Targeted NGS Revealed Pathogenic Mutation in a 13-Year-Old Patient with Homozygous Familial Hypercholesterolemia: A Case Report
Abstract
:1. Introduction
2. Results
2.1. Case Presentation
2.2. Sequencing Analysis
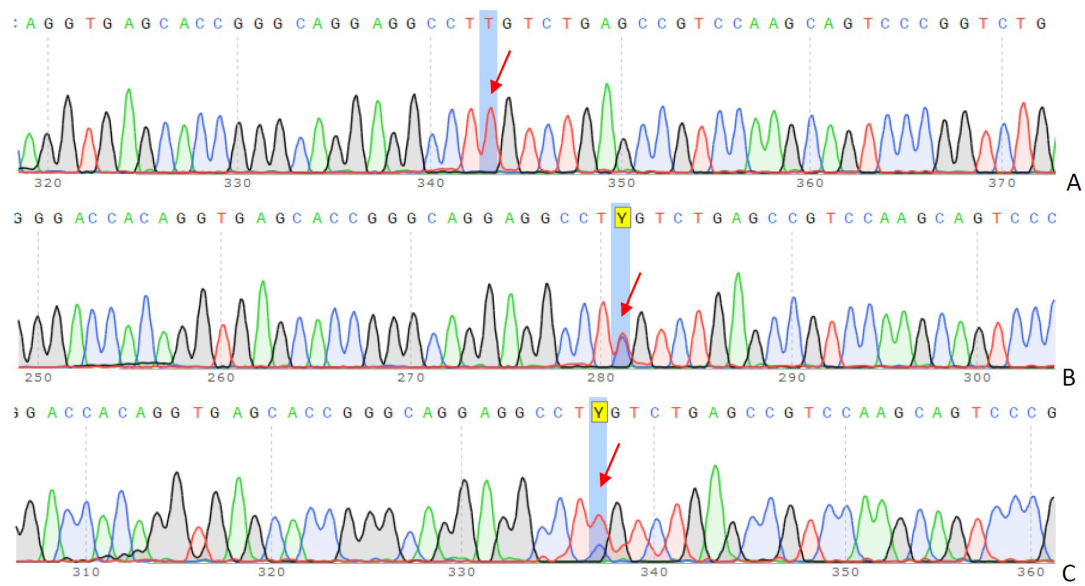
2.3. Validation Sanger Sequencing
2.4. Genetic Counseling
3. Discussion
4. Materials and Methods
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wiegman, A.; Gidding, S.S.; Watts, G.F.; Chapman, M.J.; Ginsberg, H.N.; Cuchel, M.; Ginsberg, H.N. Familial hypercholesterolaemia in children and adolescents: Gaining decades of life by optimizing detection and treatment. Eur. Heart J. 2015, 36, 2425–2437. [Google Scholar] [CrossRef] [PubMed]
- Harada-Shiba, M.; Arai, H.; Ohmura, H.; Okazaki, H.; Sugiyama, D.; Tada, H.; Dobashi, K.; Matsuki, K.; Minamino, T.; Yamashita, S.; et al. Guidelines for the Diagnosis and Treatment of Adult Familial Hypercholesterolemia 2022. J. Atheroscler. Thromb. 2023, 30, 558–586. [Google Scholar] [CrossRef] [PubMed]
- Bouhairie, V.E.; Goldberg, A.C. Familial hypercholesterolemia. Cardiol. Clin. 2015, 33, 169–179. [Google Scholar] [CrossRef] [PubMed]
- Sjouke, B.; Kusters, D.M.; Kindt, I.; Besseling, J.; Defesche, J.C.; Sijbrands, E.J.; Hovingh, G.K. Homozygous autosomal dominant hypercholesterolaemia in the Netherlands: Prevalence, genotype-phenotype relationship, and clinical outcome. Eur. Heart J. 2015, 36, 560–565. [Google Scholar] [CrossRef]
- Zubielienė, K.; Valterytė, G.; Jonaitienė, N.; Žaliaduonytė, D.; Zabiela, V. Familial Hypercholesterolemia and Its Current Diagnostics and Treatment Possibilities: A Literature Analysis. Medicina 2022, 58, 1665. [Google Scholar] [CrossRef]
- Warden, B.A.; Fazio, S.; Shapiro, M.D. Familial Hypercholesterolemia: Genes and Beyond; Endotext: South Dartmouth, MA, USA, 2021. [Google Scholar]
- Khera, A.V.; Won, H.H.; Peloso, G.M.; Lawson, K.S.; Bartz, T.M.; Deng, X.; Kathiresan, S. Diagnostic Yield and Clinical Utility of Sequencing Familial Hypercholesterolemia Genes in Patients with Severe Hypercholesterolemia. J. Am. Coll. Cardiol. 2016, 67, 2578–2589. [Google Scholar] [CrossRef] [PubMed]
- Cuchel, M.; Bruckert, E.; Ginsberg, H.N.; Raal, F.J.; Santos, R.D.; Hegele, R.A.; Wiklund, O. Homozygous familial hypercholesterolaemia: New insights and guidance for clinicians to improve detection and clinical management. A position paper from the Consensus Panel on Familial Hypercholesterolaemia of the European Atherosclerosis Society. Eur. Heart J. 2014, 35, 2146–2157. [Google Scholar] [CrossRef]
- Nohara, A.; Tada, H.; Ogura, M.; Okazaki, S.; Ono, K.; Shimano, H.; Harada-Shiba, M. Homozygous Familial Hypercholesterolemia. J. Atheroscler. Thromb. 2021, 28, 665–678. [Google Scholar] [CrossRef]
- Berberich, A.J.; Hegele, R.A. The complex molecular genetics of familial hypercholesterolaemia. Nat. Rev. Cardiol. 2019, 16, 9–20. [Google Scholar] [CrossRef]
- Raal, F.J.; Santos, R.D. Homozygous familial hypercholesterolemia: Current perspectives on diagnosis and treatment. Atherosclerosis 2012, 223, 262–268. [Google Scholar] [CrossRef]
- Page, M.M.; Bell, D.A.; Hooper, A.J.; Watts, G.F.; Burnett, J.R. Lipoprotein apheresis and new therapies for severe familial hypercholesterolemia in adults and children. Best Pract. Res. Clin. Endocrinol. Metab. 2014, 28, 387–403. [Google Scholar] [CrossRef] [PubMed]
- Thompson, G.R.; Seed, M.; Naoumova, R.P.; Neuwirth, C.; Walji, S.; Aitman, T.J.; Soutar, A.K. Improved cardiovascular outcomes following temporal advances in lipid-lowering therapy in a genetically-characterised cohort of familial hypercholesterolaemia homozygotes. Atherosclerosis 2015, 243, 328–333. [Google Scholar] [CrossRef] [PubMed]
- Harada-Shiba, M.; Ohta, T.; Ohtake, A.; Ogura, M.; Dobashi, K.; Nohara, A. Guidance for Pediatric Familial Hypercholesterolemia 2017. J. Atheroscler. Thromb. 2018, 25, 539–553. [Google Scholar] [CrossRef] [PubMed]
- Harada-Shiba, M.; Takagi, A.; Miyamoto, Y.; Tsushima, M.; Ikeda, Y.; Yokoyama, S.; Yamamoto, A. Clinical Features and Genetic Analysis of Autosomal Recessive Hypercholesterolemia. J. Clin. Endocrinol. Metab. 2003, 88, 2541–2547. [Google Scholar] [CrossRef]
- Tromp, T.R.; Hartgers, M.L.; Hovingh, G.K.; Vallejo-Vaz, A.J.; Ray, K.K.; Soran, H.; Temizhan, A. Worldwide experience of homozygous familial hypercholesterolaemia: Retrospective cohort study. Lancet 2022, 399, 719–728. [Google Scholar] [CrossRef]
- Klevmoen, M.; Mulder, J.W.C.M.; Roeters van Lennep, J.E.; Holven, K.B. Sex Differences in Familial Hypercholesterolemia. Curr. Atheroscler. Rep. 2023, 25, 861–868. [Google Scholar] [CrossRef]
- Hobbs, H.H.; Brown, M.S.; Goldstein, J.L. Molecular genetics of the LDL receptor gene in familial hypercholesterolemia. Hum. Mutat. 1992, 1, 445–466. [Google Scholar] [CrossRef]
- Do, R.; Stitziel, N.O.; Won, H.H.; Jørgensen, A.B.; Duga, S.; Angelica Merlini, P.; Kathiresan, S. Exome sequencing identifies rare LDLR and APOA5 alleles conferring risk for myocardial infarction. Nature 2015, 518, 102–106. [Google Scholar] [CrossRef]
- Han, S.M.; Hwang, B.; Park, T.G.; Kim, D.I.; Rhee, M.Y.; Lee, B.K.; Lee, S.H. Genetic testing of Korean familial hypercholesterolemia using whole-exome sequencing. PLoS ONE 2015, 10, e0126706. [Google Scholar] [CrossRef]
- Hernández Flores, T.J.; González García, J.R.; Colima Fausto, A.G.; Cárdenas, N.A.V.; López, Y.S.; Morales, C.A.Z.; Torres, M.T.M. Screening of LDLR and APOB gene mutations in Mexican patients with homozygous familial hypercholesterolemia. J. Clin. Lipidol. 2018, 12, 693–701. [Google Scholar] [CrossRef]
- Di Taranto, M.D.; de Falco, R.; Guardamagna, O.; Massini, G.; Giacobbe, C.; Auricchio, R.; Fortunato, G. Lipid profile and genetic status in a familial hypercholesterolemia pediatric population: Exploring the LDL/HDL ratio. Clin. Chem. Lab. Med. 2019, 57, 1102–1110. [Google Scholar] [CrossRef] [PubMed]
- Hori, M.; Ohta, N.; Takahashi, A.; Masuda, H.; Isoda, R.; Yamamoto, S.; Son, C.; Ogura, M.; Hosoda, K.; Miyamoto, Y.; et al. Impact of LDLR and PCSK9 pathogenic variants in Japanese heterozygous familial hypercholesterolemia patients. Atherosclerosis 2019, 289, 101–108. [Google Scholar] [CrossRef]
- Bertolini, S.; Calandra, S.; Arca, M.; Averna, M.; Catapano, A.L.; Tarugi, P.; Zenti, M.G. Homozygous familial hypercholesterolemia in Italy: Clinical and molecular features. Atherosclerosis 2020, 312, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Xu, M.J.; Chu, J.P.; Fei, W.L.; Wang, J.; Zhang, Y.M.; Wang, Y. Difficult Journey to Find the Best Treatment for Homozygous Familial Hypercholesterolemia: Case Report. Int. Med. Case Rep. J. 2022, 15, 97–103. [Google Scholar] [CrossRef] [PubMed]
- De Castro-Orós, I.; Pocoví, M.; Civeira, F. The genetic basis of familial hypercholesterolemia: Inheritance, linkage, and mutations. Appl. Clin. Genet. 2010, 3, 53–64. [Google Scholar] [CrossRef] [PubMed]
- Mabuchi, H. Half a Century Tales of Familial Hypercholesterolemia (FH) in Japan. J. Atheroscler. Thromb. 2017, 24, 189–207. [Google Scholar] [CrossRef]
- Guardamagna, O.; Restagno, G.; Rolfo, E.; Pederiva, C.; Martini, S.; Abello, F.; Bertolini, S. The type of LDLR gene mutation predicts cardiovascular risk in children with familial hypercholesterolemia. J. Pediatr. 2009, 155, 199–204. [Google Scholar] [CrossRef]
- Durst, R.; Ibe, U.K.; Shpitzen, S.; Schurr, D.; Eliav, O.; Futema, M.; Leitersdorf, E. Molecular genetics of familial hypercholesterolemia in Israel-revisited. Atherosclerosis 2017, 257, 55–63. [Google Scholar] [CrossRef]
- Gidding, S.S.; Champagne, M.A.; de Ferranti, S.D.; Defesche, J.; Ito, M.K.; Knowles, J.W.; Wierzbicki, A.S. American Heart Association Atherosclerosis, Hypertension, and Obesity in Young Committee of Council on Cardiovascular Disease in Young, Council on Cardiovascular and Stroke Nursing, Council on Functional Genomics and Translational Biology, Council on Lifestyle and Cardiometabolic Health. The agenda for familial hypercholesterolemia: A scientific statement from the American Heart Association. Circulation 2015, 132, 2167–2192. [Google Scholar] [PubMed]
- Thedrez, A.; Blom, D.J.; Ramin-Mangata, S.; Blanchard, V.; Croyal, M.; Chemello, K.; Lambert, G. Homozygous Familial Hypercholesterolemia Patients with Identical Mutations Variably Express the LDLR (Low-Density Lipoprotein Receptor): Implications for the Efficacy of Evolocumab. Arterioscler. Thromb. Vasc. Biol. 2018, 38, 592–598. [Google Scholar] [CrossRef]
- Luirink, I.K.; Determeijer, J.; Hutten, B.A.; Wiegman, A.; Bruckert, E.; Schmitt, C.P.; Groothoff, J.W. Efficacy and safety of lipoprotein apheresis in children with homozygous familial hypercholesterolemia: A systematic review. J. Clin. Lipidol. 2019, 13, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Katzmann, J.; Schürfeld, C.; März, W.; Laufs, U. Case report-Rapid regression of xanthomas under lipoprotein apheresis in a boy with homozygous familial hypercholesterolemia. J. Clin. Lipidol. 2018, 12, 868–871. [Google Scholar] [CrossRef] [PubMed]
- Wiegman, A.; Greber-Platzer, S.; Ali, S.; Reijman, M.D.; Brinton, E.A.; Charng, M.J.; Pordy, R. Evinacumab for Pediatric Patients with Homozygous Familial Hypercholesterolemia. Circulation 2024, 149, 343–353. [Google Scholar] [CrossRef] [PubMed]
- Richards, S.; Aziz, N.; Bale, S.; Bick, D.; Das, S.; Gastier-Foster, J.; Rehm, H.L. Standards and guidelines for the interpretation of sequence variants: A joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. 2015, 17, 405–424. [Google Scholar] [CrossRef] [PubMed]
- Priori, S.G.; Wilde, A.A.; Horie, M.; Cho, Y.; Behr, E.R.; Berul, C.; Tracy, C. HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes: Document endorsed by HRS, EHRA, and APHRS in May 2013 and by ACCF, AHA, PACES, and AEPC in June 2013. Heart Rhythm. 2013, 10, 1932–1963. [Google Scholar] [CrossRef]


| Subject | Proband | Father | Mother |
|---|---|---|---|
| Cholesterol, mmol/L | 17.96 ↑ | 6.82 ↑ | 6.39 ↑ |
| ApoA I, mmol/L | 25.9 ↓ | 55.5 | 43.9 |
| Triglyceride, mmol/L | 0.038 | 0.98 | 0.77 |
| LDL-C, mmol/L | 16.88 ↑ | 5.32 ↑ | 4.93 ↑ |
| HDL-C, mmol/L | 2.71 | 1.47 | 1.31 ↓ |
| ApoB, umol/L | 8.90 ↑ | 2.85 | 2.32 |
| Lp(a), nmol/L | 133.6 ↑ | 10.5 | 35.5 |
| Gene | Nucleotide Change | Protein Change | Study | Number of Affected Patients | Reference |
|---|---|---|---|---|---|
| LDLR | c.418G>T | p.Glu140 * | Cohort study (n = 4703) | 2 | Do R et al. [19], 2015 |
| LDLR | c.418G>A | p.E140K | Cohort study (n = 136) | 1 | Han et al. [20], 2015 |
| LDLR | c.418G>A | p.Glu140Lys | Family study (n = 11) | 1 | Hernández et al. [21], 2018 |
| LDLR | c.418G>T | p.Glu140 * | Cohort study (n = 127) | 2 | Di Taranto et al. [22], 2019 |
| LDLR | c.418G>A | p.Glu140Lys | Cohort study (n = 650) | 6 | Hori et al. [23], 2019 |
| LDLR | c.418G>T | p.(E140 *) | Cohort study (n = 125) | 1 | Bertolini et al. [24], 2020 |
| LDLR | c.418G>A | p.Glu140Lys | Case report | 1 | Xu et al. [25], 2022 |
| Primer | Sequence (5′–3′) | Ta (°C) | Amplicon Length (bp) |
|---|---|---|---|
| LDLR_F | AGACTTCACACGGTGATGGT | 58 °C | 529 |
| LDLR_R | TTGGAAATCCACTTCGGCAC | 58 °C | 529 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chamoieva, A.E.; Mirmanova, Z.Z.; Zhalbinova, M.R.; Rakhimova, S.E.; Daniyarov, A.Z.; Kairov, U.Y.; Baigalkanova, A.I.; Mukarov, M.A.; Bekbossynova, M.S.; Akilzhanova, A.R. Targeted NGS Revealed Pathogenic Mutation in a 13-Year-Old Patient with Homozygous Familial Hypercholesterolemia: A Case Report. Int. J. Mol. Sci. 2024, 25, 11882. https://doi.org/10.3390/ijms252211882
Chamoieva AE, Mirmanova ZZ, Zhalbinova MR, Rakhimova SE, Daniyarov AZ, Kairov UY, Baigalkanova AI, Mukarov MA, Bekbossynova MS, Akilzhanova AR. Targeted NGS Revealed Pathogenic Mutation in a 13-Year-Old Patient with Homozygous Familial Hypercholesterolemia: A Case Report. International Journal of Molecular Sciences. 2024; 25(22):11882. https://doi.org/10.3390/ijms252211882
Chicago/Turabian StyleChamoieva, Ayaulym E., Zhanel Z. Mirmanova, Madina R. Zhalbinova, Saule E. Rakhimova, Asset Z. Daniyarov, Ulykbek Y. Kairov, Almira I. Baigalkanova, Murat A. Mukarov, Makhabbat S. Bekbossynova, and Ainur R. Akilzhanova. 2024. "Targeted NGS Revealed Pathogenic Mutation in a 13-Year-Old Patient with Homozygous Familial Hypercholesterolemia: A Case Report" International Journal of Molecular Sciences 25, no. 22: 11882. https://doi.org/10.3390/ijms252211882
APA StyleChamoieva, A. E., Mirmanova, Z. Z., Zhalbinova, M. R., Rakhimova, S. E., Daniyarov, A. Z., Kairov, U. Y., Baigalkanova, A. I., Mukarov, M. A., Bekbossynova, M. S., & Akilzhanova, A. R. (2024). Targeted NGS Revealed Pathogenic Mutation in a 13-Year-Old Patient with Homozygous Familial Hypercholesterolemia: A Case Report. International Journal of Molecular Sciences, 25(22), 11882. https://doi.org/10.3390/ijms252211882







