Wearable Activity Monitoring in Day-to-Day Stroke Care: A Promising Tool but Not Widely Used
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Data Collection
2.2. Survey Development
2.3. Data Analysis
3. Results
3.1. Participants
3.2. Users
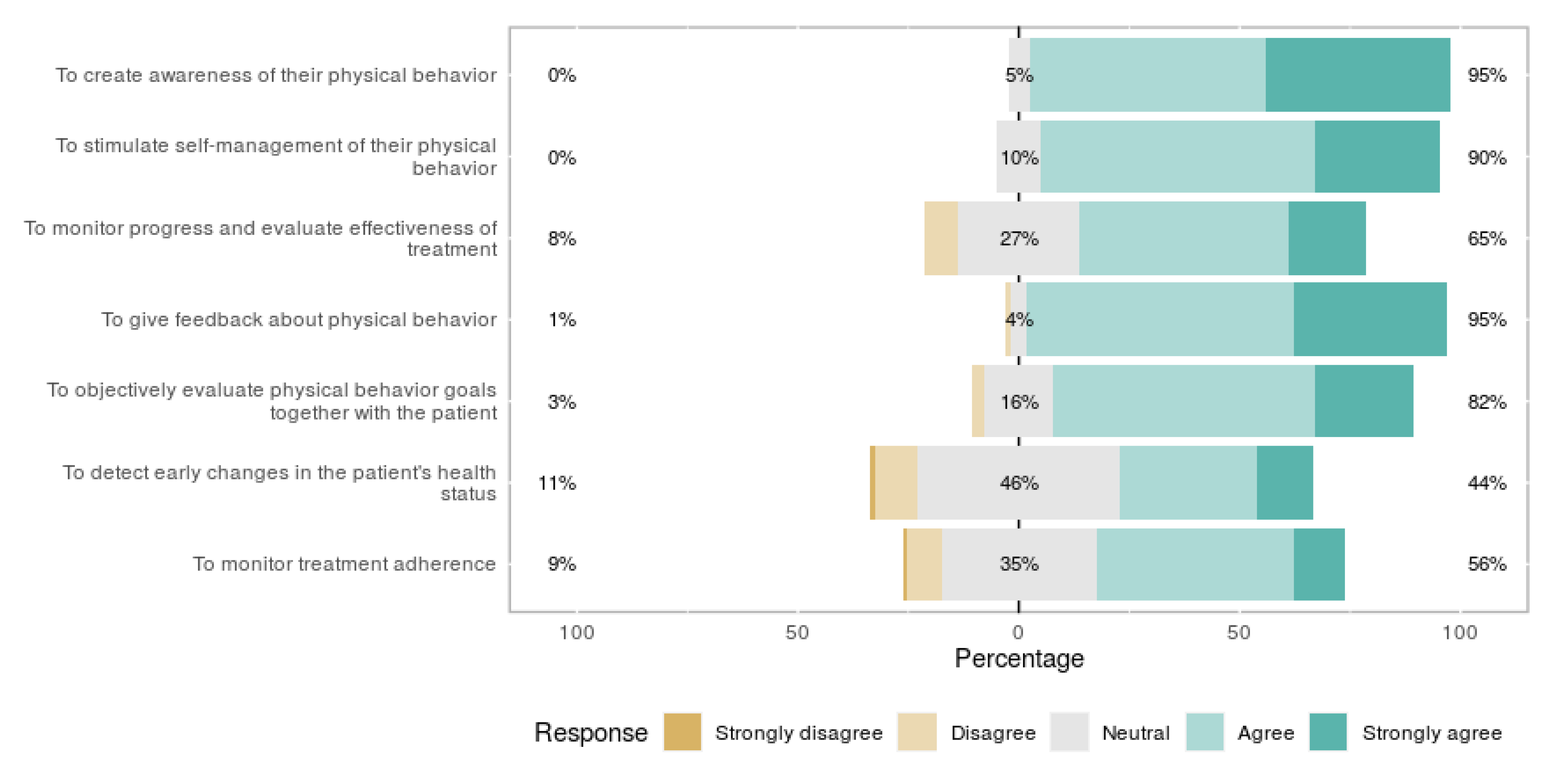
3.3. Perceived Usefulness
3.4. Barriers
3.5. Future Thoughts of Non-Users
3.6. Additional Thoughts
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Global Health Estimates: Deaths by Cause, Age, Sex and Country, 2000–2012; WHO: Geneva, Switzerland, 2014; Volume 9. [Google Scholar]
- Rajsic, S.; Gothe, H.; Borba, H.H.; Sroczynski, G.; Vujicic, J.; Toell, T.; Siebert, U. Economic burden of stroke: A systematic review on post-stroke care. Eur. J. Health Econ. 2019, 20, 107–134. [Google Scholar] [CrossRef]
- Collaborators, G.S. Global, regional, and national burden of stroke, 1990-2016: A systematic analysis for the global burden of disease study 2016. Lancet Neurol. 2019, 18, 439–458. [Google Scholar]
- Billinger, S.A.; Arena, R.; Bernhardt, J.; Eng, J.J.; Franklin, B.A.; Johnson, C.M.; MacKay-Lyons, M.; Macko, R.F.; Mead, G.E.; Roth, E.J.; et al. Physical activity and exercise recommendations for stroke survivors: A statement for healthcare professionals from the american heart association/american stroke association. Stroke 2014, 45, 2532–2553. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shaughnessy, M.; Michael, K.M.; Sorkin, J.D.; Macko, R.F. Steps after stroke: Capturing ambulatory recovery. Stroke 2005, 36, 1305–1307. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Langhorne, P.; Bernhardt, J.; Kwakkel, G. Stroke rehabilitation. Lancet 2011, 377, 1693–1702. [Google Scholar] [CrossRef]
- Thilarajah, S.; Mentiplay, B.F.; Bower, K.J.; Tan, D.; Pua, Y.H.; Williams, G.; Koh, G.; Clark, R.A. Factors associated with post-stroke physical activity: A systematic review and meta-analysis. Arch. Phys. Med. Rehabil. 2018, 99, 1876–1889. [Google Scholar] [CrossRef] [PubMed]
- Saunders, D.H.; Greig, C.A.; Mead, G.E. Physical activity and exercise after stroke: Review of multiple meaningful benefits. Stroke 2014, 45, 3742–3747. [Google Scholar] [CrossRef] [Green Version]
- Lawrence, M.; Pringle, J.; Kerr, S.; Booth, J.; Govan, L.; Roberts, N.J. Multimodal secondary prevention behavioral interventions for tia and stroke: A systematic review and meta-analysis. PLoS ONE 2015, 10, e0120902. [Google Scholar] [CrossRef] [Green Version]
- Han, P.; Zhang, W.; Kang, L.; Ma, Y.; Fu, L.; Jia, L.; Yu, H.; Chen, X.; Hou, L.; Wang, L.; et al. Clinical evidence of exercise benefits for stroke. Adv. Exp. Med. Biol. 2017, 1000, 131–151. [Google Scholar]
- Bussmann, J.B.; van den Berg-Emons, R.J. To total amount of activity..... And beyond: Perspectives on measuring physical behavior. Front. Psychol. 2013, 4, 463. [Google Scholar] [CrossRef] [Green Version]
- Teychenne, M.; Ball, K.; Salmon, J. Sedentary behavior and depression among adults: A review. Int. J. Behav. Med. 2010, 17, 246–254. [Google Scholar] [CrossRef]
- Biswas, A.; Alter, D.A. Sedentary time and risk for mortality. Ann. Intern. Med. 2015, 162, 875–876. [Google Scholar] [CrossRef]
- Marwaa, M.N.; Kristensen, H.K.; Guidetti, S.; Ytterberg, C. Physiotherapists’ and occupational therapists’ perspectives on information and communication technology in stroke rehabilitation. PLoS ONE 2020, 15, e0236831. [Google Scholar] [CrossRef] [PubMed]
- Wright, S.P.; Hall Brown, T.S.; Collier, S.R.; Sandberg, K. How consumer physical activity monitors could transform human physiology research. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2017, 312, R358–R367. [Google Scholar] [CrossRef]
- Piwek, L.; Ellis, D.A.; Andrews, S.; Joinson, A. The rise of consumer health wearables: Promises and barriers. PLoS Med. 2016, 13, e1001953. [Google Scholar] [CrossRef] [PubMed]
- Vegesna, A.; Tran, M.; Angelaccio, M.; Arcona, S. Remote patient monitoring via non-invasive digital technologies: A systematic review. Telemed. J. E Health 2017, 23, 3–17. [Google Scholar] [CrossRef] [PubMed]
- Hailey, D.; Roine, R.; Ohinmaa, A.; Dennett, L. Evidence of benefit from telerehabilitation in routine care: A systematic review. J. Telemed. Telecare 2011, 17, 281–287. [Google Scholar] [CrossRef] [PubMed]
- Braakhuis, H.E.M.; Berger, M.A.M.; Bussmann, J.B.J. Effectiveness of healthcare interventions using objective feedback on physical activity: A systematic review and meta-analysis. J. Rehabil. Med. 2019, 51, 151–159. [Google Scholar] [CrossRef] [Green Version]
- Dobkin, B.H.; Martinez, C. Wearable sensors to monitor, enable feedback, and measure outcomes of activity and practice. Curr. Neurol. Neurosci. Rep. 2018, 18, 87. [Google Scholar] [CrossRef] [Green Version]
- Langan, J.; Subryan, H.; Nwogu, I.; Cavuoto, L. Reported use of technology in stroke rehabilitation by physical and occupational therapists. Disabil. Rehabil. Assist. Technol. 2018, 13, 641–647. [Google Scholar] [CrossRef] [PubMed]
- Allouch, S.B.; van Velsen, L. Fit by bits: An explorative study of sports physiotherapists’ perception of quantified self technologies. Stud. Health Technol. Inform. 2018, 247, 296–300. [Google Scholar]
- Lang, C.E.; Barth, J.; Holleran, C.L.; Konrad, J.D.; Bland, M.D. Implementation of wearable sensing technology for movement: Pushing forward into the routine physical rehabilitation care field. Sensors 2020, 20, 5744. [Google Scholar] [CrossRef]
- Hoy, M.B. Personal activity trackers and the quantified self. Med. Ref. Serv. Q. 2016, 35, 94–100. [Google Scholar] [CrossRef]
- Sabus, C.; Spake, E. Innovative physical therapy practice: A qualitative verification of factors that support diffusion of innovation in outpatient physical therapy practice. J. Healthc. Leadersh. 2016, 8, 107–120. [Google Scholar] [CrossRef] [Green Version]
- Brouns, B.; Meesters, J.J.L.; Wentink, M.M.; de Kloet, A.J.; Arwert, H.J.; Boyce, L.W.; Vliet Vlieland, T.P.M.; van Bodegom-Vos, L. Factors associated with willingness to use erehabilitation after stroke: A cross-sectional study among patients, informal caregivers and healthcare professionals. J. Rehabil. Med. 2019, 51, 665–674. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Miguel Cruz, A.; Rios Rincon, A.; Buttar, V.; Ranson, Q.; Goertzen, D. What factors determine therapists’ acceptance of new technologies for rehabilitation–a study using the unified theory of acceptance and use of technology (utaut). Disabil. Rehabil. 2015, 37, 447–455. [Google Scholar] [CrossRef] [PubMed]
- Louie, D.R.; Bird, M.L.; Menon, C.; Eng, J.J. Perspectives on the prospective development of stroke-specific lower extremity wearable monitoring technology: A qualitative focus group study with physical therapists and individuals with stroke. J. Neuroeng. Rehabil. 2020, 17, 31. [Google Scholar] [CrossRef]
- Papi, E.; Murtagh, G.M.; McGregor, A.H. Wearable technologies in osteoarthritis: A qualitative study of clinicians’ preferences. BMJ Open 2016, 6, e009544. [Google Scholar] [CrossRef] [Green Version]
- Hamilton, C.; McCluskey, A.; Hassett, L.; Killington, M.; Lovarini, M. Patient and therapist experiences of using affordable feedback-based technology in rehabilitation: A qualitative study nested in a randomized controlled trial. Clin. Rehabil. 2018, 32, 1258–1270. [Google Scholar] [CrossRef]
- Rogers, E.M. Diffusion of innovations: Modifications of a model for telecommunications. In Die Diffusion von Innovationen in der Telekommunikation; Springer: Berlin/Heidelberg, Germany, 1995; pp. 25–38. [Google Scholar]
- Kononova, A.; Li, L.; Kamp, K.; Bowen, M.; Rikard, R.V.; Cotten, S.; Peng, W. The use of wearable activity trackers among older adults: Focus group study of tracker perceptions, motivators, and barriers in the maintenance stage of behavior change. JMIR Mhealth Uhealth 2019, 7, e9832. [Google Scholar] [CrossRef] [PubMed]
- Likert, R. A technique for the measurement of attitudes. Arch. Psychol. 1932, 22, 44–53. [Google Scholar]
- Bryer, J.; Speerschneider, K.; Bryer, M.J. Package ‘likert’. In Analysis and Visualization Likert Items. CRAN; Institute for Statistics and Mathematics; Vienna University of Economics and Business: Vienna, Austria, 2016. [Google Scholar]
- Pak, P.; Jawed, H.; Tirone, C.; Lamb, B.; Cott, C.; Brunton, K.; Mansfield, A.; Inness, E.L. Incorporating research technology into the clinical assessment of balance and mobility: Perspectives of physiotherapists and people with stroke. Physiother. Can. 2015, 67, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Farivar, S.; Abouzahra, M.; Ghasemaghaei, M. Wearable device adoption among older adults: A mixed-methods study. Int. J. Inf. Manag. 2020, 55, 102209. [Google Scholar] [CrossRef]
- Mercer, K.; Giangregorio, L.; Schneider, E.; Chilana, P.; Li, M.; Grindrod, K. Acceptance of commercially available wearable activity trackers among adults aged over 50 and with chronic illness: A mixed-methods evaluation. JMIR Mhealth Uhealth 2016, 4, e7. [Google Scholar] [CrossRef]
- Brouns, B.; Meesters, J.J.L.; Wentink, M.M.; de Kloet, A.J.; Arwert, H.J.; Vliet Vlieland, T.P.M.; Boyce, L.W.; van Bodegom-Vos, L. Why the uptake of erehabilitation programs in stroke care is so difficult-a focus group study in the netherlands. Implement. Sci. 2018, 13, 133. [Google Scholar] [CrossRef] [Green Version]
- Saywell, N.; Taylor, D. Focus group insights assist trial design for stroke telerehabilitation: A qualitative study. Physiother. Theory Pract. 2015, 31, 160–165. [Google Scholar] [CrossRef]
- Chen, C.C.; Bode, R.K. Factors influencing therapists’ decision-making in the acceptance of new technology devices in stroke rehabilitation. Am. J. Phys. Med. Rehabil. 2011, 90, 415–425. [Google Scholar] [CrossRef]
- Shin, G.; Jarrahi, M.H.; Fei, Y.; Karami, A.; Gafinowitz, N.; Byun, A.; Lu, X. Wearable activity trackers, accuracy, adoption, acceptance and health impact: A systematic literature review. J. Biomed Inform. 2019, 93, 103153. [Google Scholar] [CrossRef] [PubMed]
- Lynch, E.A.; Jones, T.M.; Simpson, D.B.; Fini, N.A.; Kuys, S.S.; Borschmann, K.; Kramer, S.; Johnson, L.; Callisaya, M.L.; Mahendran, N.; et al. Activity monitors for increasing physical activity in adult stroke survivors. Cochrane Database Syst. Rev. 2018, 7, Cd012543. [Google Scholar] [CrossRef] [PubMed]
- Bagot, K.L.; Moloczij, N.; Barclay-Moss, K.; Vu, M.; Bladin, C.F.; Cadilhac, D.A. Sustainable implementation of innovative, technology-based health care practices: A qualitative case study from stroke telemedicine. J. Telemed. Telecare 2020, 26, 79–91. [Google Scholar] [CrossRef] [PubMed]
- Urquhart, R.; Kendell, C.; Cornelissen, E.; Madden, L.L.; Powell, B.J.; Kissmann, G.; Richmond, S.A.; Willis, C.; Bender, J.L. Defining sustainability in practice: Views from implementing real-world innovations in health care. BMC Health Serv. Res. 2020, 20, 87. [Google Scholar] [CrossRef] [PubMed]



| Total (n = 103) | Users (n = 28) (27%) | Non-Users (n = 75) (73%) | p-Value | ||
|---|---|---|---|---|---|
| Age, mean (SD) | 42.2 (12.06) | 41.70 (13.24) | 45.30 (12.11) | 0.212 | |
| Gender (m/f) | 26/76 | 8/20 | 18/56 | 0.420 | |
| Years of work Experience, n (%) | <5 | 9 (8.7%) | 2 (7.1%) | 7 (9.3%) | 0.331 |
| 5–10 | 18 (17.5%) | 8 (28.6%) | 10 (13.3%) | ||
| 10–15 | 22 (21.4%) | 7 (25.0%) | 15 (20.0%) | ||
| 15–20 | 7 (6.8%) | 2 (7.1%) | 5 (6.7%) | ||
| >20 years | 47 (45.6%) | 9 (32.1%) | 38 (50.7%) | ||
| Setting a (n) | Primary care | 34 | 7 | 27 | |
| Rehabilitation | 59 | 21 | 38 | ||
| Geriatric care | 20 | 2 | 18 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Braakhuis, H.E.M.; Bussmann, J.B.J.; Ribbers, G.M.; Berger, M.A.M. Wearable Activity Monitoring in Day-to-Day Stroke Care: A Promising Tool but Not Widely Used. Sensors 2021, 21, 4066. https://doi.org/10.3390/s21124066
Braakhuis HEM, Bussmann JBJ, Ribbers GM, Berger MAM. Wearable Activity Monitoring in Day-to-Day Stroke Care: A Promising Tool but Not Widely Used. Sensors. 2021; 21(12):4066. https://doi.org/10.3390/s21124066
Chicago/Turabian StyleBraakhuis, Hanneke E. M., Johannes B. J. Bussmann, Gerard M. Ribbers, and Monique A. M. Berger. 2021. "Wearable Activity Monitoring in Day-to-Day Stroke Care: A Promising Tool but Not Widely Used" Sensors 21, no. 12: 4066. https://doi.org/10.3390/s21124066
APA StyleBraakhuis, H. E. M., Bussmann, J. B. J., Ribbers, G. M., & Berger, M. A. M. (2021). Wearable Activity Monitoring in Day-to-Day Stroke Care: A Promising Tool but Not Widely Used. Sensors, 21(12), 4066. https://doi.org/10.3390/s21124066






