Approach for Non-Intrusive Detection of the Fit of Orthopaedic Devices Based on Vibrational Data
Abstract
:1. Introduction
2. Materials and Methods
2.1. Object of Investigation
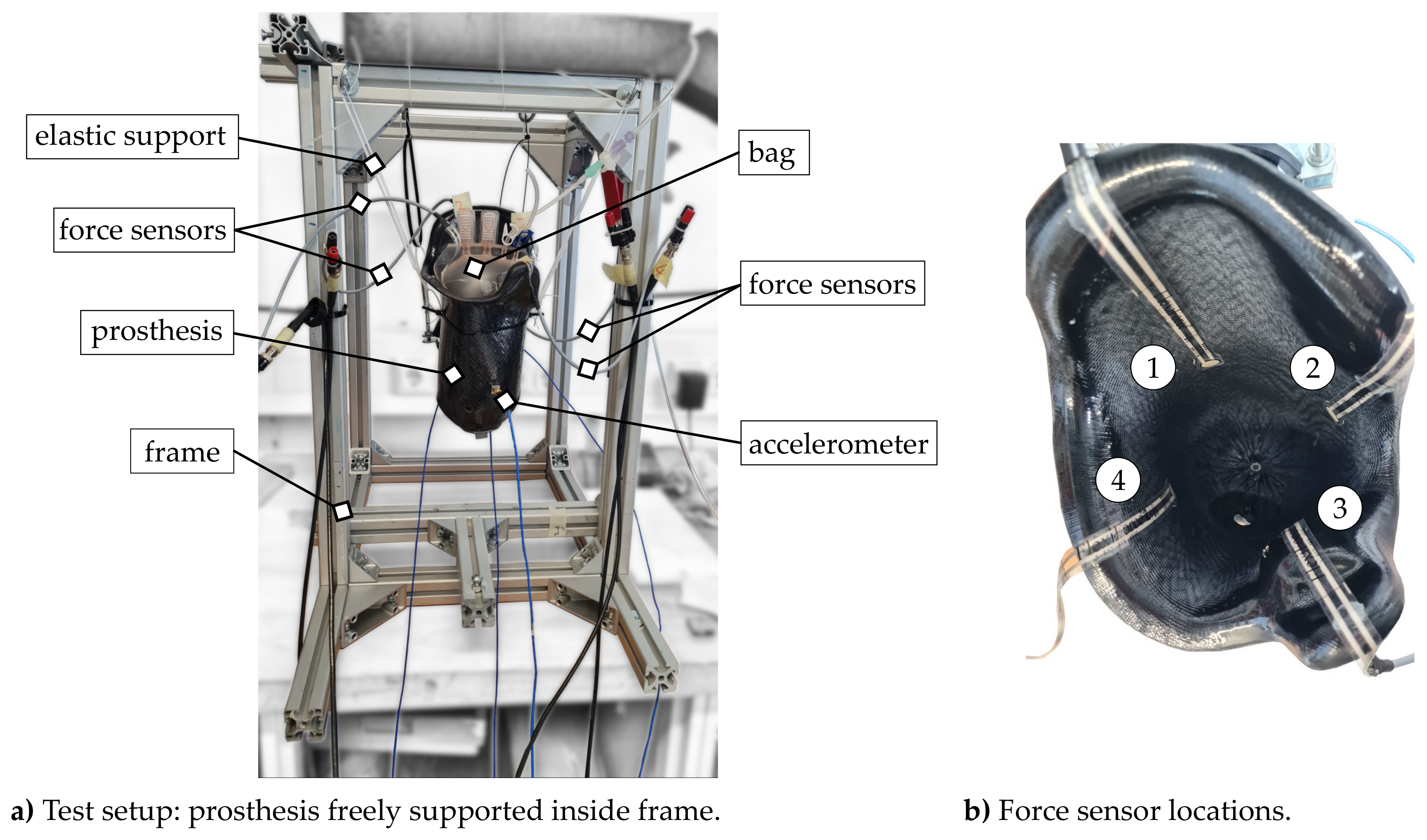
2.2. Experimental Setup
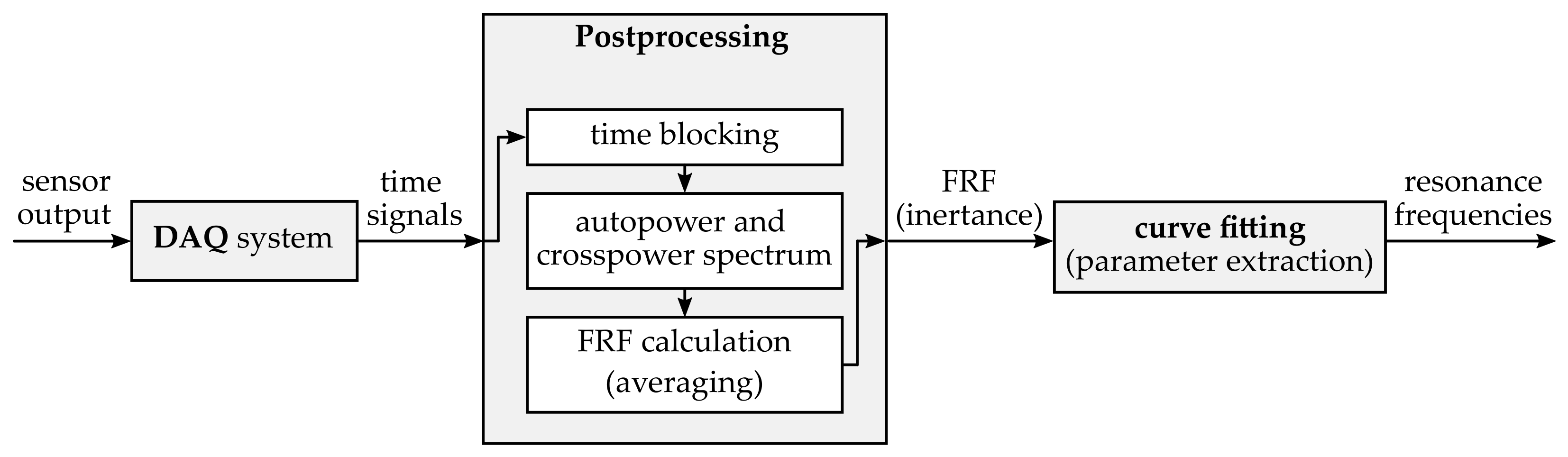
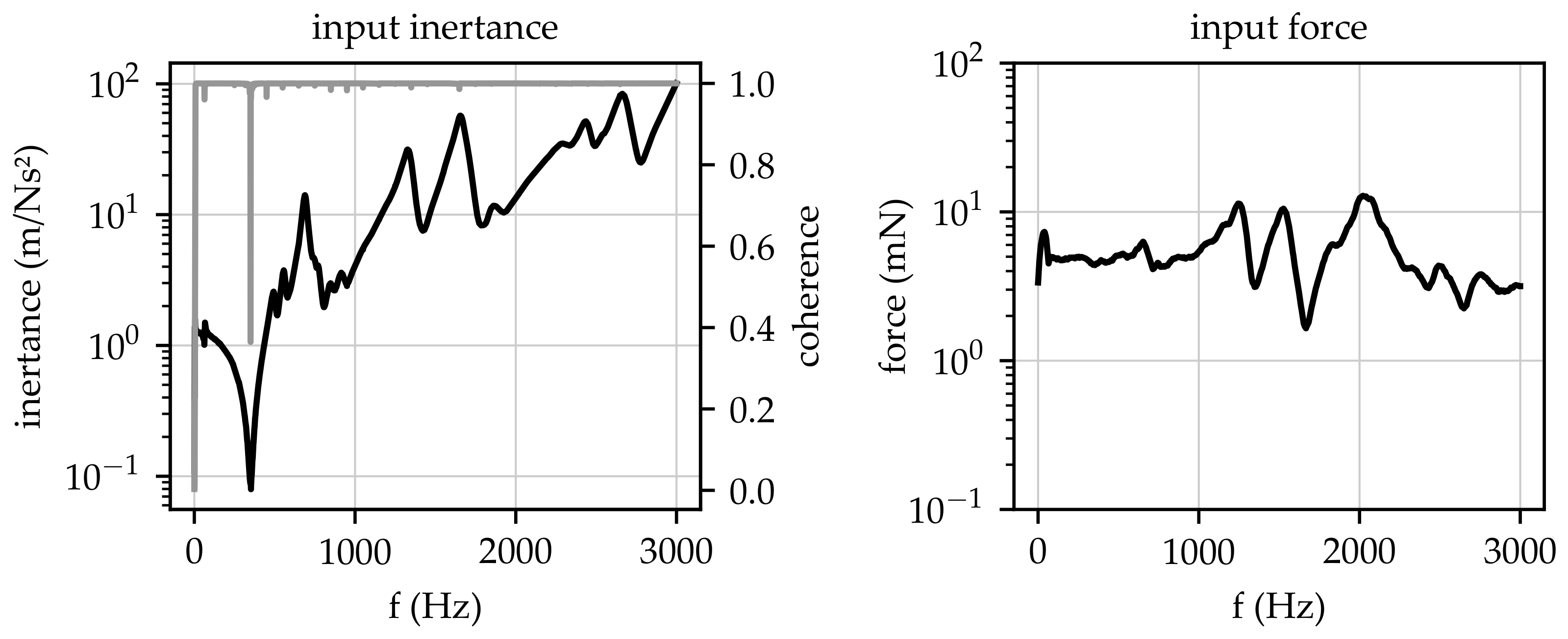
2.3. Test Program and Signal Processing
3. Results
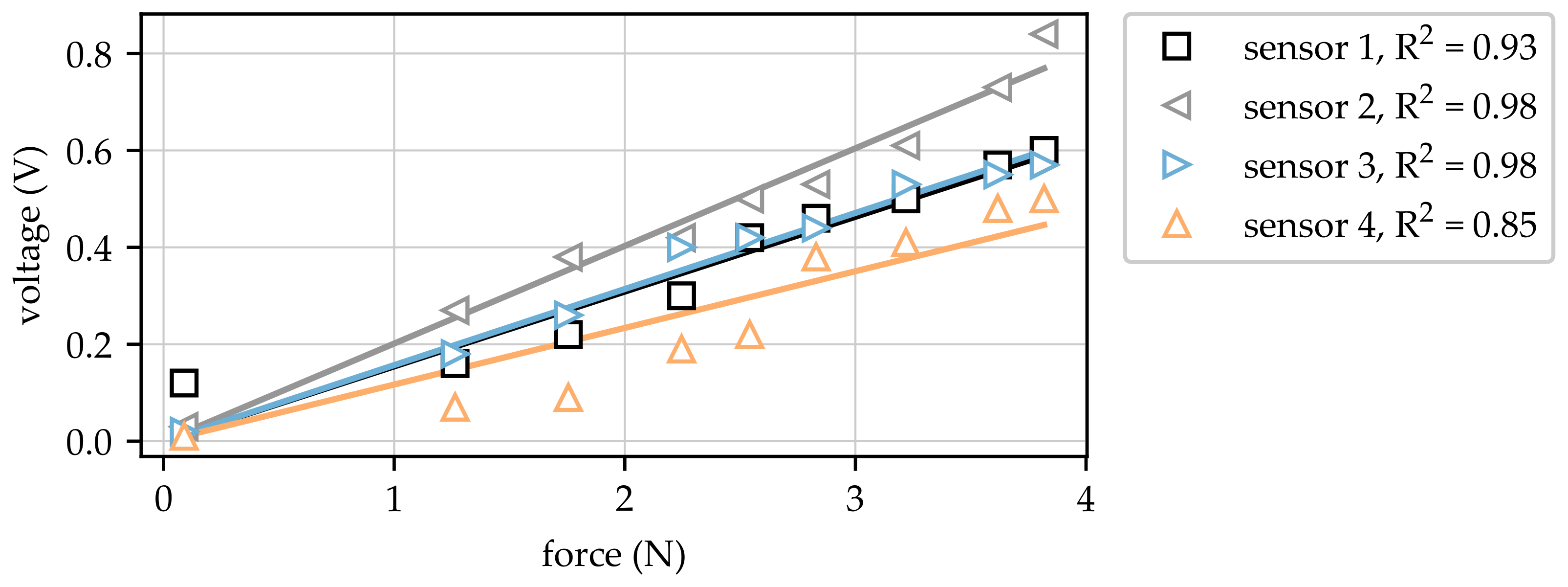
3.1. Force Measurements
3.2. Resonance Frequencies
3.3. Experimental Modal Analysis
4. Discussion
4.1. Acquired Forces Dependent on Applied System Pressure
4.2. Shift in Resonance Frequencies
4.3. Experimental Modal Analysis
4.4. Bags
5. Conclusions
- Changes in local pressure mark locations between residual limbs and prosthesis sockets lead to a change in dynamical behaviour (shift in resonance frequencies);
- System changes in dynamical behaviour can be detected by non-intrusive dynamical measurement at the outer surface of the prosthesis socket;
- The shift in the resonance frequencies depends on the contact force, with increasing forces leading to increasing frequencies;
- Changes in resonance frequencies correlate with the positions of local pressure marks and the dominant surfaces of the corresponding mode shapes.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Sample Availability
Abbreviations
| BC | boundary condition |
| DAQ | data acquisition system |
| EMA | experimental modal analysis |
| PET | polyethylenterephthalat |
| FRF | frequency response function |
References
- Nunes, M.A.; Campos-Neto, I.; Ferraz, L.C.; Lima, C.A.; Rocha, T.O.; Rocha, T.F. Adaptation to prostheses among patients with major lower-limb amputations and its association with sociodemographic and clinical data. Sao Paulo Med. J. Rev. Paul. Med. 2014, 132, 80–84. [Google Scholar] [CrossRef] [Green Version]
- Baars, E.C.; Schrier, E.; Dijkstra, P.U.; Geertzen, J.H.B. Prosthesis satisfaction in lower limb amputees: A systematic review of associated factors and questionnaires. Medicine 2018, 97, e12296. [Google Scholar] [CrossRef]
- Roth, E.V.; Pezzin, L.E.; McGinley, E.L.; Dillingham, T.R. Prosthesis use and satisfaction among persons with dysvascular lower limb amputations across postacute care discharge settings. PM R J. Inj. Funct. Rehabil. 2014, 6, 1128–1136. [Google Scholar] [CrossRef] [PubMed]
- Tran, L.; Caldwell, R.; Quigley, M.; Fatone, S. Stakeholder perspectives for possible residual limb monitoring system for persons with lower-limb amputation. Disabil. Rehabil. 2020, 42, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Bosman, C.E.; van der Sluis, C.K.; Geertzen, J.H.B.; Kerver, N.; Vrieling, A.H. User-relevant factors influencing the prosthesis use of persons with a transfemoral amputation or knee-disarticulation: A meta-synthesis of qualitative literature and focus group results. PLoS ONE 2023, 18, e0276874. [Google Scholar] [CrossRef]
- Henao, S.C.; Orozco, C.; Ramírez, J. Influence of Gait Cycle Loads on Stress Distribution at The Residual Limb/Socket Interface of Transfemoral Amputees: A Finite Element Analysis. Sci. Rep. 2020, 10, 4985. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Colombo, G.; Comotti, C.; Redaelli, D.F.; Regazzoni, D.; Rizzi, C.; Vitali, A. A Method to Improve Prosthesis Leg Design Based on Pressure Analysis at the Socket-Residual Limb Interface. In Proceedings of the ASME 2016 International Design Engineering Technical Conferences and Computers and Information in Engineering Conference, Charlotte, NC, USA, 21–24 August 2016. [Google Scholar] [CrossRef]
- Carabello, A.; Schellnock, J.; Schleifenbaum, S.; Hömme, A.K.; Felderhoff, T.; Menküc, B.; Drossel, W.G. Investigation of Orthopedic Prosthesis Socket Management after Transfemoral Amputation by Expert Survey. Prosthesis 2021, 3, 137–156. [Google Scholar] [CrossRef]
- Paternò, L.; Ibrahimi, M.; Rosini, E.; Menfi, G.; Monaco, V.; Gruppioni, E.; Ricotti, L.; Menciassi, A. Residual limb volume fluctuations in transfemoral amputees. Sci. Rep. 2021, 11, 12273. [Google Scholar] [CrossRef]
- Lorenzelli, L.; Sordo, G.; Bagolini, A.; Resta, G. Socketmaster: Integrated Sensors System for the Optimised Design of Prosthetic Socket for above Knee Amputees. In Proceedings of the 2017 New Generation of CAS (NGCAS), Genova, Italy, 6–9 September 2017; pp. 233–236. [Google Scholar] [CrossRef]
- Dejke, V.; Eng, M.P.; Brinkfeldt, K.; Charnley, J.; Lussey, D.; Lussey, C. Development of Prototype Low-Cost QTSS™ Wearable Flexible More Enviro-Friendly Pressure, Shear, and Friction Sensors for Dynamic Prosthetic Fit Monitoring. Sensors 2021, 21, 3764. [Google Scholar] [CrossRef]
- Hopkins, M.O.; Turner, S.; Vaidyanathan, R.; McGregor, A. Mapping Lower-Limb Prosthesis Load Distributions Using a Low-Cost Pressure Measurement System. Front. Med. Technol. 2022, 4, 908002. [Google Scholar] [CrossRef]
- Hopkins, M.; Vaidyanathan, R.; Mcgregor, A.H. Examination of the Performance Characteristics of Velostat as an In-Socket Pressure Sensor. IEEE Sens. J. 2020, 20, 6992–7000. [Google Scholar] [CrossRef]
- Agcayazi, T.; McKnight, M.; Sotory, P.; Huang, H.; Ghosh, T.; Bozkurt, A. A scalable shear and normal force sensor for prosthetic sensing. In Proceedings of the 2017 IEEE Sensors, Glasgow, UK, 29 October–1 November 2017; pp. 1–3. [Google Scholar] [CrossRef]
- Oldfrey, B.; Tchorzewska, A.; Jackson, R.; Croysdale, M.; Loureiro, R.; Holloway, C.; Miodownik, M. Additive manufacturing techniques for smart prosthetic liners. Med. Eng. Phys. 2021, 87, 45–55. [Google Scholar] [CrossRef]
- Kim, K.; Choi, J.; Jeong, Y.; Cho, I.; Kim, M.; Kim, S.; Oh, Y.; Park, I. Highly Sensitive and Wearable Liquid Metal-Based Pressure Sensor for Health Monitoring Applications: Integration of a 3D-Printed Microbump Array with the Microchannel. Adv. Healthc. Mater. 2019, 8, e1900978. [Google Scholar] [CrossRef] [PubMed]
- Armitage, L.; Rajan, G.; Kark, L.; Simmons, A.; Prusty, B.G. Simultaneous Measurement of Normal and Shear Stress Using Fiber Bragg Grating Sensors in Prosthetic Applications. IEEE Sens. J. 2019, 19, 7383–7390. [Google Scholar] [CrossRef]
- Bunge, C.A.; Kallweit, J.P.; Houri, M.A.; Mohr, B.; Berzios, A.; Grauberger, C.; Adi, P.; Gries, T. Textile Multitouch Force-Sensor Array Based on Circular and Non-Circular Polymer Optical Fibers. IEEE Sens. J. 2020, 20, 7548–7555. [Google Scholar] [CrossRef]
- Henrikson, K.M.; Weathersby, E.J.; Larsen, B.G.; Cagle, J.C.; McLean, J.B.; Sanders, J.E. An Inductive Sensing System to Measure In-Socket Residual Limb Displacements for People Using Lower-Limb Prostheses. Sensors 2018, 18, 3840. [Google Scholar] [CrossRef] [Green Version]
- Neupetsch, C.; Hensel, E.; Kranz, B.; Drossel, W.G.; Felderhoff, T.; Heyde, C.E. Proof of Concept for the Detection of Local Pressure Marks in Prosthesis Sockets Using Structural Dynamics Measurement. Sensors 2021, 21, 3821. [Google Scholar] [CrossRef]
- Neupetsch, C.; Hensel, E.; Werner, M.; Meißner, S.; Troge, J.; Drossel, W.G.; Rotsch, C. Development and Validation of Bone Models using Structural Dynamic Measurement Methods. Curr. Dir. Biomed. Eng. 2019, 5, 343–345. [Google Scholar] [CrossRef]
- Swanson, E.; Weathersby, E.; Cagle, J.; Sanders, J.E. Evaluation of Force Sensing Resistors for the Measurement of Interface Pressures in Lower Limb Prosthetics. J. Biomech. Eng. 2019, 141, 1010091–10100913. [Google Scholar] [CrossRef]
- Chen, D.; Su, P.; Ottikkutti, S.; Vartholomeos, P.; Tahmasebi, K.N.; Karamousadakis, M. Analyzing Dynamic Operational Conditions of Limb Prosthetic Sockets with a Mechatronics-Twin Framework. Appl. Sci. 2022, 12, 986. [Google Scholar] [CrossRef]
- Jamshidi, M.A.; Esmaili, S.; Azhari, F. A case study on the value of in-socket force measurements in gait monitoring of lower-limb prosthesis users. In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Glasgow, UK, 11–15 July 2022; pp. 4237–4240. [Google Scholar] [CrossRef]
- Ewins, D.J. Modal Testing: Theory and Practice; Mechanical Engineering Research Studies Engineering Dynamics Series; Research Studies Press: Taunton, UK, 1991; Volume 2. [Google Scholar]
- Craig, R.R.; Kurdila, A. Fundamentals of Structural Dynamics, 2nd ed.; John Wiley: Hoboken, NJ, USA, 2006. [Google Scholar]
- Al-Fakih, E.A.; Abu Osman, N.A.; Mahmad Adikan, F.R. Techniques for Interface Stress Measurements within Prosthetic Sockets of Transtibial Amputees: A Review of the Past 50 Years of Research. Sensors 2016, 16, 1119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paterno, L.; Ibrahimi, M.; Gruppioni, E.; Menciassi, A.; Ricotti, L. Sockets for Limb Prostheses: A Review of Existing Technologies and Open Challenges. IEEE Trans. Bio-Med. Eng. 2018, 65, 1996–2010. [Google Scholar] [CrossRef] [PubMed]
- Sanders, J.E.; Cagle, J.C.; Harrison, D.S.; Myers, T.R.; Allyn, K.J. How does adding and removing liquid from socket bladders affect residual-limb fluid volume? J. Rehabil. Res. Dev. 2013, 50, 845–860. [Google Scholar] [CrossRef] [PubMed]
- Highsmith, J.T.; Highsmith, M.J. Common skin pathology in LE prosthesis users. JAAPA 2007, 20, 33–36. [Google Scholar] [CrossRef] [PubMed]
- Greitemann, B. Technische Orthopädie: Prothetik an der unteren Extremität am Beispiel der Oberschenkelamputation. Z. Orthop. Unfallchir. 2017, 155, 737–749. [Google Scholar] [CrossRef]
- Müller, P.; Hensel, E. Investigation on similarity laws for dynamic properties of presses. Prod. Eng. 2017, 11, 655–664. [Google Scholar] [CrossRef]
- Ahmadizadeh, C.; Pousett, B.; Menon, C. Towards Management of Residual Limb Volume: Monitoring the Prosthetic Interface Pressure to Detect Volume Fluctuations—A Feasibility Study. Appl. Sci. 2020, 10, 6841. [Google Scholar] [CrossRef]
- Melia, M.; Schmidt, M.; Geissler, B.; König, J.; Krahn, U.; Ottersbach, H.J.; Letzel, S.; Muttray, A. Measuring mechanical pain: The refinement and standardization of pressure pain threshold measurements. Behav. Res. Methods 2015, 47, 216–227. [Google Scholar] [CrossRef]
- Tang, J.; McGrath, M.; Hale, N.; Jiang, L.; Bader, D.; Laszczak, P.; Moser, D.; Zahedi, S. A combined kinematic and kinetic analysis at the residuum/socket interface of a knee-disarticulation amputee. Med. Eng. Phys. 2017, 49, 131–139. [Google Scholar] [CrossRef] [Green Version]
- Laszczak, P.; McGrath, M.; Tang, J.; Gao, J.; Jiang, L.; Bader, D.L.; Moser, D.; Zahedi, S. A pressure and shear sensor system for stress measurement at lower limb residuum/socket interface. Med. Eng. Phys. 2016, 38, 695–700. [Google Scholar] [CrossRef] [Green Version]
- Lee, V.S.; Solomonidis, S.E.; Spence, W.D. Stump-socket interface pressure as an aid to socket design in prostheses for trans-femoral amputees—A preliminary study. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 1997, 211, 167–180. [Google Scholar] [CrossRef]
- Sadeeq, A.; Osman, N.A.A.; Eshraghi, A.; Gholizadeh, H.; bin Abd Razak, N.A.; bin Wan Abas, W.A. Interface pressure in transtibial socket during ascent and descent on stairs and its effect on patient satisfaction. Clin. Biomech. 2013, 28, 994–999. [Google Scholar] [CrossRef] [Green Version]







Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Neupetsch, C.; Hensel, E.; Heinke, A.; Stapf, T.; Stecher, N.; Malberg, H.; Heyde, C.-E.; Drossel, W.-G. Approach for Non-Intrusive Detection of the Fit of Orthopaedic Devices Based on Vibrational Data. Sensors 2023, 23, 6500. https://doi.org/10.3390/s23146500
Neupetsch C, Hensel E, Heinke A, Stapf T, Stecher N, Malberg H, Heyde C-E, Drossel W-G. Approach for Non-Intrusive Detection of the Fit of Orthopaedic Devices Based on Vibrational Data. Sensors. 2023; 23(14):6500. https://doi.org/10.3390/s23146500
Chicago/Turabian StyleNeupetsch, Constanze, Eric Hensel, Andreas Heinke, Tom Stapf, Nico Stecher, Hagen Malberg, Christoph-Eckhard Heyde, and Welf-Guntram Drossel. 2023. "Approach for Non-Intrusive Detection of the Fit of Orthopaedic Devices Based on Vibrational Data" Sensors 23, no. 14: 6500. https://doi.org/10.3390/s23146500




