Noncontact Detection of Respiration Rate Based on Forward Scatter Radar
Abstract
:1. Introduction
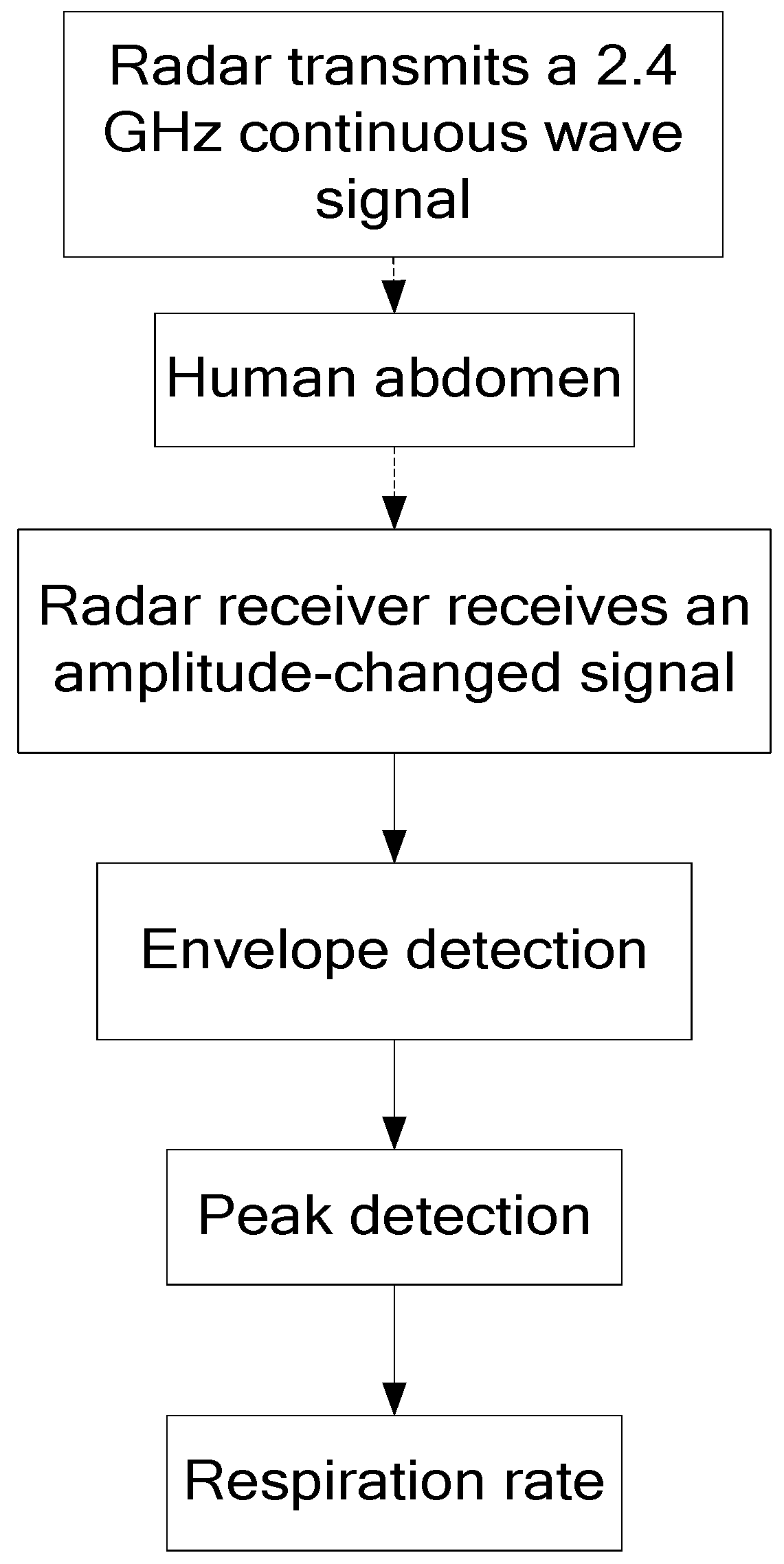
- Considering the disadvantage of traditional detection in that it relies on chest wall micromovement but is sensitive to random orientation of the human, a novel detection scheme based on human RCS changes is proposed. Respiration-based changes of RCS are analyzed. Then, the analytical expression of the received signals is derived.
- To confirm the theoretical model, we conducted the respiration detection experiments in an anechoic chamber with a forward scatter radar. Experimental results show that the respiratory rate is accurately detected by the proposed scheme.
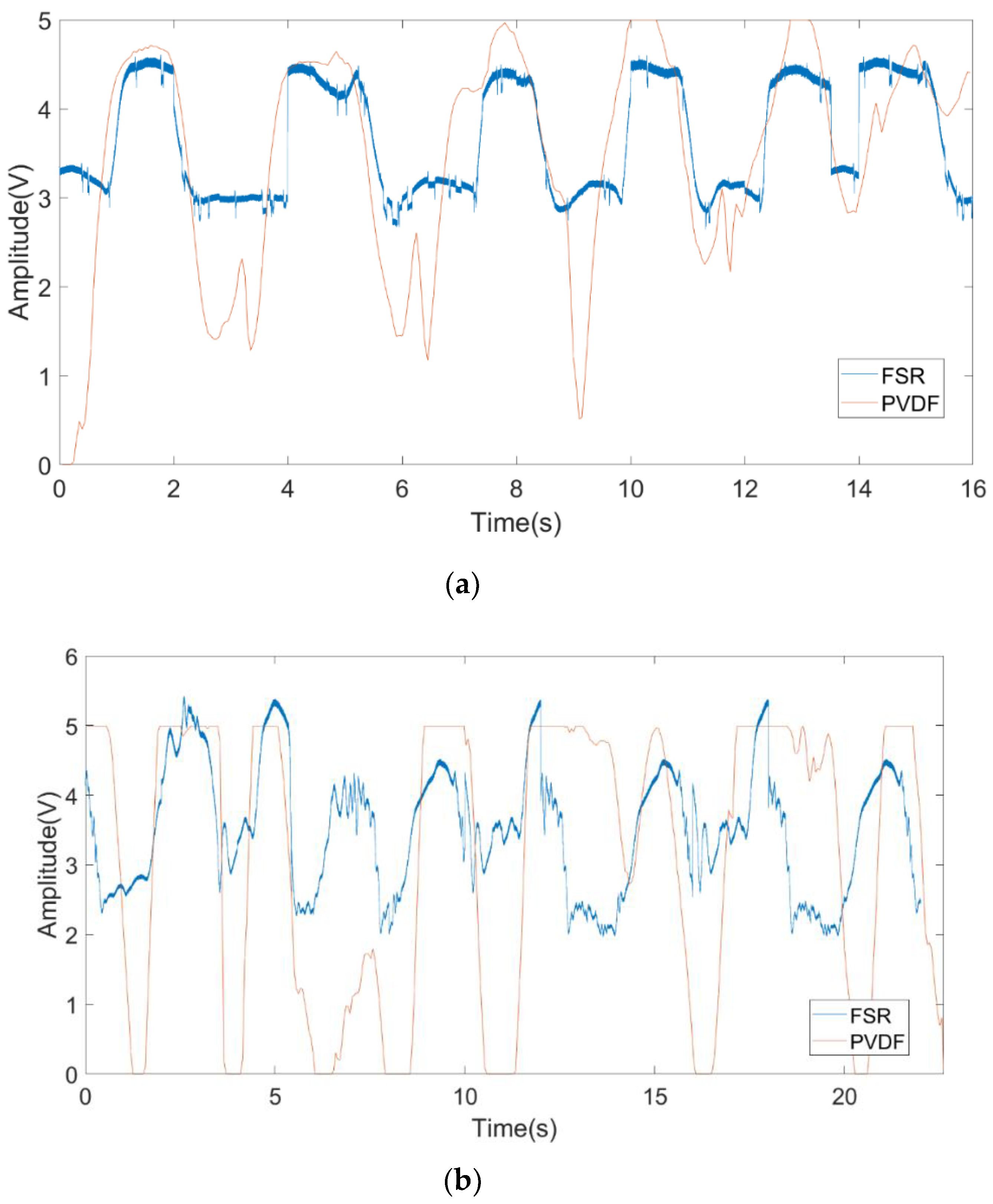
- To test the system’s performance in different orientations, the FSR system for calibration of the contact sensor was completed indoors. The verification results show that the system is insensitive to human rotation. The respiratory rate can still be measured with rotation of less than 90°. The reliability of the theoretical model is verified by the experimental data.
2. Theoretical Model
3. Experiments and Analysis
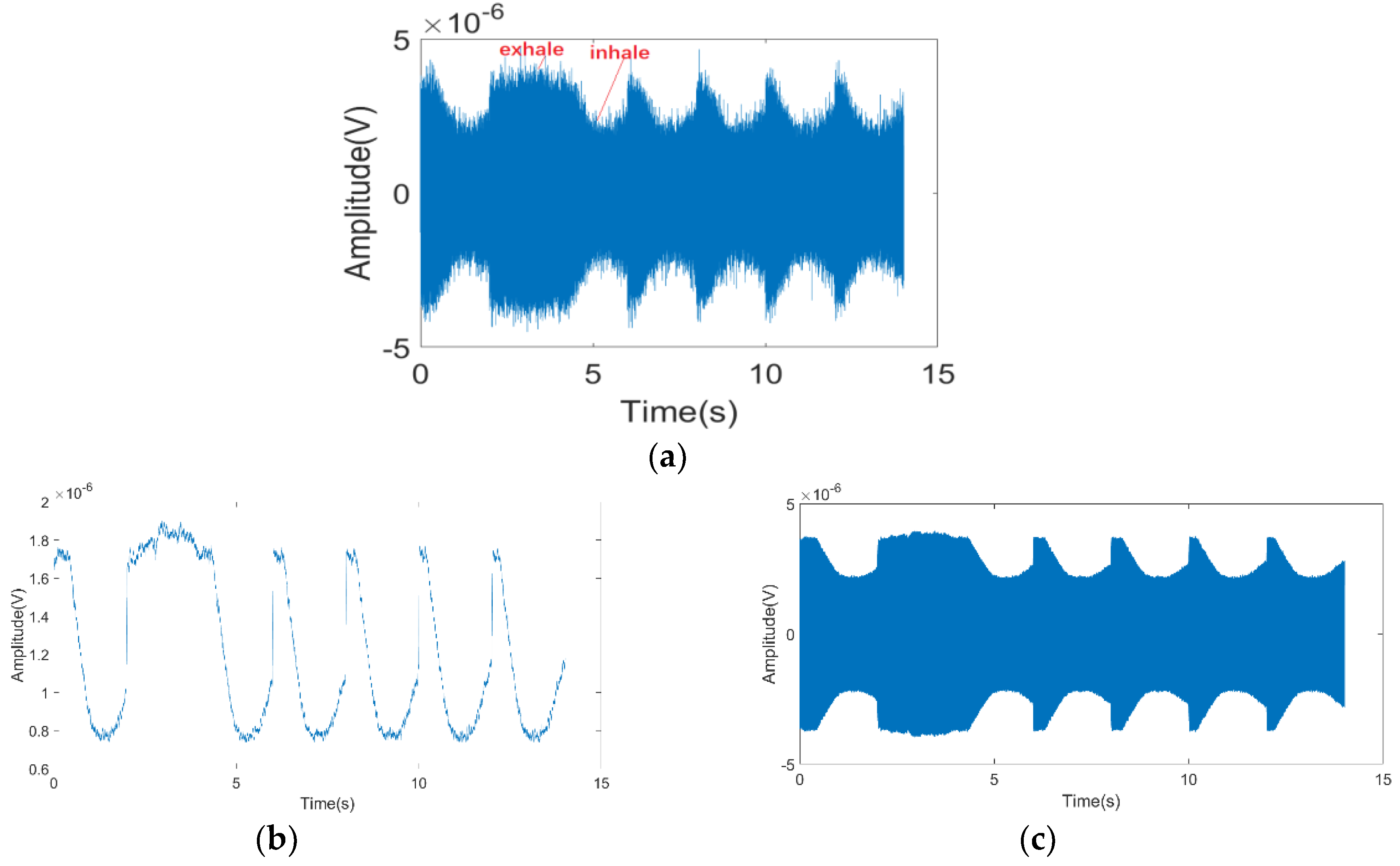
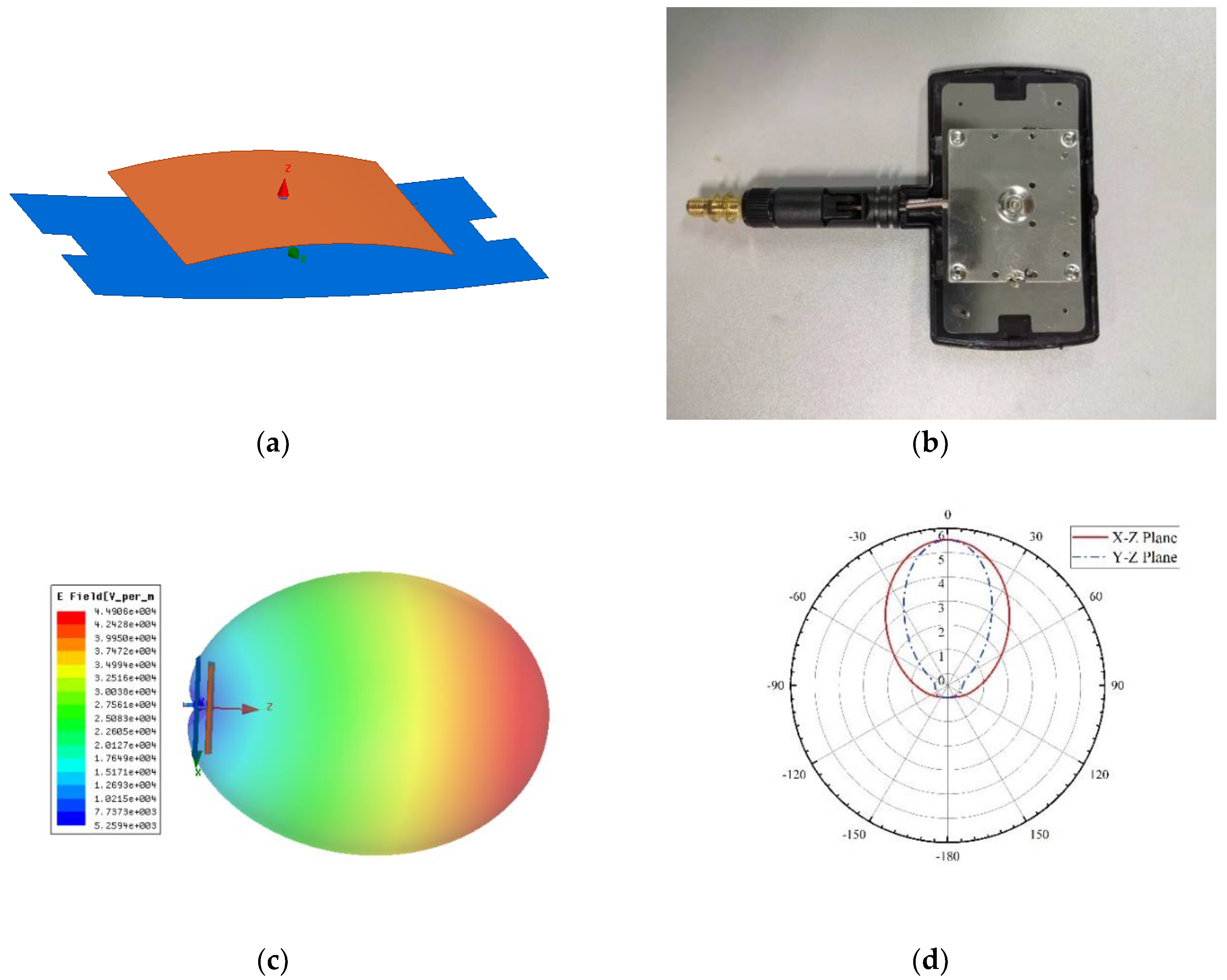
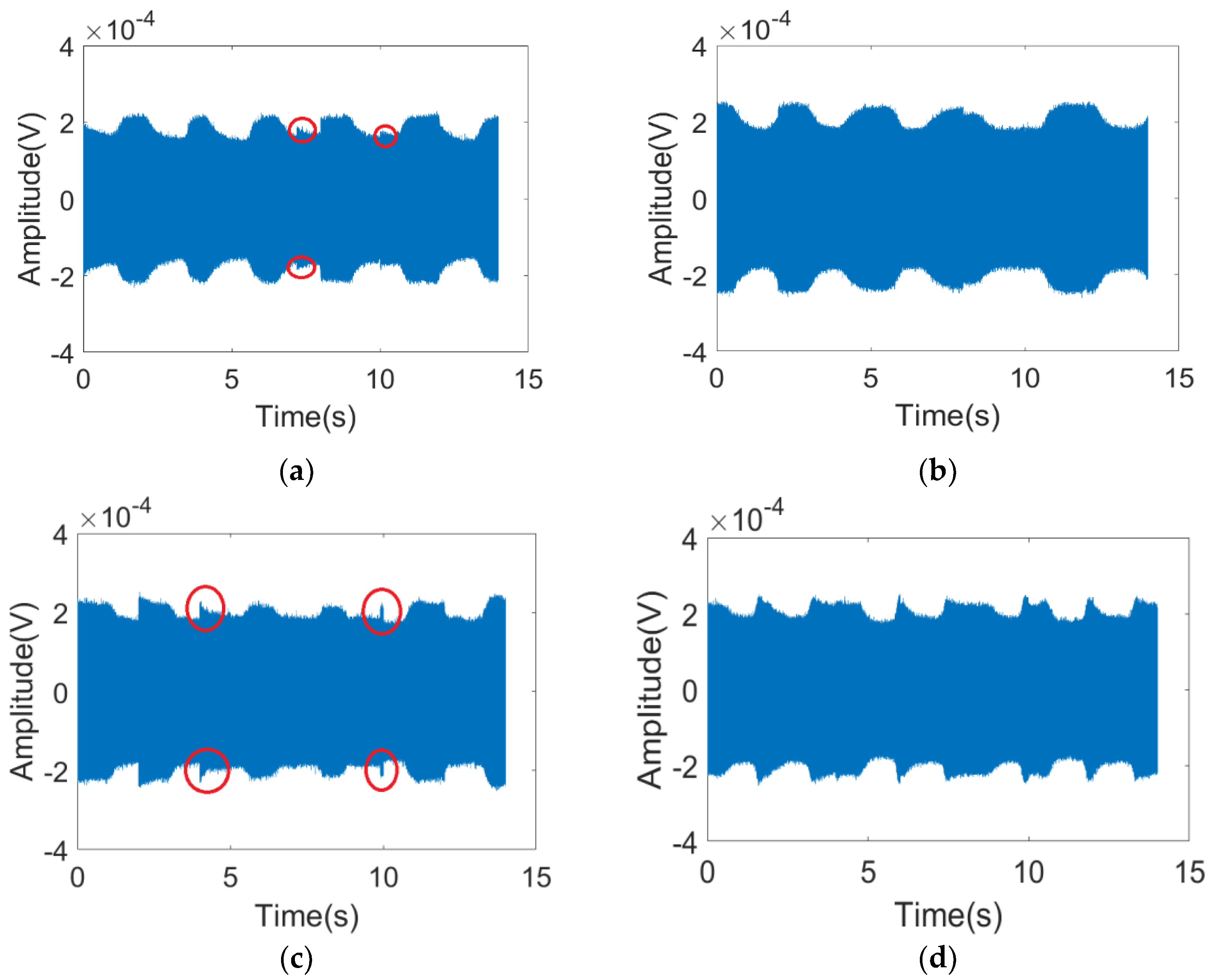
3.1. Experiment 1: Respiration Detection Testing in a Anechoic Chamber
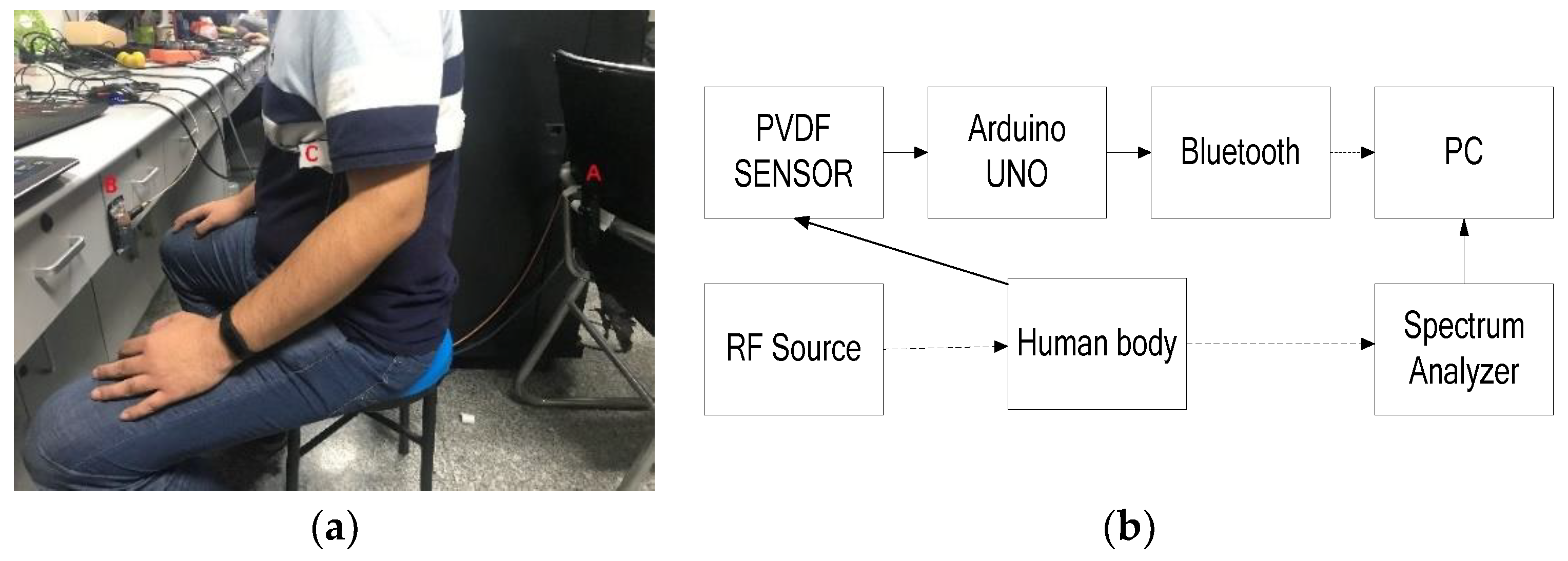
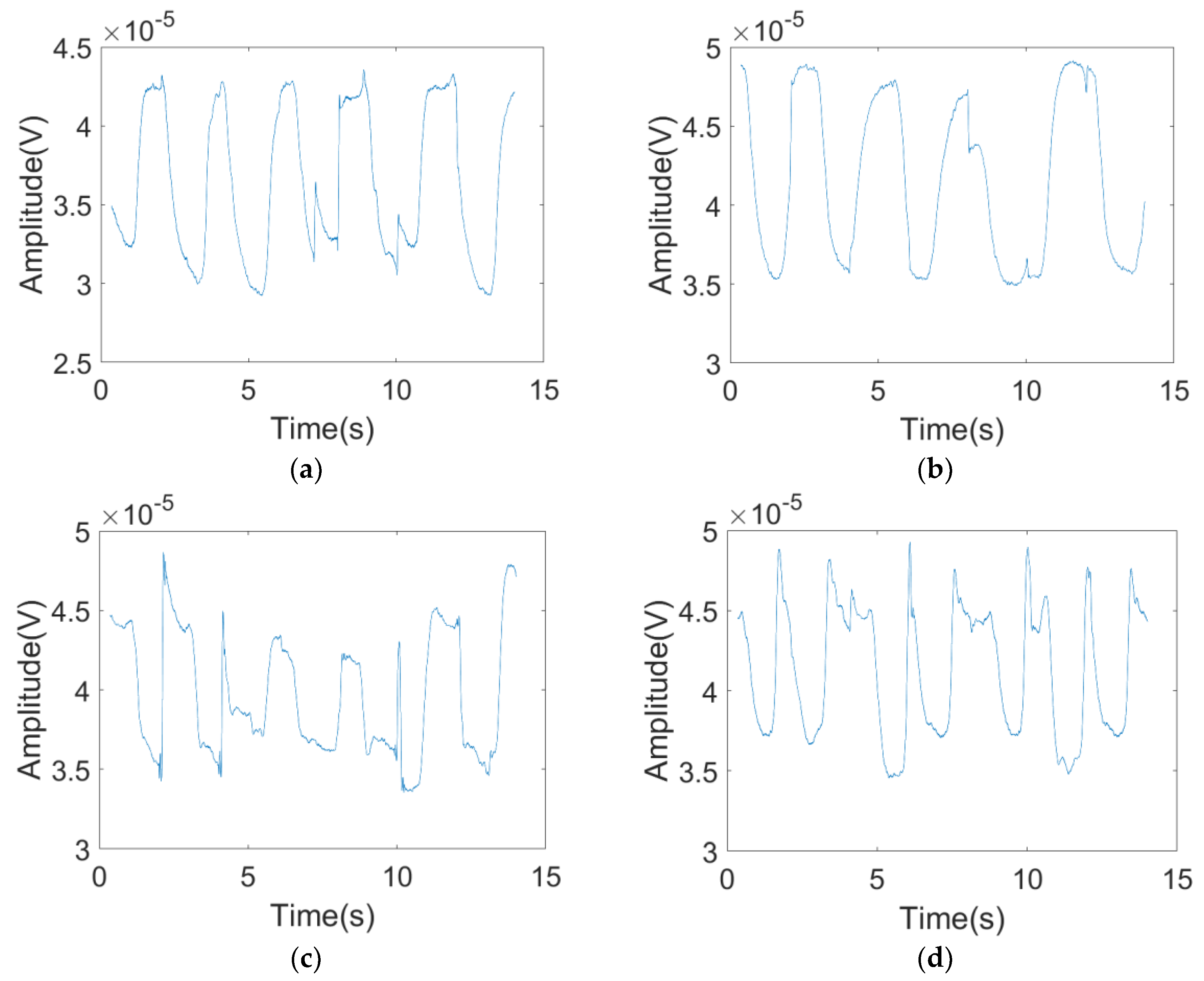
3.2. Experiment 2: Respiration Detection in a Common Room
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
Ethical Statements
References
- Khushaba, R.N.; Armitstead, J.; Schindhelm, K. Monitoring of nocturnal central sleep apnea in Heart failure patients using noncontact respiratory differences. In Proceedings of the 2017 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Seogwipo, Korea, 11–15 July 2017; pp. 1534–1538. [Google Scholar]
- Hafner, N.; Mostafanezhad, I.; Lubecke, V.M.; Boric-Lubecke, O.; Host-Madsen, A. Non-contact cardiopulmonary sensing with a baby monitor. In Proceedings of the 2007 29th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Lyon, France, 22–26 August 2007; pp. 2300–2302. [Google Scholar]
- Shyu, K.K.; Chiu, L.J.; Lee, P.L.; Tung, T.H.; Yang, S.H. Detection of Breathing and Heart Rates in UWB Radar Sensor Data Using FVPIEF-Based Two-Layer EEMD. IEEE Sens. J. 2019, 19, 774–784. [Google Scholar] [CrossRef]
- Yang, Z.; Xijing, J.; Teng, J.; Zhu, Z.; Hao, L.; Jianqi, W. Detecting and identifying two stationary-human-targets: A technique based on bioradar. In Proceedings of the First International Conference on Pervasive Computing, Signal Processing and Applications, Harbin, China, 17–19 September 2010; pp. 981–985. [Google Scholar]
- Chen, Y.; Gunawan, E.; Low, K.S.; Soh, C.B.; Thi, L.L. Human respiration rate estimation using body-worn ultra-wideband radar. In Proceedings of the 2007 IEEE Antennas and Propagation Society International Symposium, Honolulu, HI, USA, 9–15 June 2007; pp. 265–268. [Google Scholar]
- Leem, S.K.; Khan, F.; Cho, S.H. Vital Sign Monitoring and Mobile Phone Usage Detection Using IR-UWB Radar for Intended Use in Car Crash Prevention. Sensors 2017, 17, 1240. [Google Scholar] [CrossRef] [PubMed]
- Park, B.; Member, S.; Boric-lubecke, O.; Member, S.; Lubecke, V.M.; Member, S. Arctangent Demodulation With DC Offset Compensation in Quadrature Doppler Radar Receiver Systems. IEEE Trans. Microw. Theory Tech. 2007, 55, 1073–1079. [Google Scholar] [CrossRef]
- Li, C.; Lin, J. Random body movement cancellation in doppler radar vital sign detection. IEEE Trans. Microw. Theory Tech. 2008, 56, 3143–3152. [Google Scholar]
- Gu, C.; Long, J.; Huangfu, J.; Qiao, S.; Cui, W.Z.; Ma, W.; Ran, L. An instruments-built doppler radar for sensing vital signs. In Proceedings of the 2008 8th International Symposium on Antennas, Propagation and EM Theory, Kunming, China, 2–5 November 2008; pp. 1398–1401. [Google Scholar]
- Costanzo, S. Software-Defined Doppler Radar Sensor for Human Breathing Detection. Sensors 2019, 19, 3085. [Google Scholar] [CrossRef] [PubMed]
- Gouveia, C.; Vieira, J.; Pinho, P. A review on methods for random motion detection and compensation in bio-radar systems. Sensors 2019, 19, 604. [Google Scholar] [CrossRef] [PubMed]
- Raja Abdullah, R.; Ismail, A. Forward scattering radar: Current and future applications. Int. J. Eng. Technol. 2006, 3, 61–67. [Google Scholar]
- Raja Abdullah, R.S.A.; Rasid, M.F.A.; Mohamed, M.K. Improvement in detection with forward scattering radar. Sci. China Inf. Sci. 2011, 54, 2660–2672. [Google Scholar] [CrossRef] [Green Version]
- Chernyak Radar Cross Section (RCS) of Targets. Fundamentals of Multisite Radar Systems: Multistatic Radars and Multistatic Radar Systems, 1st ed.; Routledge: London, UK, 1998; pp. 32–36. [Google Scholar]
- Glaser, J.I. Bistatic RCS of complex Objects near Forward Scatter. IEEE Trans. Aerosp. Electron. Syst. 1985, AES-21, 70–78. [Google Scholar] [CrossRef]
- Silver, S. Scattering and diffraction. In Microwave Antenna Theory and Design, 1st ed.; Peter Peregrinus LTD: London, UK, 1984; pp. 139–160. [Google Scholar]
- Copper Antenna. Available online: https://www.anywlan.com/thread-108328-1-1.html (accessed on 14 November 2011).




| α | AMAX (μV) | AMIN (μV) | ξc |
|---|---|---|---|
| 0° | 227 | 144 | 87.34% |
| 30° | 255 | 180 | 87.9% |
| 60° | 240 | 170 | 88.8% |
| 90° | 240 | 175 | 89.6% |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, F.; He, Z.; Fu, Y.; Li, L.; Jiang, K.; Xie, F. Noncontact Detection of Respiration Rate Based on Forward Scatter Radar. Sensors 2019, 19, 4778. https://doi.org/10.3390/s19214778
Yang F, He Z, Fu Y, Li L, Jiang K, Xie F. Noncontact Detection of Respiration Rate Based on Forward Scatter Radar. Sensors. 2019; 19(21):4778. https://doi.org/10.3390/s19214778
Chicago/Turabian StyleYang, Fan, Zhiming He, Yuanhua Fu, Liang Li, Kui Jiang, and Fangyan Xie. 2019. "Noncontact Detection of Respiration Rate Based on Forward Scatter Radar" Sensors 19, no. 21: 4778. https://doi.org/10.3390/s19214778
APA StyleYang, F., He, Z., Fu, Y., Li, L., Jiang, K., & Xie, F. (2019). Noncontact Detection of Respiration Rate Based on Forward Scatter Radar. Sensors, 19(21), 4778. https://doi.org/10.3390/s19214778





