Applications of Platelet Concentrates (PCs) in Regenerative Onco-Urology: A Systematic Review of Literature
Abstract
1. Introduction
2. Methods
2.1. Registration and PRISMA Documents
2.2. Search Strings
- MEDLINE via PubMed (https://pubmed.ncbi.nlm.nih.gov/, accessed on 24 April 2024)
- ◦
- (“Radiation Cystitis” OR “Hemorrhagic Cystitis” OR “Actinic Cystitis” OR “Urethral Obstruction” OR “Urethral Stenosis”) AND (“Platelet-Rich Plasma” OR “PRP” OR “Platelet-Rich Fibrin” OR “PRF” OR “Platelet Concentrate” OR “Platelet Gel” OR “Platelet Derivatives”)
- CochraneLibrary (https://www.cochranelibrary.com/, accessed on 24 April 2024)
- ◦
- (see Table 1)
| ID | Search | Hits |
|---|---|---|
| 1 | Radiation Cystitis | 188 |
| 2 | Hemorrhagic Cystitis | 164 |
| 3 | Actinic Cystitis | 2 |
| 4 | Urethral Obstruction | 358 |
| 5 | Urethral Stenosis | 444 |
| 6 | Platelet-Rich Plasma | 3418 |
| 7 | PRP | 3658 |
| 8 | Platelet-Rich Fibrin | 1441 |
| 9 | PRF | 1685 |
| 10 | Platelet Concentrate | 848 |
| 11 | Platelet Gel | 496 |
| 12 | Platelet Derivatives | 2928 |
| 13 | #1 OR #2 OR #3 OR #4 OR #5 | 1065 |
| 14 | #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 | 10,003 |
| 15 | #13 AND #14 | 7 |
- ELSEVIER via ScienceDirect (https://www.sciencedirect.com/, accessed on 24 April 2024, three different searches for the limit set up to eight Boolean)
- ◦
- “Radiation Cystitis” AND (“Platelet-Rich Plasma” OR “PRP” OR “Platelet-Rich Fibrin” OR “PRF” OR “Platelet Concentrate” OR “Platelet Gel” OR “Platelet Derivatives”);
- ◦
- (“Hemorrhagic Cystitis” OR “Actinic Cystitis”) AND (“Platelet-Rich Plasma” OR “PRP” OR “Platelet-Rich Fibrin” OR “PRF” OR “Platelet Concentrate” OR “Platelet Gel” OR “Platelet Derivatives”);
- ◦
- (“Urethral Obstruction” OR “Urethral Stenosis”) AND (“Platelet-Rich Plasma” OR “PRP” OR “Platelet-Rich Fibrin” OR “PRF” OR “Platelet Concentrate” OR “Platelet Gel” OR “Platelet Derivatives”).
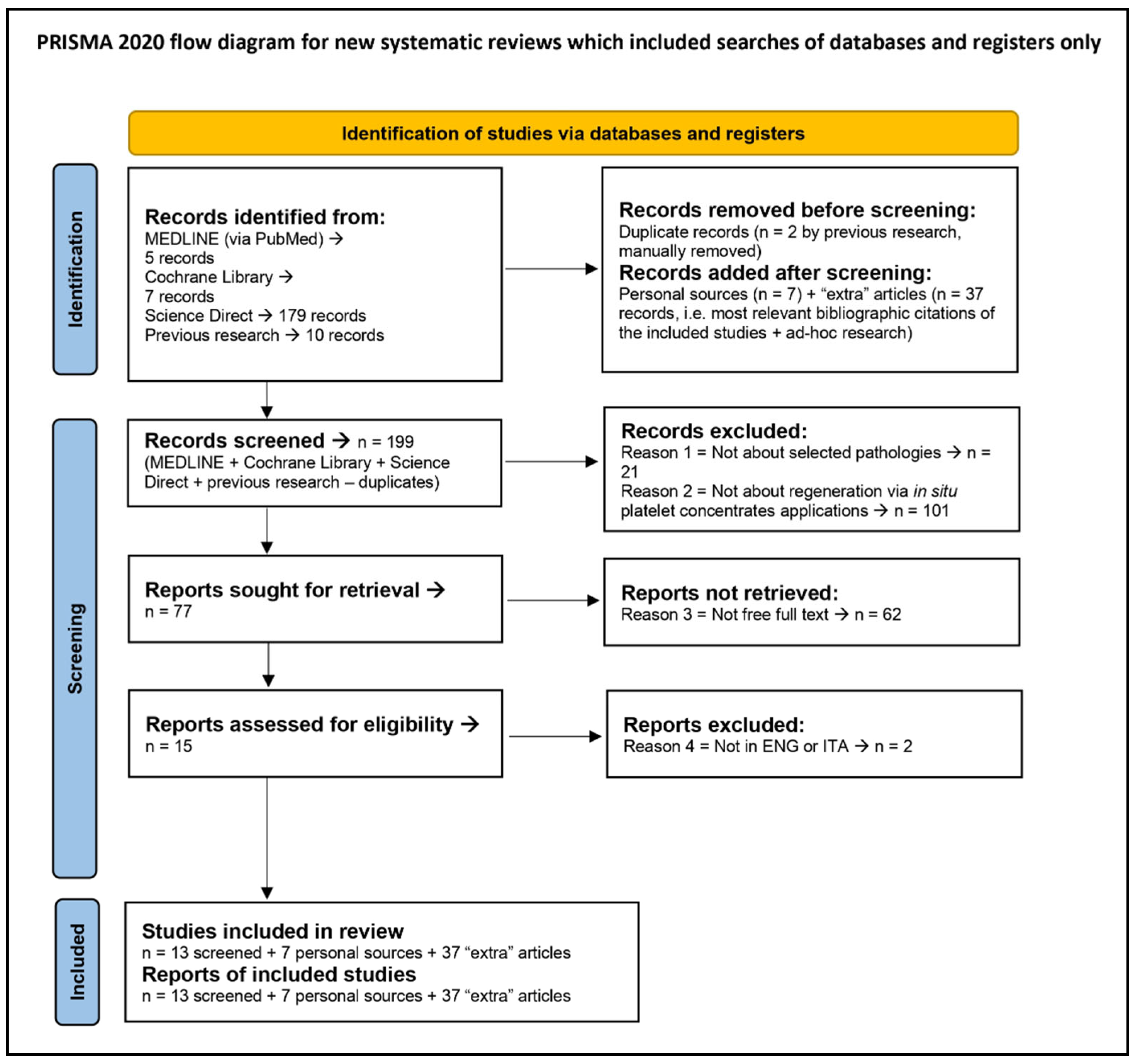
2.3. Eligibility Criteria and Screening Results
2.4. Data Extraction and Interpretation
2.5. Criteria for QA
3. Results
3.1. PRISMA 2020 Flow Diagram, Table of Results and Quality Assessment (QA)
3.2. Hemorrhagic, Actinic and Radiation Cystitis Treatment with PCs
3.3. Urethral Obstruction or Stenosis Treatment with PCs
3.4. PRP Preparation Protocols
| Article | PC’s Name | Preparation Protocol |
|---|---|---|
| Abbruzzese, et al. [20] | PL |
|
| Dönmez, et al. [16] | PRP | Protocol by Nagae et al. [61]:
|
| Chen, et al. [29] | PRP | Protocol by Nagae et al. [61]: |
| Masieri, et al. [30] | Platelet gel |
|
| Ozyuvali, et al. [32] | PRP |
|
3.5. AE Assessment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ke, Q.S.; Jhang, J.F.; Lin, T.Y.; Ho, H.C.; Jiang, Y.H.; Hsu, Y.H.; Kuo, H.C. Therapeutic potential of intravesical injections of platelet-rich plasma in the treatment of lower urinary tract disorders due to regenerative deficiency. Ci Ji Yi Xue Za Zhi 2019, 31, 135–143. [Google Scholar] [CrossRef] [PubMed]
- Yáñez-Castillo, Y.M.; Arrabal-Polo, M. Applications of Platelet Rich Plasma in Urology. Arch. Esp. Urol. 2022, 75, 669–683. [Google Scholar] [CrossRef] [PubMed]
- Gottardo, A.; Gristina, V.; Perez, A.; Di Giovanni, E.; Contino, S.; Barraco, N.; Bono, M.; Iannì, G.; Randazzo, U.; Bazan Russo, T.D.; et al. Roles of Tumor-Educated Platelets (TEPs) in the biology of Non-Small Cell Lung Cancer (NSCLC): A systematic review. “Re-discovering the neglected biosources of the liquid biopsy family”. J. Liq. Biopsy 2024, 3, 100136. [Google Scholar] [CrossRef]
- Tutino, R.; Di Franco, S.; Massani, M.; Bonventre, S.; Mazzola, G.; Lo Re, G.; Gulotta, E.; Kamdem Mambou, L.J.; Stassi, G.; Cocorullo, G.; et al. Autologous adipose-derived stromal vascular fraction and platelet concentrates for the treatment of complex perianal fistulas. Tech. Coloproctol. 2023, 27, 135–143. [Google Scholar] [CrossRef]
- Palumbo, V.D.; Rizzuto, S.; Damiano, G.; Fazzotta, S.; Gottardo, A.; Mazzola, G.; Lo Monte, A.I. Use of platelet concentrate gel in second-intention wound healing: A case report. J. Med. Case Rep. 2021, 15, 85. [Google Scholar] [CrossRef]
- Su, C.Y.; Kuo, Y.P.; Tseng, Y.H.; Su, C.H.; Burnouf, T. In vitro release of growth factors from platelet-rich fibrin (PRF): A proposal to optimize the clinical applications of PRF. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 108, 56–61. [Google Scholar] [CrossRef]
- Jhang, J.F.; Wu, S.Y.; Lin, T.Y.; Kuo, H.C. Repeated intravesical injections of platelet-rich plasma are effective in the treatment of interstitial cystitis: A case control pilot study. Low. Urin. Tract Symptoms 2019, 11, O42–O47. [Google Scholar] [CrossRef]
- Soyer, T.; Ayva, Ş.; Boybeyi, Ö.; Aslan, M.K.; Çakmak, M. The effect of platelet rich fibrin on growth factor levels in urethral repair. J. Pediatr. Surg. 2013, 48, 2545–2549. [Google Scholar] [CrossRef]
- Mussano, F.; Genova, T.; Munaron, L.; Petrillo, S.; Erovigni, F.; Carossa, S. Cytokine, chemokine, and growth factor profile of platelet-rich plasma. Platelets 2016, 27, 467–471. [Google Scholar] [CrossRef]
- Roy, S.; Driggs, J.; Elgharably, H.; Biswas, S.; Findley, M.; Khanna, S.; Gnyawali, U.; Bergdall, V.K.; Sen, C.K. Platelet-rich fibrin matrix improves wound angiogenesis via inducing endothelial cell proliferation. Wound Repair Regen. 2011, 19, 753–766. [Google Scholar] [CrossRef]
- Burgu, B.; Woolf, A.; Medina-Ortiz, W.; Pitera, J.E.; Wilcox, D.T. The Developing Bladder is Hypoxic in Vivo and Bladder Angiogenesis is Controlled Through VEGF by Tissue Oxygenisation. J. Pediatr. Urol. 2007, 3, S34. [Google Scholar] [CrossRef]
- Kuo, H.C. Intravesical injections of autologous platelet-rich plasma for the treatment of refractory interstitial cystitis. Low. Urin. Tract Symptoms 2023, 15, 210–215. [Google Scholar] [CrossRef]
- Wu, Y.; Wang, J.; Scott, P.G.; Tredget, E.E. Bone marrow-derived stem cells in wound healing: A review. Wound Repair Regen. 2007, 15 (Suppl. 1), S18–S26. [Google Scholar] [CrossRef] [PubMed]
- Scull, C.M.; Hays, W.D.; Fischer, T.H. Macrophage pro-inflammatory cytokine secretion is enhanced following interaction with autologous platelets. J. Inflamm. 2010, 7, 53. [Google Scholar] [CrossRef] [PubMed]
- Kuffler, D.P. Platelet-rich plasma and the elimination of neuropathic pain. Mol. Neurobiol. 2013, 48, 315–332. [Google Scholar] [CrossRef]
- Dönmez, M.; İnci, K.; Zeybek, N.D.; Doğan, H.S.; Ergen, A. The Early Histological Effects of Intravesical Instillation of Platelet-Rich Plasma in Cystitis Models. Int. Neurourol. J. 2016, 20, 188–196. [Google Scholar] [CrossRef]
- Jefferson, F.A.; Linder, B.J. Hemorrhagic Cystitis: Making Rapid and Shrewd Clinical and Surgical Decisions for Improving Patient Outcomes. Res. Rep. Urol. 2023, 15, 291–303. [Google Scholar] [CrossRef]
- Gilis, L.; Morisset, S.; Billaud, G.; Ducastelle-Leprêtre, S.; Labussière-Wallet, H.; Nicolini, F.E.; Barraco, F.; Detrait, M.; Thomas, X.; Tedone, N.; et al. High burden of BK virus-associated hemorrhagic cystitis in patients undergoing allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant. 2014, 49, 664–670. [Google Scholar] [CrossRef]
- Saade, A.; Styczynski, J.; Cesaro, S.; Infectious Disease Working party of EBMT. BK virus infection in allogeneic hematopoietic cell transplantation: An update on pathogenesis, immune responses, diagnosis and treatments. J. Infect. 2020, 81, 372–382. [Google Scholar] [CrossRef]
- Abbruzzese, L.; Nescis, E.; Turco, E.; Amoroso, P.; Carluccio, G. Efficacy of allogeneic platelet growth factors in actinic cystitis: The resolution of trouble? Transfus. Apher. Sci. 2023, 62, 103732. [Google Scholar] [CrossRef]
- Liu, P.; Bai, K.; Zhang, Z.; Sun, J. Analysis of early clinical signs and risk factors for severe hemorrhagic cystitis after stem cell transplantation in children. Int. J. Urol. 2024, 31, 335–341. [Google Scholar] [CrossRef] [PubMed]
- Abbasi, B.; Shaw, N.M.; Lui, J.L.; Li, K.D.; Sudhakar, A.; Low, P.; Hakam, N.; Nabavizadeh, B.; Breyer, B.N. Posterior urethral stenosis: A comparative review of the guidelines. World J. Urol. 2022, 40, 2591–2600. [Google Scholar] [CrossRef] [PubMed]
- Mathes, T.; Pieper, D. Clarifying the distinction between case series and cohort studies in systematic reviews of comparative studies: Potential impact on body of evidence and workload. BMC Med. Res. Methodol. 2017, 17, 107. [Google Scholar] [CrossRef] [PubMed]
- Mann, C.J. Observational research methods. Research design II: Cohort, cross sectional, and case-control studies. Emerg. Med. J. 2003, 20, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Hooijmans, C.R.; Rovers, M.M.; de Vries, R.B.; Leenaars, M.; Ritskes-Hoitinga, M.; Langendam, M.W. SYRCLE's risk of bias tool for animal studies. BMC Med. Res. Methodol. 2014, 14, 43. [Google Scholar] [CrossRef]
- Daramola, O.O.; Rhee, J.S. Rating Evidence in Medical Literature. 2011. Available online: https://journalofethics.ama-assn.org/article/rating-evidence-medical-literature/2011-01 (accessed on 1 August 2024).
- National Heart, Lung, and Blood Institute (NHLBI), Bethesda, Maryland, United States. Study Quality Assessment Tools; National Institutes of Health (NIH). 2021. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 1 August 2024).
- Trama, F.; Illiano, E.; Marchesi, A.; Brancorsini, S.; Crocetto, F.; Pandolfo, S.D.; Zucchi, A.; Costantini, E. Use of Intravesical Injections of Platelet-Rich Plasma for the Treatment of Bladder Pain Syndrome: A Comprehensive Literature Review. Antibiotics 2021, 10, 1194. [Google Scholar] [CrossRef]
- Chen, Y.H.; Man, K.M.; Chen, W.C.; Liu, P.L.; Tsai, K.S.; Tsai, M.Y.; Wu, Y.T.; Chen, H.Y. Platelet-Rich Plasma Ameliorates Cyclophosphamide-Induced Acute Interstitial Cystitis/Painful Bladder Syndrome in a Rat Model. Diagnostics 2020, 10, 381. [Google Scholar] [CrossRef]
- Masieri, L.; Sessa, F.; Mari, A.; Campi, R.; Cito, G.; Verrienti, P.; Nozzoli, C.; Saccardi, R.; Sforza, S.; Di Maida, F.; et al. Intravesical application of platelet-rich plasma in patients with persistent haemorrhagic cystitis after hematopoietic stem cell transplantation: A single-centre preliminary experience. Int. Urol. Nephrol. 2019, 51, 1715–1720. [Google Scholar] [CrossRef]
- Ninan, N.; Thomas, S.; Grohens, Y. Wound healing in urology. Adv. Drug Deliv. Rev. 2015, 82–83, 93–105. [Google Scholar] [CrossRef]
- Ozyuvali, E.; Yildirim, M.E.; Yaman, T.; Kosem, B.; Atli, O.; Cimentepe, E. Protective Effect of Intravesical Platelet-Rich Plasma on Cyclophosphamide-Induced Hemorrhagic Cystitis. Clin. Investig. Med. 2016, 39, 27514. [Google Scholar]
- Spartalis, E.; Tsilimigras, D.I.; Sfoungaristos, S. Letter to the editor: Safety and feasibility of platelet rich fibrin matrix injections for treatment of common urologic conditions. Investig. Clin. Urol. 2018, 59, 280–281. [Google Scholar] [CrossRef] [PubMed]
- Pascoe, C.; Duncan, C.; Lamb, B.W.; Davis, N.F.; Lynch, T.H.; Murphy, D.G.; Lawrentschuk, N. Current management of radiation cystitis: A review and practical guide to clinical management. BJU Int. 2019, 123, 585–594. [Google Scholar] [CrossRef] [PubMed]
- Smit, S.G.; Heyns, C.F. Management of radiation cystitis. Nat. Rev. Urol. 2010, 7, 206–214. [Google Scholar] [CrossRef] [PubMed]
- Zelefsky, M.J.; Chan, H.; Hunt, M.; Yamada, Y.; Shippy, A.M.; Amols, H. Long-term outcome of high dose intensity modulated radiation therapy for patients with clinically localized prostate cancer. J. Urol. 2006, 176, 1415–1419. [Google Scholar] [CrossRef] [PubMed]
- Marks, L.B.; Carroll, P.R.; Dugan, T.C.; Anscher, M.S. The response of the urinary bladder, urethra, and ureter to radiation and chemotherapy. Int. J. Radiat. Oncol. Biol. Phys. 1995, 31, 1257–1280. [Google Scholar] [CrossRef]
- Linder, B.J.; Tarrell, R.F.; Boorjian, S.A. Cystectomy for refractory hemorrhagic cystitis: Contemporary etiology, presentation and outcomes. J. Urol. 2014, 192, 1687–1692. [Google Scholar] [CrossRef]
- Tirindelli, M.C.; Flammia, G.P.; Bove, P.; Cerretti, R.; Cudillo, L.; De Angelis, G.; Picardi, A.; Annibali, O.; Nobile, C.; Cerchiara, E.; et al. Fibrin glue therapy for severe hemorrhagic cystitis after allogeneic hematopoietic stem cell transplantation. Biol. Blood Marrow Transplant. 2014, 20, 1612–1617. [Google Scholar] [CrossRef]
- Alomari, E.B.; Sultan, K. Efficacy of injectable platelet-rich plasma in reducing alveolar bone resorption following rapid maxillary expansion: A cone-beam computed tomography assessment in a randomized split-mouth controlled trial. Angle Orthod. 2019, 89, 705–712. [Google Scholar] [CrossRef]
- Hurley, E.T.; Maye, A.B.; Mullett, H. Arthroscopic Rotator Cuff Repair: A Systematic Review of Overlapping Meta-Analyses. JBJS Rev. 2019, 7, e1. [Google Scholar] [CrossRef]
- Griffin, M.F.; Naderi, N.; Kalaskar, D.M.; Seifalian, A.M.; Butler, P.E. Argon plasma surface modification promotes the therapeutic angiogenesis and tissue formation of tissue-engineered scaffolds in vivo by adipose-derived stem cells. Stem Cell Res. Ther. 2019, 10, 110. [Google Scholar] [CrossRef]
- Pereira, R.C.D.F.; De La Côrte, F.D.; Brass, K.E.; da Silva Azevedo, M.; Gallio, M.; Cantarelli, C.; Dau, S.L.; Cezar, A.S.; Inkelmann, M.A. Evaluation of Three Methods of Platelet-Rich Plasma for Treatment of Equine Distal Limb Skin Wounds. J. Equine Vet. Sci. 2019, 72, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Bennett, N.T.; Schultz, G.S. Growth factors and wound healing: Biochemical properties of growth factors and their receptors. Am. J. Surg. 1993, 165, 728–737. [Google Scholar] [CrossRef]
- Persu, C.; Ciofu, I.; Petrescu, A.; Chirca, N.; Cauni, V. Bladder Wall Structure Alterations in Patients Treated With Botulinum Toxin for Detrusor Overactivity—A Morphological Study. In Vivo 2023, 37, 898–903. [Google Scholar] [CrossRef] [PubMed]
- Jhang, J.F.; Yu, W.R.; Kuo, H.C. Comparison of the Clinical Efficacy and Adverse Events between Intravesical Injections of Platelet-Rich Plasma and Botulinum Toxin A for the Treatment of Interstitial Cystitis Refractory to Conventional Treatment. Toxins 2023, 15, 121. [Google Scholar] [CrossRef] [PubMed]
- Frey, C.; Yeh, P.C.; Jayaram, P. Effects of Antiplatelet and Nonsteroidal Anti-inflammatory Medications on Platelet-Rich Plasma: A Systematic Review. Orthop. J. Sports Med. 2020, 8, 2325967120912841. [Google Scholar] [CrossRef]
- Gul, M. Modified platelet-rich plasma with transforming growth factor β1 neutralization antibody injection may reduce recurrence rate of urethral stricture. Med. Hypotheses 2016, 97, 1–3. [Google Scholar] [CrossRef]
- Kelc, R.; Trapecar, M.; Gradisnik, L.; Rupnik, M.S.; Vogrin, M. Platelet-rich plasma, especially when combined with a TGF-β inhibitor promotes proliferation, viability and myogenic differentiation of myoblasts in vitro. PLoS ONE 2015, 10, e0117302. [Google Scholar] [CrossRef]
- Li, H.; Hicks, J.J.; Wang, L.; Oyster, N.; Philippon, M.J.; Hurwitz, S.; Hogan, M.V.; Huard, J. Customized platelet-rich plasma with transforming growth factor β1 neutralization antibody to reduce fibrosis in skeletal muscle. Biomaterials 2016, 87, 147–156. [Google Scholar] [CrossRef]
- Scarcia, M.; Maselli, F.P.; Cardo, G.; Ludovico, G.M. The use of autologous platelet rich plasma gel in bulbar and penile buccal mucosa urethroplasty: Preliminary report of our first series. Arch. Ital. Urol. Androl. 2016, 88, 274–278. [Google Scholar] [CrossRef]
- Tavukcu, H.H.; Aytaç, Ö.; Atuğ, F.; Alev, B.; Çevik, Ö.; Bülbül, N.; Yarat, A.; Çetinel, Ş.; Şener, G.; Kulaksızoğlu, H. Protective effect of platelet-rich plasma on urethral injury model of male rats. Neurourol. Urodyn. 2018, 37, 1286–1293. [Google Scholar] [CrossRef]
- Rezaei, M.; Badiei, R. The effect of platelet-rich plasma injection on post-internal urethrotomy stricture recurrence. World J. Urol. 2019, 37, 1959–1964. [Google Scholar] [CrossRef] [PubMed]
- Routh, J.C.; Wolpert, J.J.; Reinberg, Y. Tunneled tunica vaginalis flap for recurrent urethrocutaneous fistulae. Adv. Urol. 2008, 2008, 615928. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Richter, F.; Pinto, P.A.; Stock, J.A.; Hanna, M.K. Management of recurrent urethral fistulas after hypospadias repair. Urology 2003, 61, 448–451. [Google Scholar] [CrossRef] [PubMed]
- Hosseini, J.; Kaviani, A.; Mohammadhosseini, M.; Rezaei, A.; Rezaei, I.; Javanmard, B. Fistula repair after hypospadias surgery using buccal mucosal graft. Urol. J. 2009, 6, 19–22. [Google Scholar] [PubMed]
- Kajbafzadeh, A.M.; Abolghasemi, H.; Eshghi, P.; Alizadeh, F.; Elmi, A.; Shafaattalab, S.; Dianat, S.; Amirizadeh, N.; Mohseni, M.J. Single-donor fibrin sealant for repair of urethrocutaneous fistulae following multiple hypospadias and epispadias repairs. J. Pediatr. Urol. 2011, 7, 422–427. [Google Scholar] [CrossRef]
- Soyer, T.; Çakmak, M.; Aslan, M.K.; Şenyücel, M.F.; Kisa, Ü. Use of autologous platelet rich fibrin in urethracutaneous fistula repair: Preliminary report. Int. Wound J. 2013, 10, 345–347. [Google Scholar] [CrossRef]
- Choukroun, J.; Diss, A.; Simonpieri, A.; Girard, M.O.; Schoeffler, C.; Dohan, S.L.; Dohan, A.J.; Mouhyi, J.; Dohan, D.M. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part IV: Clinical effects on tissue healing. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2006, 101, e56–e60. [Google Scholar] [CrossRef]
- Sunitha Raja, V.; Munirathnam Naidu, E. Platelet-rich fibrin: Evolution of a second-generation platelet concentrate. Indian J. Dent. Res. 2008, 19, 42–46. [Google Scholar] [CrossRef]
- Nagae, M.; Ikeda, T.; Mikami, Y.; Hase, H.; Ozawa, H.; Matsuda, K.; Sakamoto, H.; Tabata, Y.; Kawata, M.; Kubo, T. Intervertebral disc regeneration using platelet-rich plasma and biodegradable gelatin hydrogel microspheres. Tissue Eng. 2007, 13, 147–158. [Google Scholar] [CrossRef]
- Spartalis, E.D.; Tomos, P.; Konofaos, P.; Dimitroulis, D.; Kouraklis, G. Breast reconstruction with autologous fat graft; does platelet-rich plasma affect patient’s survival? Int. J. Clin. Exp. Med. 2014, 7, 329–330. [Google Scholar]
- Sommeling, C.E.; Heyneman, A.; Hoeksema, H.; Verbelen, J.; Stillaert, F.B.; Monstrey, S. The use of platelet-rich plasma in plastic surgery: A systematic review. J. Plast. Reconstr. Aesthetic Surg. 2013, 66, 301–311. [Google Scholar] [CrossRef] [PubMed]
- Russo, S.; Landi, S.; Courric, S. Cost-Effectiveness Analysis for the Treatment of Diabetic Foot Ulcer in France: Platelet-Rich Plasma vs Standard of Care. Clinicoecon. Outcomes Res. 2022, 14, 1–10. [Google Scholar] [CrossRef] [PubMed]
| 1st Author (Year) | ID [cit.] | Topic (Type) | Nr. of Study Subjects | PC | Follow-Up | Treatment Course | QA |
|---|---|---|---|---|---|---|---|
| Abbruzzese L., et al. (2023) | PMID: 37263885 [20] | AC (clinical study = human case series) | 9 humans | PL | 3 months during treatment | 1st month: 3 treatments × week 2nd month: 2 treatments × week 3rd month: 1 treatment × week | Grade C, level 4—6 points out of 9 |
| Chen Y.-H., et al. (2020) | PMID: 32521683 [29] | CYP-induced cystitis (pre-clinical study) | 30 female rats, randomized in 5 groups of 6 subjects:
| PRP | 3 days after treatment | Day 0: saline or CYP application Day 1: treatments Day 4: rats sacrifice | 11 points out of 20 |
| Dönmez M.İ., et al. (2016) | PMID: 27706013 [16] | IC + HC (pre-clinical study) | 36 male rabbits, randomized in 6 groups of 6 subjects:
| PRP | 2 days after treatment | Day 0: saline, HCl, or CYP application Day 1: treatment of group 6 Day 2: treatment of groups 2 + 4 Day 3: group 5 + 6 sacrifice Day 4: other groups sacrifice | 14 points out of 20 |
| Jhang J.F., et al. (2017) | PMID: 29265766 [7] | *IC + others (clinical study)* | *///* | *///* | *///* | *///* | *Grade D, level 5* |
| Ke Q.S., et al. (2019) | PMID: 31258287 [1] | Regenerative urology (review) | /// | /// | /// | /// | Grade D, level 5 |
| Kuo H.-C., et al. (2023) | PMID: 37702275 [12] | IC + others (review) | /// | /// | /// | /// | Grade D, level 5 |
| Masieri L., et al. (2019) | PMID: 31321678 [30] | HC (clinical study = human case series) | 10 humans | Platelet gel | 1 month after treatment | Day 0: treatment 1 month: follow-up | Grade C, level 4—4 points out of 9 |
| Ninan N., et al. (2014) | PMID: 25500273 [31] | Regenerative urology (review) | /// | /// | /// | /// | Grade D, level 5 |
| Ozyuvali E., et al. (2016) | PMID: 27917804 [32] | CYP-induced HC (pre-clinical study) | 24 female rats, randomized in 4 groups of 6 subjects:
| PRP | 6 h after treatment | Day 0: saline or CYP application + group 1 sacrifice Day 1: treatment of group 4 + groups 2 and 3 sacrifice Day 1, 6 h after treatment: group 4 sacrifice | 11 points out of 20 |
| Saade A., et al. (2020) | PMID: 32526327 [19] | HC (review) | /// | /// | /// | /// | Grade D, level 5 |
| Soyer T., et al. (2013) | PMID: 24314201 [8] | Urethral regeneration (pre-clinical study) | 18 rats, divided into 3 groups of 6 subjects:
| PRF | 1 day after treatment | Day 0: sampling and sacrifice of group 1 + treatment of groups 2 and 3 Day 1: sampling and sacrifice of groups 2 and 3 | 8 points out of 20 |
| Spartalis E., et al. (2018) | PMID: 29984344 [33] | PRP in onco-urology (commentary) | /// | /// | /// | /// | Grade D, level 5 |
| Trama F., et al. (2021) | PMID: 34680774 [28] | IC + others (review) | /// | /// | /// | /// | Grade D, level 5 |
| Yáñez-Castillo Y.M., et al. (2022) | DOI: 10.56434/j.arch.esp. urol.20227508.98 [2] | PRP in urology (review) | /// | /// | /// | /// | Grade D, level 5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gottardo, A.; Tulone, G.; Pavan, N.; Fulfaro, F.; Gristina, V.; Bazan Russo, T.D.; Prestifilippo, O.; Claps, F.; Incorvaia, L.; Galvano, A.; et al. Applications of Platelet Concentrates (PCs) in Regenerative Onco-Urology: A Systematic Review of Literature. Int. J. Mol. Sci. 2024, 25, 10683. https://doi.org/10.3390/ijms251910683
Gottardo A, Tulone G, Pavan N, Fulfaro F, Gristina V, Bazan Russo TD, Prestifilippo O, Claps F, Incorvaia L, Galvano A, et al. Applications of Platelet Concentrates (PCs) in Regenerative Onco-Urology: A Systematic Review of Literature. International Journal of Molecular Sciences. 2024; 25(19):10683. https://doi.org/10.3390/ijms251910683
Chicago/Turabian StyleGottardo, Andrea, Gabriele Tulone, Nicola Pavan, Fabio Fulfaro, Valerio Gristina, Tancredi Didier Bazan Russo, Ornella Prestifilippo, Francesco Claps, Lorena Incorvaia, Antonio Galvano, and et al. 2024. "Applications of Platelet Concentrates (PCs) in Regenerative Onco-Urology: A Systematic Review of Literature" International Journal of Molecular Sciences 25, no. 19: 10683. https://doi.org/10.3390/ijms251910683
APA StyleGottardo, A., Tulone, G., Pavan, N., Fulfaro, F., Gristina, V., Bazan Russo, T. D., Prestifilippo, O., Claps, F., Incorvaia, L., Galvano, A., Russo, A., & Simonato, A. (2024). Applications of Platelet Concentrates (PCs) in Regenerative Onco-Urology: A Systematic Review of Literature. International Journal of Molecular Sciences, 25(19), 10683. https://doi.org/10.3390/ijms251910683









