Validity and Reliability of a Novel Smartphone Tele-Assessment Solution for Quantifying Hip Range of Motion
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Instrumentation
2.3. Protocol
2.3.1. Hip Internal and External Rotation during Sitting
2.3.2. Hip Internal and External Rotation in Prone
2.3.3. Hip Flexion in Supine
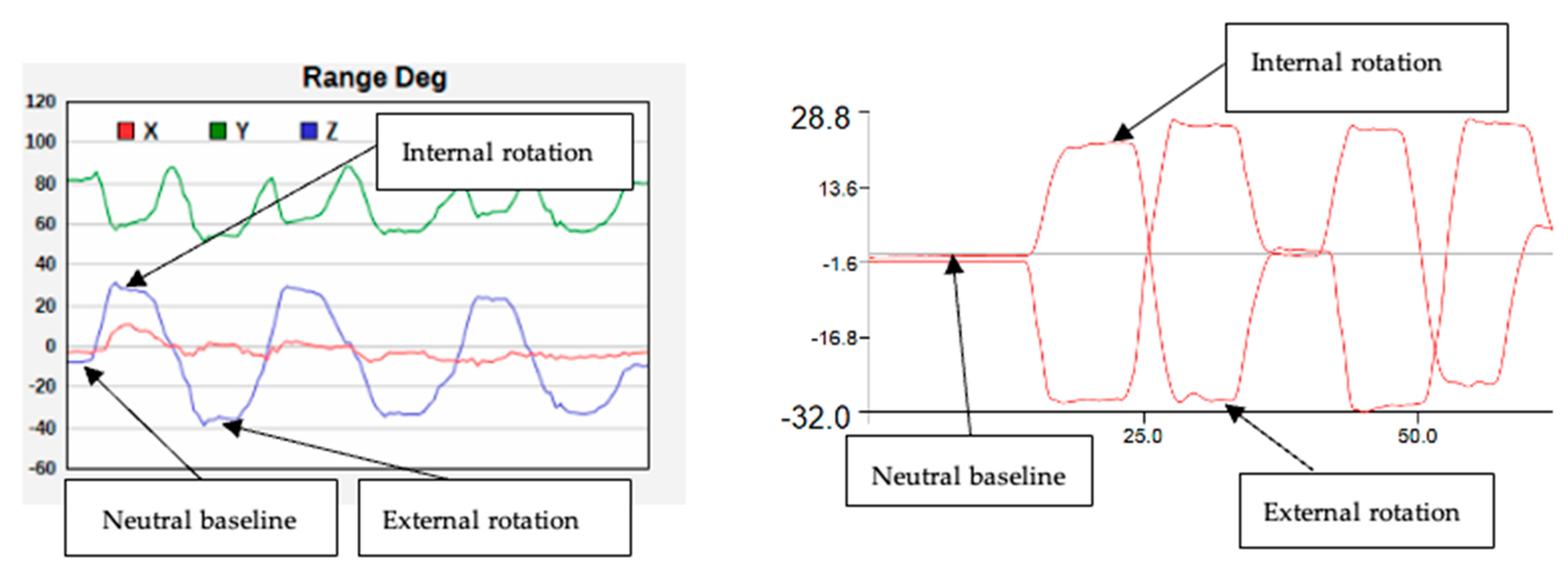
2.4. Data Analysis
2.5. Statistical Analysis
3. Results
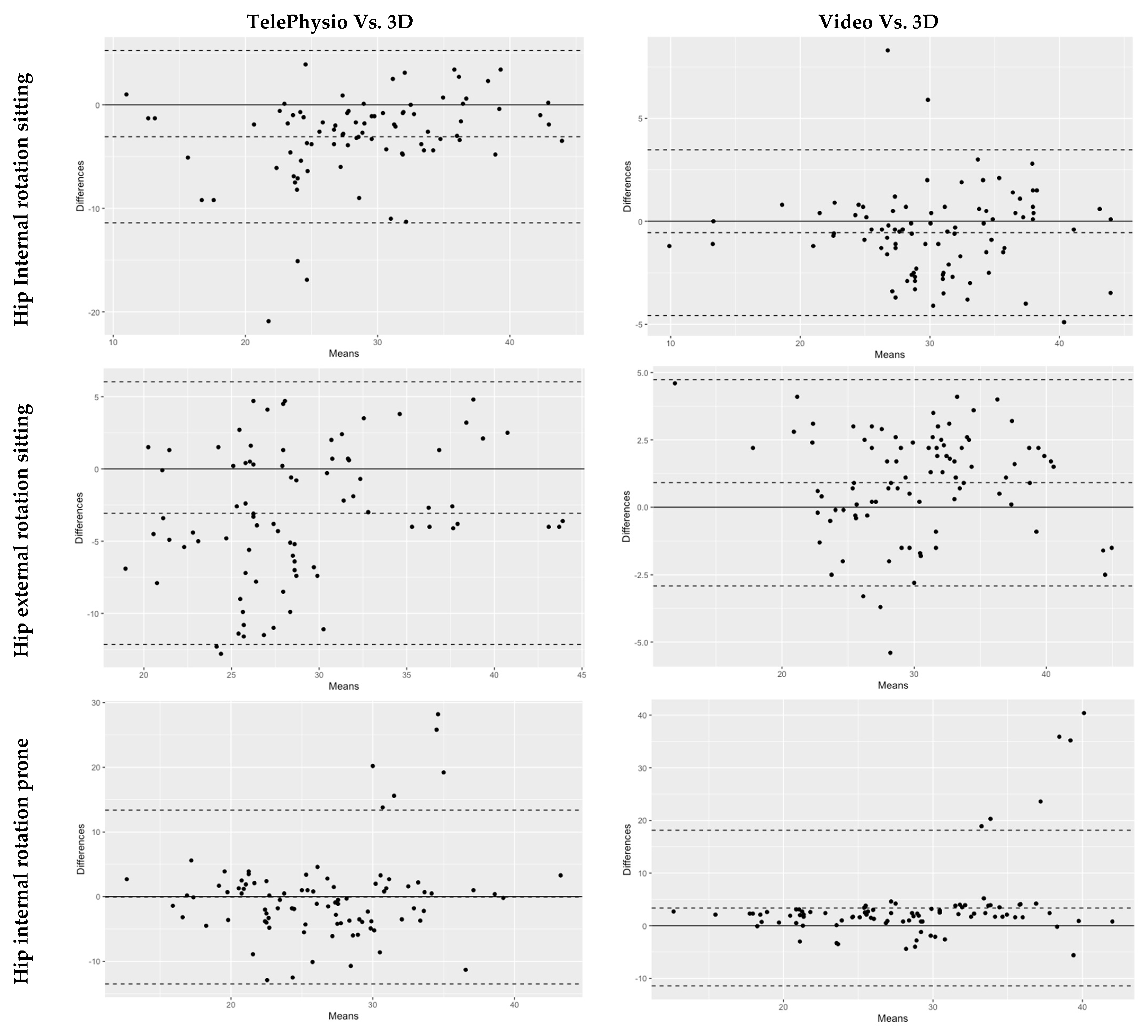
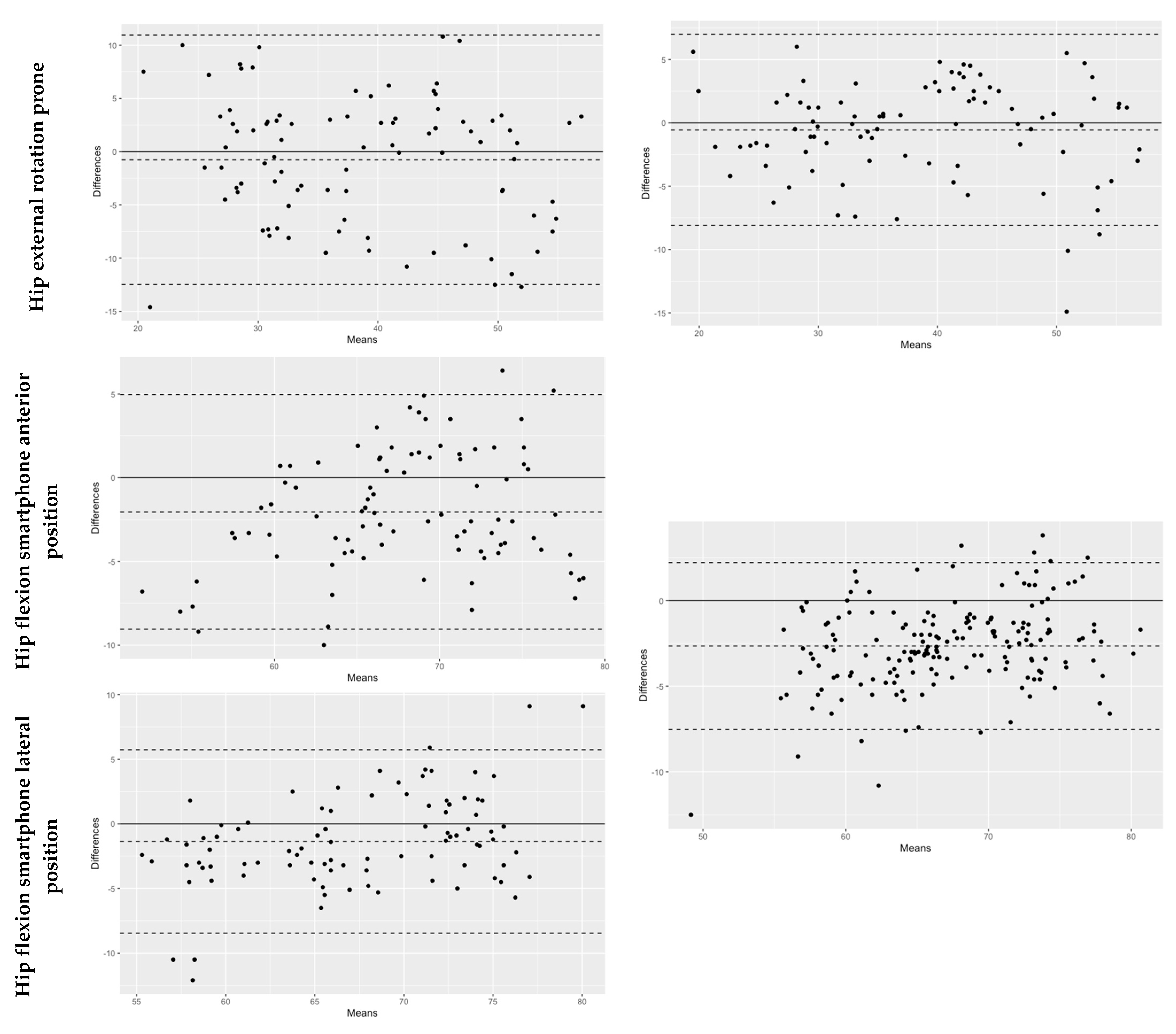
3.1. Concurrent Validity
3.2. Between-Sessions Reliability
3.3. Inter-Rater Reliability
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Brigo, E.; Rintala, A.; Kossi, O.; Verwaest, F.; Vanhoof, O.; Feys, P.; Bonnechère, B. Using Telehealth to Guarantee the Continuity of Rehabilitation during the COVID-19 Pandemic: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 10325. [Google Scholar] [CrossRef] [PubMed]
- Richardson, B.R.; Truter, P.; Blumke, R.; Russell, T.G. Physiotherapy assessment and diagnosis of musculoskeletal disorders of the knee via telerehabilitation. J. Telemed. Telecare 2016, 23, 88–95. [Google Scholar] [CrossRef] [PubMed]
- Picerno, P.; Iosa, M.; D’Souza, C.; Benedetti, M.G.; Paolucci, S.; Morone, G. Wearable inertial sensors for human movement analysis: A five-year update. Expert Rev. Med. Devices 2021, 18, 79–94. [Google Scholar] [CrossRef] [PubMed]
- Frangiamore, S.; Mannava, S.; Geeslin, A.G.; Chahla, J.; Cinque, M.E.; Philippon, M.J. Comprehensive Clinical Evaluation of Femoroacetabular Impingement: Part 1, Physical Examination. Arthrosc. Technol. 2017, 6, e1993–e2001. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Griffin, D.R.; Dickenson, E.J.; O’Donnell, J.; Agricola, R.; Awan, T.; Beck, M.; Clohisy, J.C.; Dijkstra, H.P.; Falvey, E.; Gimpel, M.; et al. The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): An international consensus statement. Br. J. Sports Med. 2016, 50, 1169–1176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lesage, J. Standard of Care: Total Hip Replacement 2015; The Brigham and Women’s Hospital, Inc., Department of Rehabilitation Services: Brookline, MA, USA, 2015; pp. 1–26. [Google Scholar]
- Jansson, M.M.; Harjumaa, M.; Puhto, A.; Pikkarainen, M. Patients’ satisfaction and experiences during elective primary fast-track total hip and knee arthroplasty journey: A qualitative study. J. Clin. Nurs. 2019, 29, 567–582. [Google Scholar] [CrossRef] [PubMed]
- Charlton, P.C.; Mentiplay, B.F.; Pua, Y.-H.; Clark, R.A. Reliability and concurrent validity of a Smartphone, bubble inclinometer and motion analysis system for measurement of hip joint range of motion. J. Sci. Med. Sport 2015, 18, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Dietz, M.J.; Sprando, D.; Hanselman, A.E.; Regier, M.D.; Frye, B.M. Smartphone assessment of knee flexion compared to radiographic standards. Knee 2017, 24, 224–230. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miyachi, Y.; Ito, M.; Furuta, K.; Ban, R.; Hanamura, S.; Kamiya, M. Reliability and validity of lower limb joint range of motion measurements using a smartphone. Nagoya J. Med. Sci. 2022, 84, 7–18. [Google Scholar] [PubMed]
- Takeda, Y.; Furukawa, K. Clinical reliability and usability of smartphone goniometers for hip range of motion measurement. J. Phys. Ther. Sci. 2022, 34, 433–439. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, K.L.; Roach, K.L.; Wajda, D.A.; Sosnoff, J.J. Smartphone technology can measure postural stability and discriminate fall risk in older adults. Gait Posture 2019, 67, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Yan, W.; Zhang, Q.; Wang, L.; Mao, Y.; Wang, A.; Zhao, C. A Modified Kalman Filter for Integrating the Different Rate Data of Gyros and Accelerometers Retrieved from Android Smartphones in the GNSS/IMU Coupled Navigation. Sensors 2020, 20, 5208. [Google Scholar] [CrossRef] [PubMed]
- Agnvall, C.; Aminoff, A.S.; Todd, C.; Jonasson, P.; Thoreson, O.; Swärd, L.; Karlsson, J.; Baranto, A. Range of Hip Joint Motion Is Correlated With MRI-Verified Cam Deformity in Adolescent Elite Skiers. Orthop. J. Sports Med. 2017, 5, 2325967117711890. [Google Scholar] [CrossRef] [PubMed]
- Kapron, A.L.; Anderson, A.E.; Peters, C.L.; Phillips, L.G.; Stoddard, G.J.; Petron, D.J.; Toth, R.; Aoki, S.K. Hip Internal Rotation Is Correlated to Radiographic Findings of Cam Femoroacetabular Impingement in Collegiate Football Players. Arthrosc. J. Arthrosc. Relat. Surg. 2012, 28, 1661–1670. [Google Scholar] [CrossRef]
- Chen, H.; Schall, M.C., Jr.; Fethke, N. Accuracy of angular displacements and velocities from inertial-based inclinometers. Appl. Ergon. 2018, 67, 151–161. [Google Scholar] [CrossRef] [PubMed]
- Landis, J.R.; Koch, G.G. The Measurement of Observer Agreement for Categorical Data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Atkinson, G.; Nevill, A.M. Statistical Methods For Assessing Measurement Error (Reliability) in Variables Relevant to Sports Medicine. Sports Med. 1998, 26, 217–238. [Google Scholar] [CrossRef] [PubMed]
- Keogh, J.W.L.; Cox, A.; Anderson, S.; Liew, B.; Olsen, A.; Schram, B.; Furness, J. Reliability and validity of clinically accessible smartphone applications to measure joint range of motion: A systematic review. PLoS ONE 2019, 14, e0215806. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ganokroj, P.; Sompornpanich, N.; Kerdsomnuek, P.; Vanadurongwan, B.; Lertwanich, P. Validity and reliability of smartphone applications for measurement of hip rotation, compared with three-dimensional motion analysis. BMC Musculoskelet. Disord. 2021, 22, 1–9. [Google Scholar] [CrossRef]
- Hamersma, D.T.; Hofste, A.; Rijken, N.H.; Rohé, M.R.O.; Oosterveld, F.G.; Soer, R. Reliability and validity of the Microgate Gyko for measuring range of motion of the low back. Musculoskelet. Sci. Pract. 2019, 45, 102091. [Google Scholar] [CrossRef] [PubMed]

| Measurement | Tele Mean ± SD (°) | 3D Mean ± SD (°) | p-Value | ICC −95%–+95% CI | Bias ± SD Lower–Upper LOA (°) | SEM (°) |
|---|---|---|---|---|---|---|
| Hip Internal rotation sitting | 27.3 ± 7.66 | 30.4 ± 6.47 | 0.007 | 0.75 0.41–0.87 | −0.11 ± 0.18 −0.53–0.29 | 2.12 |
| Hip external rotation sitting | 27.4 ± 6.59 | 30.5 ± 5.49 | 0.04 | 0.63 0.30–0.79 | 0.13± 0.18 −0.21–0.49 | 2.81 |
| Hip internal rotation prone | 26.6 ± 7.28 | 26.6 ± 6.14 | 0.99 | 0.48 0.31–0.63 | −0.11 ± 0.16 −0.21–0.44 | 4.93 |
| Hip external rotation prone | 38.2 ± 9.45 | 38.9 ± 10.4 | 0.87 | 0.81 0.73–0.87 | −0.01 ± 0.18 −0.28–0.38 | 2.60 |
| Hip flexion smartphone anterior position | 66.8 ± 6.90 | 68.9 ± 6.13 | 0.12 | 0.81 0.62–0.89 | −0.03 ± 0.05 −0.13–0.07 | 1.55 |
| Hip flexion smartphone lateral position | 66.8 ± 7.28 | 68.1 ± 5.84 | 0.38 | 0.83 0.73–0.89 | −0.02 ± 0.05 −0.12–0.10 | 1.48 |
| Measurement | Video Mean ± SD (°) | 3D Mean ± SD (°) | p-Value | ICC −95%–+95% CI | Bias Lower–Upper LOA (°) | SEM (°) |
|---|---|---|---|---|---|---|
| Hip Internal rotation sitting | 29.9 ± 6.50 | 30.4 ± 6.47 | 0.86 | 0.94 0.91–0.96 | −0.48 ± 2.06 −4.53–3.56 | 0.50 |
| Hip external rotation sitting | 31.3 ± 5.69 | 30.5 ± 5.49 | 0.61 | 0.93 0.87–0.95 | 0.82 ± 1.93 −2.97–4.62 | 0.51 |
| Hip internal rotation prone | 30.0 ± 8.58 | 26.6 ± 6.14 | 0.01 | 0.44 0.23–0.61 | 3.35 ± 7.54 −11.42–18.13 | 5.64 |
| Hip external rotation prone | 38.4 ± 10.2 | 38.9 ± 10.4 | 0.93 | 0.92 0.89–0.95 | −0.02 ± 0.09 −0.17–0.21 | 1.08 |
| Hip flexion | 65.9 ± 6.70 | 68.5 ± 5.98 | 0.0007 | 0.85 0.29–0.94 | −0.04 ± 0.04 −0.12–0.04 | 0.96 |
| Measurement | Laboratory Mean ± SD (°) | Home Mean ± SD (°) | p-Values | ICC −95%–+95% CI | SEM (°) | MDC (°) |
|---|---|---|---|---|---|---|
| Hip Internal rotation sitting | 27.3 ± 7.66 | 25.8 ± 7.20 | 0.43 | 0.47 0.13–0.71 | 5.37 | 6.42 |
| Hip external rotation sitting | 27.4 ± 6.59 | 25.5 ± 8.08 | 0.34 | 0.63 0.35–0.81 | 4.43 | 5.83 |
| Hip internal rotation prone | 26.6 ± 7.28 | 27.9 ± 7.68 | 0.46 | 0.44 0.09–0.69 | 5.54 | 6.52 |
| Hip external rotation prone | 38.2 ± 9.45 | 37.0 ± 10.7 | 0.72 | 0.50 0.15–0.73 | 7.05 | 7.36 |
| Hip flexion smartphone anterior position | 66.8 ± 6.90 | 68.4 ± 8.32 | 0.18 | 0.63 0.35–0.81 | 4.74 | 6.03 |
| Hip flexion smartphone lateral position | 66.8 ± 7.28 | 70.5 ± 8.27 | 0.94 | 0.64 0.37–0.81 | 4.86 | 6.11 |
| Measurement | Laboratory Mean ± SD (°) | Home Mean ± SD (°) | p-Values | ICC −95%–+95% CI | SEM (°) | MDC (°) |
|---|---|---|---|---|---|---|
| Hip Internal rotation sitting | 29.9 ± 6.40 | 30.1 ± 6.22 | 0.91 | 0.36 −0.01–0.64 | 5.00 | 6.20 |
| Hip external rotation sitting | 31.3 ± 5.50 | 34.2 ± 6.26 | 0.07 | 0.54 0.19–0.76 | 4.08 | 5.59 |
| Hip internal rotation prone | 29.8 ± 8.68 | 28.9 ± 8.45 | 0.71 | 0.52 0.19–0.74 | 5.37 | 6.42 |
| Hip external rotation prone | 38.6 ± 10.0 | 40.6 ± 10.80 | 0.46 | 0.60 0.31–0.79 | 7.18 | 7.43 |
| Hip flexion | 65.9 ± 6.55 | 72.0 ± 8.25 | 0.0002 | 0.52 −0.01–0.77 | 5.60 | 6.55 |
| Measurement | Assessor 1 Mean ± SD (°) | Assessor 2 Mean ± SD (°) | p-Values | ICC −95%–+95% CI | SEM (°) |
|---|---|---|---|---|---|
| Hip Internal rotation sitting | 29.6 ± 7.35 | 30.1 ± 6.22 | 0.32 | 0.93 0.88–0.96 | 1.88 |
| Hip external rotation sitting | 36.4 ± 6.79 | 34.2 ± 6.26 | 0.019 | 0.87 0.47–0.95 | 2.40 |
| Hip internal rotation prone | 27.7 ± 9.38 | 28.9 ± 8.45 | 0.48 | 0.95 0.92–0.97 | 2.04 |
| Hip external rotation prone | 39.2 ± 9.86 | 40.6 ± 10.80 | 0.37 | 0.94 0.89–0.96 | 2.54 |
| Hip flexion | 62.9 ± 9.17 | 71.8 ± 8.37 | > 0.0001 | 0.59 −0.07–0.86 | 6.28 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marshall, C.J.; El-Ansary, D.; Pranata, A.; Ganderton, C.; O’Donnell, J.; Takla, A.; Tran, P.; Wickramasinghe, N.; Tirosh, O. Validity and Reliability of a Novel Smartphone Tele-Assessment Solution for Quantifying Hip Range of Motion. Sensors 2022, 22, 8154. https://doi.org/10.3390/s22218154
Marshall CJ, El-Ansary D, Pranata A, Ganderton C, O’Donnell J, Takla A, Tran P, Wickramasinghe N, Tirosh O. Validity and Reliability of a Novel Smartphone Tele-Assessment Solution for Quantifying Hip Range of Motion. Sensors. 2022; 22(21):8154. https://doi.org/10.3390/s22218154
Chicago/Turabian StyleMarshall, Charlotte J., Doa El-Ansary, Adrian Pranata, Charlotte Ganderton, John O’Donnell, Amir Takla, Phong Tran, Nilmini Wickramasinghe, and Oren Tirosh. 2022. "Validity and Reliability of a Novel Smartphone Tele-Assessment Solution for Quantifying Hip Range of Motion" Sensors 22, no. 21: 8154. https://doi.org/10.3390/s22218154
APA StyleMarshall, C. J., El-Ansary, D., Pranata, A., Ganderton, C., O’Donnell, J., Takla, A., Tran, P., Wickramasinghe, N., & Tirosh, O. (2022). Validity and Reliability of a Novel Smartphone Tele-Assessment Solution for Quantifying Hip Range of Motion. Sensors, 22(21), 8154. https://doi.org/10.3390/s22218154







