Dual Wavelength Photoplethysmography Framework for Heart Rate Calculation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Experimental Protocol and Sensors Suite
- Stage 1: The participant stood steady on the treadmill for 1 min (here, the treadmill’s speed was 0 km/h). During this stage, clean physiological signals were collected.
- Stage 2: The participant ran at a speed of 6 km/h (about 3.7 mph) for 1 min (here, the treadmill’s speed was 6 km/h).
- Stage 3: If the participant was comfortable, the treadmill’s speed was increased gradually to 12 km/h (about 7.5 mph), for 1 min. At any time, if the participant was not comfortable, the treadmill’s speed was reduced to the participant’s comfort zone.
- Stage 4 (same as stage 2): The participant ran at a speed of 6 km/h (about 3.7 mph) for 1 min (here, the treadmill’s speed was 6 km/h).
- Stage 5 (same as stage 3): If the participant was comfortable, the treadmill’s speed was increased gradually to 12 km/h (about 7.5 mph), for 1 min. At any time, if the participant was not comfortable, the treadmill’s speed was reduced to the participant’s comfort zone.
- Stage 6: The participant stood steady on the treadmill for a duration of 1 min (here, the treadmill’s speed was 0 km/h).
2.2. Infrared PPG Signal as Noise Reference Signal
2.3. DWL Framework
2.3.1. Pre-Processing
2.3.2. Motion-Artifact Detection
2.3.3. Motion-Artifact Frequency Components Identification
2.3.4. Denoising
2.3.5. Heart Rate Estimation
- 1.
- The heart rate estimated from the previous time step l, .
- 2.
- A heart rate candidate which is obtained from the spectrum of the green PPG signal.
- 3.
- A heart rate prediction, which is obtained from the long-term (LT) trend of the past six (6) HR estimates. The LT trend is obtained using STL, the Seasonal-Trend decomposition using LOESS (locally estimated scatterplot smoothing) [32]. In this study, we used the MATLAB implementation, trenddecomp.
2.4. Alternative HR Calculation Methods
3. Results
3.1. Performance Metrics
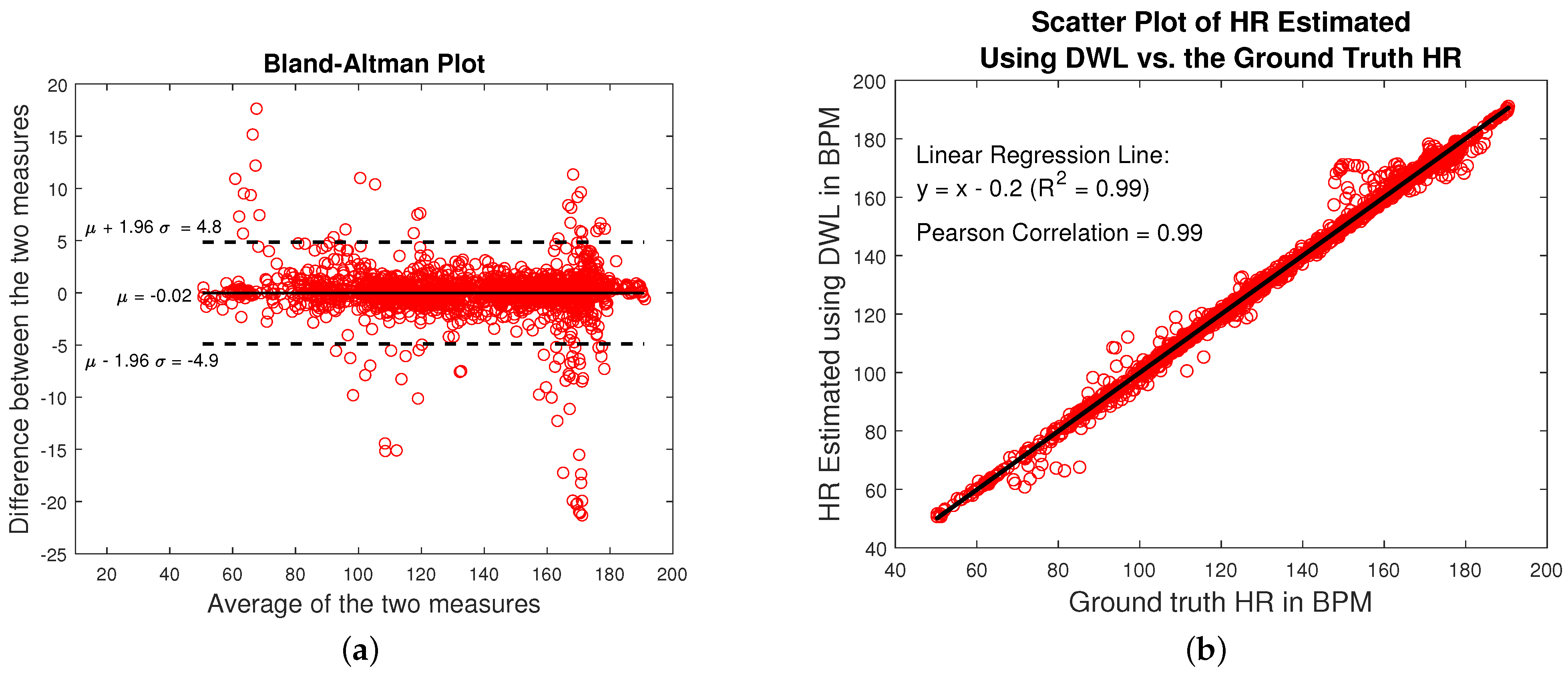
3.2. DWL Performance on Wrist Data
3.3. Validation of the DWL Method on Palm Data
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Wide, Medium, and Narrow Search Ranges
References
- Allen, J. Photoplethysmography and its application in clinical physiological measurement. Physiol. Meas. 2007, 28, R1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Webster, J.G. Design of Pulse Oximeters, 1st ed.; CRC Press: Boca Raton, FL, USA, 1997; pp. 1–260. [Google Scholar]
- Goldman, J.M.; Petterson, M.T.; Kopotic, R.J.; Barker, S.J. Masimo signal extraction pulse oximetry. J. Clin. Monit. Comput. 2000, 16, 475–483. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.W.; Lee, J.W.; Jung, W.G.; Lee, G.K. The periodic moving average filter for removing motion artifacts from PPG signals. Int. J. Control. Autom. Syst. 2007, 5, 701–706. [Google Scholar]
- Grap, M.J. Pulse Oximeter. Crit. Care Nurse 2002, 22, 69–74. [Google Scholar] [CrossRef]
- Yousefi, R.; Nourani, M.; Ostadabbas, S.; Panahi, I. A motion-tolerant adaptive algorithm for wearable photoplethysmographic biosensors. IEEE J. Biomed. Health Inform. 2014, 18, 670–681. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Pi, Z.; Liu, B. TROIKA: A general framework for heart rate monitoring using wrist-type photoplethysmographic signals during intensive physical exercise. IEEE Trans. Biomed. Eng. 2015, 62, 522–531. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Z. Photoplethysmography-based heart rate monitoring in physical activities via joint sparse spectrum reconstruction. IEEE Trans. Biomed. Eng. 2015, 62, 1902–1910. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.; Song, S.; Vullings, R.; Biswas, D.; Simões-Capela, N.; Van Helleputte, N.; Van Hoof, C.; Groenendaal, W. Motion artifact reduction for wrist-worn photoplethysmograph sensors based on different wavelengths. Sensors 2019, 19, 673. [Google Scholar] [CrossRef] [Green Version]
- Galli, A.; Narduzzi, C.; Giorgi, G. Measuring Heart Rate during Physical Exercise by Subspace Decomposition and Kalman Smoothing. IEEE Trans. Instrum. Meas. 2018, 67, 1102–1110. [Google Scholar] [CrossRef]
- Castaneda, D.; Esparza, A.; Ghamari, M.; Soltanpur, C.; Nazeran, H. A review on wearable photoplethysmography sensors and their potential future applications in health care. Physiol. Behav. 2016, 176, 139–148. [Google Scholar] [CrossRef]
- Haykin, S.O. Adaptive Filter Theory, 4th ed.; Pearson: London, UK, 2002. [Google Scholar]
- Paros, J.M. Triaxial accelerometer assembly and in situ calibration method for improved geodetic and seismic measurements. U.S. Patent 9,645,267, 9 May 2017. [Google Scholar]
- Bertec. Split-Belt Instrumented Treadmill. Available online: https://www.bertec.com/products/instrumented-treadmills (accessed on 27 October 2022).
- The Math Works Inc. MALAB 2022b. Available online: https://www.mathworks.com (accessed on 27 October 2022).
- Alkhoury, L. DWL Method GitHub Repository. Available online: https://github.com/ludvikalkhoury/DWL-Method.git (accessed on 27 October 2022).
- Vishay. High Power Infrared Emitting Diode, 940 nm, GaAlAs, MQW. Available online: https://www.farnell.com/datasheets/2049675.pdf (accessed on 27 October 2022).
- LightHouseLEDs. 5mm Round Top Pure Green LED-Ultra Bright. Available online: https://lighthouseleds.com/5mm-led-green-ultra-bright-15-000-mcd.html (accessed on 27 October 2022).
- Digi-Key. OPT101PG4. Available online: https://www.digikey.com/en/products/detail/texas-instruments/OPT101PG4/1899803 (accessed on 27 October 2022).
- Delsys Trigno Avanti Sensor. Available online: https://delsys.com/trigno-avanti/ (accessed on 27 October 2022).
- Trigno EKG Biofeedback Sensor. Available online: https://delsys.com/trigno-ekg-biofeedback/ (accessed on 27 October 2022).
- Krzywinski, M.; Altman, N. Visualizing samples with box plots. Nat. Methods 2014, 11, 119–120. [Google Scholar] [CrossRef] [PubMed]
- Kasbekar, R.S.; Mendelson, Y. Evaluation of key design parameters for mitigating motion artefact in the mobile reflectance PPG signal to improve estimation of arterial oxygenation. Physiol. Meas. 2018, 39, 075008. [Google Scholar] [CrossRef] [PubMed]
- Rubins, U.; Upmalis, V.; Rubenis, O.; Jakovels, D.; Spigulis, J. Real-time photoplethysmography imaging system. IFMBE Proceedings 2011, 34 IFMBE, 183–186. [Google Scholar] [CrossRef]
- Wijshoff, R.W.; Mischi, M.; Aarts, R.M. Reduction of periodic motion artifacts in photoplethysmography. IEEE Trans. Biomed. Eng. 2017, 64, 196–207. [Google Scholar] [CrossRef] [Green Version]
- Relente, A.R.; Sison, L.G. Characterization and adaptive filtering of motion artifacts in pulse oximetry using accelerometers. Annu. Int. Conf. IEEE Eng. Med. Biol. Proc. 2002, 2, 1769–1770. [Google Scholar] [CrossRef]
- Chan, K.W.; Zhang, Y.T. Adaptive Reduction of Motion Artifacts from Photoplethysmographic Recordings using a Variable Step-Size LMS Filter. IEEE Sens. 2002, 2, 1343–1346. [Google Scholar]
- Ram, M.R.; Madhav, K.V.; Krishna, E.H.; Komalla, N.R.; Reddy, K.A. A novel approach for motion artifact reduction in PPG signals based on AS-LMS adaptive filter. IEEE Trans. Instrum. Meas. 2012, 61, 1445–1457. [Google Scholar] [CrossRef]
- Wang, M.; Li, Z.; Zhang, Q.; Wang, G. Removal of motion artifacts in photoplethysmograph sensors during intensive exercise for accurate heart rate calculation based on frequency estimation and notch filtering. Sensors 2019, 19, 3312. [Google Scholar] [CrossRef] [Green Version]
- Sayed, A.H.; Kailath, T. A State-Space Approach to Adaptive RLS Filtering. IEEE Signal Process. Mag. 1994, 11, 18–60. [Google Scholar] [CrossRef] [Green Version]
- dsp.AdaptiveLatticeFilter. 2022. Available online: https://www.mathworks.com/help/dsp/ref/dsp.adaptivelatticefilter-system-object.html (accessed on 27 October 2022).
- Cleveland, R.B.; Cleveland, W.S.; McRae, J.E.; Terpenning, I. STL: A Seasonal-Trend Decomposition Procedure Based on Loess. J. Off. Stat. 1990, 6, 3–73. [Google Scholar] [CrossRef]
- Wood, L.B.; Asada, H.H. Noise cancellation model validation for reduced motion artifact wearable PPG sensors using MEMS accelerometers. Annu. Int. Conf. IEEE Eng. Med. Biol. Proc. 2006, 3525–3528. [Google Scholar] [CrossRef]
- Chowdhury, S.S.; Hyder, R.; Hafiz, M.S.B.; Haque, M.A. Real-Time Robust Heart Rate Estimation from Wrist-Type PPG Signals Using Multiple Reference Adaptive Noise Cancellation. IEEE J. Biomed. Health Inform. 2018, 22, 450–459. [Google Scholar] [CrossRef] [PubMed]
- Gibbs, P.; Asada, H.H. Reducing motion artifact in wearable bio-sensors using MEMS accelerometers for active noise cancellation. Proc. Am. Control Conf. 2005, 3, 1581–1586. [Google Scholar] [CrossRef]
- Hassani, H. Munich Personal RePEc Archive Singular Spectrum Analysis: Methodology and Comparison Singular Spectrum Analysis: Methodology and Comparison. J. Data Sci. 2007, 4991, 239–257. [Google Scholar]
- Stanković, L.; Sejdić, E.; Stanković, S.; Daković, M.; Orović, I. A Tutorial on Sparse Signal Reconstruction and Its Applications in Signal Processing. Circuits, Syst. Signal Process. 2019, 38, 1206–1263. [Google Scholar] [CrossRef]
- Barker, S.J. “Motion-resistant” pulse oximetry: A comparison of new and old models. Anesth. Analg. 2002, 95, 967–972. [Google Scholar]
- Giavarina, D. Understanding Bland Altman Analysis. Biochem. Medica 2015, 25, 10–16. [Google Scholar] [CrossRef]










| Instrument/Sensor | Manufacturer | Reference |
|---|---|---|
| Split-belt Instrumented Treadmill | Bertec Corp. (Columbus, OH, USA) | Catalog in [14] |
| IR LED (TSAL6100) | Vishay Intertechnology Inc. (Malvern, PA, USA) | Datasheet in [17] |
| Green LED (A-U5MUGC12) | Light House LEDs LLC (Medical Lake, WA, USA) | Datasheet in [18] |
| Photo-detector (OPT101) | Texas-Instrument Inc. (Dallas, TX, USA) | Datasheet in [19] |
| Delsys Trigno Avanti (tri-axial accelerometer) | Delsys Inc. (Natick, MA, USA) | Catalog in [20] |
| Trigno EKG Biofeedback sensor (ECG) | Delsys Inc. | Catalog in [21] |
| HR Calculation Methods | |||
|---|---|---|---|
| Participant Number | TROIKA | JOSS | DWL |
| 1 | 1.09 | 1.39 | 0.74 |
| 2 | 4.3 | 87.61 | 1.48 |
| 3 | 1.21 | 1.41 | 0.63 |
| 4 | 1.96 | 1.72 | 2.36 |
| 5 | 7.85 | 5.49 | 1.86 |
| 6 | 2.57 | 2.73 | 1.18 |
| 7 | 1.83 | 2.03 | 1.64 |
| 8 | 1.08 | 0.84 | 0.61 |
| 9 | 1.73 | 1.86 | 0.76 |
| 10 | 9.34 | 21.8 | 0.85 |
| 11 | 2.72 | 4.87 | 1.31 |
| Average | 3.24 | 2.82 BPM | 11.98 | 25.79 BPM | 1.22 | 0.57 BPM |
| Average without Lock Loss | 2.05 | 1.03 BPM | 2.11 | 1.24 BPM | 1.22 | 0.57 BPM |
| HR Calculation Methods | |||
|---|---|---|---|
| Participant Number | TROIKA | JOSS | DWL |
| 1 | 0.92 | 1.19 | 0.66 |
| 2 | 3.88 | 59.22 | 1.47 |
| 3 | 1.03 | 1.23 | 0.5 |
| 4 | 1.43 | 1.31 | 1.61 |
| 5 | 4.96 | 3.41 | 1.19 |
| 6 | 2.06 | 2.24 | 0.85 |
| 7 | 1.38 | 1.49 | 1.16 |
| 8 | 0.77 | 0.62 | 0.42 |
| 9 | 1.94 | 2.08 | 0.81 |
| 10 | 7.91 | 19.53 | 0.83 |
| 11 | 2.07 | 3.19 | 1.00 |
| Average | 2.58 | 2.19% | 8.68 | 17.6% | 0.95 | 0.38% |
| HR Calculation Methods | |||
|---|---|---|---|
| Participant Number | TROIKA | JOSS | DWL Method |
| 1 | 96.02 | 93.75 | 98.36 |
| 2 | 72.57 | 6.86 | 94.29 |
| 3 | 96.02 | 93.75 | 100 |
| 4 | 88.07 | 90.91 | 86.93 |
| 5 | 61.58 | 80.79 | 88.7 |
| 6 | 80.68 | 84.66 | 100 |
| 7 | 90.96 | 88.7 | 91.53 |
| 8 | 97.18 | 98.31 | 100 |
| 9 | 90.91 | 89.2 | 100 |
| 10 | 63.84 | 57.63 | 99.44 |
| 11 | 84.75 | 80.23 | 95.48 |
| Average | 83.87 | 12.75% | 78.62 | 26.16% | 95.88 | 4.9% |
| HR Calculation Methods | |||
|---|---|---|---|
| Participant Number | TROIKA | JOSS | DWL Method |
| 1 | 243.6 | 8.5 | 2.8 |
| 2 | 238.0 | 8.3 | 3.0 |
| 3 | 294.6 | 8.6 | 3.1 |
| 4 | 259.7 | 8.4 | 2.7 |
| 5 | 246.5 | 8.5 | 3.1 |
| 6 | 239.7 | 9.2 | 3.7 |
| 7 | 237.0 | 8.5 | 2.7 |
| 8 | 326.4 | 8.5 | 2.8 |
| 9 | 278.3 | 8.3 | 2.8 |
| 10 | 194.3 | 8.5 | 3.3 |
| 11 | 166.9 | 8.5 | 3.1 |
| Average | 247.7 | 43.8 s | 8.5 | 0.24 s | 3.0 | 0.3 s |
| Run 1 (Wrist Run) | Run 2 (Palm Run) | |||||
|---|---|---|---|---|---|---|
| TROIKA | JOSS | DWL | TROIKA | JOSS | DWL | |
| Average MAE (BPM) of all participants | 3.24|2.82 | 11.98|25.79 | 1.22|0.57 | 1.79|0.92 | 12.88|27.41 | 1.3|0.77 |
| Average MAE (BPM) of participants without Lock Loss | 2.05|1.03 | 2.11|1.24 | 1.22|0.57 | 1.79|0.92 | 1.57|0.83 | 1.3|0.77 |
| Average MAEP (%) of all participants | 2.58|2.19 | 8.68|17.6 | 0.95|0.38 | 1.43|0.69 | 8.51|17.62 | 1.01|0.6 |
| Average PI (%) of all participants | 83.87|12.75 | 78.62|26.16 | 95.88|4.9 | 90.23|8.94 | 80.93|29.18 | 95.33|6.46 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alkhoury, L.; Choi, J.; Chandran, V.D.; De Carvalho, G.B.; Pal, S.; Kam, M. Dual Wavelength Photoplethysmography Framework for Heart Rate Calculation. Sensors 2022, 22, 9955. https://doi.org/10.3390/s22249955
Alkhoury L, Choi J, Chandran VD, De Carvalho GB, Pal S, Kam M. Dual Wavelength Photoplethysmography Framework for Heart Rate Calculation. Sensors. 2022; 22(24):9955. https://doi.org/10.3390/s22249955
Chicago/Turabian StyleAlkhoury, Ludvik, JiWon Choi, Vishnu D. Chandran, Gabriela B. De Carvalho, Saikat Pal, and Moshe Kam. 2022. "Dual Wavelength Photoplethysmography Framework for Heart Rate Calculation" Sensors 22, no. 24: 9955. https://doi.org/10.3390/s22249955
APA StyleAlkhoury, L., Choi, J., Chandran, V. D., De Carvalho, G. B., Pal, S., & Kam, M. (2022). Dual Wavelength Photoplethysmography Framework for Heart Rate Calculation. Sensors, 22(24), 9955. https://doi.org/10.3390/s22249955







