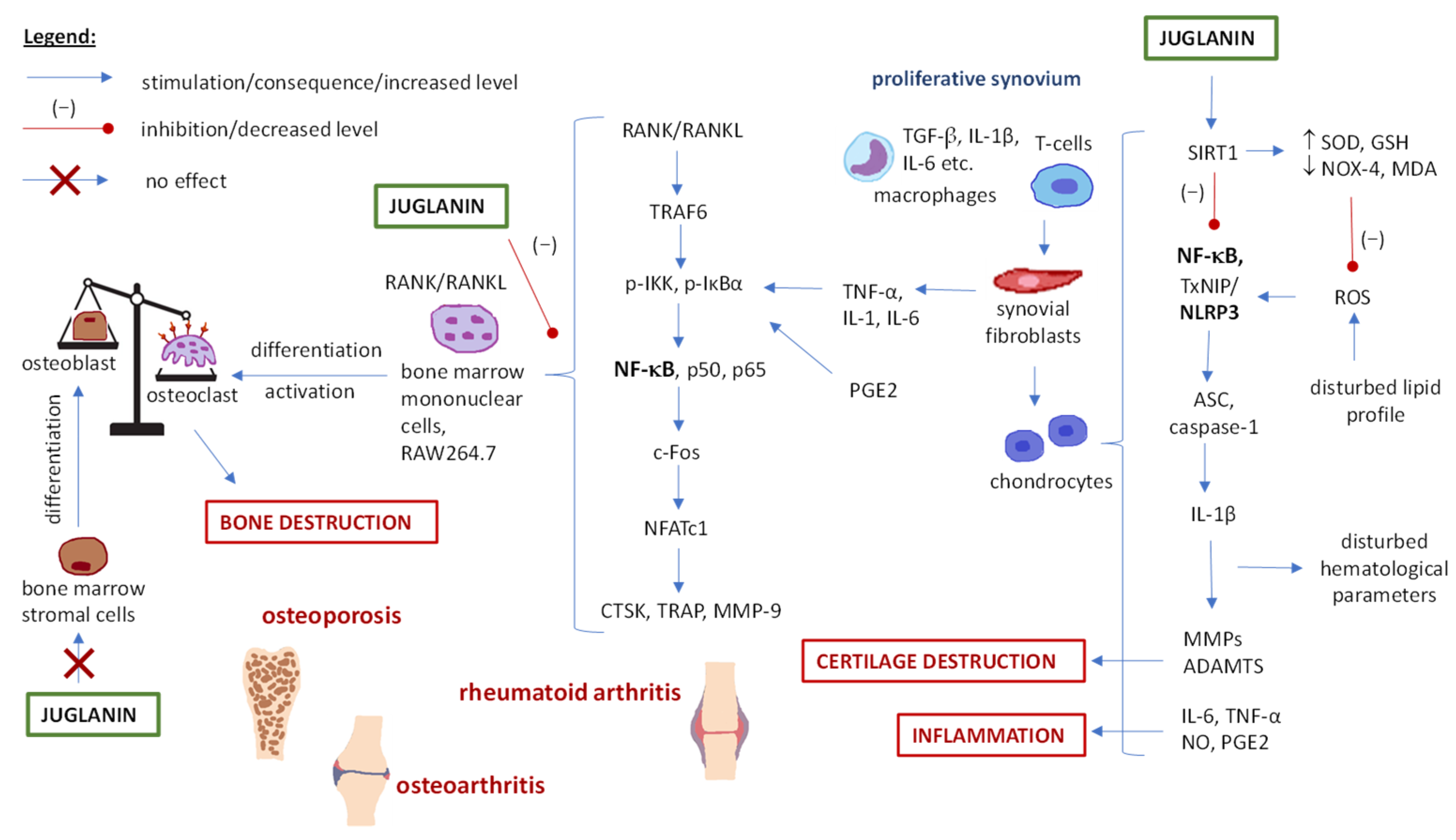
5.7. Juglanin and Skeletal System Disorders (Arthritis and Osteoporosis)
5.8. Juglanin and Anti-Cancer Potential
5.9. Juglanin and Antifungal, Antiviral and Antiparasitic Potential
5.10. Other Effects
6. Materials and Methods
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Davies, N.M.; Yáñez, J.A. (Eds.) Flavonoid Pharmacokinetics: Methods of Analysis, Preclinical and Clinical Pharmacokinetics, Safety, and Toxicology, 1st ed.; Wiley: Hoboken, NJ, USA, 2012; pp. 1–338. [Google Scholar] [CrossRef]
- Kurkin, V.A.; Zimenkina, N.I. Study of the Component composition of leaves of species of the Genus juglans L. by HPLC. Chem. Plant Raw Mater. 2022, 4, 231–239. [Google Scholar] [CrossRef]
- Shin, H.; Chung, H.; Park, B.; Lee, K.Y. Identification of antioxidative constituents from Polygonum aviculare using LC-MS coupled with DPPH assay. Nat. Prod. Sci. 2016, 22, 64–69. [Google Scholar] [CrossRef]
- Marchelak, A.; Kolodziejczyk-Czepas, J.; Ponczek, M.B.; Liudvytska, O.; Markowicz-Piasecka, M.; Bielska, B.; Miłowska, K.; Olszewska, M.A. Flavonol and A-Type Procyanidin-Rich Extracts of Prunus spinosa L. Flower Exhibit Anticoagulant Activity through Direct Thrombin Inhibition, but Do Not Affect Platelet Aggregation in Vitro. Front. Pharmacol. 2023, 14, 1307373. [Google Scholar] [CrossRef]
- Kim, M.-Y.; Choi, M.-Y.; Nam, J.-H.; Park, H.-J. Quantitative Analysis of Flavonoids in the Unripe and Ripe Fruits and the Leaves of Four Korean Rubus Species. Korean J. Pharmacogn. 2008, 39, 123–126. [Google Scholar]
- Ren, Y.; Hu, S.; Pu, H.; Zhou, Y.; Jiang, M.; Li, Y.; Deng, C.; Gao, J.; Xu, M.; Ge, C. Juglanin Ameliorates Depression-like Behavior in Chronic Unpredictable Mild Stress-Induced Mice by Improving AMPK Signaling. J. Funct. Foods 2022, 98, 105263. [Google Scholar] [CrossRef]
- Sun, J.; Song, L. Juglanin Alleviates Myocardial Injury in Rats with Acute Myocardial Infarction through Modulating MAPK Signaling Pathway. Qual. Assur. Saf. Crops Foods 2021, 13, 116–122. [Google Scholar] [CrossRef]
- Chen, L.; Xiong, Y.-Q.; Xu, J.; Wang, J.-P.; Meng, Z.-L.; Hong, Y.-Q. Juglanin Inhibits Lung Cancer by Regulation of Apoptosis, ROS and Autophagy Induction. Oncotarget 2017, 8, 93878–93898. [Google Scholar] [CrossRef]
- Sun, S.-C.; Han, R.; Hou, S.-S.; Yi, H.-Q.; Chi, S.-J.; Zhang, A.-H. Juglanin Alleviates Bleomycin-Induced Lung Injury by Suppressing Inflammation and Fibrosis via Targeting Sting Signaling. Biomed. Pharmacother. 2020, 127, 110119. [Google Scholar] [CrossRef]
- Li, Q.; Ge, C.; Tan, J.; Sun, Y.; Kuang, Q.; Dai, X.; Zhong, S.; Yi, C.; Hu, L.-F.; Lou, D.-S.; et al. Juglanin Protects against High Fat Diet-Induced Renal Injury by Suppressing Inflammation and Dyslipidemia via Regulating NF-κB/HDAC3 Signaling. Int. Immunopharmacol. 2021, 95, 107340. [Google Scholar] [CrossRef]
- Ge, C.; Tan, J.; Zhong, S.; Lai, L.; Chen, G.; Zhao, J.; Yi, C.; Wang, L.; Zhou, L.; Tang, T.; et al. Nrf2 Mitigates Prolonged PM2.5 Exposure-Triggered Liver Inflammation by Positively Regulating SIKE Activity: Protection by Juglanin. Redox Biol. 2020, 36, 101645. [Google Scholar] [CrossRef]
- Kong, Y.; Xu, S. Juglanin Administration Protects Skin against UVB-induced Injury by Reducing Nrf2-dependent ROS Generation. Int. J. Mol. Med. 2020, 46, 67–82. [Google Scholar] [CrossRef]
- Chen, X.; Zhang, C.; Wang, X.; Huo, S. Juglanin Inhibits IL-1β-Induced Inflammation in Human Chondrocytes. Artif. Cells Nanomed. Biotechnol. 2019, 47, 3614–3620. [Google Scholar] [CrossRef]
- Owczarek, A.; Kołodziejczyk-Czepas, J.; Marczuk, P.; Siwek, J.; Wąsowicz, K.; Olszewska, M. Bioactivity Potential of Aesculus hippocastanum L. Flower: Phytochemical Profile, Antiradical Capacity and Protective Effects on Human Plasma Components under Oxidative/Nitrative Stress In Vitro. Pharmaceuticals 2021, 14, 1301. [Google Scholar] [CrossRef]
- Suktap, C.; Lee, H.K.; Amnuaypol, S.; Suttisri, R.; Sukrong, S. Wound Healing Effect of Flavonoid Glycosides from Afgekia mahidolae B.L.Burtt & Chermsir. Leaves. Rec. Nat. Prod. 2018, 12, 391–396. [Google Scholar] [CrossRef]
- Nenadis, N.; Llorens, L.; Koufogianni, A.; Díaz, L.; Font, J.; Gonzalez, J.A.; Verdaguer, D. Interactive Effects of UV Radiation and Reduced Precipitation on the Seasonal Leaf Phenolic Content/Composition and the Antioxidant Activity of Naturally Growing Arbutus unedo Plants. J. Photochem. Photobiol. B 2015, 153, 435–444. [Google Scholar] [CrossRef]
- Aquino, A.J.; Da, C.; Alves, T.; Oliveira, R.V.; Ferreira, A.G.; Cass, Q.B. Chemical Secondary Metabolite Profiling of Bauhinia longifolia Ethanolic Leaves Extracts. Ind. Crops Prod. 2019, 132, 59–68. [Google Scholar] [CrossRef]
- Lavoie, S.; Côté, I.; Pichette, A.; Gauthier, C.; Ouellet, M.; Nagau-Lavoie, F.; Mshvildadze, V.; Legault, J. Chemical Composition and Anti-Herpes Simplex Virus Type 1 (HSV-1) Activity of Extracts from Cornus canadensis. BMC Complement. Altern. Med. 2017, 17, 123. [Google Scholar] [CrossRef]
- Xu, J.-F.; Tan, N.-H. Studies on the Chemical Constituents from the Branches and Leaves of Cupressus duolouxiana. J. Chin. Med. Mater. 2007, 30, 669–671. [Google Scholar]
- Kim, Y.; Lim, D.J.; Song, J.-S.; Kim, J.-A.; Lee, B.-H.; Son, Y.K. Identification and Comparison of Bioactive Components of Two Dryopteris sp. Extract Using LC-QTOF-MS. Plants 2022, 11, 3233. [Google Scholar] [CrossRef]
- Hong, H.K.; Kwak, J.H.; Kang, S.C.; Lee, J.W.; Park, J.H.; Ahn, J.W.; Kang, H.S.; Choung, E.S.; Zee, O.P. Antioxidative Constituents from the Whole Plants of Euphorbia supina. Korean J. Pharmacogn. 2008, 39, 260–264. [Google Scholar]
- Chae, H.-S.; Kim, Y.-M.; Lee, E.J.; Song, H.H.; Oh, S.-R.; Choi, Y.H.; Chin, Y.-W. Corilagin with Inhibitory Activity against NO Production from Euphorbia supina. Nat Prod. Sci. 2014, 20, 126–129. [Google Scholar]
- An, R.B.; Kwon, J.W.; Kwon, T.O.; Chung, W.T.; Lee, H.S.; Kim, Y.C. Chemical Constituents from the Whole Plants of Euphorbia supina Rafin. Korean J. Pharmacogn. 2007, 38, 291–295. [Google Scholar]
- Nugroho, A.; Rhim, T.-J.; Choi, M.-Y.; Choi, J.S.; Kim, Y.-C.; Kim, M.-S.; Park, H.-J. Simultaneous Analysis and Peroxynitrite-Scavenging Activity of Galloylated Flavonoid Glycosides and Ellagic Acid in Euphorbia supina. Arch. Pharm. Res. 2014, 37, 890–898. [Google Scholar] [CrossRef]
- Chang, S.W.; Kim, K.H.; Lee, I.K.; Choi, S.U.; Lee, K.R. Phytochemical Constituents of Geranium eriostemon. Nat. Prod. Sci. 2009, 15, 151–155. [Google Scholar]
- Żurek, N.; Pycia, K.; Pawłowska, A.; Potocki, L.; Kapusta, I.T. Chemical Profiling, Bioactive Properties, and Anticancer and Antimicrobial Potential of Juglans regia L. Leaves. Molecules 2023, 28, 1989. [Google Scholar] [CrossRef]
- Yan, M.; Chen, M.; Zhou, F.; Cai, D.; Bai, H.; Wang, P.; Lei, H.; Ma, Q. Separation and Analysis of Flavonoid Chemical Constituents in Flowers of Juglans regia L. by Ultra-High-Performance Liquid Chromatography-Hybrid Quadrupole Time-of-Flight Mass Spectrometry. J. Pharm. Biomed. Anal. 2019, 164, 734–741. [Google Scholar] [CrossRef]
- Ramon, P.; Bergmann, D.; Abdulla, H.; Sparks, J.; Omoruyi, F. Bioactive Ingredients in K. pinnata Extract and Synergistic Effects of Combined K. pinnata and Metformin Preparations on Antioxidant Activities in Diabetic and Non-Diabetic Skeletal Muscle Cells. Int. J. Mol. Sci. 2023, 24, 6211. [Google Scholar] [CrossRef]
- Matsuura, S.; Iinuma, M.; Ito, E.; Takami, H.; Kagei, K. Studies on the Constituents of the Useful Plants. VIII. The Constituents of Lespedeza cuneata G. Don. Yakugaku Zasshi 1978, 98, 1542–1544. [Google Scholar]
- Marzouk, M.S.; Soliman, F.M.; Shehata, I.A.; Rabee, M.; Fawzy, G.A. Flavonoids and Biological Activities of Jussiaea repens. Nat. Prod. Res. 2007, 21, 436–443. [Google Scholar] [CrossRef]
- Van Kiem, P.; Mai, N.T.; Van Minh, C.; Khoi, N.H.; Dang, N.H.; Thao, N.P.; Cuong, N.X.; Nam, N.H.; Nhiem, N.X.; Heyden, Y.V.; et al. Two New C-Glucosyl Benzoic Acids and Flavonoids from Mallotus nanus and Their Antioxidant Activity. Arch. Pharm. Res. 2010, 33, 203–208. [Google Scholar] [CrossRef]
- Feng, F.; Yin, Z.; Wang, P.; Zhang, Q.; Kang, W. A-Glucosidase Inhibitory Compounds in Malus halliana Koehne Tea. Curr. Top. Nutraceutical Res. 2019, 17, 236–241. [Google Scholar]
- Da Silva Sa, F.; De Paula, J.; Dos Santos, P.; De Almeida Ribeiro Oliveira, L.; De Almeida Ribeiro Oliveira, G.; Liao, L.; De Paula, J.; Do Rosario Rodrigues Silva, M. Phytochemical Analysis and Antimicrobial Activity of Myrcia tomentosa (Aubl.) DC. Leaves. Molecules 2017, 22, 1100. [Google Scholar] [CrossRef]
- Imatomi, M.; Novaes, P.; Matos, A.P.; Gualtieri, S.C.J.; Molinillo, J.M.G.; Lacret, R.; Varela, R.M.; Macías, F.A. Phytotoxic Effect of Bioactive Compounds Isolated from Myrcia tomentosa (Myrtaceae) Leaves. Biochem. Syst. Ecol. 2013, 46, 29–35. [Google Scholar] [CrossRef]
- Tajuddeen, N.; Swart, T.; Hoppe, H.C.; Van Heerden, F.R. Antiplasmodial and Cytotoxic Activities of Extract and Compounds from Ozoroa obovata (Oliv.) R. & A. Fern. Var. Obovata. Chem. Biodivers. 2021, 18, e2100240. [Google Scholar] [CrossRef]
- Park, S.; Nam, Y.H.; Rodriguez, I.; Park, J.H.; Kwak, H.J.; Oh, Y.; Oh, M.; Park, M.S.; Lee, K.W.; Lee, J.S.; et al. Chemical Constituents of Leaves of Persea americana (Avocado) and Their Protective Effects against Neomycin-Induced Hair Cell Damage. Rev. Bras. Farmacogn. 2019, 29, 739–743. [Google Scholar] [CrossRef]
- Kim, H.J.; Woo, E.-R.; Park, H. A Novel Lignan and Flavonoids from Polygonum aviculare. J. Nat. Prod. 1994, 57, 581–586. [Google Scholar] [CrossRef]
- Granica, S.; Piwowarski, J.P.; Popławska, M.; Jakubowska, M.; Borzym, J.; Kiss, A.K. Novel Insight into Qualitative Standardization of Polygoni avicularis Herba (Ph. Eur.). J. Pharm. Biomed. Anal. 2013, 72, 216–222. [Google Scholar] [CrossRef]
- Nugroho, A.; Kim, E.J.; Choi, J.S.; Park, H.-J. Simultaneous Quantification and Peroxynitrite-Scavenging Activities of Flavonoids in Polygonum aviculare L. Herb. J. Pharm. Biomed. Anal. 2014, 89, 93–98. [Google Scholar] [CrossRef]
- Central Siberian Botanical Garden SB RAS; Petruk, A.A.; Vysochina, G.I. Central Siberian Botanical Garden SB RAS Polygonum aviculare L. (Polygonaceae) phenol compounds in geographically distant populations. Proc. Univ. Appl. Chem. Biotechnol. 2019, 9, 95–101. [Google Scholar] [CrossRef]
- Olszewska, M. Quantitative HPLC Analysis of Flavonoids and Chlorogenic Acid in the Leaves and Inflorescences of Prunus serotina Ehrh. Acta Chromatogr. 2007, 19, 253–269. [Google Scholar]
- Olszewska, M. High-Performance Liquid Chromatographic Identification of Flavonoid Monoglycosides from Prunus serotina Ehrh. Acta Pol. Pharm. 2005, 62, 435–441. [Google Scholar]
- Jung, H.A.; Kim, A.R.; Chung, H.Y.; Choi, J.S. In Vitro Antioxidant Activity of Some Selected Prunus Species in Korea. Arch. Pharm. Res. 2002, 25, 865–872. [Google Scholar] [CrossRef]
- Olszewska, M.; Wolbis, M. Flavonoids from the Leaves of Prunus spinosa L. ChemInform 2002, 33, 232. [Google Scholar] [CrossRef]
- Sakar, M.; Kolodziej, H. Flavonoid Glycosides from the Flowers of Prunus spinosa. Fitoterapia 1993, 64, 180–181. [Google Scholar]
- Marchelak, A.; Olszewska, M.A.; Owczarek, A. Data on the Optimization and Validation of HPLC-PDA Method for Quantification of Thirty Polyphenols in Blackthorn Flowers and Dry Extracts Prepared Thereof. Data Brief 2020, 29, 105319. [Google Scholar] [CrossRef]
- Kim GiBeom, K.G.; Shin KwanSeog, S.K.; Kim ChangMin, K.C.; Kwon YongSoo, K.Y. Flavonoids from the Leaves of Rhododendron schlippenbachii. Korean J. Pharmacogn. 2006, 37, 177–183. [Google Scholar]
- Wang, P.; Hu, M.; Wang, L.; Qu, J.; Liu, Y.; Li, C.; Liu, Z.; Ma, C.; Kang, W. Chemical Constituents and Coagulation Effects of the Flowers of Rosa chinensis Jacq. J. Future Foods 2023, 3, 155–162. [Google Scholar] [CrossRef]
- Kumar, N.; Singh, B.; Kaul, V.K. Flavonoids from Rosa damascena Mill. Nat. Prod. Commun. 2006, 1, 623–626. [Google Scholar] [CrossRef]
- Nijat, D.; Lu, C.; Lu, J.; Abdulla, R.; Hasan, A.; Aidarhan, N.; Aisa, H.A. Spectrum-Effect Relationship between UPLC Fingerprints and Antidiabetic and Antioxidant Activities of Rosa rugosa. J. Chromatogr. B 2021, 1179, 122843. [Google Scholar] [CrossRef]
- Nijat, D.; Abdulla, R.; Liu, G.; Luo, Y.; Aisa, H.A. Identification and Quantification of Meiguihua Oral Solution Using Liquid Chromatography Combined with Hybrid Quadrupole-Orbitrap and Triple Quadrupole Mass Spectrometers. J. Chromatogr. B 2020, 1139, 121992. [Google Scholar] [CrossRef]
- Nguelefack, T.B.; Mbakam, F.H.K.; Tapondjou, L.A.; Watcho, P.; Nguelefack-Mbuyo, E.P.; Ponou, B.K.; Kamanyi, A.; Park, H.-J. A Dimeric Triterpenoid Glycoside and Flavonoid Glycosides with Free Radical-Scavenging Activity Isolated from Rubus rigidus var. camerunensis. Arch. Pharm. Res. 2011, 34, 543–550. [Google Scholar] [CrossRef]
- Rahman, A.; Ibrahim, M.; Siddiqui, J.I.; Ansari, S.A.; Ahmad, S. Metabolomic Profiling and Antidiabetic Potential of Rumex vesicarius Seed Extract in High-Fat Diet and Streptozotocin-Induced Diabetic Rat. Braz. J. Pharm. Sci. 2022, 58, e21032. [Google Scholar] [CrossRef]
- Shepeli, D.F. Studying the Composition of Salmus Preparation. Pharm. Chem. J. 2005, 39, 428–432. [Google Scholar] [CrossRef]
- Duan, S.; Tang, S.; Qin, N.; Duan, H. Chemical Constituents of Phymatopteris hastate and Their Antioxidant Activity. Zhongguo Zhong Yao Za Zhi Zhongguo Zhongyao Zazhi China J. Chin. Mater. Medica 2012, 37, 1402–1407. [Google Scholar]
- Yao, H.; Duan, J.; Ai, F.; Li, Y. Chemical Constituents from a Chinese Fern Polypodium hastatum Thunb. Biochem. Syst. Ecol. 2012, 44, 275–278. [Google Scholar] [CrossRef]
- Matsuura, S.; Yoshioka, S.; Iinuma, M. Studies on the Constituents of Useful Plants. VII. The Constituents of the Leaves of Cassia obtusifolia L. Yakugaku Zasshi 1978, 98, 1288–1291. [Google Scholar] [CrossRef]
- Tchinda, A.; Agbor, G.; Tsala, D.; Yaya, A.; Nga, E.; Talla, E.; Wauters, J.-N.; Frédérich, M. Antioxidant Activity of Flavonoids Isolated From the Fruits of Xylopia parviflora (A. Rich.) Benth. Int. J. Pharm. Sci. Res. 2014, 6, 323–328. [Google Scholar]
- Matławska, I.; Bylka, W.; Widy-Tyszkiewicz, E.; Stanisz, B. Determination of the Juglone Content of Juglans regia Leaves by GC/MS. Nat. Prod. Commun. 2015, 10, 1934578X1501000. [Google Scholar] [CrossRef]
- Islam, A.K.M.M.; Widhalm, J.R. Agricultural Uses of Juglone: Opportunities and Challenges. Agronomy 2020, 10, 1500. [Google Scholar] [CrossRef]
- Olszewska, M.; Wolbis, M. Flavonoids from the Flowers of Prunus spinosa L. Acta Pol. Pharm. 2001, 58, 367–372. [Google Scholar]
- Marciszewska, K.; Szczepkowski, A.; Lachowicz, H.; Antczak, A.; Szadkowska, D.; Suchodolski, J. The Physical, Mechanical, and Chemical Properties of Black Cherry Tree Wood (Prunus serotina Ehrh.) and Its Susceptibility to Fungal Decomposition in Areas Where It Is Secondary and Invasive: A Case Study in the Kampinos National Park (Poland). Eur. J. Wood Wood Prod. 2024, 82, 683–701. [Google Scholar] [CrossRef]
- Moerman, D.E. Native American Ethnobotany; Timber Press: Portland, Oregon, 1998; ISBN 0-88192-453-9. [Google Scholar]
- Marchelak, A.; Owczarek, A.; Matczak, M.; Pawlak, A.; Kolodziejczyk-Czepas, J.; Nowak, P.; Olszewska, M.A. Bioactivity Potential of Prunus spinosa L. Flower Extracts: Phytochemical Profiling, Cellular Safety, pro-Inflammatory Enzymes Inhibition and Protective Effects against Oxidative Stress in Vitro. Front. Pharmacol. 2017, 8, 680. [Google Scholar] [CrossRef]
- Miyashita, T.; Kunitake, H.; Yotsukura, N.; Hoshino, Y. Assessment of Genetic Relationships among Cultivated and Wild Rubus accessions Using AFLP Markers. Sci. Hortic. 2015, 193, 165–173. [Google Scholar] [CrossRef]
- ADMETlab 2.0. Available online: https://admetmesh.scbdd.com/ (accessed on 30 April 2024).
- Naeem, A.; Ming, Y.; Pengyi, H.; Jie, K.Y.; Yali, L.; Haiyan, Z.; Shuai, X.; Wenjing, L.; Ling, W.; Xia, Z.M.; et al. The Fate of Flavonoids after Oral Administration: A Comprehensive Overview of Its Bioavailability. Crit. Rev. Food Sci. Nutr. 2022, 62, 6169–6186. [Google Scholar] [CrossRef]
- Xu, F.; Guan, H.; Li, G.; Liu, H. LC Method for Analysis of Three Flavonols in Rat Plasma and Urine after Oral Administration of Polygonum aviculare Extract. Chromatographia 2009, 69, 1251–1258. [Google Scholar] [CrossRef]
- Hollman, P.C.H. Absorption, Bioavailability, and Metabolism of Flavonoids. Pharm. Biol. 2004, 42, 74–83. [Google Scholar] [CrossRef]
- Manach, C.; Donovan, J.L. Pharmacokinetics and Metabolism of Dietary Flavonoids in Humans. Free Radic. Res. 2004, 38, 771–786. [Google Scholar] [CrossRef]
- Slámová, K.; Kapešová, J.; Valentová, K. “Sweet Flavonoids”: Glycosidase-Catalyzed Modifications. Int. J. Mol. Sci. 2018, 19, 2126. [Google Scholar] [CrossRef]
- Kao, T.-Y.; Wu, H.-W.; Lee, S.-S.; Liang, P.-H.; Guh, J.-H.; Hsu, L.-C. Characterization of a Fluorescent Glucose Derivative 1-NBDG and Its Application in the Identification of Natural SGLT1/2 Inhibitors. J. Food Drug Anal. 2021, 29, 521–532. [Google Scholar] [CrossRef]
- Yang, N.; Sun, R.; Liao, X.; Aa, J.; Wang, G. UDP-Glucuronosyltransferases (UGTs) and Their Related Metabolic Cross-Talk with Internal Homeostasis: A Systematic Review of UGT Isoforms for Precision Medicine. Pharmacol. Res. 2017, 121, 169–183. [Google Scholar] [CrossRef]
- DuPont, M.S.; Day, A.J.; Bennett, R.N.; Mellon, F.A.; Kroon, P.A. Absorption of Kaempferol from Endive, a Source of Kaempferol-3-Glucuronide, in Humans. Eur. J. Clin. Nutr. 2004, 58, 947–954. [Google Scholar] [CrossRef]
- Föllmann, W.; Degen, G.; Oesch, F.; Hengstler, J.G. Ames Test. In Brenner’s Encyclopedia of Genetics; Elsevier: Amsterdam, The Netherlands, 2013; pp. 104–107. ISBN 978-0-08-096156-9. [Google Scholar]
- Zhang, F.-X.; Xu, R.-S. Juglanin Ameliorates LPS-Induced Neuroinflammation in Animal Models of Parkinson’s Disease and Cell Culture via Inactivating TLR4/NF-κB Pathway. Biomed. Pharmacother. 2018, 97, 1011–1019. [Google Scholar] [CrossRef]
- Sun, Z.-L.; Dong, J.-L.; Wu, J. Juglanin Induces Apoptosis and Autophagy in Human Breast Cancer Progression via ROS/JNK Promotion. Biomed. Pharmacother. 2017, 85, 303–312. [Google Scholar] [CrossRef]
- Yang, H.H.; Hwangbo, K.; Zheng, M.S.; Son, J.-K.; Kim, H.Y.; Baek, S.H.; Choi, H.C.; Park, S.Y.; Kim, J.-R. Inhibitory Effects of Juglanin on Cellular Senescence in Human Dermal Fibroblasts. J. Nat. Med. 2014, 68, 473–480. [Google Scholar] [CrossRef]
- Zhao, J.; Quan, X.; Xie, Z.; Zhang, L.; Ding, Z. Juglanin Suppresses Oscillatory Shear Stress-Induced Endothelial Dysfunction: An Implication in Atherosclerosis. Int. Immunopharmacol. 2020, 89, 107048. [Google Scholar] [CrossRef]
- Dong, Z.-W.; Yuan, Y.-F. Juglanin Suppresses Fibrosis and Inflammation Response Caused by LPS in Acute Lung Injury. Int. J. Mol. Med. 2018, 41, 3353–3365. [Google Scholar] [CrossRef]
- Hou, G.; Zeng, K.; Lan, H.; Wang, Q. Juglanin Ameliorates UVB-induced Skin Carcinogenesis via Anti-inflammatory and Proapoptotic Effects in Vivo and in Vitro. Int. J. Mol. Med. 2018, 42, 41–52. [Google Scholar] [CrossRef]
- Zhang, F.; Huang, X.; Qi, Y.; Qian, Z.; Ni, S.; Zhong, Z.; Zhang, X.; Li, D.; Yu, B. Juglanin Inhibits Osteoclastogenesis in Ovariectomized Mice via the Suppression of NF-κB Signaling Pathways. Front. Pharmacol. 2021, 11, 596230. [Google Scholar] [CrossRef]
- Wei, T.; Wang, L.; Tang, J.; Ashaolu, T.J.; Olatunji, O.J. Protective Effect of Juglanin against Doxorubicin-Induced Cognitive Impairment in Rats: Effect on Oxidative, Inflammatory and Apoptotic Machineries. Metab. Brain Dis. 2022, 37, 1185–1195. [Google Scholar] [CrossRef]
- Wang, G.; Wu, B.; Xu, W.; Jin, X.; Wang, K.; Wang, H. The Inhibitory Effects of Juglanin on Adipogenesis in 3T3-L1 Adipocytes. Drug Des. Devel. Ther. 2020, 14, 5349–5357. [Google Scholar] [CrossRef]
- Yuen, H.; Hung, A.; Yang, A.W.H.; Lenon, G.B. Mechanisms of Action of Cassiae Semen for Weight Management: A Computational Molecular Docking Study of Serotonin Receptor 5-HT2C. Int. J. Mol. Sci. 2020, 21, 1326. [Google Scholar] [CrossRef]
- Zhou, G.-Y.; Yi, Y.-X.; Jin, L.-X.; Lin, W.; Fang, P.-P.; Lin, X.-Z.; Zheng, Y.; Pan, C.-W. The Protective Effect of Juglanin on Fructose-Induced Hepatitis by Inhibiting Inflammation and Apoptosis through TLR4 and JAK2/STAT3 Signaling Pathways in Fructose-Fed Rats. Biomed. Pharmacother. 2016, 81, 318–328. [Google Scholar] [CrossRef]
- Yu, L.-Y.; Li, W.-Y.; Lin, J. Juglanin Improves Lipid Metabolism Disorder, Liver Injury, and Intestinal Integrity in Nonalcoholic Fatty Liver Mice. World Chin. J. Dig. 2020, 28, 113–121. [Google Scholar] [CrossRef]
- Liu, J.; Chen, L.; Zhang, X.; Pan, L.; Jiang, L. The Protective Effects of Juglanin in Cerebral Ischemia Reduce Blood–Brain Barrier Permeability via Inhibition of VEGF/VEGFR2 Signaling. Drug Des. Devel. Ther. 2020, 14, 3165–3175. [Google Scholar] [CrossRef]
- Marchelak, A.; Kolodziejczyk-Czepas, J.; Wasielewska, P.; Nowak, P.; Olszewska, M.A. The Effects of Prunus spinosa L. Flower Extracts, Model Polyphenols and Phenolic Metabolites on Oxidative/Nitrative Modifications of Human Plasma Components with Particular Emphasis on Fibrinogen in Vitro. Antioxidants 2021, 10, 581. [Google Scholar] [CrossRef]
- Marchelak, A.; Owczarek, A.; Rutkowska, M.; Michel, P.; Kolodziejczyk-Czepas, J.; Nowak, P.; Olszewska, M.A. New Insights into Antioxidant Activity of Prunus spinosa Flowers: Extracts, Model Polyphenols and Their Phenolic Metabolites in Plasma towards Multiple in Vivo-Relevant Oxidants. Phytochem. Lett. 2019, 30, 288–295. [Google Scholar] [CrossRef]
- Wang, T.; Wang, J.; Sun, T.; Li, Y. Amelioration of Juglanin against LPS-Induced Activation of NLRP3 Inflammasome in Chondrocytes Mediated by SIRT1. Inflammation 2021, 44, 1119–1129. [Google Scholar] [CrossRef]
- Ning, C.; Ning, S.; Luo, H.; Yan, L. Juglanin Attenuated Adjuvant-Induced Arthritis via Inactivating NF-κB/IκBα and a Disintegrin-like and Metalloproteinase Domain with Thrombospondin-1 Repeat Pathways in Experimental Rats. Pharmacogn. Mag. 2020, 16, 803–811. [Google Scholar] [CrossRef]
- Schwarz, S.; Sauter, D.; Wang, K.; Zhang, R.; Sun, B.; Karioti, A.; Bilia, A.; Efferth, T.; Schwarz, W. Kaempferol Derivatives as Antiviral Drugs against the 3a Channel Protein of Coronavirus. Planta Med. 2014, 80, 177–182. [Google Scholar] [CrossRef]
- Adisurja, G.P.; Parikesit, A.A. Virtual Screening of the Flavonoids Compounds with the SARS-CoV-2 3C-like Protease as the Lead Compounds for the COVID-19. Coronaviruses 2021, 2, 13–21. [Google Scholar] [CrossRef]
- Hossain, R.; Sarkar, C.; Hassan, S.M.H.; Khan, R.A.; Arman, M.; Ray, P.; Islam, M.T.; Daştan, S.D.; Sharifi-Rad, J.; Almarhoon, Z.M.; et al. In Silico Screening of Natural Products as Potential Inhibitors of SARS-CoV-2 Using Molecular Docking Simulation. Chin. J. Integr. Med. 2022, 28, 249–256. [Google Scholar] [CrossRef]
- Yang, Y.; Yang, Z.; Liu, J.; Wu, F.; Yuan, X. Screening of Potential Anti-Influenza Agents from Juglants mandshurica Maxim. by Docking and MD Simulations. Dig. J. Nanomater. Biostructures DJNB 2015, 10, 43–57. [Google Scholar]
- Renantha, R.R.; Liga, A.R.; Tanugroho, C.B.; Denovian, L.X.; Budiyanto, S.L.A.Z.; Parikesit, A.A. Flavonoids as Potential Inhibitors of Dengue Virus 2 (DENV2) Envelope Protein. J. Pharm. Pharmacogn. Res. 2022, 10, 660–675. [Google Scholar] [CrossRef]
- Anbazhakan, K.; Praveena, R.; Sadasivam, K.; Salgado, G.; Cardona, W.; Gerli, L.; Alvarado-Soto, L.; Ramirez-Tagle, R. Theoretical Insight on Structural Activities and Targets of Kaempferol Glycosides. Afinidad 2021, 78, 236–239. [Google Scholar]
- Shimizu, M.; Ito, T.; Terashima, S.; Hayashi, T.; Arisawa, M.; Morita, N.; Kurokawa, S.; Ito, K.; Hashimoto, Y. Inhibition of Lens Aldose Reductase by Flavonoids. Phytochemistry 1984, 23, 1885–1888. [Google Scholar] [CrossRef]
- Henderson, N.C.; Rieder, F.; Wynn, T.A. Fibrosis: From Mechanisms to Medicines. Nature 2020, 587, 555–566. [Google Scholar] [CrossRef]
- Jiang, F.; Liu, G.-S.; Dusting, G.J.; Chan, E.C. NADPH Oxidase-Dependent Redox Signaling in TGF-β-Mediated Fibrotic Responses. Redox Biol. 2014, 2, 267–272. [Google Scholar] [CrossRef]
- Ishida, Y.; Kuninaka, Y.; Mukaida, N.; Kondo, T. Immune Mechanisms of Pulmonary Fibrosis with Bleomycin. Int. J. Mol. Sci. 2023, 24, 3149. [Google Scholar] [CrossRef]
- Verrecchia, F.; Mauviel, A. Transforming Growth Factor-β and Fibrosis. World J. Gastroenterol. 2007, 13, 3056–3062. [Google Scholar] [CrossRef]
- Antar, S.A.; Ashour, N.A.; Marawan, M.E.; Al-Karmalawy, A.A. Fibrosis: Types, Effects, Markers, Mechanisms for Disease Progression, and Its Relation with Oxidative Stress, Immunity, and Inflammation. Int. J. Mol. Sci. 2023, 24, 4004. [Google Scholar] [CrossRef]
- Advancing Heart, Lung, Blood, and Sleep Research & Innovation|NHLBI, NIH. Available online: https://www.nhlbi.nih.gov/ (accessed on 6 May 2024).
- Cen, R.; Wang, L.; He, Y.; Yue, C.; Tan, Y.; Li, L.; Lei, X. Dermal Fibroblast Migration and Proliferation Upon Wounding or Lipopolysaccharide Exposure Is Mediated by Stathmin. Front. Pharmacol. 2022, 12, 781282. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Available online: https://www.who.int (accessed on 6 May 2024).
- Wahid, A.; Chen, W.; Wang, X.; Tang, X. High-Mobility Group Box 1 Serves as an Inflammation Driver of Cardiovascular Disease. Biomed. Pharmacother. 2021, 139, 111555. [Google Scholar] [CrossRef] [PubMed]
- Dabravolski, S.A.; Sukhorukov, V.N.; Kalmykov, V.A.; Grechko, A.V.; Shakhpazyan, N.K.; Orekhov, A.N. The Role of KLF2 in the Regulation of Atherosclerosis Development and Potential Use of KLF2-Targeted Therapy. Biomedicines 2022, 10, 254. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.; Sun, L.H.; Yang, W.; Cui, R.J.; Xu, S.B. The Role of BDNF in the Neuroimmune Axis Regulation of Mood Disorders. Front. Neurol. 2019, 10, 515. [Google Scholar] [CrossRef]
- Wang, P.; Ye, Y. Astrocytes in Neurodegenerative Diseases: A Perspective from Tauopathy and α-Synucleinopathy. Life 2021, 11, 938. [Google Scholar] [CrossRef]
- Murgas, P.; Godoy, B.; Von Bernhardi, R. Aβ Potentiates Inflammatory Activation of Glial Cells Induced by Scavenger Receptor Ligands and Inflammatory Mediators in Culture. Neurotox. Res. 2012, 22, 69–78. [Google Scholar] [CrossRef]
- Branch, N.S.C.; Arthritis, O. Available online: https://www.niams.nih.gov/health-topics/arthritis (accessed on 6 May 2024).
- Branch, N.S.C.; Osteoporosis, O. Available online: https://www.niams.nih.gov/health-topics/osteoporosis (accessed on 6 May 2024).
- Cheng, H.; Lee, S.; Chang-Chien, J.; Su, T.; Yang, J.; Su, C. Protective Mechanism of Ferulic Acid against Neomycin-induced Ototoxicity in Zebrafish. Environ. Toxicol. 2023, 38, 604–614. [Google Scholar] [CrossRef]
- The WFO Plant List|World Flora Online. Available online: https://wfoplantlist.org/ (accessed on 30 April 2024).




| Species | Family | Plant Part (Juglanin Content if Determined) | Extract (Juglanin Content if Determined) | Methods | References |
|---|---|---|---|---|---|
| Aesculus hippocastanum L. | Sapindaceae Juss. | flowers | MeOH (2.96 mg/g dw) | UHPLC–PDA–ESI–TQ–MS/MS, HPLC | [14] |
| Afgekia mahidoliae B. L. Burtt and Chermsir. | leaves | MeOH | isolation, LC-MS, 1D NMR | [15] | |
| Arbutus unedo L. | leaves (1.0–1.4 mg/g depending on season, light and precipitation treatment) | 50% MeOH | HPLC and LC-MS analysis | [16] | |
| Bauhinia longifolia (Bong.) Steud. | Fabaceae Juss. | leaves | EtOH | UHPLC-HR-QTOF-MS | [17] |
| Cornus canadensis L. | Cornaceae Bercht. ex J. Presl | leaves | 50% EtOH | isolation, 1D NMR | [18] |
| Cupressus duclouxiana Hickel | Cupressaceae Gray | leaves and branches | isolation, NMR | [19] | |
| Dryopteris lacera (Thunb.) Kuntze | Dryopteridaceae Herter | leaves | 70% EtOH | UPLC-QTOF-MS | [20] |
| Euphorbia maculata L. | Euphorbiaceae Juss. | all plant | MeOH | isolation, LC-MS, 1D NMR | [21,22,23] |
| herb (0.24 mg/g dw) | MeOH (0.99 mg/g dw) | HPLC | [24] | ||
| Geranium platyanthum Duthie | Geraniaceae Juss. | aerial parts | 80% MeOH | isolation, FAB-MS, 1D NMR | [25] |
| Juglans cinerea L. | Juglandaceae DC. ex Perleb | leaves | 70% EtOH | HPLC, 1D NMR | [2] |
| Juglans regia L. | leaves | 50% MeOH (3.23 mg/g dw) | UPLC-PDA-MS/MS | [26] | |
| 70% EtOH | HPLC, 1D NMR | [2] | |||
| flowers | 50% EtOH | UHPLC-QTOF-MS | [27] | ||
| Kalanchoe pinnata (Lam.) Pers. | Crassulaceae J. St.-Hil. | leaves | water | UPLC-OT-FTMS | [28] |
| Lespedeza cuneata (Dum.Cours.) G. Don. | Fabaceae Juss. | leaves | MeOH | isolation, IR, UV, MS, NMR | [29] |
| Ludwigia adscendens (L.) H. Hara | Onagraceae Juss. | aerial parts | CHCl3, EtOAc and then MeOH | isolation, UV, LC-MS, 1D and 2D NMR | [30] |
| Mallotus nanus Airy Shaw | Euphorbiaceae Juss. | leaves | MeOH | isolation, LC-MS, 1D and 2D NMR | [31] |
| Malus halliana Koehne | Rosaceae Juss. | leaves | 70%EtOH | isolation, LC-MS, 1D NMR | [32] |
| Myrcia tomentosa (Aubl.) DC. | Myrtaceae Juss. | leaves | EtOH | isolation, 1D and 2D NMR, GC/MS | [33] |
| EtOAc | isolation, 1D NMR | [34] | |||
| Ozoroa obovata (Oliv.) R. Fern. and A. Fern. | Anacardiaceae R. Br. | leaves | dichloromethane-methanol (1:1, v/v) | isolation, LC-MS, 1D NMR | [35] |
| Persea americana Mill. | Lauraceae Juss. | leaves | MeOH | isolation, LC-MS, 1D and 2D NMR | [36] |
| Polygonum aviculare L. | Polygonaceae Juss. | whole plant | 70% MeOH | isolation, LC-MS, 1D and 2D NMR | [37] |
| herb | 50% MeOH | UHPLC–DAD-MS | [38] | ||
| 80% MeOH | isolation, LC-MS, 1D NMR | [3] | |||
| EtOH (3.21 mg/g dw), MeOH (3.05 mg/g dw), 70% MeOH (2.42 mg/g dw), 30% MeOH (2.02 mg/g dw) | HPLC | [39] | |||
| leaves | 70% EtOH (3.6 mg/g dw) | HPLC | [40] | ||
| Prunus serotina Ehrh. | Rosaceae Juss. | leaves (0.4–2.2 mg/g dw), inflorescences (0.8–1.6 mg/g dw), depending on the collection time | MeOH | HPLC | [41] |
| leaves | 70% MeOH | isolation, TLC, UV, 1D NMR | [42] | ||
| Prunus serrulata Lindl. | leaves | MeOH | isolation, 1D NMR | [43] | |
| Prunus spinosa L. | leaves | 70% MeOH | isolation, TLC, UV, 1D NMR | [44] | |
| flowers | isolation, UV, 1D NMR | [45] | |||
| water (8.61 mg/g dw), 70% MeOH (13.73 mg/g dw) | UHPLC-ESI-MS, HPLC | [4] | |||
| flowers (2.60–5.72 mg/g dw depending on the season and source) | 70% MeOH | HPLC | [46] | ||
| Rhododendron schlippenbachii Maxim. | Ericaceae Juss. | leaves | 70% Acetone | isolation, NMR | [47] |
| Rosa chinensis Jacq. | Rosaceae Juss. | flowers | 70% EtOH | isolation, LC-MS, 1D NMR | [48] |
| Rosa damascena Herrm. | flowers (marc after essential oil distillation) | 80% MeOH | isolation, UV, IR, 1D and 2D NMR, ESI-QTOF-MS | [49] | |
| Rosa rugosa Thunb. | petals | 70% EtOH | UHPLC-Q-orbitrap-HRMS/MS | [50] | |
| flowers | commercial oral solution (Meiguihua, 23–30 µg/mL) | UHPLC-Q-orbitrap-HRMS/MS, HPLC | [51] | ||
| Rubus cuneifolius Pursh | ripe fruit (0.05 mg/g dw), unripe fruit (0.39 mg/g dw), leaves (0.68 mg/g dw) | MeOH | HPLC | [5] | |
| Rubus coreanus Miq. | ripe fruit (0.11 mg/g dw), unripe fruit (0.40 mg/g dw), leaves (0.54 mg/g dw) | ||||
| Rubus crataegifolius Bunge | ripe fruit (5 mg/g dw), unripe fruit (1.62 mg/g dw), leaves (0.83 mg/g dw) | ||||
| Rubus pungens var. oldhamii (Miq.) Maxim. | ripe fruit (0.10 mg/g dw), unripe fruit (n.d.), leaves (0.62 mg/g dw) | ||||
| Rubus rigidus Sm. | aerial part | EtOH | isolation, 1D and 2D NMR | [52] | |
| Rumex vesicarius L. | Polygonaceae Juss. | seeds | water extract | UPLC-QTOF-MS | [53] |
| Salvia sclarea L. | Lamiaceae Martinov | herb | salmus (a side product of the essential oil distillation) | TLC | [54] |
| Selliguea hastata (Thunb.) H. Ohashi and K. Ohashi | Polypodiaceae J.Presl & C.Presl | herb | isolation, NMR | [55] | |
| whole plant | EtOH | isolation, UV, MS, 1D and 2D NMR | [56] | ||
| Senna obtusifolia (L.) H. S. Irwin and Barneby | Fabaceae Juss. | leaves | MeOH | isolation, IR, MS, NMR | [57] |
| Xylopia parviflora Spruce | Annonaceae Juss. | fruits | MeOH | isolation, HPLC, LC-MS, NMR | [58] |
| Cells | Concentration Tested | Safe Concentration | Method | References |
|---|---|---|---|---|
| mice lung epithelial cells MLE 12 | 2.5, 5, 10, 20, 40, 80, 160 μM | 2.5–160 μM | MTT, 48h | [9] |
| mice primary astrocytes from 1- to 3-day-old neonatal SD mice | 10, 20, 40, 80, 160 μM | 10–160 μM | MTT, 72h | [76] |
| mice hippocampal cells line HT-22 | 2.5–100 μM | 2.5–100 μM | CCK-8, 24h | [6] |
| 40 μM | 40 μM | CCK-8, 72h | ||
| human breast cells HCC1937 | 2.5, 5, 10, 20, 30, 40 μM | 5–20 μM (at 40 μM viability about 70%) | MTS, 24 h, 48 h | [77] |
| human breast cells HGC-27 | 5–30 μM (at 40 μM viability about 80%) | |||
| human umbilical vein endothelial cells | 24 μM | 24 μM | MTT, 24 h | [78] |
| human aortic endothelial cells | 0.25–5 and 25–50 μM | 0.25–5 μM (at 50 μM viability about 75%, at 25 μM about 85%) | [79] | |
| human liver cell line L02 | 5, 10, 20, 40, 80 μM | 5–80 μM | MTT, CCK8, LDH release, 24 h | [11] |
| 40 μM | 40 μM | MTT, CCK8 and LDH, 72 h | ||
| 1.25, 2.5, 5, 10, 20, 40, 80 μM | 1.25–80 μM | CCK-8, 24 h | [80] | |
| MTT, 24 h | [8] | |||
| human lung cells line BEAS-2B | CCK-8, 24 h | [80] | ||
| human lung cells line MRC-5 | 2.5, 5, 10, 20, 40, 80, 160 μM | 2.5–80 μM (at 160 μM viability about 80%) | MTT, 24 h | [9] |
| 1.25, 2.5, 5, 10, 20, 40, 80 μM | 1.25–80 μM | [8] | ||
| human kidney cells line HK2 | ||||
| 1.25, 2.5, 5, 10, 20, 40, 80, 100 μM | 1.25–100 μM | [10] | ||
| 40 μM | 40 μM (ranging from 0 to 72 h, after 96h about 80% viability) | MTT, 96 h | ||
| human dermal fibroblasts CCD-1064sk | 1, 5, 10, 20, 40 and 80 μM | 1–20 μM | MTT, 24 h | [15] |
| human dermal fibroblasts | 24 μM | 24 μM | [78] | |
| human foreskin fibroblasts Hs68 | 2.5, 5, 10, 20, 30 μM | 2.5–30 μM | MTS, 24 h | [81] |
| human bone marrow stromal cells (BMSCs) | 10, 20, 40, 80, 160, 320, 640 μM | 10–80 μM (at 160 μM viability about 80%) | MTT, 24 h | [82] |
| primary human chondrocytes culture | 10, 20, 40, 80 μM | 10–40 μM (at 80 μM viability about 90%) | [13] | |
| human microglial cells line BV2 | 2.5–250 μM | 2.5–250 μM | CCK-8, 24 h | [6] |
| 40 μM | 40 μM | CCK-8, 84 h | ||
| human keratocytes HaCaT | 5, 10, 20, 40, 80, 160 μM | 5–160 μM | MTT, 24 h | [12] |
| Disease/Pathology Model | Activity Tested, Type of Study | Type of Groups, Treatment | Effects of Juglanin Treatment | Reference |
|---|---|---|---|---|
| Discussed mainly in Section 5.1: Juglanin and fibrosis treatment | ||||
| idiopathic pulmonary fibrosis (IPF) induced by bleomycin | anti-inflammatory, anti-fibrotic; in vivo animal model; male C57BL/6J mice; n = 20/group | 1. normal control 2. juglanin control 3. bleomycin control 4. bleomycin and juglanin (80 mg/kg/day p.o.), duration 21 days | ↑ survival rate; ↓ lung injury (↓ neutrophil alveolar infiltration and lung injury score; ↓ protein levels in BALF; ↓ neutrophils and macrophages in BALF; ↓ MPO activity; ↓ expression level of cytokines (IL-6), chemokines (CXCL1) and TNF-α in BALF and lung); ↓ pulmonary fibrosis (↓ fibrotic area in lungs; ↓ collagen I, fibronectin, TIMP-1, MMP-9, α-SMA and TGF-β1 levels in lung); ↓ expression of STING group 4 compared to group 3 for all results; no effect of juglanin on healthy mice | [9] |
| anti-inflammatory, anti-fibrotic (late stage of fibrosis); in vivo animal model; male C57BL/6J mice; n = 20/group | 1. normal control 2. bleomycin control 3. bleomycin with juglanin (80mg/kg p.o.) from 10th day of bleomycin administration, for 12 days | ↑ survival rate; ↓ histological changes in pulmonary tissues and lung injury score; ↓ neutrophils in BALF; ↓ level of IL-6 and TNF-α; ↓ collagen accumulation; ↓ expression levels of TGF-β1, fibronectin, α-SMA, collagen I, and STING group 3 compared to group 2 for all results | ||
| pulmonary fibrosis | anti-fibrotic; in vitro cellular study; the human lung fibroblast cell line MRC-5 | 1. normal control 2. cells with TGF-β1 induced pathology 3. cells with juglanin (40 μM) and TGF-β1 | ↓ expression of STING, fibronectin, MMP-9, α-SMA and collagen I group 3 compared to group 2 for all results | |
| anti-inflammatory, anti-fibrotic; in vitro cellular study; mouse lung epithelial cells MLE 12 | 1. normal control 2. cells with bleomycin induced pathology 3. cells with juglanin (40 μM) and bleomycin | ↓ mRNA expression levels of TNF-α and IL-6; ↓ expression of STING, TGF-β1 and α-SMA group 3 compared to group 2 for all results | ||
| acute lung injury caused by lipopolysaccharide | anti-inflammatory, anti-fibrotic; in vivo animal model; male C57BL6 mice; n = 10/group; | 1. normal control 2. LPS-treated group 3–4. LPS-treated group + juglanin (10 or 20 mg/kg p.o.), duration 3 weeks | ↓ inflammation scores, PAS positive cell levels, and fibrosis level (Sirius red positive cells); ↓ total number of neutrophils, lymphocytes, macrophages, eosinophils, and the total number of immune cells in BAL; ↓ eotaxin (chemokine) levels in BAL; ↓lgE and IgA levels in serum and BAL; ↓ fibrosis (↓ TGF-β1, α-SMA, collagen type I and III mRNA levels); ↓levels of IL-1β, IL-6, IL-4, IL-17, IL-18, TNF-α in the serum and lung tissue; effect on IKKα/ NF-κB signaling pathway (↓ p-IKKα, p-NF-κB, IκBα, mature IL-1 β levels) groups 3 and 4 compared to group 2 for all results | [80] |
| lung injury | anti-inflammatory, anti-fibrotic; in vitro cellular study; the human lung cell line BEAS-2B | 1. normal control 2. cells with LPS induced pathology 3. cells treated with LPS and juglanin (40 or 80 μM) | ↓ α-SMA *, Collagen I *, Collagen III *, TGF-α * levels (suppression of fibrosis markers); effect on IKKα/ NF-κB signaling pathway (↓ p-IKKα, p-NF-κB *, IκBα *, mature IL-1 β * levels) group 3–5 compared to group 2 for all tests; * juglanin at 40–80 μM; juglanin at 80 μM for other results | |
| Discussed mainly in Section 5.1: juglanin and fibrosis treatment; and Section 5.2: juglanin and metabolic syndrome therapy | ||||
| metabolic syndrome and chronic kidney disease (CKD) induced by high fat diet | anti-inflammatory, anti-fibrotic, hypolipidemic, anti-diabetic; in vivo animal model; male C57BL/6 mice; n = 4–12/group | 1. normal chow diet group 2. high fat diet (HFD) group 3–5. HFD and juglanin (7.5, 15 or 30 mg/kg/day p.o.), duration 16 weeks | ↓ body weight, weight gain in inguinal fat pad, serum TG, TC, LDLC (juglanin 15–30 mg/kg vs. HFD group); ↓ serum ALT *, AST *, and uric acid *; ↓ fasting blood glucose, fasting insulin, HOMA-IR, improved GTT and ITT parameters (↓ AUC); ↓ kidney weight; ↓ BUN, serum creatinine, creatinine clearance, UACR, UAER, collagen accumulation; improved glomerular volume, proliferated mesangial matrix, alleviated the edema and exfoliation of glomerular mesangial cells; ↓ expression of TGF-β1, SMA-α, CTGF, FN1, COL1A1 and COL1A2 (fibrosis associated genes); ↑ nephrin and podocin levels, ↓ KIM-1 (kidney damage-related molecules); ↓ lipid deposition in kidney *; ↓ expression of SREBF1, FAS *, SCD1, PPAR-γ (fatty acid synthesis); ↑ genes expression and protein levels of PPAR-α and CPT-1α (fatty acid β-oxidation); ↓ inflammatory response in kidney (↓ serum content or kidney mRNA levels of TNF-α *, IL-1β *, IL-6 *, MCP-1 *); ↓ NF-κB/ HDAC3 signaling in kidney * group 3–5 compared to group 2 for all tests; * juglanin 7.5–30 mg/kg; juglanin 15–30 mg/kg for all other results | [10] |
| kidney disease | anti-inflammatory, dyslipidemia improvement; in vitro cellular study; HK2 cells (immortalized proximal tubule epithelial cell line from adult human kidney) | 1. normal control 2. cells with palmitate induced pathology 3. cells with palmitate and juglanin (10, 20, 40 μM) | ↓ expression or protein levels of SREBF-1 **, FAS **, SCD-1 ***, ACCα *, PPAR-γ ***; ↑ expression or protein levels of PPAR-α **, CPT-1 **, UCP-2 **; ↓ TNF-α ***, IL-1β ***, IL-6 ***, and MCP-1 *** mRNA levels; ↓ p-IKKAα ***, p-IKβα ***, p-NF-κB *** levels; ↑IKβα *** level; inhibition of NF-κB/HDAC3 nuclear translocation *** Group 3 compared to group 2; *** juglanin at 10–40 μM; ** juglanin at 20–40 μM; * juglanin at 40 μM | |
| adipogenesis | inhibition of adipogenesis in vitro cellular study; 3T3-L1 preadipocytes | 1. 3T3-L1 preadipocytes 2–4. 3T3-L1 preadipocytes with juglanin (0.5, 2.5 or 5 μM) | ↓ lipid accumulation in differentiated adipocytes (day 8 of the study), the effect reversed in cells treated with AMPK inhibitor; ↓ FABP4 * and GLUT4 *expression in preadipocytes; inhibition of the gene expression of adiponectin * and leptin * during differentiation process; ↓ gene and protein levels of C/EBPα, C/EBPβ and SREBP-1c, no effect on PPAR-α and PPAR-γ; ↑ activation of the SIRT1/AMPK signaling pathway (↑ phosphorylation of AMPKα and SIRT1 mRNA and protein levels) groups 2–4 compared to group 1 for all tests; * juglanin at 5 μM; juglanin at 0.5–5 μM for other results | [84] |
| obesity | appetite suppression; molecular docking studies | - | favorable binding to 5-HT2C outside of the known agonist binding pocket (juglanin may be positive allosteric modulators of 5-HT2C receptor function) | [85] |
| diabetes, metabolic syndrome | antidiabetic; in vitro α-glucosidase inhibition | positive control: acarbose (IC50 = 1819.72 μM) | weak activity toward α-glucosidase (IC50 = 3246.17 μM) | [32] |
| Discussed mainly in Section 5.1: juglanin and fibrosis treatment; and Section 5.3: hepatoprotective potential of juglanin | ||||
| hepatitis caused by fructose | anti-inflammatory, anti-apoptotic, hepatoprotective, hypolipidemic, anti-diabetic; in vivo animal model; male Sprague-Dawley rats; n = 15/group | 1. conventional diet 2. fructose-feeding group 3–5. fructose and juglanin (5, 10 or 20 mg/kg p.o.), duration 5 weeks | ↓ body weight * and body fat *; ↓ serum endotoxin (LPS) level; ↓ serum glucose level (OGTT, ITT); ↓ TG, TC *, LDL *, and ↑ HDL * levels in serum; ↓ TG and TC levels in liver; ↓ liver inflammation * and liver fibrosis * scores; ↓ level of inflammatory cytokines in serum (TNF-α, IFN-γ, IL-17, IL-10, TGF-β, IL-35, IL-1β, IL-6, IL-18 *); ↓ level cytokines in liver (IL-1β **, IL-6, IL-18); ↓ serum and liver ALT, AST, ALP; ↓ level of TLR4 expressing liver cells, ↓ TLR4 *, MyD88 **, IRAK4 **, IRAK1 **,TRAF6 *, TSK1 ** levels; suppression of MAPK and NF-κB signaling pathway (↓ p-JNK/JNK, p-ERK/ERK, p-p38/p38, c-Jun **, p-IKKα *, p-IκBα **, p-NF-κB/NF-κB and ↑ IKKα *, IκBα * levels in liver); ↓ cytokines expression (TNF-α *, IFN-γ, IL-17, IL-10, TGF-β, IL-35, IL-1β *, IL-6, IL-18 **); ↓ apoptosis (↓ p-JAK2/JAK2 **, p-STAT3/STAT3 *, cyto-c *, caspase-9 *, caspase-3 and ↑ Bcl-xL levels in liver); ↓ cyto-c, caspase-9, caspase-3 expression and ↑ Bcl-xL expression, JAK2 and STAT3 expression not changed groups 3–5 compared to group 2 for all tests; ** juglanin at 20 mg/kg; * juglanin at 10–20 mg/kg; juglanin at 5–20 mg/kg for other results | [86] |
| Discussed mainly in Section 5.3: hepatoprotective potential of juglanin | ||||
| nonalcoholic fatty liver disease (NAFLD) induced by high-fat diet | anti-inflammatory, hepatoprotective, hypolipidemic, anti-diabetic; in vivo animal model; C57BL/6 mice; n = 6/group | 1. low-fat diet control 2. High-fat diet (HFD) control 3–5. HFD and juglanin (5, 10 or 20 mg/kg/day p.o. for 3 weeks), duration 8 weeks | ↓ inflammatory lesions and lipid accumulation in mouse liver tissue (histomorphological changes) #; ↓ serum AST *, ALT **, cholesterol **; ↓ fasting serum glucose **, insulin **, HOMA-IR **; ↑ PPAR-α *, FGF21 **, CPT-1a ** mRNA levels, ↑ p-ACC/ACC ** (lipid metabolism); ↓ TNF-α **, IL-6 # and IL-1β # levels; ↓ intestinal permeability (↑ expression of tight junction protein ZO-1 **, ↓ FITC-dextran **) groups 3–5 compared to group 2 for all tests; # lack of statistics; * juglanin at 20 mg/kg; ** juglanin at 10–20 mg/kg; juglanin at 5–20 mg/kg for other results | [87] |
| non-alcoholic steatohepatitis-like phenotype (hepatic injury) induced by PM2.5 (air pollution containing particulate matter less than 2.5 μm) | hepatoprotective, anti-inflammatory, antioxidant; in vivo animal model; wild type male C57BL/6 mice; n = 5–8/group | 1. normal control (filtered air) 2. filtered air and juglanin 3. PM2.5 control 4. PM2.5 air and juglanin (40 mg/kg/day p.o.), duration 24 weeks | body weight not changed; ↓ MBP, ↑ liver weight; ↓ ALT, AST; ↑ SOD activity, ↓ MDA level; ↑ Nrf2 # and SIKE, ↓ p-TBK1 and p- NF-κB levels; ↑ Nrf2 # expression; ↑ HO-1, NQO-1 #, GCLC and GCLM # expression; ↓ IL-1β, IL-6, TNF-α and IFN-β expression group 4 compared to group 3 for all tests (# additionally group 2 compared to group 1) | [11] |
| hepatic injury | hepatoprotective, anti-inflammatory, antioxidant; in vitro cellular study; human liver cells L02 | 1. normal cells 2. normal cells and juglanin 3. cells with PM2.5 4. PM2.5 (air pollution, particulate matter less than 2.5 μm) and juglanin (40 μM) 5. PM2.5 cells and t-BHQ (10 μM, positive control) | ↓ Nrf2 nuclear translocation in dose-dependent (5–80 μM) manner (↓ cytoplasm Nrf2 and ↑ nuclear Nrf2—tested for group 2 compared to group 1 only); ↓ oxidative stress (↓ Keap-1 and ↑ HO-1 # levels;↑ SOD #, CAT #, GPx # activity; ↓ ROS accumulation), effects comparable to t-BHQ treatment; ↓ inflammation (↑ SIKE # level, ↓ IL-1β, IL-6, TNF-α, IFN-β expression, ↓ p-TBK1, p-NF-κB levels), effects comparable to t-BHQ treatment group 4 compared to group 3 for all tests (# additionally group 2 compared to group 1) | |
| Discussed mainly in Section 5.4: Effects of juglanin on UVB-induced skin injury, wound healing and cellular senescence | ||||
| hyperplasia and cell infiltration in the skin caused by UVB radiation | anti-inflammatory, antioxidant; in vivo animal model; female SKH-1 hairless mice; n = 15/group | 1. normal control 2. animals irradiated with UVB 3–4. UVB irradiation and juglanin (15 or 30 mg/kg p.o. three times per week), duration 10 weeks | ↓ skin injury (↓ skin thickness, MPO activity, transepidermal water loss); ↓ total groove volume *, wrinkle area, wrinkle volume * and the number of wrinkles; ↓ MDA * and TBARS levels (↓ lipid peroxidation); ↑ GSH level, ↑ SOD, CAT and GPx activity; ↓ iNOS and TGF-β1, ↑ Nrf2 expression and levels; ↓ phosphorylation of p38, ERK1/2 and JNK * (↓ MAPK signaling pathway); ↓ inflammatory response (↓ NF-κB phosphorylation; ↓ COX-2, IL-1β *, TNF-α * expression) groups 3–4 compared to group 2 for all tests; * juglanin at 30 mg/kg; juglanin at 15–30 mg/kg for other results | [12] |
| UVB-induced skin injury | anti-inflammatory, antioxidant; in vitro cellular study; human epidermal cells (HaCaT) exposed to UVB radiation | 1. normal control 2. cells treated with UVB 3–4. UVB and juglanin (80 or 160 μM) | ↓ ROS generation; ↑ SOD1, SOD2 *, CAT and Nrf2, ↓ TGF-β1 and iNOS expression levels; ↓ p38, ERK1/2 * and JNK * phosphorylation (lack of effect in cells with Nrf2 knock down; synergistic activity with MAPK inhibitors); ↓ NF-κB phosphorylation; ↓ COX-2, IL-1β *, and TNF-α * expression and levels (lack of effect in cells with Nrf2 knock down; synergistic activity with NF-κB inhibitor) groups 3–4 compared to group 2 for all tests; * juglanin at 160 μM; juglanin at 80–160 μM for other results | |
| wound | wound healing; in vitro scratch-wound healing assay; human dermal fibroblasts (CCD-1064sk) | 1. scratch-wound control 2. scratch-wound and juglanin (1 or 5 μM) | promote the migration of fibroblasts (↑ % of wound closure after 16 and 24 h) group 2 compared to group 1 | [15] |
| cellular senescence | inhibition of cellular senescence; in vitro cellular study; human dermal fibroblasts or human umbilical vein endothelial cell | 1. normal control 2. cellular senescence induced by Adriamycin 3. adriamycin and juglanin (1, 3, 5 or 10 µg/mL) 4. old cells (replicative senescence) 5. old cells and juglanin (1, 3, 5 or 10 µg/mL) 6. N-acetylcysteine (5 mM, positive control) 7. rapamycin (500 nM, positive control) | no effect on senescence-associated β-galactosidase (SA-β-gal) activity observed for human umbilical vein endothelial cell, hence this model was excluded from further studies; effects on human dermal fibroblasts (group 3 compared to group 2): ↓ SA-β-gal activity (at 3–10 µg/mL comparable to both positive controls); ↓ p53 and p21 levels, no effect on pS6 (lack of statistics); ↓ intracellular ROS (tested for 10 µg/mL, comparable to rapamycin control) effects on human dermal fibroblasts (group 5 compared to group 4): ↓ SA-β-gal activity (at 5–10 µg/mL comparable or more effective than both positive controls) | [78] |
| Discussed mainly in Section 5.5: Juglanin and cardiovascular disorders | ||||
| shear stress-induced endothelial dysfunction (atherosclerosis model) | anti-inflammatory, antioxidant; anti-atherogenic in vitro cellular study; human aortic endothelial cells (HAECs) | 1. normal control 2. oscillatory shear stress control 3–4. cells with shear stress and juglanin (2.5 or 5 μM) | ↓ NOX-2 protein and mRNA levels, ↓ intracellular ROS levels; ↓ IL-1β and MCP-1 mRNA and protein expression, ↓ HMGB1 secretion (↑ HMGB1 release in normal cells at 25–50 μM dose); ↑ eNOS protein and mRNA levels, ↑ NO concentration; ↓ attachment of TPH-1 monocytes to endothelial cells, ↓ VCAM-1 and E-selectin mRNA and protein expression; ↑ atheroprotection (KLF-2 mRNA and protein expression) groups 3–4 compared to group 2 for all tests | [79] |
| acute myocardial infarction (AMI) induced by ligation of the left anterior descending artery | anti-inflammatory, anti-apoptotic in vivo animal model; male Sprague–Dawley mice; n = 8/group | 1. normal control 2. mice with AMI 3–4. mice with AMI and juglanin (10 or 30 mg/kg/day), duration 14 days | improved the morphological changes in myocardial tissue (↓ loose, edematous and necrotic cardiomyocytes, ↓ inflammatory cell infiltration); ↓ LDH and CK-MB; ↓ inflammatory response (↓ IL-6, IL-1β, TNF-α, and ↑ IL-10 levels in serum); ↓ apoptosis (↓ TUNEL-positive cells, ↓ caspase-3 and caspase-9 levels); MAPK signaling pathway regulation (↓ phosphorylation of p-38, p-ERK, p-JNK) groups 3–4 compared to group 2 for all tests | [7] |
| cerebral ischemia | anti-ischemic; in vivo animal model; C57/BL6 mice; n = unknown | 1. normal control 2. normal mice with juglanin 3. mice with middle cerebral artery occlusion (MCAO) 4. mice with MCAO and juglanin (20 mg/kg p.o. for 3 weeks before the MCAO) | ↓ infarct volume by about half; ↓ neurological score, ↓ blood-brain barrier permeability; ↓ VEGF and VEGFR2 mRNA and protein levels (inhibition of MCAO-induced angiogenesis); ↑ expression of the tight junction proteins (occludin and ZO-1) # group 4 compared to group 3 for all tests (# additionally group 2 compared to group 1) | [88] |
| anti-ischemic; in vitro cellular study; bEnd.3 human brain microvascular endothelial cells exposed to oxygen–glucose deprivation/reperfusion (OGD/R) | 1. normal control 2. cells with OGD/R 3–4. cells with OGD/R and juglanin (2.5 or 5 μM) | ↑ cells viability, ↓ release of lactate dehydrogenase (↓ cytotoxicity caused by OGD/R); ↓ brain endothelial permeability; ↑ occludin and ZO-1 protein levels; ↓ VEGF * and VEGFR2 * protein levels (the addition of VEGF-A to the experiment abolished the effects of juglanin on brain endothelial permeability) groups 3–4 compared to group 2 for all tests; * juglanin at 5 μM; juglanin at 2.5–5 μM for other results | ||
| oxidative modifications of biomolecules | antioxidant; ex vivo model on human plasma | 1. normal control 2. human plasma exposed to ONOO– in vitro 3–5. ONOO– treated plasma and juglanin (1, 5 or 50 μg/mL) 6. ONOO– treated plasma and ascorbic acid, AA (1, 5 or 50 μg/mL) | ↓ nitration of protein tyrosine residues (↓ 3-NT levels); ↓ levels of TBARS; ↑ NEAC * of plasma; effects comparable to AA at 1–5 μg/mL, AA activity at 50 μg/mL higher groups 3–5 compared to group 2 for all tests; * 1–5 μg/mL; juglanin at 1–50 μg/mL for other results | [89] |
| antioxidant; ex vivo model on human fibrinogen | 1. normal control 2. fibrinogen exposed to ONOO– in vitro 3–5. ONOO– treated fibrinogen and juglanin (1, 5 or 50 μg/mL) 6. ONOO– treated fibrinogen and ascorbic acid (1, 5 or 50 μg/mL) | ↓ high molecular weight aggregates; no effects on Aα, Bβ and γ bands; ↓ 3-NT level; ↓ tryptophan residue oxidation *; effects comparable to AA at 1–5 μg/mL, AA activity at 50 μg/mL higher groups 3–5 compared to group 2 for all tests; * juglanin at 50 μg/mL; juglanin at 1–50 μg/mL for other results | ||
| oxidative stress-related disorders | antioxidant; in vitro studies | positive control: ascorbic acid (AA, 5.68 µmol/mg) | no effect on O2•−, NO•, ONOO−; low scavenging potential toward H2O2 (SC50 = 0.64 µmol AA equivalents/mg); high scavenging potential toward HO• (SC50 = 6.35 µmol AA equivalents/mg) and HClO (IC50 = 8.56 µmol AA equivalents/mg) | [90] |
| positive control: curcumin (SC50 = 27.80 μM) | DPPH scavenging: IC50 = 89.91 μM | [3] | ||
| positive control: ascorbic acid (SC50 = 1.76 μg/mL for DPPH assay) | DPPH scavenging: IC50 = 0.16 μg/mL; β-carotene-linoleic acid assay: lower activity than ascorbic acid | [52] | ||
| positive control: L-penicillamine (SC50 = 4.62–6.90 μM) | ONOO− scavenging: SC50 = 22.3 μM | [24,39] | ||
| positive controls: ascorbic acid (DPPH, IC50 = 11.5 μM), trolox (ROS inhibition 73.6%), penicillamine (ONOO− inhibition, IC50 = 3.2 μM) | DPPH scavenging: IC50 = 100.4 μM; Total ROS inhibition (in vitro on rat kidney homogenates): 36.8% ONOO− inhibition: IC50 = 10.5 μM | [43] | ||
| positive control: Trolox | peroxyl radical-scavenging activity (ORAC): about 12 µM Trolox equivalents; hydroxyl radical-scavenging activity (ORAC): about 8 µM Trolox equivalents; metal chelating (Cu2+) and reducing (copper (I) ions) potential | [31] | ||
| positive control: Trolox | peroxyl radical-scavenging activity (ORAC): 0.62 Trolox equivalents | [21] | ||
| blood coagulation-related disorders | anti-coagulant; ex vivo study on platelet aggregation in human blood; in silico molecular docking and in vitro study of thrombin activity | 1. control platelet-rich human plasma stimulated with adenosine diphosphate (ADP) or collagen 2. stimulated plasma and juglanin (5 or 50 µg/mL) 3. stimulated plasma and indomethacin (positive control, 5 µg/mL) | weak effect on platelet aggregation after ADP stimulation * (↓ aggregation by <15%, for indomethacin ↓ by 23%); no effect on platelet aggregation after collagen stimulation (for indomethacin ↓ by 86%); no effect on thrombin activity group 2 compared to group 1; * juglanin at 50 μg/mL; juglanin at 1–50 μg/mL for other results | [4] |
| blood coagulation-related disorders | pro-coagulant; ex vivo study on platelet aggregation in New Zealand white rabbit blood | 1. control blood sample 2. blood sample with juglanin (2 mg/mL) 3. blood sample with breviscapine (13.3 mg/mL) | no effect on APTT and PT times; ↓ TT time (weaker effect than breviscapine); ↑ fibrinogen content (comparable effect to breviscapine) group 2 compared to group 1 | [48] |
| inflammation-related disorders | anti-inflammatory; in vitro cellular study; Raw264.7 cells | 1. normal control 2. LPS-stimulated control 3. LPS and juglanin (5 μg/mL) | no significant effect on NO release group 3 compared to group 2 | [22] |
| Discussed mainly in Section 5.6: Juglanin and central nervous system disorders | ||||
| cognitive impairment caused by doxorubicin | antioxidant, anti-inflammatory, anti-apoptotic; in vivo animal model; male rats; n = 6/group | 1. normal control 2. doxorubicin control 3. normal rats and juglanin 4. doxorubicin and juglanin (30 mg/kg/day p.o.), duration 4 weeks | ↑ body weight; memory and cognitive function improved (Y-maze test: ↑ % of spontaneous alternation, total arm entries not changed; Morris water maze test: ↓ the latency of escapes; space exploration test: ↑ the time spent in the target quadrant and number of crossings); depression-like behavior improved (forced swimming test: ↓ immobility time, ↑ swimming and climbing time); ↓ inflammatory mediators levels in the brain (↓ TNF-α, IL-1β, IL-6 and NF-kB); ↓ oxidative stress in the brain (↓ MDA level, ↑ SOD, CAT, GSH); alleviated histopathological alteration in the brain (pyknosis, degenerated and swollen neurons and congested blood vessels); ↓ activity of AchE and caspase-3 group 4 compared to group 2 for all tests; no effect of juglanin on healthy rats | [83] |
| chronic unpredictable mild stress (CUMS) | improvement of anxiety/depression-like behaviors, neuroprotective, anti-inflammatory; in vivo animal model; male C57BL/6N mice; n = 4–8/group | 1. normal control 2. normal mice and juglanin 3. CUMS control 4. CUMS and juglanin (30 mg/kg/day p.o), duration 8 weeks | ↑ sucrose consumption, ↓ immobility and transfer latency time, ↑ time spend in the center zone, target quadrant and the frequency of appearance in the target quadrant (behavior tests: tail suspension test; open-field test; Morris water maze test); effects on depression-related hormones (↑ 5-HTP serum level, ↑ 5-HT, DA and GABA hippocampal levels, ↓ CORT serum and hippocampal levels, ↓ ACTH serum level, ↓ glutamate hippocampal level); ↓ neuronal damage in hippocampal section; ↑ expression of p-AKT, PI3K, and BDNF in hippocampus, ↓ cleaved caspase-3 and cleaved PARP protein expression, ↑ Bcl-2 protein and gene expression, ↓ Bax gene expression; ↓ the activation of microglial cells and astrocytes (↓ CD11b and GFAP levels); ↓ neuroinflammation (↓ TNF-ɑ, IL-1β, IL-6, MCP-1 serum and hippocampal levels/expression, ↓ iNOS and COX-2 gene expression, ↓ p-IKKɑ, p-IκBɑ and p-NF-κB protein expression) ↑ AMPK activation (↑ p-AMPK) group 4 compared to group 3 for all tests, no effect of juglanin on healthy mice | [6] |
| neuroinflammation | neuroprotective, anti-apoptotic; in vitro cellular study; mouse hippocampal cell line HT-22 | 1. normal control 2. normal cells and juglanin 3. LPS control 4. LPS and juglanin (40 μM) | ↓ apoptotic cell death (↓ TUNEL-positive cells); ↓ Bax and ↑ Bcl-2 gene expression; ↑ PI3K, p-AKT, Bcl-2 protein expression; ↓ cleaved caspase-3 and cleaved PARP protein expression; ↑ p-AMPK protein expression; the observed effects were reversed in cells with silenced AMPK group 4 compared to group 3 for all tests, no effect of juglanin on normal cells | |
| neuroprotective, anti-inflammatory; in vitro cellular study; an immortalized murine microglial cell line BV2 | 1. normal control 2. normal cells and juglanin 3. LPS control 4. LPS and juglanin (40 μM) | ↓ microglial cell activation (↓ CD11b expression); ↓ nuclear NF-κB expression; ↓ p-IKKɑ, p-IκBɑ, p-NF-κB and NF-κB protein expression; ↓ TNF-ɑ, IL-1β, IL- 6, IL-18, MCP-1, iNOS and COX-2 gene expression; ↓ TNF-ɑ, IL-1β level; ↑ p-AMPK protein expression; the observed effects were reversed in cells with silenced AMPK group 4 compared to group 3 for all tests, no effect of juglanin on normal cells | ||
| neuroinflammation in Parkinson’s disease | anti-inflammatory, neuroprotective; in vivo animal model; male C57BL6 mice; n = 20/group | 1. normal control 2. LPS control 3–5. LPS and juglanin 10, 20 or 30 mg/kg p.o., five times per week), duration 13 days | attenuation of the cognitive dysfunction (↓ time to find hidden platform; ↑ number of platform crossings and time spend in target quadrant in Morris water maze test); ↑ SYP, PSD-95 and SNAP-25 *, ↓ Aβ and p-Tau expression and proteins levels in hippocampus; ↓ α-synuclein and ↑ TH expression and levels in hippocampus and/or Substantia Nigra; ↓ expression and levels of proinflammatory cytokines (IL-1β, IL-18, TNF-α) and COX-2; ↓ TLR4 **, MyD88 #, CD14 #, p-IKKα, p-IκBα and p-NF-κB levels; ↓ astrocytes and microglia activity, protective activity against neurons damages (↓ GFAP positive cells, ↓ Iba1 expression) groups 3–5 compared to group 2 for all tests; ** juglanin at 30 mg/kg; * juglanin at 20–30 mg/kg; # lack of statistics; juglanin at 10–30 mg/kg for other results | [76] |
| neuroinflammation | anti-inflammatory, neuroprotective; in vitro cellular study; mice primary astrocytes | 1. normal control 2. LPS control 3–5. cells with LPS and juglanin (40, 80 or 160 μM) | ↓ TLR4/MyD88/CD14 #, p-IKKα #, p-IκBα # and p-NF-κB #; ↓ GFAP #, BDNF # and ↑ TH # levels; ↓ GFAP and p-NF-κB activity; ↑ SYP #, PSD-95 # and SNAP-25 # levels; ↓ Aβ # and p-Tau # levels; ↓ levels of proinflammatory cytokines (IL-1β, IL-18 *, TNF-α) and COX-2 * groups 3–5 compared to group 2 for all tests; * juglanin at 80–160 μM; # lack of statistics; juglanin at 40–160 μM for other results | |
| Discussed mainly in Section 5.7: Juglanin and skeletal system disorders | ||||
| model of bone loss induced by ovariectomy | inhibition of osteoclastogenesis; anti-osteoporotic in vivo animal model; female C57BL6 mice; n = 10/group | 1. normal control 2. ovariectomized mice 3. ovariectomized mice and juglanin (10 mg/kg intraperitoneal injection every two days for 8 weeks) | ↓ bone loss (↓ number of osteoclasts, ↑ bone volume/tissue volume, ↑ trabecular number, ↓ trabecular separation, trabecular thickness not changed); group 3 compared to group 2 | [82] |
| osteoclastogenesis | inhibition of osteoclastogenesis, anti-osteoporotic in vitro cellular study; bone marrow mononuclear cells BMMs (extract from C57BL/6 mice); macrophage call line RAW264.7; bone marrow stromal cells (BMSCs) | 1. normal control 2. cells with RANKL (differentiation of osteoclasts) 3. cells with RANKL and juglanin (20, 40, 80 μmol/L) | ↓ number of osteoclasts **; ↓ osteoclasts function (↓ the size of F-actine ring and number of nuclei **, ↓ the resorptive function of osteoclasts **); ↓ RANKL-induced osteoclast formation at early stage; ↓ osteoclastogenic gene expression (of c-Fos **, TRAcP **, MMP-9 ** and CTSK **); ↓ NFATc1 ** transcriptional activity and V-ATP-ase-d2 expression; ↓ NF-κB * transcriptional activity, phosphorylation of IκBα, p65 and p50, and p65 nuclear translocation; no inhibitory or promotive effect on BMSCs differentiation (alkaline phosphatase and alizarin red staining assays) group 3 compared to group 2; ** juglanin at 20–80 μmol/L; * juglanin at 40–80 μmol/L; juglanin at 80 μmol/L for other results | |
| osteoarthritis | anti-inflammatory; in vitro cellular study; primary human osteoarthritis chondrocyte culture | 1. normal control 2. inflammation induced by IL-1β 3–5. cells with IL-1β and juglanin (10, 20 or 40 μM) | ↑ cell viability; ↓ NO and PGE2 production, ↓ iNOS and COX-2 mRNA and protein expression; ↓ TNF-α, IL-6, MMP-1, MMP-3, MMP-13 levels; ↓ expression of ADAMTS-4 and ADAMTS-5; ↓ p-p65 and ↑ IκBα expression (NF–κB pathway) Groups 3–5 compared to group 2 for all tests | [13] |
| arthritis | anti-inflammatory, antioxidant; in vitro cellular study; chondrogenic ATDC5 cells | 1. normal control 2. cells with LPS 3–4. cells with LPS and juglanin (2.5 or 5 μM) | ↓ oxidative stress (↓ ROS level, ↑ SOD activity, ↓ NOX-4 expression); ↓ activation of the NLRP3 inflammasome complex (↓ TxNIP gene and protein levels, ↓ NLRP3, ACS, P10 levels); ↓ IL-1β and IL-18 secretion; ↑ SIRT1 gene and protein levels (silencing of SIRT1 abolished the effects of juglanin against activation of NLRP3 inflammasome) groups 3–4 compared to group 2 for all tests | [91] |
| adjuvant-induced arthritis (AIA) by Freund’s complete | anti-inflammatory, antioxidant, hepatoprotective; in vivo animal model; female Wistar rats; n = 12/group | 1. normal control 2. AIA control 3. AIA and leflunomide (10 mg/kg) 4–6. AIA and juglanin (10, 20, 40 mg/kg p.o), duration 16 days | ↓ levels of hepatic TNF-α, IL-6, TNF-α, TGF-β, COX-2 and iNOS mRNA; ↓ hepatic NF-κB, IκBα, ADAMTS-4, and ADAMTS-5 proteins expression; ↓ hepatic NO and MDA levels; ↑ hepatic GSH and SOD levels; ↓ rheumatoid factor ↓ level of TG, LDL-C, TC, and VLDL-C; ↑ levels of HDL-C; ↓ serum AST, ALT, ALP, and CRP levels; ↑ level of albumin in serum; ↑ levels of RBC and Hb; ↓ level of WBC, platelets and ESR ↑ body and liver weight; ↑ paw withdrawal latency and threshold; ↓ joint diameter and paw volume attenuation of inflammatory cells infiltration, and cartilage and synovial destruction (histopathological analysis) groups 5–6 compared to group 2 for all tests (dose of juglanin 20–40 mg/kg); effects comparable to after leflunomide (10 mg/kg) treatment | [92] |
| Discussed mainly in Section 5.8: Juglanin and anti-cancer potential | ||||
| skin cancer induced by UVB | anti-inflammatory, pro-apoptotic, anti-cancer; in vivo animal model; hairless SKH-1 mice; n = 10/group | 1. normal control 2. UVB irradiation group (twice a week) 3–4. UVB irradiation and juglanin (10 or 20 mg/kg p.o., twice per week), duration 10 weeks | ↓ skin vasculate *, epidermal hyperplasia and inflammatory cell infiltration *; ↓ KI67 * expression (marker of proliferation); ↓ p-p38/p38, p-JNK/JNK *, PI3K/GAPDH *, p-AKT/AKT *, p-mTOR/mTOR *; ↓ inflammation (↓ IL-1β *, IL-18 *, TNF-α *, p-NF-κB/NF-κB *); ↓ expression of cycline D1 *, CDK1 *, PCNA *, ↑ expression of p53 *, p27 *, p21 *; ↑ caspase-3 *, caspase-8 *, and PARP-1 * levels (enhanced apoptotic cell death) * juglanin 10–20 mg/kg groups vs. UVB control group; juglanin at 20 mg/kg group vs. UVB control for other results | [81] |
| anti-inflammatory, pro-apoptotic; in vitro cellular study; B16F10 murine melanoma cells (tumor line) | 1. control cells 2. cells treated with UVB 3. cells treated with UVB and juglanin (2.5–20 μM) | ↓ cells proliferation *# (MTS cell proliferation colorimetric assay–mitochondrial activity); ↑ apoptotic cells *; ↑ caspase-3 *, caspase-8 *, and PARP * levels; Inhibition of cells proliferation (↓ levels of p-p38 *, p-JNK/JNK *,p-NF-κB *; ↑ levels of p53 *#, p27 *#, p21 *#) # group 3 compared to group 2; *Group 3 compared to group 1 | ||
| breast cancer (tumor-transplanted mouse model) | anti-cancer, pro-apoptotic; in vivo animal model; male BALB/c-nude mice; n = 10/group | 1. mice with breast cancer xenograft 2–3. mice with breast cancer and juglanin 5 or 10 mg/kg/day p.o.), duration 7 days | body weight not changed; ↓ tumor volume; ↑ level of cleaved caspase-9 and caspase-3, LC3BI, LC3BII and phosphorylated JNK; ↑ dead cells and expression level of cleaved caspase-9 groups 2 and 3 compared to group 2 for all tests | [77] |
| breast cancer | anti-cancer, pro-apoptotic; in vitro cellular study; human breast cancer cell lines MCF-7, SKBR3 (for all tests), MDA-MB-231 and BT474 (only for the viability test) | 1. breast cancer cells 2. cells with juglanin (2.5, 5, 10 μM for all tests, and up to 40 μM for the viability test) | ↓ cell proliferation (↓ cell viability at 10–40 μM for all cell lines; MTS cell proliferation colorimetric assay–mitochondrial activity); ↓ the number of cell colonies, induction of G2/M phase arrest (↑ phosphorylation of Chk2, Cdc25C, Cdc2, ↑ p27, ↓ cyclin D); ↑ apoptotic cells level (↓ Bcl-2 # expression, ↑ Bad # and Bax # level, ↑ expression of cleaved casapse-9 #, casapse-8 # and caspase-3 #); ↑ autophagy (↑ production of ROS and ↑ activation of JNK #) group 2 compared to group 1 for all tests; # lack of statistics; juglanin at 2.5–10 μM for other results | |
| xenograft tumor model (lung cancer cells A549 transplantation) | anti-cancer, pro-apoptotic, autophagy induction in vivo animal model; athymic, nude mice; n = 10/group | 1. mice with cancer 2–4. sick mice with juglanin (10, 20 or 30 mg/kg/day p.o.), duration 28 days | body weight and liver mass not changed; ↓ tumor volume and weight (after 28 days); ↓ tumor KI-67 positive cells *, ↑ autophagy and apoptosis levels; ↑ cleavage of Caspase-3 * and PARP *; ↓ Bcl-2 * and ↑ Bax * levels; ↑ p53, TRAIL, DR4, DR5 and FADD mRNA expression; ↑ IκBα, ↓ p-IκBα * and p-NF-κB * protein levels; ↓ PI3K*, AKT*, and ERK1/2 phosphorylation, ↑ p-p38; ↑ LC3 I/II, ATG-7, Beclin-1 and PIK3C3 expression groups 2–4 compared to group 1 for all tests; * juglanin at 20–30 mg/kg; juglanin at 10–30 mg/kg for other results | [8] |
| lung cancer | anti-cancer, pro-oxidant, pro-apoptotic, autophagy induction in vitro cellular study; lung cancer cell lines A549, H1975 (and HCC827 only for viability test) | 1. cancer cells 2. A549 or H1975 cells and juglanin (20, 30, 40 μM) | ↓ cells viability (10–80 μM for A549 cells, 5–80 μM for H1975 and HCC827 cells; MTT assay–mitochondrial activity); chromatin condensation *; ↑ apoptotic cells *; ↑ cleavage of caspase-8 ***, caspase-9 ***/**, caspase-3 ***, and PARP ***/**; ↓ Bcl-2 ***/** and Bcl-xL **/*, ↑ Bax ** and Bad *** levels; (effects on caspase-9, caspase-3 and call viability reversed with caspase inhibitors); ↑ TRAIL ***/**, DR4 ***, DR5 *** and FADD *** mRNA levels, ↑ c-Abl ***, p73 ***/** and p53 *** protein levels (effects reversed with the p53 inhibitor, resulted in apoptotic cells ↓); regulation of NF-κB, PI3K/AKT and MAPKs signaling pathways: ↓ NF-κB ***/**, p-IκBα **, p-PI3K **/***, p-AKT ***/**, p-ERK1/2 *** protein levels, ↑ IκBα */**, p-p38 ***, p-JNK *** and p-cJun *** protein levels (apoptosis enhanced with the use of PI3K/AKT inhibitor or p38 activator or ERK1/2 inhibitor or JNK activator); ↑ ROS production * (the effects on cell viability and apoptosis reversed with the use of ROS scavenger); autophagy induction: ↑ LC3 ***, ATG-7 ***, ATG-3 **, Beclin-1 **/***, PIK3C3 ***, and AMBRA1 **/*** levels group 2 compared to group 1 for all tests; * juglanin at 40 μM, ** juglanin at 30–40 μM, *** juglanin at 20–40 μM (active dose for A549/H1975 cells) | |
| cancer | cytotoxic; in vitro cellular study on different human cancer cell lines | positive control: doxorubicin (IC50 = 0.001–0.02 µM depending on cell lines) | no toxicity observed based on sulforhodamine B assay–protein content, IC50 > 100 µM on A549 (non-small cell lung adenocarcinoma), SK-OV-3 (ovarian cancer cells), SK-MEL-2 (skin melanoma cells), HCT-15 (colon cancer cells)—no effects on cells proliferation | [25] |
| cancer | cytotoxic; in vitro cellular study on Ehrlich ascitis carcinoma cells | cells treated with juglanin 25, 50 or 100 μg/mL | ↓ cells viability (>90% inhibition) | [30] |
| Discussed mainly in Section 5.9: Juglanin and antifungal, antiviral and antiparasitic potential | ||||
| fungal infections | antifungal; in vitro study | positive control: fluconazole | Candida albicans: for ATCC 90028, 03, 48, 111, 181 strains MIC > 128 μg/mL; for the 02 strain MIC = 128 μg/mL (fluconazole = 2 μg/mL); for the 138 strain MIC = 16 μg/mL (fluconazole = 8 μg/mL); Candida parapsilosis: for the ATCC 22019 strain MIC = 128 μg/mL; for the 11 strain MIC = 64 μg/mL (fluconazole = 1 μg/mL) | [33] |
| malaria | antiplasmodial, cytotoxic; in vitro study on Plasmodium falciparum strain 3D7 and HeLa (human cervix adenocarcinoma) cells | positive controls: chloroquine (IC50 = 0.014 µM) for Plasmodium 3D7; emetin (IC50 = 0.04 µM) for HeLa (human cervix adenocarcinoma) cells | ↓ parasite viability (about 16.5% viability at 120 µM and about 73.6% viability at 24 µM); ↓ HeLa cells viability (about 2.8% viability at 120 µM and about 71.8% viability at 24 µM) | [35] |
| virus infections (e.g., SARS coronavirus) | anti-viral; in vitro cellular study on Xenopus oocyte cells with a heterologously expressed 3a protein | - | IC50 of 3a-protein channel = 2.3 µM; at 10 and 20 µM near-complete and complete inhibition—juglanin activity was the highest from all tested flavonoids, potential to ↓ virus release | [93] |
| SARS-CoV-2 | anti-viral; computational studies: QSAR analysis and molecular docking studies | positive control: remdesivir | potential inhibition of the 3CLPRO of SARS-CoV-2 (the best binding score from 23 tested flavonoids, better than positive control), potential to ↓ viral replication complex and transcription | [94] |
| anti-viral; computational studies: molecular docking studies | positive controls e.g., ritonavir, lopinavir, trametinib, selumetinib | good binding affinity to 3CLPRO (better than ritonavir and lopinavir), PLPRO (better than lopinavir), ABL1 (better than selumetinib, worse than trametinib), and TMPRSS2; no effect on RdRp, non-structural proteins (nsp10, nsp14, nsp15, nsp16), hACE2R, S protein, NFAT | [95] | |
| influenza | anti-viral; molecular docking studies | - | good binding affinity to the surface glycoproteins of influenza virus (hemagglutinin and neuraminidase) | [96] |
| dengue disease | anti-viral; computational studies: QSAR analysis and molecular docking studies | positive controls: octyl beta-D-glucopyranoside and 2-acetamido-2-deoxy-beta-D-glucopyranose | potential inhibition of dengue virus 2 (DENV2) envelope protein (the lowest atomic contact energy (ACE) score in the molecular docking studies of 54 flavonoids, both the docking score and ACE score better than the positive controls, but unstable conformation based on molecular dynamic simulation) | [97] |
| Discussed mainly in Section 5.10: other effects | ||||
| - | enzyme inhibitory potential; computational studies: structural activity relationship analysis using density functional theory | - | prediction of affinity toward enzymes: the best for lyase (26.65%), next family A-G protein coupled receptor (19.96%), next hydrolase/kinase/oxidoreductase/phosphodiesterase (6.69%) | [98] |
| diabetes | improvement of diabetes complications; in vitro rat lens aldose reductase inhibition | 73 flavonoids tested, no positive control | 64.8% inhibition at 10 µM; 6.3% inhibition at 1µM | [99] |
| hearing loss | cell-protective; in vivo animal model; wild-type larvae zebrafish (Danio rerio); n = unknown | 1. normal control 2. neomycin-induced hair cell damage 3. neomycin and juglanin (1 µM for 8h) | ↑ number of otic hair cells (significant but moderate effect) group 3 compared to group 2 for all tests | [36] |
| cell-protective; in vitro cellular study; mouse auditory cell line HEI-OC1 | 1. normal control 2. neomycin-induced cell damage 3. neomycin and juglanin (1 µM) | ↑ cell viability (from about 63% to about 95%) group 3 compared to group 2 for all tests | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rutkowska, M.; Witek, M.; Olszewska, M.A. A Comprehensive Review of Molecular Mechanisms, Pharmacokinetics, Toxicology and Plant Sources of Juglanin: Current Landscape and Future Perspectives. Int. J. Mol. Sci. 2024, 25, 10323. https://doi.org/10.3390/ijms251910323
Rutkowska M, Witek M, Olszewska MA. A Comprehensive Review of Molecular Mechanisms, Pharmacokinetics, Toxicology and Plant Sources of Juglanin: Current Landscape and Future Perspectives. International Journal of Molecular Sciences. 2024; 25(19):10323. https://doi.org/10.3390/ijms251910323
Chicago/Turabian StyleRutkowska, Magdalena, Martyna Witek, and Monika A. Olszewska. 2024. "A Comprehensive Review of Molecular Mechanisms, Pharmacokinetics, Toxicology and Plant Sources of Juglanin: Current Landscape and Future Perspectives" International Journal of Molecular Sciences 25, no. 19: 10323. https://doi.org/10.3390/ijms251910323
APA StyleRutkowska, M., Witek, M., & Olszewska, M. A. (2024). A Comprehensive Review of Molecular Mechanisms, Pharmacokinetics, Toxicology and Plant Sources of Juglanin: Current Landscape and Future Perspectives. International Journal of Molecular Sciences, 25(19), 10323. https://doi.org/10.3390/ijms251910323






