Robotic Medtronic Hugo™ RAS System Is Now Reality: Introduction to a New Simulation Platform for Training Residents
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
- -
- Sex;
- -
- Age;
- -
- Year of residency (ranging from 1 to 5);
- -
- Hours spent playing video games per day (categorized as 0 h/day, <3 h/day or >3 h/day);
- -
- Previous laparoscopic exposure (categorized based on roles: observer (>50 procedures), assistant or first surgeon);
- -
- Robotic exposure (categorized based on roles: observer (>50 procedures), bed-assistant or console surgeon);
- -
- Interest in robotic surgery (measured on a Likert scale from 0 to 4 points).
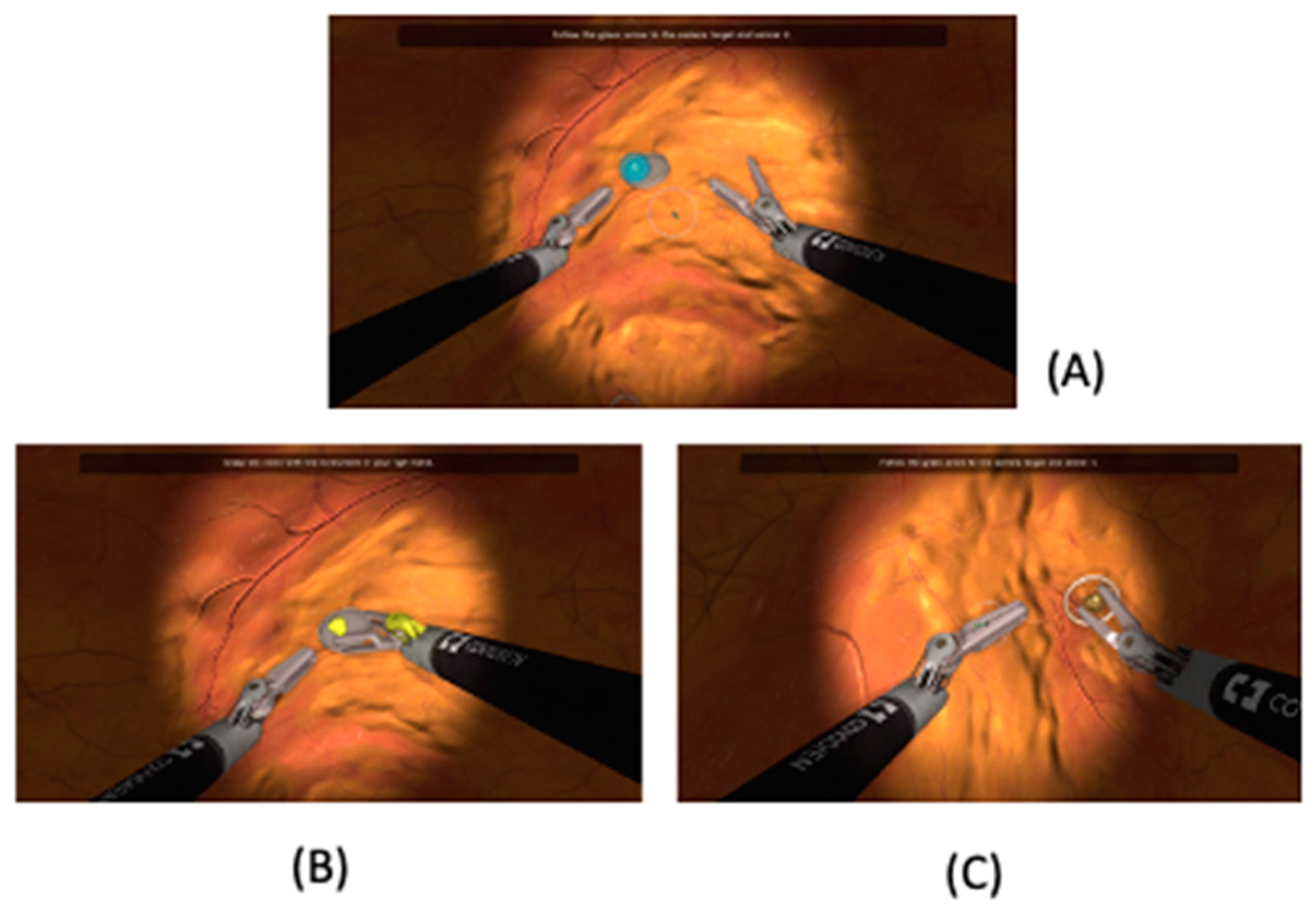
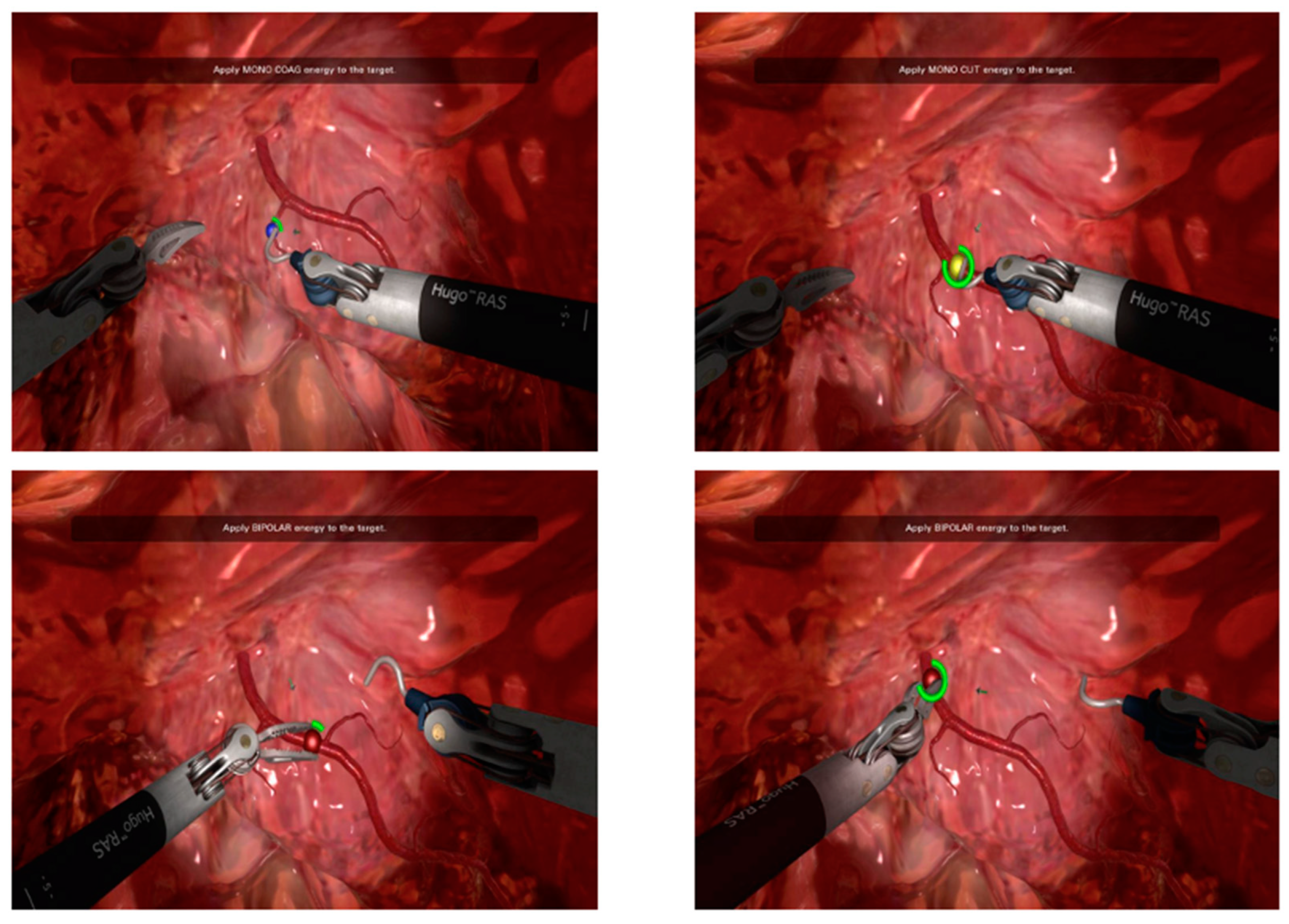
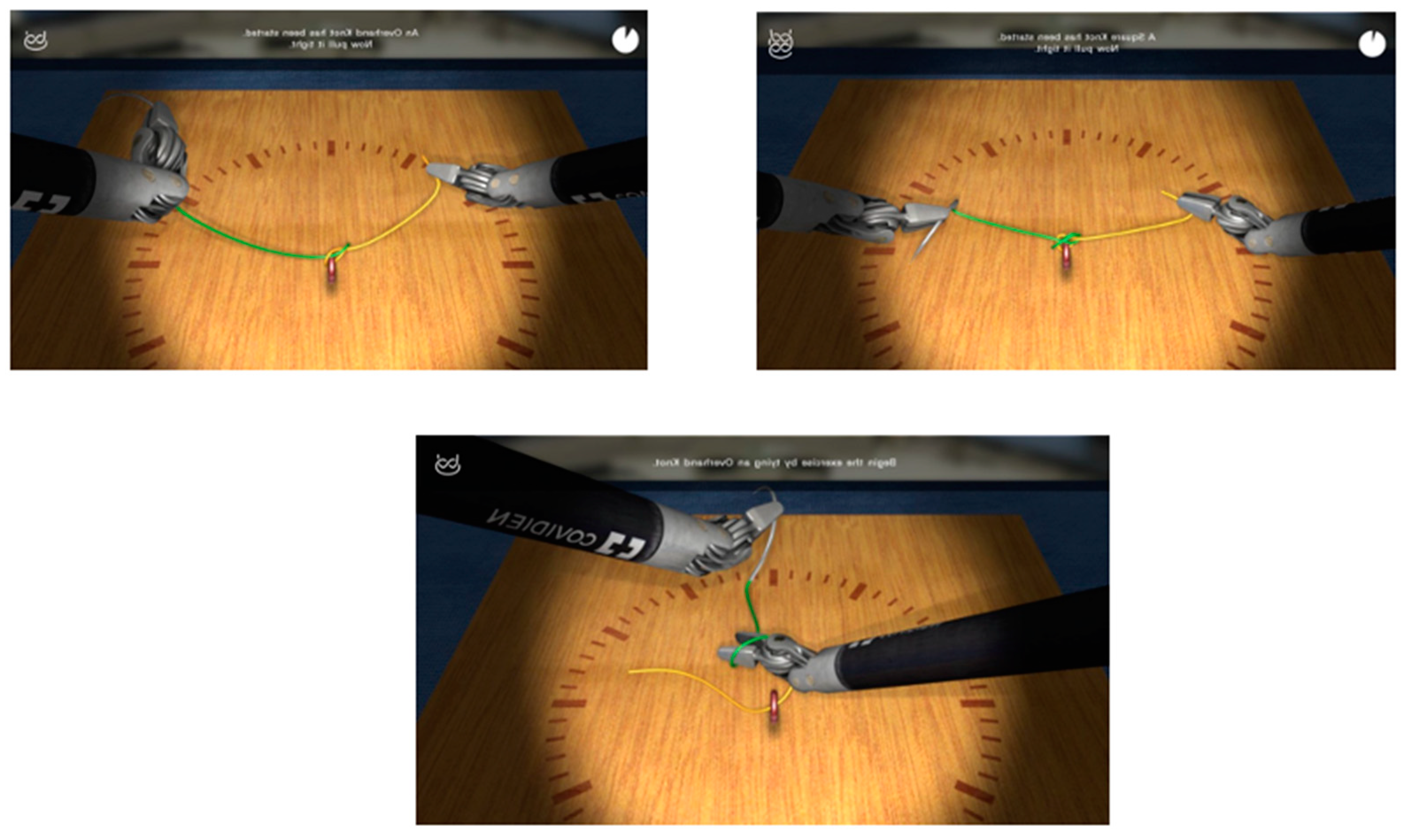
2.2. Training Session
- -
- Timing (parameter A): The time taken by the resident to complete the task.
- -
- Range of motion (parameter B): The extent of movement and control exhibited by the resident while performing the task.
- -
- Panoramic view (parameter C): The ability of the resident to maintain a clear and comprehensive view of the surgical field during the task.
- -
- Conflict of instruments (parameter D): The level of efficiency demonstrated by the resident in managing instrument movements and avoiding conflicts during the task.
- -
- Exercise completed (parameter E): Whether the resident successfully completed the exercise or not in the time chosen by the simulation program.
2.3. Statistical Analysis
3. Results
- -
- In the first exercise, year of residency was the only potential predictor of proficiency for parameter A (OR 1.94; 95% CI [1.12–3.34], p = 0.01) and B (OR 1.68; 95% CI [1.02–2.27], p = 0.04), while for parameter D, male sex was the only predictor of proficiency (OR 0.1; 95% CI [0.02–0.43], p = 0.002).
- -
- In the second exercise, laparoscopic exposure was a potential predictor of proficiency for parameter C (OR 0.41; 95% CI [0.19–0.85], p = 0.01), while interest in robot-assisted surgery was the only predictor of proficiency for parameter E (OR 3.37; 95% CI [1.25–9.07], p = 0.01).
- -
- In the last exercise, interest in robot-assisted surgery was a predictor of proficiency for parameters C (OR 1.80; 95% CI [1.02–3.19], p = 0.04) and E (OR 3.71; 95% CI [1.59–8.62], p = 0.002).
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Esperto, F.; Cacciatore, L.; Tedesco, F.; Testa, A.; Callè, P.; Ragusa, A.; Deanesi, N.; Minore, A.; Prata, F.; Brassetti, A.; et al. Impact of Robotic Technologies on Prostate Cancer Patients’ Choice for Radical Treatment. J. Pers. Med. 2023, 13, 794. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.E.; Kaldany, A.; Lichtbroun, B.; Singer, E.A.; Jang, T.L.; Ghodoussipour, S.; Kim, M.M.; Kim, I.Y. Single-Port Robotic Radical Prostatectomy: Short-Term Outcomes and Learning Curve. J. Endourol. 2022, 36, 1285–1289. [Google Scholar] [CrossRef] [PubMed]
- Esperto, F.; Prata, F.; Antonelli, A.; Alloni, R.; Campanozzi, L.; Cataldo, R.; Civitella, A.; Fiori, C.; Ghilardi, G.; Guglielmelli, E.; et al. Bioethical Implications of Robotic Surgery in Urology: A Systematic Review. Minerva Urol. Nephrol. 2021, 73, 700–710. [Google Scholar] [CrossRef] [PubMed]
- Okrainec, A.; Soper, N.J.; Swanstrom, L.L.; Fried, G.M. Trends and Results of the First 5 Years of Fundamentals of Laparoscopic Surgery (FLS) Certification Testing. Surg. Endosc. 2011, 25, 1192–1198. [Google Scholar] [CrossRef] [PubMed]
- Tom, C.M.; Maciel, J.D.; Korn, A.; Ozao-Choy, J.J.; Hari, D.M.; Neville, A.L.; de Virgilio, C.; Dauphine, C. A Survey of Robotic Surgery Training Curricula in General Surgery Residency Programs: How Close Are We to a Standardized Curriculum? Am. J. Surg. 2019, 217, 256–260. [Google Scholar] [CrossRef]
- Brook, N.R.; Dell’Oglio, P.; Barod, R.; Collins, J.; Mottrie, A. Comprehensive Training in Robotic Surgery. Curr. Opin. Urol. 2019, 29, 1–9. [Google Scholar] [CrossRef]
- Zhao, B.; Lam, J.; Hollandsworth, H.M.; Lee, A.M.; Lopez, N.E.; Abbadessa, B.; Eisenstein, S.; Cosman, B.C.; Ramamoorthy, S.L.; Parry, L.A. General Surgery Training in the Era of Robotic Surgery: A Qualitative Analysis of Perceptions from Resident and Attending Surgeons. Surg. Endosc. 2020, 34, 1712–1721. [Google Scholar] [CrossRef]
- Carrion, D.M.; Rodriguez-Socarrás, M.E.; Mantica, G.; Esperto, F.; Cebulla, A.; Duijvesz, D.; Patruno, G.; Vásquez, J.L.; Veneziano, D.; Díez-Sebastian, J.; et al. Current Status of Urology Surgical Training in Europe: An ESRU-ESU-ESUT Collaborative Study. World J. Urol. 2020, 38, 239–246. [Google Scholar] [CrossRef]
- Chen, R.; Rodrigues Armijo, P.; Krause, C.; SAGES Robotic Task Force; Siu, K.-C.; Oleynikov, D. A Comprehensive Review of Robotic Surgery Curriculum and Training for Residents, Fellows, and Postgraduate Surgical Education. Surg. Endosc. 2020, 34, 361–367. [Google Scholar] [CrossRef]
- Chowriappa, A.J.; Shi, Y.; Raza, S.J.; Ahmed, K.; Stegemann, A.; Wilding, G.; Kaouk, J.; Peabody, J.O.; Menon, M.; Hassett, J.M.; et al. Development and Validation of a Composite Scoring System for Robot-Assisted Surgical Training—The Robotic Skills Assessment Score. J. Surg. Res. 2013, 185, 561–569. [Google Scholar] [CrossRef]
- Liss, M.A.; Abdelshehid, C.; Quach, S.; Lusch, A.; Graversen, J.; Landman, J.; McDougall, E.M. Validation, Correlation, and Comparison of the Da Vinci Trainer™ and the Da Vinci Surgical Skills Simulator™ Using the Mimic™ Software for Urologic Robotic Surgical Education. J. Endourol. 2012, 26, 1629–1634. [Google Scholar] [CrossRef]
- Butterworth, J.; Sadry, M.; Julian, D.; Haig, F. Assessment of the Training Program for Versius, a New Innovative Robotic System for Use in Minimal Access Surgery. BMJ Surg. Interv. Health Technol. 2021, 3, e000057. [Google Scholar] [CrossRef] [PubMed]
- Alip, S.L.; Kim, J.; Rha, K.H.; Han, W.K. Future Platforms of Robotic Surgery. Urol. Clin. N. Am. 2022, 49, 23–38. [Google Scholar] [CrossRef] [PubMed]
- Peters, B.S.; Armijo, P.R.; Krause, C.; Choudhury, S.A.; Oleynikov, D. Review of Emerging Surgical Robotic Technology. Surg. Endosc. 2018, 32, 1636–1655. [Google Scholar] [CrossRef] [PubMed]
- Silberstein, J.L.; Maddox, M.M.; Dorsey, P.; Feibus, A.; Thomas, R.; Lee, B.R. Physical Models of Renal Malignancies Using Standard Cross-Sectional Imaging and 3-Dimensional Printers: A Pilot Study. Urology 2014, 84, 268–272. [Google Scholar] [CrossRef]
- Carey, J.N.; Minneti, M.; Leland, H.A.; Demetriades, D.; Talving, P. Perfused Fresh Cadavers: Method for Application to Surgical Simulation. Am. J. Surg. 2015, 210, 179–187. [Google Scholar] [CrossRef]
- Costello, D.M.; Huntington, I.; Burke, G.; Farrugia, B.; O’Connor, A.J.; Costello, A.J.; Thomas, B.C.; Dundee, P.; Ghazi, A.; Corcoran, N. A Review of Simulation Training and New 3D Computer-Generated Synthetic Organs for Robotic Surgery Education. J. Robot. Surg. 2022, 16, 749–763. [Google Scholar] [CrossRef]
- Julian, D.; Tanaka, A.; Mattingly, P.; Truong, M.; Perez, M.; Smith, R. A Comparative Analysis and Guide to Virtual Reality Robotic Surgical Simulators. Int. J. Med. Robot. 2018, 14, e1874. [Google Scholar] [CrossRef]
- Goh, A.C.; Goldfarb, D.W.; Sander, J.C.; Miles, B.J.; Dunkin, B.J. Global Evaluative Assessment of Robotic Skills: Validation of a Clinical Assessment Tool to Measure Robotic Surgical Skills. J. Urol. 2012, 187, 247–252. [Google Scholar] [CrossRef]
- Soputro, N.A.; Olivares, R. Current Urological Applications of the Hugo™ RAS System. World J. Urol. 2023. [Google Scholar] [CrossRef]
- Ragavan, N.; Bharathkumar, S.; Chirravur, P.; Sankaran, S.; Mottrie, A. Evaluation of Hugo RAS System in Major Urologic Surgery: Our Initial Experience. J. Endourol. 2022, 36, 1029–1035. [Google Scholar] [CrossRef] [PubMed]
- Raffaelli, M.; Voloudakis, N.; Pennestrì, F.; Gallucci, P.; Modesti, C.; Salvi, G.; Greco, F.; Ciccoritti, L. Feasibility of Roux-En-Y Gastric Bypass with the Novel Robotic Platform HUGO™ RAS. Front. Surg. 2023, 10, 1181790. [Google Scholar] [CrossRef] [PubMed]
- Panico, G.; Campagna, G.; Caramazza, D.; Vacca, L.; Mastrovito, S.; Ercoli, A.; Scambia, G. HUGO(TM) RAS System in Urogynaecology: The First Nerve Sparing Sacral Colpopexy for Pelvic Organ Prolapse. Facts Views Vis. Obgyn 2023, 15, 83–87. [Google Scholar] [CrossRef] [PubMed]
- Vicente, E.; Quijano, Y.; Ferri, V.; Caruso, R. Robot-Assisted Cholecystectomy with the New HUGO™ Robotic-Assisted System: First Worldwide Report with System Description, Docking Settings, and Video. Updates Surg. 2023. [Google Scholar] [CrossRef]
- Gallioli, A.; Uleri, A.; Gaya, J.M.; Territo, A.; Aumatell, J.; Verri, P.; Basile, G.; Fontanet, S.; Tedde, A.; Diana, P.; et al. Initial Experience of Robot-Assisted Partial Nephrectomy with Hugo™ RAS System: Implications for Surgical Setting. World J. Urol. 2023, 41, 1085–1091. [Google Scholar] [CrossRef]
- Mottaran, A.; Bravi, C.A.; Sarchi, L.; Paciotti, M.; Nocera, L.; Piro, A.; Piazza, P.; De Backer, P.; Farinha, R.; De Groote, R.; et al. Robot-Assisted Sacropexy with the Novel HUGO Robot-Assisted Surgery System: Initial Experience and Surgical Setup at a Tertiary Referral Robotic Center. J. Endourol. 2023, 37, 35–41. [Google Scholar] [CrossRef]
- Mottaran, A.; Paciotti, M.; Bravi, C.A.; Sarchi, L.; Nocera, L.; Piro, A.; Farinha, R.; DE Backer, P.; Piazza, P.; Pauwaert, K.; et al. Robot-Assisted Simple Prostatectomy with the Novel HUGO™ RAS System: Feasibility, Setting, and Perioperative Outcomes. Minerva Urol. Nephrol. 2022, 75, 235–239. [Google Scholar] [CrossRef]
- Gueli Alletti, S.; Chiantera, V.; Arcuri, G.; Gioè, A.; Oliva, R.; Monterossi, G.; Fanfani, F.; Fagotti, A.; Scambia, G. Introducing the New Surgical Robot HUGO™ RAS: System Description and Docking Settings for Gynecological Surgery. Front. Oncol. 2022, 12, 898060. [Google Scholar] [CrossRef]
- Dubin, A.K.; Smith, R.; Julian, D.; Tanaka, A.; Mattingly, P. A Comparison of Robotic Simulation Performance on Basic Virtual Reality Skills: Simulator Subjective Versus Objective Assessment Tools. J. Minim. Invasive Gynecol. 2017, 24, 1184–1189. [Google Scholar] [CrossRef]
- Sheth, S.S.; Fader, A.N.; Tergas, A.I.; Kushnir, C.L.; Green, I.C. Virtual Reality Robotic Surgical Simulation: An Analysis of Gynecology Trainees. J. Surg. Educ. 2014, 71, 125–132. [Google Scholar] [CrossRef]
- Mikhail, A.; Connor, A.A.; Ahmed, N. Impact of Research Training on Performance in General Surgery Residency. J. Surg. Educ. 2022, 79, 342–348. [Google Scholar] [CrossRef] [PubMed]
- Sighinolfi, M.C.; Terzoni, S.; Scanferla, E.; Bianchi, P.P.; Formisano, G.; Gaia, G.; Marconi, A.M.; Chiumello, D.; Patel, V.; Moschovas, M.C.; et al. Impact of Hands-on Practice with HugoRAS and Versius System Simulators on the Attractiveness of Robotic Surgery among Medical and Nurse Undergraduate Students. J. Robot. Surg. 2023, 17, 1471–1476. [Google Scholar] [CrossRef] [PubMed]

| Pre-Training Data | Median or N (IQR or %) |
|---|---|
| Age (years) | 28.5 (28–30) |
| Gender | |
| F | 16 (36.4%) |
| M | 28 (63.6%) |
| Specialty | |
| General surgery | 12 (27.3%) |
| Gynaecology | 8 (18.2%) |
| Urology | 24 (54.5%) |
| Year of residency | |
| 1 | 16 (36.4%) |
| 2 | 16 (36.4%) |
| 3 | 2 (4.5%) |
| 4 | 4 (9.1%) |
| 5 | 6 (13.6%) |
| Time spent playing video games (hours/day) | |
| 0 | 18 (40.9%) |
| <3 | 26 (59.1%) |
| >3 | 0 |
| Laparoscopic exposure | |
| No exposure | 14 (31.8%) |
| Observer > 50 procedures/assistant surgeon/first surgeon | 30 (68.2%) |
| Robotic exposure | |
| No exposure | 44 (100%) |
| Observer > 50 procedures/bed assistant/console surgeon | |
| Interest in robotic surgery | 0 |
| Interest in robotic surgery | |
| 0 | 4 (9.1%) |
| 1 | 2 (4.5%) |
| 2 | 12 (27.3%) |
| 3 | 14 (31.8%) |
| 4 | 12 (27.3%) |
| Hugo RAS™ System Simulator Parameters (Score from 0 to 200) | Endoscope Targeting (1st Exercise) | Cut and Coagulation (2nd Exercise) | Suturing Skills (3rd Exercise) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| First Attempt | Last Attempt | p * | First Attempt | Last Attempt | p * | First Attempt | Last Attempt | p * | |
| Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | ||||
| Timing (A) | 66 | 101.5 | <0.001 | 93 | 133 | 0.001 | 0 | 13.5 | 0.001 |
| (23–87) | (85–115) | (85–120) | (118–144) | (0–50) | |||||
| Range of motion (B) | 70.5 | 112.5 | <0.001 | 149.5 | 168.5 | 0.001 | 10 | 88.5 | 0.001 |
| (53–99) | (91–122) | (126–162) | (162–180) | (0–79) | (21–110) | ||||
| Panoramic view (C) | 133 | 200 | <0.001 | 100 | 200 | 0.001 | 150 | 200 | 0.10 |
| (63–167) | (170–200) | (100–200) | (200–200) | (100–200) | (150–200) | ||||
| Conflict of instruments (D) | 196 | 200 | 0.001 | 200 | 200 | 0.41 | 97.5 | 189.5 | <0.001 |
| (190–200) | (199–200) | (200–200) | (200–200) | (38–182) | (85–200) | ||||
| Exercise completed (E) | 198 | 200 | <0.001 | 200 | 200 | 0.02 | 200 | 200 | 0.41 |
| (187–200) | (199–200) | (139–200) | (200–200) | (103–200) | (132–200) | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cacciatore, L.; Costantini, M.; Tedesco, F.; Prata, F.; Machiella, F.; Iannuzzi, A.; Ragusa, A.; Deanesi, N.; Qaddourah, Y.R.; Brassetti, A.; et al. Robotic Medtronic Hugo™ RAS System Is Now Reality: Introduction to a New Simulation Platform for Training Residents. Sensors 2023, 23, 7348. https://doi.org/10.3390/s23177348
Cacciatore L, Costantini M, Tedesco F, Prata F, Machiella F, Iannuzzi A, Ragusa A, Deanesi N, Qaddourah YR, Brassetti A, et al. Robotic Medtronic Hugo™ RAS System Is Now Reality: Introduction to a New Simulation Platform for Training Residents. Sensors. 2023; 23(17):7348. https://doi.org/10.3390/s23177348
Chicago/Turabian StyleCacciatore, Loris, Manuela Costantini, Francesco Tedesco, Francesco Prata, Fabio Machiella, Andrea Iannuzzi, Alberto Ragusa, Noemi Deanesi, Yussef Rashed Qaddourah, Aldo Brassetti, and et al. 2023. "Robotic Medtronic Hugo™ RAS System Is Now Reality: Introduction to a New Simulation Platform for Training Residents" Sensors 23, no. 17: 7348. https://doi.org/10.3390/s23177348





