Plasma Biomarkers in the Distinction of Alzheimer’s Disease and Frontotemporal Dementia
Abstract
:1. Introduction
2. Results
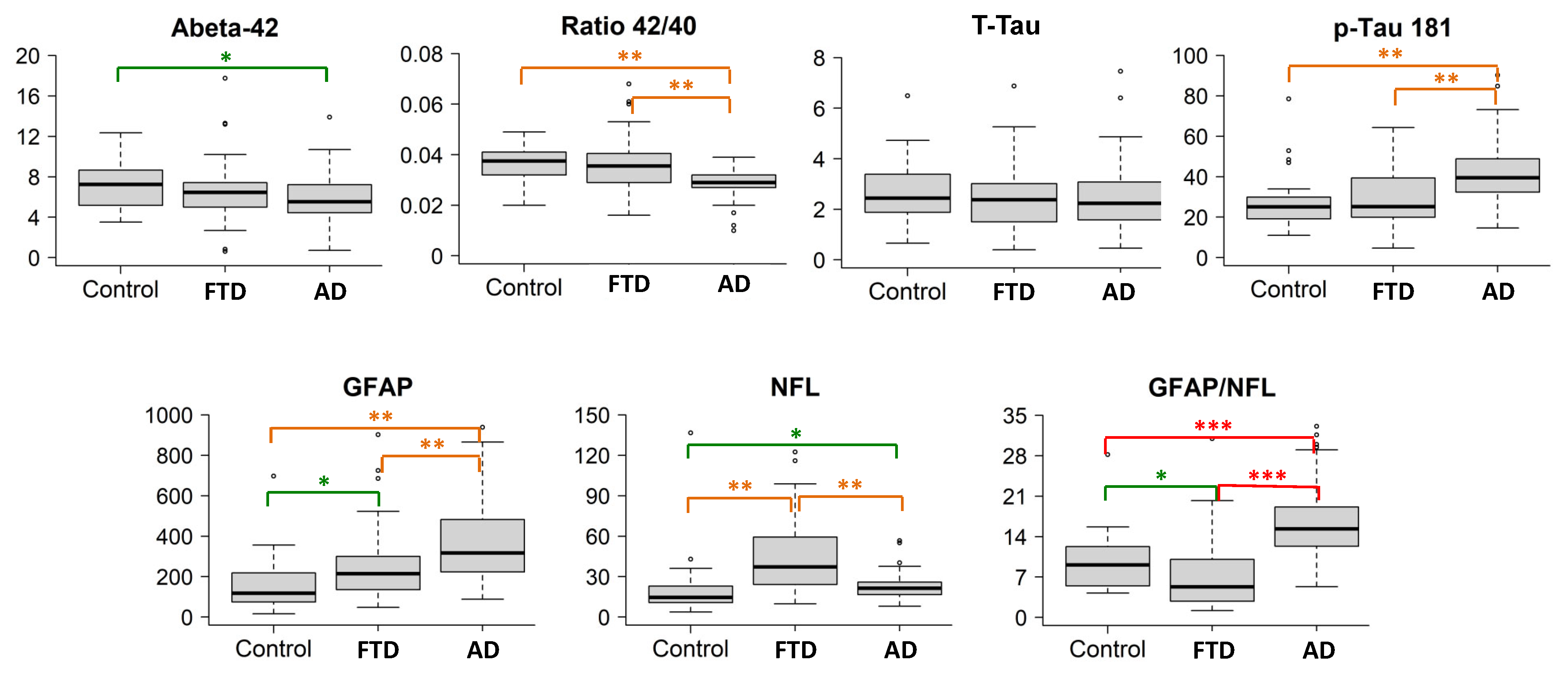
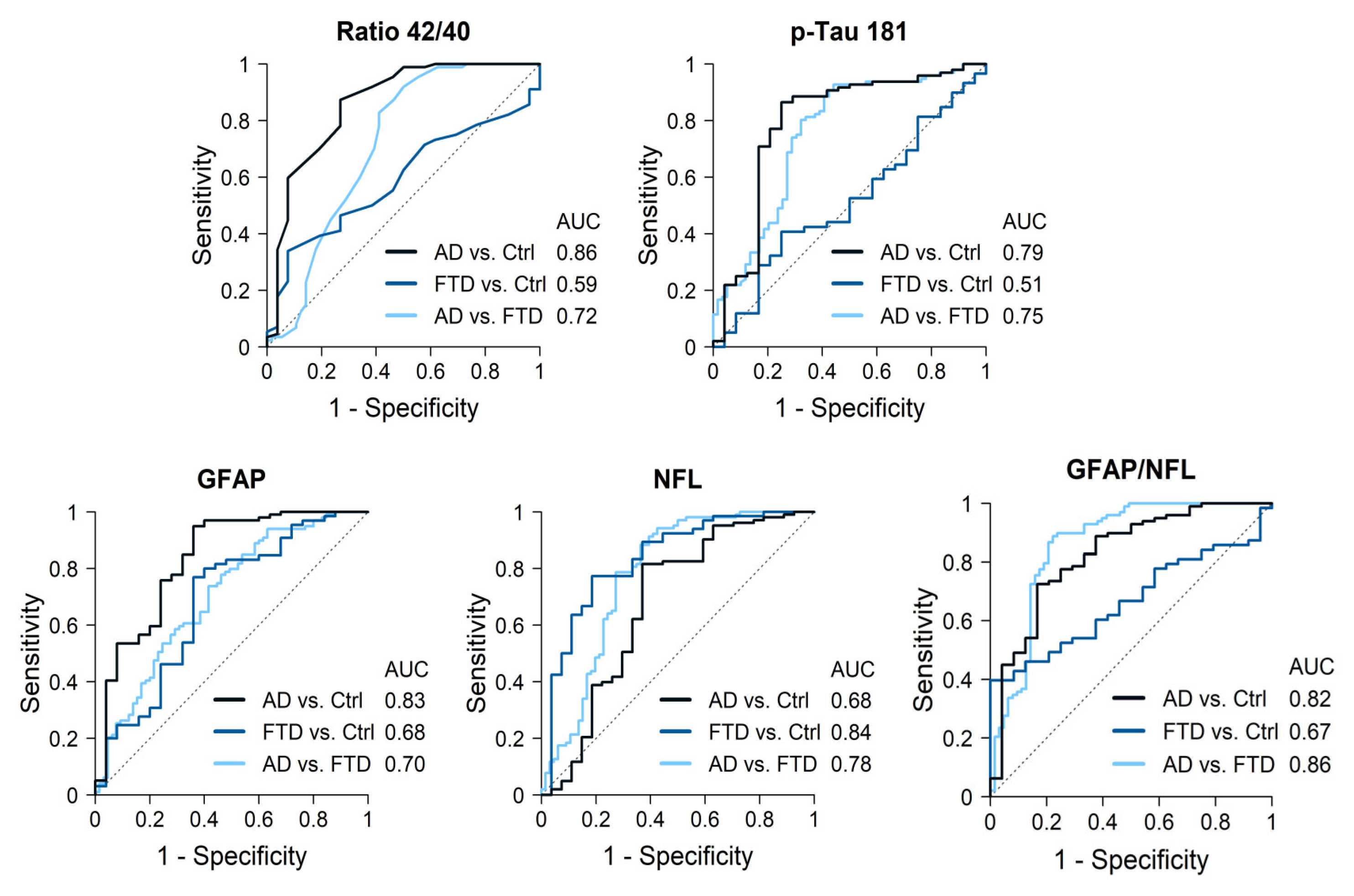
2.1. AD Cases Compared with Controls
2.2. AD Cases Compared with FTD Patients
2.3. FTD Cases Compared with Controls
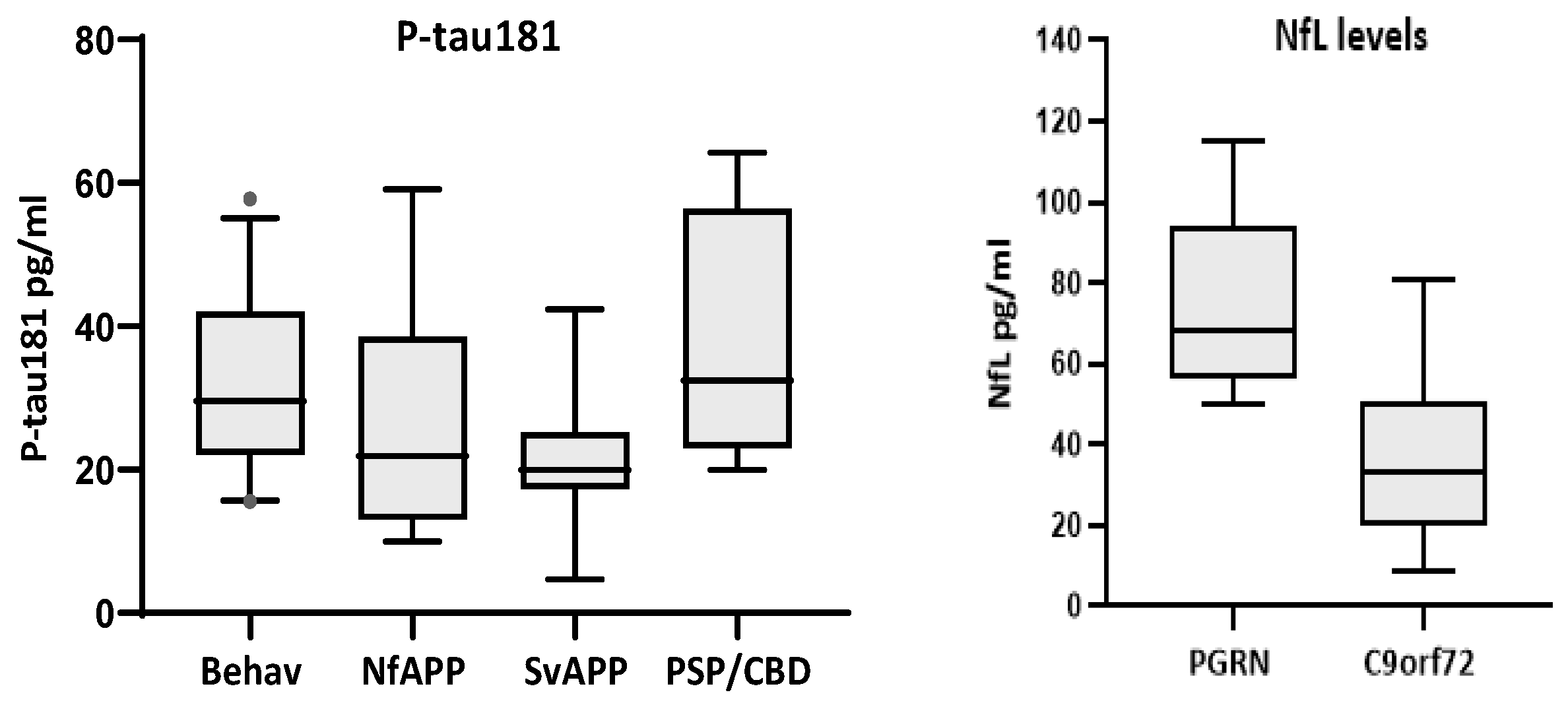
2.4. Biomarkers in FTD Subtypes
2.5. Other Correlations
3. Discussion
4. Materials and Methods
4.1. Population Studied
4.2. Methods
4.3. Analysis of the Data
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jack, C.R.; Bennett, D.A.; Blennow, K.; Carrillo, M.C.; Dunn, B.; Haeberlin, S.B.; Holtzman, D.M.; Jagust, W.; Jessen, F.; Kar-lawish, J.; et al. NIA-AA Research Framework:Toward a biological definition of Alzheimer’s disease. Alzheimer’s Dement. 2018, 14, 535–562. [Google Scholar] [CrossRef] [PubMed]
- Antonioni, A.; Raho, E.M.; Lopriore, P.; Pace, A.P.; Latino, R.R.; Assogna, M.; Mancuso, M.; Gragnaniello, D.; Granieri, E.; Pugliatti, M.; et al. Frontotemporal Dementia, Where Do We Stand? A Narrative Review. Int. J. Mol. Sci. 2023, 24, 11732. [Google Scholar] [CrossRef] [PubMed]
- Perrin, R.J.; Franklin, E.E.; Bernhardt, H.; Burns, A.; Schwetye, K.E.; Cairns, N.J.; Baxter, M.; Weiner, M.W.; Morris, J.C.; Initiative, A.D.N. The Alzheimer’s Disease Neuroimaging Initiative Neuropathology Core: An update. Alzheimer’s Dement. 2024, 20, 7859–7870. [Google Scholar] [CrossRef] [PubMed]
- Lewczuk, P.; Riederer, P.; O’Bryant, S.E.; Verbeek, M.M.; Dubois, B.; Visser, P.J.; Jellinger, K.A.; Engelborghs, S.; Ramirez, A.; Parnetti, L.; et al. Cerebrospinal fluid and blood biomarkers for neurodegenerative dementias: An update of the consensus of the task force on biological markers in psychiatry of the World Federation of Societies of Biological Psychiatry. World J. Biol. Psychiatry 2018, 19, 244–328. [Google Scholar] [CrossRef]
- Delaby, C.; Teunissen, C.E.; Blennow, K.; Alcolea, D.; Arisi, I.; Amar, E.B.; Beaume, A.; Bedel, A.; Bellomo, G.; Bigot-Corbel, E.; et al. Clinical reporting following the quantification of cerebrospinal fluid biomarkers in Alzheimer’s disease: An international overview. Alzheimer’s Dement. 2021, 18, 1868–1879. [Google Scholar] [CrossRef]
- Palmqvist, S.; Zetterberg, H.; Mattsson, N.; Johansson, P.; Alzheimer’s Disease Neuroimaging Initiative; Minthon, L.; Blennow, K.; Olsson, M.; Hansson, O.; Swedish BioFINDER Study Group. Detailed comparison of amyloid PET and CSF biomarkers for identifying early Alzheimer disease. Neurology 2015, 85, 1240–1249. [Google Scholar] [CrossRef]
- Alcolea, D.; Pegueroles, J.; Muñoz, L.; Camacho, V.; López-Mora, D.; Fernández-León, A.; Le Bastard, N.; Huyck, E.; Nadal, A.; Olmedo, V.; et al. Agreement of amyloid PET and CSF biomarkers for Alzheimer’s disease on Lumipulse. Ann. Clin. Transl. Neurol. 2019, 6, 1815–1824. [Google Scholar] [CrossRef]
- Teunissen, C.E.; Verberk, I.M.W.; Thijssen, E.H.; Vermunt, L.; Hansson, O.; Zetterberg, H.; van der Flier, W.M.; Mielke, M.M.; Del Campo, M. Blood-based biomarkers for Alzheimer’s disease: Towards clinical implementation. Lancet Neurol. 2022, 21, 66–77. [Google Scholar] [CrossRef]
- Garcia-Escobar, G.; Manero, R.M.; Fernández-Lebrero, A.; Ois, A.; Navalpotro-Gómez, I.; Puente-Periz, V.; Contador-Muñana, J.; Estragués-Gazquez, I.; Puig-Pijoan, A.; Jiménez-Balado, J. Blood Biomarkers of Alzheimer’s Disease and Cognition: A Literature Review. Biomolecules 2024, 14, 93. [Google Scholar] [CrossRef]
- Planche, V.; Bouteloup, V.; Pellegrin, I.; Mangin, J.-F.; Dubois, B.; Ousset, P.-J.; Pasquier, F.; Blanc, F.; Paquet, C.; Hanon, O.; et al. Validity and Performance of Blood Biomarkers for Alzheimer Disease to Predict Dementia Risk in a Large Clinic-Based Cohort. Neurology 2023, 100, e473–e484. [Google Scholar] [CrossRef]
- Martínez-Dubarbie, F.; Guerra-Ruiz, A.; López-García, S.; Lage, C.; Fernández-Matarrubia, M.; Infante, J.; Pozueta-Cantudo, A.; García-Martínez, M.; Corrales-Pardo, A.; Bravo, M.; et al. Accuracy of plasma Aβ40, Aβ42, and p-tau181 to detect CSF Alzheimer’s pathological changes in cognitively unimpaired subjects using the Lumipulse automated platform. Alzheimer’s Res. Ther. 2023, 15, 163. [Google Scholar] [CrossRef] [PubMed]
- Baiardi, S.; Quadalti, C.; Mammana, A.; Dellavalle, S.; Zenesini, C.; Sambati, L.; Pantieri, R.; Polischi, B.; Romano, L.; Suffritti, M.; et al. Diagnostic value of plasma p-tau181, NfL, and GFAP in a clinical setting cohort of prevalent neurodegenerative dementias. Alzheimer’s Res. Ther. 2022, 14, 153. [Google Scholar] [CrossRef] [PubMed]
- Palmqvist, S.; Stomrud, E.; Cullen, N.; Janelidze, S.; Manuilova, E.; Jethwa, A.; Bittner, T.; Eichenlaub, U.; Suridjan, I.; Kollmorgen, G.; et al. An accurate fully automated panel of plasma biomarkers for Alzheimer’s disease. Alzheimer’s Dement. 2022, 19, 1204–1215. [Google Scholar] [CrossRef] [PubMed]
- Delaby, C.; Bousiges, O.; Bouvier, D.; Fillée, C.; Fourier, A.; Mondésert, E.; Nezry, N.; Omar, S.; Quadrio, I.; Rucheton, B.; et al. Neurofilaments contribution in clinic: State of the art. Front. Aging Neurosci. 2022, 14, 1034684. [Google Scholar] [CrossRef] [PubMed]
- Mattsson-Carlgren, N.; Salvadó, G.; Ashton, N.J.; Tideman, P.; Stomrud, E.; Zetterberg, H.; Ossenkoppele, R.; Betthauser, T.J.; Cody, K.A.; Jonaitis, E.M.; et al. Prediction of Longitudinal Cognitive Decline in Preclinical Alzheimer Disease Using Plasma Biomarkers. JAMA Neurol. 2023, 80, 360–369. [Google Scholar] [CrossRef]
- Cullen, N.C.; Leuzy, A.; Janelidze, S.; Palmqvist, S.; Svenningsson, A.L.; Stomrud, E.; Dage, J.L.; Mattsson-Carlgren, N.; Hansson, O. Plasma biomarkers of Alzheimer’s disease improve prediction of cognitive decline in cognitively unimpaired elderly populations. Nat. Commun. 2021, 12, 3555. [Google Scholar] [CrossRef]
- VandeVrede, L.; Rabinovici, G.D. Blood-Based Biomarkers for Alzheimer Disease—Ready for Primary Care? JAMA Neurol. 2024, 81, 1030–1031. [Google Scholar] [CrossRef]
- Zhu, N.; Santos-Santos, M.; Illán-Gala, I.; Montal, V.; Estellés, T.; Barroeta, I.; Altuna, M.; Arranz, J.; Muñoz, L.; Belbin, O.; et al. Plasma glial fibrillary acidic protein and neurofilament light chain for the diagnostic and prognostic evaluation of frontotemporal dementia. Transl. Neurodegener. 2021, 10, 50. [Google Scholar] [CrossRef]
- Gaetani, L.; Blennow, K.; Calabresi, P.; Di Filippo, M.; Parnetti, L.; Zetterberg, H. Neurofilament light chain as a biomarker in neurological disorders. J. Neurol. Neurosurg. Psychiatry 2019, 90, 870–881. [Google Scholar]
- Katisko, K.; Cajanus, A.; Jääskeläinen, O.; Kontkanen, A.; Hartikainen, P.; Korhonen, V.E.; Helisalmi, S.; Haapasalo, A.; Koivumaa-Honkanen, H.; Herukka, S.K.; et al. Serum neurofilament light chain is a discriminative biomarker between frontotemporal lobar degeneration and primary psychiatric disorders. J. Neurol. 2020, 267, 162–167. [Google Scholar] [CrossRef]
- Pressman, P.S.; Matlock, D.; Ducharme, S. Distinguishing Behavioral Variant Frontotemporal Dementia From Primary Psychiatric Disorders: A Review of Recently Published Consensus Recommendations From the Neuropsychiatric International Consortium for Frontotemporal Dementia. J. Neuropsychiatry 2021, 33, 152–156. [Google Scholar] [CrossRef] [PubMed]
- Eratne, D.; Kang, M.; Malpas, C.; Simpson-Yap, S.; Lewis, C.; Dang, C.; Grewal, J.; Coe, A.; Dobson, H.; Keem, M.; et al. Plasma neurofilament light in behavioural variant frontotemporal dementia compared to mood and psychotic disorders. Aust. New Zealand J. Psychiatry 2023, 58, 70–81. [Google Scholar] [CrossRef] [PubMed]
- Steinacker, P.; Anderl-Straub, S.; Diehl-Schmid, J.; Semler, E.; Uttner, I.; von Arnim, C.A.F.; Barthel, H.; Danek, A.; Fassbender, K.; Fliessbach, K.; et al. Serum neurofilament light chain in behavioral variant frontotemporal dementia. Neurology 2018, 91, e1390–e1401. [Google Scholar] [CrossRef] [PubMed]
- Ashton, N.J.; Janelidze, S.; Al Khleifat, A.; Leuzy, A.; van der Ende, E.L.; Karikari, T.K.; Benedet, A.L.; Pascoal, T.A.; Lleó, A.; Parnetti, L.; et al. A multicentre validation study of the diagnostic value of plasma neurofilament light. Nat. Commun. 2021, 12, 3400. [Google Scholar] [CrossRef]
- Götze, K.; Vrillon, A.; Bouaziz-Amar, E.; Mouton-Liger, F.; Hugon, J.; Martinet, M.; Dumurgier, J.; Cognat, E.; Zetterberg, H.; Blennow, K.; et al. Plasma neurofilament light chain in memory clinic practice: Evidence from a real-life study. Neurobiol. Dis. 2023, 176, 105937. [Google Scholar] [CrossRef]
- van der Ende, E.L.; van Swieten, J.C. Fluid Biomarkers of Frontotemporal Lobar Degeneration. In Frontotemporal Dementias; Ghetti, B., Buratti, E., Boeve, B., Rademakers, R., Eds.; Advances in Experimental Medicine and Biology Series 1281; Springer: Cham, Switzerland, 2021. [Google Scholar] [CrossRef]
- Liampas, I.; Kyriakoulopoulou, P.; Karakoida, V.; Kavvoura, P.A.; Sgantzos, M.; Bogdanos, D.P.; Stamati, P.; Dardiotis, E.; Siokas, V. Blood-Based Biomarkers in Frontotemporal Dementia: A Narrative Review. Int. J. Mol. Sci. 2024, 25, 11838. [Google Scholar] [CrossRef]
- Milà-Alomà, M.; Salvadó, G.; Gispert, J.D.; Vilor-Tejedor, N.; Grau-Rivera, O.; Sala-Vila, A.; Sánchez-Benavides, G.; Arenaza-Urquijo, E.M.; Crous-Bou, M.; González-De-Echávarri, J.M.; et al. Amyloid beta, tau, synaptic, neurodegeneration, and glial biomarkers in the preclinical stage of the Alzheimer’s continuum. Alzheimer’s Dement. 2020, 16, 1358–1371. [Google Scholar] [CrossRef]
- Pereira, J.B.; Janelidze, S.; Smith, R.; Mattsson-Carlgren, N.; Palmqvist, S.; E Teunissen, C.; Zetterberg, H.; Stomrud, E.; Ashton, N.J.; Blennow, K.; et al. Plasma GFAP is an early marker of amyloid-β but not tau pathology in Alzheimer’s disease. Brain 2021, 144, 3505–3516. [Google Scholar] [CrossRef]
- Gómez-Tortosa, E.; Agüero-Rabes, P.; Ruiz-González, A.; Wagner, S.; Téllez, R.; Mahillo, I.; Ruiz-Calvo, A.; Sainz, M.J.; Nystrom, A.L.; Cremades-Jimeno, L.; et al. Plasma Neurodegenerative Biomarkers in Cognitively Preserved Nonagenarians. Aging Dis. 2024. [Google Scholar] [CrossRef]
- Thijssen, E.H.; Verberk, I.M.W.; Kindermans, J.; Abramian, A.; Vanbrabant, J.; Ball, A.J.; Pijnenburg, Y.; Lemstra, A.W.; van der Flier, W.M.; Stoops, E.; et al. Differential diagnostic performance of a panel of plasma biomarkers for different types of dementia. Alzheimer Dement. Diagn. Assess. Dis. Monit. 2022, 14, e12285. [Google Scholar] [CrossRef]
- Mattsson, N.; Zetterberg, H.; Janelidze, S.; Insel, P.S.; Andreasson, U.; Stomrud, E.; Palmqvist, S.; Baker, D.; Hehir, C.A.T.; Jeromin, A.; et al. Plasma tau in Alzheimer disease. Neurology 2016, 87, 1827–1835. [Google Scholar] [CrossRef] [PubMed]
- Forgrave, L.M.; Ma, M.; Best, J.R.; DeMarco, M.L. The diagnostic performance of neurofilament light chain in CSF and blood for Alzheimer’s disease, frontotemporal dementia, and amyotrophic lateral sclerosis: A systematic review and meta-analysis. Alzheimer Dement. Diagn. Assess. Dis. Monit. 2019, 11, 730–743. [Google Scholar] [CrossRef] [PubMed]
- Verberk, I.M.W.; Jutte, J.; Kingma, M.Y.; Vigneswaran, S.; Gouda, M.M.T.E.E.; van Engelen, M.; Alcolea, D.; Arranz, J.; Fortea, J.; Lleó, A.; et al. Development of thresholds and a visualization tool for use of a blood test in routine clinical dementia practice. Alzheimer’s Dement. 2024, 20, 6115–6132. [Google Scholar] [CrossRef] [PubMed]
- Cousins, K.A.Q.; Phillips, J.S.; Das, S.R.; O’Brien, K.; Tropea, T.F.; Chen-Plotkin, A.; Shaw, L.M.; Nasrallah, I.M.; Mechanic-Hamilton, D.; McMillan, C.T.; et al. Pathologic and cognitive correlates of plasma biomarkers in neurodegenerative disease. Alzheimer’s Dement. 2024, 20, 3889–3905. [Google Scholar] [CrossRef]
- Chen, Y.; Wang, Y.; Tao, Q.; Lu, P.; Meng, F.; Zhuang, L.; Qiao, S.; Zhang, Y.; Luo, B.; Liu, Y.; et al. Diagnostic value of isolated plasma biomarkers and its combination in neurodegenerative dementias: A multicenter cohort study. Clin. Chim. Acta 2024, 558, 118784. [Google Scholar] [CrossRef]
- Saracino, D.; Dorgham, K.; Camuzat, A.; Rinaldi, D.; Rametti-Lacroux, A.; Houot, M.; Clot, F.; Martin-Hardy, P.; Jornea, L.; Azuar, C.; et al. Plasma NfL levels and longitudinal change rates in C9orf72 and GRN-associated diseases: From tailored references to clinical applications. J. Neurol. Neurosurg. Psychiatry 2021, 92, 1278–1288. [Google Scholar] [CrossRef]
- Meeter, L.H.; Dopper, E.G.; Jiskoot, L.C.; Sanchez-Valle, R.; Graff, C.; Benussi, L.; Ghidoni, R.; Pijnenburg, Y.A.; Borroni, B.; Galimberti, D.; et al. Neurofilament light chain: A biomarker for genetic frontotemporal dementia. Ann. Clin. Transl. Neurol. 2016, 3, 623–636. [Google Scholar] [CrossRef]
- van der Ende, E.L.; Meeter, L.H.; Poos, J.M.; Panman, J.L.; Jiskoot, L.C.; Dopper, E.G.P.; Papma, J.M.; de Jong, F.J.; Verberk, I.M.W.; Teunissen, C.; et al. Serum neurofilament light chain in genetic frontotemporal dementia: A longitudinal, multicentre cohort study. Lancet Neurol. 2019, 18, 1103–1111. [Google Scholar] [CrossRef]
- Bendstrup, N.; Hejl, A.-M.; Salvesen, L. Neurofilament light chain levels in frontotemporal dementia and progressive supranuclear palsy: A systematic review. J. Alzheimer’s Dis. 2022, 87, 131–140. [Google Scholar] [CrossRef]
- Cousins, K.A.Q.; Shaw, L.M.; Chen-Plotkin, A.; Wolk, D.A.; Van Deerlin, V.M.; Lee, E.B.; McMillan, C.T.; Grossman, M.; Irwin, D.J. Distinguishing frontotemporal lobar degeneration tau from TDP-43 using plasma biomarkers. JAMA Neurol. 2022, 79, 1155–1164. [Google Scholar] [CrossRef]
- Rascovsky, K.; Hodges, J.R.; Knopman, D.; Mendez, M.F.; Kramer, J.H.; Neuhaus, J.; van Swieten, J.C.; Seelaar, H.; Dopper, E.G.; Onyike, C.U.; et al. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain 2011, 134, 2456–2477. [Google Scholar] [CrossRef] [PubMed]
- Gorno-Tempini, M.L.; Hillis, A.E.; Weintraub, S.; Kertesz, A.; Mendez, M.; Cappa, S.F.; Ogar, J.M.; Rohrer, J.D.; Black, S.; Boeve, B.F.; et al. Classification of primary progressive aphasia and its variants. Neurology 2011, 76, 1006–1014. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, M.J.; Litvan, I.; Lang, A.E.; Bak, T.H.; Bhatia, K.P.; Borroni, B.; Boxer, A.L.; Dickson, D.W.; Grossman, M.; Hallett, M.; et al. Criteria for the diagnosis of corticobasal degeneration. Neurology 2013, 80, 496–503. [Google Scholar] [CrossRef] [PubMed]
- Hoglinger, G.U.; Respondek, G.; Stamelou, M.; Kurz, C.; Josephs, K.A.; Lang, A.E.; Mollenhauer, B.; Müller, U.; Nilsson, C.; Whitwell, J.L.; et al. Clinical diagnosis of progressive supranuclear palsy: The movement disorder society criteria. Mov. Disord. 2017, 32, 853–864.46. [Google Scholar] [CrossRef] [PubMed]
- Olazarán, J.; Valentí, M.; Frades, B.; Zea-Sevilla, M.A.; Ávila-Villanueva, M.; Fernández-Blázquez, M.Á.; Calero, M.; Dobato, J.L.; Hernández-Tamames, J.A.; León-Salas, B.; et al. The Vallecas Project: A Cohort to Identify Early Markers and Mechanisms of Alzheimer’s Disease. Front. Aging Neurosci. 2015, 7, 181. [Google Scholar] [CrossRef]
| GROUP | N Plasma | N CSF | Age (yrs) Mean ± SD | Gender % Female | APOE Genotype | Genetics |
|---|---|---|---|---|---|---|
| AD | 108 | 108 | 68 ± 6 | 56% | 3/3 (43%); 3/4 (43%); 4/4 (11%) | -- |
| FTD Bv-FTD Nf-PPA Sv-PPA Bv/ALS PSP/CBD | 73 32 16 13 7 5 | 28 13 7 5 1 2 | 65 ± 9 66 ± 10 63 ± 8 65 ± 8 61 ± 6 68 ± 5 | 64% 52% 75% 76% 85% 60% | 3/3 (77%); 3/4 (19%); 2/3 (6%); 4/4 (2%) | 13 C9ORF72 7 PGRN 2 TBK1 1 KIF5A 1 MAPT |
| Controls | 54 | 14 | 69 ± 5 | 57% | 3/3 (67%); 3/4 (13%); 2/3 (13%); 2/4 (7%) | -- |
| Kruskal-Wallis | Comparison Between Two Groups * | |||
|---|---|---|---|---|
| Biomarker | P | AD vs. Controls | AD vs. FTD | FTD vs. Controls |
| Aβ40 Aβ42 Aβ42/40 ratio T-tau p-tau181 T-tau/Aβ42 GFAP NfL GFAP/NfL ratio | 0.503 0.028 <0.001 0.539 <0.001 0.812 <0.001 <0.001 <0.0001 | ns 0.039 <0.001 ns <0.001 ns <0.001 0.005 <0.0001 | ns ns <0.001 ns <0.001 ns <0.001 <0.001 <0.0001 | ns ns ns ns ns ns 0.007 <0.001 <0.007 |
| Comparison | Biomarker | Cutoff pg/mL | Sensitivity | Specificity | AUC (95% CI) |
|---|---|---|---|---|---|
| AD-Controls | Aß42 Aß42/40 ratio p-tau181 GFAP NfL GFAP/NfL ratio | <7.17 <0.034 >28.1 >134 >15.5 >12.8 | 75% 87% 86% 95% 82% 72% | 57% 73% 75% 64% 63% 83% | 0.66 (0.54–0.77) 0.86 (0.77–0.95) 0.79 (0.67–0.91) 0.83 (0.73–0.94) 0.68 (0.54–0.81) 0.82 (0.72–0.92) |
| AD-FTD | Aß42/40 ratio p-tau181 GFAP NfL GFAP/NfL ratio | <0.036 >25.6 >231 <29.8 >10.4 | 92% 93% 74% 88% 89% | 50% 56% 58% 64% 78% | 0.72 (0.62–0.81) 0.75 (0.67–0.75) 0.70 (0.62–0.79) 0.78 (0.70–0.86) 0.86 (0.80–0.93) |
| FTD-Controls | GFAP NfL GFAP/NfL ratio | >134 >23.5 <4.2 | 77% 77% 40% | 64% 81% 100% | 0.68 (0.55–0.82) 0.84 (0.74–0.93) 0.67 (0.55–0.78) |
| Groups | Adding a Second Biomarker | Adding a Third Biomarker | ||
|---|---|---|---|---|
| Main Discriminative Biomarker: AUC | Quantitative AUC (95% CI) | Quantitative AUC (95% CI) | ||
| AD vs. Controls Aβ42/40 ratio: 0.86 | + p-tau181 + GFAP + NfL | 0.87 (0.76–0.98) 0.87 (0.75–0.99) 0.87 (0.76–0.97) | + NfL | 0.92 (0.83–1.00) |
| AD vs. FTD NfL: 0.80 | + p-tau181 + Aβ42/40 ratio + GFAP + Aβ42 | 0.87 (0.79–0.95) 0.84 (0.76–0.93) 0.84 (0.76–0.92) 0.81 (0.72–0.89) | + Aβ42/40 ratio + p-tau181 + p-tau181 | 0.90 (0.83–0.97) 0.89 (0.81–0.96) 0.88 (0.80–0.95) |
| FTD vs. controls NfL: 0.87 | + Aβ40 + T-tau | 0.88 (0.78–0.98) 0.88 (0.77–0.98) | No increase | |
| Genetics | Presumed Pathology | |||
|---|---|---|---|---|
| Biomarker | Non-genetic # (n = 52) | Genetic (n = 24) | TDP43 like (n = 41) | Tau like (n =13) |
| Aβ42 | 6.7 (5.6, 7.6) | 5.7 (4.8, 6.5) | 6.2 (4.9, 7.3) | 7.0 (5.6, 7.7) |
| 42/40 ratio | 0.036 (0.030, 0.042) | 0.034 (0.027, 0.038) | 0.034 (0.028, 0.038) | 0.036 (0.030, 0.039) |
| T-tau | 2.6 (1.9, 3.0) | 2.0 (1.4, 3.0) | 2.4 (1.5, 3.0) | 2.0 (1.2, 2.6) |
| p-tau181 | 25 (20, 33) | 25 (16, 42) | 24 (18, 41) | 26 (19, 32) |
| GFAP | 214 (143, 322) | 214 (127, 308) | 216 (135, 300) | 210 (178, 324) |
| NfL | 32 (12, 47) | 50 (27, 66) | 47 (28, 63) | 30 (27, 57) |
| P * | P Ns for every biomarker | P Ns for every biomarker | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gómez-Tortosa, E.; Agüero-Rabes, P.; Ruiz-González, A.; Wagner-Reguero, S.; Téllez, R.; Mahillo, I.; Ruiz-Calvo, A.; Sainz, M.J.; Nystrom, A.L.; del Ser, T.; et al. Plasma Biomarkers in the Distinction of Alzheimer’s Disease and Frontotemporal Dementia. Int. J. Mol. Sci. 2025, 26, 1231. https://doi.org/10.3390/ijms26031231
Gómez-Tortosa E, Agüero-Rabes P, Ruiz-González A, Wagner-Reguero S, Téllez R, Mahillo I, Ruiz-Calvo A, Sainz MJ, Nystrom AL, del Ser T, et al. Plasma Biomarkers in the Distinction of Alzheimer’s Disease and Frontotemporal Dementia. International Journal of Molecular Sciences. 2025; 26(3):1231. https://doi.org/10.3390/ijms26031231
Chicago/Turabian StyleGómez-Tortosa, Estrella, Pablo Agüero-Rabes, Alicia Ruiz-González, Sonia Wagner-Reguero, Raquel Téllez, Ignacio Mahillo, Andrea Ruiz-Calvo, María José Sainz, Anna Lena Nystrom, Teodoro del Ser, and et al. 2025. "Plasma Biomarkers in the Distinction of Alzheimer’s Disease and Frontotemporal Dementia" International Journal of Molecular Sciences 26, no. 3: 1231. https://doi.org/10.3390/ijms26031231
APA StyleGómez-Tortosa, E., Agüero-Rabes, P., Ruiz-González, A., Wagner-Reguero, S., Téllez, R., Mahillo, I., Ruiz-Calvo, A., Sainz, M. J., Nystrom, A. L., del Ser, T., & Sánchez-Juan, P. (2025). Plasma Biomarkers in the Distinction of Alzheimer’s Disease and Frontotemporal Dementia. International Journal of Molecular Sciences, 26(3), 1231. https://doi.org/10.3390/ijms26031231






