A Multi-Parametric Wearable System to Monitor Neck Movements and Respiratory Frequency of Computer Workers
Abstract
:1. Introduction
2. Description of the Wearable System
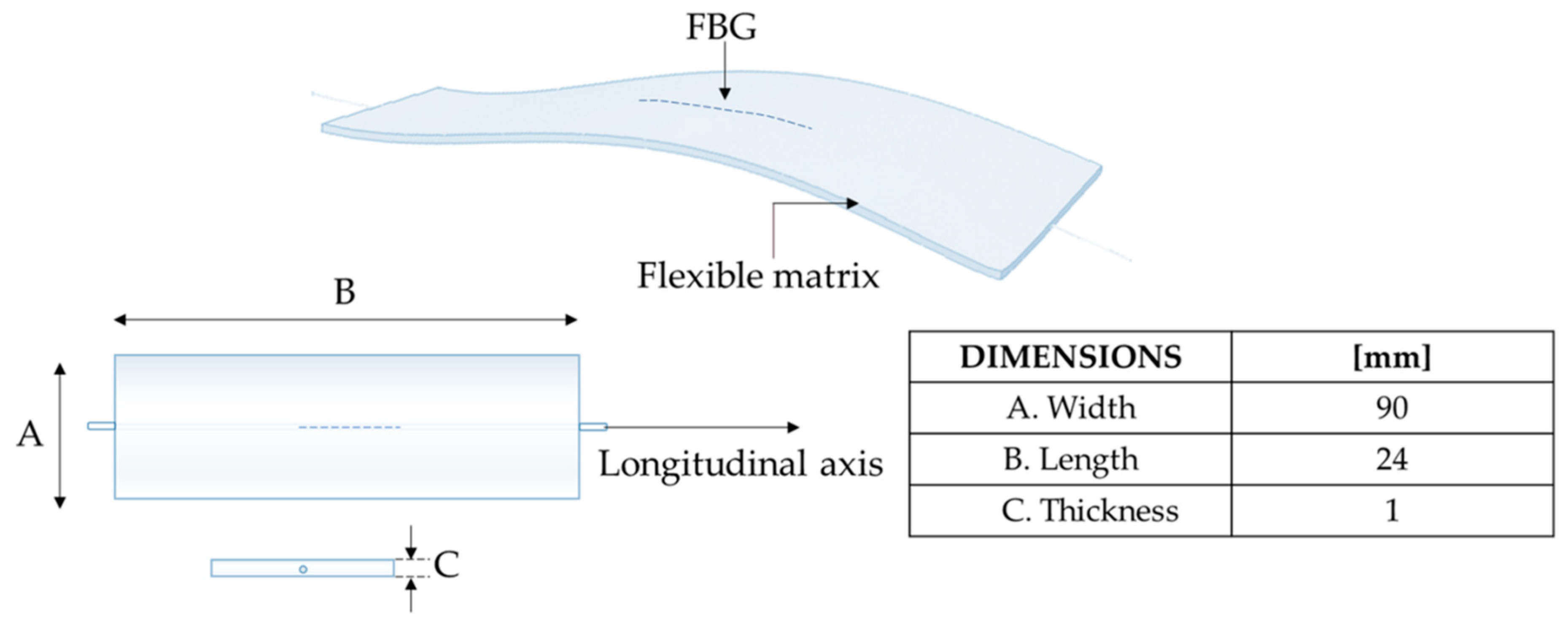
2.1. Flexible Sensors Based on FBG
2.2. Sensors Positioning and Measurement Parameters
3. System Assessment
3.1. Experimental Set-Up and Protocol
3.2. Data Analysis
3.2.1. Neck Movements
- the outputs of both the wearable and the MoCap systems were normalized in amplitude and plotted over time to evaluate trend similarity between signals;
- the FE and AR repetitions were detected by using a custom peak detection algorithm in MATLAB environment. FE movements were detected by considering the maximum peaks of both MoCap and FBG1 signals: when increases during the neck flexion (signal provided by the MoCap) FBG1 is strained with a consequent increase of λB (Figure 5A,B). Right AR movements were detected by considering the minimum peaks of both MoCap and FBG2 signals: when θAR decreases during the right AR (signal provided by the MoCap) FBG2 is compressed with a consequent decrement of λB (Figure 5C). These data were collected during the first 5 AR repetitions; left AR movements were detected by considering the maximum peaks of both MoCap and FBG2 signals because when θAR increases during the left AR (signal provided by the MoCap) FBG2 is strained with a consequent increment of λB (Figure 5B). These data were collected during the last 5 AR repetitions.
3.2.2. Breathing Activity
- The outputs of the wearable system and the flowmeter were normalized in amplitude and split into quiet breathing-related signals and tachypnea-related ones (i.e., FBG1qb, FBG2qb, FLOWqb, FBG1tc, FBG2tc, and FLOWtc), as shown in Figure 6;
- The signal of both FBG1qb and FBG1tc were inverted since the FBG1 was compressed during the inspiration (when the volume of lungs increases) and tensioned during the expiration (when the volume of lungs decreases). This step was not implemented on the FBG2 output since its trend in time matches that of the reference system;
- a third-order Butterworth low pass filter was applied on signals collected during quiet breathing (cut-off frequency, fc, of 0.5 Hz) and during tachypnea (fc of 3 Hz);
- spectral analysis in terms of power spectral density (PSD) was performed on the filtered signals and the maximum frequency (f0) of both the reference and the wearable systems signals were evaluated (Figure 7);
- peak detection was performed by using findpeaks in MATLAB environment: the input parameter related to minimum peaks distance was set starting from the value of f0 (Figure 7);
- the respiratory periods of each breath (i.e., TRi) was computed as the time elapsed between two consecutive maximum peaks of the signal provided by FBG1, FBG2, and the flowmeter, see Figure 7. The fRi values during both quiet breathing and tachypnea were estimated as 60/TRi and expressed as breaths per minute (bpm).
- in terms of percentage error () as in:where is the mean value of fR;
- in terms of absolute percentage errors for a breath-by-breath analysis:where and are the values of the ith fR estimated either by FBG1 or FBG2 and by the flowmeter;
- by calculating the mean value of the breath-by-breath absolute percentage errors (i.e., MAPE), for each volunteer as in:
3.3. Results
3.3.1. Detection of Neck Movements
3.3.2. Breathing Activity: Respiratory Frequency Estimation
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ailneni, R.C.; Syamala, K.R.; Kim, I.-S.; Hwang, J. Influence of the wearable posture correction sensor on head and neck posture: Sitting and standing workstations. Work 2019, 62, 27–35. [Google Scholar] [CrossRef]
- Barbieri, D.F.; Srinivasan, D.; Mathiassen, S.E.; Oliveira, A.B. Variation in upper extremity, neck and trunk postures when performing computer work at a sit-stand station. Appl. Ergon. 2019, 75, 120–128. [Google Scholar] [CrossRef]
- Bevan, S. Economic impact of musculoskeletal disorders (MSDs) on work in Europe. Best Pract. Res. Clin. Rheumatol. 2015, 29, 356–373. [Google Scholar] [CrossRef]
- Näf, M.B.; Koopman, A.S.; Baltrusch, S.; Rodriguez-Guerrero, C.; Vanderborght, B.; Lefeber, D. Passive back support exoskeleton improves range of motion using flexible beams. Front. Robot. AI 2018, 5. [Google Scholar] [CrossRef] [Green Version]
- Jun, D.; Zoe, M.; Johnston, V.; O’Leary, S. Physical risk factors for developing non-specific neck pain in office workers: A systematic review and meta-analysis. Int. Arch. Occup. Environ. Health 2017, 90, 373–410. [Google Scholar] [CrossRef] [PubMed]
- Ekinci, Y.; Uysal, S.A.; Kabak, V.Y.; Duger, T. Does ergonomics training have an effect on body posture during computer usage? J. Back Musculoskelet. Rehabil. 2019, 32, 191–1955. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, C.A.; Amick, B.C.; Dennerlein, J.T.; Brewer, S.; Catli, S.; Williams, R.; Serra, C.; Gerr, F.; Irvin, E.; Mahood, Q.; et al. Systematic review of the role of occupational health and safety interventions in the prevention of upper extremity musculoskeletal symptoms, signs, disorders, injuries, claims and lost time. J. Occup. Rehabil. 2010, 20, 127–162. [Google Scholar] [CrossRef] [PubMed]
- Cunha, B.; Tadi, P.; Bragg, B.N. Congenital Torticollis. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2019. [Google Scholar]
- Jaturongkhasumrit, K.; Mekhora, K.; Somprasong, S. Immediate Effect of Stress-induced Computer Typing on EMG Activity of Accessory Breathing Muscles and Respiratory Rate. J. Public Health 2019, 49, 144–154. [Google Scholar]
- Shikdar, A.A.; Al-Kindi, M.A. Office ergonomics: Deficiencies in computer workstation design. Int. J. Occup. Saf. Ergon. 2007, 13, 215–223. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elwardany, S.H.; El-Sayed, W.H.; Ali, M.F. Reliability of Kinovea computer program in measuring cervical range of motion in sagittal plane. OALib 2015, 2, 1–10. [Google Scholar] [CrossRef]
- Kang, B.-R.; Her, J.-G.; Lee, J.-S.; Ko, T.-S.; You, Y.-Y. Effects of the Computer Desk Level on the Musculoskeletal Discomfort of Neck and Upper Extremities and EMG Activities in Patients with Spinal Cord Injuries. Occup. Ther. Int. 2019, 2019, 3026150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Intolo, P.; Shalokhon, B.; Wongwech, G.; Wisiasut, P.; Nanthavanij, S.; Baxter, D.G. Analysis of neck and shoulder postures, and muscle activities relative to perceived pain during laptop computer use at a low-height table, sofa and bed. Work 2019, 63, 361–367. [Google Scholar] [CrossRef] [PubMed]
- Mekhora, K.; Liston, C.B.; Nanthavanij, S.; Cole, J.H. The effect of ergonomic intervention on discomfort in computer users with tension neck syndrome. Int. J. Ind. Ergon. 2000, 26, 367–379. [Google Scholar] [CrossRef]
- Saravanan, K.; Kumar, I.P. Effects of Ergonomic Training and Active Exercises for Non–Specific Work Related Upper Extremity Musculoskeletal Disorders in Women Working in Video Display Units. Asian J. Orthop. Res. 2019, 2, 1–12. [Google Scholar]
- Kahlaee, A.H.; Ghamkhar, L.; Arab, A.M. The Association between Neck Pain and Pulmonary Function: A Systematic Review. Am. J. Phys. Med. Rehabil. 2017, 96, 203–210. [Google Scholar] [CrossRef]
- Zafar, H.; Albarrati, A.; Alghadir, A.H.; Iqbal, Z.A. Effect of different head-neck postures on the respiratory function in healthy males. Biomed Res. Int. 2018, 2018, 4518269. [Google Scholar] [CrossRef] [Green Version]
- Grassmann, M.; Vlemincx, E.; von Leupoldt, A.; Mittelstädt, J.M.; Van den Bergh, O. Respiratory changes in response to cognitive load: A systematic review. Neural Plast. 2016, 2016, 8146809. [Google Scholar] [CrossRef] [Green Version]
- Grassmann, M.; Vlemincx, E.; von Leupoldt, A.; Van den Bergh, O. The role of respiratory measures to assess mental load in pilot selection. Ergonomics 2016, 59, 745–753. [Google Scholar] [CrossRef] [Green Version]
- Tipton, M.; Harper, A.; Paton, J.F.R.; Costello, J.T. The human ventilatory response to stress: Rate or depth? J. Physiol. 2017, 595, 5729–5752. [Google Scholar] [CrossRef]
- Massaroni, C.; Nicolò, A.; Lo Presti, D.; Sacchetti, M.; Silvestri, S.; Schena, E. Contact-Based Methods for Measuring Respiratory Rate. Sensors 2019, 19, 908. [Google Scholar] [CrossRef] [Green Version]
- Massaroni, C.; Lopes, D.S.; Lo Presti, D.; Schena, E.; Silvestri, S. Contactless monitoring of breathing patterns and respiratory rate at the pit of the neck: A single camera approach. J. Sensors 2018, 2018, 4567213. [Google Scholar] [CrossRef]
- Malasinghe, L.P.; Ramzan, N.; Dahal, K. Remote patient monitoring: A comprehensive study. J. Ambient Intell. Humaniz. Comput. 2019, 10, 57–76. [Google Scholar] [CrossRef] [Green Version]
- Massaroni, C.; Venanzi, C.; Silvatti, A.P.; Lo Presti, D.; Saccomandi, P.; Formica, D.; Giurazza, F.; Caponero, M.A.; Schena, E. Smart textile for respiratory monitoring and thoraco-abdominal motion pattern evaluation. J. Biophotonics 2018, 11, e201700263. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khan, Y.; Ostfeld, A.E.; Lochner, C.M.; Pierre, A.; Arias, A.C. Monitoring of vital signs with flexible and wearable medical devices. Adv. Mater. 2016, 28, 4373–4395. [Google Scholar] [CrossRef]
- Carnevale, A.; Longo, U.G.; Schena, E.; Massaroni, C.; Presti, D.L.; Berton, A.; Candela, V.; Denaro, V. Wearable systems for shoulder kinematics assessment: A systematic review. BMC Musculoskelet. Disord. 2019, 20, 546. [Google Scholar] [CrossRef]
- Gong, T.; Zhang, H.; Huang, W.; Mao, L.; Ke, Y.; Gao, M.; Yu, B. Highly responsive flexible strain sensor using polystyrene nanoparticle doped reduced graphene oxide for human health monitoring. Carbon N. Y. 2018, 140, 286–295. [Google Scholar] [CrossRef]
- Xu, H.; Lu, Y.F.; Xiang, J.X.; Zhang, M.K.; Zhao, Y.J.; Xie, Z.Y.; Gu, Z.Z. A multifunctional wearable sensor based on a graphene/inverse opal cellulose film for simultaneous, in situ monitoring of human motion and sweat. Nanoscale 2018, 10, 2090–2098. [Google Scholar] [CrossRef]
- Papi, E.; Koh, W.S.; McGregor, A.H. Wearable technology for spine movement assessment: A systematic review. J. Biomech. 2017, 64, 186–197. [Google Scholar] [CrossRef]
- Voinea, G.-D.; Butnariu, S.; Mogan, G. Measurement and geometric modelling of human spine posture for medical rehabilitation purposes using a wearable monitoring system based on inertial sensors. Sensors 2017, 17, 3. [Google Scholar] [CrossRef] [Green Version]
- Fathi, A.; Curran, K. Detection of spine curvature using wireless sensors. J. King Saud Univ. Sci. 2017, 29, 553–560. [Google Scholar] [CrossRef]
- O’Sullivan, K.; O’Sullivan, L.; Campbell, A.; O’Sullivan, P.; Dankaerts, W. Towards monitoring lumbo-pelvic posture in real-life situations: Concurrent validity of a novel posture monitor and a traditional laboratory-based motion analysis system. Man. Ther. 2012, 17, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Williams, J.M.; Haq, I.; Lee, R.Y. Dynamic measurement of lumbar curvature using fibre-optic sensors. Med. Eng. Phys. 2010, 32, 1043–1049. [Google Scholar] [CrossRef] [PubMed]
- Dunne, L.E.; Walsh, P.; Hermann, S.; Smyth, B.; Caulfield, B. Wearable monitoring of seated spinal posture. IEEE Trans. Biomed. Circuits Syst. 2008, 2, 97–105. [Google Scholar] [CrossRef] [PubMed]
- Dunne, L.; Walsh, P.; Smyth, B.; Caulfield, B. A system for wearable monitoring of seated posture in computer users. In 4th International Workshop on Wearable and Implantable Body Sensor Networks (BSN 2007); Springer: Berlin/Heidelberg, Germany, 2007; pp. 203–207. [Google Scholar]
- Duc, C.; Salvia, P.; Lubansu, A.; Feipel, V.; Aminian, K. A wearable inertial system to assess the cervical spine mobility: Comparison with an optoelectronic-based motion capture evaluation. Med. Eng. Phys. 2014, 36, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhou, H.; Yang, Z.; Samuel, O.W.; Liu, W.; Cao, Y.; Li, G. An intelligent wearable device for human’s cervical vertebra posture monitoring. In Proceedings of the 2018 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Honolulu, HI, USA, 17–21 July 2018; pp. 3280–3283. [Google Scholar]
- Maselli, M.; Mussi, E.; Cecchi, F.; Manti, M.; Tropea, P.; Laschi, C. A wearable sensing device for monitoring single planes neck movements: Assessment of its performance. IEEE Sens. J. 2018, 18, 6327–6336. [Google Scholar] [CrossRef]
- Presti, D.L.; Massaroni, C.; Di Tocco, J.; Schena, E.; Carnevale, A.; Longo, U.G.; D’Abbraccio, J.; Massari, L.; Oddo, C.M.; Caponero, M.A. Single-plane neck movements and respiratory frequency monitoring: A smart system for computer workers. In Proceedings of the 2019 II Workshop on Metrology for Industry 4.0 and IoT (MetroInd4. 0&IoT), Naples, Italy, 4–6 June 2019; pp. 167–170. [Google Scholar]
- Dinia, L.; Mangini, F.; Muzi, M.; Frezza, F. FBG multifunctional pH sensor-monitoring the pH rain in cultural heritage. Acta IMEKO 2018, 7, 24–30. [Google Scholar] [CrossRef]
- Tosi, D.; Poeggel, S.; Iordachita, I.; Schena, E. Fiber Optic Sensors for Biomedical Applications. In Opto-Mechanical Fiber Optic Sensors: Research, Technology, and Applications in Mechanical Sensing; Butterworth-Heinemann: Oxford, UK, 2018; pp. 301–333. ISBN 9780128031469. [Google Scholar]
- Presti, D.L.; Massaroni, C.; D’Abbraccio, J.; Massari, L.; Caponero, M.; Longo, U.G.; Formica, D.; Oddo, C.; Schena, E. Wearable system based on flexible FBG for respiratory and cardiac monitoring. IEEE Sens. J. 2019, 19, 7391–7398. [Google Scholar] [CrossRef]
- Roriz, P.; Lobo Ribeiro, A.B. Fiber Optical Sensors in Biomechanics. In Opto-Mechanical Fiber Optic Sensors: Research, Technology, and Applications in Mechanical Sensing; Butterworth-Heinemann: Oxford, UK, 2018; pp. 263–300. ISBN 9780128031469. [Google Scholar]
- Servati, A.; Zou, L.; Jane Wang, Z.; Ko, F.; Servati, P. Novel flexible wearable sensor materials and signal processing for vital sign and human activity monitoring. Sensors 2017, 17, 1622. [Google Scholar] [CrossRef] [Green Version]
- Lo Presti, D.; Massaroni, C.; Formica, D.; Giurazza, F.; Schena, E.; Saccomandi, P.; Caponero, M.A.; Muto, M. Respiratory and cardiac rates monitoring during MR examination by a sensorized smart textile. In Proceedings of the I2MTC 2017—2017 IEEE International Instrumentation and Measurement Technology Conference, Turin, Italy, 22–25 May 2017. [Google Scholar]
- Massaroni, C.; Saccomandi, P.; Formica, D.; Lo Presti, D.; Caponero, M.A.; Di Tomaso, G.; Giurazza, F.; Muto, M.; Schena, E. Design and Feasibility Assessment of a Magnetic Resonance-Compatible Smart Textile Based on Fiber Bragg Grating Sensors for Respiratory Monitoring. IEEE Sens. J. 2016, 16, 8103–8110. [Google Scholar] [CrossRef]
- Erdogan, T. Fiber grating spectra. J. Light. Technol. 1997, 15, 1277–1294. [Google Scholar] [CrossRef] [Green Version]
- Kang, J.-I.; Jeong, D.-K.; Choi, H. Correlation between pulmonary functions and respiratory muscle activity in patients with forward head posture. J. Phys. Ther. Sci. 2018, 30, 132–135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taffoni, F.; Formica, D.; Saccomandi, P.; Di Pino, G.; Schena, E. Optical fiber-based MR-compatible sensors for medical applications: An overview. Sensors 2013, 13, 14105–14120. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, S.; Hao, J.Z.; Lee, Y.W.A.; Cai, Z.; Do, T.T.; Ng, B.Y.R. Effect of bending methods on FBG lateral force sensor. Electron. Lett. 2005, 41, 1270–1271. [Google Scholar] [CrossRef]
- Dziuda, Ł.; Skibniewski, F.W.; Krej, M.; Baran, P.M. Fiber Bragg grating-based sensor for monitoring respiration and heart activity during magnetic resonance imaging examinations. J. Biomed. Opt. 2013, 18, 057006. [Google Scholar] [CrossRef] [Green Version]
- Massaroni, C.; Di Tocco, J.; Presti, D.L.; Longo, U.G.; Miccinilli, S.; Sterzi, S.; Formica, D.; Saccomandi, P.; Schena, E. Smart textile based on piezoresistive sensing elements for respiratory monitoring. IEEE Sens. J. 2019, 19, 7718–7725. [Google Scholar] [CrossRef]
- Huang, C.T.; Shen, C.L.; Tang, C.F.; Chang, S.H. A wearable yarn-based piezo-resistive sensor. Sens. Actuators Phys. 2008, 141, 396–403. [Google Scholar] [CrossRef]
- Sierra, G.; Telfort, V.; Popov, B.; Pelletier, M.; Despault, P.; Agarwal, R.; Lanzo, V. Comparison of respiratory rate estimation based on tracheal sounds versus a capnograph. In Proceedings of the 2005 Annual International Conference of the IEEE Engineering in Medicine and Biology, Shanghai, China, 17–18 January 2006. [Google Scholar]
- Mimoz, O.; Benard, T.; Gaucher, A.; Frasca, D.; Debaene, B. Accuracy of respiratory rate monitoring using a non-invasive acoustic method after general anaesthesia. Br. J. Anaesth. 2012, 108, 872–875. [Google Scholar] [CrossRef] [Green Version]
- Corbishley, P.; Rodríguez-Villegas, E. Breathing detection: Towards a miniaturized, wearable, battery-operated monitoring system. IEEE Trans. Biomed. Eng. 2008, 55, 196–204. [Google Scholar] [CrossRef]








| Age (Years) | Height (cm) | Body Mass (kg) | Neck Circumference (cm) | |
|---|---|---|---|---|
| Volunteer 1 | 23 | 183 | 125 | 46 |
| Volunteer 2 | 28 | 171 | 61 | 32 |
| Volunteer 3 | 27 | 178 | 85 | 38 |
| Volunteer 4 | 31 | 163 | 60 | 38 |
| Volunteer 5 | 39 | 171 | 71 | 43 |
| Quiet Breathing | |||
| Volunteer | FBG1 [bpm] | FLOW [bpm] | [%] |
| 1 | - | 15.37 | - |
| 2 | 14.47 | 14.63 | −1.09 |
| 3 | 14.36 | 14.14 | 1.53 |
| 4 | 22.36 | 22.09 | 1.22 |
| 5 | 15.15 | 15.22 | −0.45 |
| FBG2 [bpm] | FLOW [bpm] | [%] | |
| 1 | 15.30 | 15.37 | −0.48 |
| 2 | 14.65 | 14.63 | 0.15 |
| 3 | 15.00 | 14.14 | 6.09 |
| 4 | 22.40 | 22.09 | 1.40 |
| 5 | 15.10 | 15.22 | −0.79 |
| Tachypnea | |||
| Volunteer | FBG1 [bpm] | FLOW [bpm] | [%] |
| 1 | - | 83.62 | - |
| 2 | 48.65 | 48.80 | −0.32 |
| 3 | 83.28 | 83.87 | −0.71 |
| 4 | 54.53 | 54.58 | −0.09 |
| 5 | 37.88 | 38.09 | −0.56 |
| FBG2 [bpm] | FLOW [bpm] | [%] | |
| 1 | 82.02 | 83.62 | −1.90 |
| 2 | 48.46 | 48.80 | −0.72 |
| 3 | 82.98 | 83.87 | −1.05 |
| 4 | 54.99 | 54.58 | 0.75 |
| 5 | 38.01 | 38.09 | −0.19 |
| Quiet Breathing | ||||||||||
| Volunteer | |epFBG1| [%] | MAPEFBG1 [%] | ||||||||
| 1 | - | - | - | - | - | - | - | - | - | - |
| 2 | 10.40 | 0.34 | 0.28 | 0.19 | 0.58 | 1.91 | 2.24 | 2.93 | 3.22 | 2.45 |
| 3 | 16.66 | 10.88 | 2.28 | 4.97 | 10.26 | 7.75 | 13.7 | 5.62 | 8.17 | 8.92 |
| 4 | 12.32 | 7.11 | 14.04 | 13.51 | 10.17 | 28.65 | 1.24 | 15.56 | 13.21 | 12.87 |
| 5 | 0.21 | 8.24 | 4.48 | 5.92 | 0.91 | 3.56 | 6.58 | 4.71 | 1.04 | 1.47 |
| |epFBG2| [%] | MAPEFBG2 [%] | |||||||||
| 1 | 5.28 | 3.76 | 0.20 | 2.18 | 4.75 | 4.19 | 1.33 | 4.92 | 4.33 | 3.44 |
| 2 | 2.69 | 0.86 | 2.06 | 1.14 | 0.97 | 2.09 | 0.19 | 6.76 | 4.42 | 2.36 |
| 3 | 29.36 | 12.12 | 4.05 | 3.63 | 17.35 | 27.82 | 8.21 | 15.75 | 19.93 | 15.36 |
| 4 | 15.34 | 16.03 | 4.22 | 0.85 | 7.36 | 3.46 | 3.33 | 0.16 | 1.35 | 5.79 |
| 5 | 2.53 | 1.52 | 0.95 | 1.95 | ~0 | 0.41 | 2.31 | 2.89 | 1.23 | 1.53 |
| Tachypnea | ||||||||||
| Volunteer | |epFBG1| [%] | MAPEFBG1 [%] | ||||||||
| 1 | - | - | - | - | - | - | - | - | - | - |
| 2 | 3.74 | 0.65 | 3.11 | 3.34 | 7.56 | 6.21 | 4.64 | 11.54 | 3.75 | 4.95 |
| 3 | 1.69 | 2.70 | 1.71 | 0.55 | 3.72 | 4.09 | ~0 | 5.82 | 1.16 | 2.38 |
| 4 | 2.95 | 9.77 | 4.48 | 18.86 | 0.37 | 1.46 | 1.44 | 5.35 | 8.10 | 5.86 |
| 5 | 0.52 | 1.06 | 0.77 | 1.84 | 0.50 | 0.73 | 0.24 | 1.31 | 2.11 | 1.01 |
| |epFBG2| [%] | MAPEFBG2 [%] | |||||||||
| 1 | 6.95 | 2.26 | 0.56 | 2.72 | 2.63 | 3.68 | 1.63 | 2.81 | 5.13 | 3.15 |
| 2 | 4.07 | 0.97 | 3.67 | 2.52 | 3.34 | 0.96 | 0.97 | 6.69 | 3.45 | 2.96 |
| 3 | 8.85 | 7.14 | 0.55 | ~0 | 1.12 | 1.14 | 0.55 | 1.11 | 7.41 | 3.10 |
| 4 | 6.41 | 2.47 | 9.92 | 5.24 | 5.43 | 2.11 | 6.23 | 6.29 | ~0 | 4.90 |
| 5 | 0.52 | 1.33 | 0.26 | 1.84 | 0.49 | ~0 | 1.72 | 1.02 | 0.72 | 0.88 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lo Presti, D.; Carnevale, A.; D’Abbraccio, J.; Massari, L.; Massaroni, C.; Sabbadini, R.; Zaltieri, M.; Di Tocco, J.; Bravi, M.; Miccinilli, S.; et al. A Multi-Parametric Wearable System to Monitor Neck Movements and Respiratory Frequency of Computer Workers. Sensors 2020, 20, 536. https://doi.org/10.3390/s20020536
Lo Presti D, Carnevale A, D’Abbraccio J, Massari L, Massaroni C, Sabbadini R, Zaltieri M, Di Tocco J, Bravi M, Miccinilli S, et al. A Multi-Parametric Wearable System to Monitor Neck Movements and Respiratory Frequency of Computer Workers. Sensors. 2020; 20(2):536. https://doi.org/10.3390/s20020536
Chicago/Turabian StyleLo Presti, Daniela, Arianna Carnevale, Jessica D’Abbraccio, Luca Massari, Carlo Massaroni, Riccardo Sabbadini, Martina Zaltieri, Joshua Di Tocco, Marco Bravi, Sandra Miccinilli, and et al. 2020. "A Multi-Parametric Wearable System to Monitor Neck Movements and Respiratory Frequency of Computer Workers" Sensors 20, no. 2: 536. https://doi.org/10.3390/s20020536
APA StyleLo Presti, D., Carnevale, A., D’Abbraccio, J., Massari, L., Massaroni, C., Sabbadini, R., Zaltieri, M., Di Tocco, J., Bravi, M., Miccinilli, S., Sterzi, S., Longo, U. G., Denaro, V., Caponero, M. A., Formica, D., Oddo, C. M., & Schena, E. (2020). A Multi-Parametric Wearable System to Monitor Neck Movements and Respiratory Frequency of Computer Workers. Sensors, 20(2), 536. https://doi.org/10.3390/s20020536














