A Revised Point-to-Point Calibration Approach with Adaptive Errors Correction to Weaken Initial Sensitivity of Cuff-Less Blood Pressure Estimation
Abstract
:1. Introduction
2. Methods
2.1. Two Popular Cuff-Less BP Estimate Models
2.2. Two Point-to-Point Calibration Methods (mPTP and fPTP)
2.3. Experiment and Data Collecting
2.3.1. Experimental Protocol
2.3.2. Subjects and Data Collecting
2.4. Data Analysis
3. Results
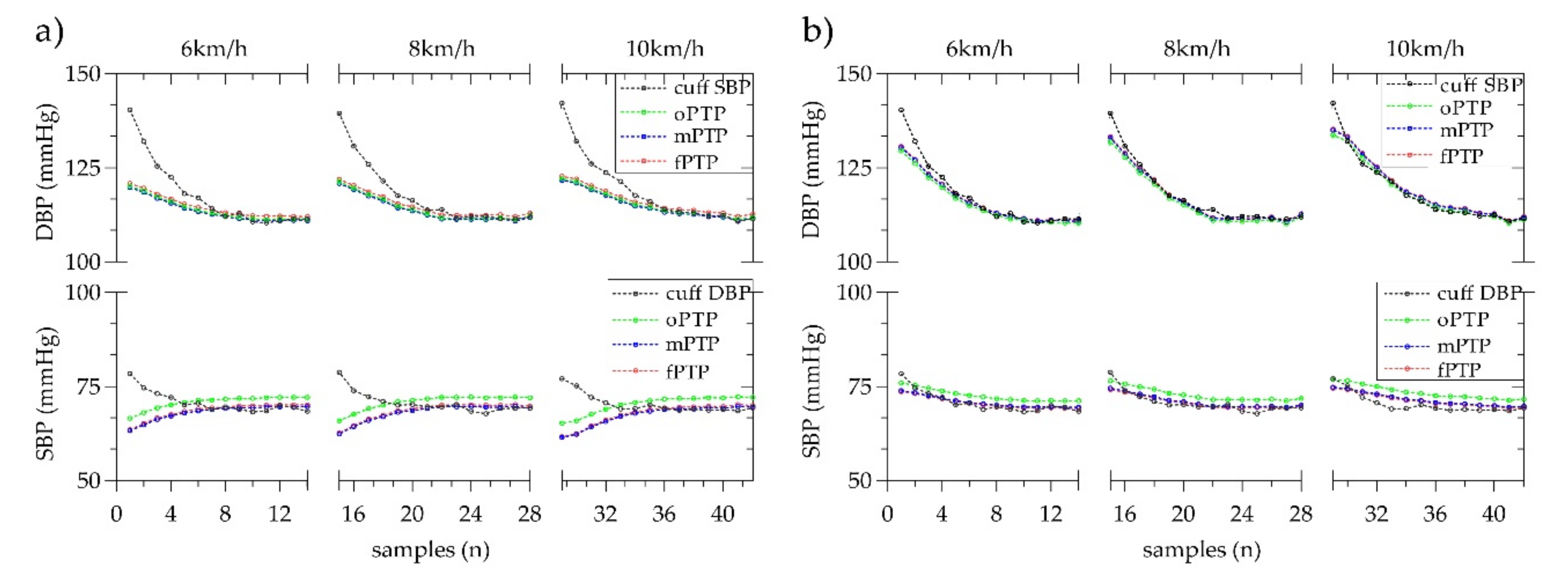
3.1. Consistency
3.2. Correlation
3.3. Overall Performance
3.4. Comparison with Prior Works
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lewington, S.; Clarke, R.; Qizilbash, N. Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002, 361, 1389–1390. [Google Scholar]
- Kachuee, M.; Kiani, M.; Mohammadzade, H. Cuff-Less blood pressure estimation algorithms for continuous health-care monitoring. IEEE Trans. Biomed. Eng. 2017, 64, 859–869. [Google Scholar] [CrossRef] [PubMed]
- Tang, Z.; Tamura, T.; Sekine, M. A chair-based unobtrusive cuffless blood pressure monitoring system based on pulse arrival time. IEEE J. Biomed. Health Inf. 2016, 21, 1194–1205. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Hahn, J.O.; Mukkamala, R. Error mechanisms of the oscillometric fixed-ratio blood pressure measurement method. Ann. Biomed. Eng. 2013, 41, 587–597. [Google Scholar] [CrossRef] [PubMed]
- Solà, J.; Chételat, O.; Sartori, C. Chest pulse-wave velocity: A novel approach to assess arterial stiffness. IEEE Trans. Biomed. Eng. 2011, 58, 215–223. [Google Scholar] [CrossRef]
- O’Brien, E.; Asmar, R.; Beilin, L. European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J. Hypertens. 2003, 21, 821–848. [Google Scholar] [CrossRef]
- Luo, N.; Dai, W.; Li, C. Flexible piezoresistive sensor patch enabling ultralow power cuffless blood pressure measurement. Adv. Funct. Mater. 2016, 26, 1178–1187. [Google Scholar] [CrossRef]
- Martin, L.O.; Carek, A.M.; Kim, C.S. Weighing scale-based pulse transit time is a superior marker of blood pressure than conventional pulse arrival time. Sci. Rep. 2016, 6, 39273. [Google Scholar] [CrossRef]
- Choi, Y.; Zhang, Q.; Ko, S. Noninvasive cuffless blood pressure estimation using pulse transit time and Hilbert–Huang transform. Comput. Electr. Eng. 2013, 39, 103–111. [Google Scholar] [CrossRef]
- Ding, X.; Zhao, N.; Yang, G. Continuous blood pressure measurement from invasive to unobtrusive: Celebration of 200th birth anniversary of Carl Ludwig. IEEE J. Biomed. Health. 2016, 20, 1455–1465. [Google Scholar] [CrossRef]
- Mccarthy, B.M.; Vaughan, C.J. An examination of calibration intervals required for accurately tracking blood pressure using pulse transit time algorithms. J. Hum. Hypertens. 2013, 27, 744–750. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ding, X.; Yan, B.P.; Zhang, Y.T. Pulse transit time based continuous cuffless blood pressure estimation: A new extension and a comprehensive evaluation. Sci. Rep. 2017, 7, 11554. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.; Xu, W.; Guan, N. Noninvasive and continuous blood pressure monitoring using wearable body sensor networks. IEEE Intell. Syst. 2015, 30, 38–48. [Google Scholar] [CrossRef]
- Bilo, G.; Zorzi, C.; Munera, J.E.O. Validation of the somnotouch-NIBP noninvasive continuous blood pressure monitor according to the European society of hypertension international protocol revision 2010. Blood Press. Monit. 2015, 20, 291–294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mukkamala, R.; Hahn, J.O.; Inan, O.T. Toward ubiquitous blood pressure monitoring via pulse transit time: Theory and practice. IEEE Trans. Biomed. Eng. 2015, 62, 1879–1901. [Google Scholar] [CrossRef] [Green Version]
- Wong, Y.M.; Poon, C.Y.; Zhang, Y.T. An evaluation of the cuffless blood pressure estimation based on pulse transit time technique: A half year study on normotensive subjects. Cardiovasc. Eng. 2009, 9, 32–38. [Google Scholar] [CrossRef]
- Zheng, Y.; Poon, C.C.; Yan, B.P. Pulse arrival time based on cuff-less and 24-H wearable blood pressure monitoring and its diagnostic value in hypertension. J. Med. Syst. 2016, 40, 195. [Google Scholar] [CrossRef]
- Chen, W.; Kobayashi, T.; Ichikawa, S. Continuous estimation of systolic blood pressure using the pulse arrival time and intermittent calibration. Med. Biol. Eng. Comput. 2000, 38, 569–574. [Google Scholar] [CrossRef]
- Nabeel, P.; Joseph, J.; Sivaprakasam, M. Single-source PPG based local pulse wave velocity measurement: A potential cuffless blood pressure estimation technique. Physiol. Meas. 2017, 38, 2122–2140. [Google Scholar] [CrossRef]
- Zhang, Q.; Chen, X.; Fang, Z. Cuff-less blood pressure measurement using pulse arrival time and a Kalman filter. Micromech. Microeng. 2017, 27, 024002. [Google Scholar] [CrossRef]
- Baek, H.J.; Kim, K.K.; Kim, J.S. Enhancing the estimation of blood pressure using pulse arrival time and two confounding factors. Physiol. Meas. 2010, 31, 145–157. [Google Scholar] [CrossRef]
- Chen, S.; Ji, Z.; Wu, H. A non-invasive continuous blood pressure estimation approach based on machine learning. Sensors 2019, 19, 2585. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Monte-Moreno, E. Non-invasive estimate of blood glucose and blood pressure from a photoplethysmograph by means of machine learning techniques. Artif. Intell. Med. 2011, 53, 127–138. [Google Scholar] [CrossRef] [PubMed]
- Pandian, P.S.; Mohanavelu, K.; Safeer, K.P. Smart Vest: Wearable multi-parameter remote physiological monitoring system. Med. Eng. Phys. 2008, 30, 466–477. [Google Scholar] [CrossRef] [PubMed]
- AAMI. American National Standard for Electronic or Automated Sphygmomanometers; ANSI/AAMI SP 10 2002; AAMI: Arlington, VA, USA, 2002. [Google Scholar]
- Liu, Q.; Yan, B.P.; Yu, C.M. Attenuation of systolic blood pressure and pulse transit time hysteresis during exercise and recovery in cardiovascular patients. IEEE Trans. Biomed. Eng. 2014, 61, 346–352. [Google Scholar] [PubMed]
- Ding, X.R.; Zhang, Y.T.; Liu, J. Continuous cuffless blood pressure estimation using pulse transit time and photoplethysmogram intensity ratio. IEEE Trans. Biomed. Eng. 2016, 63, 964–972. [Google Scholar] [CrossRef]
- Korteweg, D.J. Ueber die Fortpflanzungsgeschwindigkeit des schalles in elastischen Röhren. Ann. Phys. Chem. 2006, 241, 525–542. [Google Scholar] [CrossRef] [Green Version]
- Gil, E.; Orini, M.; Bailón, R. Photoplethysmography pulse rate variability as a surrogate measurement of heart rate variability during non-stationary conditions. Physiol. Meas. 2010, 31, 1271–1290. [Google Scholar] [CrossRef]
- Jeong, I.C.; Finkelstein, J. Introducing contactless blood pressure assessment using a high speed video camera. J. Med. Syst. 2016, 40, 77. [Google Scholar] [CrossRef]
- Monika, S.; Martin, G.; Matja, G. Non-invasive blood pressure estimation from ECG using machine learning techniques. Sensors 2018, 18, 1160. [Google Scholar]
- Chen, Y.; Wen, C.; Tao, G. Continuous and noninvasive measurement of systolic and diastolic blood pressure by one mathematical model with the same model parameters and two separate pulse wave velocities. Ann Biomed. Eng. 2012, 40, 871–882. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.S.; Carek, A.M.; Mukkamala, R. Ballistocardiogram as proximal timing reference for pulse transit time measurement: Potential for cuffless blood pressure monitoring. IEEE Trans. Biomed. Eng. 2015, 62, 2657–2664. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huynh, T.H.; Jafari, R.; Chung, W.Y. Noninvasive cuffless blood pressure estimation using pulse transit time and impedance plethysmography. IEEE Trans. Biomed. Eng. 2019, 66, 967–976. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, B.; Jafari, R. Cuffless blood pressure monitoring from an array of wrist bio-impedance sensors using subject-specific regression models: Proof of concept. IEEE Trans. Biomed. Circuits Syst. 2019, 13, 1723–1735. [Google Scholar] [CrossRef]
- Liu, J.; Yan, B.; Zhang, Y. Multi-wavelength photoplethysmography enabling continuous blood pressure measurement with compact wearable electronics. IEEE Trans. Biomed. Eng. 2018, 66, 1514–1525. [Google Scholar] [CrossRef]
- Johnson, A.E.W.; Pollard, T.J.; Shen, L. MIMIC-III, a freely accessible critical care database. Sci. Data 2016, 3, 160035. [Google Scholar] [CrossRef] [Green Version]
- Wong, Y.M.; Pickwell-Macpherson, E.; Zhang, Y.T. The acute effects of running on blood pressure estimation using pulse transit time in normotensive subjects. Eur. J. Appl. Physiol. 2009, 107, 169–175. [Google Scholar] [CrossRef]
- Shao, J.; Shi, P.; Hu, S.J. An optimization study of estimating blood pressure models based on pulse arrival time for continuous monitoring. J. Healthc. Eng. 2020, 2020, 1078251. [Google Scholar] [CrossRef]
- Cattivelli, F.S.; Garudadri, H. Noninvasive cuffless estimation of blood pressure from pulse arrival time and heart rate with adaptive calibration. In Proceedings of the 6th International Workshop on Wearable and Implantable Body Sensor Networks, Berkeley, CA, USA, 3–5 June 2009; pp. 114–119. [Google Scholar]
- Poon, C.C.Y.; Zhang, Y.T. Cuff-less and noninvasive measurements of arterial blood pressure by pulse transit time. In Proceedings of the 27th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Shanghai, China, 1–4 September 2005; Volume 6, pp. 5877–5880. [Google Scholar]
- Hughes, D.J.; Babbs, C.F.; Geddes, L.A. Measurements of Young’s modulus of elasticity of the canine aorta with ultrasound. Ultrason. Imaging 1979, 1, 356–367. [Google Scholar] [CrossRef] [Green Version]
- Buxi, D.; Redouté, J.M.; Yuce, M.R. A survey on signals and systems in ambulatory blood pressure monitoring using pulse transit time. Physiol. Meas. 2015, 36, R1. [Google Scholar] [CrossRef]
- Mukkamala, R.; Hahn, J.O.; Inan, O.T. Toward ubiquitous blood pressure monitoring via pulse transit time: Predictions on maximum calibration period and acceptable error limits. IEEE Trans. Biomed. Eng. 2018, 65, 1410–1420. [Google Scholar] [CrossRef] [PubMed]
- Baldoumas, G.; Peschos, D.; Tatsis, G. A prototype photoplethysmography electronic device that distinguishes congestive heart failure from healthy individuals by applying natural time analysis. Electronics 2019, 8, 1288. [Google Scholar] [CrossRef] [Green Version]
- Escobar, B.; Torres, R. Feasibility of non-invasive blood pressure estimation based on pulse arrival time: A MIMIC database study. In Proceedings of the 41st Computing in Cardiology Conference (CinC), Cambridge, MA, USA, 7–10 September 2014; pp. 1113–1116. [Google Scholar]






| Models | SBP | DBP |
|---|---|---|
| MK-BH [3] | ||
| dMK-BH [17] |
| Selection Factor | Values |
|---|---|
| Total number (M, F) | 21 (14, 7) |
| Age (years) | 22.48 ± 1.03 |
| Height (cm) | 171.52 ± 8.14 |
| Body mass (kg) | 63.81 ± 11.68 |
| BMI (kg/m2) | 21.46 ± 2.89 |
| SBP (mmHg) | 122.84 ± 13.04 |
| DBP (mmHg) | 74.42 ± 6.65 |
| Methods | MK-BH; dMK-BH/mmHg | |||
|---|---|---|---|---|
| Bias | Bias of SD | 95% Limits of Agreement | within Agreement/% | |
| oPTP | 3.56; 1.33 | 8.95; 8.58 | (−13.98, 21.11); (−15.48, 18.13) | 86.73; 93.01 |
| mPTP | 3.89; 0.77 | 8.86; 7.79 | (−13.47, 21.25); (−14.50, 16.03) | 82.07; 93.52 |
| fPTP | 2.73; 0.54 | 8.38; 6.95 | (−13.71, 19.14); (−13.08, 14.15) | 83.89; 94.12 |
| Methods | MK-BH; dMK-BH/mmHg | |||
|---|---|---|---|---|
| Bias | Bias of SD | 95% Limits of Agreement | Within Agreement/% | |
| oPTP | −0.14; −2.38 | 8.53; 6.51 | (−16.85, 16.57); (−15.14, 10.39) | 85.01; 89.67 |
| mPTP | 2.61; −0.51 | 7.79; 5.70 | (−12.65, 17.87); (−11.69, −11.69) | 81.46; 93.11 |
| fPTP | 2.16; −0.24 | 7.52; 5.21 | (−12.58, 16.91); (−11.69; −11.69) | 82.78; 93.72 |
| Methods | SBP | DBP | ||
|---|---|---|---|---|
| MK-BH | dMK-BH | MK-BH | dMK-BH | |
| oPTP | 0.76 | 0.80 | 0.53 | 0.70 |
| mPTP | 0.78 | 0.83 | 0.54 | 0.74 |
| fPTP | 0.81 | 0.87 | 0.56 | 0.78 |
| Calibration | Subjects | Acquired Signals (Measure Location) | Accuracy w.r.t. cuff BP [mean ± SD (MAD)/mmHg; r] | |
|---|---|---|---|---|
| Method | Intervention | |||
| Probability distributions [31] | Daily activities | N = 51 | Only ECG: chest | SBP:/± 10.22 (7.72);/ DBP:/± 10.03 (9.45);/ |
| oPTP [32] | Supine position | N = 26 | Only PPG: ear, toe | SBP: 2.16 ± 6.23 (8†);/ DBP: −1.49 ± 6.51 (9†);/ |
| oPTP [33] | Deep breathing + Sustained handgrip | N = 15 | ECG: chest BCG: foots | SBP: −0.03 ± 8.58 (9) †; 0.70 DBP: −0.02 ± 5.81 (7) †; 0.66 |
| oPTP [34] | handgrip exercises | N = 15 | IPG: wrist PPG: finger | SBP: 0.31 ± 8.55 (5†); 0.88 DBP: −0.5 ± 5.07 (4†); 0.88 |
| PTP, three pairs [35] | Post-exercise | N = 10 | PPG: finger Bio-Z: wrist | SBP: −0.09 ± 7.16 (6†); 0.86 DBP: −0.02 ± 2.56 (5†); 0.77 |
| Multi-wavelength [36] | Deep breathing + Valsalva maneuver | N = 40 | ECG: wrist, foot PPG: finger ICG: neck, thorax | SBP: 0.00† ± 2.85 (2.2); 0.98 DBP: 0.00† ± 1.75 (1.4); 0.99 |
| Machine learning [22] | MIMIC-III [37] | N = 155† | ECG and PPG [37] | SBP: 0.03 ± 5.52 (3.27); 0.97 DBP: 0.10 ± 1.97 (1.16); 0.97 |
| mPTP, this work (dMK-BH model) | Running exercise | N = 21 | ECG: wrist, foot PPG: finger | SBP: −0.77 ± 7.79 (6.0); 0.83 DBP: 0.51 ± 5.70 (4.4); 0.74 |
| fPTP, this work (dMK-BH model) | Running exercise | N = 21 | ECG: wrist, foot PPG: finger | SBP: −0.54 ± 6.95 (5.3); 0.87 DBP: 0.24 ± 5.21 (4.0); 0.78 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shao, J.; Shi, P.; Hu, S.; Yu, H. A Revised Point-to-Point Calibration Approach with Adaptive Errors Correction to Weaken Initial Sensitivity of Cuff-Less Blood Pressure Estimation. Sensors 2020, 20, 2205. https://doi.org/10.3390/s20082205
Shao J, Shi P, Hu S, Yu H. A Revised Point-to-Point Calibration Approach with Adaptive Errors Correction to Weaken Initial Sensitivity of Cuff-Less Blood Pressure Estimation. Sensors. 2020; 20(8):2205. https://doi.org/10.3390/s20082205
Chicago/Turabian StyleShao, Jiang, Ping Shi, Sijung Hu, and Hongliu Yu. 2020. "A Revised Point-to-Point Calibration Approach with Adaptive Errors Correction to Weaken Initial Sensitivity of Cuff-Less Blood Pressure Estimation" Sensors 20, no. 8: 2205. https://doi.org/10.3390/s20082205





