Botulinum Toxin: A Comprehensive Review of Its Molecular Architecture and Mechanistic Action
Abstract
1. Introduction
- Genomic Organization and Horizontal Gene Transfer: Botulinum toxin’s synthesis is tightly regulated by the genes within Clostridium botulinum. One intriguing question is the role of horizontal gene transfer in shaping the genomic organization of these bacteria. How do mobile genetic elements, such as plasmids and bacteriophages, influence the diversity of botulinum toxin serotypes, and what implications might this have for its pathogenicity?
- Structural Composition and Mechanism of Action: While the general mechanism of botulinum toxin action is well understood—namely, its ability to cleave proteins involved in neurotransmitter release—many details about its structure remain under active investigation. How do variations in the structural components of the toxin influence its potency and specificity for different target cells? Furthermore, what molecular adaptations allow it to bind with such high specificity to neuronal receptors?
- Interactions with Intestinal Epithelial Cells: In addition to its well-known action on neurons, there is increasing interest in botulinum toxin’s interactions with intestinal epithelial cells, especially in cases of foodborne botulism. How does the toxin cross the intestinal epithelium to reach its target tissues? Does botulinum toxin utilize specific transport mechanisms for absorption, and how do these processes differ in infant botulism, where gastrointestinal colonization is the primary route of infection?
- Potential Effects on the Central Nervous System (CNS): While botulinum toxin primarily affects peripheral neurons, recent research has suggested that it may also influence the central nervous system. Does botulinum toxin cross the blood–brain barrier, and if so, what are the potential implications for neurological disorders and the development of new therapeutic strategies? Can botulinum toxin have direct effects on central nervous system disorders, and what would be its therapeutic potential in this regard?
- Interactions with Associated Proteins and Pathogenesis: Botulinum toxin interacts with a variety of host proteins during its entry into cells and its subsequent action. Understanding the full scope of these interactions is crucial for understanding its pathogenesis. Are there any novel protein interactions that could reveal new targets for therapeutic intervention, and could these interactions extend beyond neurons to other cell types?
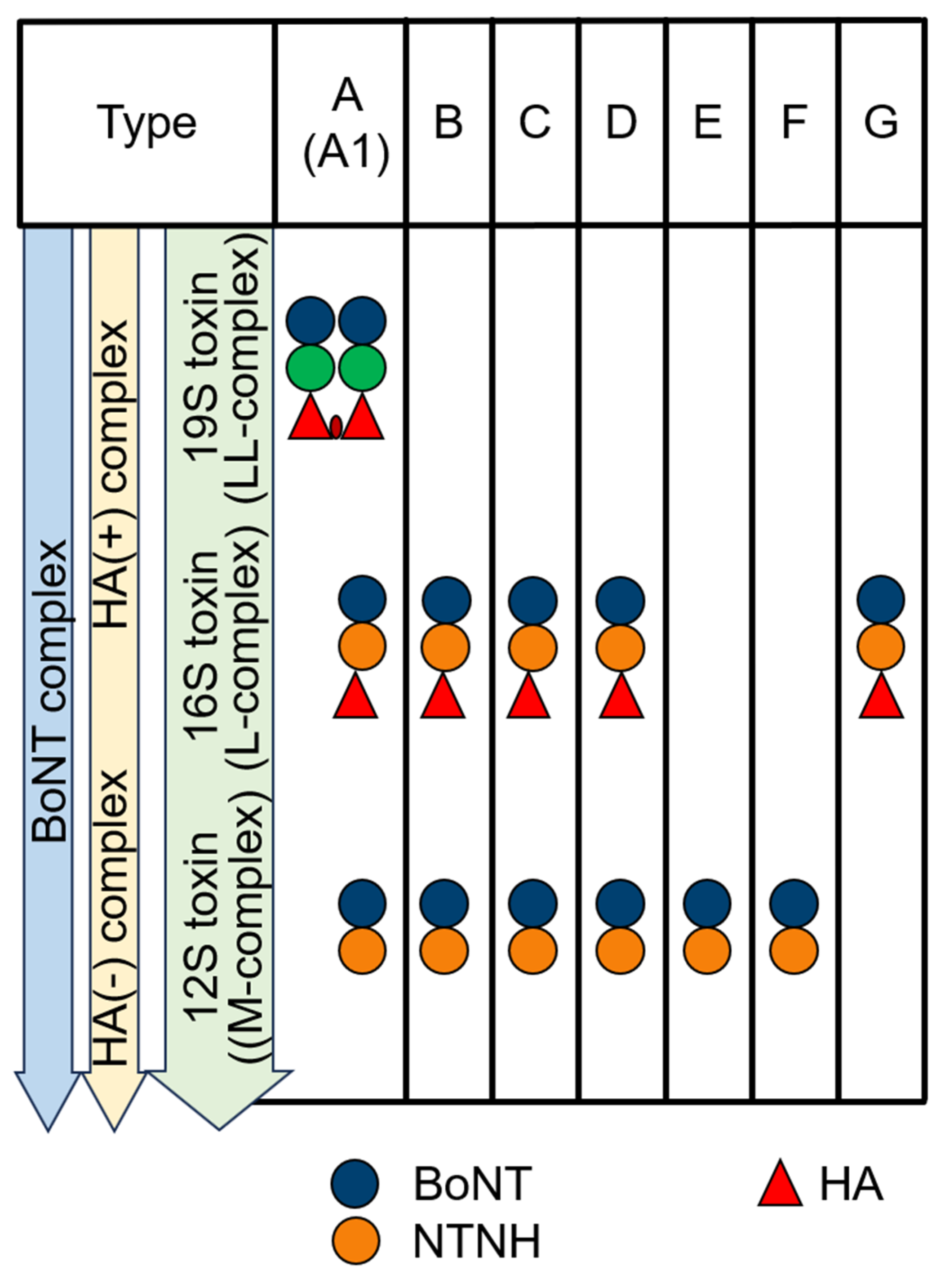
2. Organizational Intricacies
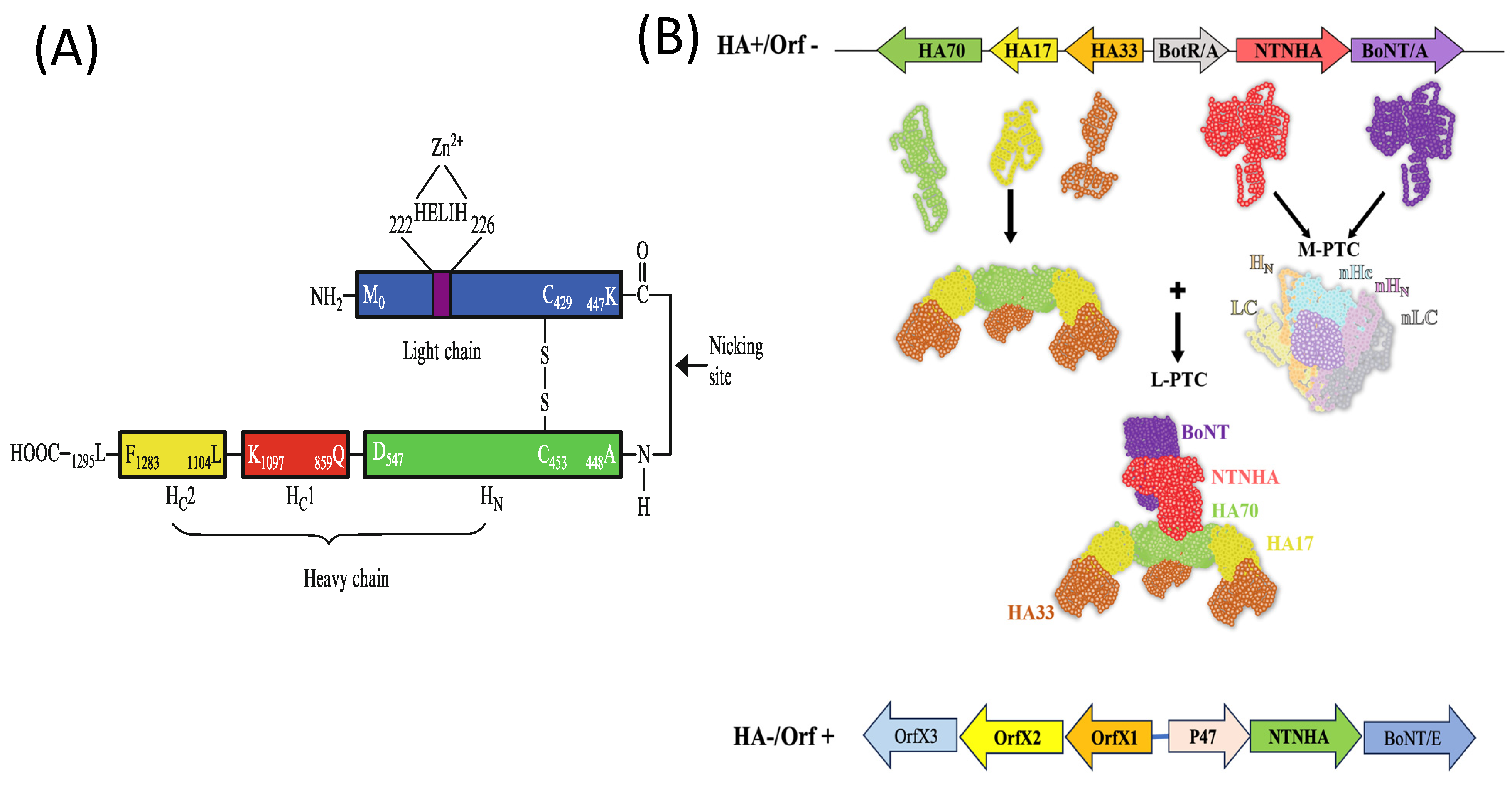
3. Structural Composition
- Binding specificity across serotypes: Given the high sequence identity and probable structural similarity between NTNHA proteins, could NTNHA from one BoNT serotype interact similarly with botulinum neurotoxin from another serotype, or is this interaction highly specific? This is a critical question because the interaction between NTNHA and BoNT may be influenced by subtle structural differences, which could affect the cross-serotype functionality.
- High sequence similarity of NTNHA: Why does NTNHA exhibit such a high sequence similarity to BoNT? This raises questions about the evolutionary pressures that led to such a conserved structure. Is this similarity a result of a shared function, or is it indicative of an ancestral origin?
- Biological function of NTNHA: Since NTNHA lacks catalytic activity, what is its biological function? Despite its structural resemblance to BoNT, NTNHA does not participate in the enzymatic cleavage of substrates. Its role likely lies in supporting the stability, transport, or protease resistance of the neurotoxin complex, but further studies are needed to fully elucidate its function.
- Evolutionary divergence in catalytic activity: Why did one component of the BoNT complex (BoNT) acquire metalloprotease activity, while a similar structural component (NTNHA) lacks this activity? This raises intriguing questions about the evolutionary forces that led to functional divergence despite similar structural motifs.
- BoNT-NTNHA complex as a toxin–antitoxin system: Although the BoNT-NTNHA complex resembles a toxin–antitoxin system, its biological behavior does not align with traditional toxin–antitoxin systems. Why is this the case? While toxin–antitoxin systems typically involve an equilibrium between a toxic protein and its inhibitor, the interaction between BoNT and NTNHA appears to serve different functional roles, particularly in protecting the toxin from protease degradation and aiding in its transport.
- Absence of a Zn-binding motif in NTNHA: Why does NTNHA, despite its structural similarity to BoNT, lack the Zn2+-binding motif? The absence of the HEXXH motif in NTNHA raises questions about its functional divergence from BoNT. This structural variation may be a key aspect of NTNHA’s non-catalytic role and its interaction with BoNT. The purpose of this motif’s absence in NTNHA may relate to its role as a stabilizing or protective partner rather than an active enzymatic component.
- NTNHA as a non-neuronal binding protein: Why is NTNHA not a neuronal binding protein? Despite its structural similarity to the heavy chain of BoNT, which is involved in binding to neuronal cells, NTNHA does not exhibit similar binding characteristics. This suggests that NTNHA’s role in the BoNT complex may be distinct from the toxin’s interaction with neuronal membranes, potentially focusing on stability or other functions that do not involve direct neuronal binding.
4. Evolutionary Insights: BoNT/NTNHA Gene Cluster
- RXXY (active-site stabilizing motif);
- PWISQSLN (translocation motif);
- Two cysteine residues, C376 and C386, located between the translocation and catalytic domains (similar to the disulfide bond found in BoNT).
5. HA Proteins and Their Role in BoNT Complexes
6. Interaction with E-Cadherin
7. OrfX Proteins and Their Role in BoNT Complex Formation
8. Regulatory Role of OrfX
9. Interaction of Botulinum Toxin with the Epithelial Barrier
- 1.
- First Hurdle: The Harsh Environment of the Digestive Tract
- 2.
- Second Hurdle: The Epithelial Barrier
- 3.
- Disruption of the Epithelial Barrier by HAs
- 4.
- Efficient Transport Across Epithelial Cells
- 5.
- Retrograde Transport and Interaction with the Enteric Nervous System
10. Interaction of Botulinum Toxin with Neuronal Cells
| Serotype | Species | Cleavage Site of Substrate | ||
|---|---|---|---|---|
| Mouse | Rat | Human | ||
| BoNT/A | SNAP23 | T202–R203 | T202–R203 | A203–R204 |
| SNAP25a/b | Q197–R198 | Q197–R198 | Q197–R198 | |
| SNAP29 | K255–K256 | K253–K254 | R253–K254 | |
| SNAP47 | R407–R408 | R413–R414 | R459–R460 | |
| BoNT/B | VAMP1 | Q78–F79 | V78–F80 | Q78–F79 |
| VAMP2 | Q76–F77 | Q76–F77 | Q76–F77 | |
| VAMP3 | Q63–F64 | Q63–F64 | Q63–F64 | |
| VAMP4 | A98–F99 | A98–F99 | A98–F99 | |
| VAMP5 | A51–F52 | A51–F52 | T51–F52 | |
| YKT6 | A183–F184 | A183–F184 | A183–F184 | |
| VAMP7 | T171–F172 | T171–F172 | T171–F172 | |
| VAMP8 | H58–F59 | H59–F60 | H58–F59 | |
| SEC22 | K180–Y181 | K180–Y181 | K180–Y181 | |
| BoNT/C and BoNT/CD | SNAP23 | R203–A204 | R203–A204 | R203–A204 |
| SNAP25 a/b | R198–A199 | R198–A199 | R198–A199 | |
| SNAP29 | K256–V257 | K254–V255 | K254–V255 | |
| SNAP47 | R408–M409 | A414–M415 | A459–M460 | |
| STX1A | K253–A254 | K253–A254 | K253–A254 | |
| STX1B | K252–A253 | K252–A253 | K252–A253 | |
| STX2 | K253–A254 | K254–A255 | K252–A253 | |
| STX3 | R253–A254 | R253–A254 | K253–A254 | |
| STX4 | I261–A262 | I261–A262 | I261–A262 | |
| STX5 | K324–Y325 | K324–Y325 | K324–Y325 | |
| STX6 | K224–V225 | K224–V225 | K224–V225 | |
| STX7 | R226–M227 | R226–M227 | R226–M227 | |
| STX8 | L206–V207 | L206–V207 | L206–V207 | |
| STX11 | K265–A266 | K265–A266 | K265–A266 | |
| STX12 | R239–A240 | R239–A240 | R239–A240 | |
| STX16 | K292–A293 | K292–A293 | K292–A293 | |
| STX17 | K222–A223 | K222–A223 | K222–A223 | |
| STX18 | E203–A204 | E203–A204 | E203–A204 | |
| STX19 | L268–A269 | ND | R270–L271 | |
| BoNT/E | SNAP23 | K185–I186 | K185–I186 | R185–I186 |
| SNAP25 a/b | R180–I81 | R180–I81 | R180–I81 | |
| SNAP29 | R238–L239 | R236–L237 | R236–L237 | |
| SNAP47 | G390–I391 | G396–I397 | G441–V442 | |
| BoNT/F5 and BoNT/FA | VAMP1 | L56–E57 | L56–E57 | L56–E57 |
| VAMP2 | L54–E55 | L54–E55 | L54–E55 | |
| VAMP3 | L41–E42 | L41–E42 | L41–E42 | |
| VAMP4 | I76–E77 | I76–E77 | I76–E77 | |
| VAMP5 | L29–E30 | L29–E30 | L29–E30 | |
| YKT6 | L1622–E163 | L162–E163 | L162–E163 | |
| VAMP7 | A149–Q150 | A149–Q150 | A149–Q150 | |
| VAMP8 | L36–S37 | L36–S37 | L36–S37 | |
| SEC22 | L58–Q59 | L58–Q59 | L58–Q59 | |
| BoNT/F1 | VAMP1 | Q60–K61 | Q60–K61 | Q60–K61 |
| VAMP2 | Q58–K59 | Q58–K59 | Q58–K59 | |
| VAMP3 | Q45–K46 | Q45–K46 | Q45–K46 | |
| VAMP4 | E80–R81 | E80–R81 | E80–R81 | |
| VAMP5 | G60–K61 | G60–K61 | V60–K61 | |
| YKT6 | E166–K167 | E166–K167 | E166–K167 | |
| VAMP7 | E153–R154 | E153–R154 | E153–R154 | |
| VAMP8 | E40–N41 | E39–N40 | E40–N41 | |
| Sec22 | E162–A163 | E162–A163 | E162–A163 | |
| BoNT/G | VAMP1 | A83–A84 | A83–A84 | A83–A84 |
| VAMP2 | A81–A82 | A81–A82 | A81–A82 | |
| VAMP3 | A68–A69 | A68–A69 | A68–A69 | |
| VAMP4 | S103–K104 | S103–K104 | S103–K104 | |
| VAMP5 | T56–K57 | T56–K57 | T56–Q57 | |
| YKT6 | A189–R190 | A189–R190 | A189–R190 | |
| VAMP7 | S176–R177 | S176–R177 | S176–R177 | |
| VAMP8 | S63–Q64 | S63–Q64 | S63–Q64 | |
| Sec22 | A185–K186 | A185–K186 | A185–K186 | |
| BoNT/D and BoNT/DC | VAMP1 | K61–L62 | K61–L62 | K61–L62 |
| VAMP2 | K59–L60 | K59–L60 | K59–L60 | |
| VAMP3 | K46–L47 | K46–L47 | K46–L47 | |
| VAMP4 | R81–L82 | R81–L82 | R81–L82 | |
| VAMP5 | K61–L62 | K61–L62 | K61–L62 | |
| YKT6 | K167–L168 | K167–L168 | K167–L168 | |
| VAMP7 | R154–L155 | R154–L155 | R154–L155 | |
| VAMP8 | N41–L42 | N41–L42 | N41–L42 | |
| Sec22 | A163–L164 | A163–L164 | A163–L164 | |
11. Trafficking in the CNS
- Peripheral BoNT injections produce indirect effects on the CNS.
- BoNT may utilize alternative internalization pathways, such as a retrograde pathway followed by transcytosis to reach secondary neurons.
- Receptors and targets for BoNT are present in CNS neurons, meaning that the direct administration of BoNT could have therapeutic effects.
- Non-neuronal cells may also be affected by BoNT, indirectly altering the neuronal circuitry.
- Peripheral SNARE cleavage could trigger pathways leading to the degradation, reduced expression, or inhibition of neurotransmitter release in distal neurons.
12. Conclusions
- Inhibition of acetylcholine release before SNAP-25 cleavage: It has been shown that acetylcholine release is inhibited before the detection of SNAP-25 cleavage. This raises the question: How is acetylcholine release inhibited before SNAP-25 cleavage occurs?
- Central effects after peripheral administration: Evidence suggests that BoNT has central effects following peripheral administration, but the mechanisms underlying this action remain unclear. Understanding how BoNT affects the central nervous system (CNS) after being injected into peripheral sites is crucial.
- Longevity of BoNT inside the cell: The duration of BoNT inside the cell, particularly how long it remains active after internalization and translocation to the cytosol, is still under investigation. What mechanisms allow BoNT to exert prolonged effects once inside the cell?
- Other effects beyond acetylcholine inhibition: While BoNT is primarily known for inhibiting acetylcholine release, there may be other effects of BoNT administration that have not been fully explored. Does BoNT affect other signaling pathways or cellular functions beyond its well-known impact on neurotransmitter release?
- Transport of BoNT through the gut: Since botulism is primarily a food-borne disease, the transport of BoNT through the gut needs to be studied in more detail. Additionally, the potential effects of BoNT on the gut–brain axis could provide new insights into its systemic impacts and open up new avenues of research.
Funding
Conflicts of Interest
References
- Smith, T.J.; Hill, K.K.; Raphael, B.H. Historical and current perspectives on Clostridium botulinum diversity. Res. Microbiol. 2015, 166, 290–302. [Google Scholar] [CrossRef] [PubMed]
- Hill, K.K.; Smith, T.J. Genetic diversity within Clostridium botulinum serotypes, botulinum neurotoxin gene clusters and toxin subtypes. Curr. Top. Microbiol. Immunol. 2013, 364, 1–20. [Google Scholar] [PubMed]
- Kumar, R.; Chang, T.W.; Singh, B.R. Evolutionary traits of toxins. In Biological Toxins and Bioterrorism; Goparlakrishnakone, P., Ed.; Springer: Berlin/Heidelberg, Germany, 2015. [Google Scholar] [CrossRef]
- Sebaihia, M.; Peck, M.W.; Minton, N.P.; Thomson, N.R.; Holden, M.T.; Mitchell, W.J.; Carter, A.T.; Bentley, S.D.; Mason, D.R.; Crossman, L.; et al. Genome sequence of a proteolytic (Group I) Clostridium botulinum strain Hall A and comparative analysis of the clostridial genomes. Genome Res. 2007, 17, 1082–1092. [Google Scholar] [CrossRef]
- Fairweather, N.F.; Lyness, V.A.; Pickyard, D.J.; Allen, G.; Thomson, R.O. Cloning, nucleotide sequencing and expression of tetanus toxin fragment C in Eschericia coli. J. Bacteriol. 1986, 165, 21–27. [Google Scholar] [CrossRef]
- Hill, K.K.; Xie, G.; Foley, B.T.; Smith, T.J.; Munk, A.C.; Bruce, D.; Smith, L.A.; Brettin, T.S.; Detter, J.C. Recombination and insertion events involving the botulinum neurotoxin complex genes in Clostridium botulinum types A, B, E and F and Clostridium butyricumtype E strains. BMC Biol. 2009, 7, 66. [Google Scholar] [CrossRef]
- Fu, F.N.; Sharma, S.K.; Singh, B.R. A Protease-Resistant Novel Hemagglutinin Purified from Type A Clostridium botulinum. J Protein Chem. 1998, 17, 53–60. [Google Scholar] [CrossRef]
- Bryant, A.M.; Davis, J.; Cai, S.; Singh, B.R. Molecular composition and extinction coefficient of native botulinum neurotoxin complex produced by Clostridium botulinum hall A strain. Protein J. 2013, 32, 106–117. [Google Scholar] [CrossRef]
- Inoue, K.; Fujinaga, Y.; Watanabe, T.; Ohyama, T.; Takeshi, K.; Moriishi, K.; Nakajima, H.; Oguma, K. Molecular composition of Clostridium botulinum type A progenitor toxins. Infect. Immun. 1996, 64, 1589–1594. [Google Scholar] [CrossRef]
- Suzuki, T.; Watanabe, T.; Mutoh, S.; Hasegawa, K.; Kouguchi, H.; Sagane, Y.; Fujinaga, Y.; Oguma, K.; Ohyama, T. Characterization of the interaction between subunits of the botulinum toxin complex produced by serotype D through tryptic susceptibility of the isolated components and complex forms. Microbiology 2005, 151, 1475–1483. [Google Scholar] [CrossRef][Green Version]
- Lietzow, M.A.; Gielow, E.T.; Le, D.; Zhang, J.; Verhagen, M.F. Subunit stoichiometry of the Clostridium botulinum type A neurotoxin complex determined using denaturing capillary electrophoresis. Protein J. 2008, 27, 420–425. [Google Scholar] [CrossRef]
- Gu, S.; Rumpel, S.; Zhou, J.; Strotmeier, J.; Bigalk, H.; Perry, K.; Shoemaker, C.B.; Rummel, A.; Jin, R. Botulinum neurotoxin is shielded by NTNHA in an interlocked complex. Science 2012, 335, 977–981. [Google Scholar] [CrossRef] [PubMed]
- Gu, S.; Jin, R. Assembly and function of the botulinum neurotoxin progenitor complex. Curr. Top. Microbiol. Immunol. 2013, 364, 21–44. [Google Scholar] [PubMed]
- Lee, K.; Gu, S.; Jin, L.; Le, T.T.N.; Cheng, L.W.; Strotmeier, J.; Kruel, A.M.; Yao, G.; Perry, K.; Rummel, A.; et al. Structure of a bimodular botulinum neurotoxin complex provides insights into its oral toxicity. PLOS Pathog. 2013, 9, e1003690. [Google Scholar] [CrossRef] [PubMed]
- Benefield, D.A.; Dessain, S.K.; Shine, N.; Ohi, M.D.; Lacy, D.B. Molecular assembly of botulinum neurotoxin progenitor complexes. Proc. Natl. Acad. Sci. USA 2013, 110, 5630–5635. [Google Scholar] [CrossRef]
- Nowakowska, M.B.; Douillard, F.P.; Lindström, M. Looking for the X Factor in Bacterial Pathogenesis: Association of orfX-p47 Gene Clusters with Toxin Genes in Clostridial and Non-Clostridial Bacterial Species. Toxins 2019, 12, 19. [Google Scholar] [CrossRef]
- Inoue, K.; Fujnaga, Y.; Honke, K.; Arimitsu, H.; Mahmut, N.; Sakaguchi, Y.; Ohyama, T.; Watanabe, T.; Inoue, K.; Oguma, K. Clostridium botulinum type A haemagglutinin positive progenitor toxin (HA+-PTX) binds to oligosaccharides containing Galb1-4GlcNAc through one subcomponent of haemagglutinin (HA1). Microbiology 2001, 147, 811–819. [Google Scholar] [CrossRef]
- Inoue, K.; Fujinaga, Y.; Honke, K.; Yokota, K.; Ikeda, T.; Ohyama, T.; Takeshi, K.; Watanabe, T.; Inoue, K.; Oguma, K. Characterization of haemagglutinin activity of Clostridium botulinum type C and D 16S toxins, and one subcomponent of haemagglutinin (HA1). Microbiology 1999, 145, 2533–2542. [Google Scholar] [CrossRef]
- Fujinaga, Y.; Inoue, K.; Watarai, S.; Sakaguchi, G.; Arimitsu, H.; Lee, J.C.; Jin, Y.; Matsumura, T.; Kabumoto, Y.; Watanabe, T.; et al. Molecular characterization of binding subcomponents of Clostridium botulinum type C progenitor toxin for intestinal epithelial cells and erythrocytes. Microbiolo 2004, 150, 1529–1538. [Google Scholar] [CrossRef]
- Amatsu, S.; Sugawara, Y.; Matsumara, T.; Kitadokoro, K.; Fujinaga, Y. Crystal structure of Clostridium botulinum whole hemagglutinin reveals a huge riskelion-shaped molecular complex. Microbiology 2013, 288, 35617–35625. [Google Scholar]
- Sharma, S.K.; Fu, F.N.; Singh, B.R. Molecular properties of a hemagglutinin purified from type A Clostridium botulinum. J. Protein Chem. 1999, 18, 29–38. [Google Scholar] [CrossRef]
- Ghosal, K.J.; Patel, K.; Singh, B.R.; Hale, M.L. Role of critical elements in botulinum neurotoxin complex in toxin routing across intestinal and bronchial barriers. PLoS ONE 2018, 13, e0199524. [Google Scholar] [CrossRef] [PubMed]
- Gustafsson, R.; Berntsson, R.P.; Martínez-Carranza, M.; El Tekle, G.; Odegrip, R.; Johnson, E.A.; Stenmark, P. Crystal structures of OrfX2 and P47 from a Botulinum neurotoxin OrfX-type gene cluster. FEBS Lett. 2017, 591, 3781–3792. [Google Scholar] [CrossRef] [PubMed]
- Gao, L.; Lam, K.H.; Liu, S.; Przykopanski, A.; Lübke, J.; Qi, R.; Krüger, M.; Nowakowska, M.B.; Selby, K.; Douillard, F.P.; et al. Crystal structures of OrfX1, OrfX2 and the OrfX1-OrfX3 complex from the orfX gene cluster of botulinum neurotoxin E1. FEBS Lett. 2023, 597, 524–537. [Google Scholar] [CrossRef] [PubMed]
- Sugii, S.; Ohishi, I.; Sakaguchi, G. Intestinal absorption of botulinum toxins of different molecular sizes in rats. Infect. Immun. 1977, 17, 491–496. [Google Scholar] [CrossRef] [PubMed]
- Sugii, S.; Ohishi, I.; Sakaguchi, G. Correlation between oral toxicity and in vitro stability of Clostridium botulinum type A and B toxins of different molecular sizes. Infect. Immun. 1977, 16, 910–914. [Google Scholar] [CrossRef]
- Couesnon, A.; Pereira, Y.; Popoff, M.R. Receptor-mediated transcytosis of botulinum neurotoxin A through intestinal cell monolayers. Cell. Microbiol. 2007, 10, 375–387. [Google Scholar] [CrossRef]
- Nishikawa, A.; Uotsu, N.; Arimitsu, H.; Lee, J.-C.; Miura, Y.; Fujinaga, Y.; Nakada, H.; Watanabe, T.; Ohyama, T.; Sakano, Y.; et al. The receptor and transporter for internalization of Clostridium botulinum type C progenitor toxin into HT-29 cells. Biochem. Biophys. Res. Commun. 2004, 319, 327–333. [Google Scholar] [CrossRef]
- Couesnon, A.; Shimizu, T.; Popoff, M.R. Differential entry of botulinum neurotoxin A into neuronal and intestinal cells. Cell. Microbiol. 2009, 11, 289–308. [Google Scholar] [CrossRef]
- Maksymowych, A.B.; Simpson, L.L. Binding and transcytosis of botulium neurotoxin by polarized human colon carcinoma cells. J. Biol. Chem. 1998, 273, 21950–21957. [Google Scholar] [CrossRef]
- Phan, Q.T.; Myers, C.L.; Fu, Y.; Sheppard, D.C.; Yeaman, M.R.; Welch, W.H.; Ibrahim, A.S.; Edwards, J.E., Jr.; Filler, S.G. Als3 is a Candida albicans invasin that binds to cadherins and induces endocytosis by host cells. PLoS Biol. 2007, 5, e64. [Google Scholar] [CrossRef]
- Sugawar, Y.; Fujinaga, Y. The botulinum toxin complex meets E-cadherin on the way to its destination. Cell Adhes. Migr. 2010, 5, 34–36. [Google Scholar] [CrossRef] [PubMed]
- Kerneis, S.; Bogdanova, A.; Kraenhenbul, J.P.; Pringault, E. Conversion by Payer’s patche lymphocyte of human enterocytes into M cells that transport bacteria. Science 1997, 277, 949–952. [Google Scholar] [CrossRef] [PubMed]
- Ouzilou, L.; Caliot, E.; Pelletier, I.; Prévost, M.-C.; Pringault, E.; Colbère-Garapin, F. Poliovirus transcytosis through M-like cells. J. Gen. Virol. 2002, 83, 2177–2182. [Google Scholar] [CrossRef] [PubMed]
- Couesnon, A.; Colasante, C.; Molgo, J.; Popoff, M.R. Differential entry of Botulinum neurotoxin A into neuronal and intestinal cells: An ultrastructural approach. Botulinum J. 2011, 1, 375–392. [Google Scholar] [CrossRef]
- Connan, C.; Voillequin, M.; Chavez, C.V.; Mazuet, C.; Leveque, C.; Vitry, S.; Vandewalle, A.; Popoff, M.R. Botulinum neurotoxin type B uses a distinct entry pathway mediated by CDC42 into intestinal cells versus neuronal cells. Cell. Microbiol. 2017, 19, e12738. [Google Scholar] [CrossRef]
- Fujinaga, Y.; Popoff, M.R. Translocation and dissemination of botulinum neurotoxin from the intestinal tract. Toxicon 2018, 147, 13–18. [Google Scholar] [CrossRef]
- Antonucci, F.; Rossi, C.; Gianfranceschi, L.; Rossetto, O.; Caleo, M. Long-distance retrograde effects of botulinum neurotoxin A. J. Neurosci. 2008, 28, 3689–3696. [Google Scholar] [CrossRef]
- Restani, L.; Antonucci, F.; Gianfranceschi, L.; Rossi, C.; Rossetto, O.; Caleo, M. Evidence for anterograde transport and transcytosis of botulinum neurotoxin a (BoNT/A). J. Neurosci. 2011, 31, 15650–15659. [Google Scholar] [CrossRef]
- Restani, L.; Giribaldi, F.; Manich, M.; Bercsenyi, K.; Menendez, G.; Rossetto, O.; Caleo, M.; Schiavo, G. Botulinum neurotoxins A and E undergo retrograde axonal transport in primary motor neurons. PLoS Pathog. 2012, 8, e1003087. [Google Scholar] [CrossRef]
- Simpson, L. The life history of a botulinum toxin molecule. Toxicon 2013, 68, 40–59. [Google Scholar] [CrossRef]
- Schiavo, G.; Matteoli, M.; Montecucco, C. Neurotoxins affecting neuroexocytosis. Physiol. Rev. 2000, 80, 717–766. [Google Scholar] [CrossRef] [PubMed]
- Montal, M. Botulinum neurotoxin: A marvel of protein design. Annu. Rev. Biochem. 2010, 79, 591–617. [Google Scholar] [CrossRef] [PubMed]
- Bullens, R.W.; O’Hanlon, G.M.; Wagner, E.; Molenaar, P.C.; Furukawa, K.; Plomp, J.J.; Willison, H.J. Complex gangliosides at the neuromuscular junction are membrane receptors for autoantibodies and botulinum neurotoxin. J. Neurosci. 2002, 22, 6876–6884. [Google Scholar] [CrossRef] [PubMed]
- Yowler, B.C.; Kensinger, R.D.; Schengrund, C.L. Botulinum neurotoxin A activity is dependent upon the presence of specific gangliosides in neuroblastoma cells expressing synaptotagmin I. J. Biol. Chem. 2002, 277, 32815–32819. [Google Scholar] [CrossRef]
- Kitamura, M.; Igimi, S.; Furukawa, K. Different response of the knockout mice lacking β-series gangliosides against botulinum and tetanus toxins. Biochim. Biophys. Acta 2005, 1741, 1–3. [Google Scholar] [CrossRef]
- Rummel, A.; Eichner, T.; Weil, T.; Karnath, T.; Gutcaits, A.; Mahrhold, S.; Sandhoff, K.; Proia, R.L.; Acharya, K.R.; Bigalke, H.; et al. Identification of the protein receptor binding site of botulinum neurotoxins B and G proves the double-receptor concept. Proc. Natl. Acad. Sci. USA 2007, 104, 359–364. [Google Scholar] [CrossRef]
- Tsukamoto, K.; Kohda, T.; Mukamoto, M.; Takeuchi, K.; Ihara, H.; Saito, M.; Kozaki, S. Binding of Clostridium botulinum type C and D neurotoxins to ganglioside and phospholipid: Novel insights into the receptor for clostridial neurotoxins. J. Biol. Chem. 2005, 280, 35164–35171. [Google Scholar] [CrossRef]
- Schnaar, R.L.; Gerardy-Schahn, R.; Hildebrandt, H. Sialic acids in the brain: Gangliosides and polysialic acid in nervous system development, stability, disease, and regeneration. Physiol. Rev. 2014, 94, 461–518. [Google Scholar] [CrossRef]
- Lopez, P.H.H.; Baez, B.B. Gangliosides in axon stability and regeneration. Prog. Mol. Biol. Trans. Sci. 2018, 156, 383–412. [Google Scholar]
- Poulain, B.; Lemichez, E.; Popoff, M.R. Neuronal selectivity of botulinum neurotoxins. Toxicon 2020, 178, 20–32. [Google Scholar] [CrossRef]
- Nishiki, T.; Kamata, Y.; Nemoto, Y.; Omori, A.; Ito, T.; Takahashi, M.; Kozaki, S. Identification of protein receptor for Clostridium botulinum type B neurotoxin in rat brain synaptosomes. J. Biol. Chem. 1994, 269, 10498–10503. [Google Scholar] [CrossRef] [PubMed]
- Mahrhold, S.; Rummel, A.; Bigalke, H.; Davletov, B.; Binz, T. The synaptic vesicle protein 2C mediates the uptake of botulinum neurotoxin A into phrenic nerves. FEBS Lett. 2006, 580, 2011–2014. [Google Scholar] [CrossRef] [PubMed]
- Dong, M.; Liu, H.; Tepp, W.H.; Johnson, E.A.; Janz, R.; Chapman, E.R. Glycosylated SV2A and SV2B mediate the entry of botulinum neurotoxin E into neurons. Mol. Biol. Cell 2008, 19, 5226–5237. [Google Scholar] [CrossRef] [PubMed]
- Rummel, A.; Hafner, K.; Mahrhold, S.; Darashchonak, N.; Holt, M.; Jahn, R.; Beermann, S.; Karnath, T.; Bigalke, H.; Binz, T. Botulinum neurotoxins C, E and F bind ganglioside via a conserved binding site prior to stimulation-deendent uptake with botulinum neurotoxin F utilisig the three isoforms of SV2 as second receptor. J. Neurochem. 2009, 110, 1942–1954. [Google Scholar] [CrossRef]
- Peng, L.; Tepp, W.H.; Johnson, E.A.; Dong, M. Botulinum neurotoxin D uses synaptic vesicle protein SV2 and gangliosides as receptors. PLos Pathog. 2011, 7, e1002008. [Google Scholar] [CrossRef]
- Rummel, A.; Karnath, T.; Henke, T.; Bigalke, H.; Binz, T. Synaptotagmins I and II act as nerve cell receptors for botulinum neurotoxin G. J. Biol. Chem. 2004, 279, 30865–30870. [Google Scholar] [CrossRef]
- Karalewitz, A.P.-A.; Fu, Z.; Baldwin, M.R.; Kim, J.-J.P.; Barbieri, J.T. Botulinum neurotoxin serotype C associates with dual ganglioside receptors to facilitate cell entry. J. Biol. Chem. 2012, 287, 40806–40816. [Google Scholar] [CrossRef]
- Wang, J.; Meng, J.; Nugent, M.; Tang, M.; Dolly, J.O. Neuronal entry and high neurotoxicity of botulinum neurotoxin A require its N-terminal binding sub-domain. Sci. Rep. 2017, 7, srep44474. [Google Scholar] [CrossRef]
- Colasante, C.; Rossetto, O.; Morbiato, L.; Pirazzini, M.; Molgo, J.; Montecucco, C. Botulinum neurotoxin type A is internalized and translocated from small synaptic vesicles at the neuromuscular junction. Mol. Neurobiol. 2013, 48, 120–127. [Google Scholar] [CrossRef]
- Flores, A.; Ramirez-Franco, J.; Desplantes, R.; Debreux, K.; Ferracci, G.; Wernert, F.; Blanchard, M.-P.; Maulet, Y.; Youssouf, F.; Sangiardi, M.; et al. Gangliosides interact with synaptotagmin to form the high-affinity receptor complex for botulinum neurotoxin B. Proc. Natl. Acad. Sci. USA 2019, 116, 18098–18108. [Google Scholar] [CrossRef]
- Nishiki, T.-I.; Tokuyama, Y.; Kamata, Y.; Nemoto, Y.; Yoshida, A.; Sekiguchi, M.; Takahashi, M.; Kozaki, S. Binding of botulinum type B neurotoxin to Chinese hamster ovary cells transfected with rat synaptotagmin II cDNA. Neurosci. Lett. 1996, 208, 105–108. [Google Scholar] [CrossRef] [PubMed]
- Dong, M.; Richards, D.A.; Goodnough, M.C.; Tepp, W.H.; Johnson, E.A.; Chapman, E.R. Synaptotagmins I and II mediate entry of botulinum neurotoxin B into cells. J. Cell Biol. 2003, 162, 1293–1303. [Google Scholar] [CrossRef] [PubMed]
- Berntsson, R.P.; Peng, L.; Dong, M.; Stenmark, P. Structure of dual receptor binding to botulinum neurotoxin B. Nat. Commun. 2013, 4, 2058. [Google Scholar] [CrossRef] [PubMed]
- Kumar, R. Therapeutic use of botulinum toxin in pain treatment. Neuronal Signal. 2018, 2, NS20180058. [Google Scholar] [CrossRef]
- Morris, J.L.; Jobling, P.; Gibbins, I.L. Botulinum neurotoxin A attenuates release of norepinephrine but not NPY from vasoconstrictor neurons. Am. J. Physiol. Circ. Physiol. 2002, 283, H2627–H2635. [Google Scholar] [CrossRef]
- Swartling, C.; Naver, H.; Pihl-Lundin, I.; Hagforsen, E.; Vahlquist, A. Sweat gland morphology and periglandular innervation in essential palmar hyperhidrosis before and after treatment with intradermal botulinum toxin. J. Am. Acad. Dermatol. 2004, 51, 739–745. [Google Scholar] [CrossRef]
- Pirazzini, M.; Rossetto, O.; Eleopra, R.; Montecucco, C. Biological actions of botulinum neurotoxins. Pharmacol. Rev. 2017, 69, 200–235. [Google Scholar] [CrossRef]
- Raciborska, D.A.; Trimble, W.S.; Charlton, M.P. Presynaptic protein interactions in vivo: Evidence from botulinum A, C, D and E action at frog neuromuscular junction. Eur. J. Neurosci. 1998, 10, 2617–2628. [Google Scholar] [CrossRef]
- Thirunavukkarasu, N.; Ghosal, K.; Kukreja, R.; Zhou, Y.; Dombkowski, A.; Cai, S.; Singh, B.R. Microarray analysis of diffentially regulated genes in neuronal and epithelial cell lines upon exposure to type A botulinum neurotoxin. BBRC 2011, 405, 684–690. [Google Scholar]
- Grando, S.A.; Zachary, C.B. The non-neuronal and neuromuscular effects of botulinum toxin: An opportunity for a deadly molecule to treat disease in skin and beyond. Br. J. Dermatol. 2018, 178, 1011–1019. [Google Scholar] [CrossRef]
- Sobel, J. Botulism. Clin. Infect. Dis. 2005, 41, 1167–1173. [Google Scholar] [CrossRef] [PubMed]
- Rossetto, O. The binding of botulinum neurotoxins to different peripheral neurons. Toxicon 2018, 147, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Pirazzini, M.; Rossetto, O.; Eleopra, R.; Montecucco, C. Botulinum Neurotoxins: Biology, Pharmacology, and Toxicology. Pharmacol. Rev. 2017, 69, 200–235. [Google Scholar] [CrossRef] [PubMed]
- Esquenazi, A.; Mayer, N.; Garreta, R. Influence of botulinum toxin type A treatment of elbow flexor spasticity on hemiparetic gait. Am. J. Phys. Med. Rehabil. 2008, 87, 305–310. [Google Scholar] [CrossRef]
- Weise, D.; Weise, C.M.; Naumann, M. Central effects of botulinum neurotoxin—Evidence from Human studies. Toxins 2019, 11, 21. [Google Scholar] [CrossRef]
- Verderio, C.; Pozzi, D.; Pravettoni, E.; Inverardi, F.; Schenk, U.; Coco, S.; Proux-Gillardeaux, V.; Galli, T.; Rossetto, O.; Frassoni, C.; et al. SNAP-25 modulation of calcium dynamics underlies differences in GABAergic and glutamatergic responsiveness to depolarization. Neuron 2004, 41, 599–610. [Google Scholar] [CrossRef]
- Akaike, N.; Ito, Y.; Shin, M.C.; Nonaka, K.; Torii, Y.; Harakawa, T.; Ginnaga, A.; Kozaki, S.; Kaji, R. Effects of A2 type botulinum toxin on spontaneous miniature and evoked transmitter release from the rat spinal excitatory and inhibitory synapses. Toxicon 2010, 56, 1315–1326. [Google Scholar] [CrossRef]
- Restani, L.; Novelli, E.; Bottari, D.; Leone, P.; Barone, I.; Galli-Resta, L.; Strettoi, E.; Caleo, M. Botulinum neurotoxin a impairs neurotransmission following retrograde transynaptic transport. Traffic 2012, 13, 1083–1089. [Google Scholar] [CrossRef]
- Caleo, M.; Restani, L. Direct central nervous system effects of botulinum neurotoxin. Toxicon 2018, 147, 68–72. [Google Scholar] [CrossRef]
- Blood, A.J.; Tuch, D.S.; Makris, N.; Makhlouf, M.L.; Sudarsky, L.R.; Sharma, N. White matter abnormalities in dystonia normalize after botulinum toxin treatment. NeuroReport 2006, 17, 1251–1255. [Google Scholar] [CrossRef]
- Delnooz, C.C.S.; Pasman, J.W.; van de Warrenburg, B.P.C. Dynamic cortical gray matter volume changes after botulinum toxin in cervical dystonia. Neurobiol. Dis. 2015, 73, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Alexandru, H.; Muthuraman, M.; Chirumamilla, V.C.; Koirala, N.; Paktas, B.; Deuschl, G.; Zeuner, K.E.; Groppa, S. Grey Matter Microstructural Integrity Alterations in Blepharospasm Are Partially Reversed by Botulinum Neurotoxin Therapy. PLoS ONE 2016, 11, e0168652. [Google Scholar] [CrossRef] [PubMed]
- Giladi, N. The mechanism of action of Botulinum toxin type A in focal dystonia is most probably through its dual effect on efferent (motor) and afferent pathways at the injected site. J. Neurol. Sci. 1997, 152, 132–135. [Google Scholar] [CrossRef]
- Currà, A.; Trompetto, C.; Abbruzzese, G.; Berardelli, A. Central Effects of Botulinum Toxin Type A: Evidence and Supposition. Mov. Disord. 2004, 19, S60–S64. [Google Scholar] [CrossRef]
- Bach-Rojecky, L.; Lacković, Z. Central origin of the antinociceptive action of botulinum toxin type A. Pharmacol. Biochem. Behav. 2009, 94, 234–238. [Google Scholar] [CrossRef]
- Filipović, B.; Matak, I.; Bach-Rojecky, L.; Lacković, Z. Central action of peripherally applied botulinum toxin type A on pain and dural protein extravasation in rat model of trigeminal neuropathy. PLoS ONE 2012, 7, e29803. [Google Scholar] [CrossRef]
- Matak, I.; Rossetto, O.; Lacković, Z. Botulinum toxin type A selectivity for certain types of pain is associated with capsaicin-sensitive neurons. Pain 2014, 155, 1516–1526. [Google Scholar] [CrossRef]
- Nevrlý, M.; Hluštík, P.; Hok, P.; Otruba, P.; Tüdös, Z.; Kaňovský, P. Changes in sensorimotor network activation after botulinum toxin type A injections in patients with cervical dystonia: A functional MRI study. Exp. Brain Res. 2018, 236, 2627–2637. [Google Scholar] [CrossRef]
- Dresel, C.; Bayer, F.; Castrop, F.; Rimpau, C.; Zimmer, C.; Haslinger, B. Botulinum toxin modulates basl ganglia but not deficient somatosensory activation in orofacial dystonia. Mov. Disord. 2011, 26, 1496–1502. [Google Scholar] [CrossRef]
- Delnooz, C.C.S.; Pasman, J.W.; Beckmann, C.F.; van de Warrenburg, B.P.C. Task-Free Functional MRI in Cervical Dystonia Reveals Multi-Network Changes That Partially Normalize with Botulinum Toxin. PLoS ONE 2013, 8, e62877. [Google Scholar] [CrossRef]
- Delnooz, C.C.S.; Pasman, J.W.; Beckmann, C.F.; van de Warrenburg, B.P.C. Altered striatal and pallidal connectivity in cervical dystonia. Brain Struct. Funct. 2015, 220, 513–523. [Google Scholar] [CrossRef] [PubMed]
- Brodoehl, S.; Wagner, F.; Prell, T.; Klingner, C.; Witte, O.W.; Gunther, A. Cause or effect: Altered brain network activity in cervical dystonia is partially normalized by botulinum toxin treatment. Neuroimage Clin. 2019, 22, 101792. [Google Scholar] [CrossRef] [PubMed]
- Yesudhas, A.; Roshan, S.A.; Radhakrishnan, R.K.; Abirami, G.P.P.; Manickam, N.; Selvaraj, K.; Elumalai, G.; Shanmugaapriya, S.; Anusuyadevi, M.; Kandasamy, M. Intramuscular injection of BOTOX boosts learning and memory in adult mice in association with enriched circulation of platelets and enhanced density of pyramidal neurons in the Hippocampus. Neurochem. Res. 2020, 45, 2856–2867. [Google Scholar] [CrossRef]
- Papagiannopoulou, D.; Vardouli, L.; Dimitriadis, F.; Apostolidis, A. Retrograde transport of radiolabelled botulinum neurotoxin type A to the CNS after intradetrusor inejection in rats. BJU Int. 2016, 117, 697–704. [Google Scholar] [CrossRef]
- Luvisetto, S. Botulinum Neurotoxins in Central Nervous System: An Overview from Animal Models to Human Therapy. Toxins 2021, 13, 751. [Google Scholar] [CrossRef]
- Koizumi, H.; Goto, S.; Okita, S.; Morigaki, R.; Akaike, N.; Torii, Y.; Harakawa, T.; Ginnaga, A.; Kaji, R. Spinal Central Effects of Peripherally Applied BotulinumNeurotoxin A in Comparison between Its Subtypes A1 and A2. Front. Neurol 2014, 5, 98. [Google Scholar]
- Lee, W.-H.; Shin, T.J.; Kim, H.J.; Lee, J.-K.; Suh, H.-W.; Lee, S.C.; Seo, K. Intrathecal administration of botulinum neurotoxin type A attenuates formalin-induced nociceptive responses in mice. Anesth. Analg. 2011, 112, 228–235. [Google Scholar] [CrossRef]
- Coelho, A.; Oliveira, R.; Rossetto, O.; Cruz, C.; Cruz, F.; Avelino, A. Intrathecal administration of botulinum toxin type A improves urinary bladder function and reduces pain in rats with cystitis. Eur. J. Pain 2014, 18, 1480–1489. [Google Scholar] [CrossRef]
- Vlah, V.D.; Bach-Rojecky, L.; Lacković, Z. Antinociceptive action of botulinum toxin type A in carrageenan-induced mirror pain. J. Neural Transm. 2016, 123, 1403–1413. [Google Scholar] [CrossRef]
- Huang, P.P.; Khan, I.; Suhail, M.S.A.; Malkmus, S.; Yaksh, T.L. Spinal botulinum neurotoxin B: Effects on afferent transmitter release and nociceptive processing. PLoS ONE 2011, 6, e19126. [Google Scholar] [CrossRef]
- Antipova, V.; Wree, A.; Holzmann, C.; Mann, T.; Palomero-Gallagher, N.; Zilles, K.; Schmitt, O.; Hawlitschka, A. UnilateralBotulinum Neurotoxin-A Injection into the Striatum of C57BL/6 Mice Leads to a Different Motor Behavior Compared with Rats. Toxins 2018, 10, 295. [Google Scholar] [CrossRef] [PubMed]
- Antipova, V.; Holzmann, C.; Hawlitschka, A.; Wree, A. Botulinum Neurotoxin-A Injected Intrastriatally into Hemiparkinsonian Rats Improves the Initiation Time for Left and Right Forelimbs in Both Forehand and Backhand Directions. Int. J. Mol. Sci. 2019, 20, 992. [Google Scholar] [CrossRef] [PubMed]
- Hawlitschka, A.; Holzmann, C.; Wree, A.; Antipova, V.; Hawlitschka, A.; Holzmann, C.; Wree, A.; Antipova, V. Repeated Intrastriatal Botulinum Neurotoxin-A Injection in Hemiparkinsonian Rats Increased the Beneficial Effect on Rotational Behavior. Toxins 2018, 10, 368–389. [Google Scholar] [CrossRef] [PubMed]
- Ando, S.; Kobayashi, S.; Waki, H.; Kon, K.; Fukui, F.; Tadenuma, T.; Iwamoto, M.; Takeda, Y.; Izumiyama, N.; Watanabe, K.; et al. Animal model of dementia induced by entorhinal synaptic damage and partial restoration of cognitive deficits by BDNF and carnitine. J. Neurosci. Res. 2002, 70, 519–527. [Google Scholar] [CrossRef]
| Group/ Bacteria | Toxin Serotypes/ Subtypes | Biochemistry | Substrate (Cleavage Site) | Substrate Location | Neurotoxin Gene Location | Botulism |
|---|---|---|---|---|---|---|
| C. botulinum group I | A1 to A10, A(B), Ab, Af, Af84, A2F4F5 | Proteolytic | SNAP-25 (QR) SNAP 23 (AR) | Presynaptic plasma membrane | Chromosome or plasmid | Human/animal |
| B1 to B3, B5 (Bc), B6, B7, Ba, Bf | VAMP (QF) | Synaptic Vesicle | ||||
| F1 to F5 | VAMP 1 (QK) and VAMP 2 (LE) | Synaptic Vesicle | ||||
| X | VAMP 1, VAMP 2, VAMP 3, VAMP 4, VAMP 5 And Ykt6 (RA) | Synaptic Vesicle | ||||
| H | VAMP 1, VAMP 2, VAMP 3 (LE) | |||||
| C. botulinum group II | B4 | Non-proteolytic | VAMP 1 (QF) | Synaptic vesicle | Chromosome or plasmid | Human/animal |
| E1, E2, E3, E6 to E10 | SNAP25 (RI) | Presynaptic plasma membrane | ||||
| F6 | VAMP1, VAMP2, VAMP 3 (QK) | Synaptic vesicle | ||||
| C. botulinum group III | C, CD | Non-proteolytic | SNAP25 (RA), Syntaxin 1A (KA), Syntaxin 1B (KA), Syntaxin 2 (KA), Syntaxin 3 (KA) | Presynaptic plasma membrane | bacteriophage | Animal, very rare in human |
| D, DC | VAMP1, VAMP2, VAMP 3 (KL) | Synaptic vesicle | ||||
| C. botulinum group IV (C. argentinase) | G | Proteolytic | VAMP 1, VAMP 2, VAMP 3 (AA) | Synaptic vesicle | Plasmid | No natural case reported |
| C. butyricum group V | F7 | Non-proteolytic | VAMP 1, VAMP 2 (QK) | Synaptic vesicle | Transposon | Human |
| C. baratii group VI | E4, E5 | Non-proteolytic | SNAP-25 (RI) | Pre-synaptic plasma membrane | Transposon | Human |
| Other organisms producing BoNTs | En (Enterococcus faecium strain) | Non-proteolytic | VAMP 2 (DL), SNAP25, SNAP 23 (KD), Syntaxin (MD) | Synaptic vesicle/Plasma membrane | Conjugative plasmid | NA |
| BoNT/Wo or BoNT/I (Weissella Oryzae) | Non-proteolytic | VAMP2 | Synaptic vesicle | NA | ||
| Cp1 toxin (BoNT homolog) Chryseobacterium piperi | ? | ? | ? | ? |
| Serotypes | Ganglioside | Ganglioside-Binding Site |
|---|---|---|
| BoNT/A | GT1b, GD1a, GD1b, GM1 | H…SXWY…G |
| BoNT/B | GT1b, GD1a, GD1b, GM1 | H…SXWY…G |
| BoNT/C | GD1b, GT1b, GD1a, GM1a | -ND- |
| BoNT/D | GD2, GT1b, GD1b, PE | DXY…VXN |
| BoNT/DC | GM1a, GD1a, GD1b, GT1b | -ND- |
| BoNT/E | GD1a, GQ1b, GT1b, GM1 | K…SXWY..G |
| BoNT/F | GT1b, GD1a, GM3, GD1a, GM1 | H…SXWY..G |
| BoNT/G | GT1b, GD1a, GD1b, GM3, GM1 | G…SXWY..G |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kumar, R.; Singh, B.R. Botulinum Toxin: A Comprehensive Review of Its Molecular Architecture and Mechanistic Action. Int. J. Mol. Sci. 2025, 26, 777. https://doi.org/10.3390/ijms26020777
Kumar R, Singh BR. Botulinum Toxin: A Comprehensive Review of Its Molecular Architecture and Mechanistic Action. International Journal of Molecular Sciences. 2025; 26(2):777. https://doi.org/10.3390/ijms26020777
Chicago/Turabian StyleKumar, Raj, and Bal Ram Singh. 2025. "Botulinum Toxin: A Comprehensive Review of Its Molecular Architecture and Mechanistic Action" International Journal of Molecular Sciences 26, no. 2: 777. https://doi.org/10.3390/ijms26020777
APA StyleKumar, R., & Singh, B. R. (2025). Botulinum Toxin: A Comprehensive Review of Its Molecular Architecture and Mechanistic Action. International Journal of Molecular Sciences, 26(2), 777. https://doi.org/10.3390/ijms26020777




