Application of Wearable Sensors in Actuation and Control of Powered Ankle Exoskeletons: A Comprehensive Review
Abstract
1. Introduction
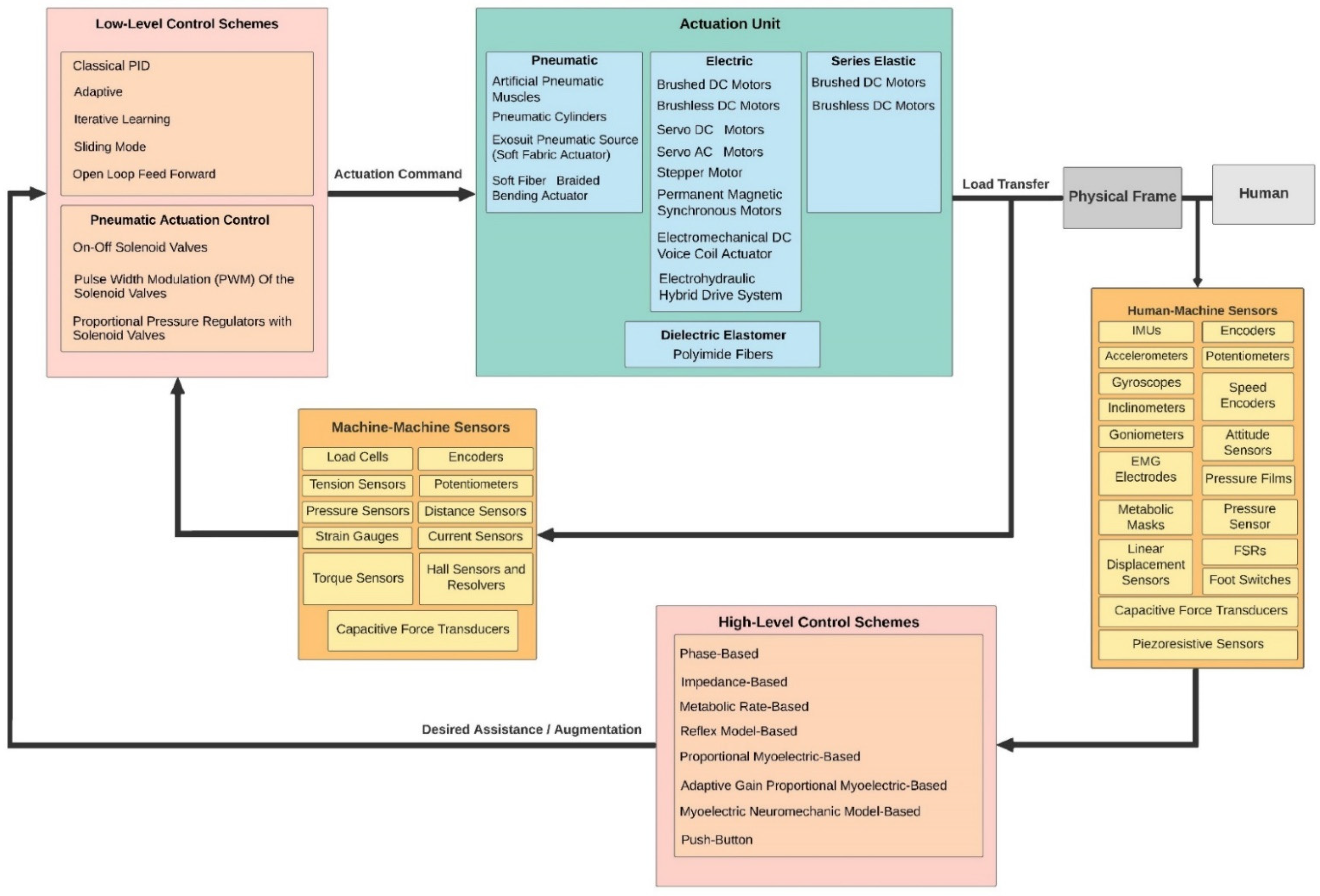
- General information including the exoskeleton purpose and target population, target limb side (bilateral or unilateral), degree of freedom (DoF), and assistance direction (dorsiflexion or plantar flexion or both), portability, and the total weight.
- Actuation principle and actuator type.
- Control hierarchy including high-level and low-level control schemes.
- Sensor system including human–machine and machine–machine sensors
2. Sensor Technologies Used in Control Hierarchy of the PAEs
- Robustness and reliability: the redundant data generated by multiple sensor units enables the system to provide information in case of partial failure.
- Extended spatial and temporal coverage: one sensor can look where others cannot and can perform a measurement while others cannot.
- Increased confidence: a measurement from one sensor is confirmed by measurements from other sensors.
- Reduced ambiguity and uncertainty: joint information reduces the set of ambiguous interpretations of the measured value.
- Robustness against interference: by increasing the dimensionality of the measurement (e. g., measuring the desired quantity with optical encoders and IMUs), the system becomes less vulnerable to interference.
- Improved resolution: when multiple independent measurements of the same property are fused, the resolution of the resulting value is better than for a single sensor measurement [46].

2.1. High-Level Control and Human–Machine Sensors
2.1.1. Phase-Based Control and Physical Sensors
2.1.2. Myoelectric-Based Control and Biosensors
2.2. Low-Level Control and Machine–Machine Sensors
| Actuation Principle | Actuator Type | Portability | References |
|---|---|---|---|
| Pneumatic | Artificial Pneumatic Muscles (PAM) | Yes | [131,146,174,175,176] |
| No | [11,38,49,50,62,63,88,89,90,91,92,93,95,96,97,98,99,132,133,134,135,142,179,190,191,192,193,194,195,196,197,198,199,200,201,203] | ||
| Pneumatic Cylinders | Yes | [43,166,167,168,169,170,171] | |
| Exosuit Pneumatic Source (Soft Fabric Actuator) | No | [156,232] | |
| Soft Fiber Braided Bending Actuator | No | [211] | |
| Electric | Brushed DC Motors | Yes | [115,172] |
| No | [86,121] | ||
| Brushless DC Motors | Yes | [37,39,40,42,57,65,66,76,77,78,79,80,81,82,83,84,100,101,102,111,112,113,117,118,122,123,127,157,158,159,160,178,184,185,186,187] | |
| No | [64,103,104,105,106,107,108,109,110,116,124,125,129,143,147,148,149,150,151,161,162,163,164,165,210] | ||
| Servo DC Motors | Yes | [74,75,87,119,120,144,145,177] | |
| No | [141] | ||
| Servo AC Motors | No | [53,58,68,69,70,71,72,73,180,181,182,183,202,204] | |
| Stepper Motor | No | [189] | |
| Permanent Magnetic Synchronous Motors | No | [85] | |
| Electromechanical DC Voice Coil Actuator | No | [154,155] | |
| Electrohydraulic Hybrid Drive System | Yes | [173] | |
| No | [138,139,140] | ||
| Electric Motors (Type Not Specified) | Yes | [56,114] | |
| No | [41,126,128] | ||
| Series Elastic | Brushed DC Motors | Yes | [234,235] |
| No | [67] | ||
| Brushless DC Motors | Yes | [130] | |
| No | [10,54,55,59,60,61,136,152,153,188,207] | ||
| Not Specified | [236] | ||
| Servo DC Motors | No | [137] | |
| Electric Motors (Type Not Specified) | Yes | [206] | |
| No | [205] | ||
| Dielectric Elastomer | Polyimide Fibers | Yes | [94] |
3. Towards Fully Autonomous Portable PAEs
Role of Wearable Sensors in Developing Autonomous Portable Ankle Exoskeletons
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alqahtani, M.S.; Cooper, G.; Diver, C.; Bártolo, P.J. Exoskeletons for Lower Limb Applications: A Review. In Bio-Materials and Prototyping Applications in Medicine; Springer International Publishing: Berlin/Heidelberg, Germany, 2021; pp. 139–164. [Google Scholar] [CrossRef]
- Kubasad, P.R.; Todeti, S.R.; Kamat, Y.D. A Review on Designs of Various Ankle Foot Orthosis (AFO) Used to Treat Drop Foot Disease. In Mechanism and Machine Science; Springer Singapore: Singapore, 2021; pp. 789–807. [Google Scholar] [CrossRef]
- World Health Organization. World Report on Disability; World Health Organization: Geneva, Switzerland, 2011; Available online: https://www.who.int/teams/noncommunicable-diseases/sensory-functions-disability-and-rehabilitation/world-report-on-disability (accessed on 11 March 2022).
- Herr, H. Exoskeletons and orthoses: Classification, design challenges and future directions. J. Neuroeng. Rehabil. 2009, 6, 21. [Google Scholar] [CrossRef] [PubMed]
- Proud, J.K.; Lai, D.T.; Mudie, K.L.; Carstairs, G.L.; Billing, D.C.; Garofolini, A.; Begg, R.K. Exoskeleton Application to Military Manual Handling Tasks. Hum. Factors 2020, 0018720820957467. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Bumpusher-A Powered Aid to Locomotion; World Health Organization: Geneva, Switzerland, 1963. [Google Scholar]
- Gilbert, K. Exoskeleton Prototype Project: Final Report on Phase I; General Electric Company: Schenectady, NY, USA, 1967. [Google Scholar]
- Jaukovic, N. Active peroneal orthosis. In Proceedings of the International Symposium on External Control of Human Extremities; Yugoslav Committee for Electronics and Automation: Belgrade, Serbia, 1981; pp. 13–20. [Google Scholar]
- Dollar, A.M.; Herr, H. Lower Extremity Exoskeletons and Active Orthoses: Challenges and State-of-the-Art. IEEE Trans. Robot. 2008, 24, 144–158. [Google Scholar] [CrossRef]
- Blaya, J.A.; Herr, H. Adaptive control of a variable-impedance ankle-foot orthosis to assist drop-foot gait. IEEE Trans. Neural Syst. Rehabil. Eng. 2004, 12, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Ferris, D.P.; Czerniecki, J.M.; Hannaford, B. An ankle-foot orthosis powered by artificial pneumatic muscles. J. Appl. Biomech. 2005, 21, 189–197. [Google Scholar] [CrossRef] [PubMed]
- Hollander, K.W.; Ilg, R.; Sugar, T.G.; Herring, D. An efficient robotic tendon for gait assistance. J. Biomech. Eng. 2006, 128, 788–791. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, A.; Banala, S.K.; Agrawal, S.K.; Binder-Macleod, S.A. Design of a two degree-of-freedom ankle-foot orthosis for robotic rehabilitation. In Proceedings of the 9th International Conference on Rehabilitation Robotics, ICORR 2005, Chicago, IL, USA, 28 June–1 July 2005; IEEE: Piscataway, NJ, USA, 2005. [Google Scholar]
- Jimenez-Fabian, R.; Verlinden, O. Review of control algorithms for robotic ankle systems in lower-limb orthoses, prostheses, and exoskeletons. Med. Eng. Phys. 2012, 34, 397–408. [Google Scholar] [CrossRef]
- Brockett, C.L.; Chapman, G.J. Biomechanics of the ankle. Orthop. Trauma 2016, 30, 232–238. [Google Scholar] [CrossRef]
- Best, R.; Begg, R. Overview of movement analysis and gait features. In Computational Intelligence for Movement Sciences: Neural Networks and Other Emerging Techniques; IGI Global: Hershey, PA, USA, 2006; pp. 1–69. [Google Scholar]
- Neumann, D.A. Kinesiology of the Musculoskeletal System-E-Book: Foundations for Rehabilitation; Elsevier Health Sciences: Amsterdam, The Netherlands, 2016. [Google Scholar]
- Whittle, M.W. Gait Analysis: An Introduction; Butterworth-Heinemann: Oxford, UK, 2014. [Google Scholar]
- Nagano, H.; James, L.; Sparrow, W.A.; Begg, R.K. Effects of walking-induced fatigue on gait function and tripping risks in older adults. J. Neuroeng. Rehabil. 2014, 11, 1–7. [Google Scholar] [CrossRef]
- Lythgo, N.; Begg, R.; Best, R. Stepping responses made by elderly and young female adults to approach and accommodate known surface height changes. Gait Posture 2007, 26, 82–89. [Google Scholar] [CrossRef]
- Khandoker, A.H.; Lynch, K.; Karmakar, C.K.; Begg, R.K.; Palaniswami, M. Toe clearance and velocity profiles of young and elderly during walking on sloped surfaces. J. Neuroeng. Rehabil. 2010, 7, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Tamburini, P.; Storm, F.; Buckley, C.; Bisi, M.C.; Stagni, R.; Mazzà, C. Moving from laboratory to real life conditions: Influence on the assessment of variability and stability of gait. Gait Posture 2018, 59, 248–252. [Google Scholar] [CrossRef] [PubMed]
- Benson, L.C.; Clermont, C.A.; Bošnjak, E.; Ferber, R. The use of wearable devices for walking and running gait analysis outside of the lab: A systematic review. Gait Posture 2018, 63, 124–138. [Google Scholar] [CrossRef] [PubMed]
- Khoshmanesh, F.; Thurgood, P.; Pirogova, E.; Nahavandi, S.; Baratchi, S. Wearable sensors: At the frontier of personalised health monitoring, smart prosthetics and assistive technologies. Biosens. Bioelectron. 2021, 176, 112946. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, A.; Rocchi, L.; van den Noort, J.; Harlaar, J. Toward the Use of Wearable Inertial Sensors to Train Gait in Subjects with Movement Disorders. In Converging Clinical and Engineering Research on Neurorehabilitation; Springer: Berlin/Heidelberg, Germany, 2013; pp. 937–940. [Google Scholar] [CrossRef]
- Vavasour, G.; Giggins, O.M.; Doyle, J.; Kelly, D. How wearable sensors have been utilised to evaluate frailty in older adults: A systematic review. J. Neuroeng. Rehabil. 2021, 18, 112. [Google Scholar] [CrossRef] [PubMed]
- Santhiranayagam, B.K.; Lai, D.T.; Jiang, C.; Shilton, A.; Begg, R. Automatic detection of different walking conditions using inertial sensor data. In Proceedings of the 2012 International Joint Conference on Neural Networks (IJCNN), Brisbane, Australia, 10–15 June 2012; IEEE: Piscataway, NJ, USA, 2012. [Google Scholar]
- Santhiranayagam, B.K.; Lai, D.; Shilton, A.; Begg, R.; Palaniswami, M. Regression models for estimating gait parameters using inertial sensors. In Proceedings of the 2011 Seventh International Conference on Intelligent Sensors, Sensor Networks and Information Processing, Adelaide, Australia, 6–9 December 2011; IEEE: Piscataway, NJ, USA, 2011. [Google Scholar]
- Lai, D.T.; Begg, R.K.; Palaniswami, M. Computational intelligence in gait research: A perspective on current applications and future challenges. IEEE Trans. Inf. Technol. Biomed. 2009, 13, 687–702. [Google Scholar] [CrossRef] [PubMed]
- del Carmen Sanchez-Villamañan, M.; Gonzalez-Vargas, J.; Torricelli, D.; Moreno, J.C.; Pons, J.L. Compliant lower limb exoskeletons: A comprehensive review on mechanical design principles. J. Neuroeng. Rehabil. 2019, 16, 55. [Google Scholar] [CrossRef] [PubMed]
- Hussain, S.; Jamwal, P.K.; Ghayesh, M.H. State-of-the-art robotic devices for ankle rehabilitation: Mechanism and control review. Proc. Inst. Mech. Eng. H 2017, 231, 1224–1234. [Google Scholar] [CrossRef] [PubMed]
- Kalita, B.; Narayan, J.; Dwivedy, S.K. Development of Active Lower Limb Robotic-Based Orthosis and Exoskeleton Devices: A Systematic Review. Int. J. Soc. Robot. 2020, 13, 775–793. [Google Scholar] [CrossRef]
- Jiang, J.; Lee, K.-M.; Ji, J. Review of anatomy-based ankle–foot robotics for mind, motor and motion recovery following stroke: Design considerations and needs. Int. J. Intell. Robot. Appl. 2018, 2, 267–282. [Google Scholar] [CrossRef]
- Shi, B.; Chen, X.; Yue, Z.; Yin, S.; Weng, Q.; Zhang, X.; Wang, J.; Wen, W. Wearable Ankle Robots in Post-stroke Rehabilitation of Gait: A Systematic Review. Front. Neurorobot. 2019, 13, 63. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Perez, M.G.; Garcia-Murillo, M.A.; Cervantes-Sanchez, J.J. Robot-assisted ankle rehabilitation: A review. Disabil. Rehabil. Assist. Technol. 2019, 15, 394–408. [Google Scholar] [CrossRef] [PubMed]
- Moltedo, M.; Bacek, T.; Verstraten, T.; Rodriguez-Guerrero, C.; Vanderborght, B.; Lefeber, D. Powered ankle-foot orthoses: The effects of the assistance on healthy and impaired users while walking. J. Neuroeng. Rehabil. 2018, 15, 86. [Google Scholar] [CrossRef] [PubMed]
- Fang, Y.; Orekhov, G.; Lerner, Z.F. Adaptive ankle exoskeleton gait training demonstrates acute neuromuscular and spatiotemporal benefits for individuals with cerebral palsy: A pilot study. Gait Posture 2020. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.S.; Baek, Y.S. Effects of the degree of freedom and assistance characteristics of powered ankle-foot orthoses on gait stability. PLoS ONE 2020, 15, e0242000. [Google Scholar] [CrossRef] [PubMed]
- Bougrinat, Y.; Achiche, S.; Raison, M. Design and development of a lightweight ankle exoskeleton for human walking augmentation. Mechatronics 2019, 64, 102297. [Google Scholar] [CrossRef]
- Guerrero-Castellanos, J.F.; Rifaï, H.; Arnez-Paniagua, V.; Linares-Flores, J.; Saynes-Torres, L.; Mohammed, S. Robust Active Disturbance Rejection Control via Control Lyapunov Functions: Application to Actuated-Ankle–Foot-Orthosis. Control. Eng. Pract. 2018, 80, 49–60. [Google Scholar] [CrossRef]
- Sloot, L.; Bae, J.; Baker, L.; O’Donnell, K.; Menard, N.; Porciuncula, F.; Choe, D.; Ellis, T.; Awad, L.; Walsh, C. O 089—A soft robotic exosuit assisting the paretic ankle in patients post-stroke: Effect on muscle activation during overground walking. Gait Posture 2018. [Google Scholar] [CrossRef] [PubMed]
- Emmens, A.R.; van Asseldonk, E.H.F.; van der Kooij, H. Effects of a powered ankle-foot orthosis on perturbed standing balance. J. Neuroeng. Rehabil. 2018, 15, 50. [Google Scholar] [CrossRef] [PubMed]
- Boes, M.K.; Bollaert, R.E.; Kesler, R.M.; Learmonth, Y.C.; Islam, M.; Petrucci, M.N.; Motl, R.W.; Hsiao-Wecksler, E.T. Six-Minute Walk Test Performance in Persons With Multiple Sclerosis While Using Passive or Powered Ankle-Foot Orthoses. Arch. Phys. Med. Rehabil. 2018, 99, 484–490. [Google Scholar] [CrossRef] [PubMed]
- Yin, K.; Pang, M.; Xiang, K.; Jing, C. Optimization Parameters of PID Controller for Powered Ankle-Foot Prosthesis Based on CMA Evolution Strategy; IEEE: Piscataway, NJ, USA, 2018. [Google Scholar] [CrossRef]
- Al-Shuka, H.F.N.; Rahman, M.H.; Leonhardt, S.; Ciobanu, I.; Berteanu, M. Biomechanics, actuation, and multi-level control strategies of power-augmentation lower extremity exoskeletons: An overview. Int. J. Dyn. Control. 2019, 7, 1462–1488. [Google Scholar] [CrossRef]
- Elmenreich, W. An Introduction to Sensor Fusion; Vienna University of Technology: Vienna, Austria, 2002; Volume 502, pp. 1–28. [Google Scholar]
- Novak, D.; Riener, R. A survey of sensor fusion methods in wearable robotics. Robot. Auton. Syst. 2015, 73, 155–170. [Google Scholar] [CrossRef]
- Antoniou, A. Digital Signal Processing; McGraw-Hill: Toronto, ON, Canada, 2006. [Google Scholar]
- Sawicki, G.S.; Gordon, K.E.; Ferris, D.P. Powered Lower Limb Orthoses: Applications in Motor Adaptation and Rehabilitation; IEEE: Piscataway, NJ, USA, 2005. [Google Scholar] [CrossRef]
- Sawicki, G.S.; Domingo, A.; Ferris, D.P. The effects of powered ankle-foot orthoses on joint kinematics and muscle activation during walking in individuals with incomplete spinal cord injury. J. Neuroeng. Rehabil. 2006, 3, 3. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kapsalyamov, A.; Jamwal, P.K.; Hussain, S.; Ghayesh, M.H. State of the Art Lower Limb Robotic Exoskeletons for Elderly Assistance. IEEE Access 2019, 7, 95075–95086. [Google Scholar] [CrossRef]
- Sharbafi, M.; Naseri, A.; Seyfarth, A.; Grimmer, M. Neural Control in Prostheses and Exoskeletons. In Powered Prostheses; Elsevier: Amsterdam, The Netherlands, 2020; pp. 153–178. [Google Scholar] [CrossRef]
- Zhao, J.; Yang, T.; Sun, X.; Dong, J.; Wang, Z.; Yang, C. Sliding mode control combined with extended state observer for an ankle exoskeleton driven by electrical motor. Mechatronics 2021, 76, 102554. [Google Scholar] [CrossRef]
- Shao, Y.; Zhang, W.; Xu, K.; Ding, X. Design of a Novel Compact Adaptive Ankle Exoskeleton for Walking Assistance. In Advances in Mechanism and Machine Science; Springer International Publishing: Berlin/Heidelberg, Germany, 2019; pp. 2159–2168. [Google Scholar] [CrossRef]
- Shao, Y.; Zhang, W.; Su, Y.; Ding, X. Design and optimisation of load-adaptive actuator with variable stiffness for compact ankle exoskeleton. Mech. Mach. Theory 2021, 161, 104323. [Google Scholar] [CrossRef]
- Xing, K.; Wang, Y.; Chen, D.; Wang, M.; Lu, S. Flexible Ankle-Assisted Robot Technology Based on Rope Drive; IEEE: Piscataway, NJ, USA, 2020. [Google Scholar] [CrossRef]
- Wang, T.-M.; Pei, X.; Hou, T.-G.; Fan, Y.-B.; Yang, X.; Herr, H.M.; Yang, X.-B. An untethered cable-driven ankle exoskeleton with plantarflexion-dorsiflexion bidirectional movement assistance. Front. Inf. Technol. Electron. Eng. 2020, 21, 723–739. [Google Scholar] [CrossRef]
- Jackson, R.W.; Collins, S.H. An experimental comparison of the relative benefits of work and torque assistance in ankle exoskeletons. J. Appl. Physiol. 2015, 119, 541–557. [Google Scholar] [CrossRef] [PubMed]
- Hwang, S.; Kim, J.; Yi, J.; Tae, K.; Ryu, K.; Kim, Y. Development of an active ankle foot orthosis for the prevention of foot drop and toe drag. In Proceedings of the 2006 International Conference on Biomedical and Pharmaceutical Engineering, Singapore, 11–14 December 2006; IEEE: Piscataway, NJ, USA, 2007. [Google Scholar]
- Kim, J.; Hwang, S.; Kim, Y. Development of an active ankle-foot orthosis for hemiplegic patients. In Proceedings of the 1st international convention on Rehabilitation engineering & assistive technology: In conjunction with 1st Tan Tock Seng Hospital Neurorehabilitation Meeting, Singapore, 23–26 April 2007. [Google Scholar]
- Kim, J.; Hwang, S.; Sohn, R.; Lee, Y.; Kim, Y. Development of an active ankle foot orthosis to prevent foot drop and toe drag in hemiplegic patients: A preliminary study. Appl. Bionics Biomech. 2011, 8, 377–384. [Google Scholar] [CrossRef]
- Choi, H.S.; Lee, C.H.; Baek, Y.S. Design and Validation of a Two-Degree-of-Freedom Powered Ankle-Foot Orthosis with Two Pneumatic Artificial Muscles. Mechatronics 2020, 72, 102469. [Google Scholar] [CrossRef]
- Choi, H.S.; Lee, C.H.; Baek, Y.S. Design of a Pneumatic Actuated Ankle-Foot Orthosis which Has Talocrural and Subtalar Joint; IEEE: Piscataway, NJ, USA, 2019. [Google Scholar] [CrossRef]
- Lee, T.; Kim, I.; Baek, Y.S. Design of a 2DoF Ankle Exoskeleton with a Polycentric Structure and a Bi-Directional Tendon-Driven Actuator Controlled Using a PID Neural Network. Actuators 2021, 10, 9. [Google Scholar] [CrossRef]
- Choi, H.; Park, Y.J.; Seo, K.; Lee, J.; Lee, S.-E.; Shim, Y. A Multifunctional Ankle Exoskeleton for Mobility Enhancement of Gait-Impaired Individuals and Seniors. IEEE Robot. Autom. Lett. 2018, 3, 411–418. [Google Scholar] [CrossRef]
- Seo, K.; Park, Y.J.; Lee, J.; Hyung, S.; Lee, M.; Kim, J.; Choi, H.; Shim, Y. RNN-Based on-Line Continuous Gait Phase Estimation from Shank-Mounted IMUs to Control Ankle Exoskeletons; IEEE: Piscataway, NJ, USA, 2019. [Google Scholar] [CrossRef]
- Kirtas, O.; Savas, Y.; Bayraker, M.; Baskaya, F.; Basturk, H.; Samur, E. Design, implementation, and evaluation of a backstepping control algorithm for an active ankle–foot orthosis. Control. Eng. Pract. 2021, 106, 104667. [Google Scholar] [CrossRef]
- Zhang, J.; Cheah, C.C.; Collins, S.H. Experimental Comparison of Torque Control Methods on an Ankle Exoskeleton during Human Walking; IEEE: Piscataway, NJ, USA, 2015. [Google Scholar] [CrossRef]
- Witte, K.A.; Zhang, J.; Jackson, R.W.; Collins, S.H. Design of two lightweight, high-bandwidth torque-controlled ankle exoskeletons. In Proceedings of the 2015 IEEE International Conference on Robotics and Automation (ICRA), Seattle, WA, USA, 26–30 May 2015; IEEE: Piscataway, NJ, USA. [Google Scholar]
- Zhang, J.; Fiers, P.; Witte, K.A.; Jackson, R.W.; Poggensee, K.L.; Atkeson, C.G.; Collins, S.H. Human-in-the-loop optimization of exoskeleton assistance during walking. Science 2017, 356, 1280–1284. [Google Scholar] [CrossRef] [PubMed]
- Steele, K.M.; Jackson, R.W.; Shuman, B.R.; Collins, S.H. Muscle recruitment and coordination with an ankle exoskeleton. J. Biomech. 2017, 59, 50–58. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Chen, J.; Ji, Y.; Jin, W.; Liu, J.; Zhang, J. Evaluation of Lower Leg Muscle Activities During Human Walking Assisted by an Ankle Exoskeleton. IEEE Trans. Ind. Inform. 2020, 16, 7168–7176. [Google Scholar] [CrossRef]
- Witte, K.A.; Fiers, P.; Sheets-Singer, A.L.; Collins, S.H. Improving the energy economy of human running with powered and unpowered ankle exoskeleton assistance. Sci. Robot. 2020, 5, eaay9108. [Google Scholar] [CrossRef] [PubMed]
- Manchola, M.; Serrano, D.; Gómez, D.; Ballen, F.; Casas, D.; Munera, M.; Cifuentes, C.A. T-FLEX: Variable stiffness ankle-foot orthosis for gait assistance. In International Symposium on Wearable Robotics; Springer: Berlin/Heidelberg, Germany, 2018. [Google Scholar]
- Gomez-Vargas, D.; Ballen-Moreno, F.; Barria, P.; Aguilar, R.; Azorin, J.M.; Munera, M.; Cifuentes, C.A. The Actuation System of the Ankle Exoskeleton T-FLEX: First Use Experimental Validation in People with Stroke. Brain Sci. 2021, 11, 412. [Google Scholar] [CrossRef] [PubMed]
- Lerner, Z.F.; Gasparri, G.M.; Bair, M.O.; Lawson, J.L.; Luque, J.; Harvey, T.A.; Lerner, A.T. An Untethered Ankle Exoskeleton Improves Walking Economy in a Pilot Study of Individuals with Cerebral Palsy. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 1985–1993. [Google Scholar] [CrossRef] [PubMed]
- Gasparri, G.M.; Bair, M.O.; Libby, R.P.; Lerner, Z.F. Verification of a Robotic Ankle Exoskeleton Control Scheme for Gait Assistance in Individuals with Cerebral Palsy; IEEE: Piscataway, NJ, USA, 2018. [Google Scholar] [CrossRef]
- Lerner, Z.F.; Harvey, T.A.; Lawson, J.L. A Battery-Powered Ankle Exoskeleton Improves Gait Mechanics in a Feasibility Study of Individuals with Cerebral Palsy. Ann. Biomed. Eng. 2019, 47, 1345–1356. [Google Scholar] [CrossRef] [PubMed]
- Lerner, Z.F.; Conner, B.C.; Remec, N.M. Adaptation of Gait Energetics to Ankle Exoskeleton Assistance within and across Visits: A Clinical Case Series; IEEE: Piscataway, NJ, USA, 2019. [Google Scholar] [CrossRef]
- Gasparri, G.M.; Luque, J.; Lerner, Z.F. Proportional Joint-Moment Control for Instantaneously Adaptive Ankle Exoskeleton Assistance. IEEE Trans. Neural Syst. Rehabil. Eng. 2019, 27, 751–759. [Google Scholar] [CrossRef] [PubMed]
- Orekhov, G.; Fang, Y.; Luque, J.; Lerner, Z.F. Ankle Exoskeleton Assistance Can Improve Over-Ground Walking Economy in Individuals with Cerebral Palsy. IEEE Trans. Neural Syst. Rehabil. Eng. 2020, 28, 461–467. [Google Scholar] [CrossRef]
- Jain, T.K.; Carter, V.; Lerner, Z.F. Effects of Lightweight Wearable Ankle Exoskeleton in an Individual With Parkinson Disease. Top. Geriatr. Rehabil. 2020, 36, 146–151. [Google Scholar] [CrossRef]
- Conner, B.C.; Luque, J.; Lerner, Z.F. Adaptive Ankle Resistance from a Wearable Robotic Device to Improve Muscle Recruitment in Cerebral Palsy. Ann. Biomed. Eng. 2020, 48, 1309–1321. [Google Scholar] [CrossRef] [PubMed]
- Fang, Y.; Lerner, Z.F. Feasibility of Augmenting Ankle Exoskeleton Walking Performance with Step Length Biofeedback in Individuals With Cerebral Palsy. IEEE Trans. Neural Syst. Rehabil. Eng. 2021, 29, 442–449. [Google Scholar] [CrossRef]
- Lv, G.; Zhu, H.; Elery, T.; Li, L.; Gregg, R.D. Experimental implementation of underactuated potential energy shaping on a powered ankle-foot orthosis. In Proceedings of the 2016 IEEE International Conference on Robotics and Automation (ICRA), Stockholm, Sweden, 16–21 May 2016; IEEE: Piscataway, NJ, USA, 2016. [Google Scholar]
- Zhou, Y.; Lu, L. Development and Testing of a User-Adaptive Ankle Foot Orthosis; IEEE: Piscataway, NJ, USA, 2020. [Google Scholar] [CrossRef]
- Kwon, J.; Park, J.-H.; Ku, S.; Jeong, Y.; Paik, N.-J.; Park, Y.-L. A Soft Wearable Robotic Ankle-Foot-Orthosis for Post-Stroke Patients. IEEE Robot. Autom. Lett. 2019, 4, 2547–2552. [Google Scholar] [CrossRef]
- Gordon, K.E.; Sawicki, G.S.; Ferris, D.P. Mechanical performance of artificial pneumatic muscles to power an ankle-foot orthosis. J. Biomech. 2006, 39, 1832–1841. [Google Scholar] [CrossRef] [PubMed]
- Cain, S.M.; Gordon, K.E.; Ferris, D.P. Locomotor adaptation to a powered ankle-foot orthosis depends on control method. J. Neuroeng. Rehabil. 2007, 4, 48. [Google Scholar] [CrossRef]
- Malcolm, P.; Fiers, P.; Segers, V.; van Caekenberghe, I.; Lenoir, M.; De Clercq, D. Experimental study on the role of the ankle push off in the walk-to-run transition by means of a powered ankle-foot-exoskeleton. Gait Posture 2009, 30, 322–327. [Google Scholar] [CrossRef]
- Malcolm, P.; Derave, W.; Galle, S.; de Clercq, D. A simple exoskeleton that assists plantarflexion can reduce the metabolic cost of human walking. PLoS ONE 2013, 8, e56137. [Google Scholar] [CrossRef]
- Galle, S.; Malcolm, P.; Derave, W.; De Clercq, D. Adaptation to walking with an exoskeleton that assists ankle extension. Gait Posture 2013, 38, 495–499. [Google Scholar] [CrossRef] [PubMed]
- Galle, S.; Malcolm, P.; Derave, W.; De Clercq, D. Enhancing performance during inclined loaded walking with a powered ankle-foot exoskeleton. Eur. J. Appl. Physiol. 2014, 114, 2341–2351. [Google Scholar] [CrossRef] [PubMed]
- Allen, D.P.; Little, R.; Laube, J.; Warren, J.; Voit, W.; Gregg, R.D. Towards an ankle-foot orthosis powered by a dielectric elastomer actuator. Mechatronics 2021, 76, 102551. [Google Scholar] [CrossRef]
- Galle, S.; Malcolm, P.; Derave, W.; de Clercq, D. Uphill walking with a simple exoskeleton: Plantarflexion assistance leads to proximal adaptations. Gait Posture 2015, 41, 246–251. [Google Scholar] [CrossRef] [PubMed]
- Koller, J.R.; Gates, D.H.; Ferris, D.P.; Remy, C.D. ‘Body-in-the-Loop’Optimization of Assistive Robotic Devices: A Validation Study. In Robotics: Science and Systems; MIT Press: Cambridge, MA, USA, 2016. [Google Scholar] [CrossRef]
- Galle, S.; Malcolm, P.; Collins, S.H.; De Clercq, D. Reducing the metabolic cost of walking with an ankle exoskeleton: Interaction between actuation timing and power. J. Neuroeng. Rehabil. 2017, 14, 35. [Google Scholar] [CrossRef] [PubMed]
- Galle, S.; Derave, W.; Bossuyt, F.; Calders, P.; Malcolm, P.; De Clercq, D. Exoskeleton plantarflexion assistance for elderly. Gait Posture 2017, 52, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Antonellis, P.; Galle, S.; de Clercq, D.; Malcolm, P. Altering gait variability with an ankle exoskeleton. PLoS ONE 2018, 13, e0205088. [Google Scholar] [CrossRef] [PubMed]
- Meijneke, C.; van Dijk, W.; van der Kooij, H. Achilles: An Autonomous Lightweight Ankle Exoskeleton to Provide Push-off Power; IEEE: Piscataway, NJ, USA, 2014. [Google Scholar] [CrossRef]
- Pinheiro, C.; Figueiredo, J.; Magalhaes, N.; Santos, C.P. Wearable Biofeedback Improves Human-Robot Compliance during Ankle-Foot Exoskeleton-Assisted Gait Training: A Pre-Post Controlled Study in Healthy Participants. Sensors 2020, 20, 5876. [Google Scholar] [CrossRef] [PubMed]
- Lopes, J.; Pinheiro, C.; Figueiredo, J.; Reis, L.P.; Santos, C.P. Assist-as-Needed Impedance Control Strategy for a Wearable Ankle Robotic Orthosis; IEEE: Piscataway, NJ, USA, 2020. [Google Scholar] [CrossRef]
- Moltedo, M.; Bacek, T.; Junius, K.; Vanderborght, B.; Lefeber, D. Mechanical Design of a Lightweight Compliant and Adaptable Active Ankle Foot Orthosis; IEEE: Piscataway, NJ, USA, 2016. [Google Scholar] [CrossRef]
- Moltedo, M.; Bacek, T.; Langlois, K.; Junius, K.; Vanderborght, B.; Lefeber, D. Design and Experimental Evaluation of a Lightweight, High-Torque and Compliant Actuator for an Active Ankle Foot Orthosis; IEEE: Piscataway, NJ, USA, 2017. [Google Scholar] [CrossRef]
- Moltedo, M.; Bacek, T.; Langlois, K.; Junius, K.; Vanderborght, B.; Lefeber, D. A Compliant Lightweight and Adaptable Active Ankle Foot Orthosis for Robotic Rehabilitation. In Wearable Robotics: Challenges and Trends; Springer International Publishing: Berlin/Heidelberg, Germany, 2017; pp. 45–49. [Google Scholar] [CrossRef]
- Moltedo, M.; Cavallo, G.; Baček, T.; Lataire, J.; Vanderborght, B.; Lefeber, D.; Rodriguez-Guerrero, C. Variable stiffness ankle actuator for use in robotic-assisted walking: Control strategy and experimental characterization. Mech. Mach. Theory 2019, 134, 604–624. [Google Scholar] [CrossRef]
- Moltedo, M.; Bacek, T.; Serrien, B.; Langlois, K.; Vanderborght, B.; Lefeber, D.; Rodriguez-Guerrero, C. Walking with a powered ankle-foot orthosis: The effects of actuation timing and stiffness level on healthy users. J. Neuroeng. Rehabil. 2020, 17, 98. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Kleinmann, R.J.; Nolan, K.J.; Zanotto, D. Design and Evaluation of an Active/Semiactive Ankle-Foot Orthosis for Gait Training; IEEE: Piscataway, NJ, USA, 2018. [Google Scholar] [CrossRef]
- Zhang, Y.; Nolan, K.J.; Zanotto, D. Oscillator-Based Transparent Control of an Active/Semiactive Ankle-Foot Orthosis. IEEE Robot. Autom. Lett. 2019, 4, 247–253. [Google Scholar] [CrossRef]
- Zhang, Y.; Kleinmann, R.J.; Nolan, K.J.; Zanotto, D. Preliminary Validation of a Cable-Driven Powered Ankle–Foot Orthosis with Dual Actuation Mode. IEEE Trans. Med. Robot. Bionics 2019, 1, 30–37. [Google Scholar] [CrossRef]
- Mooney, L.M.; Rouse, E.J.; Herr, H.M. Autonomous exoskeleton reduces metabolic cost of human walking during load carriage. J. Neuroeng. Rehabil. 2014, 11, 80. [Google Scholar] [CrossRef] [PubMed]
- Mooney, L.M.; Herr, H.M. Biomechanical walking mechanisms underlying the metabolic reduction caused by an autonomous exoskeleton. J. Neuroeng. Rehabil. 2016, 13, 4. [Google Scholar] [CrossRef] [PubMed]
- Wu, A.; Yang, X.; Kuan, J.-Y.; Herr, H.M. An Autonomous Exoskeleton for Ankle Plantarflexion Assistance; IEEE: Piscataway, NJ, USA, 2019. [Google Scholar] [CrossRef]
- Martinez-Hernandez, U.; Rubio-Solis, A.; Cedeno-Campos, V.; Dehghani-Sanij, A.A. Towards an Intelligent Wearable Ankle Robot for Assistance to Foot Drop; IEEE: Piscataway, NJ, USA, 2019. [Google Scholar] [CrossRef]
- Fu, C.; Xiong, C.; Liu, J. An Ankle Exoskeleton Using a Lightweight Motor to Create High Power Assistance for Push-Off. J. Mech. Robot. 2019, 11, 041001. [Google Scholar] [CrossRef]
- Dong, W.; Liu, C.; Zhang, Q.; Xiong, C. Design and Evaluation of an Active Ankle Exoskeleton in Gait Assistance; IEEE: Piscataway, NJ, USA, 2019. [Google Scholar] [CrossRef]
- Arnez-Paniagua, V.; Rifai, H.; Mohammed, S.; Amirat, Y. Adaptive Control of an Actuated Ankle Foot Orthosis for Foot-Drop Correction. IFAC-PapersOnLine 2017, 50, 1384–1389. [Google Scholar] [CrossRef]
- Arnez-Paniagua, V.; Rifaï, H.; Amirat, Y.; Ghedira, M.; Gracies, J.M.; Mohammed, S. Adaptive control of an actuated ankle foot orthosis for paretic patients. Control. Eng. Pract. 2019, 90, 207–220. [Google Scholar] [CrossRef]
- Yeung, L.F.; Ockenfeld, C.; Pang, M.K.; Wai, H.W.; Soo, O.Y.; Li, S.W.; Tong, K.Y. Design of an Exoskeleton Ankle Robot for Robot-assisted Gait Training of Stroke Patients; IEEE: Piscataway, NJ, USA, 2017. [Google Scholar] [CrossRef]
- Yeung, L.F.; Ockenfeld, C.; Pang, M.K.; Wai, H.W.; Soo, O.Y.; Li, S.W.; Tong, K.Y. Randomized controlled trial of robot-assisted gait training with dorsiflexion assistance on chronic stroke patients wearing ankle-foot-orthosis. J. Neuroeng. Rehabil. 2018, 15, 51. [Google Scholar] [CrossRef] [PubMed]
- Weerasingha, A.; Pragnathilaka, A.; Withanage, W.; Ranaweera, R.; Gopura, R. C-JAE: 3 DOF Robotic Ankle Exoskeleton with Compatible Joint Axes; IEEE: Piscataway, NJ, USA, 2018. [Google Scholar] [CrossRef]
- Asbeck, A.T.; De Rossi, S.M.M.; Holt, K.G.; Walsh, C.J. A biologically inspired soft exosuit for walking assistance. Int. J. Robot. Res. 2015, 34, 744–762. [Google Scholar] [CrossRef]
- Lee, S.; Crea, S.; Malcolm, P.; Galiana, I.; Asbeck, A.; Walsh, C. Controlling Negative and Positive Power at the Ankle with a Soft Exosuit; IEEE: Piscataway, NJ, USA, 2016. [Google Scholar] [CrossRef]
- Quinlivan, B.T.; Lee, S.; Malcolm, P.; Rossi, D.M.; Grimmer, M.; Siviy, C.; Karavas, N.; Wagner, D.; Asbeck, A.; Galiana, I.; et al. Assistance magnitude versus metabolic cost reductions for a tethered multiarticular soft exosuit. Sci. Robot. 2017, 2, eaah4416. [Google Scholar] [CrossRef] [PubMed]
- Malcolm, P.; Lee, S.; Crea, S.; Siviy, C.; Saucedo, F.; Galiana, I.; Panizzolo, F.A.; Holt, K.G.; Walsh, C.J. Varying negative work assistance at the ankle with a soft exosuit during loaded walking. J. Neuroeng. Rehabil. 2017, 14, 62. [Google Scholar] [CrossRef] [PubMed]
- Awad, L.N.; Bae, J.; O’Donnell, K.; de Rossi, S.M.M.; Hendron, K.; Sloot, L.H.; Kudzia, P.; Allen, S.; Holt, K.G.; Ellis, T.D.; et al. A soft robotic exosuit improves walking in patients after stroke. Sci. Transl. Med. 2017, 9, eaai9084. [Google Scholar] [CrossRef] [PubMed]
- Bae, J.; Siviy, C.; Rouleau, M.; Menard, N.; O’Donnell, K.; Geliana, I.; Athanassiu, M.; Ryan, D.; Bibeau, C.; Sloot, L.; et al. A Lightweight and Efficient Portable Soft Exosuit for Paretic Ankle Assistance in Walking after Stroke; IEEE: Piscataway, NJ, USA, 2018. [Google Scholar] [CrossRef]
- Bae, J.; Awad, L.N.; Long, A.; O’Donnell, K.; Hendron, K.; Holt, K.G.; Ellis, T.D.; Walsh, C.J. Biomechanical mechanisms underlying exosuit-induced improvements in walking economy after stroke. J. Exp. Biol. 2018, 221, jeb168815. [Google Scholar] [CrossRef] [PubMed]
- Grimmer, M.; Quinlivan, B.T.; Lee, S.; Malcolm, P.; Rossi, D.M.; Siviy, C.; Walsh, C.J. Comparison of the human-exosuit interaction using ankle moment and ankle positive power inspired walking assistance. J. Biomech. 2019, 83, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Esposito, E.R.; Schmidtbauer, K.A.; Wilken, J.M. Experimental comparisons of passive and powered ankle-foot orthoses in individuals with limb reconstruction. J. Neuroeng. Rehabil. 2018, 15, 111. [Google Scholar] [CrossRef] [PubMed]
- Noda, T.; Takai, A.; Teramae, T.; Hirookai, E.; Hase, K.; Morimoto, J. Robotizing Double-Bar Ankle-Foot Orthosis; IEEE: Piscataway, NJ, USA, 2018. [Google Scholar] [CrossRef]
- Koller, J.R.; Gates, D.H.; Ferris, D.P.; Remy, C.D. Confidence in the curve: Establishing instantaneous cost mapping techniques using bilateral ankle exoskeletons. J. Appl. Physiol. 2017, 122, 242–252. [Google Scholar] [CrossRef] [PubMed]
- Koller, J.R.; Remy, C.D.; Ferris, D.P. Comparing Neural Control and Mechanically Intrinsic Control of Powered Ankle Exoskeletons; IEEE: Piscataway, NJ, USA, 2017. [Google Scholar] [CrossRef]
- Koller, J.R.; Remy, C.D.; Ferris, D.P. Biomechanics and energetics of walking in powered ankle exoskeletons using myoelectric control versus mechanically intrinsic control. J. Neuroeng. Rehabil. 2018, 15, 42. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, D.A.; Koller, J.R.; Steele, K.M.; Ferris, D.P. Motor modules during adaptation to walking in a powered ankle exoskeleton. J. Neuroeng. Rehabil. 2018, 15, 2. [Google Scholar] [CrossRef] [PubMed]
- Baser, O.; Kizilhan, H. Mechanical design and preliminary tests of VS-AnkleExo. J. Braz. Soc. Mech. Sci. Eng. 2018, 40. [Google Scholar] [CrossRef]
- Chinh, N.D.; Tan, P.N.; Long, C.B.; Tien, N.T. Design of Force Support Device for Human Ankle Joint; IEEE: Piscataway, NJ, USA, 2017. [Google Scholar] [CrossRef]
- Noel, M.; Cantin, B.; Lambert, S.; Gosselin, C.M.; Bouyer, L.J. An electrohydraulic actuated ankle foot orthosis to generate force fields and to test proprioceptive reflexes during human walking. IEEE Trans. Neural Syst. Rehabil. Eng. 2008, 16, 390–399. [Google Scholar] [CrossRef]
- Noel, M.; Fortin, K.; Bouyer, L.J. Using an electrohydraulic ankle foot orthosis to study modifications in feedforward control during locomotor adaptation to force fields applied in stance. J. Neuroeng. Rehabil. 2009, 6, 16. [Google Scholar] [CrossRef] [PubMed]
- Belley, A.F.; Bouffard, J.; Brochu, K.; Mercier, C.; Roy, J.-S.; Bouyer, L. Development and reliability of a measure evaluating dynamic proprioception during walking with a robotized ankle-foot orthosis, and its relation to dynamic postural control. Gait Posture 2016, 49, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Dhule, S.V.; Shete, V.V.; Somani, S.B. Implementation of Adaptive Dorsiflexion and Plantar Flexion in Active Ankle Foot Orthosis; IEEE: Piscataway, NJ, USA, 2015. [Google Scholar] [CrossRef]
- Murphy, P.; Adolf, G.; Daly, S.; Bolton, M.; Maurice, O.; Bonia, T.; Mavroidis, C.; Yen, S.-C. Test of a Customized Compliant Ankle Rehabilitation Device in Unpowered Mode; IEEE: Piscataway, NJ, USA, 2014. [Google Scholar] [CrossRef]
- Polinkovsky, A.; Bachmann, R.J.; Kern, N.I.; Quinn, R.D. An Ankle Foot Orthosis with Insertion Point Eccentricity Control; IEEE: Piscataway, NJ, USA, 2012. [Google Scholar] [CrossRef]
- Patar, A.; Jamlus, N.; Makhtar, K.; Mahmud, J.; Komeda, T. Development of Dynamic Ankle Foot Orthosis for Therapeutic Application. Procedia Eng. 2012, 41, 1432–1440. [Google Scholar] [CrossRef][Green Version]
- Hamid, A.; Patar, M.N.A.A.; Ayub, M.A. Force Sensor Detection and Performance Evaluation of New Active System Ankle Foot Orthosis. Procedia Eng. 2012, 41, 510–515. [Google Scholar] [CrossRef]
- Bharadwaj, K.; Sugar, T.G.; Koeneman, J.B.; Koeneman, E.J. Design of a robotic gait trainer using spring over muscle actuators for ankle stroke rehabilitation. J. Biomech. Eng. 2005, 127, 1009–1013. [Google Scholar] [CrossRef] [PubMed]
- Oymagil, A.M.; Hitt, J.K.; Sugar, T.; Fleeger, J. Control of a Regenerative Braking Powered Ankle Foot Orthosis; IEEE: Piscataway, NJ, USA, 2007. [Google Scholar] [CrossRef]
- Hitt, J.; Oymagil, A.; Sugar, T.; Hollander, K.; Boehler, A.; Fleeger, J. Dynamically Controlled Ankle-Foot Orthosis (DCO) with Regenerative Kinetics: Incrementally Attaining User Portability; IEEE: Piscataway, NJ, USA, 2007. [Google Scholar] [CrossRef]
- Boehler, A.W.; Hollander, K.W.; Sugar, T.G.; Shin, D. Design, Implementation and Test Results of a Robust Control Method for a Powered Ankle Foot Orthosis (AFO); IEEE: Piscataway, NJ, USA, 2008. [Google Scholar] [CrossRef]
- Ward, J.; Sugar, T.; Standeven, J.; Engsberg, J.R. Stroke Survivor Gait Adaptation and Performance after Training on a Powered Ankle Foot Orthosis; IEEE: Piscataway, NJ, USA, 2010. [Google Scholar] [CrossRef]
- Ward, J.; Sugar, T.; Boehler, A.; Standeven, J.; Engsberg, J.R. Stroke Survivors’ Gait Adaptations to a Powered Ankle Foot Orthosis. Adv. Robot. 2011, 25, 1879–1901. [Google Scholar] [CrossRef] [PubMed]
- Caltran, C.; Siqueira, A.A.G.; Inoue, R.S.; Terra, M.H. Robust Filtering Applied to Position Estimation of an Active Ankle-Foot Orthosis. IFAC Proc. Vol. 2011, 44, 9391–9396. [Google Scholar] [CrossRef]
- Jardim, B.; Siqueira, A.A.G. Development and analysis of series elastic actuators for impedance control of an active ankle–foot orthosis. J. Braz. Soc. Mech. Sci. Eng. 2013, 36, 501–510. [Google Scholar] [CrossRef]
- Boiadjiev, G.V.; Veneva, I.P. Control System for Data Acquisition and Processing of Ankle-Foot Orthosis. IFAC Proc. Vol. 2009, 42, 597–602. [Google Scholar] [CrossRef]
- Veneva, I. Intelligent device for control of active ankle-foot orthosis. In Proceedings of the 7th IASTED International Conference on Biomedical Engineering, Innsbruck, Austria, 17–19 February 2010; Acta Press: Calgary, AB, Canada, 2010. [Google Scholar]
- Thalman, C.M.; Hertzell, T.; Lee, H. Toward a Soft Robotic Ankle-Foot Orthosis (SR-AFO) Exosuit for Human Locomotion: Preliminary Results in Late Stance Plantarflexion Assistance; IEEE: Piscataway, NJ, USA, 2020. [Google Scholar] [CrossRef]
- Ingraham, K.A.; Remy, C.D.; Rouse, E.J. User Preference of Applied Torque Characteristics for Bilateral Powered Ankle Exoskeletons; IEEE: Piscataway, NJ, USA, 2020. [Google Scholar] [CrossRef]
- Khazoom, C.; Veronneau, C.; Bigue, J.-P.L.; Grenier, J.; Girard, A.; Plante, J.-S. Design and Control of a Multifunctional Ankle Exoskeleton Powered by Magnetorheological Actuators to Assist Walking, Jumping, and Landing. IEEE Robot. Autom. Lett. 2019, 4, 3083–3090. [Google Scholar] [CrossRef]
- Arnez-Paniagua, V.; Rifai, H.; Amirat, Y.; Mohammed, S.; Ghedira, M.; Gracies, J.M. Modified Adaptive Control of an Actuated Ankle Foot Orthosis to Assist Paretic Patients; IEEE: Piscataway, NJ, USA, 2018. [Google Scholar] [CrossRef]
- Huo, W.; Arnez-Paniagua, V.; Ding, G.; Amirat, Y.; Mohammed, S. Adaptive Proxy-Based Controller of an Active Ankle Foot Orthosis to Assist Lower Limb Movements of Paretic Patients. Robotica 2019, 37, 2147–2164. [Google Scholar] [CrossRef]
- Roy, A.; Krebs, H.I.; Patterson, S.L.; Judkins, T.N.; Khanna, I.; Forrester, L.W.; Macko, R.M.; Hogan, N. Measurement of Human Ankle Stiffness Using the Anklebot; IEEE: Piscataway, NJ, USA, 2007. [Google Scholar] [CrossRef]
- Roy, A.; Krebs, H.I.; Williams, D.J.; Bever, C.T.; Forrester, L.W.; Macko, R.M.; Hogan, N. Robot-Aided Neurorehabilitation: A Novel Robot for Ankle Rehabilitation. IEEE Trans. Robot. 2009, 25, 569–582. [Google Scholar] [CrossRef]
- Roy, A.; Krebs, H.I.; Barton, J.E.; Macko, R.F.; Forrester, L.W. Anklebot-Assisted Locomotor Training after Stroke: A novel Deficit-Adjusted Control Approach; IEEE: Piscataway, NJ, USA, 2013. [Google Scholar] [CrossRef]
- Roy, A.; Krebs, H.I.; Iqbal, K.; Macko, N.R.; Macko, R.F.; Forrester, L.W. Facilitating Push-off Propulsion: A Biomechanical Model of Ankle Robotics Assistance for Plantarflexion Gait Training in Stroke; IEEE: Piscataway, NJ, USA, 2014. [Google Scholar] [CrossRef]
- Roy, A.; Chornay, C.; Forrester, L.W.; Hafer-Macko, C.E.; Macko, R.F. Quantifying Human Autonomy Recovery during Ankle Robot-Assisted Reversal of Foot Drop after Stroke; IEEE: Piscataway, NJ, USA, 2018. [Google Scholar] [CrossRef]
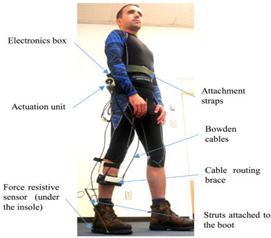
- Shorter, K.A.; Kogler, G.F.; Loth, E.; Durfee, W.K.; Hsiao-Wecksler, E.T. A portable powered ankle-foot orthosis for rehabilitation. J. Rehabil. Res. Dev. 2011, 48, 459–472. [Google Scholar] [CrossRef] [PubMed]
- Li, D.Y.; Becker, A.; Shorter, K.A.; Bretl, T.; Hsiao-Wecksler, E. Estimating system state during human walking with a powered ankle-foot orthosis. Mechatronics 2011, 16, 835–844. [Google Scholar] [CrossRef]
- Shorter, K.A.; Li, Y.; Morris, E.A.; Kogler, G.F.; Hsiao-Wecksler, E.T. Experimental Evaluation of a Portable Powered Ankle-Foot Orthosis; IEEE: Piscataway, NJ, USA, 2011. [Google Scholar] [CrossRef]
- Petrucci, M.N.; MacKinnon, C.D.; Hsiao-Wecksler, E.T. Modulation of Anticipatory Postural Adjustments of Gait Using a Portable Powered Ankle-Foot Orthosis; IEEE: Piscataway, NJ, USA, 2013. [Google Scholar] [CrossRef]
- Li, Y.D.; Hsiaowecksler, E.T. Gait Mode Recognition and Control for a Portable-Powered Ankle-Foot Orthosis; IEEE: Piscataway, NJ, USA, 2013. [Google Scholar] [CrossRef]
- Boes, M.K.; Islam, M.; Li, Y.D.; Hsiao-Wecksler, E.T. Fuel Efficiency of a Portable Powered Ankle-Foot Orthosis; IEEE: Piscataway, NJ, USA, 2013. [Google Scholar] [CrossRef]
- Xu, K.; Li, J.; Li, W.; Cai, X.; Xia, Z. A Hybrid Powered Ankle Exoskeleton for Walking; IEEE: Piscataway, NJ, USA, 2017. [Google Scholar] [CrossRef]
- Gu, G.M.; Kyeong, S.; Park, D.-S.; Kim, J. SMAFO: Stiffness Modulated Ankle Foot Orthosis for a Patient with Foot Drop; IEEE: Piscataway, NJ, USA, 2015. [Google Scholar] [CrossRef]
- Park, Y.-L.; Chen, B.-R.; Young, D.; Stirling, L.; Wood, R.J.; Goldfield, E.; Nagpal, R. Bio-Inspired Active Soft Orthotic Device for Ankle Foot Pathologies; IEEE: Piscataway, NJ, USA, 2011. [Google Scholar] [CrossRef]
- Park, Y.L.; Chen, B.R.; Perez-Arancibia, N.O.; Young, D.; Stirling, L.; Wood, R.J.; Goldfield, E.C.; Nagpal, R. Design and control of a bio-inspired soft wearable robotic device for ankle-foot rehabilitation. Bioinspir. Biomim. 2014, 9, 016007. [Google Scholar] [CrossRef] [PubMed]
- Ward, J.A.; Balasubramanian, S.; Sugar, T.; He, J. Robotic Gait Trainer Reliability and Stroke Patient Case Study. In Proceedings of the 2007 IEEE 10th International Conference on Rehabilitation Robotics, Noordwijk, The Netherlands, 13–15 June 2007. [Google Scholar] [CrossRef]
- Xia, H.; Kwon, J.; Pathak, P.; Ahn, J.; Shull, P.B.; Park, Y.-L. Design of A Multi-Functional Soft Ankle Exoskeleton for Foot-Drop Prevention, Propulsion Assistance, and Inversion/Eversion Stabilization; IEEE: Piscataway, NJ, USA, 2020. [Google Scholar] [CrossRef]
- van Dijk, W.; Meijneke, C.; van der Kooij, H. Evaluation of the Achilles Ankle Exoskeleton. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 25, 151–160. [Google Scholar] [CrossRef] [PubMed]
- Norris, J.A.; Granata, K.P.; Mitros, M.R.; Byrne, E.M.; Marsh, A.P. Effect of augmented plantarflexion power on preferred walking speed and economy in young and older adults. Gait Posture 2007, 25, 620–627. [Google Scholar] [CrossRef] [PubMed]
- Nuckols, R.W.; Sawicki, G.S. Impact of elastic ankle exoskeleton stiffness on neuromechanics and energetics of human walking across multiple speeds. J. Neuroeng. Rehabil. 2020, 17, 75. [Google Scholar] [CrossRef] [PubMed]
- Han, H.; Wang, W.; Zhang, F.; Li, X.; Chen, J.; Han, J.; Zhang, J. Selection of Muscle-Activity-Based Cost Function in Human-in-the-Loop Optimization of Multi-Gait Ankle Exoskeleton Assistance. IEEE Trans. Neural Syst. Rehabil. Eng. 2021, 29, 944–952. [Google Scholar] [CrossRef] [PubMed]
- Yan, H.; Tang, B.; Xiang, K.; Pang, M. Human-in-the-Loop Optimization Control for the Ankle Exoskeleton during Walking Based on Iterative Learning and Particle Swarm Optimization Algorithm; IEEE: Piscataway, NJ, USA, 2019. [Google Scholar] [CrossRef]
- Shafer, B.A.; Philius, S.A.; Nuckols, R.W.; McCall, J.; Young, A.J.; Sawicki, G.S. Neuromechanics and energetics of walking with an ankle exoskeleton using neuromuscular-model based control: A parameter study. Front. Bioeng. Biotechnol. 2021, 9, 615358. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.; Kim, J.; Hyung, S.; Lee, J.; Seo, K.; Park, Y.J.; Cho, J.; Choi, B.-k.; Shim, Y.; Choi, H. A Compact Ankle Exoskeleton with a Multiaxis Parallel Linkage Mechanism. IEEE/ASME Trans. Mechatron. 2021, 26, 191–202. [Google Scholar] [CrossRef]
- Dzeladini, F.; Wu, A.R.; Renjewski, D.; Arami, A.; Burdet, E.; van Asseldonk, E.; van der Kooij, H.; Ijspeert, A.J. Effects of a Neuromuscular Controller on a Powered Ankle Exoskeleton during Human Walking; IEEE: Piscataway, NJ, USA, 2016. [Google Scholar] [CrossRef]
- Tamburella, F.; Tagliamonte, N.L.; Pisotta, I.; Masciullo, M.; Arquilla, M.; van Asseldonk, E.H.F.; van der Kooij, H.; Wu, A.R.; Dzeladini, F.; Ijspeert, A.J.; et al. Neuromuscular Controller Embedded in a Powered Ankle Exoskeleton: Effects on Gait, Clinical Features and Subjective Perspective of Incomplete Spinal Cord Injured Subjects. IEEE Trans. Neural Syst. Rehabil. Eng. 2020, 28, 1157–1167. [Google Scholar] [CrossRef] [PubMed]
- Tamburella, F.; Tagliamonte, N.L.; Masciullo, M.; Pisotta, I.; Arquilla, M.; van Asseldonk, E.H.F.; van der Kooij, H.; Wu, A.R.; Dzeladini, F.; Ijspeert, A.J.; et al. Gait training with Achilles ankle exoskeleton in chronic incomplete spinal cord injury subjects. J. Biol. Regul. Homeost. Agents 2020, 34 (5 Suppl. 3), 147–164, Technology in Medicine. Available online: https://www.ncbi.nlm.nih.gov/pubmed/33386045 (accessed on 11 March 2022). [PubMed]
- Li, M.; Pang, M.; Xiang, K.; Ju, Z.; Zhou, S. Design and Reflex Control for a Series Elastic Actuator Based Ankle Joint Emulator; IEEE: Piscataway, NJ, USA, 2018. [Google Scholar] [CrossRef]
- Kumar, S.; Zwall, M.; Bolivar-Nieto, E.; Gregg, R.D.; Gans, N. Extremum Seeking Control for Stiffness Auto-Tuning of a Quasi-Passive Ankle Exoskeleton. IEEE Robot. Autom. Lett. 2020, 5, 4604–4611. [Google Scholar] [CrossRef]
- Ferris, D.P.; Gordon, K.E.; Sawicki, G.S.; Peethambaran, A. An improved powered ankle-foot orthosis using proportional myoelectric control. Gait Posture 2006, 23, 425–428. [Google Scholar] [CrossRef] [PubMed]
- Gordon, K.E.; Ferris, D.P. Learning to walk with a robotic ankle exoskeleton. J. Biomech. 2007, 40, 2636–2644. [Google Scholar] [CrossRef] [PubMed]
- Sawicki, G.S.; Ferris, D.P. Mechanics and energetics of level walking with powered ankle exoskeletons. J. Exp. Biol. 2008, 211, 1402–1413. [Google Scholar] [CrossRef] [PubMed]
- Sawicki, G.S.; Ferris, D.P. Powered ankle exoskeletons reveal the metabolic cost of plantar flexor mechanical work during walking with longer steps at constant step frequency. J. Exp. Biol. 2009, 212, 21–31. [Google Scholar] [CrossRef] [PubMed]
- Sawicki, G.S.; Ferris, D.P. Mechanics and energetics of incline walking with robotic ankle exoskeletons. J. Exp. Biol. 2009, 212, 32–41. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Malcolm, P.; Segers, V.; Van Caekenberghe, I.; De Clercq, D. Experimental study of the influence of the m. tibialis anterior on the walk-to-run transition by means of a powered ankle-foot exoskeleton. Gait Posture 2009, 29, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Kinnaird, C.R.; Ferris, D.P. Medial gastrocnemius myoelectric control of a robotic ankle exoskeleton. IEEE Trans. Neural Syst. Rehabil. Eng. 2009, 17, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Kao, C.; Ferris, D.P. Motor adaptation during dorsiflexion-assisted walking with a powered orthosis. Gait Posture 2009, 29, 230–236. [Google Scholar] [CrossRef] [PubMed]
- Kao, C.; Lewis, C.L.; Ferris, D.P. Short-term locomotor adaptation to a robotic ankle exoskeleton does not alter soleus Hoffmann reflex amplitude. J. Neuroeng. Rehabil. 2010, 7, 33. [Google Scholar] [CrossRef] [PubMed]
- Kao, C.; Lewis, C.L.; Ferris, D.P. Joint kinetic response during unexpectedly reduced plantar flexor torque provided by a robotic ankle exoskeleton during walking. J. Biomech. 2010, 43, 1401–1407. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kao, C.; Lewis, C.L.; Ferris, D.P. Invariant ankle moment patterns when walking with and without a robotic ankle exoskeleton. J. Biomech. 2010, 43, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, K.Z.; Lewek, M.D.; Sawicki, G.S. A neuromechanics-based powered ankle exoskeleton to assist walking post-stroke: A feasibility study. J. Neuroeng. Rehabil. 2015, 12, 23. [Google Scholar] [CrossRef] [PubMed]
- Jackson, R.W.; Collins, S.H. Heuristic-Based Ankle Exoskeleton Control for Co-Adaptive Assistance of Human Locomotion. IEEE Trans. Neural Syst. Rehabil. Eng. 2019, 27, 2059–2069. [Google Scholar] [CrossRef] [PubMed]
- Koller, J.R.; Jacobs, D.A.; Ferris, D.P.; Remy, C.D. Learning to walk with an adaptive gain proportional myoelectric controller for a robotic ankle exoskeleton. J. Neuroeng. Rehabil. 2015, 12, 97. [Google Scholar] [CrossRef] [PubMed]
- McCain, E.M.; Dick, T.J.M.; Giest, T.N.; Nuckols, R.W.; Lewek, M.D.; Saul, K.R.; Sawicki, G.S. Mechanics and energetics of post-stroke walking aided by a powered ankle exoskeleton with speed-adaptive myoelectric control. J. Neuroeng. Rehabil. 2019, 16, 57. [Google Scholar] [CrossRef]
- Zhang, Z.; Wang, Z.; Jiang, J.-X.; Qian, J.-W. Control method for exoskeleton ankle with surface electromyography signals. J. Shanghai Univ. 2009, 13, 270–273. [Google Scholar] [CrossRef]
- Durandau, G.; Rampeltshammer, W.F.; van der Kooij, H.; Sartori, M. Myoelectric model-based control of a bi-lateral robotic ankle exoskeleton during even ground locomotion. In Proceedings of the 2020 8th IEEE RAS/EMBS International Conference for Biomedical Robotics and Biomechatronics (BioRob), New York, NY, USA, 29 November–1 December 2020; IEEE: Piscataway, NJ, USA, 2020. [Google Scholar]
- Durandau, G.; Rampeltshammer, W.; van der Kooij, H.; Sartori, M.J.A.P.A. Neuromechanical Model-Based Control of Bi-Lateral Ankle Exoskeletons: Biological Joint Torque and Electromyogram Reduction across Walking Conditions. arXiv 2021, arXiv:2108.00980. [Google Scholar]
- Zajac, F.E. Muscle and tendon: Properties, models, scaling, and application to biomechanics and motor control. Crit. Rev. Biomed. Eng. 1989, 17, 359–411. Available online: https://www.ncbi.nlm.nih.gov/pubmed/2676342 (accessed on 11 March 2022). [PubMed]
- Gurney, J.K.; Kersting, U.G.; Rosenbaum, D. Between-day reliability of repeated plantar pressure distribution measurements in a normal population. Gait Posture 2008, 27, 706–709. [Google Scholar] [CrossRef] [PubMed]
- Langlois, K.; Moltedo, M.; Bacek, T.; Rodriguez-Guerrero, C.; Vanderborght, B.; Lefeber, D. Design and Development of Customized Physical Interfaces to Reduce Relative Motion Between the User and a Powered Ankle Foot Exoskeleton; IEEE: Piscataway, NJ, USA, 2018. [Google Scholar] [CrossRef]
- Kamarudin, N.E.M. Soft Actuated Foot Exoskeleton for Ankle Rehabilitation. Int. J. Adv. Trends Comput. Sci. Eng. 2020, 9, 367–373. [Google Scholar] [CrossRef]
- Pérez-Ibarra, J.C.; Williams, H.; Siqueira, A.A.; Krebs, H.I. Real-time identification of impaired gait phases using a single foot-mounted inertial sensor: Review and feasibility study. In Proceedings of the 2018 7th IEEE International Conference on Biomedical Robotics and Biomechatronics (Biorob), Enschede, The Netherlands, 26–29 August 2018; IEEE: Piscataway, NJ, USA, 2018. [Google Scholar]
- Arganaras, J.G.; Wong, Y.T.; Begg, R.; Karmakar, N.C. State-of-the-Art Wearable Sensors and Possibilities for Radar in Fall Prevention. Sensors 2021, 21, 6836. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J. A Review of Wearable IMU (Inertial-Measurement-Unit)-based Pose Estimation and Drift Reduction Technologies. In Journal of Physics: Conference Series; IOP Publishing: Bristol, UK, 2018. [Google Scholar]
- Charry, E.; Lai, D.T.; Begg, R.K.; Palaniswami, M. A study on band-pass filtering for calculating foot displacements from accelerometer and gyroscope sensors. In Proceedings of the 2009 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Minneapolis, MN, USA, 3–6 September 2009; pp. 4826–4827. [Google Scholar] [CrossRef]
- Santhiranayagam, B.K.; Lai, D.T.; Sparrow, W.A.; Begg, R.K. A machine learning approach to estimate minimum toe clearance using inertial measurement units. J. Biomech. 2015, 48, 4309–4316. [Google Scholar] [CrossRef] [PubMed]
- Ferris, D.P.; Sawicki, G.S.; Daley, M.A. A Physiologist’s Perspective on Robotic Exoskeletons for Human Locomotion. Int. J. Humanoid Robot. 2007, 4, 507–528. [Google Scholar] [CrossRef] [PubMed]
- De Luca, C.J. The use of surface electromyography in biomechanics. J. Appl. Biomech. 1997, 13, 135–163. [Google Scholar] [CrossRef]
- Wang, J.; Tang, L.; Bronlund, J.E. Surface EMG signal amplification and filtering. Int. J. Comput. Appl. 2013, 82, 15–22. [Google Scholar] [CrossRef]
- Wu, Y.-D.; Ruan, S.-J.; Lee, Y.-H. An Ultra-Low Power Surface EMG Sensor for Wearable Biometric and Medical Applications. Biosensors 2021, 11, 411. [Google Scholar] [CrossRef] [PubMed]
- Manal, K.; Gravare-Silbernagel, K.; Buchanan, T.S. A Real-Time EMG-Driven Musculoskeletal Model of the Ankle. Multibody Syst. Dyn. 2012, 28, 169–180. [Google Scholar]
- Lloyd, D.G.; Besier, T.F. An EMG-driven musculoskeletal model to estimate muscle forces and knee joint moments in vivo. J. Biomech. 2003, 36, 765–776. [Google Scholar] [CrossRef]
- Kian, A.; Pizzolato, C.; Halaki, M.; Ginn, K.; Lloyd, D.; Reed, D.; Ackland, D. Static optimization underestimates antagonist muscle activity at the glenohumeral joint: A musculoskeletal modeling study. J. Biomech. 2019, 97, 109348. [Google Scholar] [CrossRef] [PubMed]
- Albertus-Kajee, Y.; Tucker, R.; Derman, W.; Lamberts, R.P.; Lambert, M.I. Alternative methods of normalising EMG during running. J. Electromyogr. Kinesiol. 2011, 21, 579–586. [Google Scholar] [CrossRef] [PubMed]
- Zellers, J.A.; Parker, S.; Marmon, A.; Silbernagel, K.G. Muscle activation during maximum voluntary contraction and m-wave related in healthy but not in injured conditions: Implications when normalizing electromyography. Clin. Biomech. 2019, 69, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Sartori, M.; Reggiani, M.; Farina, D.; Lloyd, D.G. EMG-driven forward-dynamic estimation of muscle force and joint moment about multiple degrees of freedom in the human lower extremity. PLoS ONE 2012, 7, e52618. [Google Scholar] [CrossRef] [PubMed]
- Kian, A.; Pizzolato, C.; Halaki, M.; Ginn, K.; Lloyd, D.; Reed, D.; Ackland, D. The effectiveness of EMG-driven neuromusculoskeletal model calibration is task dependent. J. Biomech. 2021, 129, 110698. [Google Scholar] [CrossRef] [PubMed]
- Sloot, L.H.; van der Krogt, M.M. Interpreting Joint Moments and Powers in Gait. In Handbook of Human Motion; Springer International Publishing: Berlin/Heidelberg, Germany, 2016; pp. 1–19. [Google Scholar] [CrossRef]
- Onen, U.; Botsali, F.M.; Kalyoncu, M.; Tinkir, M.; Yilmaz, N.; Sahin, Y. Design and actuator selection of a lower extremity exoskeleton. IEEE/ASME Trans. Mechatron. 2013, 19, 623–632. [Google Scholar] [CrossRef]
- Véronneau, C.; Bigué, J.-P.L.; Lussier-Desbiens, A.; Plante, J.-S.J.I.R.; Letters, A. A high-bandwidth back-drivable hydrostatic power distribution system for exoskeletons based on magnetorheological clutches. IEEE Robot. Autom. Lett. 2018, 3, 2592–2599. [Google Scholar] [CrossRef]
- Gopura, R.; Bandara, D.; Kiguchi, K.; Mann, G.K.J.R.; Systems, A. Developments in hardware systems of active upper-limb exoskeleton robots: A review. Robot. Auton. Syst. 2016, 75, 203–220. [Google Scholar] [CrossRef]
- Thalman, C.M.; Lee, H. Design and Validation of a Soft Robotic Ankle-Foot Orthosis (SR-AFO) Exosuit for Inversion and Eversion Ankle Support; IEEE: Piscataway, NJ, USA, 2020. [Google Scholar] [CrossRef]
- Hunter, I.W.; Hollerbach, J.M.; Ballantyne, J.J.R.R. A comparative analysis of actuator technologies for robotics. Robot. Rev. 1991, 2, 299–342. [Google Scholar]
- Zhu, J.; She, H.; Sun, W.; Li, X.; Zhang, X.; Huang, Q. Design of Compliant Joints and Human-Robot Connection in an Ankle-Foot Exoskeleton; IEEE: Piscataway, NJ, USA, 2017. [Google Scholar] [CrossRef]
- Zhu, J.; Wang, Q.; Huang, Y.; Wang, L. Adding compliant joints and segmented foot to bio-inspired below-knee exoskeleton. In Proceedings of the 2011 IEEE International Conference on Robotics and Automation, Shanghai, China, 9–13 May 2011; IEEE: Piscataway, NJ, USA, 2011. [Google Scholar]
- Rahman, S.M.M.; Ikeura, R. A Novel Variable Impedance Compact Compliant Ankle Robot for Overground Gait Rehabilitation and Assistance. Procedia Eng. 2012, 41, 522–531. [Google Scholar] [CrossRef]
- Oh, S.; Kong, K. High-precision robust force control of a series elastic actuator. IEEE/ASME Trans. Mechatron. 2016, 22, 71–80. [Google Scholar] [CrossRef]
- Allen, D.P. Design Principles for Using Dielectric Elastomer Transducers Applied to Powered Prosthetics and Orthotics; The University of Texas at Dallas: Richardson, TX, USA, 2020. [Google Scholar]
- Lee, C.-H. A survey of PID controller design based on gain and phase margins. Int. J. Comput. Cogn. 2004, 2, 63–100. [Google Scholar]
- Bristow, D.A.; Tharayil, M.; Alleyne, A.G. A survey of iterative learning control. IEEE Control. Syst. 2006, 26, 96–114. [Google Scholar] [CrossRef]
- Young, K.D.; Utkin, V.I.; Ozguner, U. A control engineer’s guide to sliding mode control. IEEE Trans. Control. Syst. Technol. 1999, 7, 328–342. [Google Scholar] [CrossRef]
- Grimmer, M.; Eslamy, M.; Seyfarth, A. Energetic and Peak Power Advantages of Series Elastic Actuators in an Actuated Prosthetic Leg for Walking and Running. Actuators 2014, 3, 1–19. [Google Scholar] [CrossRef]
- Liang, Y.; Zhao, C.Z.; Yuan, H.; Chen, Y.; Zhang, W.; Huang, J.Q.; Yu, D.; Liu, Y.; Titirici, M.M.; Chueh, Y.L.; et al. A review of rechargeable batteries for portable electronic devices. InfoMat 2019, 1, 6–32. [Google Scholar] [CrossRef]
- Sawicki, G.S.; Beck, O.N.; Kang, I.; Young, A.J. The exoskeleton expansion: Improving walking and running economy. J. Neuroeng. Rehabil. 2020, 17, 25. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.Y.; Zheng, Y.P.; Xie, H.B.; Chen, X. Continuous monitoring of electromyography (EMG), mechanomyography (MMG), sonomyography (SMG) and torque output during ramp and step isometric contractions. Med. Eng. Phys. 2010, 32, 1032–1042. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.M.; Housh, T.J.; Hill, E.C.; Keller, J.L.; Johnson, G.O.; Schmidt, R.J. A biosignal analysis for reducing prosthetic control durations: A proposed method using electromyographic and mechanomyographic control theory. J. Musculoskelet. Neuronal Interact. 2019, 19, 142. [Google Scholar] [PubMed]
- Ribeiro, J.; Mota, F.; Cavalcante, T.; Nogueira, I.; Gondim, V.; Albuquerque, V.; Alexandria, A. Analysis of man-machine interfaces in upper-limb prosthesis: A review. Robotics 2019, 8, 16. [Google Scholar] [CrossRef]
- Contreras-Vidal, J.L.; Grossman, R.G. NeuroRex: A Clinical Neural Interface Roadmap for EEG-Based Brain Machine Interfaces to a Lower Body Robotic Exoskeleton; IEEE: Piscataway, NJ, USA, 2013. [Google Scholar] [CrossRef]
- Young, A.J.; Ferris, D.P. State of the Art and Future Directions for Lower Limb Robotic Exoskeletons. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 25, 171–182. [Google Scholar] [CrossRef] [PubMed]
- Zaroug, A.; Garofolini, A.; Lai, D.T.; Mudie, K.; Begg, R. Prediction of gait trajectories based on the Long Short Term Memory neural networks. PLoS ONE 2021, 16, e0255597. [Google Scholar] [CrossRef] [PubMed]
- Khushaba, R.N.; Krasoulis, A.; Al-Jumaily, A.; Nazarpour, K. Spatio-Temporal Inertial Measurements Feature Extraction Improves Hand Movement Pattern Recognition without Electromyography; IEEE: Piscataway, NJ, USA, 2018. [Google Scholar] [CrossRef]
- Al-dabbagh, A.H.A.; Ronsse, R. A review of terrain detection systems for applications in locomotion assistance. Robot. Auton. Syst. 2020, 133, 103628. [Google Scholar] [CrossRef]
- Fan, Z.; Zheng, F.; Ming, L.; He, H. Preliminary Design of a Terrain Recognition System; IEEE: Piscataway, NJ, USA, 2011. [Google Scholar] [CrossRef]
- Liu, M.; Wang, D.; Huang, H.H. Development of an Environment-Aware Locomotion Mode Recognition System for Powered Lower Limb Prostheses. IEEE Trans. Neural Syst. Rehabil. Eng. 2016, 24, 434–443. [Google Scholar] [CrossRef] [PubMed]
- Scandaroli, G.G.; Borges, G.A.; Ishihara, J.Y.; Terra, M.H.; da Rocha, A.F.; Nascimento, F.A.D.O. Estimation of Foot Orientation with Respect to Ground for an above Knee Robotic Prosthesis; IEEE: Piscataway, NJ, USA, 2009. [Google Scholar] [CrossRef]
- Krausz, N.E.; Lenzi, T.; Hargrove, L.J. Depth Sensing for Improved Control of Lower Limb Prostheses. IEEE Trans. Biomed. Eng. 2015, 62, 2576–2587. [Google Scholar] [CrossRef] [PubMed]
- Diaz, J.P.; Da Silva, R.L.; Zhong, B.; Huang, H.H.; Lobaton, E. Visual Terrain Identification and Surface Inclination Estimation for Improving Human Locomotion with a Lower-Limb Prosthetic; IEEE: Piscataway, NJ, USA, 2018. [Google Scholar] [CrossRef]
- Manduchi, R.; Castano, A.; Talukder, A.; Matthies, L. Obstacle detection and terrain classification for autonomous off-road navigation. Auton. Robot. 2005, 18, 81–102. [Google Scholar] [CrossRef]
- Yue, H.; Chen, W.; Wu, X.; Zhang, J. Kinect based real time obstacle detection for legged robots in complex environments. In Proceedings of the 2013 IEEE 8th Conference on Industrial Electronics and Applications (ICIEA), Melbourne, Australia, 19–21 June 2013; IEEE: Piscataway, NJ, USA, 2013. [Google Scholar]
- Costa, P.; Fernandes, H.; Martins, P.; Barroso, J.; Hadjileontiadis, L.J. Obstacle Detection using Stereo Imaging to Assist the Navigation of Visually Impaired People. Procedia Comput. Sci. 2012, 14, 83–93. [Google Scholar] [CrossRef][Green Version]
- Vlaminck, M.; Jovanov, L.; van Hese; Goossens, B.; Philips, W.; Pizurica, A. Obstacle Detection for Pedestrians with a Visual Impairment Based on 3D Imaging; IEEE: Piscataway, NJ, USA, 2013. [Google Scholar] [CrossRef]
- Kuthirummal, S.; Das, A.; Samarasekera, S. A Graph Traversal Based Algorithm for Obstacle Detection Using Lidar or Stereo; IEEE: Piscataway, NJ, USA, 2011. [Google Scholar] [CrossRef]
- Wu, W.; Lei, N.; Tang, J. Smart Shoes for Obstacle Detection. In The 10th International Conference on Computer Engineering and Networks; Springer Singapore: Singapore, 2021; pp. 1319–1326. [Google Scholar] [CrossRef]
- Castano, L.M.; Flatau, A.B. Smart fabric sensors and e-textile technologies: A review. Smart Mater. Struct. 2014, 23, 053001. [Google Scholar] [CrossRef]
- Custodio, V.; Herrera, F.J.; Lopez, G.; Moreno, J.I. A review on architectures and communications technologies for wearable health-monitoring systems. Sensors 2012, 12, 13907–13946. [Google Scholar] [CrossRef] [PubMed]
- Heo, J.S.; Eom, J.; Kim, Y.H.; Park, S.K. Recent Progress of Textile-Based Wearable Electronics: A Comprehensive Review of Materials, Devices, and Applications. Small 2018, 14, 1703034. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Lee, M.; Shim, H.J.; Ghaffari, R.; Cho, H.R.; Son, D.; Jung, Y.H.; Soh, M.; Choi, C.; Jung, S.; et al. Stretchable silicon nanoribbon electronics for skin prosthesis. Nat. Commun. 2014, 5, 5747. [Google Scholar] [CrossRef] [PubMed]
- Peng, B.; Zhao, F.; Ping, J.; Ying, Y. Recent Advances in Nanomaterial-Enabled Wearable Sensors: Material Synthesis, Sensor Design, and Personal Health Monitoring. Small 2020, 16, e2002681. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Nassar, J.; Xu, C.; Min, J.; Yang, Y.; Dai, A.; Doshi, R.; Huang, A.; Song, Y.; Gehlhar, R.; et al. Biofuel-powered soft electronic skin with multiplexed and wireless sensing for human-machine interfaces. Sci. Robot. 2020, 5. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.A.; Walia, S.; Naznee, S.; Taha, M.; Nirantar, S.; Rahman, F.; Bhaskaran, M.; Sriram, S. Artificial Somatosensors: Feedback Receptors for Electronic Skins. Adv. Intell. Syst. 2020, 2, 2000094. [Google Scholar] [CrossRef]
- Hua, Q.; Sun, J.; Liu, H.; Bao, R.; Yu, R.; Zhai, J.; Pan, C.; Wang, Z.L. Skin-inspired highly stretchable and conformable matrix networks for multifunctional sensing. Nat. Commun. 2018, 9, 244. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Liu, Y.; Zhou, Y.; Man, Q.; Hu, C.; Asghar, W.; Li, F.; Yu, Z.; Shang, J.; Liu, G.; et al. A skin-inspired tactile sensor for smart prosthetics. Sci. Robot. 2018, 3, eaat0429. [Google Scholar] [CrossRef] [PubMed]

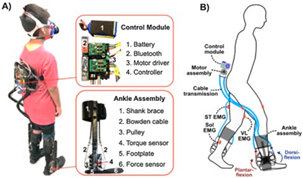 Fang et al., 2020 [37] (copyrights authorized by Elsevier) | Purpose: Assistive Device: Cerebral Palsy, Neuromuscular Impaired, and Parkinson Patients Bilateral: Yes DoF: 1 DoF Plantar Flexion Portability: Portable Weight: 1.85 kg–2.20 kg | High-Level Control Scheme: Phase-based Human-Machine Sensors: FSRs Low-Level Control Scheme: Adaptive PID Machine–Machine Sensors: Torque Sensors Actuation Mechanism: Brushless DC Motors |
 Choi et al., 2020 [38] | Purpose: Assistive Device: Elderly Bilateral: No DoF: 2 DoF Plantar Flexion and Eversion/Inversion Portability: Tethered Weight: 2.14 kg | High-Level Control Scheme: Phase-based Human–Machine Sensors: FSR, Encoder Low-Level Control Scheme: Pulse Width Modulation (PWM) with Solenoid Valves Machine–Machine Sensors: Load Cell Actuation Mechanism: Pneumatic Muscle |
 Bougrinat et al., 2019 [39] (copyrights authorized by Elsevier) | Purpose: General Augmentation Bilateral: No DoF: 1 DoF Plantar Flexion Portability: Portable Weight: 2.045 kg | High-Level Control Scheme: Phase-based Human–Machine Sensors: FSR, Low-Level Control Scheme: PID Machine–Machine Sensors: Load Cell, Current Sensor, Encoder Actuation Mechanism: Brushless DC Motors |
 Guerro-Castellanos et al., 2018 [40] (copyrights authorized by Elsevier) | Purpose: Assistive Device: Drop Foot and Paretic Patients Bilateral: No DoF: 1 DoF Dorsiflexion/Plantar Flexion Portability: Portable Weight: 3.5 | High-Level Control Scheme: Phase-based Human–Machine Sensors: FSR, Encoder, IMU, EMG Low-Level Control Scheme: Adaptive (active disturbance rejection) Actuation Mechanism: Brushless DC Motors |
 Sloot et al., 2018 [41] (copyrights authorized by Elsevier) | Purpose: General Augmentation Bilateral: Yes DoF: 1 DoF Plantar Flexion Portability: Tethered Weight: 3.8 kg | High-Level Control Scheme: Phase-based Human–Machine Sensors: Angle Sensor, IMU Low-Level Control Scheme: Simple position control Machine–Machine Sensors: Load Cell, Actuation Mechanism: Brushless DC Motor |
 Emmens et al., 2018 [42] | Purpose: Assistive Device: Patients with Spinal Cord Injuries Bilateral: Yes DoF: 1 DoF Dorsiflexion/Plantar Flexion Portability: Portable Weight: 6.7 kg | High-Level Control Scheme: Reflex Model-based Human–Machine Sensors: FSR, Encoder, EMG Low-Level Control Scheme: P, PI Machine–Machine Sensors: Encoder Actuation Mechanism: Brushless DC Motor |
 Boes et al., 2018 [43] (copyrights authorized by Elsevier) | Purpose: Assistive Device: Multiple Sclerosis Patients Bilateral: No DoF: 1 DoF Dorsiflexion/Plantar Flexion Portability: Portable Weight: 3.1 kg | High-Level Control Scheme: Phase-based Human–Machine Sensors: FSR, Encoder Low-Level Control Scheme: Proportional Pressure Regulators with Solenoid Valves Machine–Machine Sensors: Pressure Sensors Actuation Mechanism: Pneumatic Cylinders |
| High-Level Control Scheme | Reference |
|---|---|
| Phase-based | [10,37,38,39,40,41,43,49,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158,159,160,161,162,163,164,165,166,167,168,169,170,171,172,173,174,175,176,177,178,179] |
| Impedance-based | [74,75,102,136,161,162,163,164,165,180] |
| Metabolic-rate-based | [70,96,132,181,182] |
| Reflex-model-based | [68,183,184,185,186,187,188] |
| Proportional-myoelectric-based | [11,49,68,89,189,190,191,192,193,194,195,196,197,198,199,200,201] |
| Adaptive gain proportional-myoelectric-based | [133,134,135,202,203,204,205] |
| Myoelectric neuromechanical-model-based | [206,207] |
| Push-button | [49,50] |
| Measured Parameter | Sensor | References |
|---|---|---|
| Gait events | FSR | [37,38,39,40,43,56,57,59,60,61,62,63,64,65,67,76,77,78,79,80,81,82,83,84,85,87,94,107,116,117,118,119,120,141,142,143,145,147,148,149,150,151,152,153,156,159,160,166,167,168,170,171,173,174,175,177,178,184,186,187,189] |
| Footswitch | [10,49,58,69,72,73,88,89,91,92,93,97,98,99,111,113,122,139,154,155,163,164,165,181,198,199,202] | |
| IMU | [57,66,74,75,102,158,170] | |
| Gyroscope | [112] | |
| Piezoresistive sensor | [109,110] | |
| Ankle joint angle | Encoder | [38,40,42,58,62,63,64,68,69,72,73,85,86,100,103,104,106,108,109,110,117,118,138,139,142,149,150,151,159,160,161,162,165,173,178,181,185,186,187,188,202,206,207,210], |
| Potentiometer | [10,43,59,101,102,114,143,147,148,154,155,166,167,170,171] | |
| Gyroscope | [172] | |
| Linear displacement sensor | [97,98,99] | |
| IMU | [64,127,152,211] | |
| Goniometer | [180,183] | |
| Attitude sensor | [116] | |
| Custom strain sensor combined with IMU | [174,175] | |
| Strain sensor | [87] | |
| Knee joint angle | IMU | [206,207] |
| Strain sensor | [87] | |
| Absolute shank angle | IMU | [40,85,87,117,118,159,160,177] |
| Orientation of shank, thigh, and trunk | IMU | [42] |
| Inclinometer | [82] | |
| Angular velocity | Gyroscope | [123,124,125,126,128,129,150,151,157,172] |
| IMU | [114,119,120] | |
| Translational acceleration of wearer | IMU | [40,117,118,119,120,159,160] |
| Foot tilting | Accelerometer | [141] |
| IMU | [119,120] | |
| Walking speed | Speed encoder | [204] |
| Ground reaction force | Force sensor | [10,136] |
| FSR | [101,117,131] | |
| Muscle activity | EMG | [11,40,49,68,89,116,117,133,134,135,181,185,186,190,191,192,193,194,196,197,198,199,200,201,202,203,204,205,206,207] |
| Anatomical ankle generated torque | Strain gauges | [101,102] |
| Exoskeleton frame–user interaction forces | Force sensor | [136] |
| Respirometry | Metabolic mask | [70,96,132] |
| Sensor | Specific Sensor Details | Measurement | Location | Reference |
|---|---|---|---|---|
| IMU | IMU (gyroscope and accelerometer) | Ankle joint angle | Foot and calf | [56] |
| WT901C485, WitMotion, Shenzhen, China | Gait cycle | Shoe | [57] | |
| EBIMU-9DoFV5, E2BOX Inc., Shanghai, China | Ankle joint angle | Shin and thigh parts of the exoskeleton | [64] | |
| 6-DoF IMU, 100Hz | Gait phase | Shank | [66] | |
| BNO055 (Bosch, Germany) | Gait phase | Foot | [74,75] | |
| 3DM-GX4-25-RS232-SK1, LORD MicroStrain, Inc., Williston, VT, USA | Absolute shank angle | Main structure | [85] | |
| MW-AHRS, NTRexLAB | Absolute shank angle | Shank | [87] | |
| EBIMU-9DoFV4, E2BOX | Shank angle in sagittal plane | Medial shank | [177] | |
| 3 × Xsens (Xsens Technologies B.V., Enschede, The Netherlands) | Orientation of the shank, thigh, and trunk | Shank, thigh, and trunk | [42] | |
| MPU6050 | Ankle joint angle | Foot | [211] | |
| Not specified | Gait phase segmentation | Foot | [102] | |
| IMU (Shimmer Inc., Dublin, Ireland ) | Angular velocity | Shank | [114] | |
| SN-IMU5D-LC, Cytron, Simpang Ampat, Malaysia | Shank’s angular velocity in the sagittal plane and accelerations along the y and z axes. | Mechanical structure, near shank | [158] | |
| 2 × Xsens (Xsens Technologies B.V., Enschede, The Netherlands) | #1: Angle between the shank and the vertical axis #2: Translational acceleration of the wearer along the three axes. | #1 Shank #2 Foot | [40,117,118,159,160] | |
| Mpu6050 6-axis MotionTrackingTM device, InvenSense, San Jose, CA, USA | Leg linear acceleration | Leg brace | [119,120] | |
| MTi-3, (Xsens Technologies B.V., Enschede, The Netherlands) | Foot angle and angular velocity | Lateral side of the shoe | [127] | |
| Link, Xsens, The Netherlands | Knee joint angle | Not specified | [206,207] | |
| XSens MTi-28A53G35, (XSens Technologies. Enschede, The Netherlands) | Orientation and position of the exoskeleton | Medial side of the exoskeleton | [170] | |
| SEN-09623, 9DoF Razor IMU, Sparkfun Electronics, Boulder, CO 80301, USA. | Orientation of lower leg and foot | Foot and lower leg | [174,175] | |
| IMU (Sparkfun Electronics, Boulder, CO 80301, USA, with a gyroscope ADXRS610 and two accelerometers ADXL320, from Analog Devices) | Absolute position of the exoskeleton | Not specified | [152] | |
| Gyroscope | Gyroscope | Shank angular velocity to identify heel contact | Not specified | [157] |
| Single axis Gyroscope | Gait phase | On the shin | [112] | |
| 2 × Single axis Gyroscope (LY3100ALH, STMicroelectronics, Geneva, Switzerland) | Sagittal angular velocity of the shank and foot | One at the top of the mid-foot and the other at the anterior side of the shank | [123,125,129] | |
| LY3100ALH, STMicroelectronics-single axis | Angular motion of the foot for gait segmentation | Top of the mid-foot | [124] | |
| Sparkfun, NIWOT, CO, USA | Angular motion of the foot for gait segmentation | Integrated in the shoe | [126,128] | |
| 2 × Gyroscopes | Sagittal angular motion and velocity of the foot for gait segmentation | Not specified | [172] | |
| Rate gyro | Angular velocity of shank | Not specified | [150,151] | |
| Accelerometer | Tilt sensor | Tilt of foot | Not specified | [141] |
| Attitude sensor | 2 × JY901 attitude sensors | Ankle joint angle | Parallel to the lever and shank | [116] |
| angular | Ankle joint angle and angular velocity | Ankle joint | [113] | |
| Foot pressure sensors | 3 × Membrane pressure sensors | Plantar pressure distribution for gait cycle detection | Integrated insole | [56] |
| Insole-shaped foot pressure sensors (RX-ES39, Roxi Technology, Jiangsu, China) | Identify the gait state using pressure of three parts, i.e., forefoot, toe, and heel | Shoes | [57] | |
| 4 × FSR (MA-152, Motion Lab System Inc., Baton Rouge, LA, USA) | Ground contact, gait phase | Heel, hallux, first metatarsal head, and fifth metatarsal base | [59,60,61] | |
| FSR sensor | Gait phase | Heel and big toe | [38,62,63] | |
| 3 × FSR sensors | Gait phase | Toe, heel, and medial of the insole | [64] | |
| 2 × FSR (FlexiForce A401, Tekscan, Boston, MA, USA) | Gait phase | Heel and the metatarsal bone | [65,184] | |
| FSR sensor | Gait cycle | Under the arch support of the shoe | [67] | |
| 2 × FSR sensor | Gait phase | Under the ball and heel of the foot | [76,77,78,79,81,82,84] | |
| 2 × FSR (FlexiForce A201, Tekscan, Inc., Boston, MA, USA) | Ground reaction force | Under forefoot | [37,80,83] | |
| 2 × FSR (FlexiForce A301, Tekscan, Inc., South Boston, MA, USA) | Gait phase | Embedded into the insole | [85,189] | |
| Toe contact sensor like pressure switch or force-sensing resistor | Gait timing | Not specified | [94] | |
| 3 × FSR (FlexiForce, Tekscan, Boston, MA, USA) | Ground contact of each foot | Insole | [87] | |
| Custom-designed FSR sole | Gait phase | Beneath the foot brace | [177] | |
| FSR (Interlink 406, Adafruit, New York, NY, USA) | Gait phase | The user’s shoe at the anterior and posterior ends of the shoe insoles | [156] | |
| FSR-151AS pressure sensor (IEE, Contern, Luxembourg) | Heel strike | Heel | [178,186,187] | |
| 2 × FSR sensors | Ground reaction force | Heel and toe | [101] | |
| FSR (SEN-09376 Antratek used with Phidgets Voltage Divider 1121) | Initiation of new step | Heel | [107] | |
| IMS009-C7.5 (FSR) | Heel strike | Heel | [116] | |
| 3 × FSR in a force sensitive resistor matrix (FSRM)—(Tekscan, Inc., Boston, MA, USA) | Distribution of ground reaction force | Heel, hallux, fifth metatarsal phalange joints | [40,117,118,159,160] | |
| FSR | Heel strike | Not specified | [39] | |
| 2 × FSR-402 (Interlink Electronics Inc., Camarillo, CA, USA) | Foot loading pattern as an on/off switch. | Forefoot and heel | [119,120] | |
| 4 × FSR-402 (Interlink Electronics Inc., Camarillo, CA, USA) | Ground reaction force | Below the shoe insoles at the heels and toes | [131] | |
| 2 × FSR-402, 0.5 in circle; (Interlink Electronics Inc., Camarillo, CA, USA) | Gait phase | Heel and metatarsal heads | [43,166,167,168,170,171] | |
| 2 × FSR | Gait phase | Toe and heel | [141] | |
| 4 × FSR (FlexiForce-A201-25lb, Tekscan Inc., Boston, MA 02127, USA) | Gait phase | Embedded in a shoe insole | [174,175] | |
| Sparkfun SEN-09375) | Gait phase | Heel of the plate | [142] | |
| FSR | Heel and toe contact | In the shoes | [143] | |
| 3 × FSR (FlexiForce-A201-25lb, Tekscan Inc., Boston, MA 02127, USA) | Ground reaction force | Heel, lower forefoot, and big toe | [145] | |
| FSR | Heel strike | Heel | [146,147,148,149,150,151] | |
| 3 × FSR | Gait phase | Under heel, middle, and front part of the shoe | [152] | |
| 4 × FSR | Gait phase | Flexible insole | [153] | |
| Force sensor | Ultraflex system—with 6 capacitive force transducers 25 mm square and 3 mm thick | Ground reaction force | Bottom of the exoskeleton, two sensors beneath the heel and four beneath the forefoot region. | [10] |
| 2 × Force sensors | Interaction forces—the ground reaction forces during the contact of robotic device with the ground and other force sensors measure the interaction forces between the shank of the user and the robotic device. | Not specified | [136] | |
| GRF sensing system consisting of two force sensors | Gait phase | Integrated into shoe | [173] | |
| Footswitch | McMaster-Carr, Aurora, OH, USA | Heel strike | In the heel of the shoe | [58,69,72,73,181,202] |
| Footswitch | Foot contact | Not specified | [49] | |
| Footswitch | Foot contact | Under left forefoot inside the shoe | [88] | |
| Footswitch (B&L Engineering, Santa Ana, CA, USA) | Foot contact | Inside shoe | [89,199] | |
| IP67, Herga Electric, Suffolk, UK | Foot contact | Heel | [91,92] | |
| Multimec 5E/5G, Mec, Ballerup, Denmark | Foot contact | In the heel of the shoe | [93,97,98,99] | |
| Footswitch, model MA-153 | Heel strike | In the heel of a shoe worn with the orthosis | [10] | |
| FSW (B&L Engineering, Santa Ana, CA, USA) | Heel and toe contact | Not specified | [111,113] | |
| B&L Engineering, Santa Ana, CA, USA | Heel strike | Under foot | [122] | |
| Footswitch (B&L Engineering, Santa Ana, CA, USA) with 4 individual footswitches | Gait phase | Inside shoe—at the heel, forefoot, medial, and lateral zones at the level of metatarsals. | [163,164,165] | |
| Pressure sensor (footswitch) | Heel strike moment and stride length | Under the shoe | [139] | |
| 2 × Tactile Arrays | Position of orthosis | Incorporated in the foot part of the exoskeleton and in the insole of the healthy leg | [154,155] | |
| Potentiometer | Rotary potentiometer | Ankle joint angle | Attached to the hinged ankle joint of the exoskeleton | [59,60,61] |
| Precision potentiometer (resolution of 0.5°) | Ankle joint angle | Exoskeleton ankle joint | [101,102] | |
| Bourns 6637S-1-502 5-k rotary potentiometer | Ankle joint angle | Not specified | [10] | |
| Motorized linear potentiometer | Ankle joint angle | Integrated in wearable ankle robot | [114] | |
| Rotary potentiometer 53 Series, Honeywell, Golden Valley, CA, USA). | Ankle joint angle | Exoskeleton ankle joint | [43,166,167,170,171] | |
| Linear potentiometer | Ankle joint angle | Exoskeleton ankle joint | [143,148] | |
| linear and an angular potentiometer | Ankle motion | Not specified | [147] | |
| Rotary potentiometer | Ankle joint angle | Exoskeleton ankle joint | [154,155] | |
| Encoder | Optical encoder (E8P; US Digital, Vancouver, WA, USA) | Ankle joint angle | Exoskeleton ankle joint | [58] |
| 2 × Absolute encoders (AMT203-V, CUI Inc., Tualatin, OR, USA) | Ankle joint angle | Exoskeleton joints corresponding to the talocrural and subtalar joints | [38,62,63,64] | |
| Digital optical encoder | Ankle joint angle | Exoskeleton ankle joint | [68] | |
| E4P and E5(US Digital Corp., Vancouver, WA, USA), for alpha and beta exoskeleton | Ankle joint angle | Exoskeleton ankle joint | [69] | |
| Absolute magnetic encoder (MAE3, US Digital, Vancouver, WA, USA) | Ankle joint angle | Lateral side of each exoskeleton’s ankle joint | [73,202] | |
| Digital optical encoders (E5, US Digital, Vancouver, WA, USA) | Ankle joint angle | Exoskeleton joint shaft | [72,181] | |
| Angular sensor, PandAuto P3022, Mexico, Mexico | Absolute angle of Link 1 in exoskeleton | Exoskeleton | [86] | |
| Optical incremental encoder (2048 CPR, E6-2048-250-IE-S-H-D-3, US Digital, Inc.) | Ankle joint angle | Exoskeleton ankle joint | [85] | |
| RMB20IC13BC SSI-encoder (RLS-Renishaw, Ljubljana, Slovenia) | Ankle joint angle | Exoskeleton ankle joint | [42,100,178,185,186,187] | |
| Incremental optical encoder (US Digital HUBDISK-2-2000-625-IE, module EM1-2-2000-I, DI/O type, 5 pins, 5V) | Ankle joint angle | Exoskeleton ankle joint | [103,104,106,210] | |
| Joint encoder (2000 CPT, HEDS-5600, Broadcom, San Jose, CA, USA), quadrature encoder-70 | Ankle joint angle | Lateral 3D-printed mount on exoskeleton ankle joint | [108,109,110] | |
| Encoder E2 | Ankle joint angle | Exoskeleton ankle joint | [188] | |
| Incremental encoder | Ankle joint angle | Exoskeleton ankle joint | [40,117,118,159,160] | |
| linear incremental encoders (Renishaw, Chicago, IL, USA) | Ankle joint angle | Traction drive | [161,162,165] | |
| Optical 3 phase 4000 CPR | Ankle joint angle | Exoskeleton ankle joint | [131] | |
| Absolute rotary encoder 20 b Aksim, RLS (Renishaw), Kemnda, Slovenia). | Ankle joint angle | Exoskeleton ankle joint | [206,207] | |
| Optical encoder (US Digital Inc.) | Ankle joint angle | Exoskeleton ankle joint | [138,139] | |
| Magnetic encoder (AN25-analog, KD Mechatech Co., Korea) | Ankle joint angle | Exoskeleton ankle joint | [173] | |
| Rotary encoder | Foot rotation | Base of shank | [142] | |
| Absolute angular encoder | Ankle joint angle | Exoskeleton ankle joint | [149,150,151] | |
| Goniometer | Goniometer (5 kHz, 250 Hz Biometrics, Newport, UK) | Ankle joint angle | Exoskeleton ankle joint | [180] |
| Goniometers (500 Hz, Biometrics, Newport, UK) | Ankle joint angle | Exoskeleton ankle joint | [183] | |
| Linear displacement sensor | 100 Hz; SLS130, Penny & Giles, Christchurch, Newport, UK | Ankle joint angle | Foot and shank sections of the exoskeletons | [97,98,99] |
| Strain sensor | Soft strain sensor | Ankle and knee joint angle | Knee and the ankle joints | [87] |
| 4 × strain gauges connected to a full Wheatstone bridge | Human–exoskeleton interaction torque | On the exoskeleton frame, near the ankle joint | [101,102] | |
| 4 × custom-built strain sensors | Ankle joint angle | Dorsal and medial side of the ankle | [174,175] | |
| Piezoresistive sensor | 3 × Piezoresistive sensors | Gait phase | Foot section of the exoskeleton, underneath the calcaneus, the first metatarsal head, and the hallux. | [109] |
| Piezoresistive sensor | Heel strike | Underneath the calcaneus | [110] | |
| EMG | Surface electrodes, high-pass filtered at 20 Hz, rectified, low-pass filtered at 6 Hz | Muscle activity | Gastrocnemius muscle | [68] |
| 2 × Wired, bipolar electrodes (Bagnoli Desktop System, Delsys Inc., Boston, MA, USA) | Muscle activity | Medial and lateral aspects of the soleus | [202] | |
| Wireless EMG system (Bagnoli, Delsys, MA, USA) | Muscle activity of four lower-leg muscles on the exoskeleton side | Medial gastrocnemius, lateral gastrocnemius, soleus, and tibialis anterior | [181] | |
| 1200 Hz, TeleMyo, Noraxon USA, Scottsdale, AZ, USA | Muscle activity | Soleus and tibialis anterior | [11] | |
| 1200 Hz, Konigsberg Instruments, Inc., Pasadena, CA, USA | Muscle activity | Soleus, medial gastrocnemius, tibialis anterior | [49,89,190,191,192,193,194,196,197,198,199,200,203] | |
| Surface EMG (960 Hz SX230, Biometrics, Newport, UK). | Muscle activity of the paretic side | Soleus | [201,204] | |
| Surface EMG | Muscle activity | Tibialis anterior and soleus muscles | [185,186] | |
| Not specified | Muscle activity | Tibialis anterior, gastrocnemius, soleus, and the rectus femoris | [116] | |
| 2 × Electromyography sensors (Delsys) | Muscle activity | Tibialis anterior and gastrocnemius | [117] | |
| EMG surface electrodes-1000 Hz; SX230, Biometrics | Muscle activity | Soleus | [133,134,135] | |
| AxonMaster 13E500, Ottobock, Germany | Muscle activity | Lower limb | [206,207] | |
| Surface EMG | Muscle activity | Tibialis anterior, lateral gastrocnemius, medial gastrocnemius, peroneus longus, and soleus | [205] |
| Low-Level Control Scheme | References | |
|---|---|---|
| Classical PID | PID [39,53,54,55,56,67,68,76,77,78,79,82,86,101,102,108,109,110,114,119,120,121,136,138,139,140,154,155] | |
| P [100,106,107,113,146,172,178,185,186,187,204] | ||
| PI [85,100,105,178,185,186,187] | ||
| PD [10,57,65,66,69,70,71,72,73,81,137,147,148,149,150,151,152,153,161,162,163,164,165,180,181,202,206,207] | ||
| Adaptive PID [37,64,80,83,84] | ||
| Iterative Learning | [58,68,69,70,71,72,73,131,181,182,202] | |
| Adaptive | [40,68,159,160,189] | |
| Sliding Mode | [53] | |
| Open-Loop Feed-Forward | [94,158,184,206,207] | |
| Pneumatic Actuation Controls | On-Off Solenoid Valves | [146,156,166,167,170,171,173,174,175] |
| Pulse Width Modulation (PWM) with Solenoid Valves | [38,62,63,141,173,188] | |
| Proportional Pressure Regulators with Solenoid Valves | [11,43,49,50,88,89,90,91,92,93,95,96,97,98,99,132,133,134,135,142,168,169,190,191,192,193,194,195,196,197,198,199,200,201,203] | |
| Measured Parameter | Sensor |
|---|---|
| Cable/rope tension | Tension sensor [53,182] force sensor [57] load cell [39,58,69,108,109,110,122,123,124,125,126,127,128,129,180,183,204] strain gauge [72,113,181] |
| Mechanical deflection | Potentiometer [10,55,67,108,110,137,146,153,176] encoder [206,207,236] |
| Pressure | Pressure sensor [62,63,146,156,158,166,171,173,176,232] |
| Pneumatic muscle force | Load cell [11,38,49,50,62,63,88,89,91,96,97,98,99,131,134,190,191,192,193,194,196,197,198,199,200,203] |
| Real torque measured from actuator | Torque sensor [85] |
| Reaction torque measured at the ankle | Torque sensor [37,76,77,78,79,80,81,82,83,84,104,105,106] linear potentiometer [234] strain gauges [68,69,73,202] |
| Forces delivered by exoskeleton | Load cell [138,139] |
| Motor current | Current sensor [39,85,161,162] |
| Motor position/velocity | Encoder [39,55,57,59,67,68,72,108,110,111,112,113,115,116,121,141,143,147,148,149,150,151,161,162,165,172,180,181,188,206,207,235] Hall sensor and resolver [85] |
| Cable position | Potentiometer [126] |
| Motor stroke | Encoder [42,100,178,185,186,187] |
| Slave cylinder stroke | Optical distance sensor [158] |
| Actuator lever/link angles | Encoder [103,104,106,210] |
| Sensor | Specific Sensor Details | Measurement | Location | Reference |
|---|---|---|---|---|
| Load cell | LC201 Series; OMEGA Engineering, Stamford, CT, USA | Cable tension | At the ankle | [58] |
| Inline tensile load cell: DCE-2500N, LCM Systems, Newport, UK,250Hz LP Filter | Actuation force | Attached to the end effector moment arm (~ 10 cm) through a series elastic element | [180] | |
| Load cells (500 Hz, LCM Systems Ltd., Newport, UK) | Cable tension | In series with the force transmission cables and series elastic element | [183] | |
| Tension load cell (CDFS-200, BONGSHIN LOADCELL, Osan, Korea)—one with each pneumatic artificial muscle | Pneumatic muscle force | Attached at the end of the pneumatic muscle | [38,62,63] | |
| LC201, OMEGA Engineering Inc., Stamford, CT, USA) | Bowden cable tension | Alpha exoskeleton, Bowden cable | [69] | |
| Tension load cell-(LC8150-375-1K 0–100 lbs, 1200Hz, OMEGA Engineering, Stamford, CT, USA) | Pneumatic muscle force | Between the pneumatic muscle and the rod end | [11,49,50,88,89,96,190,191,192,193,194,196,197,198,199,200,203] | |
| Load cell (W2, A.L. Design, Buffalo, NY, USA) | Tensile force of pneumatic muscle | Not specified | [91] | |
| 100 Hz; 210 Series, Richmond Industries Ltd., Reading, UK | Pneumatic muscle force | Connected between the orthoses and the pneumatic muscles | [97,98,99] | |
| Two in-line load cells (LSB200, FUTEK Advanced Sensor Technology, Irving, CA, USA) | Actuation force | Posterior side of the calf, near the proximal part of the orthosis. | [108,109,110] | |
| Inline tensile load cell (DCE-2500N, LCM Systems, Newport, UK) | Actuation force | Bowden cable | [204] | |
| LFT-13B, Shenzhen Ligent Sensor Tech Co., Ltd., Shenzhen, China (inline load cell) | Force applied on the struts | Not specified | [39] | |
| 2 × Load cell—one cantilevered load cell (Phidgets 3135 50 kg Micro Load Cell), second load cell (LCM300, FUTEK Advanced Sensor Technology, Irving, CA, USA) | Cable force at the top of the Bowden cable and forces delivered to the wearer | First one in pulley module, second one at the ankle in series with the cable | [122] | |
| LTH300, FUTEK Advanced Sensor Technology, Irving, CA, USA | Bowden cable force | In series with the Bowden cable and the calf wrap | [123,124,125,129] | |
| LSB200, FUTEK Advanced Sensor Technology Irving, CA, USA | Assistive force transmitted to the hip joint via straps | Left side of exosuit in series with the two vertical straps and the waist belt | [124,129] | |
| 2 × LSB200, FUTEK Advanced Sensor Technology, Irving, CA, USA | Delivered force at the ankle—DF and PF forces generated by Bowden cable retractions | Integrated into the exosuit’s textile loops of the calf wrap | [126,127,128] | |
| Not specified | Pneumatic muscle force | Between the NcPAM and the bottom plate | [131] | |
| OMEGA Engineering, Stamford, Connecticut | Actuation kinetics | In series with actuator | [134] | |
| Load cell (range +/− 220 N; Transducer Techniques Inc.) | Forces transmitted to wearer | At the extremity of the slave cylinder | [138,139] | |
| Strain gauge | Not specified | Plantar flexion torque | On heel lever | [68,73] |
| 4 ×strain gauges (MMF003129, Micro Measurements, Wendell, NC, USA) in a Wheatstone-bridge | Torque | On ankle lever | [69,202] | |
| Wheatstone bridge consisting of four strain gauges (KFH-6-350-C1-11L1M2R, OMEGA Engineering, Norwalk, CT, USA) | Assistive torque | End of titanium ankle lever | [72,181] | |
| LCM200, FUTEK Advanced Sensor Technology, Inc., Irvine, CA, USA | Cable tension | On transmission cable | [113] | |
| Encoder | Incremental encoder | Motor position and velocity | Motor | [55] |
| AMT103-V, CUI Inc., OR, USA (2048 counts per revolution). | Motor position and velocity | Motor | [57] | |
| Optical encoder (E5 Optical Encoder, US Digital, Vancouver, WA, USA) | Motor pulley velocity | Motor | [180] | |
| Not specified | Motor position and velocity | Motor | [59,60,61] | |
| Incremental encoder with 1024 count per turn | Motor position | Motor | [67] | |
| Digital optical encoders | Motor position | Motor | [68] | |
| Digital optical encoders (E5, US Digital, Vancouver, WA, USA) | Motor position | Motor shaft | [72,181] | |
| Incremental encoder (SCH24-200-D-03-64-3-B, Scancon, Allerød, Danmark) | Motor stroke | Motor axis | [42,100,178,185,186,187] | |
| Absolute magnetic encoder (AS5048A, SPI type, 6pins, 5V, a4-bit) | Torque angle/lever arm angle | In actuator | [103,104,106,210] | |
| Motor-shaft encoder | Motor position and velocity | Motor | [108,110] | |
| Encoder E1 | Motor position | Motor | [188] | |
| 500-Count quadrature incremental optical encoders (model: HEDL 5540, Maxon Motors, Sachseln, CH). | Motor position | Motor | [111,112] | |
| 14-Bit magnetic on-axis relative encoder (AS5047P and AS5047D, AMS AG, Premstaetten, AT) | Motor position | Motor | [113] | |
| Encoder (ENX16 EASY 500IMP) | Motor position | In actuator module | [115,116] | |
| Motor Encoder | Motor position and velocity | Motor | [39,143,147,148] | |
| Quadrature encoders (2×195 RPM and 2×60 RPM HD premium planetary gearheads) | Motor position and velocity | Motor | [121] | |
| Rotary encoder—Gurley R119 rotary encoders (Gurley, Troy, NY) | Commutate the motor | Mounted coaxially with the motors | [161,162,165] | |
| Encoder FPC optical 3 phase 4000 CPR | Not specified | Inside the thrust bearing | [131] | |
| Absolute angle Hall encoder (MHM, IC Haus, Germany) | Motor position | Motor | [206,207] | |
| Angle encoder | Motor position and velocity | Motor | [235] | |
| Absolute rotary encoder 20 b AksIM, RLS (Renishaw), Kemnda, Slovenia). | Spring deflection | Not specified | [206,207] | |
| Encoder (5540 HEDL) | Motor position | Motor | [172] | |
| 2 × Rotary encoder and linear encoder | Spring deflection | In actuator | [236] | |
| Encoder with servo motor | Actual position sensing of actuator | Motor | [141] | |
| Digital incremental motor encoder | Determine position of lead screw | Not Specified | [149,150,151] | |
| Hall sensors and resolver | Not specified | Motor position | Motor | [85] |
| Potentiometer | Linear potentiometer | Spring deflection | Motor housing | [55] |
| Linear potentiometer (50 mm travel length) | Spring deflection | Assembled to stainless steel pipe with a 3D-printed plastic housing. | [67] | |
| Linear potentiometer | Spring deflection | Top of spring module | [10,108,110] | |
| Linear potentiometer (P3 America Inc., San Diego, CA, USA) | Cable position | With actuator | [126] | |
| Linear potentiometer | Joint torque | Mounted in parallel with series spring | [234] | |
| Softpot linear position sensor | Transpose of spring | Not specified | [137] | |
| Linear potentiometer | Deflection of links | Upper part of actuator link | [146,176] | |
| Linear sliding potentiometer | Spring deflection | Fixed in the two-support platforms of the springs. | [153] | |
| Tension sensor | Not specified | Cable tension | Bowden cable | [53] |
| Not specified | Cable tension | At the end of Bowden cable | [182] | |
| Pressure sensor | TST-20.0, TIVAL Sensors GmbH, Wuppertal, Germany | Pressure of pneumatic muscle | Pneumatic muscle | [62,63] |
| ASDXAVX 100PGAA5, Honeywell Sensing and Productivity Solutions, Charlotte, NC, USA | Actuator pressure | Actuator | [156,232] | |
| Pressure sensors (PX3AN1BH667PSAAX, Honeywell) | Measure the pressure in each hydraulic transmission | Not specified | [158] | |
| Tethered pressure transducer: 4100 series, American Sensor Technology; Mt. Olive, NJ, USA) | Assistive torque-pressure in actuator | In actuator chamber | [166] | |
| Pressure transducers (AST4000A00150P3B1000, 150 psig and AST4000A00100P3B0000, 100 psig, American Sensor Technologies, Inc, Mount Olive, NJ, USA) | Compressed CO2 pressure on both sides of the actuator | Actuator | [171] | |
| 5V G1/4 0–1.2 MPa, China | Senses the pressure in the cylinder chamber system | With the control hardware, attached to the waist of user | [173] | |
| Not specified | Not specified | Upper end of actuator | [146,176] | |
| Torque sensor | TRT-500, Transducer Techniques, Temecula, CA, USA | Reaction torque provided by the motors through the ankle pulley | Placed in line with each exoskeleton ankle joint/mounted on the insole | [37,76,77,78,79,80,81,82,83,84] |
| Torque sensor (TPM 004+, Wittenstein, Inc., Igersheim, Germany) | Actuator torque output | Installed between the actuator case and the main structure | [85] | |
| DRBK, ETH Messtechnik, 200 Nm, 0.0122 Nm resolution | Actuator torque output | Attached to test setup | [104,105,106] | |
| Current sensor | Not specified | Active current | Motor | [85] |
| Not specified | Motor current | Motor | [39] | |
| Analog current sensor (Interactive Motion Technologies board employing TI/Burr-Brown 1NA117P) | Motor current to estimate motor torque | Motor | [161,162] | |
| Distance sensor | Optical sensor (GP2Y0A51SK0F, Sharp) | Slave cylinder stroke | Not specified | [158] |
| Force sensor | ZZ210-013, Zhizhan Measurement and Control, Shanghai, China | Cable force | Heel cable and forefoot cable | [57] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kian, A.; Widanapathirana, G.; Joseph, A.M.; Lai, D.T.H.; Begg, R. Application of Wearable Sensors in Actuation and Control of Powered Ankle Exoskeletons: A Comprehensive Review. Sensors 2022, 22, 2244. https://doi.org/10.3390/s22062244
Kian A, Widanapathirana G, Joseph AM, Lai DTH, Begg R. Application of Wearable Sensors in Actuation and Control of Powered Ankle Exoskeletons: A Comprehensive Review. Sensors. 2022; 22(6):2244. https://doi.org/10.3390/s22062244
Chicago/Turabian StyleKian, Azadeh, Giwantha Widanapathirana, Anna M. Joseph, Daniel T. H. Lai, and Rezaul Begg. 2022. "Application of Wearable Sensors in Actuation and Control of Powered Ankle Exoskeletons: A Comprehensive Review" Sensors 22, no. 6: 2244. https://doi.org/10.3390/s22062244
APA StyleKian, A., Widanapathirana, G., Joseph, A. M., Lai, D. T. H., & Begg, R. (2022). Application of Wearable Sensors in Actuation and Control of Powered Ankle Exoskeletons: A Comprehensive Review. Sensors, 22(6), 2244. https://doi.org/10.3390/s22062244








