A Scoping Review of the Validity and Reliability of Smartphone Accelerometers When Collecting Kinematic Gait Data
Abstract
:1. Introduction
2. Methods
2.1. Protocol
2.2. Eligibility Criteria
2.3. Information Sources
2.4. Search
2.5. Selection of Sources of Evidence
2.6. Data Charting
2.7. Data Items
2.8. Synthesis of Results
3. Results
3.1. Study Selection
3.2. Study Characteristics
3.3. Results of Individual Sources of Evidence
3.4. Synthesis of Results
3.4.1. Equipment
3.4.2. Capture Frequency
3.4.3. Location of Markers and Phone
3.4.4. Walking Protocols
3.4.5. Analysis
| Study | Filtered | Resampled | Sample Size Calculation | Gait Characteristics | Determination of Characteristic | Reliability/Validity Measure |
|---|---|---|---|---|---|---|
| Di Bacco et al. (2023) [17] | For linear analysis only | Y | Y | Stride time DFA Entropy | As [46] | ICC B/A |
| Olson et al. (2023) [18] | N | N | Y | Step length Step time Periodicity | As [23] | ICC B/A |
| Grouios et al. (2022) [19] | N | N | N | Raw acceleration | N/A | ICC Pearson |
| Christensen et al. (2022) [20] | N | N | Y | Stance time Step length Cadence Stride length Swing time | Identified by researcher | ICC B/A |
| Kelly et al. (2022) [21] | Y | Y | N | Cadence | Positive peaks from the AP direction were identified as heel strikes | Pearson |
| Shema-Shiratzky et al., 2022) [22] | N | N | N | Step length Cadence Single/double support % | PearsonB/A | |
| Rashid et al. (2021) [23] | N | N | N | Step length Step time Periodicity | A wavelet-based step-event detection algorithm and a double-pendulum gait model | ICC B/A Pearson |
| Shahar et al. (2021) [24] | N | N | Y | Cadence Step length Gait stance phase % Swing phase % | Not stated | ICC B/A |
| Alberto et al. (2021) [25] | Y | Y | N | Stride duration Stance phase duration Stride length Cadence | As [46] | B/A |
| Lugade et al. (2021) [26] | Y | N | Y | Step time Cadence | Video-based concurrently with accelerometer capture | B/A Pearson |
| Su et al. (2021) [27] | Y | N | N | Stride time Stride time variability | As [46] | Pearson |
| Silsupadol et al. (2020) [29] | Y | N | N | Step time Step length Cadence | Positive peaks in the filtered AP direction were identified as heel strikes | B/A Pearson |
| Howell et al. (2020) [30] | Y | N | N | Stride length Cadence | Positive peaks in the filtered AP direction were identified as heel strikes | ICC Pearson |
| Kuntapun et al. (2020) [28] | Y | N | N | Step time Step length Cadence COM displacement | Positive peaks in the filtered AP direction were identified as heel strikes COM identified via double integration of the acceleration time series | Pearson B/A |
| Tchelet et al. (2019) [31] | N | Y | N | Step length Cadence | B/A | |
| Silsupadol et al. (2017) [32] | Y | Y | N | Step length Step time Cadence | Positive peaks in the filtered AP direction were identified as heel strikes | ICC B/A |
| Pepa et al. (2017) [33] | N | N | Y | Step period Step length | Various algorithms to identify heel strike compared | B/A Pearson |
| Ellis et al. (2015) [34] | N | Y | Y | Step time Step length | Peaks in AP signal | ANOVA and effect sizes |
| Furrer et al. (2015) [35] | Y | N | N | Step length. COM displacement. | Double integration of accelerations | B/A Pearson |
| Steins et al. (2014) [36] | Y | Y | N | COM position. COM acceleration. | Integration of acceleration | ICC B/A |
| Nishiguchi et al. (2012) [37] | Y | Y | N | Peak frequency | Peak frequency calculated from smoothed acceleration data | Pearson |
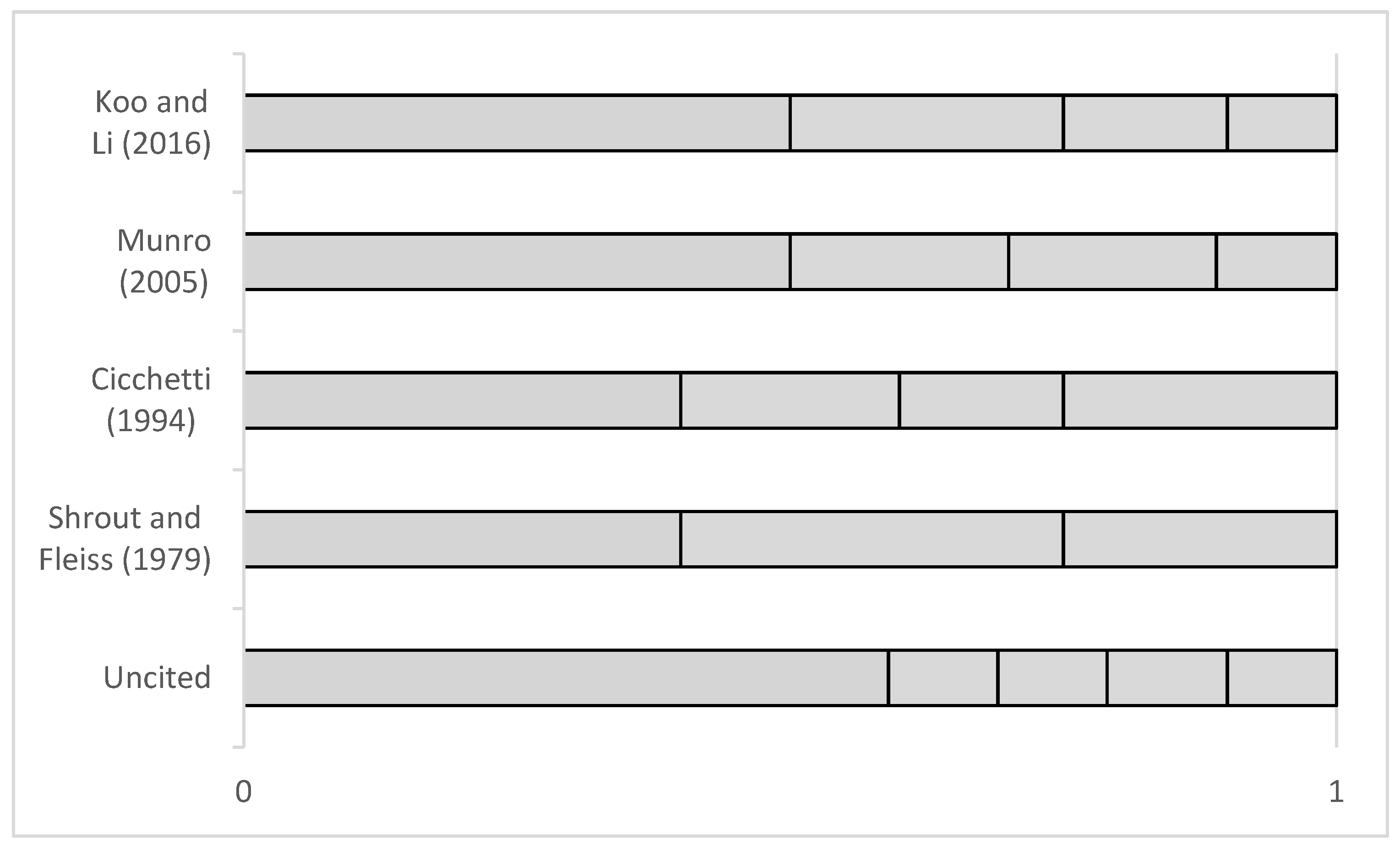
3.4.6. Findings
4. Discussion
4.1. Summary of Evidence
4.1.1. Ecological Validity
4.1.2. Analysis
4.2. Limitations
5. Conclusions
Recommendations for Future Research
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A

References
- Weygers, I.; Kok, M.; Konings, M.; Hallez, H.; De Vroey, H.; Claeys, K. Inertial Sensor-Based Lower Limb Joint Kinematics: A Methodological Systematic Review. Sensors 2020, 20, 673. [Google Scholar] [CrossRef] [PubMed]
- Kobsar, D.; Charlton, J.M.; Tse, C.T.; Esculier, J.F.; Graffos, A.; Krowchuk, N.M.; Thatcher, D.; Hunt, M.A. Validity and reliability of wearable inertial sensors in healthy adult walking: A systematic review and meta-analysis. J. Neuroeng. Rehabil. 2020, 17, 62. [Google Scholar] [CrossRef] [PubMed]
- Benson, L.C.; Clermont, C.A.; Bošnjak, E.; Ferber, R. The use of wearable devices for walking and running gait analysis outside of the lab: A systematic review. Gait Posture 2018, 63, 124–138. [Google Scholar] [CrossRef] [PubMed]
- Mathunny, J.J.; Karthik, V.; Devaraj, A.; Jacob, J. A scoping review on recent trends in wearable sensors to analyze gait in people with stroke: From sensor placement to validation against gold-standard equipment. Proc. Inst. Mech. Eng. H 2023, 237, 309–326. [Google Scholar] [CrossRef]
- Peters, J.; Abou, L.; Wong, E.; Senan Dossou, M.; Sosnoff, J.J.; Rice, L.A. Smartphone-based gait and balance assessment in survivors of stroke: A systematic review. Disabil. Rehabil. Assist. Technol. 2022. [CrossRef] [PubMed]
- Abou, L.; Peters, J.; Wong, E.; Akers, R.; Dossou, M.S.; Sosnoff, J.J.; Rice, L.A. Gait and Balance Assessments using Smartphone Applications in Parkinson’s Disease: A Systematic Review. J. Med. Syst. 2021, 45, 87. [Google Scholar] [CrossRef] [PubMed]
- Abou, L.; Wong, E.; Peters, J.; Dossou, M.S.; Sosnoff, J.J.; Rice, L.A. Smartphone applications to assess gait and postural control in people with multiple sclerosis: A systematic review. Mult. Scler. Relat. Disord. 2021, 51, 102943. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–42. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K. Scoping studies: Advancing the methodology. Implement Sci. 2010, 5, 69. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.D.J.; Godfrey, C.; McInerney, P.; Khalil, H.; Larsen, P.; Marnie, C.; Pollock, D.; Tricco, A.C.; Munn, Z. Best Practice Guidance and Reporting Items for the Development of Scoping Review Protocols. JBI Evid. Synth. 2022, 20, 953–968. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Strongman, C.; Morrison, A. A scoping review of non-linear analysis approaches measuring variability in gait due to lower body injury or dysfunction. Hum. Mov. Sci. 2020, 69, 102562. [Google Scholar] [CrossRef] [PubMed]
- Littell, J.; Corcoran, J.; Pillai, V. Systematic Reviews and Meta-Analysis; Oxford University Press: Oxford, UK, 2008. [Google Scholar]
- Munn, Z.; Peters, M.D.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Di Bacco, V.E.; Gage, W.H. Evaluation of a smartphone accelerometer system for measuring nonlinear dynamics during treadmill walking: Concurrent validity and test-retest reliability. J. Biomech. 2023, 151, 111527. [Google Scholar] [CrossRef]
- Olsen, S.; Rashid, U.; Allerby, C.; Brown, E.; Leyser, M.; McDonnell, G.; Alder, G.; Barbado, D.; Shaikh, N.; Lord, S.; et al. Smartphone-based gait and balance accelerometry is sensitive to age and correlates with clinical and kinematic data. Gait Posture 2023, 100, 57–64. [Google Scholar] [CrossRef]
- Grouios, G.; Ziagkas, E.; Loukovitis, A.; Chatzinikolaou, K.; Koidou, E. Accelerometers in Our Pocket: Does Smartphone Accelerometer Technology Provide Accurate Data? Sensors 2022, 23, 192. [Google Scholar] [CrossRef]
- Christensen, J.C.; Stanley, E.C.; Oro, E.G.; Carlson, H.B.; Naveh, Y.Y.; Shalita, R.; Teitz, L.S. The validity and reliability of the OneStep smartphone application under various gait conditions in healthy adults with feasibility in clinical practice. J. Orthop. Surg. Res. 2022, 17, 417. [Google Scholar] [CrossRef] [PubMed]
- Kelly, M.; Jones, P.; Wuebbles, R.; Lugade, V.; Cipriani, D.; Murray, N.G. A novel smartphone application is reliable for repeat administration and comparable to the Tekscan Strideway for spatiotemporal gait. Measurement 2022, 192, 110882. [Google Scholar] [CrossRef]
- Shema-Shiratzky, S.; Beer, Y.; Mor, A.; Elbaz, A. Smartphone-based inertial sensors technology—Validation of a new application to measure spatiotemporal gait metrics. Gait Posture 2022, 93, 102–106. [Google Scholar] [CrossRef]
- Rashid, U.; Barbado, D.; Olsen, S.; Alder, G.; Elvira, J.L.L.; Lord, S.; Niazi, I.K.; Taylor, D. Validity and Reliability of a Smartphone App for Gait and Balance Assessment. Sensors 2021, 22, 124. [Google Scholar] [CrossRef] [PubMed]
- Shahar, R.T.; Agmon, M. Gait Analysis Using Accelerometry Data from a Single Smartphone: Agreement and Consistency between a Smartphone Application and Gold-Standard Gait Analysis System. Sensors 2021, 21, 7497. [Google Scholar] [CrossRef]
- Alberto, S.; Cabral, S.; Proença, J.; Pona-Ferreira, F.; Leitão, M.; Bouça-Machado, R.; Kauppila, L.A.; Veloso, A.P.; Costa, R.M.; Ferreira, J.J.; et al. Validation of quantitative gait analysis systems for Parkinson’s disease for use in supervised and unsupervised environments. BMC Neurol. 2021, 21, 331. [Google Scholar] [CrossRef]
- Lugade, V.; Kuntapun, J.; Prupetkaew, P.; Boripuntakul, S.; Verner, E.; Silsupadol, P. Three-Day Remote Monitoring of Gait Among Young and Older Adults Using Participants’ Personal Smartphones. J. Aging Phys. Act. 2021, 29, 1026–1033. [Google Scholar] [CrossRef] [PubMed]
- Su, D.; Liu, Z.; Jiang, X.; Zhang, F.; Yu, W.; Ma, H.; Wang, C.; Wang, Z.; Wang, X.; Hu, W.; et al. Simple Smartphone-Based Assessment of Gait Characteristics in Parkinson Disease: Validation Study. JMIR mHealth uHealth 2021, 9, e25451. [Google Scholar] [CrossRef]
- Kuntapun, J.; Silsupadol, P.; Kamnardsiri, T.; Lugade, V. Smartphone Monitoring of Gait and Balance During Irregular Surface Walking and Obstacle Crossing. Front. Sports Act. Living 2020, 2, 560577. [Google Scholar] [CrossRef] [PubMed]
- Silsupadol, P.; Prupetkaew, P.; Kamnardsiri, T.; Lugade, V. Smartphone-Based Assessment of Gait During Straight Walking, Turning, and Walking Speed Modulation in Laboratory and Free-Living Environments. IEEE J. Biomed. Health Inform. 2020, 24, 1188–1195. [Google Scholar] [CrossRef]
- Howell, D.R.; Lugade, V.; Taksir, M.; Meehan, W.P., 3rd. Determining the utility of a smartphone-based gait evaluation for possible use in concussion management. Phys. Sportsmed. 2020, 48, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Tchelet, K.; Stark-Inbar, A.; Yekutieli, Z. Pilot Study of the EncephaLog Smartphone Application for Gait Analysis. Sensors 2019, 19, 5179. [Google Scholar] [CrossRef] [PubMed]
- Silsupadol, P.; Teja, K.; Lugade, V. Reliability and validity of a smartphone-based assessment of gait parameters across walking speed and smartphone locations: Body, bag, belt, hand, and pocket. Gait Posture 2017, 58, 516–522. [Google Scholar] [CrossRef]
- Pepa, L.; Verdini, F.; Spalazzi, L. Gait parameter and event estimation using smartphones. Gait Posture 2017, 57, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Ellis, R.J.; Ng, Y.S.; Zhu, S.; Tan, D.M.; Anderson, B.; Schlaug, G.; Wang, Y. A Validated Smartphone-Based Assessment of Gait and Gait Variability in Parkinson’s Disease. PLoS ONE 2015, 10, e0141694. [Google Scholar] [CrossRef]
- Furrer, M.; Bichsel, L.; Niederer, M.; Baur, H.; Schmid, S. Validation of a smartphone-based measurement tool for the quantification of level walking. Gait Posture 2015, 42, 289–294. [Google Scholar] [CrossRef] [PubMed]
- Steins, D.; Sheret, I.; Dawes, H.; Esser, P.; Collett, J. A smart device inertial-sensing method for gait analysis. J. Biomech. 2014, 47, 3780–3785. [Google Scholar] [CrossRef]
- Nishiguchi, S.; Yamada, M.; Nagai, K.; Mori, S.; Kajiwara, Y.; Sonoda, T.; Yoshimura, K.; Yoshitomi, H.; Ito, H.; Okamoto, K.; et al. Reliability and validity of gait analysis by android-based smartphone. Telemed. J. E Health 2012, 18, 292–296. [Google Scholar] [CrossRef] [PubMed]
- Suner-keklik, S.; Çobanoğlu, G.; Ecemiş, Z.B.; Atalay Güzel, N. Gender Differences in Gait Parameters of Healthy Adult Individuals. J. Basic Clin. Health Sci. 2023, 7, 277–283. [Google Scholar] [CrossRef]
- Dionisio, V.C.; Faria, M.N.; Soares, F.d.S.; Moreira, V.M.P.S.; Furtado, D.A.; Pereira, A.A.; Jafarnezhad, A. Clinical measures and gait parameters in individuals with knee Osteoarthritis: A comparison between men and women. Obs. Econ. Latinoam. 2023, 21, 5284–5299. [Google Scholar] [CrossRef]
- Monfrini, R.; Rossetto, G.; Scalona, E.; Galli, M.; Cimolin, V.; Lopomo, N.F. Technological Solutions for Human Movement Analysis in Obese Subjects: A Systematic Review. Sensors 2023, 23, 3175. [Google Scholar] [CrossRef]
- Android Developers. Sensor Manager. 2023. Available online: developer.android.com/reference/android/hardware/SensorManager (accessed on 10 October 2023).
- Kavanagh, J.J.; Menz, H.B. Accelerometry: A technique for quantifying movement patterns during walking. Gait Posture 2008, 28, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Phinyomark, A.; Larracy, R.; Scheme, E. Fractal Analysis of Human Gait Variability via Stride Time Interval Time Series. Front. Physiol. 2020, 11, 333. [Google Scholar] [CrossRef] [PubMed]
- Yentes, J. Entropy. In Nonlinear Analysis for Human Movement Variability; Stergiou, N., Ed.; CRC Press: Boca Raton, FL, USA, 2016. [Google Scholar]
- Bujang, M.A.; Baharum, N. A simplified guide to determination of sample size requirements for estimating the value of intraclass correlation coefficient: A review. Arch. Orofac. Sci. 2017, 12, 1–11. [Google Scholar]
- Manor, B.; Yu, W.; Zhu, H.; Harrison, R.; Lo, O.Y.; Lipsitz, L.; Travison, T.; Pascual-Leone, A.; Zhou, J. Smartphone App-Based Assessment of Gait During Normal and Dual-Task Walking: Demonstration of Validity and Reliability. JMIR mHealth uHealth 2018, 6, e36. [Google Scholar] [CrossRef]
- Zijlstra, W.; Hof, A.L. Assessment of spatio-temporal gait parameters from trunk accelerations during human walking. Gait Posture 2003, 18, 1–10. [Google Scholar] [CrossRef]
- Munro, B. Statistical Methods for Health Care Research; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2005; Volume 1. [Google Scholar]
- Cicchetti, D.V. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol. Assess. 1994, 6, 284. [Google Scholar] [CrossRef]
- Shrout, P.E.; Fleiss, J.L. Intraclass correlations: Uses in assessing rater reliability. Psychol. Bull. 1979, 86, 420–428. [Google Scholar] [CrossRef] [PubMed]
- Myers, S. Time series. In Nonlinear Analysis for Human Movement Variability; Stergiou, N., Ed.; CRC Press: Boca Raton, FL, USA, 2016. [Google Scholar]
- Ghaffari, A.; Rahbek, O.; Lauritsen, R.E.K.; Kappel, A.; Kold, S.; Rasmussen, J. Criterion Validity of Linear Accelerations Measured with Low-Sampling-Frequency Accelerometers during Overground Walking in Elderly Patients with Knee Osteoarthritis. Sensors 2022, 22, 5289. [Google Scholar] [CrossRef] [PubMed]
- Plotnik, M.; Azrad, T.; Bondi, M.; Bahat, Y.; Gimmon, Y.; Zeilig, G.; Inzelberg, R.; Siev-Ner, I. Self-selected gait speed—Over ground versus self-paced treadmill walking, a solution for a paradox. J. Neuroeng. Rehabil. 2015, 12, 20. [Google Scholar] [CrossRef] [PubMed]
- Brinkerhoff, S.A.; Murrah, W.M.; Hutchison, Z.; Miller, M.; Roper, J.A. Words matter: Instructions dictate “self-selected” walking speed in young adults. Gait Posture 2022, 95, 223–226. [Google Scholar] [CrossRef]
- Redmayne, M. Where’s Your Phone? A Survey of Where Women Aged 15-40 Carry Their Smartphone and Related Risk Perception: A Survey and Pilot Study. PLoS ONE 2017, 12, e0167996. [Google Scholar]
- Glaister, B.C.; Bernatz, G.C.; Klute, G.K.; Orendurff, M.S. Video task analysis of turning during activities of daily living. Gait Posture 2007, 25, 289–294. [Google Scholar] [CrossRef]
- Ulrich, B.; Santos, A.N.; Jolles, B.M.; Benninger, D.H.; Favre, J. Gait events during turning can be detected using kinematic features originally proposed for the analysis of straight-line walking. J. Biomech. 2019, 91, 69–78. [Google Scholar] [CrossRef] [PubMed]
- Spildooren, J.; Vinken, C.; Van Baekel, L.; Nieuwboer, A. Turning problems and freezing of gait in Parkinson’s disease: A systematic review and meta-analysis. Disabil. Rehabil. 2019, 41, 2994–3004. [Google Scholar] [CrossRef] [PubMed]
- Leach, J.M.; Mellone, S.; Palumbo, P.; Bandinelli, S.; Chiari, L. Natural turn measures predict recurrent falls in community-dwelling older adults: A longitudinal cohort study. Sci. Rep. 2018, 8, 4316. [Google Scholar] [CrossRef] [PubMed]
- Moher, D. Reporting guidelines: Doing better for readers. BMC Med. 2018, 16, 233. [Google Scholar] [CrossRef]
- Chen, G.; Taylor, P.A.; Haller, S.P.; Kircanski, K.; Stoddard, J.; Pine, D.S.; Leibenluft, E.; Brotman, M.A.; Cox, R.W. Intraclass correlation: Improved modeling approaches and applications for neuroimaging. Hum. Brain Mapp. 2018, 39, 1187–1206. [Google Scholar] [CrossRef]
- Bunce, C. Correlation, agreement, and Bland-Altman analysis: Statistical analysis of method comparison studies. Am. J. Ophthalmol. 2009, 148, 4–6. [Google Scholar] [CrossRef] [PubMed]
- von Klinggraeff, L.; Ramey, K.; Pfledderer, C.D.; Burkart, S.; Armstrong, B.; Weaver, R.G.; Beets, M.W. The mysterious case of the disappearing pilot study: A review of publication bias in preliminary behavioral interventions presented at health behavior conferences. Pilot Feasibility Stud. 2023, 9, 115. [Google Scholar] [CrossRef] [PubMed]

| Study | Journal | Location | Participants | Age (Years) | Height (m) | Mass (kg) | BMI (kg·m−2) |
|---|---|---|---|---|---|---|---|
| Di Bacco et al. (2023) [17] | J. Biomech. | Canada | 9M 8F | 24.7 ± 3.7 | 1.73 ± 0.1 | 73.1 ± 14.2 | |
| Olson et al. (2023) [18] | Gait Posture | New Zealand | 14M 20F | 42–92 | 25.3 (median) | ||
| Grouios et al. (2022) [19] | Sensors | Greece | 1M | 29 | 1.78 | 72 | |
| Christensen et al. (2022) [20] | J. Orthop. Surg. Res. | USA | 8M 12F healthy; 7M 5F TKA/THA | 42.3 ± 19.7 58.7 ± 6.5 | 1.63 ± 0.24 | 77.0 ± 17.4 | |
| Kelly et al. (2022) [21] | Measurement | USA | 10M 13F | 21 ± 2 | 90.0 ± 15.5 | ||
| Shema-Shiratzky et al. (2022) [22] | Gait Posture | Israel | 35M 37F Knee OA (49) Ankle/hip OA (11) Low back pain (12) | 57.2 ± 1.9 | |||
| Rashid et al. (2021) [23] | Sensors | New Zealand | 5M 15F | 46 ± 27 | 1.67 ± 0.17 | 76 ± 19 | |
| Shahar et al. (2021) [24] | Sensors | Israel | 60 | 37.2 ± 13.4 | 1.71 ± 0.10 | ||
| Alberto et al. (2021) [25] | BMC Neurol. | Portugal | 12M 7F PD | 62 ± 12.3 | |||
| Lugade et al. (2021) [26] | J. Aging Phy. Act. | 8M 13F 7M 14F non-faller older 3M 18F faller older | 22.9 ± 2.2 71.8 ± 4.5 72.9 ± 5.3 | 1.64 ± 0.08 1.56 ± 0.07 1.56 ± 0.07 | 56.1 ± 9.1 57.6 ± 5.5 56.7 ± 7.5 | ||
| Su et al. (2021) [27] | JMIR Mhealth Uhealth | China | 33M 19F PD | 63 ± 10 | 1.7 ± 0.9 | 70 ± 21 | |
| Kuntapun et al. (2020) [28] | Frontiers in Sports and Active Living | 3M 9F young 3M 9F older | 23.4 ± 2.2 75.6 ± 5.6 | 1.63 ± 0.07 1.60 ± 0.09 | 58.3 ± 9.9 58.0 ± 6.6 | ||
| Silsupadol et al. (2020) [29] | IEEE J. Biomed. | 4M 8F young 0M 12F older | 21.4 ± 1.2 72.4 ± 6.1 | ||||
| Howell et al. (2020) [30] | Phys. Sportsmed | USA | 6M 14F | 22.2 ± 2.1 | 1.70 ± 0.08 | ||
| Tchelet et al. (2019) [31] | Sensors | Israel | 4 | 33.5 ± 3.9 | |||
| Silsupadol et al. (2017) [32] | Gait Posture | 1M 11F younger 7M 15F older | 22.7 ± 0.9 73.9 ± 5.6 | 21.2 ± 4.1 23.7 ± 3.6 | |||
| Pepa et al. (2017) [33] | Gait Posture | Italy | 8M 3F | 22–30 | |||
| Ellis et al. (2015) [34] | PLoS One | Singapore | 7M 5F PD 8M 4F controls | 65.0 ± 8.4 63.1 ± 7.8 | |||
| Furrer et al. (2015) [35] | Gait Posture | Switzerland | 10M 12F | 27.4 ± 3.9 | 1.74 ± 0.08 | 65.5 ± 10.2 | |
| Steins et al. (2014) [36] | J. Biomech. | UK | 10 | 25.6 ± 3.5 | 1.73 ± 0.17 | 73.0 ± 17.1 | |
| Nishiguchi et al. (2012) [37] | Telemed. J. E.Health | Japan | 17M 13F | 20.9 ± 2.1 | 1.67 ± 0.08 | 60.4 ± 7.7 |
| Study | Comparator | Smartphone | ||||
|---|---|---|---|---|---|---|
| Equipment | Markers | SF | App/Phone (OS) | SF | Location | |
| Di Bacco et al. (2023) [17] | Motion capture (7 camera Vicon) | Heel of right shoe. | 100 | - Google (Android) | 100 | Front right pocket |
| Delsys footswitch sensor | Right heel | 296 | ||||
| Olson et al. (2023) [18] | Motion capture (12 camera Qualisys) | Marker in centre of phone screen, plus posterior calcaneus and head of the fifth metatarsal bilaterally | Gait&Balance iPhone (iOS) | L5/S1 | ||
| Grouios et al. (2022) [19] | Motion capture (10 camera Vicon) | 16 markers, lower body. | 15 | Accelerometer iPhone (iOS) Accelerometer Acceleration Log Samsung/Huawei (Android) | 15 | Lumbar spine |
| Christensen et al. (2022) [20] | Motion capture (10 camera Vicon) | 53 markers. | 200 | OneStep iPhone (iOS) | 100 | 2 phones, anterior thigh. |
| Kelly et al. (2022) [21] | Tekscan Strideway pressure sensitive walkway | 30 | Gait Analyzer LGK40 (Android) | 95–105 | L5 | |
| Shema-Shiratzky et al. (2022) [22] | Protokinetics Zeno pressure sensitive walkway | OneStep Samsung (Android) | 100 | Upper left and right thigh. | ||
| Rashid et al. (2021) [23] | Motion capture (7 camera Vicon) | One marker on the centre of the smartphone, and two were placed on each foot, at the posterior calcaneus and lateral fifth metatarsal. | 200 | Gait&Balance iPhone (iOS) | 100 | L5/S1 |
| Shahar et al. (2021) [24] | APDM mobility lab | 3 IMUs, on both feet and L5 | 128 | OneStep (Android) | 100 | Front pocket |
| Alberto et al. (2021) [25] | Motion capture (10 camera Qualisys) | 48 markers, plus clusters. | 120 | Kinetikos Nokia (Android) | 100 | Both sides front pocket |
| 15 × Xsens IMU | Head, thorax, scapulae, upper arms, forearms, hands, sacrum, thighs, shanks, and feet. | 120 | ||||
| Lugade et al. (2021) [26] | Video (gait events identified) | 30 | Gait Analyzer (Android) | 50 | Right hip | |
| Su et al. (2021) [27] | APDM mobility lab | 3 IMUs, on both feet and L5 | 100 | - iPhone (iOS) | 100 | Front pocket |
| Kuntapun et al. (2020) [28] | Motion capture (9 camera BTS) | 28 markers | 120 | Gait Analyzer Samsung (Android) | 50 | L3, bag |
| Silsupadol et al. (2020) [29] | Motion capture (9 camera BTS) | 28 markers. | 120 | SensorData Samsung and Asus (Android) | 100 | L3, L5, bag |
| Video (gait events identified) | ||||||
| Howell et al. (2020) [30] | 3 × Opal IMU | Feet and lumbosacral junction. | 128 | Gait Analyzer Samsung (Android) | 50 | Lumbar spine |
| Tchelet et al. (2019) [31] | Motion capture (10 camera Qualisys) | 8 markers (shoulders, sternum, back, inside/outside feet). | Enchephalog Android and iPhone (iOS) | Sternum | ||
| 1 × Opal IMU | Sternum | 128 | ||||
| Silsupadol et al. (2017) [32] | GAITrite pressure sensitive walkway | 80 | SensorData vivo (Android) | 95–105 | L3, bag near right hip, front pocket (both vertical and horizontal orientation), handheld (as if speaking) | |
| Pepa et al. (2017) [33] | Motion capture (6 cameras BTS) | 9 markers on ASISx2, mid PSIS, heel, 1st, 5th metatarsal. | 100 | AccOrient iPhone (iOS) | 100 | L3. Lateral pelvis. |
| Ellis et al. (2015) [34] | Footswitch, sensor mat, GAITrite pressure sensitive walkway | Footswitch on heel pad. | SmartMove iPod Touch (iOS) | 100 | Navel | |
| Furrer et al. (2015) [35] | Motion capture (8 camera Vicon) | 34 markers. | 200 | - Android | 50 | L3 |
| Steins et al. (2014) [36] | Motion capture (6 camera Qualisys) | L3 | 100 | - iPod Touch (iOS) | 100 | L3 |
| 1 × Xsens IMU | L3 | 100 | ||||
| Nishiguchi et al. (2012) [37] | 1 × WAA-006 accelerometer | L3 | 33.3 | - Android | 33.3 | L3 |
| Study | Environment | Speed | Duration |
|---|---|---|---|
| Di Bacco et al. (2023) [17] | Treadmill | PWS | 3 × 8 min |
| Olson et al. (2023) [18] | PWS, PWS + dual task | 4 × 6 s | |
| Grouios et al. (2022) [19] | 6 m walkway | PWS | 9 × 6 steps |
| Christensen et al. (2022) [20] | Treadmill, indoor home environment | Treadmill: PWS, 0.8 ms−2, 2 ms−2, PWS + dual task | Treadmill: 15 steps Home: 30 s. |
| Kelly et al. (2022) [21] | 10 m walkway | PWS | 6 × 20 m |
| Shema-Shiratzky et al. (2022) [22] | 10 m walkway | PWS | 4 × 10 m |
| Rashid et al. (2021) [23] | PWS, PWS + dual task | 4 × 6 s | |
| Shahar et al. (2021) [24] | 10 m walkway | PWS, ‘as fast as you can’, ‘as if the floor was slippery’, PWS + dual task | 2 min |
| Alberto et al. (2021) [25] | Walkway | PWS | 3 × 10 m |
| Lugade et al. (2021) [26] | Lab overground, circular | PWS | 2 × 2 min |
| Su et al. (2021) [27] | 10 m hallway (turns removed in analysis) | PWS, PWS + dual task | 2 × 20 m |
| Kuntapun et al. (2020) [28] | Walkway Outdoor area. | PWS. Indoors and outdoors, level, irregular, obstacle crossing | 10 m |
| Silsupadol et al. (2020) [29] | Walkway Outdoor area. | Speed changes and turns in separate trials. Slow = ‘as slow as they can’ Fast = ‘as fast as they can without running’ | 10 m |
| Howell et al. (2020) [30] | Walkway | PWS. Turns included. Dual task. | 5 min, 5 × 20 m (with turn). |
| Tchelet et al. (2019) [31] | Walkway | Various—not specified what. | 3 m/5 m |
| Silsupadol et al. (2017) [32] | Walkway | PWS, slow, fast (actual values not specified) | 10 m |
| Pepa et al. (2017) [33] | Walkway | PWS, higher, lower (actual values not specified) | 10 m platform. Back and forth. |
| Ellis et al. (2015) [34] | Walkway | PWS, cued PWS, cued PWS + 10% | 26 m path, turn halfway |
| Furrer et al. (2015) [35] | Walkway | PWS | 10 × 10 m |
| Steins et al. (2014) [36] | Walkway | PWS | 4 × 10 m |
| Nishiguchi et al. (2012) [37] | Walkway | PWS | 3 × 20 m |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Strongman, C.; Cavallerio, F.; Timmis, M.A.; Morrison, A. A Scoping Review of the Validity and Reliability of Smartphone Accelerometers When Collecting Kinematic Gait Data. Sensors 2023, 23, 8615. https://doi.org/10.3390/s23208615
Strongman C, Cavallerio F, Timmis MA, Morrison A. A Scoping Review of the Validity and Reliability of Smartphone Accelerometers When Collecting Kinematic Gait Data. Sensors. 2023; 23(20):8615. https://doi.org/10.3390/s23208615
Chicago/Turabian StyleStrongman, Clare, Francesca Cavallerio, Matthew A. Timmis, and Andrew Morrison. 2023. "A Scoping Review of the Validity and Reliability of Smartphone Accelerometers When Collecting Kinematic Gait Data" Sensors 23, no. 20: 8615. https://doi.org/10.3390/s23208615
APA StyleStrongman, C., Cavallerio, F., Timmis, M. A., & Morrison, A. (2023). A Scoping Review of the Validity and Reliability of Smartphone Accelerometers When Collecting Kinematic Gait Data. Sensors, 23(20), 8615. https://doi.org/10.3390/s23208615








