A Compact Modified Two-Arm Rectangular Spiral Implantable Antenna Design for ISM Band Biosensing Applications
Abstract
:1. Introduction
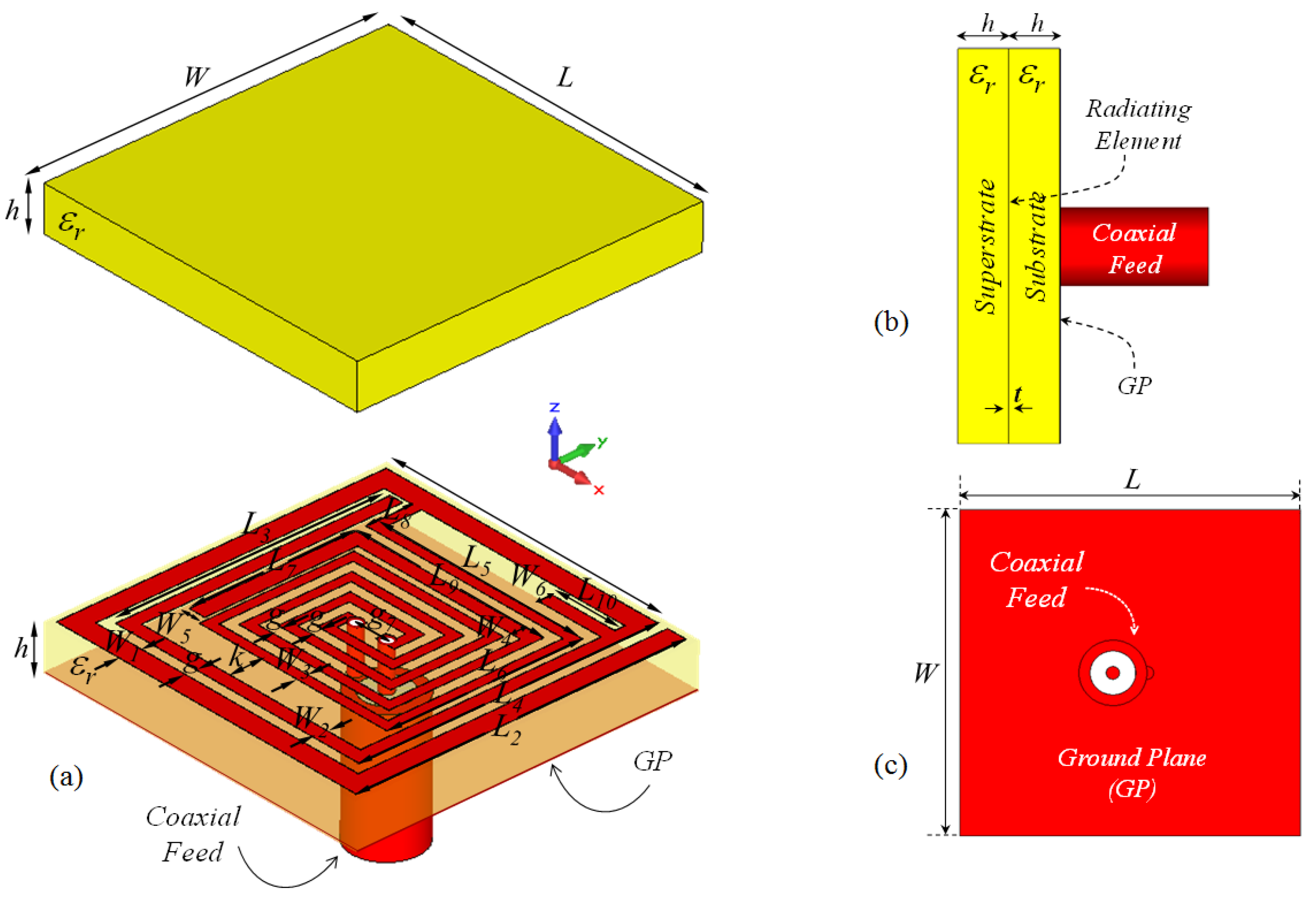
2. Antenna Design
3. Effects of Critical Design Parameters on the Antenna Performance
3.1. Effect of Length L3 on the Input Reflection Coefficient (S11)
3.2. Effect of Length L2 on the Input Reflection Coefficient (S11)
3.3. Effect of Length L10 on the Input Reflection Coefficient (S11)
3.4. Effect of Superstrate Thickness h on Input Reflection Coefficient (S11)
4. Results and Discussions
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| MIA | Microstrip Implantable Antenna |
| TARS | Two-Arm Rectangular spiral |
| ISM | Industrial, Scientific, and Medical |
| MICS | Medical Implant Communication Services |
| RF | Radio Frequency |
| RFID | Radio Frequency Identification |
| FCC | Federal Communications Commission |
| FIT | Finite Integration Technique |
| IC | Integrated Circuit |
| DGBE | Diethylene Glycol Butyl Ether |
| CAD | Computer-Aided Design |
| CAE | Computer-Aided Engineering |
| SAR | Specific Absorption Rate |
| SMA | SubMiniature Version A |
| Triton X-100 | Polyethylene Glycol Monophenyl Ether |
References
- Auciello, O. Biomaterials and Multifunctional Biocompatible Ultrananocrystalline Diamond (UNCD™) Technologies Transfer Pathway: From the Laboratory to the Market for Medical Devices and Prostheses. In Ultrananocrystalline Diamond Coatings for Next-Generation High-Tech and Medical Devices; Auciello, O., Ed.; Cambridge University Press: Cambridge, UK, 2022; pp. 263–276. [Google Scholar] [CrossRef]
- Hall, P.S.; Hao, Y. Antennas and Propagation for Body-Centric Wireless Communications; Artech House: Norwood, MA, USA, 2012. [Google Scholar]
- Elmqvist, R.; Senning, A. An implantable pacemaker for the heart. In Proceedings of the Second International Conference on Medical Electronics, Paris, France, 24–27 June 1959; Volume 24, p. 27. [Google Scholar]
- Kim, J.; Rahmat-Samii, Y. Implanted antennas inside a human body: Simulations, designs, and characterizations. IEEE Trans. Microw. Theory Tech. 2004, 52, 1934–1943. [Google Scholar] [CrossRef]
- Izdebski, P.M.; Rajagopalan, H.; Rahmat-Samii, Y. Conformal ingestible capsule antenna: A novel chandelier meandered design. IEEE Trans. Antennas Propag. 2009, 57, 900–909. [Google Scholar] [CrossRef]
- Lee, J.H. Human implantable arrhythmia monitoring sensor with wireless power and data transmission technique. Austin J. Biosens. Bioelectron. 2015, 1, 1008. [Google Scholar]
- Kwak, S.; Chang, K.; Yoon, Y.J. Small spiral antenna for wideband capsule endoscope system. Electron. Lett. 2006, 42, 1328–1329. [Google Scholar] [CrossRef]
- Rodrigues, D.; Barbosa, A.I.; Rebelo, R.; Kwon, I.K.; Reis, R.L.; Correlo, V.M. Skin-integrated wearable systems and implantable biosensors: A comprehensive review. Biosensors 2020, 10, 79. [Google Scholar] [CrossRef]
- Godfrey, A. Digital Health: Exploring Use and Integration of Wearables; Academic Press: Cambridge, MA, USA, 2021. [Google Scholar]
- Bhunia, S.; Majerus, S.; Sawan, M. Implantable Biomedical Microsystems: Design Principles and Applications; Elsevier: Amsterdam, The Netherlands, 2015. [Google Scholar]
- Karacolak, T.; Hood, A.Z.; Topsakal, E. Design of a dual-band implantable antenna and development of skin mimicking gels for continuous glucose monitoring. IEEE Trans. Microw. Theory Tech. 2008, 56, 1001–1008. [Google Scholar] [CrossRef]
- Topsakal, E. Antennas for medical applications: Ongoing research and future challenges. In Proceedings of the 2009 International Conference on Electromagnetics in Advanced Applications, Turin, Italy, 14–18 September 2009; pp. 890–893. [Google Scholar]
- Duan, Z.; Guo, Y.X.; Xue, R.F.; Je, M.; Kwong, D.L. Differentially fed dual-band implantable antenna for biomedical applications. IEEE Trans. Antennas Propag. 2012, 60, 5587–5595. [Google Scholar] [CrossRef]
- Sondaş, A.; Ucar, M.H.B. An implantable microstrip antenna design for MICS-band biomedical applications. Turk. J. Electr. Eng. Comput. Sci. 2016, 24, 2267–2273. [Google Scholar] [CrossRef]
- Palandoken, M. Compact bioimplantable MICS and ISM band antenna design for wireless biotelemetry applications. Radioengineering 2017, 26, 917–923. [Google Scholar] [CrossRef]
- Akbarpour, A.; Chamaani, S. Dual-band electrically coupled loop antenna for implant applications. IET Microwaves Antennas Propag. 2017, 11, 1020–1023. [Google Scholar] [CrossRef]
- Basir, A.; Bouazizi, A.; Zada, M.; Iqbal, A.; Ullah, S.; Naeem, U. A dual-band implantable antenna with wide-band characteristics at MICS and ISM bands. Microw. Opt. Technol. Lett. 2018, 60, 2944–2949. [Google Scholar] [CrossRef]
- Yeap, K.; Voon, C.; Hiraguri, T.; Nisar, H. A compact dual-band implantable antenna for medical telemetry. Microw. Opt. Technol. Lett. 2019, 61, 2105–2109. [Google Scholar] [CrossRef]
- Usluer, M.; Cetindere, B.; Basaran, S.C. Compact implantable antenna design for MICS and ISM band biotelemetry applications. Microw. Opt. Technol. Lett. 2020, 62, 1581–1587. [Google Scholar] [CrossRef]
- Yamac, Y.E.; Basaran, S.C. An SRR based miniature implantable antenna with a slit loaded ground at MedRadio and ISM bands for biotelemetry applications. Int. J. Microw.-Comput.-Aided Eng. 2020, 30, e22406. [Google Scholar] [CrossRef]
- Wu, Q.H.; Xuan, X.W.; Wang, W.; Li, K.; Zhao, H.B. A miniaturized implantable planar inverted-F antenna for biotelemetry applications at 2.45 GHz industrial, scientific, and medical band. Microw. Opt. Technol. Lett. 2020, 62, 391–396. [Google Scholar] [CrossRef]
- Ucar, M.H.B.; Uras, E. Multilayer Archimedean spiral antenna design for dual-band intra-arm implantable biotelemetric smart health care monitoring system covering MICS and ISM bands. Frequenz 2022, 76, 441–452. [Google Scholar] [CrossRef]
- Ucar, M.H.B.; Uras, E. Numerical analysis, prototype implementation and in-vitro measurement of MICS/ISM band microstrip implant antennas for medical implant communication systems. J. Fac. Eng. Archit. Gazi Univ. 2022, 37, 2177–2191. [Google Scholar]
- Yamac, Y.E.; Ciflik, M.; Basaran, S.C. Miniaturized multiband implantable antenna designs for in-body compact medical devices. Int. J. Microw.-Comput.-Aided Eng. 2022, 32, e23335. [Google Scholar] [CrossRef]
- Celik, O.F.; Yamac, Y.E.; Basaran, S.C. Compact multi-band implantable antenna designs for versatile in-body applications. AEU-Int. J. Electron. Commun. 2022, 150, 154204. [Google Scholar] [CrossRef]
- Karacolak, T.; Cooper, R.; Topsakal, E. Electrical properties of rat skin and design of implantable antennas for medical wireless telemetry. IEEE Trans. Antennas Propag. 2009, 57, 2806–2812. [Google Scholar] [CrossRef]
- Karacolak, T.; Cooper, R.; Butler, J.; Fisher, S.; Topsakal, E. In vivo verification of implantable antennas using rats as model animals. IEEE Antennas Wirel. Propag. Lett. 2010, 9, 334–337. [Google Scholar] [CrossRef]
- Kiourti, A.; Psathas, K.A.; Lelovas, P.; Kostomitsopoulos, N.; Nikita, K.S. In vivo tests of implantable antennas in rats: Antenna size and intersubject considerations. IEEE Antennas Wirel. Propag. Lett. 2013, 12, 1396–1399. [Google Scholar] [CrossRef]
- Liu, C.; Guo, Y.X.; Jegadeesan, R.; Xiao, S. In vivo testing of circularly polarized implantable antennas in rats. IEEE Antennas Wirel. Propag. Lett. 2014, 14, 783–786. [Google Scholar] [CrossRef]
- Lei, W.; Guo, Y.X. Miniaturized differentially fed dual-band implantable antenna: Design, realization, and in vitro test. Radio Sci. 2015, 50, 959–967. [Google Scholar] [CrossRef]
- Liu, Y.; Chen, Y.; Lin, H.; Juwono, F.H. A novel differentially fed compact dual-band implantable antenna for biotelemetry applications. IEEE Antennas Wirel. Propag. Lett. 2016, 15, 1791–1794. [Google Scholar] [CrossRef]
- Nguyen, V.T.; Jung, C.W. Radiation-pattern reconfigurable antenna for medical implants in MedRadio band. IEEE Antennas Wirel. Propag. Lett. 2015, 15, 106–109. [Google Scholar] [CrossRef]
- Fan, Y.; Huang, J.; Chang, T.; Liu, X. A miniaturized four-element MIMO antenna with EBG for implantable medical devices. IEEE J. Electromagn. Microwaves Med. Biol. 2018, 2, 226–233. [Google Scholar] [CrossRef]
- Blauert, J.; Kang, Y.S.; Kiourti, A. In vivo testing of a miniature 2.4/4.8 GHz implantable antenna in postmortem human subject. IEEE Antennas Wirel. Propag. Lett. 2018, 17, 2334–2338. [Google Scholar] [CrossRef]
- Faisal, F.; Yoo, H. A miniaturized novel-shape dual-band antenna for implantable applications. IEEE Trans. Antennas Propag. 2018, 67, 774–783. [Google Scholar] [CrossRef]
- Ketavath, K.N.; Gopi, D.; Rani, S.S. In-vitro test of miniaturized CPW-fed implantable conformal patch antenna at ISM band for biomedical applications. IEEE Access 2019, 7, 43547–43554. [Google Scholar] [CrossRef]
- Ganeshwaran, N.; Jeyaprakash, J.K.; Alsath, M.G.N.; Sathyanarayanan, V. Design of a dual-band circular implantable antenna for biomedical applications. IEEE Antennas Wirel. Propag. Lett. 2019, 19, 119–123. [Google Scholar] [CrossRef]
- Parveen, F.; Wahid, P. Design of Miniaturized Antipodal Vivaldi Antennas for Wideband Microwave Imaging of the Head. Electronics 2022, 11, 2258. [Google Scholar] [CrossRef]
- ETSI EN 300 328; Data Transmission Equipment Operating in the 2, 4 GHz ISM Band and Using Wide Band Modulation Techniques. ETSI: Valbonne, France, 2006.
- ETSI EN 301 839-1; Ultra Low Power Active Medical Implants (ULP-AMI) and Associated Peripherals (ULP-AMI-P) Operating in the Frequency Range 402 MHz to 405 MHz. ETSI: Valbonne, France, 2007.
- Federal Communications Commission. FCC CFR 95.601-95.673 Subpart E 47; Medical Implant Communication Service; FCC: Washington, DC, USA, 1999. [Google Scholar]
- Cole, K.S.; Cole, R.H. Dispersion and absorption in dielectrics I. Alternating current characteristics. J. Chem. Phys. 1941, 9, 341–351. [Google Scholar] [CrossRef]
- CadNav. Laboratory Rat 3D Model 2023. Available online: https://www.cadnav.com/3d-models/model-19550.html (accessed on 20 April 2023).
- Li, J.; Yuan, Y.; Yang, G.; Wu, Q.; Zhang, W.; Burokur, S.N.; Zhang, K. Hybrid dispersion engineering based on chiral metamirror. Laser Photonics Rev. 2023, 17, 2200777. [Google Scholar] [CrossRef]
















| Coefficients | Single-Pole | Two-Pole | Three-Pole |
|---|---|---|---|
| 21 | |||
| − | |||
| − | |||
| − | − | ||
| − | − | ||
| Liquid Components | Mixture Percentage (%) |
|---|---|
| DGBE (Diethylene Glycol Butyl Ether) | 6.98 |
| Deionized Water | 46.51 |
| Triton X-100 (Polyethylene Glycol Monophenyl Ether) | 46.51 |
| Ref. | Year | Tissue | Band | Bandwidth (MHz) | Geometry | Number of Layers | Dimensions (mm) | SC * Pin |
|---|---|---|---|---|---|---|---|---|
| [27] | 2009 | Rat Skin | MICS ISM | 27 180 | Meander Line | 1 | 23 × 23 × 5 | Yes |
| [29] | 2015 | Rat Muscle | ISM | 355 | Helical | 3 | D = 5.5, h = 3.81 | No |
| [30] | 2015 | Human | MedRadio ISM | 32 151 | Meander Arms | 1 | 27 × 9 × 1.27 | Yes |
| [31] | 2016 | Human Skin | MICS ISM | 30 168 | Meander Strip | 1 | 22 × 23 × 1.27 | Yes |
| [33] | 2018 | Human Tissue | ISM | 440 | Four−Element | 2 | 18.5 × 18.5 × 1.27 | No |
| [34] | 2018 | Postmortem Human Subject | ISM | − | E-Shape with Meandering Arms | 1 | 7.7 × 6.9 × 1.52 | Yes |
| [35] | 2019 | Human Skin | ISM | 184.1 219.7 | Novel Flower−Shape | 1 | 7 × 7.2 × 0.2 | Yes |
| [36] | 2019 | Human Tissue | ISM | 810 | Conformal Patch | 2 | 24 × 22 × 0.07 | No |
| [37] | 2020 | Human Tissue | MICS ISM | 127 903 | Patch | 2 | D = 10, h = 2.54 | Yes |
| This Work | Rat Skin | ISM | 100 | Two-Arm rectangular spiral | 2 | 10 × 10 × 2.54 | Yes |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ucar, M.H.B.; Uras, E. A Compact Modified Two-Arm Rectangular Spiral Implantable Antenna Design for ISM Band Biosensing Applications. Sensors 2023, 23, 4883. https://doi.org/10.3390/s23104883
Ucar MHB, Uras E. A Compact Modified Two-Arm Rectangular Spiral Implantable Antenna Design for ISM Band Biosensing Applications. Sensors. 2023; 23(10):4883. https://doi.org/10.3390/s23104883
Chicago/Turabian StyleUcar, Mustafa Hikmet Bilgehan, and Erdem Uras. 2023. "A Compact Modified Two-Arm Rectangular Spiral Implantable Antenna Design for ISM Band Biosensing Applications" Sensors 23, no. 10: 4883. https://doi.org/10.3390/s23104883





