VEGF in Tears as a Biomarker for Exudative Age-Related Macular Degeneration: Molecular Dynamics in a Mouse Model and Human Samples
Abstract
1. Introduction
2. Results
2.1. Demographic Data
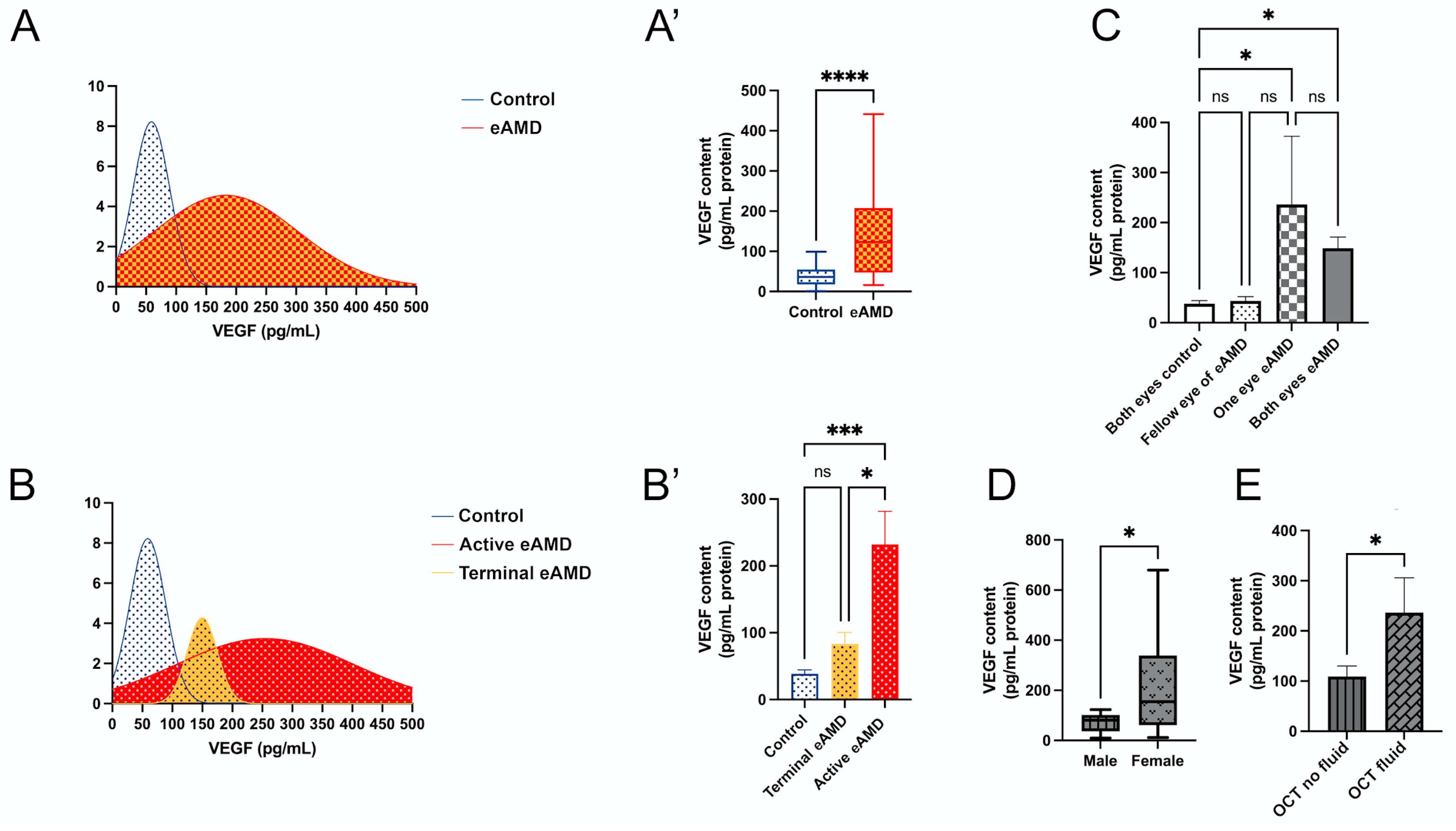
2.2. VEGF Levels in Human Tears
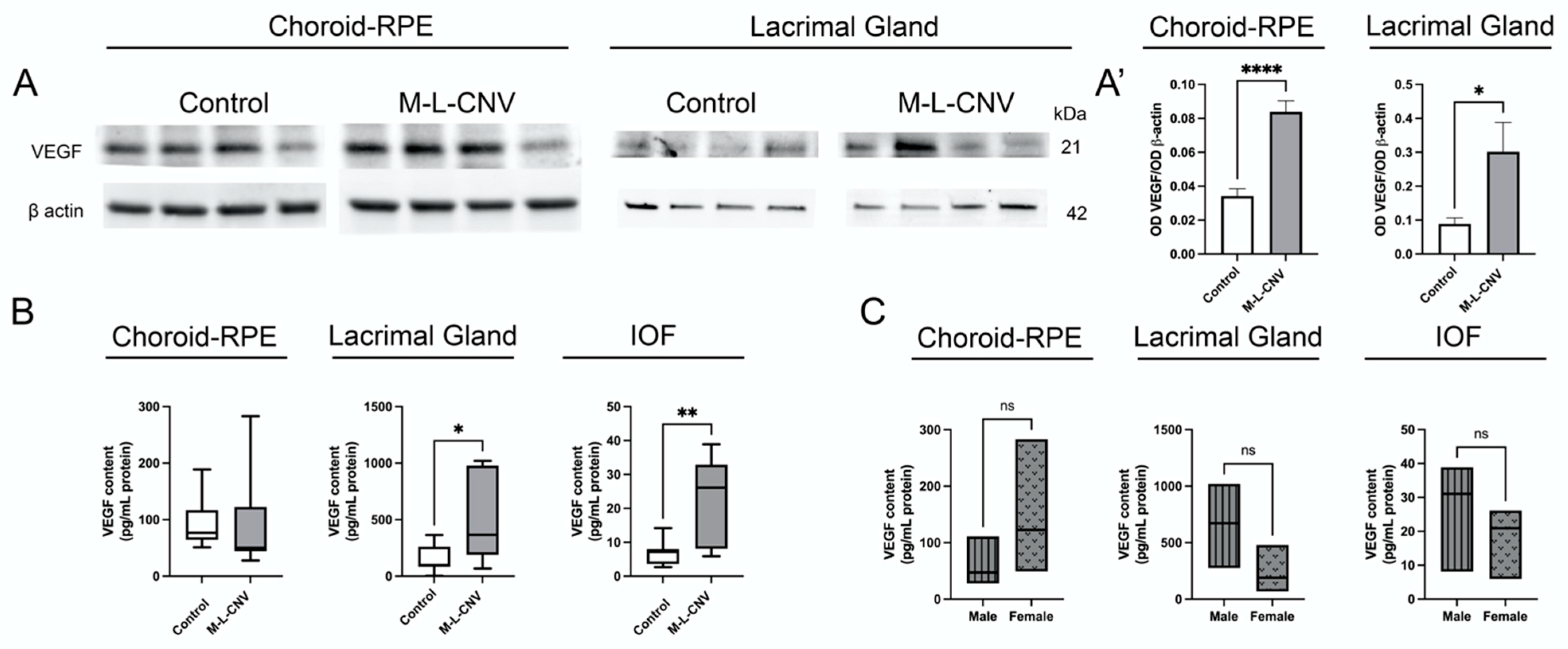
2.3. VEGF Levels in lCNV
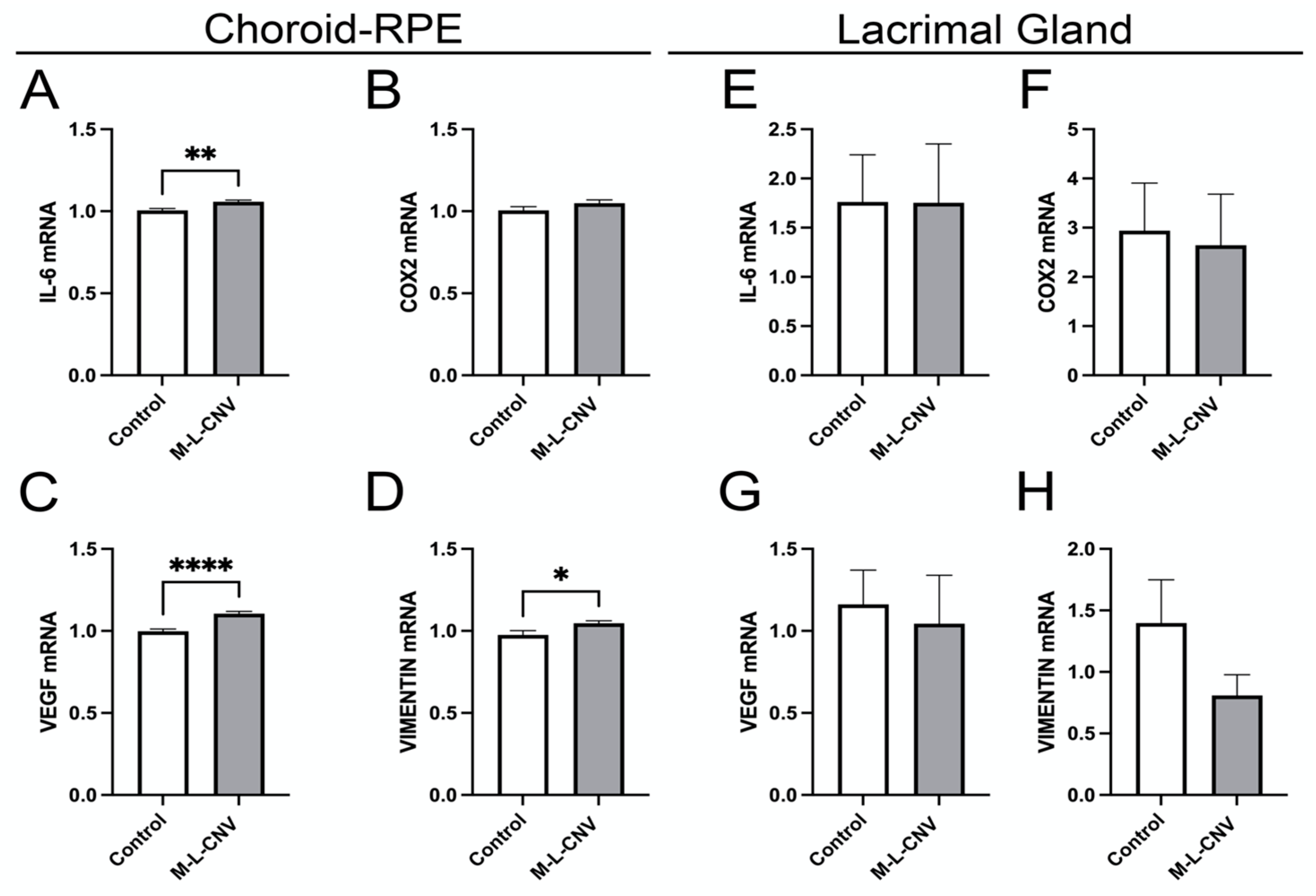
2.4. Transcription Factor Activation in Response to VEGF Elevation in the lCNV Mouse Model
2.5. Dynamic Transcriptional Regulation of Key Genes in the lCNV Model
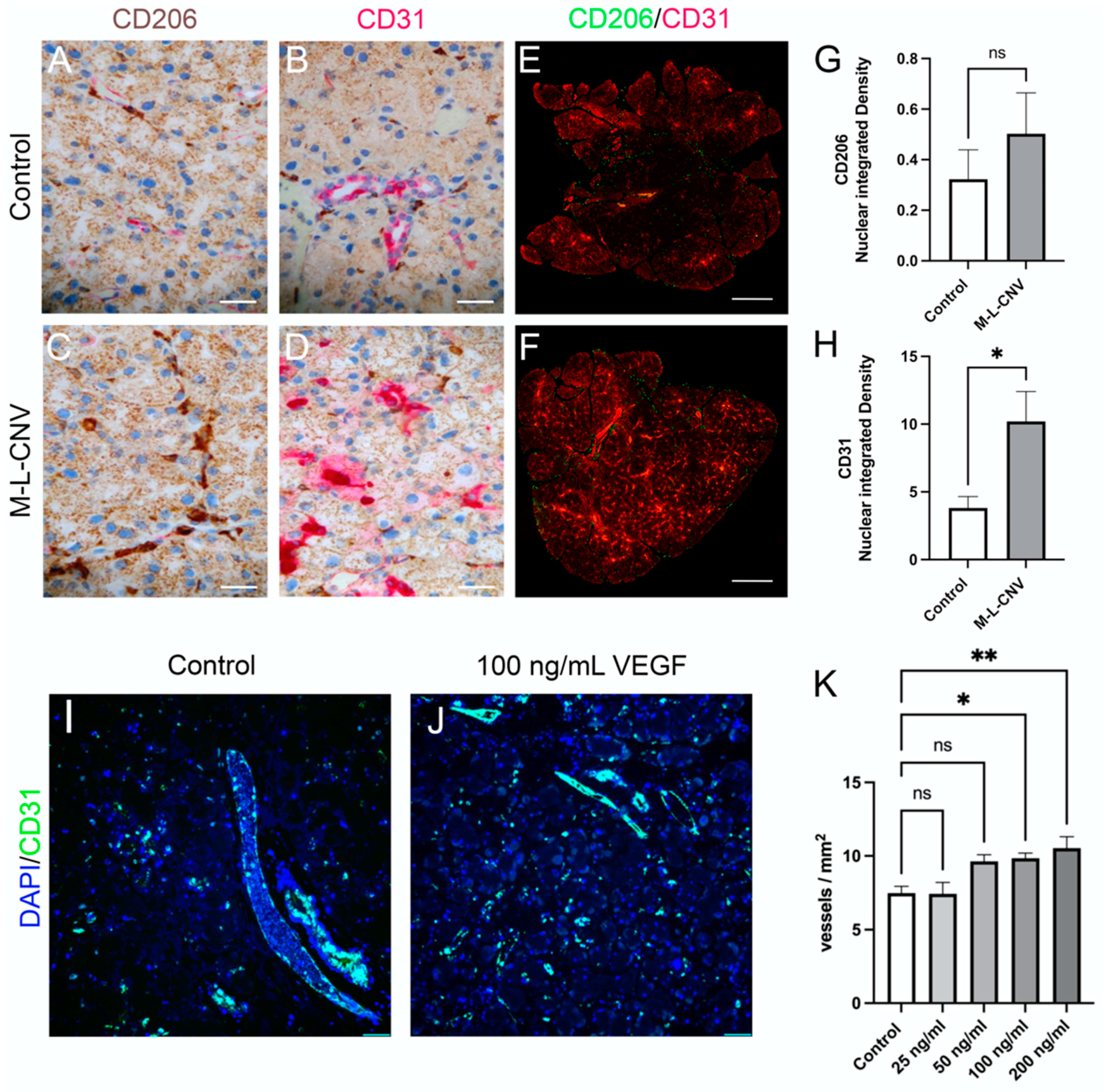
2.6. Evaluation of LG Neovascularization and Immune Cell Recruitment in Response to VEGF
3. Discussion
4. Materials and Methods
4.1. Recruitment of Study Participants and Tear Fluid Collection
4.2. Proximity Real-Time PCR Immunoassays
4.3. Animals and CNV Induction
4.4. Animal Tears, Aqueous and Vitreous Humors, and RPE–Choroid Complex Dissection
4.5. Ex Vivo Culture and Treatment
4.6. Tissue Processing for Histology and Immunohistochemistry
4.7. Western Blot
4.8. Quantitative PCR
4.9. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AMD | Age-related macular degeneration |
| BCVA | Best-corrected visual acuity |
| BMI | Body mass index |
| CFT | Central foveal thickness |
| CI | Confidence interval |
| CNV | Choroidal neovascularization |
| eAMD | Exudative age-related macular degeneration |
| HTN | Hypertension |
| CI | Confidence interval |
| IHD | Ischemic heart disease |
| IOF | Intraocular fluid |
| qPCR | Quantitative real-time PCR |
| LG | Lacrimal glands |
| lCNV | Laser-induced choroidal neovascularization |
| OCT | Optical coherence tomography |
| OD | Optical density |
| PB | Phosphate buffer |
| PBS | Phosphate-buffered saline |
| RpL13a | Ribosomal protein L13a |
| RPE | Retinal pigment epithelium |
| SEM | Standard error of the mean |
| VA | Visual acuity |
| VEGF | Vascular endothelial growth factor |
References
- Curcio, C.A. Soft Drusen in Age-Related Macular Degeneration: Biology and Targeting Via the Oil Spill Strategies. Investig. Opthalmol. Vis. Sci. 2018, 59, AMD160–AMD181. [Google Scholar] [CrossRef]
- Fleckenstein, M.; Keenan, T.D.L.; Guymer, R.H.; Chakravarthy, U.; Schmitz-Valckenberg, S.; Klaver, C.C.; Wong, W.T.; Chew, E.Y. Age-related macular degeneration. Nat. Rev. Dis. Primers 2021, 7, 31. [Google Scholar] [CrossRef] [PubMed]
- Christoforidis, J.B.; Tecce, N.; Dell’Omo, R.; Mastropasqua, R.; Verolino, M.; Costagliola, C. Age related macular degeneration and visual disability. Curr. Drug Targets 2011, 12, 221–233. [Google Scholar] [CrossRef] [PubMed]
- Ziemssen, F.; Eter, N.; Fauser, S.; Bopp, S.; Radermacher, M.; Hasanbasic, Z.; Holz, F.G.; AURA-Studiengruppe. Retrospective investigation of anti-VEGF treatment reality and effectiveness in patients with neovascular age-related macular degeneration (AMD) in Germany: Treatment reality of ranibizumab for neovascular AMD in Germany. Ophthalmologe 2015, 112, 246–254. [Google Scholar] [CrossRef] [PubMed]
- Schmidt-Erfurth, U.; Chong, V.; Loewenstein, A.; Larsen, M.; Souied, E.; Schlingemann, R.; Eldem, B.; Monés, J.; Richard, G.; Bandello, F. Guidelines for the management of neovascular age-related macular degeneration by the European Society of Retina Specialists (EURETINA). Br. J. Ophthalmol. 2014, 98, 1144–1167. [Google Scholar] [CrossRef]
- Nguyen, C.L.; Oh, L.J.; Wong, E.; Wei, J.; Chilov, M. Anti-vascular endothelial growth factor for neovascular age-related macular degeneration: A meta-analysis of randomized controlled trials. BMC Ophthalmol. 2018, 18, 130. [Google Scholar] [CrossRef]
- Yu, Y.; Bhangale, T.R.; Fagerness, J.; Ripke, S.; Thorleifsson, G.; Tan, P.L.; Souied, E.H.; Richardson, A.J.; Merriam, J.E.; Buitendijk, G.H.; et al. Common variants near FRK/COL10A1 and VEGFA are associated with advanced age-related macular degeneration. Hum. Mol. Genet. 2011, 20, 3699–3709. [Google Scholar] [CrossRef]
- Kozhevnikova, O.; Fursova, A.Z.; Markovets, A.M.; Telegina, D.; Muraleva, N.; Kolosova, N.G. VEGF and PEDF levels in the rat retina: Effects of aging and AMD-like retinopathy. Adv. Gerontol. 2018, 31, 339–344. [Google Scholar]
- Falavarjani, K.G.; Nguyen, Q.D. Adverse events and complications associated with intravitreal injection of anti-VEGF agents: A review of literature. Eye 2013, 27, 787–794. [Google Scholar] [CrossRef]
- Pennesi, M.E.; Neuringer, M.; Courtney, R.J. Animal models of age related macular degeneration. Mol. Asp. Med. 2012, 33, 487–509. [Google Scholar] [CrossRef]
- Huang, C.; Xu, Y.; Li, X.; Wang, W. Vascular endothelial growth factor A polymorphisms and age-related macular degeneration: A systematic review and meta-analysis. Mol. Vis. 2013, 19, 1211. [Google Scholar] [PubMed]
- Cascella, R.; Strafella, C.; Caputo, V.; Errichiello, V.; Zampatti, S.; Milano, F.; Potenza, S.; Mauriello, S.; Novelli, G.; Ricci, F.; et al. Towards the application of precision medicine in Age-Related Macular Degeneration. Prog. Retin. Eye Res. 2017, 63, 132–146. [Google Scholar] [CrossRef]
- Oca, A.I.; Pérez-Sala, Á.; Pariente, A.; Ochoa, R.; Velilla, S.; Peláez, R.; Larráyoz, I.M. Predictive Biomarkers of Age-Related Macular Degeneration Response to Anti-VEGF Treatment. J. Pers. Med. 2021, 11, 1329. [Google Scholar] [CrossRef]
- Salas, A.; Badia, A.; Fontrodona, L.; Zapata, M.; García-Arumí, J.; Duarri, A. Neovascular Progression and Retinal Dysfunction in the Laser-Induced Choroidal Neovascularization Mouse Model. Biomedicines 2023, 11, 2445. [Google Scholar] [CrossRef] [PubMed]
- Zhan, P.; Cui, Y.; Cao, Y.; Bao, X.; Wu, M.; Yang, Q.; Yang, J.; Zheng, H.; Zou, J.; Xie, T.; et al. PGE2 promotes macrophage recruitment and neovascularization in murine wet-type AMD models. Cell Commun. Signal. 2022, 20, 155. [Google Scholar] [CrossRef] [PubMed]
- Xu, N.; Sun, T.; Wang, Y.; Tong, X.; Lu, S.; Yang, F.; Wang, J.; Bo, Q.; Sun, J.; Sun, X. Dynamic changes in macrophage morphology during the progression of choroidal neovascularization in a laser-induced choroidal neovascularization mouse model. BMC Ophthalmol. 2023, 23, 401. [Google Scholar] [CrossRef]
- Muller, W.A. The role of PECAM-1 (CD31) in leukocyte emigration: Studies in vitro and in vivo. J. Leukoc. Biol. 1995, 57, 523–528. [Google Scholar] [CrossRef]
- Mitchell, P.; Liew, G.; Gopinath, B.; Wong, T.Y. Age-related macular degeneration. Lancet 2018, 392, 1147–1159. [Google Scholar] [CrossRef]
- Lambert, N.G.; ElShelmani, H.; Singh, M.K.; Mansergh, F.C.; Wride, M.A.; Padilla, M.; Keegan, D.; Hogg, R.E.; Ambati, B.K. Risk factors and biomarkers of age-related macular degeneration. Prog. Retin. Eye Res. 2016, 54, 64–102. [Google Scholar] [CrossRef]
- Lukacs, R.; Schneider, M.; Nagy, Z.Z.; Sandor, G.L.; Kaan, K.; Asztalos, A.; Enyedi, L.; Pek, G.; Barcsay, G.; Szabo, A.; et al. Seven-year outcomes following intensive anti-vascular endothelial growth factor therapy in patients with exudative age-related macular degeneration. BMC Ophthalmol. 2023, 23, 110. [Google Scholar] [CrossRef]
- Corazza, P.; D’alterio, F.M.; Kabbani, J.; Alam, M.M.R.; Mercuri, S.; Orlans, H.O.; Younis, S. Long-term outcomes of intravitreal anti-VEGF therapies in patients affected by neovascular age-related macular degeneration: A real-life study. BMC Ophthalmol. 2021, 21, 300. [Google Scholar] [CrossRef] [PubMed]
- Moraru, A.D.; Danielescu, C.; Iorga, R.E.; Moraru, R.L.; Zemba, M.; Branisteanu, D.C. Review of Guideline Recommendations for Optimal Anti-VEGF Therapy in Age-Related Macular Degeneration. Life 2024, 14, 1220. [Google Scholar] [CrossRef] [PubMed]
- Malamitsi-Puchner, A.; Tziotis, J.; Tsonou, A.; Protonotariou, E.; Sarandakou, A.; Creatsas, G. Changes in serum levels of vascular endothelial growth factor in males and females throughout life. J. Soc. Gynecol. Investig. 2000, 7, 309–312. [Google Scholar] [CrossRef]
- Tillmann, A.; Ceklic, L.; Dysli, C.; Munk, M.R. Gender differences in retinal diseases: A review. Clin. Exp. Ophthalmol. 2024, 52, 317–333. [Google Scholar] [CrossRef] [PubMed]
- Gustafsdottir, S.M.; Schallmeiner, E.; Fredriksson, S.; Gullberg, M.; Söderberg, O.; Jarvius, M.; Jarvius, J.; Howell, M.; Landegren, U. Proximity ligation assays for sensitive and specific protein analyses. Anal. Biochem. 2005, 345, 2–9. [Google Scholar] [CrossRef]
- Lundberg, M.; Eriksson, A.; Tran, B.; Assarsson, E.; Fredriksson, S. Homogeneous antibody-based proximity extension assays provide sensitive and specific detection of low-abundant proteins in human blood. Nucleic Acids Res. 2011, 39, e102. [Google Scholar] [CrossRef]
- Shahidatul-Adha, M.; Zunaina, E.; Aini-Amalina, M.N. Evaluation of vascular endothelial growth factor (VEGF) level in the tears and serum of age-related macular degeneration patients. Sci. Rep. 2022, 12, 4423. [Google Scholar] [CrossRef]
- Spaide, R.F.; Jaffe, G.J.; Sarraf, D.; Freund, K.B.; Sadda, S.R.; Staurenghi, G.; Waheed, N.K.; FRCOphth, U.C.; Rosenfeld, P.J.; Holz, F.G.; et al. Consensus Nomenclature for Reporting Neovascular Age-Related Macular Degeneration Data: Consensus on Neovascular Age-Related Macular Degeneration Nomenclature Study Group. Ophthalmology 2020, 127, 616–636. [Google Scholar] [CrossRef]
- Ferris, F.L., 3rd; Wilkinson, C.P.; Bird, A.; Chakravarthy, U.; Chew, E.; Csaky, K.; Sadda, S.R. Clinical classification of age-related macular degeneration. Ophthalmology 2013, 120, 844–851. [Google Scholar] [CrossRef]
- Deak, G.; Gerendas, B.S.; Mylonas, G.; Weigert, G.; Michl, M.; Goldbach, F.; Leingang, O.; Steiner, I.; Schmidt-Erfurth, U. Concordance of OCT and FA-based MNV classifications in neovascular AMD and correlation with fluid volumes. Investig. Ophthalmol. Vis. Sci. 2023, 64, 288. [Google Scholar]
- Albert, M.S.; DeKosky, S.T.; Dickson, D.; Dubois, B.; Feldman, H.H.; Fox, N.C.; Gamst, A.; Holtzman, D.M.; Jagust, W.J.; Petersen, R.C.; et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer Dement. 2011, 7, 270–279. [Google Scholar] [CrossRef] [PubMed]
- Takei, A.; Ekström, M.; Mammadzada, P.; Aronsson, M.; Yu, M.; Kvanta, A.; André, H. Gene Transfer of Prolyl Hydroxylase Domain 2 Inhibits Hypoxia-inducible Angiogenesis in a Model of Choroidal Neovascularization. Sci. Rep. 2017, 7, srep42546. [Google Scholar] [CrossRef] [PubMed]
- André, H.; Tunik, S.; Aronsson, M.; Kvanta, A. Hypoxia-Inducible Factor-1α Is Associated With Sprouting Angiogenesis in the Murine Laser-Induced Choroidal Neovascularization Model. Investig. Opthalmol. Vis. Sci. 2015, 56, 6591–6604. [Google Scholar] [CrossRef] [PubMed]
- Shinomiya, K.; Ueta, M.; Kinoshita, S. A new dry eye mouse model produced by exorbital and intraorbital lacrimal gland excision. Sci. Rep. 2018, 8, 1483. [Google Scholar] [CrossRef]
- Finley, J.K.; Farmer, D.; Emmerson, E.; Pacheco, N.C.; Knox, S.M. Manipulating the Murine Lacrimal Gland. JoVE (J. Vis. Exp.) 2014, 93, e51970. [Google Scholar]

| Variable | Total Subjects (n = 50) | Active eAMD (n = 18) | Terminal eAMD (n = 11) | Control (n = 21) | p Value |
|---|---|---|---|---|---|
| Age (years) | |||||
| (Mean ± SD) | 73.5 ± 10.7 | 74.1 ± 9.2 | 81.9 ± 8.3 | 68.6 ± 10.3 | <0.001 a |
| Sex (n, %) | |||||
| Male | 24 (48) | 9 (50) | 7 (63) | 8 (38) | 0.38 b |
| Female | 26 (52) | 9 (50) | 4 (37) | 13 (62) | |
| Lifestyle (n, %) | |||||
| Cigarette smoking | 17 (34) | 8 (44) | 4 (37) | 5 (24) | 0.39 b |
| BMI (n, %) | |||||
| Overweight | 10 (20) | 3 (17) | 3 (27) | 4 (19) | 0.44 c |
| Obesity | 9 (18) | 4 (22) | 4 (37) | 1 (5) | |
| Family history of AMD (n, %) | 20 (40) | 9 (50) | 5 (45) | 6 (28) | 0.36 b |
| Comorbidity (n, %) | |||||
| HTN | 22 (44) | 10 (55) | 7 (63) | 5 (24) | 0.04 b |
| IHD | 8 (16) | 4 (22) | 2 (18) | 2 (9) | 0.61 c |
| Cataract surgery (n, %) | 19 (38) | 9 (50) | 6 (55) | 4 (19) | 0.06 b |
| Groups | Total | Male | Female | |||
|---|---|---|---|---|---|---|
| VEGF | Control | eAMD | Control | eAMD | Control | eAMD |
| Median (pg/mL) (95%, CI) | 36.46 (26.53–50.46) | 124.9 *** (115.3–255.9) | 40.06 (16.35–72.6) | 101.2 * (66.58–189.6) | 28.78 (21.97–47.62) | 166 *** (116.9–395.8) |
| Variable | Subgroups | Median Difference (pg/mL) (95%, CI) | p-Value |
|---|---|---|---|
| Sex | Female eAMD vs. Male eAMD | 85.67 (0.7163–284.5) | 0.04 |
| Male control vs. Female control | 11.29 (−14.30–37.80) | 0.64 | |
| VA of eAMD | VA ≥ 0.4 vs. VA < 0.4 | 12.27 (−101.2–120.2) | 0.74 |
| CFT of eAMD | CFT ≥ 250 vs. CFT < 250 | 7.61 (−52.95–126.9) | 0.35 |
| Intravitreal injection | Injection < 10 vs. Injection ≥ 10 | 45.65 (−50.76–277.6) | 0.45 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moshtaghion, S.M.M.; Locri, F.; Reyes, A.P.; Plastino, F.; Kvanta, A.; Morillo-Sanchez, M.J.; Rodríguez-de-la-Rúa, E.; Gutierrez-Sanchez, E.; Montero-Sánchez, A.; Lucena-Padros, H.; et al. VEGF in Tears as a Biomarker for Exudative Age-Related Macular Degeneration: Molecular Dynamics in a Mouse Model and Human Samples. Int. J. Mol. Sci. 2025, 26, 3855. https://doi.org/10.3390/ijms26083855
Moshtaghion SMM, Locri F, Reyes AP, Plastino F, Kvanta A, Morillo-Sanchez MJ, Rodríguez-de-la-Rúa E, Gutierrez-Sanchez E, Montero-Sánchez A, Lucena-Padros H, et al. VEGF in Tears as a Biomarker for Exudative Age-Related Macular Degeneration: Molecular Dynamics in a Mouse Model and Human Samples. International Journal of Molecular Sciences. 2025; 26(8):3855. https://doi.org/10.3390/ijms26083855
Chicago/Turabian StyleMoshtaghion, Seyed Mohamad Mehdi, Filippo Locri, Alvaro Plaza Reyes, Flavia Plastino, Anders Kvanta, Maria Jose Morillo-Sanchez, Enrique Rodríguez-de-la-Rúa, Estanislao Gutierrez-Sanchez, Adoración Montero-Sánchez, Helena Lucena-Padros, and et al. 2025. "VEGF in Tears as a Biomarker for Exudative Age-Related Macular Degeneration: Molecular Dynamics in a Mouse Model and Human Samples" International Journal of Molecular Sciences 26, no. 8: 3855. https://doi.org/10.3390/ijms26083855
APA StyleMoshtaghion, S. M. M., Locri, F., Reyes, A. P., Plastino, F., Kvanta, A., Morillo-Sanchez, M. J., Rodríguez-de-la-Rúa, E., Gutierrez-Sanchez, E., Montero-Sánchez, A., Lucena-Padros, H., André, H., & Díaz-Corrales, F. J. (2025). VEGF in Tears as a Biomarker for Exudative Age-Related Macular Degeneration: Molecular Dynamics in a Mouse Model and Human Samples. International Journal of Molecular Sciences, 26(8), 3855. https://doi.org/10.3390/ijms26083855








