A Gesture-Controlled Rehabilitation Robot to Improve Engagement and Quantify Movement Performance
Abstract
:1. Introduction
2. Methods
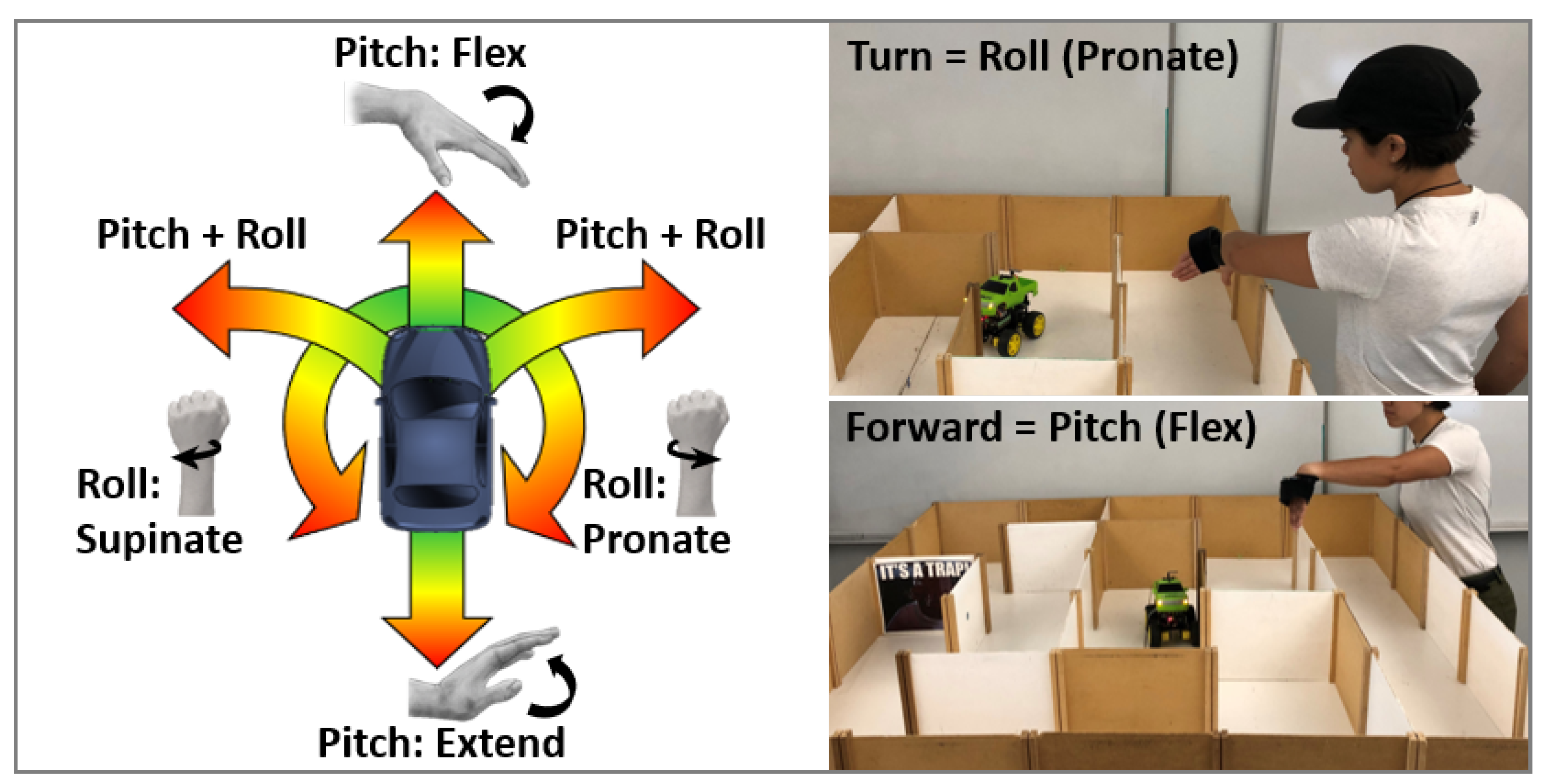
2.1. System Design
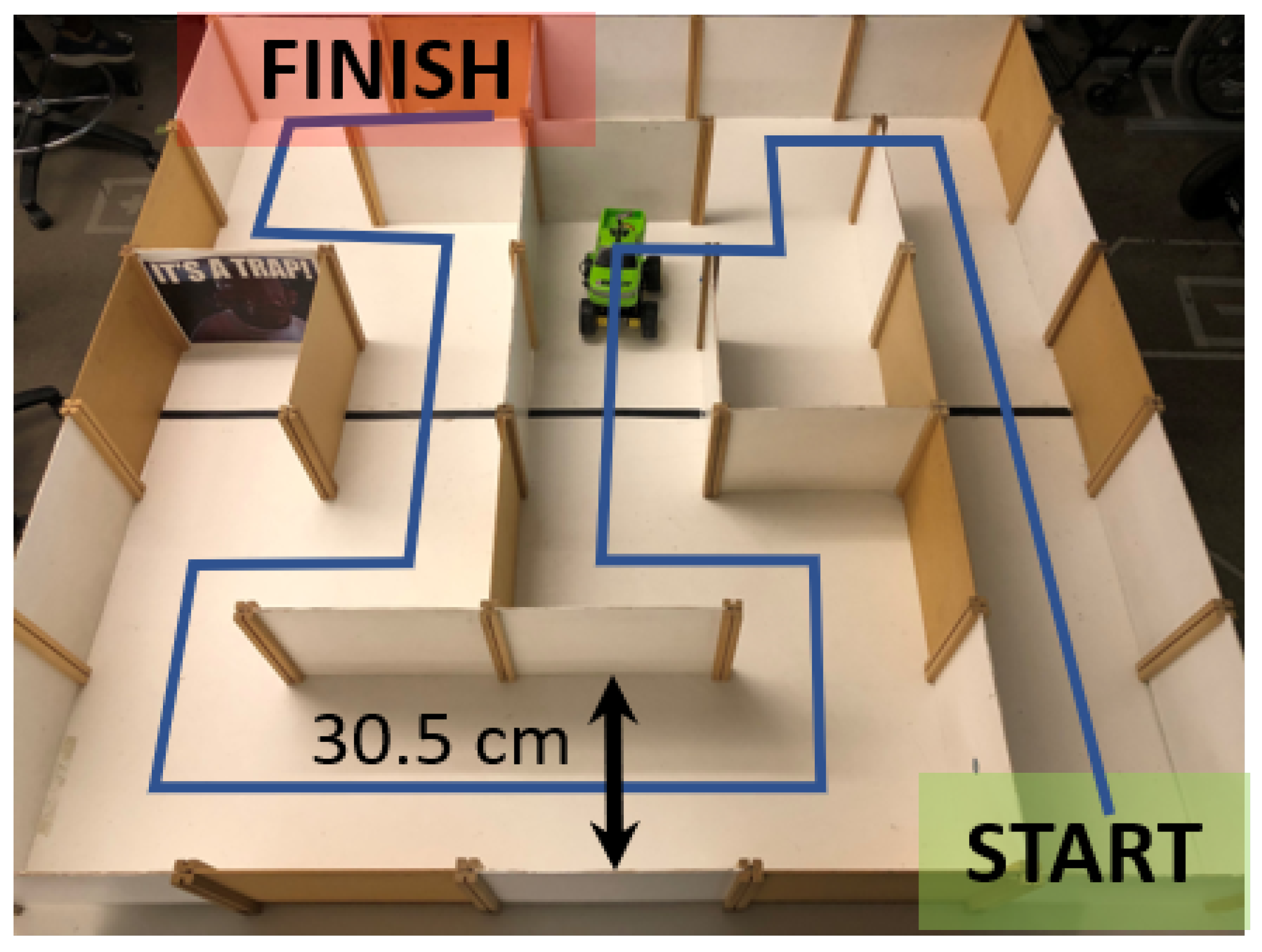
2.2. Human Subject Experiment
2.3. Questionnaires
2.4. Data Analysis
3. Results
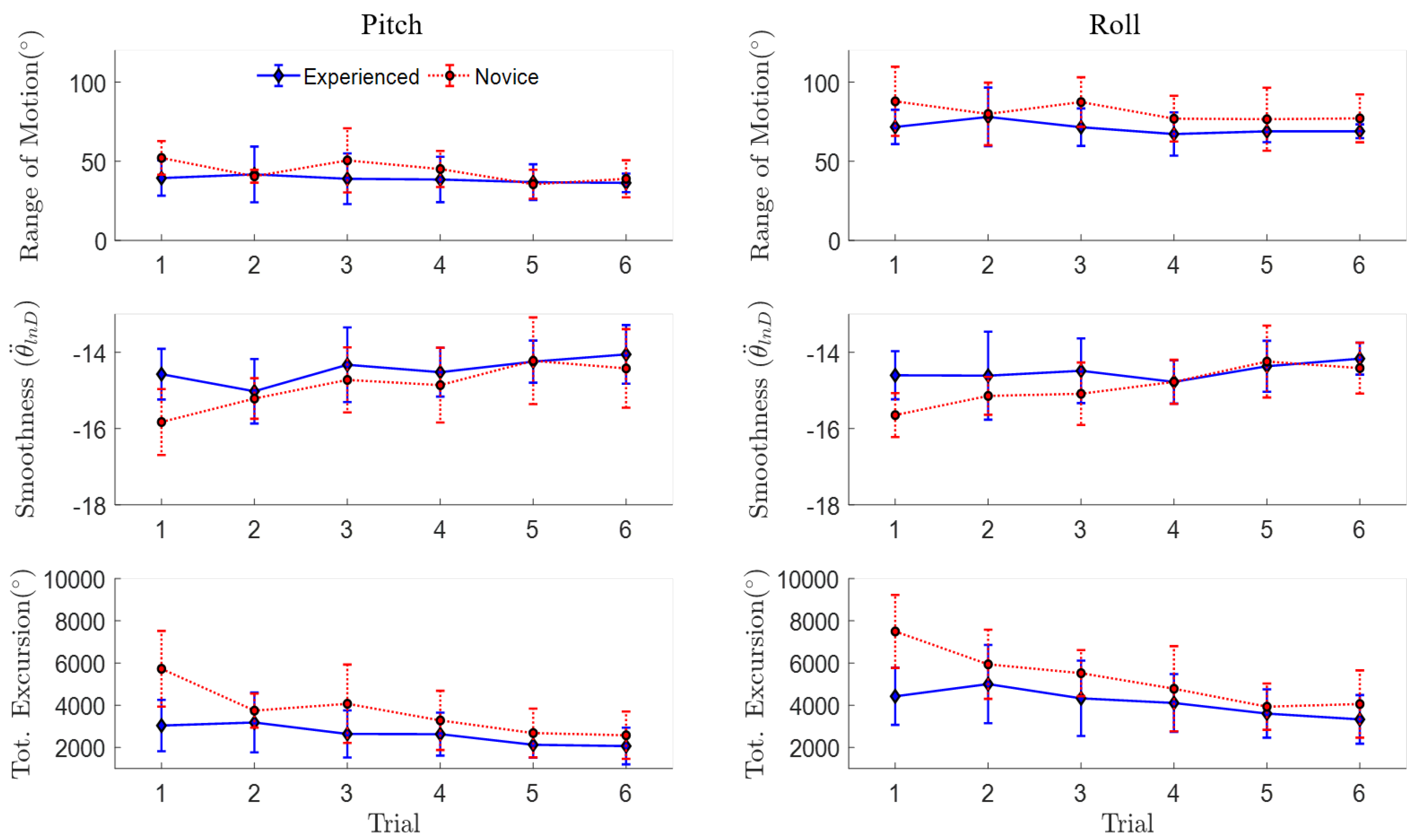
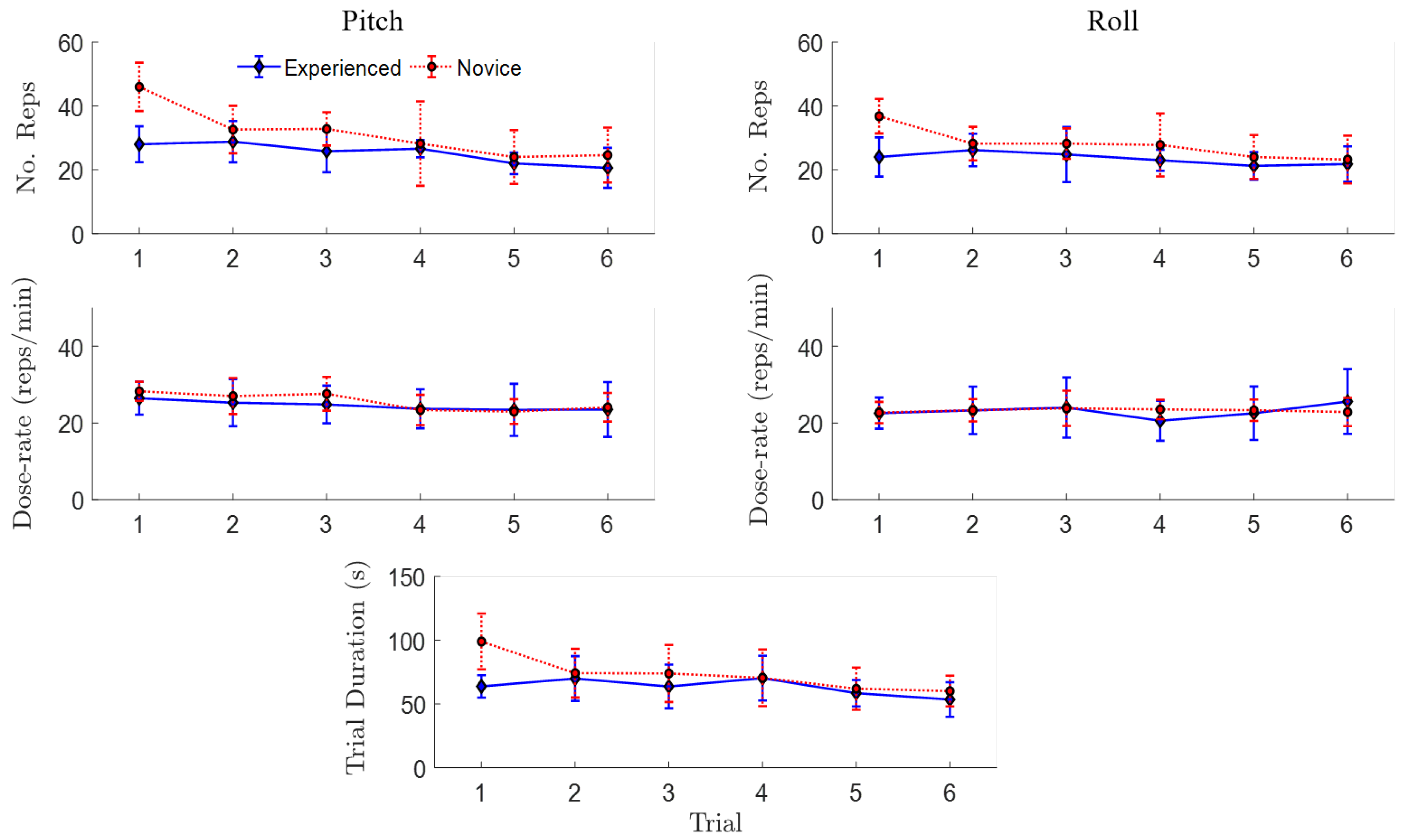
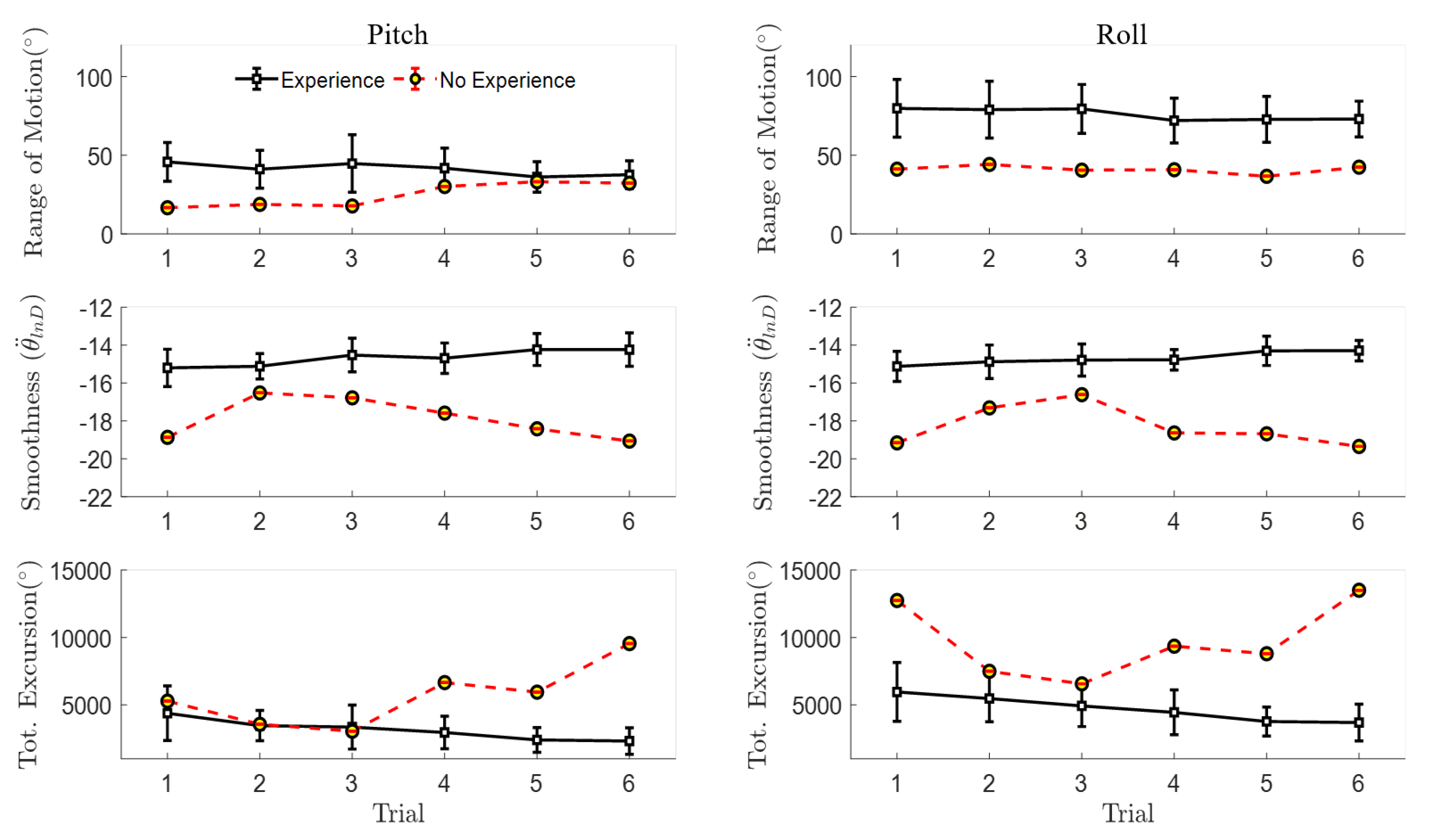
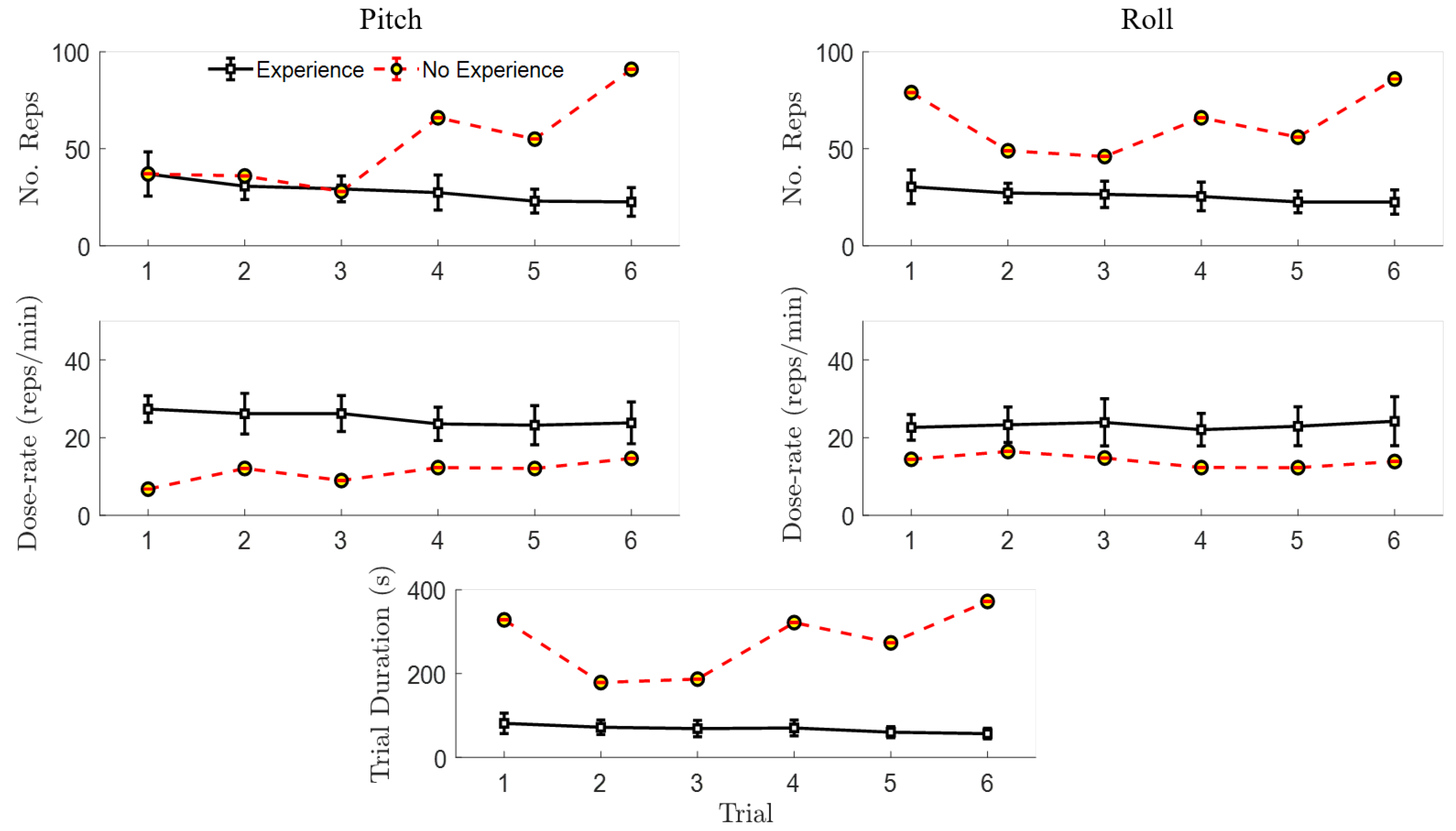
3.1. Quantitative Performance Metrics
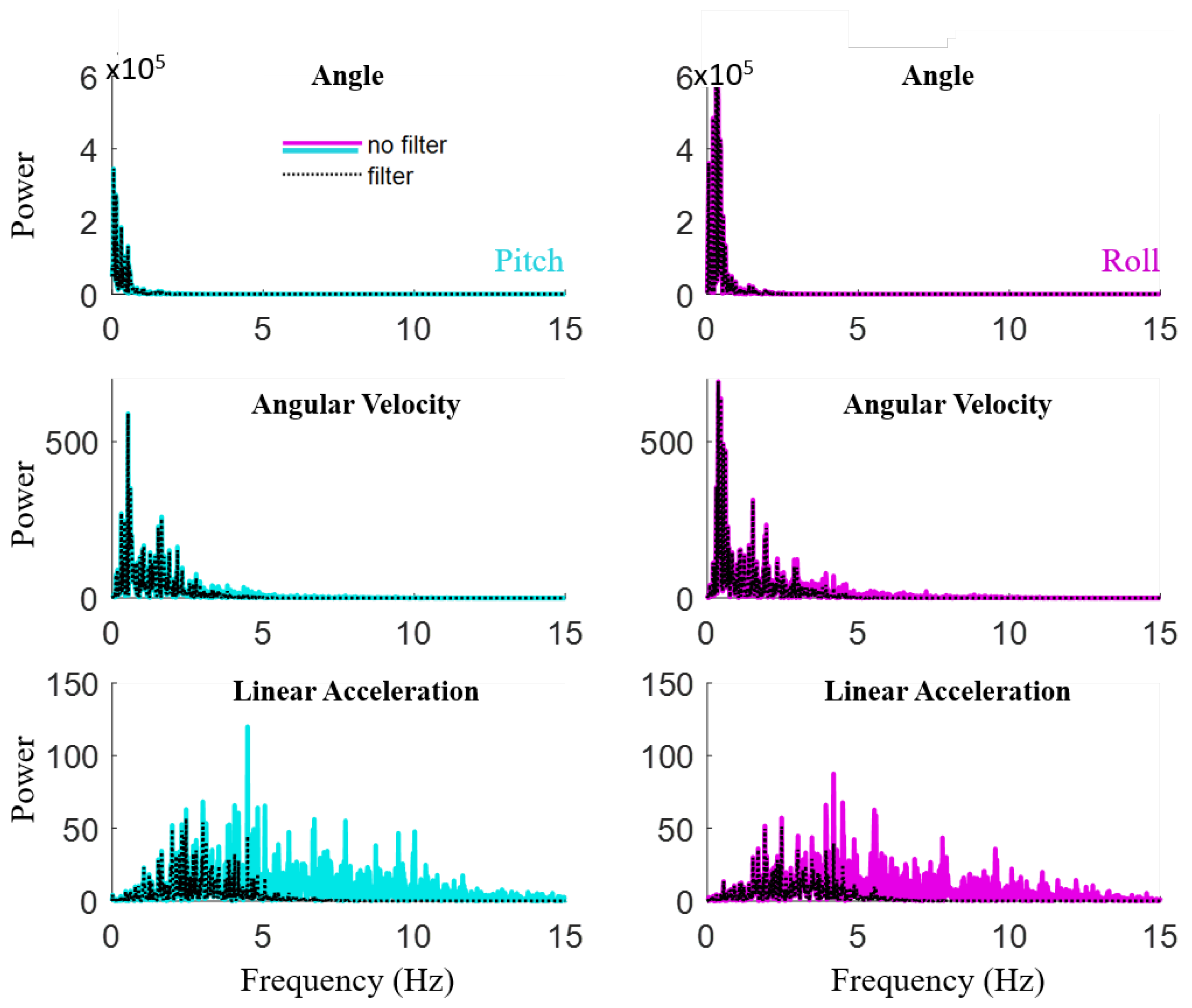
3.2. Signal Processing
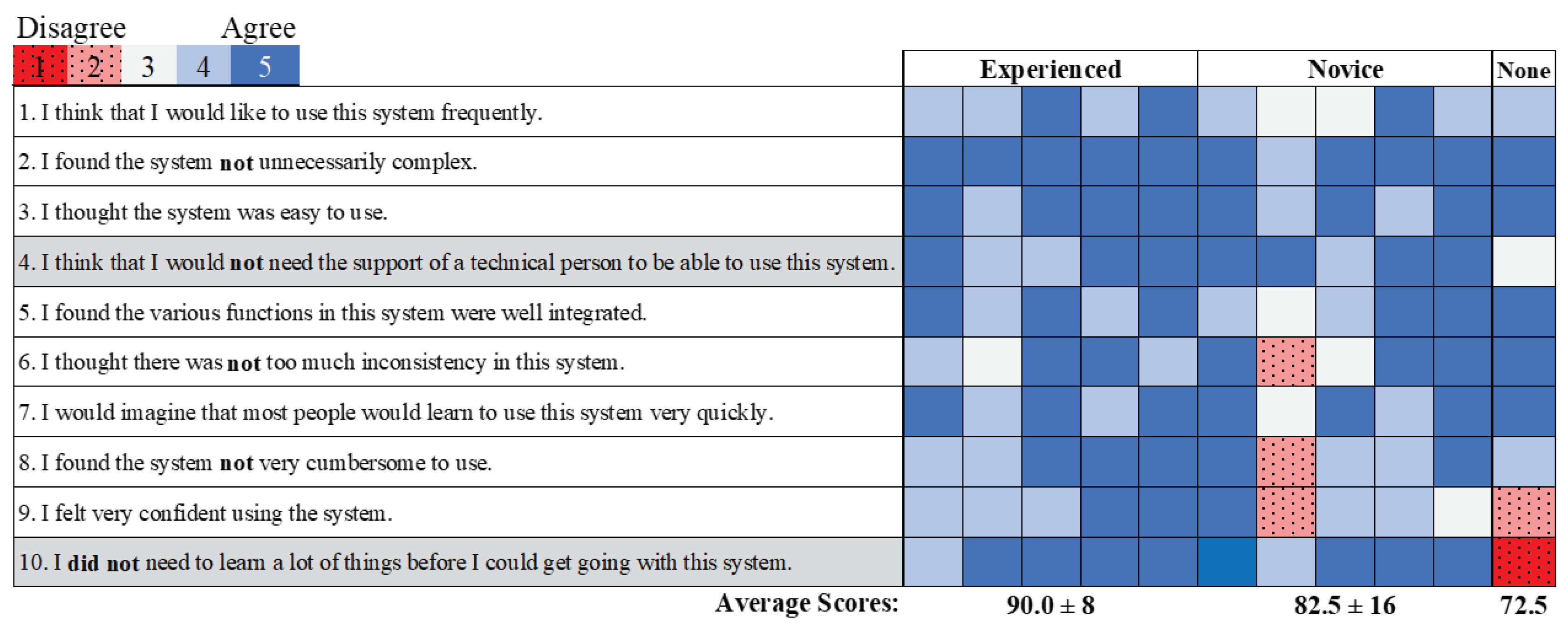
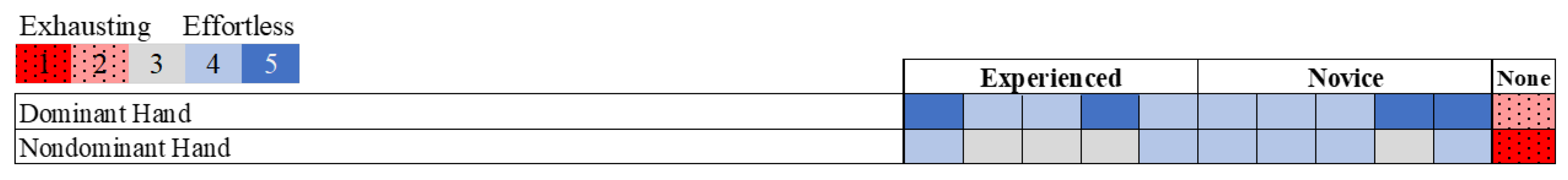
3.3. Surveys
4. Discussion
4.1. Quantified Performance
4.2. Skill-Based Motor Learning
4.3. Engagement: Usability and Effort
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Pomeroy, V.; Aglioti, S.M.; Mark, V.W.; McFarland, D.; Stinear, C.; Wolf, S.L.; Corbetta, M.; Fitzpatrick, S.M. Neurological principles and rehabilitation of action disorders: Rehabilitation interventions. Neurorehabil. Neural Repair 2011, 25, 33S–43S. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taylor, A.H.; May, S. Threat and coping appraisal as determinants of compliance with sports injury rehabilitation: An application of Protection Motivation Theory. J. Sport. Sci. 1996, 14, 471–482. [Google Scholar] [CrossRef]
- Sluijs, E.M.; Knibbe, J.J. Patient compliance with exercise: Different theoretical approaches to short-term and long-term compliance. Patient Educ. Couns. 1991, 17, 191–204. [Google Scholar] [CrossRef] [Green Version]
- Lang, C.E.; MacDonald, J.R.; Reisman, D.S.; Boyd, L.; Kimberley, T.J.; Schindler-Ivens, S.M.; Hornby, T.G.; Ross, S.A.; Scheets, P.L. Observation of amounts of movement practice provided during stroke rehabilitation. Arch. Phys. Med. Rehabil. 2009, 90, 1692–1698. [Google Scholar] [CrossRef] [Green Version]
- Levin, M.F.; Weiss, P.L.; Keshner, E.A. Emergence of virtual reality as a tool for upper limb rehabilitation: Incorporation of motor control and motor learning principles. Phys. Ther. 2015, 95, 415–425. [Google Scholar] [CrossRef] [Green Version]
- Broeks, J.G.; Lankhorst, G.J.; Rumping, K.; Prevo, A.J.H. The long-term outcome of arm function after stroke: Results of a follow-up study. Disabil. Rehabil. 1999, 21, 357–364. [Google Scholar] [CrossRef]
- Yue, Z.; Zhang, X.; Wang, J. Hand rehabilitation robotics on poststroke motor recovery. Behav. Neurol. 2017, 2017, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Duncan, P.W.; Horner, R.D.; Reker, D.M.; Samsa, G.P.; Hoenig, H.; Hamilton, B.; LaClair, B.J.; Dudley, T.K. Adherence to postacute rehabilitation guidelines is associated with functional recovery in stroke. Stroke 2002, 33, 167–178. [Google Scholar] [CrossRef] [PubMed]
- Timmermans, A.A.; Seelen, H.A.; Willmann, R.D.; Kingma, H. Technology-assisted training of arm-hand skills in stroke: Concepts on reacquisition of motor control and therapist guidelines for rehabilitation technology design. J. Neuroeng. Rehabil. 2009, 6, 1–18. [Google Scholar] [CrossRef] [Green Version]
- Lohse, K.; Shirzad, N.; Verster, A.; Hodges, N.; Van der Loos, M. Video games and rehabilitation: Using design principles to enhance engagement in physical therapy. J. Neurol. Phys. Ther. 2013, 37, 166–175. [Google Scholar] [CrossRef]
- Zollo, L.; Rossini, L.; Bravi, M.; Magrone, G.; Sterzi, S.; Guglielmelli, E. Quantitative evaluation of upper-limb motor control in robot-aided rehabilitation. Med. Biolog. Eng. Comp. 2011, 49, 1131–1144. [Google Scholar] [CrossRef] [PubMed]
- Graves, L.E.; Ridgers, N.D.; Williams, K.; Stratton, G.; Atkinson, G.; Cable, N.T. The physiological cost and enjoyment of Wii Fit in adolescents, young adults, and older adults. J. Phys. Act. Health 2010, 7, 393–401. [Google Scholar] [CrossRef] [PubMed]
- Segal, A.D.; Lesak, M.C.; Suttora, N.E.; Silverman, A.K.; Petruska, A.J. iRebot: An interactive rehabilitation robot with gesture control. In Proceedings of the IEEE International Confrence Engineering in Medicine and Biology Society (EMBC), Montreal, QC, Canada, 20–24 July 2020; pp. 1–4. [Google Scholar]
- Timmermans, A.A.A.; Seelen, H.A.M.; Geers, R.P.J.; Saini, P.K.; Winter, S.; te Vrugt, J.; Kingma, H. Sensor-based arm skill training in chronic stroke patients: Results on treatment outcome, patient motivation, and system usability. IEEE Trans. Neural. Sys. Rehabil. Eng. 2010, 18, 284–292. [Google Scholar] [CrossRef] [PubMed]
- Brutsch, K.; Koenig, A.; Zimmerli, L.; Merillat-Koeneke, S.; Riener, R.; Jancke, L.; van Hedel, H.J.A.; Meyer-Heim, A. Virtual reality for enhancement of robot-assisted gait training in children with neurological gait disorders. J. Rehabil. Med. 2011, 43, 493–499. [Google Scholar] [CrossRef] [Green Version]
- Prahm, C.; Kayali, F.; Vujaklija, I.; Sturma, A.; Aszmann, O. Increasing motivation, effort and performance through game-based rehabilitation for upper limb myoelectric prosthesis control. In Proceedings of the 2017 International Conference on Virtual Rehabilitation (ICVR), Montreal, QC, Canada, 19–22 June 2017; pp. 1–6. [Google Scholar]
- Warraich, Z.; Kleim, J.A. Neural plasticity: The biological substrate for neurorehabilitation. PM&R 2010, 2, S208–S219. [Google Scholar]
- Sathiyanarayanan, M.; Azharuddin, S.; Kumar, S.; Khan, G. Gesture controlled robot for military Purpose. Int. J. Technol. Res. Eng. 2014, 1, 1300–1303. [Google Scholar]
- Nemec, D.; Janota, A.; Gregor, M.; Hruboš, M.; Pirník, R. Control of the mobile robot by hand movement measured by inertial sensors. Electr. Eng. 2017, 99, 1161–1168. [Google Scholar] [CrossRef]
- Wolf, M.T.; Assad, C.; Vernacchia, M.T.; Fromm, J.; Jethani, H.L. Gesture-based robot control with variable autonomy from the JPL BioSleeve. In Proceedings of the 2013 IEEE International Conference on Robotics and Automation, Karlsruhe, Germany, 6–10 May 2013; pp. 1160–1165. [Google Scholar]
- Wen, R.; Tay, W.L.; Nguyen, B.P.; Chng, C.B.; Chui, C.K. Hand gesture guided robot-assisted surgery based on a direct augmented reality interface. Comp. Meth. Prog. Biomed. 2014, 116, 68–80. [Google Scholar] [CrossRef]
- Yang, G.; Lv, H.; Chen, F.; Pang, Z.; Wang, J.; Yang, H.; Zhang, J. A novel gesture recognition system for intelligent interaction with a nursing-care assistant robot. Appl. Sci. 2018, 8, 2349. [Google Scholar] [CrossRef] [Green Version]
- Balasubramanian, S.; Colombo, R.; Sterpi, I.; Sanguineti, V.; Burdet, E. Robotic assessment of upper limb motor function after stroke. Am. J. Phys. Med. Rehabil. 2012, 91, S255–S269. [Google Scholar] [CrossRef]
- Standen, P.J.; Threapleton, K.; Connell, L.; Richardson, A.; Brown, D.J.; Battersby, S.; Sutton, C.J.; Platts, F. Patients’ use of a home-based virtual reality system to provide rehabilitation of the upper limb following stroke. Phys. Ther. 2015, 95, 350–359. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Semprini, M.; Laffranchi, M.; Sanguineti, V.; Avanzino, L.; De Icco, R.; De Michieli, L.; Chiappalone, M. Technological approaches for neurorehabilitation: From robotic devices to brain stimulation and beyond. Front. Neurol. 2018, 9, 212. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barlett, N.D.; Gentile, D.A.; Barlett, C.P.; Eisenmann, J.C.; Walsh, D.A. Sleep as a mediator of screen time effects on US children’s health outcomes: A prospective study. J. Child. Media 2012, 6, 37–50. [Google Scholar] [CrossRef]
- Lissak, G. Adverse physiological and psychological effects of screen time on children and adolescents: Literature review and case study. Environ. Res. 2018, 164, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Guadagnoli, M.A.; Lee, T.D. Challenge point: A framework for conceptualizing the effects of various practice conditions in motor learning. J. Mot. Behav. 2004, 36, 212–224. [Google Scholar] [CrossRef] [PubMed]
- Paulich, M.; Schepers, M.; Rudigkeit, N.; Bellusci, G. Xsens MTw Awinda: Miniature Wireless Inertial-Magnetic Motion Tracker for Highly Accurate 3D Kinematic Applications; Xsens: Enschede, The Netherlands, 2018; pp. 1–9. [Google Scholar]
- Snoddy, G.S. Learning and stability: A psychophysiological analysis of a case of motor learning with clinical applications. J. App. Psyc. 1926, 10, 1. [Google Scholar] [CrossRef]
- Renewal Lodge.com. Available online: https://www.renewallodge.com/5-ways-quitting-drinking-affects-your-brain/ (accessed on 21 June 2020).
- Brooke, J. SUS: A Quick and Dirty usability scale. Usability Eval. Ind. 1996, 189, 4–7. [Google Scholar]
- Likert, R. A technique for the measurement of attitudes. Arch. Psychol. 1932, 140, 1–55. [Google Scholar]
- Balasubramanian, S.; Melendez-Calderon, A.; Burdet, E. A robust and sensitive metric for quantifying movement smoothness. IEEE Trans. Biomed. Eng. 2012, 59, 2126–2136. [Google Scholar] [CrossRef]
- Flash, T.; Hogan, N. The coordination of arm movements: An experimentally confirmed mathematical model. J. Neurosci. 1985, 5, 1688–1703. [Google Scholar] [CrossRef]
- Rodgers, J.L.; Nicewander, W.A. Thirteen ways to look at the correlation coefficient. Am. Stat. 1988, 42, 59–66. [Google Scholar] [CrossRef]
- Taylor, R. Interpretation of the correlation coefficient: A basic review. J. Diagnos. Med. Sonogr. 1990, 6, 35–39. [Google Scholar] [CrossRef]
- Brooke, J. SUS: A Retrospective. J. Usability Stud. 2013, 8, 29–40. [Google Scholar]
- Lewis, J.R.; Sauro, J. The factor structure of the System Usability Scale. In International Conference on Human Centered Design; Human Centered Design. HCD 2009. Lecture Notes in Computer Science; Kurosu, M., Ed.; Springer: Berlin/Heidelberg, Germany, 2009; Volume 5619, pp. 94–103. [Google Scholar]
- Borsci, S.; Federici, S.; Lauriola, M. On the dimensionality of the System Usability Scale: A test of alternative measurement models. Cog. Process. 2009, 10, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Birkenmeier, R.L.; Prager, E.M.; Lang, C.E. Translating animal doses of task-specific training to people with chronic stroke in 1-hour therapy sessions: A proof-of-concept study. Neurorehabil. Neural Rep. 2010, 24, 620–635. [Google Scholar] [CrossRef] [PubMed]
- Colombo, R.; Pisano, F.; Micera, S.; Mazzone, A.; Delconte, C.; Carrozza, M.C.; Dario, P.; Minuco, G. Robotic techniques for upper limb evaluation and rehabilitation of stroke patients. IEEE Trans. Neural Sys. Rehabil. Eng. 2005, 13, 311–324. [Google Scholar] [CrossRef]
- Chen, Y.; Duff, M.; Lehrer, N.; Sundaram, H.; He, J.; Wolf, S.L.; Rikakis, T. A computational framework for quantitative evaluation of movement during rehabilitation. AIP Conf. Proc. Am. Inst. Phys 2011, 1371, 317–326. [Google Scholar]
- Charles, S.K.; Hogan, N. The curvature and variability of wrist and arm movements. Exp. Brain Res. 2010, 203, 63–73. [Google Scholar] [CrossRef]
- Brewer, B.R.; McDowell, S.K.; Worthen-Chaudhari, L.C. Poststroke upper extremity rehabilitation: A review of robotic systems and clinical results. Top. Stroke Rehabil. 2007, 14, 22–44. [Google Scholar] [CrossRef]
- Wulf, G. Self-controlled practice enhances motor learning: Implications for physiotherapy. Physiotherapy 2007, 93, 96–101. [Google Scholar] [CrossRef]
- Snodgrass, S.J.; Rivett, D.A.; Robertson, V.J.; Stojanovski, E. Real-time feedback improves accuracy of manually applied forces during cervical spine mobilisation. Man. Ther. 2010, 15, 19–25. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, A.; Gandy, M.; Allaire, J.; Whitlock, L. Putting fun into video games for older adults. Ergon. Des. 2012, 20, 13–22. [Google Scholar] [CrossRef]
- Feys, H.M.; De Weerdt, W.J.; Selz, B.E.; Cox Steck, G.A.; Spichiger, R.; Vereeck, L.E.; Putman, K.D.; Van Hoydonck, G.A. Effect of a therapeutic intervention for the hemiplegic upper limb in the acute phase after stroke: A single-blind, randomized, controlled multicenter trial. Stroke 1998, 29, 785–792. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.Y.; Chen, C.l.; Tang, S.F.; Lin, K.C.; Huang, Y.Y. Kinematic and clinical analyses of upper-extremity movements after constraint-induced movement therapy in patients with stroke: A randomized controlled trial. Arch. Phys. Med. Rehabil. 2007, 88, 964–970. [Google Scholar] [CrossRef] [PubMed]
- Sigrist, R.; Rauter, G.; Riener, R.; Wolf, P. Augmented visual, auditory, haptic, and multimodal feedback in motor learning: A review. Psychon. Bull. Rev. 2013, 20, 21–53. [Google Scholar] [CrossRef] [Green Version]
- Patel, K.; Bailenson, J.N.; Hack-Jung, S.; Diankov, R.; Bajcsy, R. The effects of fully immersive virtual reality on the learning of physical tasks. In Proceedings of the 9th Annual International Workshop on Presence, Cleveland, OH, USA, 24–26 August 2006; pp. 87–94. [Google Scholar]
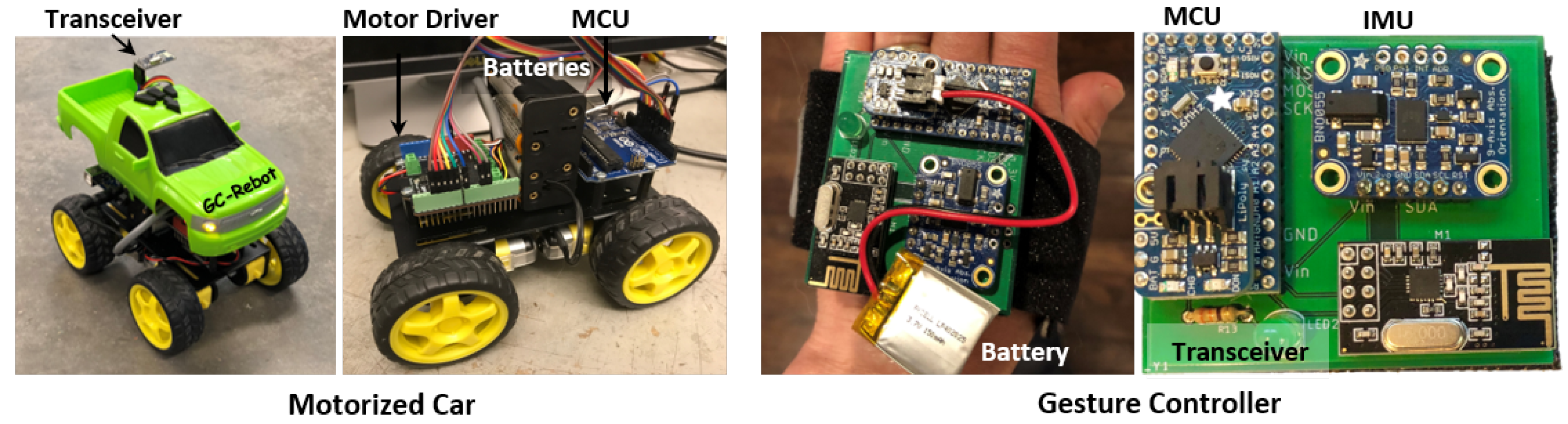




| Part Type | Description | Details |
|---|---|---|
| Gesture Controller | Total Cost: $60 | |
| IMU | Adafruit BNO055 9-DOF | 5 V, 16 MHz |
| MCU | Adafruit ItsyBitsy (Atmega32u4) | 5 V, 16 MHz |
| Transceiver | NRF24L01 wireless module | 1.9–3.6 V, 2.4 GHz |
| Battery | Adafruit lithium ion polymer | 3.7 V, 150 mA |
| Motorized Car | Total cost: $75 | |
| Car Platform | SZDOIT Smart Robot Car Kit | 2 mm alum.panel |
| Motors | 4 TT DC Gearbox Motors (1:48) | 4.5 V, 200 RPM |
| Motor Driver | Quad DC motor driver shield | SKU:DRI0039 |
| MCU | Arduino Uno R3 (ATmega328P) | 5 V, 16 MHz |
| Transceiver | NRF24L01 wireless module | 1.9–3.6 V, 2.4 GHz |
| Metric | Mean ± SD | Nov | %Diff | Exp | %Diff | p-Value | |
|---|---|---|---|---|---|---|---|
| Active Range of Motion (°) | 41.6 ± 13 | −11.8 | −28% | −1.3 | −3.1% | 0.3 | |
| 76.8 ± 16 | −12.9 | −17% | −3.4 | −4.4% | 0.2 | ||
| Smoothness () | −14.1 ± 0.9 | 1.8 | 13% | 0.80 | 5.7% | 0.04 | |
| −14.1 ± 0.7 | 1.4 | 10% | 0.99 | 7.0% | 0.4 | ||
| Total Ang. Excursion: (°) | 3150 ± 1490 | −3170 | −101% | −967 | −31% | 0.03 | |
| 4710 ± 1770 | −3440 | −73% | −1090 | −23% | 0.01 |
| Metric | Mean ± SD | Nov | %Diff | Exp | %Diff | p-Value | |
|---|---|---|---|---|---|---|---|
| Number of Repetitions | 28.5 ± 9 | −20.8 | −73% | −7.4 | −26% | 0.04 | |
| 25.8 ± 7 | −13.4 | −52% | −2.0 | −7.8% | 0.02 | ||
| Dose-rate (reps/min) | 25.1 ± 5 | −3.8 | −15% | −2.7 | −11% | 0.9 | |
| 23.2 ± 5 | 0.25 | 1.1% | 3.2 | 14% | 0.4 | ||
| Trial duration (s) | 68.3 ± 19 | −38.9 | −57% | −10.3 | −15% | 0.03 |
| Metric | Novice | Experienced | |||
|---|---|---|---|---|---|
| r | p-Value | r | p-Value | ||
| Number of Repetitions | 0.909 | 0.0000 | 0.613 | 0.0003 | |
| 0.906 | 0.0000 | 0.363 | 0.05 | ||
| Total Ang. Excursion (°) | 0.910 | 0.0000 | 0.407 | 0.03 | |
| 0.685 | 0.0000 | 0.383 | 0.04 | ||
| Smoothness () | −0.929 | 0.0000 | −0.771 | 0.0000 | |
| −0.896 | 0.0000 | −0.831 | 0.0000 | ||
| Dose-rate (reps/min) | 0.102 | 0.6 | −0.430 | 0.02 | |
| −0.356 | 0.05 | −0.582 | 0.0008 | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Segal, A.D.; Lesak, M.C.; Silverman, A.K.; Petruska, A.J. A Gesture-Controlled Rehabilitation Robot to Improve Engagement and Quantify Movement Performance. Sensors 2020, 20, 4269. https://doi.org/10.3390/s20154269
Segal AD, Lesak MC, Silverman AK, Petruska AJ. A Gesture-Controlled Rehabilitation Robot to Improve Engagement and Quantify Movement Performance. Sensors. 2020; 20(15):4269. https://doi.org/10.3390/s20154269
Chicago/Turabian StyleSegal, Ava D., Mark C. Lesak, Anne K. Silverman, and Andrew J. Petruska. 2020. "A Gesture-Controlled Rehabilitation Robot to Improve Engagement and Quantify Movement Performance" Sensors 20, no. 15: 4269. https://doi.org/10.3390/s20154269
APA StyleSegal, A. D., Lesak, M. C., Silverman, A. K., & Petruska, A. J. (2020). A Gesture-Controlled Rehabilitation Robot to Improve Engagement and Quantify Movement Performance. Sensors, 20(15), 4269. https://doi.org/10.3390/s20154269






