Development of an Obesity Information Diagnosis Model Reflecting Body Type Information Using 3D Body Information Values
Abstract
:1. Introduction
2. Literature Review
2.1. Obesity Diagnosis Method
2.2. Importance and Necessity of Accurate Diagnosis of Obesity Information
2.3. Body Image Distortion
2.4. Importance of Dimensional Awaresness
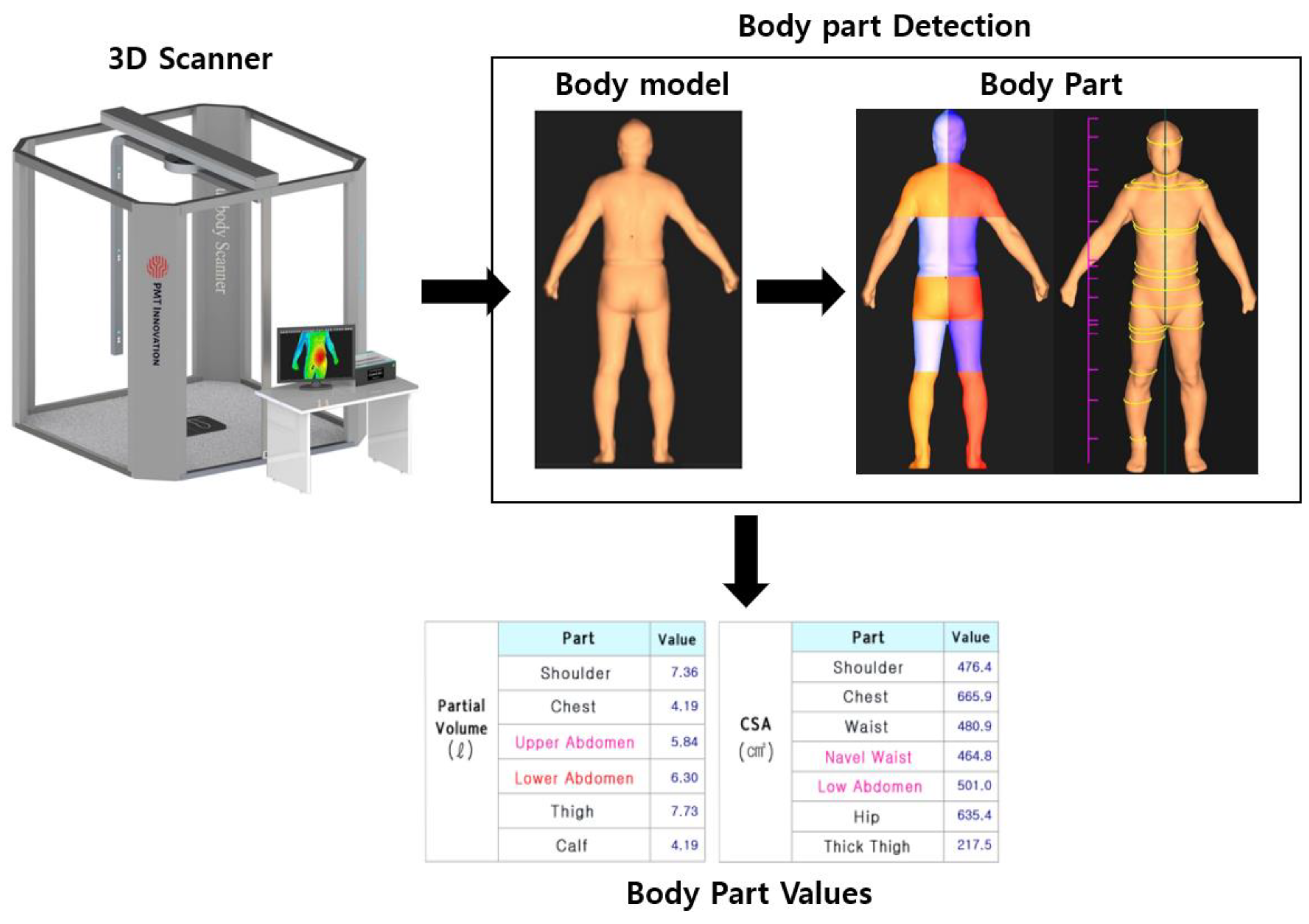
3. Materials and Methods
3.1. Data Selection
3.2. Data Preprocessing
3.3. Data Analysis
4. Results
5. Conclusions and Future Research
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lee, K.; Shin, D. Relationships of Dietary Factors with Obesity, Hypertension, and Diabetes by Regional Type among Single-Person Households in Korea. Nutrients 2021, 13, 1218. [Google Scholar] [CrossRef] [PubMed]
- Bae, Y.-J.; Yu, K.-W.; Lee, K.-H.; Jang, K.-I. Association of the Healthy Eating Index with Metabolic Abnormalities among Middle-Aged Adults Living in Single-Person Households in Korea. Nutrients 2021, 13, 3937. [Google Scholar] [CrossRef] [PubMed]
- Finkelstein, E.A.; Khavjou, O.A.; Thompson, H.; Trogdon, J.G.; Pan, L.; Sherry, B.; Dietz, W. Obesity and Severe Obesity Forecasts Through 2030. Am. J. Prev. Med. 2012, 42, 563–570. [Google Scholar] [CrossRef]
- Bray, G.A. Obesity: The disease. J. Med. Chem. 2006, 49, 4001–4007. [Google Scholar] [CrossRef] [PubMed]
- Thombs, B.D.; Saadat, N.; Riehm, K.E.; Karter, J.M.; Karter, A.; Andrews, B.K.; Simons, P.; Simons, L. Consistency and sources of divergence in recommendations on screening with questionnaires for presently experienced health problems or symptoms: A comparison of recommendations from the Canadian Task Force on Preventive Health Care, UK National Screening Committee, and US Preventive Services Task Force. BMC Med. 2017, 15, 150. [Google Scholar]
- Kim, K.B.; Han, K.H. A study of the digital healthcare industry in the fourth industrial revolution. J. Converg. Inf. Technol. 2020, 10, 7–15. [Google Scholar]
- Blüher, S.; Molz, E.; Wiegand, S.; Otto, K.-P.; Sergeyev, E.; Tuschy, S.; L’Allemand-Jander, D.; Kiess, W.; Holl, R.W.; Adiposity Patients Registry Initiative and German Competence Net Obesity. Body mass index, waist circumference, and waist-to-height ratio as predictors of cardiometabolic risk in childhood obesity depending on pubertal development. J. Clin. Endocrinol. Metab. 2013, 98, 3384–3393. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lam, B.C.C.; Koh, C.H.G.; Chen, C.; Wong, M.T.K.; Fallows, S.J. Comparison of Body Mass Index (BMI), Body Adiposity Index (BAI), Waist Circumference (WC), Waist-To-Hip Ratio (WHR) and Waist-To-Height Ratio (WHtR) as Predictors of Cardiovascular Disease Risk Factors in an Adult Population in Singapore. PLoS ONE 2015, 10, e0122985. [Google Scholar] [CrossRef]
- Malbrain, M.L.; Huygh, J.; Dabrowski, W.; De Waele, J.J.; Staelens, A.; Wauters, J. The use of bio-electrical impedance analysis (BIA) to guide fluid management, resuscitation and deresuscitation in critically ill patients: A bench-to-bedside review. Anaesthesiol. Intensiv. Ther. 2014, 46, 381–391. [Google Scholar] [CrossRef] [PubMed]
- Haarbo, J.; Gotfredsen, A.; Hassager, C.; Christiansen, C. Validation of body composition by dual energy X-ray absorptiometry (DEXA). Clin. Physiol. 1991, 11, 331–341. [Google Scholar] [CrossRef]
- Gurunathan, U.; Myles, P.S. Limitations of body mass index as an obesity measure of perioperative risk. Br. J. Anaesth. 2016, 116, 319–321. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deurenberg, P. Limitations of the bioelectrical impedance method for the assessment of body fat in severe obesity. Am. J. Clin. Nutr. 1996, 64, 449S–452S. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.M.Y.; Huxley, R.R.; Wildman, R.P.; Woodward, M. Indices of abdominal obesity are better discriminators of cardiovascular risk factors than BMI: A meta-analysis. J. Clin. Epidemiol. 2008, 61, 646–653. [Google Scholar] [CrossRef]
- Wiltink, J.; Michal, M.; Wild, P.S.; Zwiener, I.; Blettner, M. Associations between depression and different measures of obesity (BMI, WC, WHtR, WHR). BMC Psychiatry 2013, 13, 223. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mokha, J.S.; Srinivasan, S.R.; Dasmahapatra, P.; Fernandez, C.; Fernandez, W.; Xu, J.; Berenson, G.S. Utility of waist-to-height ratio in assessing the status of central obesity and related cardiometabolic risk profile among normal weight and overweight/obese children: The Bogalusa Heart Study. BMC Pediatr. 2010, 10, 73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jeong, S.-M.; Yoh, E. Consumer characteristics of Body Mass Index groups, and the effect of body satisfaction and self-esteem on the involvement in dieting among females aged 25–49 years. Res. J. Costume Cult. 2020, 28, 591–606. [Google Scholar] [CrossRef]
- Jonnalagadda, S.S.; Skinner, R.; Moore, L. Overweight athlete: Fact or fiction? Curr. Sport. Med. Rep. 2004, 3, 198–205. [Google Scholar] [CrossRef] [PubMed]
- Hamdy, O.; Porramatikul, S.; Al-Ozairi, E. Metabolic obesity: The paradox between visceral and subcutaneous fat. Curr. Diabetes Rev. 2006, 2, 367–373. [Google Scholar] [PubMed]
- Maffeis, C.; Banzato, C.; Talamini, G.; Obesity Study Group of the Italian Society of Pediatric Endocrinology and Diabetology. Waist–to–Height Ratio, a Useful Index to Identify High Metabolic Risk in Overweight Children. J. Pediatr. 2008, 152, 207–213.e2. [Google Scholar] [CrossRef]
- Bachrach, L.K. Dual energy X-ray absorptiometry (DEXA) measurements of bone density and body composition: Promise and pitfalls. J. Pediatr. Endocrinol. Metab. 2000, 13, 983–988. [Google Scholar] [PubMed]
- Browning, L.M.; Mugridge, O.; Dixon, A.K.; Aitken, S.W.; Prentice, A.M.; Jebb, S.A. Measuring abdominal adipose tissue: Comparison of simpler methods with MRI. Obes. Facts 2011, 4, 9–15. [Google Scholar] [CrossRef]
- Thomas, A.D. Study of Health Traits and Relative Values Using Simulation. Master’s Thesis, University of Guelph, Guelph, ON, Canada, 2011. [Google Scholar]
- Peterson, C.M.; Su, H.; Thomas, D.M.; Heo, M.; Golnabi, A.H.; Pietrobelli, A.; Heymsfield, S.B. Tri-Ponderal Mass Index vs Body Mass Index in Estimating Body Fat During Adolescence. JAMA Pediatr. 2017, 171, 629–636. [Google Scholar] [CrossRef]
- Woolcott, O.O.; Bergman, R.N. Relative fat mass (RFM) as a new estimator of whole-body fat percentage—A cross-sectional study in American adult individuals. Sci. Rep. 2018, 8, 10980. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hart, P.D.; Buck, D.J. The effect of resistance training on health-related quality of life in older adults: Systematic review and meta-analysis. Health Promot. Perspect. 2019, 9, 1. [Google Scholar] [CrossRef] [Green Version]
- Krakauer, N.Y.; Krakauer, J.C. A New Body Shape Index Predicts Mortality Hazard Independently of Body Mass Index. PLoS ONE 2012, 7, e39504. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wong, J.C.; O’Neill, S.; Beck, B.R.; Forwood, M.R.; Khoo, S.K. Comparison of obesity and metabolic syndrome prevalence using fat mass index, body mass index and percentage body fat. PLoS ONE 2021, 16, e0245436. [Google Scholar] [CrossRef] [PubMed]
- Hosseini, S.A.; Padhy, R.K. Body Image Distortion; StatPearls Publishing: Tampa, FL, USA, 2021. [Google Scholar]
- Mable, H.M.; Balance, W.D.G.; Galgan, R.J. Body-Image Distortion and Dissatisfaction in University Students. Percept. Mot. Ski. 1986, 63, 907–911. [Google Scholar] [CrossRef]
- Yun, H.J. Effect of Body Image Distortion on Mental Health in Adolescents. J. Health Inform. Stat. 2018, 43, 191–199. [Google Scholar] [CrossRef] [Green Version]
- Brooks, K.R.; Mond, J.M.; Stevenson, R.J.; Stephen, I.D. Body image distortion and exposure to extreme body types: Contingent adaptation and cross adaptation for self and other. Front. Neurosci. 2016, 10, 334. [Google Scholar] [CrossRef] [Green Version]
- Mond, J.; Mitchison, D.; Latner, J.; Hay, P.; Owen, C.; Rodgers, B. Quality of life impairment associated with body dissatisfaction in a general population sample of women. BMC Public Health 2013, 13, 920. [Google Scholar] [CrossRef] [Green Version]
- Abdi, H.; Williams, L.J. Principal component analysis. Wiley Interdiscip. Rev. Comput. Stat. 2010, 2, 433–459. [Google Scholar] [CrossRef]
- Oliveros, E.; Somers, V.K.; Sochor, O.; Sochor, K.; Lopez-Jimenez, L. The concept of normal weight obesity. Prog. Cardiovasc. Dis. 2014, 56, 426–433. [Google Scholar] [CrossRef] [PubMed]
- Batsis, J.A.; Sahakyan, K.R.; Rodriguez-Escudero, J.P.; Bartels, S.J.; Somers, V.K.; Lopez-Jimenez, F. Normal Weight Obesity and Mortality in United States Subjects ≥60 Years of Age (from the Third National Health and Nutrition Examination Survey). Am. J. Cardiol. 2013, 112, 1592–1598. [Google Scholar] [CrossRef] [PubMed]
- Kapoor, N.; Lotfaliany, M.; Sathish, T.; Thankappan, K.R.; Thomas, N.; Furler, J.; Oldenburg, B.; Tapp, R.J. Prevalence of normal weight obesity and its associated cardio-metabolic risk factors—Results from the baseline data of the Kerala Diabetes Prevention Program (KDPP). PLoS ONE 2020, 15, e0237974. [Google Scholar] [CrossRef] [PubMed]
- Cockburn, A. Revisiting 2D vs 3D implications on spatial memory. In Proceedings of the Fifth Conference on Australasian User Interface—Volume 2004, Dunedin, New Zealand, 18–22 January 2004; pp. 25–31. [Google Scholar]
- Cockburn, A.; McKenzie, B. Evaluating the effectiveness of spatial memory in 2D and 3D physical and virtual environments. In Proceedings of the SIGCHI Conference on Human Factors in Computing Systems, Minneapolis, MN, USA, 20 April 2002; pp. 203–210. [Google Scholar]
- Srivastav, V.; Kadkhodamohammadi, A.; De Mathelin, M. MVOR: A multi-view RGB-D operating room dataset for 2D and 3D human pose estimation. arXiv 2018, arXiv:1808.08180. [Google Scholar]
- Chatzitofis, A.; Saroglou, L.; Boutis, P.; Drakoulis, P.; Zioulis, N.; Subramanyam, S.; Kevelham, B.; Charbonnier, C.; Cesar, P.; Zarpalas, D.; et al. Human4d: A Human-Centric Multimodal Dataset for Motions and Immersive Media. IEEE Access 2020, 8, 176241–176262. [Google Scholar] [CrossRef]
- MS ISO 7250; Basic Human Body Measurements for Technological Design (ISO 7250: 1996, IDT). Department of Standards Malaysia: Cyberjaya, Malaysia, 2003.
- Bracco, D.; Thiébaud, D.; Chioléro, R.; Landry, M.; Burckhardt, P.; Schutz, Y. Segmental body composition assessed by bioelectrical impedance analysis and DEXA in humans. J. Appl. Physiol. 1996, 81, 2580–2587. [Google Scholar] [CrossRef] [Green Version]
- Fuller, N.J.; Laskey, M.A.; Elia, M. Assessment of the composition of major body regions by dual-energy X-ray absorptiometry (DEXA), with special reference to limb muscle mass. Clin. Physiol. 1992, 12, 253–266. [Google Scholar] [CrossRef]
- Hong, S.; Oh, H.J.; Choi, H.; Kim, J.G.; Kil Lim, S.; Kim, E.K.; Pyo, E.Y.; Oh, K.; Kim, Y.T.; Wilson, K.; et al. Characteristics of Body Fat, Body Fat Percentage and Other Body Composition for Koreans from KNHANES IV. J. Korean Med. Sci. 2011, 26, 1599–1605. [Google Scholar] [CrossRef] [Green Version]
- Gallagher, D.; Heymsfield, S.B.; Heo, M.; Jebb, S.A.; Murgatroyd, P.R.; Sakamoto, Y. Healthy percentage body fat ranges: An approach for developing guidelines based on body mass index. Am. J. Clin. Nutr. 2000, 72, 694–701. [Google Scholar] [CrossRef] [Green Version]
- Available online: https://jaecwp2015.wordpress.com/ (accessed on 4 March 2015).
- Granato, D.; Santos, J.S.; Escher, G.B.; Ferreira, B.L.; Maggio, R.M. Use of principal component analysis (PCA) and hierarchical cluster analysis (HCA) for multivariate association between bioactive compounds and functional properties in foods: A critical perspective. Trends Food Sci. Technol. 2018, 72, 83–90. [Google Scholar] [CrossRef]
- Camacho, J.; Picó, J.; Ferrer, A. Data understanding with PCA: Structural and Variance Information plots. Chemom. Intell. Lab. Syst. 2010, 100, 48–56. [Google Scholar] [CrossRef]








| Collected Data | Explanation |
|---|---|
| Males (n = 87) | Height (cm) (Mean169.15/Max197/Min161) Weight (kg) (Mean 68.8/Max 120.6/Min 54.3) BMI (kg/m2) (Mean 23.35/ Max 16.6/Min 38.1) |
| Females (n = 73) | Height (cm) (Mean 162.8/Max 151/Min 175.7) Weight (kg) (Mean 56.6/Max 40.7/Min 89.6) BMI (kg/m2) (Mean 21/Max 16.2/Min 33.32) |
| 3D Scanner Variable Name | Explanation |
| Height | Participant height |
| Weight | Participant weight |
| Volume | Participant body volume |
| Chest length | Shoulder height–chest height |
| Shoulder height | Height from the floor to the shoulders in standing position |
| Chest height | Height from the floor to the top of the nipples and the beginning of the chest in standing position |
| Breast height | Height from the floor to nipples in the standing position |
| Waist length | Waist height–hip height |
| Waist height | Height from the floor to the point in front of the waist in standing position |
| Belly button height | Height from standing position to the navel |
| Height below the belly button | Height from standing position to the iliac bone below the navel |
| Hip length | Hip height–groin |
| Hip height | Height from the floor to hip protrusion in standing position |
| Groin height | Vertical height from the floor to the groin (actual leg length) |
| Thigh length | Hip height–groin height |
| Thick thigh height | Height from the floor to the thickest part of the thigh |
| Mid-thigh height | Height from the floor to the mid-thigh |
| Knee height | Vertical height from the floor to the top of the shinbone |
| Calf height | Height from the floor to the point of the thickest part of the calf |
| Neck circumference | Circumference passing under the back of the neck and under the shield cartilage |
| Shoulder circumference | Circumference from the end of the shoulder to the end of the shoulder opposite the back of the neck |
| Chest circumference | Horizontal circumference through the midpoint of the sternum |
| Breast circumference | Horizontal circumference through the nipple point |
| Waist circumference | Horizontal circumference passing through the point in the front of the waist, the point in the side of the waist, and the point in the back of the waist |
| Belly waist circumference | Horizontal circumference passing through the navel point, the navel level, the waist point, the waist level, and the back point |
| Circumference below the belly button | Horizontal circumference through the iliac crest below the navel |
| Hip circumference | Horizontal circumference passing through the buttock protrusion |
| Groin circumference | Groin circumference |
| Thick thigh circumference | The circumference of the thickest part of the innermost thigh |
| Mid-thigh circumference | Circumference of the middle of the thigh |
| Knee circumference | Horizontal circumference through the midpoint of the kneecap |
| Calf circumference | Circumference of the most convex part of the calf |
| Arm circumference | Circumference of the thickest part of the upper arm with the arm raised |
| Cross-sectional area of the back of the neck | Cross-sectional area of the back of the neck |
| Shoulder cross-section | Cross-sectional area of the shoulder end point opposite the back neck point from the shoulder end point |
| Chest area | Cross-sectional area of the part that passes through the midpoint of the sternum |
| Breast area | Cross-sectional area of the part that passes through the nipple point |
| Waist area | Cross-sectional area of the part that passes through the front of the waist, the side of the waist, and the back of the waist |
| Navel waist area | Cross-sectional area of the part that passes through the navel point, the navel level, the waist point, the waist level, and the back point |
| Below the navel area | Cross-sectional area of the part that passes through the iliac crest below the navel |
| Hip area | Cross-sectional area of the part that passes through the buttock protrusion |
| Groin area | Cross-sectional area of the groin |
| Thick thigh area | Cross-sectional area of the thickest part of the innermost thigh |
| Median thigh area | Cross-sectional area of the middle part of the thigh |
| Knee area | Cross-sectional area passing through the midpoint of the kneecap |
| Calf area | Cross-sectional area of the most convex part of the calf |
| Total volume | Total body volume |
| Shoulder volume | Total volume at shoulder height |
| Chest volume | Total volume at chest height |
| Epigastric volume | Total volume corresponding to the upper abdomen |
| Lower abdominal volume | Total volume corresponding to the lower abdomen |
| Thigh volume | Total volume at thigh height |
| Calf volume | Total volume equivalent to calf height |
| Total abdominal volume | Upper abdominal volume + lower abdominal volume |
| DEXA Variable Data | Explanation |
| Chest Tissue | Percentage of fat in tissue (=Fat (g)/Tissue (g)) |
| Android Tissue | Percentage of fat in tissue (=Fat (g)/Tissue (g)) |
| Gynoid Tissue | Percentage of fat in tissue (=Fat (g)/Tissue (g)) |
| Arm Tissue | Percentage of fat in tissue (=Fat (g)/Tissue (g)) |
| Leg Tissue | Percentage of fat in tissue (=Fat (g)/Tissue (g)) |
| Total Tissue | Percentage of fat in tissue (=Fat (g)/Tissue (g)) |
| Obesity Class | Men | Women |
|---|---|---|
| Underweight | 8% or less | 14% or less |
| Normal | More than 8%, less than 18.6% | More than 14%, less than 22.7% |
| Overweight | More than 18.6%, less than 23.1% | More than 22.7%, less than 27.1% |
| Obese | More than 23.1% | More than 27.1% |
| Body Part | Variables |
|---|---|
| Chest | Height, weight, chest length, shoulder area, chest area, breast area, shoulder volume, and chest volume |
| Abdomen | Height, weight, waist length, waist circumference, navel waist circumference, lower navel circumference, waist area, navel waist area, lower navel area, upper abdominal volume, and lower abdominal volume |
| Hips | Height, weight, hip length, hip circumference, groin circumference, hip area, and groin area |
| Arms/Legs | Height, weight, groin height, thigh length, knee height, calf height, thick thigh circumference, mid-thigh circumference, knee circumference, calf circumference, thick thigh area, mid-thigh area, knee area, calf area, and arm circumference |
| Men | ||||
|---|---|---|---|---|
| Body Part | Class 1 | Class 2 | Class 3 | Class 4 |
| Chest Abdomen Hips Arms/Legs | 8% or less | More than 8%, less than 18.6% | More than 18.6%, less than 23.1% | More than 23.1% |
| Women | ||||
| Body Part | Class 1 | Class 2 | Class 3 | Class 4 |
| Chest Abdomen Hips Arms/Legs | 14% or less | More than 14%, less than 22.7% | More than 22.7%, less than 27.1% | More than 27.1% |
| Men | |||||
|---|---|---|---|---|---|
| Eigenvalue percentage of variance | Comp 1 | Comp 2 | Comp 3 | Comp 4 | Comp 5 |
| Chest | 63.8301 | 15.631 | 11.801 | 6.501 | 1.408 |
| Abdomen | 61.424 | 18.083 | 12.752 | 5.194 | 1.849 |
| Hips | 79.498 | 12.125 | 5.63 | 1.646 | 0.579 |
| Arms/Legs | 60.3 | 25.5 | 6.1 | 3.8 | 2.8 |
| Women | |||||
| Eigenvalue percentage of variance | Comp 1 | Comp 2 | Comp 3 | Comp 4 | Comp 5 |
| Chest | 68.951 | 13.346 | 11.37 | 2.5 | 2.4 |
| Abdomen | 61.493 | 16.343 | 13.454 | 1.11 | 0.63 |
| Hips | 77.557 | 13.416 | 5.65 | 1.87 | 0.887 |
| Arms/Legs | 61.6 | 27.5 | 4.5 | 2.8 | 2.2 |
| Body Fat Percentage | Chest | Abdomen | Hips | Arms/Legs | |||||
|---|---|---|---|---|---|---|---|---|---|
| Type 1 | Type 2 | Type 1 | Type 2 | Type 1 | Type 2 | Type 1 | Type 2 | ||
| Under 8 | Mean | −1.97 | 0.25 | −2.95 | −0.46 | −4.56 | −0.87 | −5.05 | −2.08 |
| Median | −1.9 | −0.01 | −3.34 | −0.48 | −1.81 | 0.66 | −2.25 | 0.05 | |
| Min | −3.18 | −0.17 | −3.86 | −1.16 | −2.21 | −0.16 | −5.11 | −1.04 | |
| Max | −0.4 | 1.13 | −1.67 | 0.27 | −0.76 | 1.39 | 0.57 | 0.8 | |
| 8–18.6 | Mean | −1.39 | 0.1 | −2.42 | −0.14 | −3.25 | −0.54 | −2.69 | −0.61 |
| Median | −1 | 0.09 | −2.32 | −0.12 | −1.17 | −0.04 | −0.89 | 0.76 | |
| Min | −4.67 | −2.7 | −4.41 | −2.06 | −4.32 | −4.34 | −6.81 | −2.63 | |
| Max | 0.81 | 2.76 | −0.42 | 1.61 | 2.31 | 1.22 | 5.42 | 4.84 | |
| 18.6–23.1 | Mean | −0.5 | 0.15 | −2.14 | 0.42 | −2.03 | −0.26 | −1.79 | 0.27 |
| Median | −0.34 | 0.63 | −2.46 | 0.86 | −0.21 | −0.45 | −0.39 | −0.001 | |
| Min | −2.42 | −2.66 | −4.59 | −1.74 | −3.9 | −3.83 | −2.32 | −3.99 | |
| Max | 1.52 | 0.96 | 0.37 | 1.76 | 4.02 | 1.57 | 7.02 | 3.48 | |
| Over 23.1 | Mean | 1.07 | −0.11 | 1.28 | 0.01 | 0.14 | 0.02 | 0.15 | 0.04 |
| Median | 0.57 | −0.23 | 0.68 | 0.02 | 0.8 | 0.37 | 1.53 | −0.97 | |
| Min | −2.83 | −3.69 | −4.03 | −2.6 | −2.83 | −1.96 | −2.82 | −4.71 | |
| Max | 6.75 | 2.16 | 8.59 | 2.94 | 5.1 | 2.62 | 6.79 | 3.9 | |
| Body Fat Percentage | Chest | Abdomen | Hips | Arms/Legs | |||||
|---|---|---|---|---|---|---|---|---|---|
| Type 1 | Type 2 | Type 1 | Type 2 | Type 1 | Type 2 | Type 1 | Type 2 | ||
| Under 14 | Mean | −2.29 | −1.54 | −3.4 | −1.22 | −4.56 | −0.87 | −5.05 | −2.08 |
| Median | −2.71 | −1.196 | −3.4 | −1.22 | −3.85 | −0.75 | −4.79 | −1.52 | |
| Min | −3.01 | −2.59 | −3.41 | −1.3 | −4.56 | −0.87 | −5.05 | −2.08 | |
| Max | −1.35 | −0.85 | −3.38 | −1.15 | −3.15 | −0.64 | −4.53 | −0.97 | |
| 15–22.7 | Mean | −1.97 | 0.03 | −2.53 | −0.7 | −3.25 | −0.54 | −2.69 | −0.61 |
| Median | −1.96 | −0.04 | −2.57 | −0.88 | −2.32 | −0.22 | −2.71 | 0.19 | |
| Min | −3.13 | −1.33 | −3.3 | −2.33 | −2.88 | −0.8 | −3.19 | −2.92 | |
| Max | −0.25 | 1.29 | −1.67 | 1.39 | −0.53 | 1.48 | −2.29 | 2.91 | |
| 22.8–27.1 | Mean | −0.88 | 0.26 | −1.93 | −0.34 | −2.03 | −0.26 | −1.79 | 0.27 |
| Median | −1.36 | 0.165 | −2.21 | −0.42 | −1.45 | −0.08 | −1.37 | −0.21 | |
| Min | −2.34 | −1.14 | −3.25 | −1.85 | −3.4 | −1.14 | −4.84 | −2.61 | |
| Max | 1.68 | 1.3 | 0.14 | 0.87 | 2 | 0.85 | 3.32 | 1.95 | |
| Over 27.1 | Mean | 1.6 | 0.01 | 0.94 | 0.22 | 0.14 | 0.02 | 1.15 | 0.04 |
| Median | 1.29 | 0.082 | 0.59 | 0.14 | 0.72 | −0.01 | 1.1 | 0.25 | |
| Min | −3.09 | −2.72 | −3.37 | −4.13 | −3.35 | −3.69 | −4.5 | −5.81 | |
| Max | 7.02 | 2.43 | 9.37 | 3.22 | 5.53 | 3.35 | 7.63 | 5.48 | |
| Obesity Diagnosis | Chest | Abdomen | Hip | Legs/Arms | Obesity |
|---|---|---|---|---|---|
| Male | C | D | D | C | Overweight |
| Male | A | B | B | B | Normal |
| Male | B | C | B | B | Normal |
| Male | D | D | B~C | B~C | Overweight |
| Male | A~B | C~D | A~B | A~B | Normal |
| Female | B~C | D | D | D | Overweight |
| Female | B | C~D | D | C~D | Overweight |
| Obesity Diagnosis | DEXA | BMI | WHtR | WHR | Proposal Model |
|---|---|---|---|---|---|
| Sample 1 | D | D | D | C | D |
| Sample 2 | C | B | C | C | C |
| Sample 3 | B | B | B | B | B |
| Sample 4 | C | B | C | C | C |
| Sample 5 | C | B | C | B | C |
| Sample 6 | B | A | A | B | B |
| Sample 7 | D | C | C | C | C |
| Sample 8 | A | A | B | B | A |
| Sample 9 | A | A | A | A | B |
| Sample 10 | B | B | B | B | B |
| Accuracy | Ground Truth | 50% | 70% | 60% | 80% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, C.; Youm, S. Development of an Obesity Information Diagnosis Model Reflecting Body Type Information Using 3D Body Information Values. Sensors 2022, 22, 7808. https://doi.org/10.3390/s22207808
Kim C, Youm S. Development of an Obesity Information Diagnosis Model Reflecting Body Type Information Using 3D Body Information Values. Sensors. 2022; 22(20):7808. https://doi.org/10.3390/s22207808
Chicago/Turabian StyleKim, Changgyun, and Sekyoung Youm. 2022. "Development of an Obesity Information Diagnosis Model Reflecting Body Type Information Using 3D Body Information Values" Sensors 22, no. 20: 7808. https://doi.org/10.3390/s22207808
APA StyleKim, C., & Youm, S. (2022). Development of an Obesity Information Diagnosis Model Reflecting Body Type Information Using 3D Body Information Values. Sensors, 22(20), 7808. https://doi.org/10.3390/s22207808









