A Miniaturized Tri-Band Implantable Antenna for ISM/WMTS/Lower UWB/Wi-Fi Frequencies
Abstract
1. Introduction
- The proposed structure is a compact antenna with simple and planar configurations. Existing structures are designed using multiple layers, shoring pins, and PIFA technology, making the antenna thicker and more complex.
- Most Tri-band antennas are designed to resonate at ISM and WMTS bands, whereas the literature shows that the Ultra-wideband spectrum has significant advantages for Intra-body communication. Triple-band resonance was selected to make the antenna suitable for commercial body area network applications.
- The antenna has flexible characteristics, robust to structural deformation, size and shape of the tissue.
- Wider impedance bandwidth to sustain the frequency detuning effect caused by the heterogeneous body tissue effect in real-time scenarios.
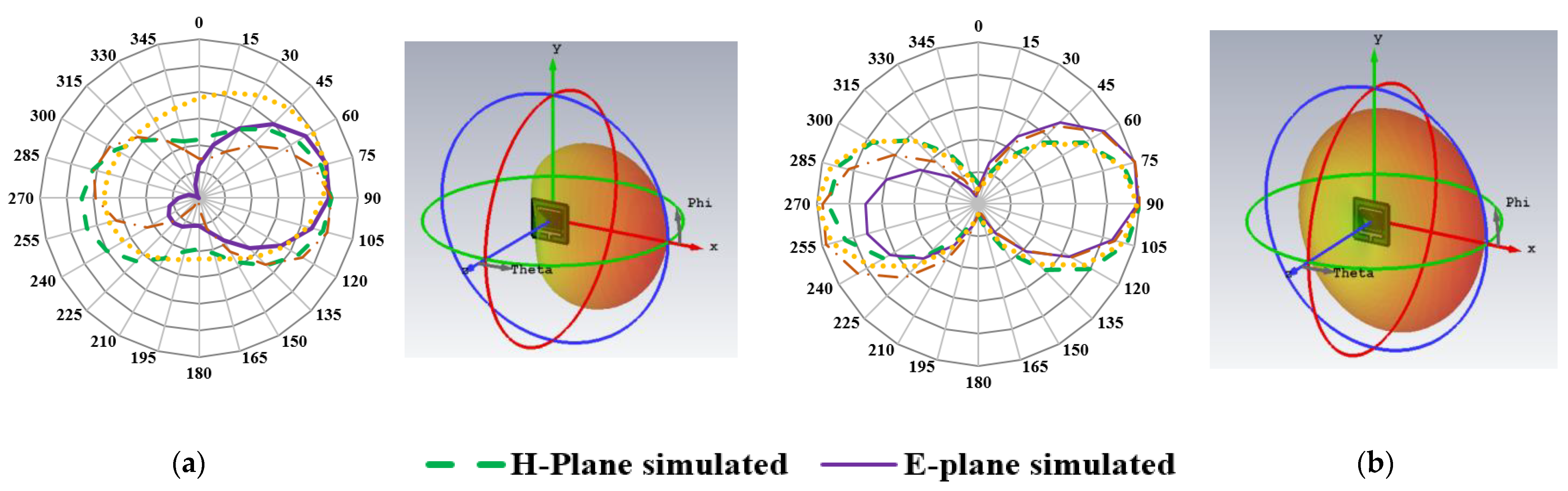
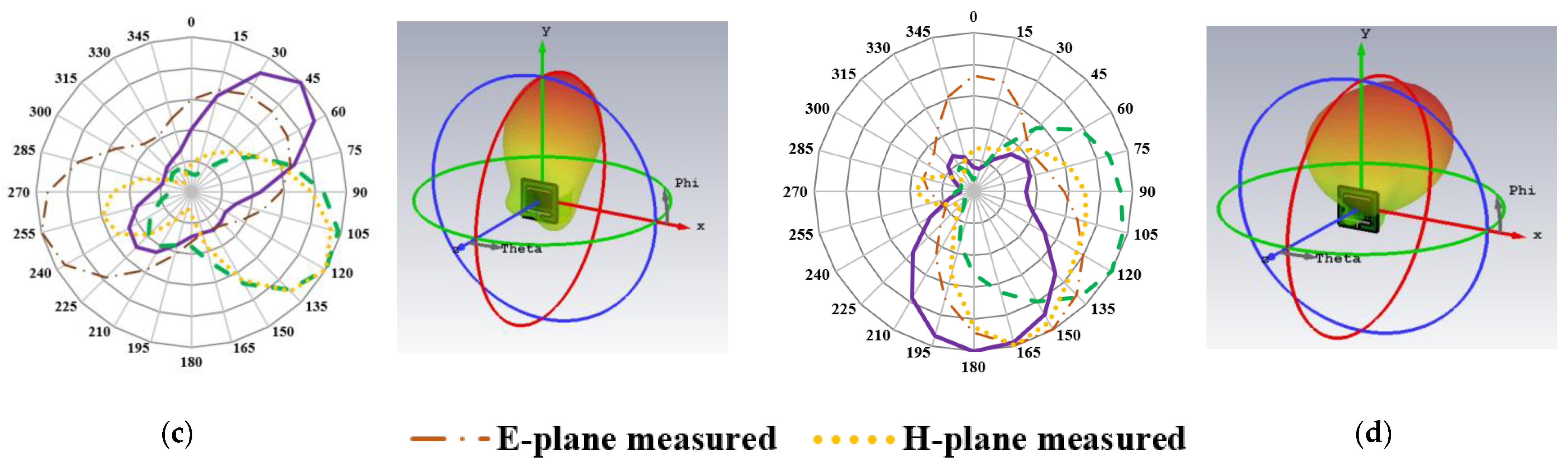
- Broadside radiation characteristics with better gain for reliable communication link and low specific absorption rates.
2. Geometry and Design Mechanism of Antenna
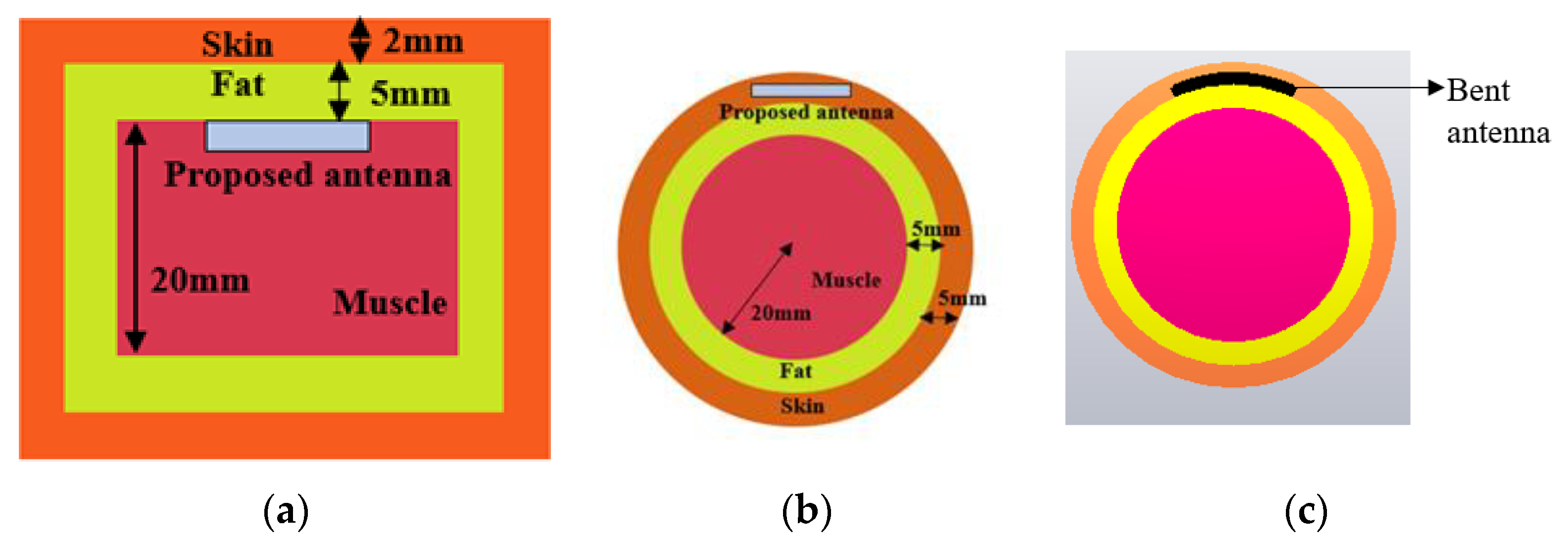
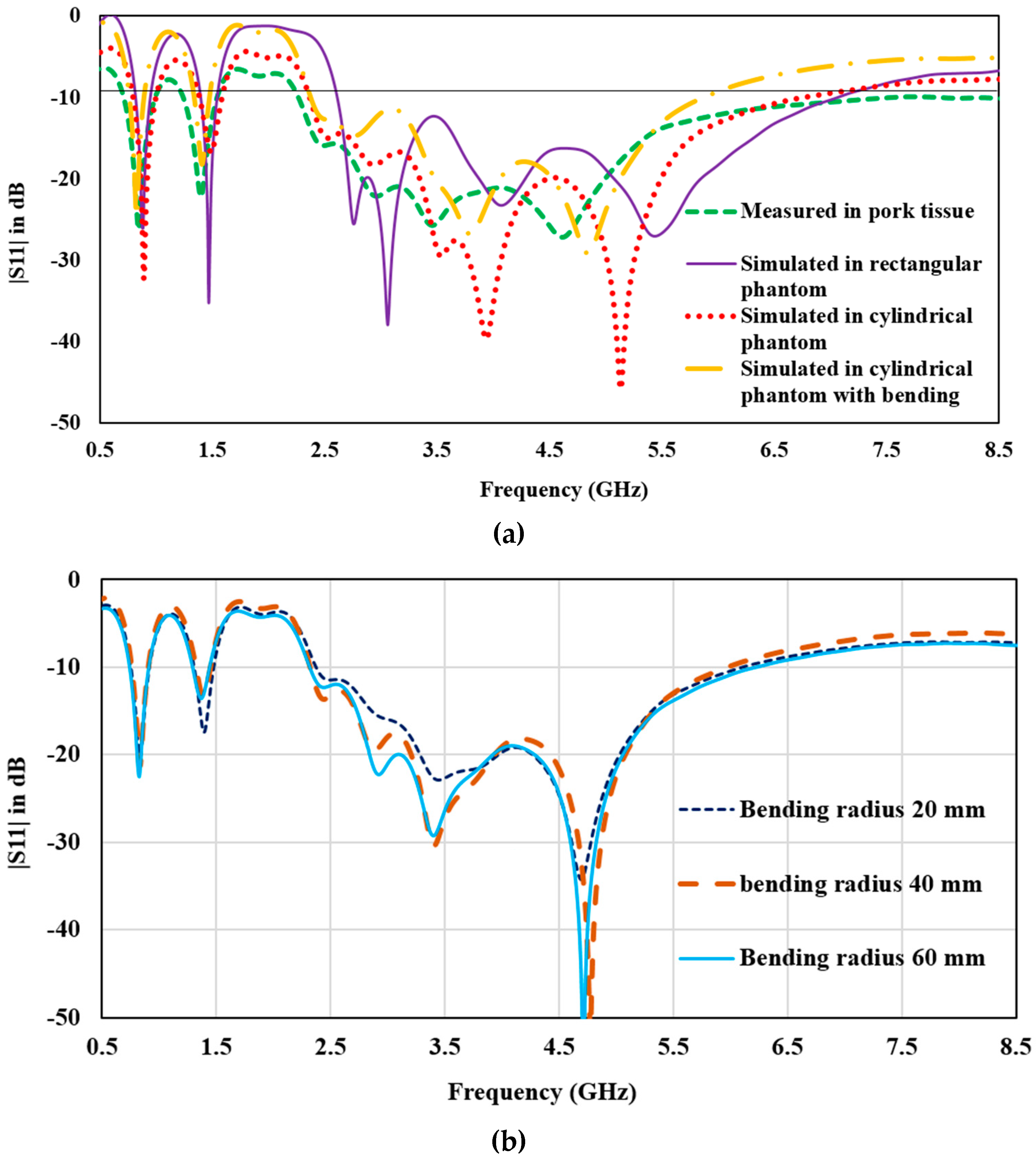
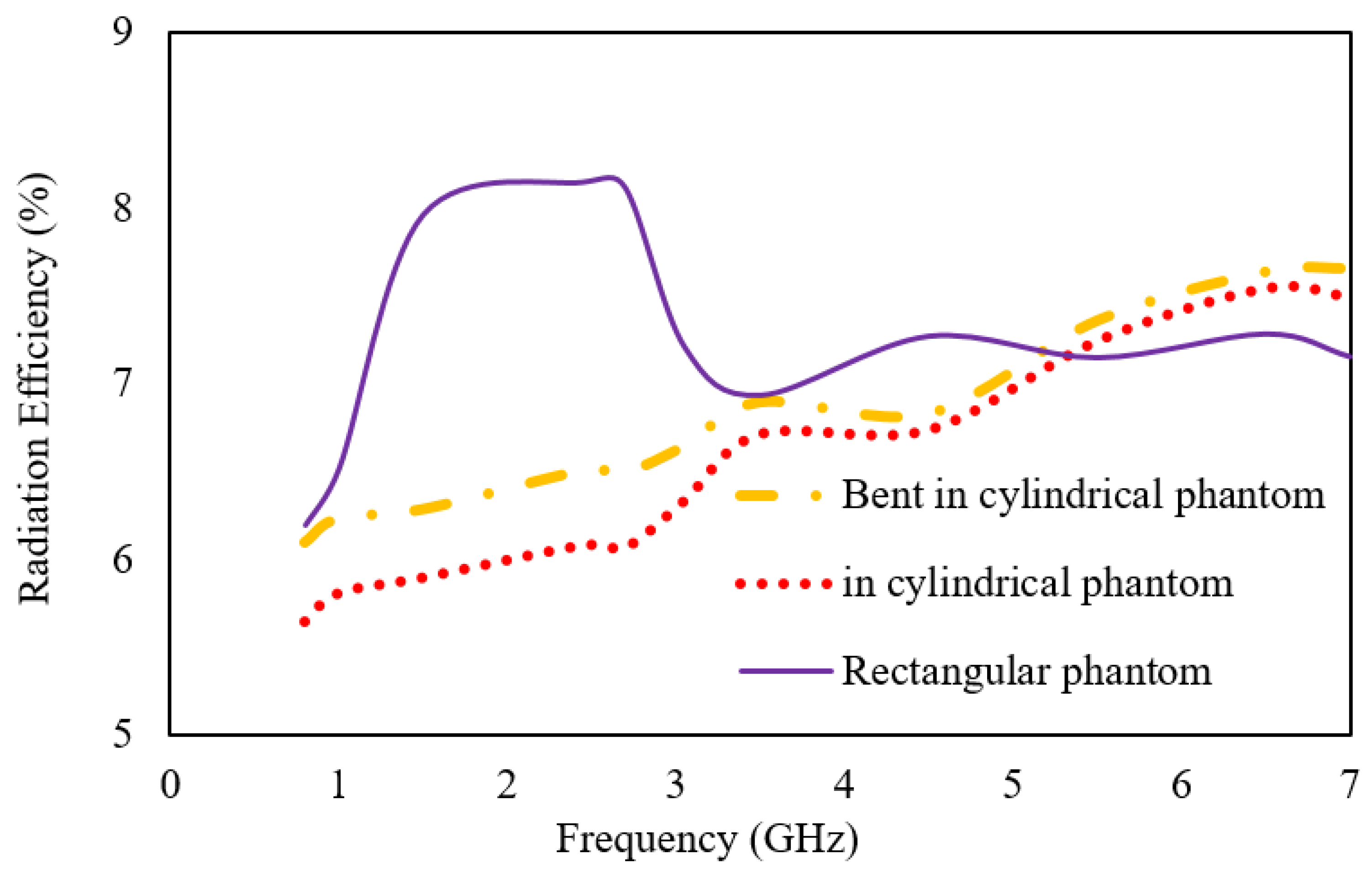
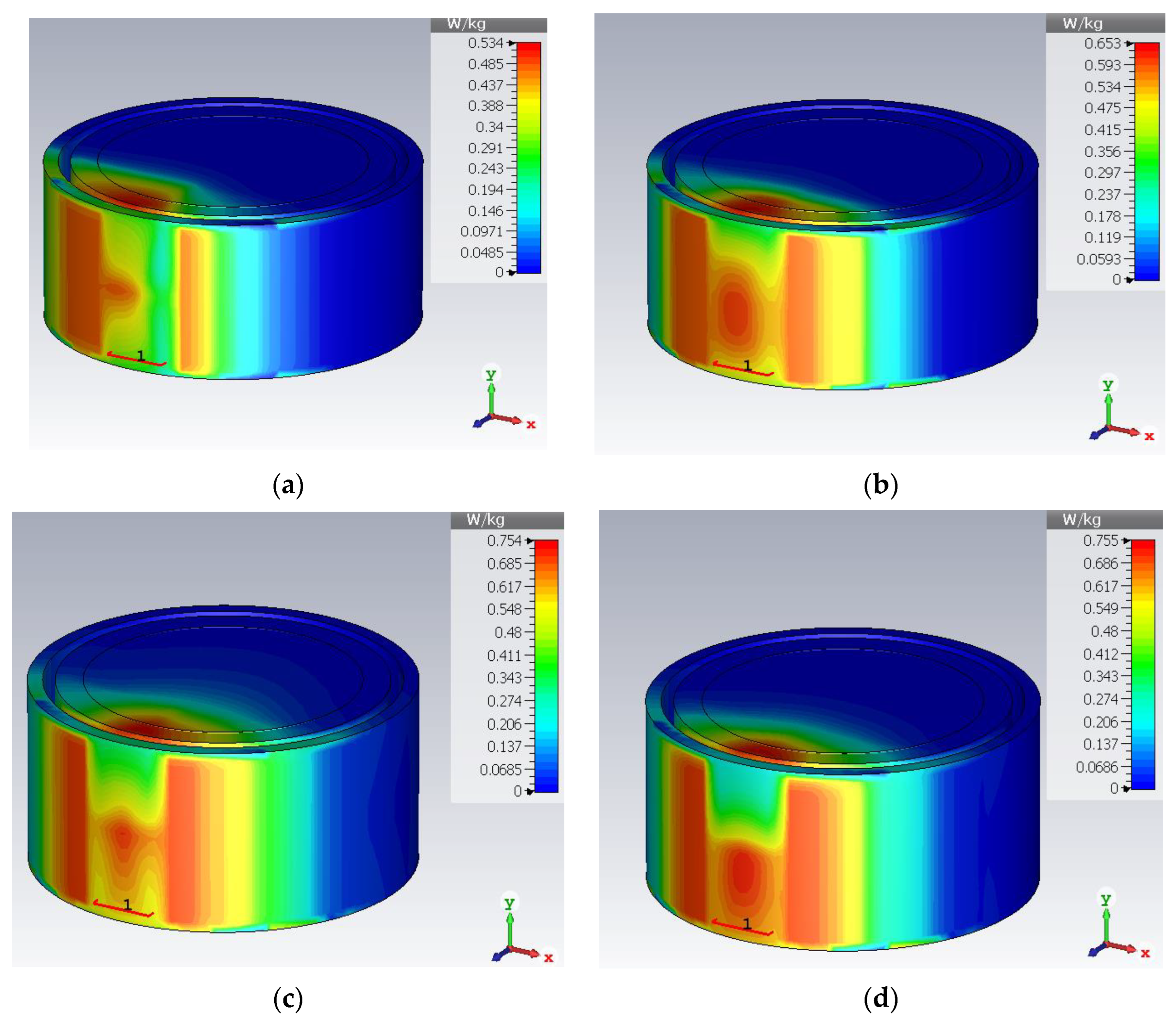
- Numerical modelling of tissue: As the proposed structure is designed for implantable application, and a numerical model for the heterogeneous body tissue layers is created. It has three layers: the innermost layer is muscle tissue with a thickness of 20 mm, the middle layer is fat tissue with a 5 mm thickness, and the top layer is skin tissue with a 2 mm thickness. The human body can have different thicknesses of tissues depending upon body type, body fat or mass index, and different organs. In our model, average values for tissue thickness are considered [36,37]. Electromagnetic properties of human tissues have dispersive properties; thus, dispersive models for all three layers are taken from the CST material library for the numerical modelling of the body tissue. The planar dimensions of each layer are taken as 60 mm × 60 mm. Furthermore, to assess the sensitivity and reliability of antenna performance in practical environments, a cylindrical phantom model (radius = 30 mm, height = 40 mm) consists of skin (εr = 38 and σ = 1.46 s/m), fat (εr = 5.2 and σ = 0.10 s/m) and muscle (εr = 52.7 and σ = 1.8 s/m) layers is designed. According to the in-body deployment location, it may be required to bend the structure for the specific tissue. Thus, antenna performance is also observed for bending. Figure 1 shows the modelled tissue phantoms, with the antenna implanted in the muscle layer (rectangular phantom) and skin layer (in cylindrical phantom) for both the flat and bent state.
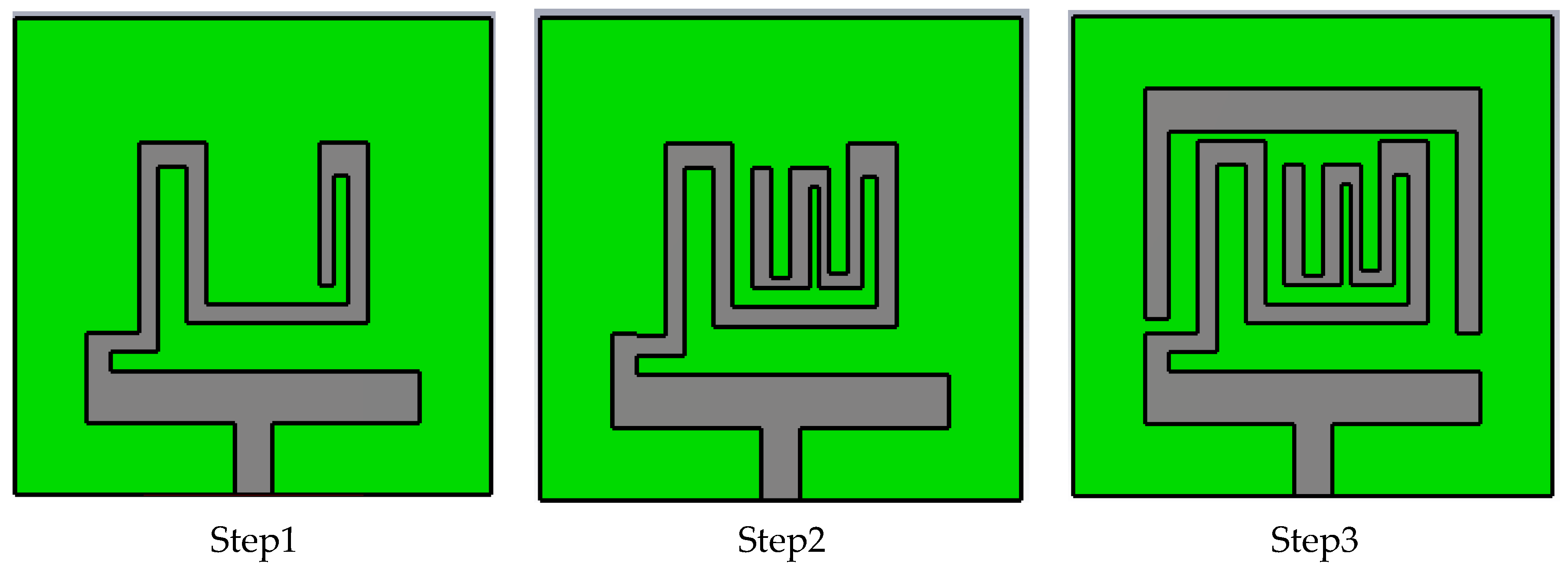
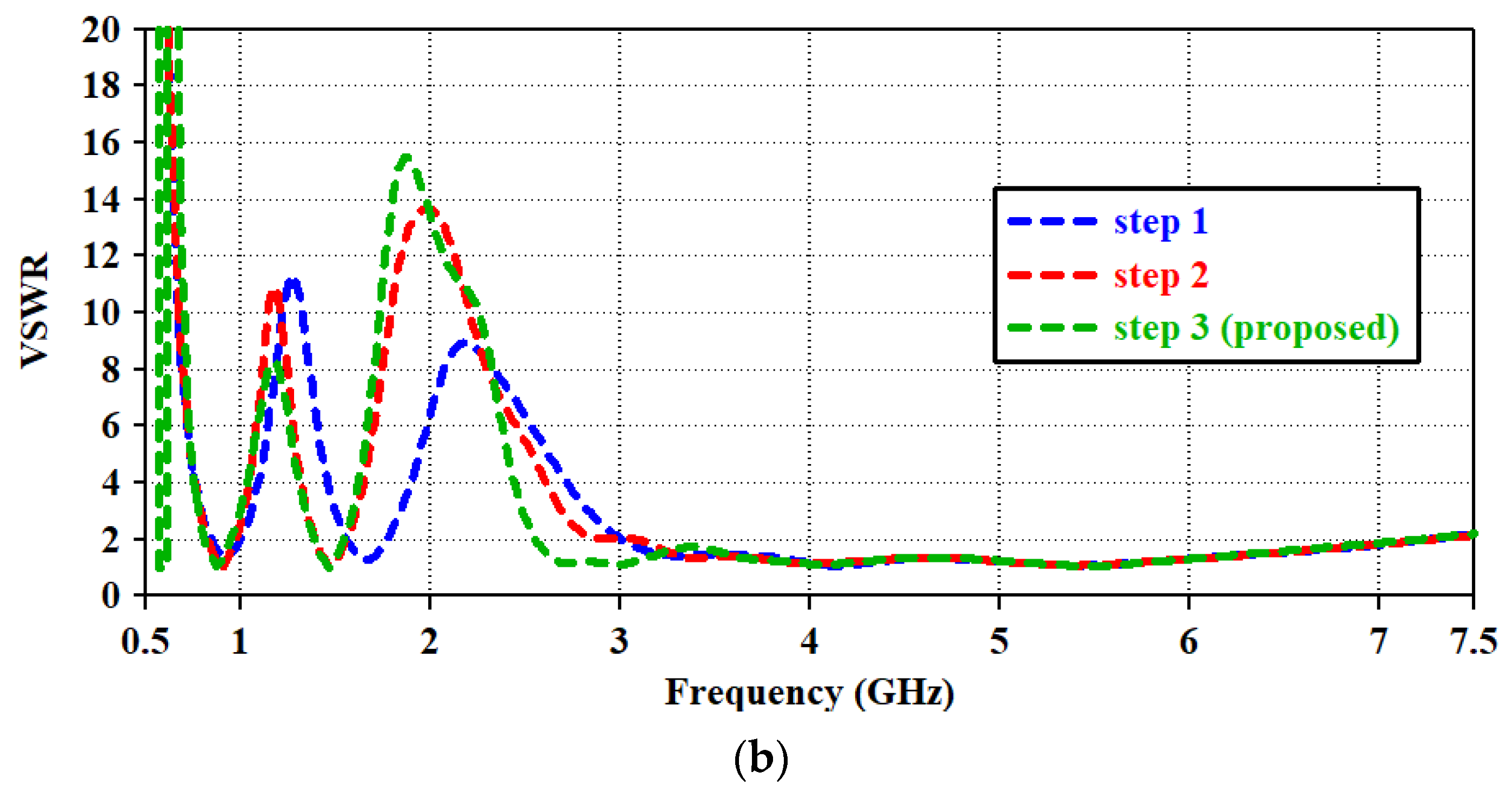
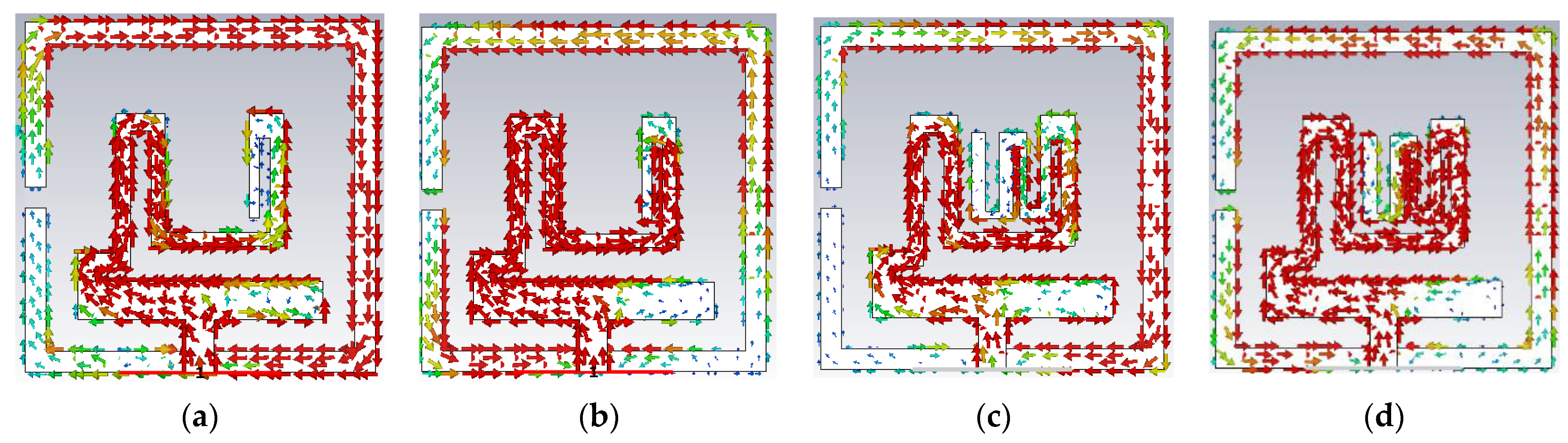
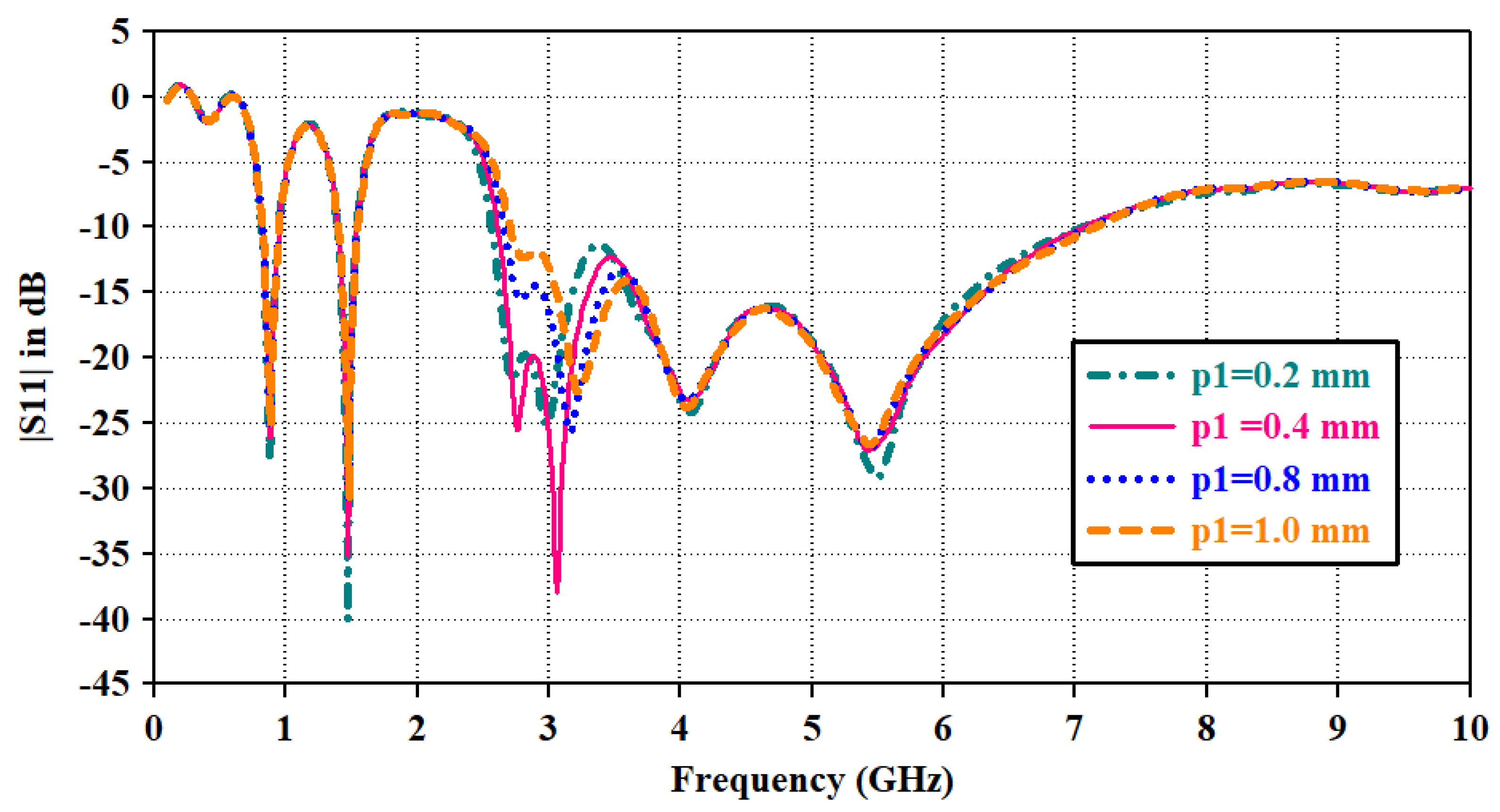
- Antenna Geometry and Design Process: Configuration and geometry of the designed tri-band patch antenna is depicted in Figure 2. Table 2 contains the dimensional parameters of the proposed antenna geometry. The designed microstrip patch antenna consisted of an open-ended square loop-shaped ground plane, an asynchronous meandered radiator and a parasitic patch. The antenna structure is designed on dielectric material RO 3010 with a thickness (h) of 0.125 mm, εr value of 10.2 and δ = 0.0022. The planar size of the structure is 10 mm × 10 mm, which is equivalent to (0.029 λo × 0.029 λo), where λo represents the free-space wavelength at 0.868 GHz (lowest resonance frequency). To use the antenna inside the body tissue, the radiator and ground are covered with the dielectric material layers (RO 3010). It insulates the conducting part of the antenna from lossy tissue layers and also contributes to lowering the resonance frequency. Design evaluation of the proposed structure for attaining wider bandwidth is explained in three steps. Figure 3 shows the step-wise antenna topologies used to attain the desired antenna characteristics.

| Parameter | wg | W, l | w1 | w2 | w3 | w4 | w5 | w6 | w7 | w8 | w9 | w10 | l7 | l9 |
| Value (mm) | 9.4 | 10, 10 | 7 | 4.8 | 1.1 | 0.6 | 1.3 | 1.2 | 0.4 | 0.4 | 0.4 | 1.0 | 0.4 | 7 |
| Parameter | w11 | w12 | w13 | w14 | w15 | l16 | lc | l1 | l2 | l3 | l4 | l5 | l6 | l8 |
| Value (mm) | 1 | 0.9 | 0.3 | 0.5 | 0.8 | 3 | 0.6 | 4.8 | 1.7 | 1.1 | 4.8 | 1.5 | 4.2 | 0.4 |
3. Results and Discussions
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zheng, Y.-L.; Ding, X.-R.; Poon, C.C.Y.; Lo, B.P.L.; Zhang, H.; Zhou, X.-L.; Yang, G.-Z.; Zhao, N.; Zhang, Y.-T. Unobtrusive sensing and wearable devices for health informatics. IEEE Trans. Biomed. Eng. 2014, 61, 1538–1554. [Google Scholar] [CrossRef]
- Rahmat-Samii, Y.; Topsakal, E. Antenna and Sensor Technologies in Modern Medical Applications; Wiley: Hoboken, NJ, USA, 2021. [Google Scholar]
- Andreu-Perez, J.; Leff, D.R.; Ip, H.M.D.; Yang, G. From wearable sensors to smart implants–toward pervasive and personalized healthcare. IEEE Trans. Biomed. Eng. 2015, 62, 2750–2762. [Google Scholar] [CrossRef] [PubMed]
- Joo, H.; Lee, Y.; Kim, J.; Yoo, J.S.; Yoo, S.; Kim, S.; Arya, A.K.; Kim, S.; Choi, S.H.; Lu, N.; et al. Soft Implantable Drug Delivery Device Integrated Wirelessly with Wearable Devices to Treat Fatal Seizures. Sci. Adv. 2021, 7, eabd4639. [Google Scholar] [CrossRef]
- Huang, Z.; Wu, H.; Mahmoud, S.S.; Fang, Q. Design of a Novel Compact MICS Band PIFA Antenna for Implantable Biotelemetry Applications. Sensors 2022, 22, 8182. [Google Scholar] [CrossRef] [PubMed]
- Jovanov, E.; Poon, C.C.; Yang, G.Z.; Zhang, Y.T. Guest editorial body sensor networks: From theory to emerging applications. IEEE Trans. Inf. Technol. Biomed. 2009, 13, 859–863. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.; Wang, J. Applications, challenges, and prospective in emerging body area networking technologies. IEEE Wirel. Commun. 2010, 17, 80–88. [Google Scholar] [CrossRef]
- Duan, Z.; Xu, L.J.; Geyi, W. Metal frame repeater antenna with partial slotted ground for bandwidth enhancement of wristband devices. IET Microw. Antennas Propag. 2017, 11, 1438–1444. [Google Scholar] [CrossRef]
- Liu, C.; Guo, Y.; Xio, S. A review of implantable antennas for wireless biomedical devices. Forum Electromagn. Res. Methods Appl. Technol. (FERMAT) 2016, 14, 1–11. [Google Scholar]
- Soliman, M.M.; Chowdhury, M.E.H.; Khandakar, A.; Islam, M.T.; Qiblawey, Y.; Musharavati, F.; Zal Nezhad, E. Review on Medical Implantable Antenna Technology and Imminent Research Challenges. Sensors 2021, 21, 3163. [Google Scholar] [CrossRef]
- Bonefačić, D.; Bartolić, J. Small Antennas: Miniaturization Techniques and Applications. Automatika 2012, 53, 20–30. [Google Scholar] [CrossRef]
- Wheeler, A. Fundamental Limitations of Small Antennas. Proc. IRE 1947, 35, 1479–1484. [Google Scholar] [CrossRef]
- Le Trong, T.-A.; Shah, S.I.H.; Shin, G.; Radha, S.M.; Yoon, I.-J. A compact triple-band antenna with a broadside radiation characteristic for head-implantable wireless communications. IEEE Antennas Wirel. Propag. Lett. 2021, 20, 958–962. [Google Scholar] [CrossRef]
- Zada, M.; Yoo, H. A miniaturized triple-band implantable antenna system for bio-telemetry applications. IEEE Trans. Antennas Propag. 2018, 66, 7378–7382. [Google Scholar] [CrossRef]
- Shah, S.A.A.; Yoo, H. Scalp-implantable antenna systems for intracranial pressure monitoring. IEEE Trans. Antennas Propag. 2018, 66, 2170–2173. [Google Scholar] [CrossRef]
- Xu, L.-J.; Guo, Y.-X.; Wu, W. Miniaturized dual-band antenna for implantable wireless communications. IEEE Antennas Wirel. Propag. Lett. 2014, 13, 1160–1163. [Google Scholar]
- Gani, I.; Yoo, H. Multi-band antenna system for skin implant. IEEE Microw. Wirel. Compon. Lett. 2016, 26, 294–296. [Google Scholar] [CrossRef]
- Shin, G.; Yoon, I.-J. Investigation on insulated, brain-implanted antenna for highly reliable biotelemetry communication in MICS and ISM bands. Sensors 2019, 20, 242. [Google Scholar] [CrossRef]
- Kaim, V.; Kanaujia, B.K.; Kumar, S.; Choi, H.C.; Kim, K.W.; Rambabu, K. Ultra-miniature circularly polarized CPW-fed implantable antenna design and its validation for biotelemetry applications. Sci. Rep. 2020, 10, 6795. [Google Scholar] [CrossRef]
- Shahverdi, K.; Hashemi, S.; Sarafan, S.; Cao, H. Triple-Band Implantable Antenna Design for Biotelemetry Applications in MICS/ISM/Wi-Fi/Bluetooth Bands. Technologies 2022, 10, 91. [Google Scholar] [CrossRef]
- Çelik, F.; Başaran, S.C. Compact triple-band implantable antenna for multitasking medical devices. J. Electr. Eng. 2022, 73, 166–173. [Google Scholar] [CrossRef]
- Pournoori, N.; Sydänheimo, L.; Rahmat-Samii, Y.; Ukkonen, L.; Björninen, T. Small Triple-Band Meandered PIFA for Brain-Implantable Biotelemetric Systems: Development and Testing in a Liquid Phantom. Int. J. Antennas Propag. 2021, 2021, 6035169. [Google Scholar] [CrossRef]
- Singh, M.S.; Ghosh, J.; Ghosh, S.; Sarkhel, A. Miniaturized dual-antenna system for implantable biotelemetry application. IEEE Antennas Wirel. Propag. Lett. 2021, 20, 1394–1398. [Google Scholar] [CrossRef]
- Shin, G.; Kim, W.; Kim, M.C.; Kim, J.; Chung, J.-Y.; Nah, J.; Yoon, I.-J. A Deionized Water Infilled Dual-Layer Insulator Applied Brain-implanted UWB Antenna for Wireless Biotelemetry Applications. IEEE Trans. Antennas Propag. 2022, 70, 6469–6478. [Google Scholar] [CrossRef]
- Shang, J.; Yu, Y.; Xu, L.-J. Compact dual band implantable planar Inverted-F antenna with bandwidth enhancement. Microw. Opt. Technol. Lett. 2020, 62, 322–328. [Google Scholar] [CrossRef]
- Gupta, V.K.; Thakur, D. Design and performance analysis of a CPW-fed circularly polarized implantable antenna for 2.45 GHz ISM band. Microw. Opt. Technol. Lett. 2020, 62, 3952–3959. [Google Scholar] [CrossRef]
- Nikolayev, D.; Joseph, W.; Skrivervik, A.; Zhadobov, M.; Martens, L.; Sauleau, R. Dielectric-loaded conformal microstrip antennas for versatile in-body applications. IEEE Antennas Wirel. Propag. Lett. 2019, 18, 2686–2690. [Google Scholar] [CrossRef]
- Hadda, L.; Sharma, M.; Gupta, N.; Kumar, S.; Singh, A.K. On-demand reconfigurable WiMAX/WLAN UWB-X band high isolation 2 × 2 MIMO antenna for imaging applications. IETE J. Res. 2021, 1–13. [Google Scholar] [CrossRef]
- Sharma, M.; Kumar, R.; Kaur, P.; Dhasarathan, V.; Nguyen, T.K. Design and analysis of on-demand reconfigurable WiMAX/WLAN high isolation 2 × 2 MIMO antenna oriented adjacent/orthogonally for imaging applications in UWB-X band. Int. J. RF Microw. Comput. Aided Eng. 2021, 32, e22928. [Google Scholar] [CrossRef]
- Čuljak, I.; Vasić, L.; Mihaldinec, H.; Džapo, H. Wireless body sensor communication systems based on UWB and IBC technologies: State-of-the-art and open challenges. Sensors 2020, 20, 3587. [Google Scholar] [CrossRef]
- Jhunjhunwala, V.K.; Ali, T.; Kumar, P.; Kumar, P.; Kumar, P.; Shrivastava, S.; Bhagwat, A.A. Flexible UWB and MIMO antennas for wireless body area network: A review. Sensors 2022, 22, 9549. [Google Scholar] [CrossRef]
- Kangeyan, R.; Karthikeyan, M. Miniaturized meander-line dual-band implantable antenna for biotelemetry applications. ETRI J. 2023. [Google Scholar] [CrossRef]
- Salama, S.; Zyoud, D.; Abuelhaija, A. A Compact-Size Multiple-Band Planar Inverted LC Implantable Antenna Used for Biomedical Applications. Micromachines 2023, 14, 1021. [Google Scholar] [CrossRef] [PubMed]
- Ucar, M.H.B.; Uras, E. A Compact Modified Two-Arm Rectangular Spiral Implantable Antenna Design for ISM Band Biosensing Applications. Sensors 2023, 23, 4883. [Google Scholar] [CrossRef] [PubMed]
- Faisal, F.; Zada, M.; Yoo, H.; Mabrouk, I.B.; Chaker, M.; Djerafi, T. An Ultra-Miniaturized Antenna with Ultra-Wide Bandwidth for Future Cardiac Leadless Pacemaker. IEEE Trans. Antennas Propag. 2022, 70, 5923–5928. [Google Scholar] [CrossRef]
- Nösslinger, H.; Mair, E.; Toplak, H.; Hörmann-Wallner, M. Measuring subcutaneous fat thickness using skinfold calipers vs. high-resolution B-scan ultrasonography in healthy volunteers: A pilot study. Clin. Nutr. Open Sci. 2022, 41, 19–32. [Google Scholar] [CrossRef]
- Augustine, R. Electromagnetic Modeling of Human Tissues and Its Application on the Interaction between Antenna and Human Body in the BAN Context. Ph.D. Thesis, Paris-Est University, Créteil, France, 2009. [Google Scholar]
- Feng, Y.; Li, Z.; Qi, L.; Shen, W.; Li, G. A compact and miniaturized implantable antenna for ISM band in wireless cardiac pacemaker system. Sci. Rep. 2022, 12, 238. [Google Scholar] [CrossRef]
- Yoon, Y.; Kim, B. A new formula for effective dielectric constant in multi-dielectric layer microstrip structure. In Proceedings of the IEEE 9th Tropical Meeting on Electrical Performance of Electronic Packaging, Scottsdale, AZ, USA, 23–25 October 2000; IEEE: New York, NY, USA, 2010. [Google Scholar]
- Garg, R.; Bahl, I.; Bozzi, M. Microstrip Lines and Slotlines, 3rd ed.; Archtech House Publication: London, UK, 1996. [Google Scholar]
- Liu, N.-W.; Zhu, L.; Choi, W.-W. A Differential-Fed Microstrip Patch Antenna with Bandwidth Enhancement Under Operation of TM10and TM30Modes. IEEE Trans. Antennas Propag. 2017, 65, 1607–1614. [Google Scholar] [CrossRef]
- Peng, L.; Mao, J.-Y.; Li, X.-F.; Jiang, X.; Ruan, C.-L. Bandwidth enhancement of microstrip antenna loaded by parasitic zeroth-order resonators. Microw. Opt. Technol. Lett. 2017, 59, 1096–1100. [Google Scholar] [CrossRef]
- Khan, Q.U.; Ihsan, M.B. Higher order mode excitation for high gain microstrip patch antenna. AEU Int. J. Electron. Commun. 2014, 68, 1073–1077. [Google Scholar] [CrossRef]







| Refs. | Frequency | Technique | Performance Enhancement Factor | Flexible | Gain | Implant Tissue | Bandwidth |
|---|---|---|---|---|---|---|---|
| [32] 2023 | 1.4, 2.4 GHz | Meandered stack patch | Miniaturization 10 × 10 × 0.635 mm3 | No | −37, −21 | Homogeneous Skin/4 mm | 3.57, 6.37% |
| [33] 2023 | 402.5 MHz, 2.45, 2.95 GHz | Capacitive loading | To achieve multiple bands and miniaturization 20 × 12 × 2.2 mm3 | No | −29.7, −3.1, −7.3 | Three layered tissue, implanted in muscle at 8 mm | 13.98 MHz, 0.3 GHz, 0.62 GHz |
| [34] 2023 | 2.45 GHz | Stacked patch | For gain enhancement | No | −18.41 | Scalp implant | 100 MHz |
| [35] 2022 | 0.79 to 3.83 GHz (UWB) | Shorting pin and defected ground | For bandwidth enhancement | No | −20.22 | Homogeneous skin tissue and heart | 3040 MHz |
| [24] 2023 | 3.0 to 5.0 GHz (UWB) | Defected ground and adding of insulating layer | Gain and bandwidth enhancement | No | −18.6 dBi | Brain implant in Dura layer | 2000 MHz |
| [5] 2022 | 403 MHz | PIFA | Miniaturized 10 × 10 × 1.905 mm3 | No | −18.8 dBi | Three-layered phantom, implant in muscle tissue | 29 MHz |
| [19] 2022 | 2.45 GHz | CPW fed with defected ground | miniaturization (585.55 mm3) | No | −15 dBc | Three-layered phantom, implant in muscle tissue at 4 mm | 1100 MHz |
| This work | 0.86 GHz 1.43 GHz 2.6–6.8 GHz | Patch with parasitic resonator | Multiband structure with wider impedance bandwidth and robust in-body performance | Yes | −26 dBi −14 dBi −16 dBi | Three-layered structure, implant in muscle (rectangle), skin (cylinder) | 120 140 4200 |
| Phntom | Impant Layer | Operating Frequency Range (GHz) | Bandwidth | Resonance Frequency (GHz) | |S11| in dB | Gain (dBi) | Effifiency (%) | SAR (W/kg.) for 10 mW |
|---|---|---|---|---|---|---|---|---|
| 3-Layered rectangular | Muscle | 0.82–0.94 | 120 MHz | 0.83 | −27.66 | −26 | 6.2 | 0.409 |
| 1.39–1.53 | 140 MHz | 1.43 | −35.18 | −14 | 7.97 | 0.534 | ||
| 2.6–6.8 | 4.2 GHz | 3.5 5.5 | −12.56 −25.88 | −16 −14.32 | 6.94 7.15 | 0.529 0.665 | ||
| 3-layered cylindrical | Skin | 0.82–0.942 | 118 MHz | 0.83 | −32.20 | −27 | 5.65 | - |
| 1.41–1.54 | 139 MHz | 1.43 | −17.68 | −24 | 5.9 | - | ||
| 2.45–6.85 | 4.4 GHz | 3.5 5.5 | −29.42 −15.38 | −17.04 −14.48 | 6.71 7.24 | - | ||
| 3-layered cylindrical (antenna in bent state) | Skin | 0.82–0.936 | 116 MHz | 0.83 | −24.66 | −26 | 6.09 | 0.534 |
| 1.38–1.50 | 120 MHz | 1.43 | −18.23 | −23 | 6.28 | 0.653 | ||
| 2.45–5.77 | 3.32 GHz | 3.5 5.5 | −21.52 −21.68 | −16.26 −13.46 | 6.89 7.36 | 0.754 0.755 |
| Ref. | Frequency GHz | Volume (mm3) | Impedance Bandwidth | Gain (dBi) | SAR (W/Kg) for 1 g Tissue with 1 W Power |
|---|---|---|---|---|---|
| [13] | 0.402 (MICS) | 197.04 | 23.13% | −33 | 241 |
| 1.430 (WMTS) | 14.93% | −21.9 | 269 | ||
| 2.450 (ISM) | 18.12% | −19.6 | 290 | ||
| [20] | 0.400 (MICS) | 201.6 | 120 MHz | −35 | 94 |
| 1.450 (ISM) | 320 MHz | −10 | 296 | ||
| 5.780 (Wi-Fi) | 1200 MHz | −16 | 572 | ||
| [14] | 0.915 (ISM) | 21 | 8.7% | −26.4 | 380 |
| 1.900 (MF) | 8.2% | −23 | 388 | ||
| 2.450 (ISM) | 7.3% | −20.47 | 363 | ||
| [21] | 0.433 (MICS) | 255 | 18.94% | −33.76 | 229 |
| 0.915 (ISM) | 17.04% | −16.8 | 264 | ||
| 2.450 (ISM) | 30.96% | −21.2 | 245 | ||
| [22] | 0.402 (MICS) | 405.9 | - | −43.6 | 99.5 |
| 0.902 (ISM) | - | −25.8 | 207.8 | ||
| 2.400 (ISM) | - | −20.1 | 272 | ||
| This work | 0.86 (ISM) | 75 | 120 MHz (181.8%) | −26 | 0.409 (for 10 mW) |
| 1.430 (WMTS) | 140 MHz (9.58%) | −14 | 0.534 (for 10 mW) | ||
| 2.6–6.8 (UWB subset and Wi-Fi) | 4.2 GHz (285.7%) | −16 (3.5 GHz) −14.2 (5.5 GHz) | 0.529 (for 10 mW) 0.665 (for 10 mW) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gupta, A.; Kumar, V.; Bansal, S.; Alsharif, M.H.; Jahid, A.; Cho, H.-S. A Miniaturized Tri-Band Implantable Antenna for ISM/WMTS/Lower UWB/Wi-Fi Frequencies. Sensors 2023, 23, 6989. https://doi.org/10.3390/s23156989
Gupta A, Kumar V, Bansal S, Alsharif MH, Jahid A, Cho H-S. A Miniaturized Tri-Band Implantable Antenna for ISM/WMTS/Lower UWB/Wi-Fi Frequencies. Sensors. 2023; 23(15):6989. https://doi.org/10.3390/s23156989
Chicago/Turabian StyleGupta, Anupma, Vipan Kumar, Shonak Bansal, Mohammed H. Alsharif, Abu Jahid, and Ho-Shin Cho. 2023. "A Miniaturized Tri-Band Implantable Antenna for ISM/WMTS/Lower UWB/Wi-Fi Frequencies" Sensors 23, no. 15: 6989. https://doi.org/10.3390/s23156989
APA StyleGupta, A., Kumar, V., Bansal, S., Alsharif, M. H., Jahid, A., & Cho, H.-S. (2023). A Miniaturized Tri-Band Implantable Antenna for ISM/WMTS/Lower UWB/Wi-Fi Frequencies. Sensors, 23(15), 6989. https://doi.org/10.3390/s23156989











