Gait Analysis in Children with Cerebral Palsy: Are Plantar Pressure Insoles a Reliable Tool?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participants Selection
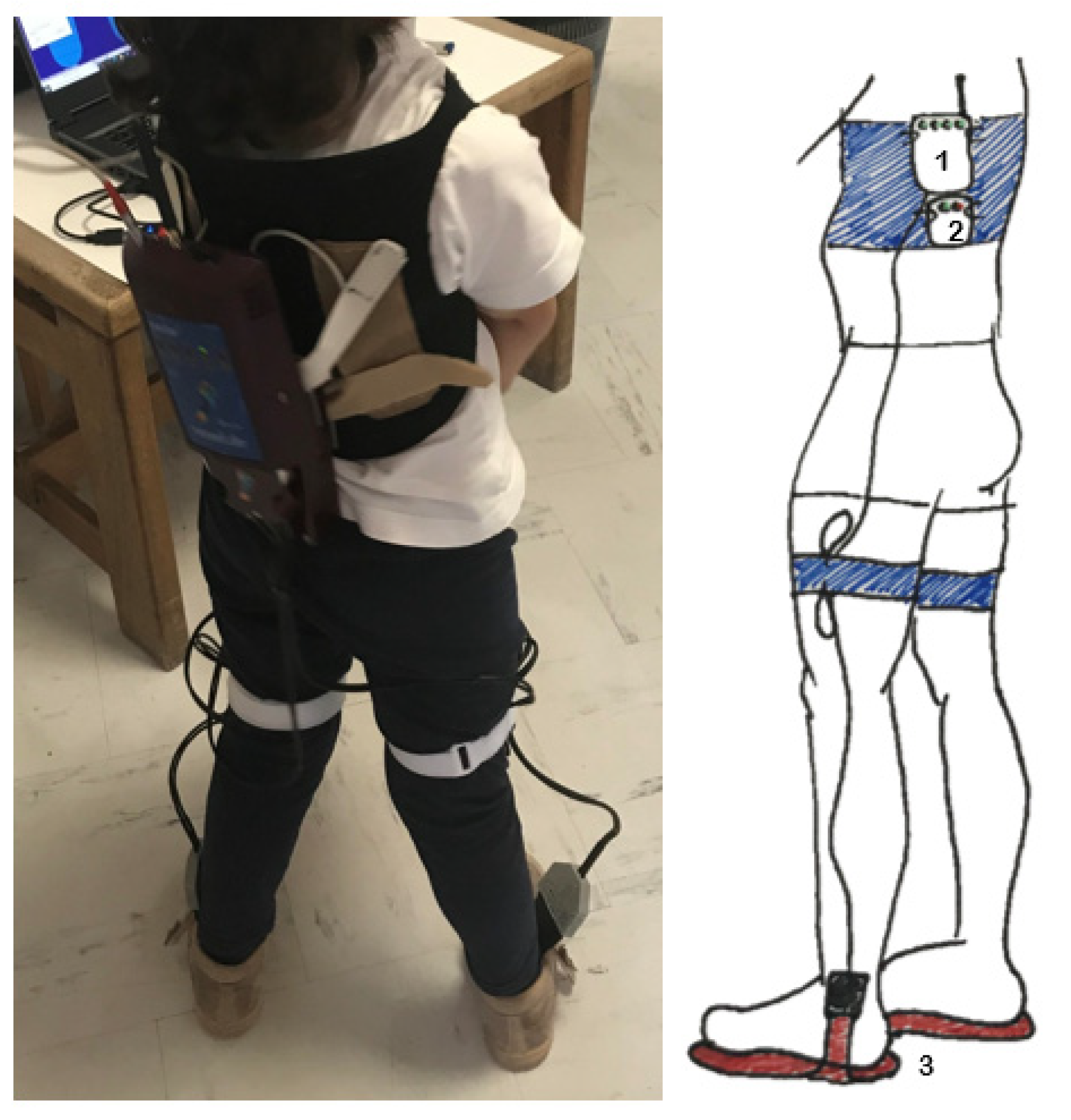
2.3. Data Collection Protocol
2.4. Data Processing
2.5. Statistical Analysis
3. Results
3.1. Reliability of Whole Foot Measurements
3.2. Reliability of Segmented Foot Measurements
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Eunson, P. Aetiology and epidemiology of cerebral palsy. Paediatr. Child Health 2012, 22, 361–366. [Google Scholar] [CrossRef]
- Graham, H.K.; Rosenbaum, P.; Paneth, N.; Dan, B.; Lin, J.-P.; Damiano, D.L.; Becher, J.G.; Gaebler-Spira, D.; Colver, A.; Reddihough, D.S.; et al. Cerebral palsy. Nat. Rev. Dis. Primers 2016, 2, 15082. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, P.; Paneth, N.; Leviton, A.; Goldstein, M.; Bax, M.; Damiano, D.; Dan, B.; Fabiola, R.; Jacobsson, B. A report: The definition and classification of cerebral palsy April 2006 Peter Rosenbaum (Definition Panel Chair) MD. Dev. Med. Child Neurol. 2007, 49, 8–14. [Google Scholar]
- Colver, A.; Fairhurst, C.; Pharoah, P.O.D.; Hospital, C. Cerebral palsy. Lancet 2014, 383, 1240–1249. [Google Scholar] [CrossRef]
- Maenner, M.J.; Blumberg, S.J.; Kogan, M.D.; Christensen, D.; Yeargin-allsopp, M.; Schieve, L.A. Prevalence of cerebral palsy and intellectual disability among children identified in two U.S. national surveys, 2011–2013. Ann. Epidemiol. 2016, 26, 222–226. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Graham, H.K.; Selber, P. Musculoskeletal aspects of cerebral palsy. J. Bone Jt. Surg. Ser. B 2003, 85, 157–166. [Google Scholar] [CrossRef]
- Galli, M.; Cimolin, V.; Pau, M.; Leban, B.; Brunner, R.; Albertini, G. Foot pressure distribution in children with cerebral palsy while standing. Res. Dev. Disabil. 2015, 41–42, 52–57. [Google Scholar] [CrossRef]
- Kedem, P.; Scher, D.M. Foot deformities in children with cerebral palsy. Curr. Opin. Pediatr. 2015, 27, 67–74. [Google Scholar] [CrossRef]
- Gage, J.R.; Schwartz, M.H.; Koop, S.E.; Novacheck, T.F. Patient Assessment—Introduction and Overview; Mac Keith Press: London, UK, 2009; Volume 58, ISBN 9781909962347. [Google Scholar]
- Yeo, S.S.; Park, G.Y. Accuracy Verification of Spatio-Temporal and Kinematic Parameters for Gait Using Inertial Measurement Unit System. Sensors 2020, 20, 1343. [Google Scholar] [CrossRef] [Green Version]
- Glowinski, S.; Blazejewski, A.; Krzyzynski, T. Inertial sensors and wavelets analysis as a tool for pathological gait identification. Adv. Intell. Syst. Comput. 2017, 526, 106–114. [Google Scholar] [CrossRef]
- Chow, T.H. Traceable Features of Static Plantar Pressure Characteristics and Foot Postures in College Students with Hemiplegic Cerebral Palsy. J. Pers. Med. 2022, 12, 394. [Google Scholar] [CrossRef]
- Chang, W.-D.; Chang, N.-J.; Lin, H.-Y.; Lai, P.-T. Changes of Plantar Pressure and Gait Parameters in Children with Mild Cerebral Palsy Who Used a Customized External Strap Orthosis: A Crossover Study. BioMed Res. Int. 2015, 2015, 813942. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Riad, J.; Coleman, S.; Henley, J.; Miller, F. Reliability of pediobarographs for paediatric foot deformity. J. Child. Orthop. 2007, 1, 307–312. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stebbins, J.; Harrington, M.; Giacomozzi, C.; Thompson, N.; Zavatsky, A.; Theologis, T. Assessment of sub-division of plantar pressure measurement in children. Gait Posture 2005, 22, 372–376. [Google Scholar] [CrossRef] [PubMed]
- Hafer, J.F.; Lenhoff, M.W.; Song, J.; Jordan, J.M.; Hannan, M.T.; Hillstrom, H.J. Reliability of plantar pressure platforms. Gait Posture 2013, 38, 544–548. [Google Scholar] [CrossRef] [Green Version]
- Niiler, T.; Church, C.; Lennon, N.; Henley, J.; George, A.; Taylor, D.; Montes, A.; Miller, F. The Foot Reliability and minimal detectable change in foot pressure measurements in typically developing children. Foot 2016, 29, 29–35. [Google Scholar] [CrossRef]
- Alvarez, C.; De Vera, M.; Chhina, H.; Black, A. Normative data for the dynamic pedobarographic profiles of children. Gait Posture 2008, 28, 309–315. [Google Scholar] [CrossRef]
- Dulai, S.; Ramadi, A.; Lewicke, J.; Watkins, B.; Prowse, M.; Vette, H. Functional characterization of plantar pressure patterns in gait of typically developing children using dynamic pedobarography. Gait Posture 2021, 84, 267–272. [Google Scholar] [CrossRef]
- Kasovi, M.; Štefan, L.; Zvonár, M. Foot characteristics during walking in 6–14 year-old children. Sci. Rep. 2020, 10, 950. [Google Scholar] [CrossRef]
- Femery, V.; Moretto, P.; Renaut, H.; Thévenon, A. Spasticité et distribution des pressions plantaires chez des enfants atteints d ’ hémiplégie cérébrale infantile. Ann. Readapt. Med. Phys. 2001, 44, 26–34. [Google Scholar] [CrossRef]
- Femery, V.; Moretto, P.; Renaut, H.; Thévenon, A.; Lensel, G. Measurement of plantar pressure distribution in hemiplegic children: Changes to adaptative gait patterns in accordance with deficiency. Clin. Biomech. 2002, 17, 406–413. [Google Scholar] [CrossRef]
- Buldt, A.A.K.; Allan, J.J.; Landorf, K.B.; Menz, H.B. The relationship between foot posture and plantar pressure during walking in adults: A systematic review. Gait Posture 2018, 62, 56–67. [Google Scholar] [CrossRef]
- Godi, M.; Turcato, A.M.; Schieppati, M.; Nardone, A. Test-retest reliability of an insole plantar pressure system to assess gait along linear and curved trajectories. J. Neuroeng. Rehabil. 2014, 11, 95. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palisano, R.J.; Hanna, S.E.; Russell, D.J.; Walter, S.D.; Wood, E.P.; Raina, P.S.; Galuppi, B.E. Validation of a Model of Gross Motor Function for Children With. Phys. Ther. 2000, 80, 975–985. [Google Scholar] [CrossRef] [Green Version]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fernandes, R.; Armada-da-silva, P.; Pool-goudaazward, A.; Moniz-pereira, V. Test-retest reliability and minimal detectable change of three-dimensional gait analysis in chronic low back pain patients. Gait Posture 2015, 42, 491–497. [Google Scholar] [CrossRef]
- Ricardo, D.; Teles, J.; Raposo, M.R.; João, F. Test-Retest Reliability of a 6DoF Marker Set for Gait Analysis in Cerebral Palsy Children. Appl. Sci. 2021, 11, 6515. [Google Scholar] [CrossRef]
- Li, L.; Zeng, L.; Lin, Z.-J.; Cazzell, M.; Liu, H. Tutorial on use of intraclass correlation coefficients for assessing intertest reliability and its application in functional near-infrared spectroscopy-based brain imaging. J. Biomed. Opt. 2015, 20, 050801. [Google Scholar] [CrossRef]
- Rodda, J.; Graham, H.K. Classification of gait patterns in spastic hemiplegia and spastic diplegia: A basis for a management algorithm. Eur. J. Neurol. 2001, 8, 98–108. [Google Scholar] [CrossRef]
- Rodda, J.M.; Graham, H.K.; Carson, L.; Galea, M.P.; Wolfe, R. Sagittal gait patterns in spastic diplegia. J. Bone Jt. Surg. Ser. B 2004, 86, 251–258. [Google Scholar] [CrossRef]
- Harb, A.; Kishner, S. Modified Ashworth Scale; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Cousins, S.D.; Morrison, S.C.; Drechsler, W.I. The reliability of plantar pressure assessment during barefoot level walking in children aged 7–11 years. J. Foot Ankle Res. 2012, 5, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bickley, A.C.; Linton, J.; Sullivan, E.; Mitchell, K.; Slota, G.; Barnes, D. Comparison of Simultaneous Static Standing Balance Data on a Pressure Mat and Force Plate in Typical Children and in Children with Cerebral Palsy. Gait Posture 2018, 67, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Team, R.C. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2022. [Google Scholar]
- Rathbone, A.; Shaw, S.; Kumbhare, D.; Rathbone, M.A. “ICC.Sample.Size.” Package, 1.0. 2015. Available online: https://CRAN.R-project.org/package=ICC.Sample.Size (accessed on 13 June 2022).
- Ayán-pérez, C.; Bouzas-rico, S. Test-retest reliability of the Wii Balance Board for assessing standing balance in young people with intellectual disability. Int. J. Dev. Disabil. 2019, 65, 231–238. [Google Scholar] [CrossRef]
- Llorens, R.; Latorre, J.; Noé, E.; Keshner, E.A. Posturography using the Wii Balance BoardTM. A feasibility study with healthy adults and adults post-stroke. Gait Posture 2016, 43, 228–232. [Google Scholar] [CrossRef] [Green Version]
- Blomqvist, S.; Wester, A.; Sundelin, G.; Rehn, B. Test-retest reliability, smallest real difference and concurrent validity of six different balance tests on young people with mild to moderate intellectual disability. Physiotherapy 2012, 98, 313–319. [Google Scholar] [CrossRef]


| Participant | Gender | Age (Months) | Diagnosis | Affected Side | GMFCS Level [25] | Interval between Trials (Days) | Mass (kg) | Height (cm) | Sagittal Gait Pattern [30,31] | Gastrocnemius Spasticity (Modified Ashworth Scale) [32] | Foot Length (cm) | Number of Steps (Average from Both Trials) | Status | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Right | Left | Right | Left | Right | Left | Right | Left | ||||||||||
| 001 | Male | 54 | Unilateral CP | Right | I | 14 | 16.5 | 105 | Drop Foot | - | 1 | 0 | 15 | 16 | 70 | 70 | Completed trials |
| 002 | Male | 65 | Unilateral CP | Left | II | 9 | 20 | 118 | - | True Equinus | 0 | 4 | 19 | 17 | 52 | 59 | Completed trials |
| 003 | Female | 41 | Unilateral CP | Right | II | 7 | 19 | 105 | True Equinus | - | 1+ | 0 | 16 | 17 | 55 | 52 | Completed trials |
| 004 | Female | 56 | Bilateral CP | Both | II | 7 | 18 | 110 | Apparent Equinus | Apparent Equinus | 1 | 1 | 17 | 17 | 55 | 55 | Completed trials |
| 005 | Female | 65 | Unilateral CP | Right | I | 7 | 20.4 | 120 | True Equinus | - | 1 | 0 | 20 | 19 | 64 | 65 | Completed trials |
| 006 | Male | 45 | Unilateral CP | Left | I | - | 13 | 97 | - | True Equinus | 0 | 1 | 15 | 15 | - | Dropped out | |
| 007 | Male | 41 | Unilateral CP | Right | I | - | 16 | 103 | True Equinus | - | 1 | 0 | 15 | 16 | - | Dropped out | |
| 008 | Male | 74 | Unilateral CP | Right | I | 7 | 20.5 | 115 | True Equinus | - | 1 | 0 | 20 | 20 | 75 | 74 | Completed trials |
| 009 | Male | 80 | Unilateral CP | Right | I | 6 | 20.1 | 115 | True Equinus | - | 1+ | 0 | 19 | 19 | 122 | 120 | Completed trials |
| 010 | Female | 58 | Unilateral CP | Right | I | 7 | 17 | 116 | Equinus/Jump Knee | - | 2 | 0 | 16 | 18 | 112 | 119 | Completed trials |
| Pedobarograpy Measurements | ICC | ICC 95% CI | Mean | Mean Diff | SD Diff | 95% LOA | SEM | MDC |
|---|---|---|---|---|---|---|---|---|
| Force–time integral (N·s) | 0.76 | (0.30; 0.92) | 73.72 | −2.08 | 18.57 | (−38.47; 34.31) | 13.13 | 36.39 |
| Pressure–time integral (kPa·s) | 0.89 | (0.70; 0.96) | 55.40 | 0.63 | 10.04 | (−19.05; 20.31) | 7.10 | 19.68 |
| Maximum force (N) | 0.79 | (0.42; 0.93) | 161.30 | −7.61 | 25.00 | (−56.61; 41.40) | 17.68 | 49.00 |
| Peak pressure (kPa) | 0.81 | (0.47; 0.93) | 136.45 | 6.84 | 27.48 | (−47.01; 60.70) | 19.43 | 53.85 |
| Contact area (cm2) | 0.83 | (0.53; 0.94) | 56.80 | −3.69 | 8.15 | (−19.66; 12.27) | 5.76 | 15.97 |
| Contact time (ms) | 0.37 | (0; 0.78) | 669.93 | 4.29 | 137.30 | (−264.81; 273.40) | 97.08 | 269.11 |
| Pedobarograpy Measurements | ICC | ICC 95% CI | Mean | Mean Diff | SD Diff | 95% LOA | SEM | MDC | |
|---|---|---|---|---|---|---|---|---|---|
| Hindfoot | Force–time integral (N·s) | 0.83 | (0.51; 0.94) | 17.44 | −1.43 | 11.35 | (−23.67; 20.82) | 8.02 | 22.24 |
| Pressure–time integral (kPa·s) | 0.97 | (0.92; 0.99) | 21.41 | 0.62 | 12.01 | (−22.93; 24.16) | 8.49 | 23.54 | |
| Maximum force (N) | 0.92 | (0.77; 0.97) | 70.50 | −6.38 | 28.65 | (−62.53; 49.77) | 20.26 | 56.15 | |
| Peak pressure (kPa) | 0.88 | (0.65; 0.96) | 78.56 | −3.84 | 18.48 | (−40.06; 32.37) | 13.07 | 36.22 | |
| Contact area (cm2) | 0.91 | (0.75; 0.97) | 13.68 | −1.76 | 6.19 | (−13.89; 10.36) | 4.38 | 12.13 | |
| Contact time (ms) | 0.86 | (0.62; 0.95) | 365.79 | 38.16 | 272.29 | (−495.53; 571.85) | 192.54 | 533.69 | |
| Middle Foot | Force–time integral (N·s) | 0.91 | (0.75; 0.97) | 15.32 | 0.52 | 3.14 | (−5.63; 6.67) | 2.22 | 6.15 |
| Pressure–time integral (kPa·s) | 0.97 | (0.92; 0.99) | 30.19 | 0.91 | 5.95 | (−10.75; 12.57) | 4.21 | 11.66 | |
| Maximum force (N) | 0.91 | (0.74; 0.97) | 47.92 | −2.32 | 7.84 | (−17.69; 13.05) | 5.54 | 15.37 | |
| Peak pressure (kPa) | 0.97 | (0.92; 0.99) | 74.89 | 1.19 | 8.31 | (−15.09; 17.47) | 5.87 | 16.28 | |
| Contact area (cm2) | 0.98 | (0.94; 0.99) | 16.54 | −0.34 | 2.07 | (−4.39; 3.72) | 1.46 | 4.06 | |
| Contact time (ms) | 0.73 | (0.25; 0.90) | 621.32 | 9.79 | 118.82 | (−223.09; 242.67) | 84.02 | 232.88 | |
| Forefoot | Force–time integral (N·s) | 0.73 | (0.25; 0.90) | 40.95 | −1.18 | 11.14 | (−23.02; 20.66) | 7.88 | 21.84 |
| Pressure–time integral (kPa·s) | 0.97 | (0.92; 0.99) | 42.35 | 1.53 | 7.30 | (−12.77; 15.83) | 5.16 | 14.30 | |
| Maximum force (N) | 0.73 | (0.26; 0.90) | 123.44 | −5.93 | 23.40 | (−51.80; 39.95) | 16.55 | 45.87 | |
| Peak pressure (kPa) | 0.44 | (0; 0.81) | 124.59 | 8.68 | 28.00 | (−46.19; 63.55) | 19.80 | 54.87 | |
| Contact area (cm2) | 0.68 | (0.07; 0.89) | 25.59 | −3.57 | 7.21 | (−17.70; 10.55) | 5.10 | 14.12 | |
| Contact time (ms) | 0.55 | (0; 0.85) | 578.39 | 22.66 | 194.57 | (−358.70; 404.02) | 137.58 | 381.36 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raposo, M.R.; Ricardo, D.; Teles, J.; Veloso, A.P.; João, F. Gait Analysis in Children with Cerebral Palsy: Are Plantar Pressure Insoles a Reliable Tool? Sensors 2022, 22, 5234. https://doi.org/10.3390/s22145234
Raposo MR, Ricardo D, Teles J, Veloso AP, João F. Gait Analysis in Children with Cerebral Palsy: Are Plantar Pressure Insoles a Reliable Tool? Sensors. 2022; 22(14):5234. https://doi.org/10.3390/s22145234
Chicago/Turabian StyleRaposo, Maria Raquel, Diogo Ricardo, Júlia Teles, António Prieto Veloso, and Filipa João. 2022. "Gait Analysis in Children with Cerebral Palsy: Are Plantar Pressure Insoles a Reliable Tool?" Sensors 22, no. 14: 5234. https://doi.org/10.3390/s22145234
APA StyleRaposo, M. R., Ricardo, D., Teles, J., Veloso, A. P., & João, F. (2022). Gait Analysis in Children with Cerebral Palsy: Are Plantar Pressure Insoles a Reliable Tool? Sensors, 22(14), 5234. https://doi.org/10.3390/s22145234






