Companion: A Pilot Randomized Clinical Trial to Test an Integrated Two-Way Communication and Near-Real-Time Sensing System for Detecting and Modifying Daily Inactivity among Adults >60 Years—Design and Protocol
Abstract
:1. Introduction
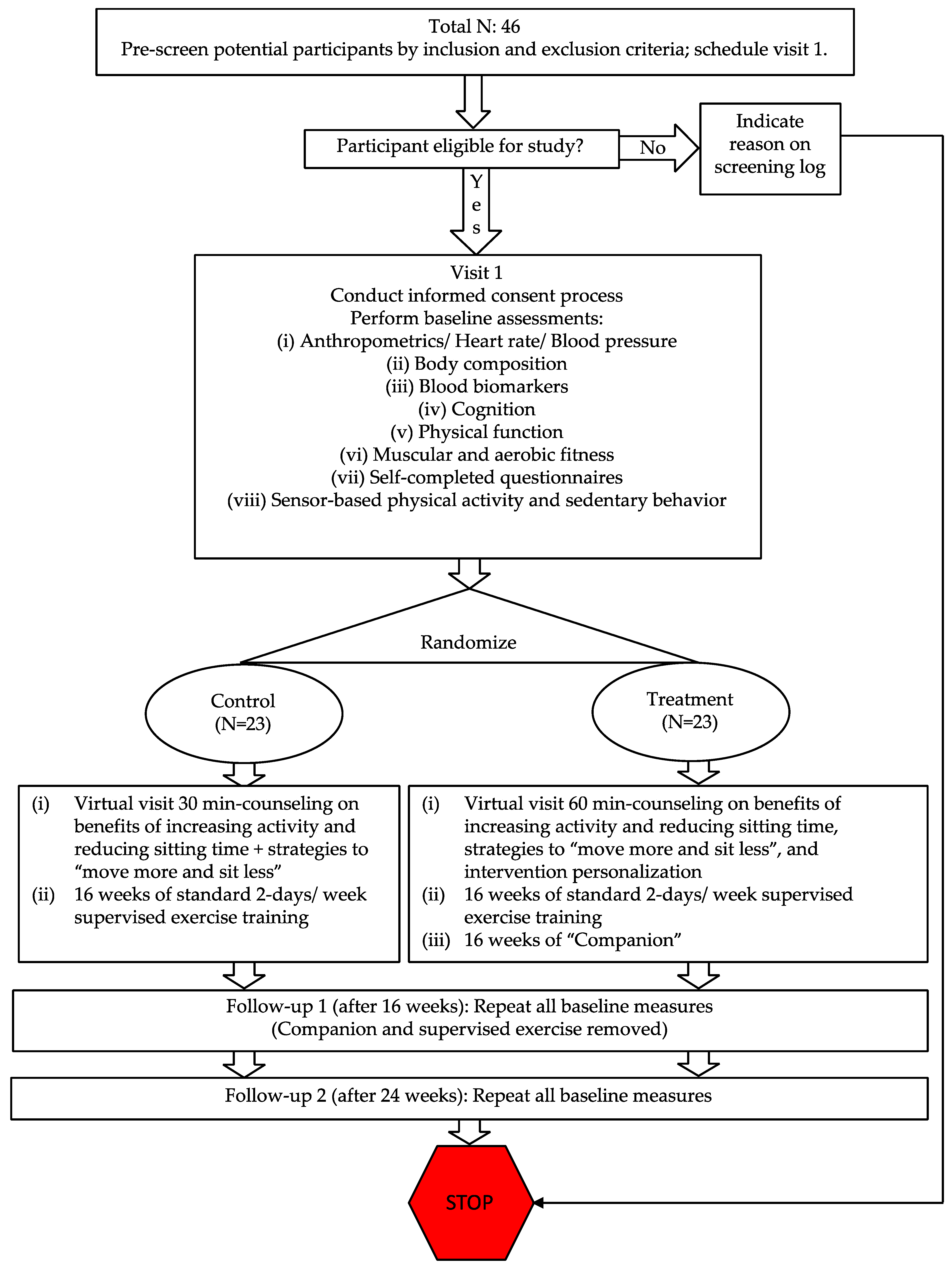
2. Materials and Methods
2.1. Hypotheses and Experimental Design
2.2. Rationale and Feasibility Testing
2.2.1. Supervised Exercise Programs Fail to Increase Daily Habitual Behavior
2.2.2. Feasibility Testing
2.3. Participants
2.3.1. Inclusion and Exclusion Criteria
2.3.2. Recruitment, Screening Procedures and Randomization
2.4. Measurements
2.4.1. Primary Outcomes
2.4.2. Exploratory Outcomes
2.5. Control and Intervention Components
2.5.1. Virtual Counseling
2.5.2. Supervised Exercise Training
2.5.3. The Companion
2.5.4. Exercise Prescription Database
2.6. Sample Size and Power Analysis
2.7. Planned Data Analyses
2.7.1. Analyses of Primary and Exploratory Outcomes
2.7.2. Exploratory Analyses of Intensive Longitudinal Physical Behavior Measurement
2.7.3. Exploratory Analyses of Intensive Longitudinal Two-Way Communication Data
3. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Disclaimer Statement
Abbreviations
| AI | Artificial Intelligence |
| MIMS | Monitor-Independent Movement Summary Unit |
| SDT | Self-Determination Theory |
| ACSM | American College of Sports Medicine |
| MI | Motivational Interviewing |
| QC | Quality Control |
| SWaN | Sleep, Wear, and Non-wear |
| MUSS | Multi-Site Sensing for Activity Recognition |
| mHealth | Mobile Health |
References
- Devereux-Fitzgerald, A.; Powell, R.; Dewhurst, A.; French, D.P. The acceptability of physical activity interventions to older adults: A systematic review and meta-synthesis. Soc. Sci. Med. 2016, 158, 14–23. [Google Scholar] [CrossRef] [PubMed]
- Erickson, K.I.; Grove, G.A.; Burns, J.; Hillman, C.H.; Kramer, A.; McAuley, E.; Vidoni, E.D.; Becker, J.T.; Butters, M.A.; Gray, K.; et al. Investigating gains in neurocognition in an Intervention Trial of Exercise (IGNITE): Protocol. Contemp. Clin. Trials 2019, 85, 105832. [Google Scholar] [CrossRef] [PubMed]
- Evidence-Based Programs for Professionals—Exercise Programs That Promote Senior Fitness: National Council on Aging. Available online: https://www.ncoa.org/article/exercise-programs-that-promote-senior-fitness (accessed on 29 January 2021).
- Pahor, M.; Guralnik, J.M.; Ambrosius, W.T.; Blair, S.; Bonds, D.E.; Church, T.S.; Espeland, M.A.; Fielding, R.A.; Gill, T.M.; Groessl, E.J.; et al. Effect of structured physical activity on prevention of major mobility disability in older adults: The LIFE study randomized clinical trial. JAMA 2014, 311, 2387–2396. [Google Scholar] [CrossRef] [PubMed]
- Pavey, T.; Taylor, A.; Hillsdon, M.; Fox, K.; Campbell, J.; Foster, C.; Moxham, T.; Mutrie, N.; Searle, J.; Taylor, R. Levels and predictors of exercise referral scheme uptake and adherence: A systematic review. J. Epidemiol. Community Health 2012, 66, 737–744. [Google Scholar] [CrossRef]
- Picorelli, A.M.; Pereira, L.S.; Pereira, D.S.; Felicio, D.; Sherrington, C. Adherence to exercise programs for older people is influenced by program characteristics and personal factors: A systematic review. J. Physiother. 2014, 60, 151–156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shubert, T.E. Evidence-based exercise prescription for balance and falls prevention: A current review of the literature. J. Geriatr. Phys 2011, 34, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Williams, N.H.; Hendry, M.; France, B.; Lewis, R.; Wilkinson, C. Effectiveness of exercise-referral schemes to promote physical activity in adults: Systematic review. Br. J. Gen. Pr. 2007, 57, 979–986. [Google Scholar] [CrossRef]
- Courneya, K.S.; Karvinen, K.H.; McNeely, M.L.; Campbell, K.L.; Brar, S.; Woolcott, C.G.; McTiernan, A.; Ballard-Barbash, R.; Friedenreich, C.M. Predictors of adherence to supervised and unsupervised exercise in the Alberta Physical Activity and Breast Cancer Prevention Trial. J. Phys. Act. Health 2012, 9, 857–866. [Google Scholar] [CrossRef]
- Lacroix, A.; Kressig, R.W.; Muehlbauer, T.; Gschwind, Y.J.; Pfenninger, B.; Bruegger, O.; Granacher, U. Effects of a Supervised versus an Unsupervised Combined Balance and Strength Training Program on Balance and Muscle Power in Healthy Older Adults: A Randomized Controlled Trial. Gerontology 2016, 62, 275–288. [Google Scholar] [CrossRef]
- Meijer, E.P.; Westerterp, K.R.; Verstappen, F.T. Effect of exercise training on total daily physical activity in elderly humans. Eur. J. Appl. Physiol. Occup. Physiol. 1999, 80, 16–21. [Google Scholar] [CrossRef]
- Meijer, E.P.; Westerterp, K.R.; Verstappen, F.T. Effect of exercise training on physical activity and substrate utilization in the elderly. Int. J. Sport. Med. 2000, 21, 499–504. [Google Scholar] [CrossRef]
- Morio, B.; Montaurier, C.; Pickering, G.; Ritz, P.; Fellmann, N.; Coudert, J.; Beaufrère, B.; Vermorel, M. Effects of 14 weeks of progressive endurance training on energy expenditure in elderly people. Br. J. Nutr. 1998, 80, 511–519. [Google Scholar] [CrossRef]
- Drenowatz, C. Reciprocal Compensation to Changes in Dietary Intake and Energy Expenditure within the Concept of Energy Balance. Adv. Nutr. 2015, 6, 592–599. [Google Scholar] [CrossRef] [Green Version]
- Melanson, E.L.; Keadle, S.K.; Donnelly, J.E.; Braun, B.; King, N.A. Resistance to exercise-induced weight loss: Compensatory behavioral adaptations. Med. Sci. Sport. Exerc. 2013, 45, 1600–1609. [Google Scholar] [CrossRef] [Green Version]
- Doucet, E.; McInis, K.; Mahmoodianfard, S. Compensation in response to energy deficits induced by exercise or diet. Obes.Rev. Off. J. Int. Assoc. Study Obes. 2018, 19 (Suppl. S1), 36–46. [Google Scholar] [CrossRef]
- Melanson, E.L. The effect of exercise on non-exercise physical activity and sedentary behavior in adults. Obes.Rev. Off. J. Int. Assoc. Study Obes. 2017, 18 (Suppl. S1), 40–49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bankoski, A.; Harris, T.B.; McClain, J.J.; Brychta, R.J.; Caserotti, P.; Chen, K.Y.; Berrigan, D.; Troiano, R.P.; Koster, A. Sedentary activity associated with metabolic syndrome independent of physical activity. Diabetes Care 2011, 34, 497–503. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elosua, R.; Bartali, B.; Ordovas, J.M.; Corsi, A.M.; Lauretani, F.; Ferrucci, L.; on Behalf of the InCHIANTI Investigators. Association between physical activity, physical performance, and inflammatory biomarkers in an elderly population: The InCHIANTI study. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2005, 60, 760–767. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Physical Activity Guidelines for Americans 2nd Edition: U.S. Department of Health and Human Services. Available online: https://health.gov/sites/default/files/2019-09/Physical_Activity_Guidelines_2nd_edition.pdf (accessed on 20 January 2021).
- Czaja, S.J. Can technology empower older adults to manage their health? Generations 2015, 39, 46–51. [Google Scholar]
- Roess, A. The Promise, Growth, and Reality of Mobile Health—Another Data-free Zone. N. Engl. J. Med. 2017, 377, 2010–2011. [Google Scholar] [CrossRef] [PubMed]
- Nunes, D.S.; Zhang, P.; Silva, J.S. A survey on human-in-the-loop applications towards an internet of all. IEEE Commun. Surv. Tutor. 2015, 17, 944–965. [Google Scholar] [CrossRef]
- John, D.; Castaneda-Sceppa, C.; Hillman, C.; Kramer, A. An Integrated Two-Way Communication and Near-Real-Time Sensing System to Detect and Modify Daily Inactivity among Adults > 60 y, Grant ID: P30 AG048785; Sponsored by the National Institute on Aging: Washington, DC, USA, Total costs: 117,681, Project Period: 5/1/2020-5/31/2022.
- Onken, L.S.; Carroll, K.M.; Shoham, V.; Cuthbert, B.N.; Riddle, M. Reenvisioning Clinical Science: Unifying the Discipline to Improve the Public Health. Clin. Psychol. Sci. 2014, 2, 22–34. [Google Scholar] [CrossRef] [Green Version]
- Onken, L. Implementation Science at the National Institute on Aging: The Principles of It. Public Policy Aging Rep. 2022, 32, 39–41. [Google Scholar] [CrossRef]
- Castaneda, C.; Layne, J.E.; Munoz-Orians, L.; Gordon, P.L.; Walsmith, J.; Foldvari, M.; Roubenoff, R.; Tucker, K.L.; Nelson, M.E. A randomized controlled trial of resistance exercise training to improve glycemic control in older adults with type 2 diabetes. Diabetes Care 2002, 25, 2335–2341. [Google Scholar] [CrossRef] [Green Version]
- Nelson, M.; Layne, J.; Bernstein, M.; Nuernberger ACastaneda, C.; Kaliton, D.; Hausdorff, J.; Judge, J.; Buchner, D.M.; Roubenoff, R.; Fiatarone Singh, M.A. The effects of multidimensional home based exercise on functional performance in the elderly. J. Gerontol. A 2004, 59, 154–160. [Google Scholar] [CrossRef]
- Franco, M.R.; Tong, A.; Howard, K.; Sherrington, C.; Ferreira, P.H.; Pinto, R.Z.; Ferreira, M.L. Older people’s perspectives on participation in physical activity: A systematic review and thematic synthesis of qualitative literature. Br. J. Sport. Med. 2015, 49, 1268–1276. [Google Scholar] [CrossRef]
- Fedewa, M.V.; Hathaway, E.D.; Williams, T.D.; Schmidt, M.D. Effect of Exercise Training on Non-Exercise Physical Activity: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Sport. Med. 2017, 47, 1171–1182. [Google Scholar] [CrossRef]
- Arguello, D.; Ponnada, A.; Cloutier, G.; Intille, S.; John, D. Communication with a Smartphone-Based Virtual Health Companion: A Pilot Study. 2016; Unpublished Work. [Google Scholar]
- Troiano, R.P.; Berrigan, D.; Dodd, K.W.; Masse, L.C.; Tilert, T.; McDowell, M. Physical activity in the United States measured by accelerometer. Med. Sci. Sport. Exerc. 2008, 40, 181–188. [Google Scholar] [CrossRef]
- Tudor-Locke, C.; Burkett, L.; Reis, J.; Ainsworth, B.; Macera, C.; Wilson, D. How many days of pedometer monitoring predict weekly physical activity in adults? Prev. Med. 2005, 40, 293–298. [Google Scholar] [CrossRef]
- Judice, P.B.; Santos, D.A.; Hamilton, M.T.; Sardinha, L.B.; Silva, A.M. Validity of GT3X and Actiheart to estimate sedentary time and breaks using ActivPAL as the reference in free-living conditions. Gait. Posture 2015, 41, 917–922. [Google Scholar] [CrossRef] [PubMed]
- Klenk, J.; Büchele, G.; Lindemann, U.; Kaufmann, S.; Peter, R.; Laszlo, R.; Kobel, S.; Rothenbacher, D. Concurrent Validity of activPAL and activPAL3 Accelerometers in Older Adults. J. Aging Phys. Act. 2016, 24, 444–450. [Google Scholar] [CrossRef] [PubMed]
- Kozey-Keadle, S.; Libertine, A.; Lyden, K.; Staudenmayer, J.; Freedson, P.S. Validation of wearable monitors for assessing sedentary behavior. Med. Sci. Sport. Exerc. 2011, 43, 1561–1567. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lyden, K.; Kozey Keadle, S.L.; Staudenmayer, J.W.; Freedson, P.S. Validity of two wearable monitors to estimate breaks from sedentary time. Med. Sci. Sport. Exerc. 2012, 44, 2243–2252. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carlson, J.A.; Tuz-Zahra, F.; Bellettiere, J.; Ridgers, N.D.; Steel, C.; Bejarano, C.; LaCroix, A.Z.; Rosenberg, D.E.; Greenwood-Hickman, M.A.; Jankowska, M.M.; et al. Validity of Two Awake Wear-Time Classification Algorithms for activPAL in Youth, Adults, and Older Adults. J. Meas. Phys. Behav. 2021, 4, 151–162. [Google Scholar] [CrossRef] [PubMed]
- Lyden, K.; Speirs, C.; Loudon, D.; Christopher, C.; Barnett, R.; Martinez, J.; Takeda, M.; Keadle, S. Using A Thigh Worn Accelerometer To Identify Periods Of Seated Car Travel. Med. Sci. Sport. Exerc. 2019, 51, 163–164. [Google Scholar] [CrossRef]
- John, D.; Tang, Q.; Albinali, F.; Intille, S. An Open-Source Monitor-Independent Movement Summary for Accelerometer Data Processing. J. Meas. Phys. Behav. 2019, 2, 268–281. [Google Scholar] [CrossRef]
- Mannini, A.; Intille, S.S.; Rosenberger, M.; Sabatini, A.M.; Haskell, W. Activity recognition using a single accelerometer placed at the wrist or ankle. Med. Sci. Sport. Exerc. 2013, 45, 2193. [Google Scholar] [CrossRef] [Green Version]
- Ponnada, A.; Cooper, S.; Tang, Q.; Thapa-Chhetry, B.; Miller, J.A.; John, D.; Intille, S. Signaligner Pro: A Tool to Explore and Annotate Multi-day Raw Accelerometer Data. Proc. IEEE Int. Conf. Pervasive Comput. Commun. 2021, 2021, 475–480. [Google Scholar]
- Tang, Q.; John, D.; Thapa-Chhetry, B.; Arguello, D.; Intille, S. Posture and Physical Activity Detection: Impact of Number of Sensors and Feature Type. Med. Sci. Sport. Exerc. 2020, 52, 1834–1845. [Google Scholar] [CrossRef]
- Thapa-Chhetry, B.; Arguello, D.J.; John, D.; Intille, S. Detecting Sleep and Nonwear in 24-h Wrist Accelerometer Data from the National Health and Nutrition Examination Survey. Med. Sci. Sport. Exerc. 2022, 54, 1936–1946. [Google Scholar] [CrossRef] [PubMed]
- Heyward, V. ASEP Methods Recommendation: Body Composition Assessment. J. Exerc. Physiol. Online 2001, 4, 1–12. [Google Scholar]
- Denboer, J.W.; Nicholls, C.; Corte, C.; Chestnut, K. National Institutes of Health Toolbox Cognition Battery. Arch. Clin. Neuropsychol. 2014, 29, 692–694. [Google Scholar] [CrossRef] [Green Version]
- Gomez, J.F.; Curcio, C.L.; Alvarado, B.; Zunzunegui, M.V.; Guralnik, J. Validity and reliability of the Short Physical Performance Battery (SPPB): A pilot study on mobility in the Colombian Andes. Colomb Med. 2013, 44, 165–171. [Google Scholar] [CrossRef]
- Guralnik, J.M.; Simonsick, E.M.; Ferrucci, L.; Glynn, R.J.; Berkman, L.F.; Blazer, D.G.; Scherr, P.A.; Wallace, R.B. A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. J. Gerontol. 1994, 49, M85–M94. [Google Scholar] [CrossRef]
- American College of Sports Medicine; Liguori, G.; Feito, Y.; Fountaine, C.; Roy, B. ACSM’s Guidelines for Exercise Testing and Prescription, 11th ed.; Wolter Klugers: Philadelphia, PA, USA, 2021. [Google Scholar]
- Sadaria, K.S.; Bohannon, R.W. The 6-minute walk test: A brief review of the literature. Clin. Exerc. Physiol. 2001, 3, 127–132. [Google Scholar]
- Bohannon, R.W. Six-Minute Walk Test: A Meta-Analysis of Data from Apparently Healthy Elders. Top. Geriatr. Rehabiliation 2007, 23, 155–160. [Google Scholar] [CrossRef] [Green Version]
- Block, G.; Hartman, A.M.; Dresser, C.M.; Carroll, M.D.; Gannon, J.; Gardner, L. A data-based approach to diet questionnaire design and testing. Am. J. Epidemiol. 1986, 124, 453–469. [Google Scholar] [CrossRef]
- Mares-Perlman, J.A.; Klein, B.E.; Klein, R.; Ritter, L.L.; Fisher, M.R.; Freudenheim, J.L. A diet history questionnaire ranks nutrient intakes in middle-aged and older men and women similarly to multiple food records. J. Nutr. 1993, 123, 489–501. [Google Scholar] [CrossRef]
- Williams, G.C.; Freedman, Z.R.; Deci, E.L. Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care 1998, 21, 1644–1651. [Google Scholar] [CrossRef]
- Williams, G.C.; Deci, E.L. Internalization of biopsychosocial values by medical students: A test of self-determination theory. J. Pers. Soc. Psychol. 1996, 70, 767–779. [Google Scholar] [CrossRef] [PubMed]
- Ryan, R.M.; Connell, J.P. Perceived locus of causality and internalization: Examining reasons for acting in two domains. J. Pers. Soc. Psychol. 1989, 57, 749–761. [Google Scholar] [CrossRef] [PubMed]
- Ryan, R.; Deci, E.; Cerasoli, S.H.; Lemos, K. Self-Regulation Questionnaires (SRQ) Selfdeterminationtheory.org: Center for Self Determination Theory. Available online: https://selfdeterminationtheory.org/self-regulation-questionnaires/ (accessed on 20 January 2021).
- Johnston, M.M.; Finney, S.J. Measuring basic needs satisfaction: Evaluating previous research and conducting new psychometric evaluations of the Basic Needs Satisfaction in General Scale. Contemp. Educ. Psychol. 2010, 35, 280–296. [Google Scholar] [CrossRef]
- Ryan, R.M.; Deci, E.L. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am. Psychol. 2000, 55, 68–78. [Google Scholar] [CrossRef]
- Deci, E.L.; Ryan, R.M. Intrinsic Motivation and Self-Determination in Human Behavior. Plenum Publishing Co.: New York, NY, USA, 1985. [Google Scholar]
- King, A.C.; Powell, K.E.; Buchner, D.; Campbell, W.; DiPietro, L.; Erickson, K.I.; Hillman, C.H.; Jakicic, J.M.; Janz, K.F.; Katzmarzyk, P.T.; et al. Physical Activity Guidelines Advisory Committee Scientific Report; U.S. Department of Health and Human Services: Washington, DC, USA, 2018. Available online: https://health.gov/sites/default/files/2019-09/PAG_Advisory_Committee_Report.pdf (accessed on 20 January 2022).
- “Steps to a Healtier Way of Life”: America on the Move Foundation. 2007. Available online: https://wellness.illinoisstate.edu/downloads/living/100waystoaddsteps.pdf (accessed on 20 January 2021).
- “Physical Activity Breaks for the Workplace”: The Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/workplacehealthpromotion/initiatives/resource-center/pdf/Workplace-Physical-Activity-Break-Guide-508.pdf (accessed on 20 January 2021).
- Pescatello, L.S.; American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription, 9th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2014. [Google Scholar]
- Nelson, M.E.; Rejeski, W.J.; Blair, S.N.; Duncan, P.W.; Judge, J.O.; King, A.C.; Macera, C.A.; Castaneda-Sceppa, C. Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Circulation 2007, 116, 1094–1105. [Google Scholar] [CrossRef] [Green Version]
- American College of Sports M; American College of Sports Medicine Position Stand. Progression models in resistance training for healthy adults. Med. Sci. Sport. Exerc. 2009, 41, 687–708. [Google Scholar] [CrossRef]
- Arguello, D.; Denmark, G.H.; Cloutier, G.; Lena, J.; Anderson-Song, Q.; John, D. Companion Study: Exercise Prescription Database. 2022. Available online: https://www.youtube.com/channel/UCZsg8fPtquiVrsv8INIvC0g (accessed on 11 November 2022).
- Miller, W.R.; Rollnick, S. Motivational Interviewing: Helping People Change, 3rd ed.; Guilford Press: New York, NY, USA, 2012. [Google Scholar]
- Gourlan, M.; Sarrazin, P.; Trouilloud, D. Motivational interviewing as a way to promote physical activity in obese adolescents: A randomised-controlled trial using self-determination theory as an explanatory framework. Psychol. Health 2013, 28, 1265–1286. [Google Scholar] [CrossRef]
- Miller, W.R.; Rollnick, S. Meeting in the middle: Motivational interviewing and self-determination theory. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 25. [Google Scholar] [CrossRef] [Green Version]
- Vansteenkiste, M.; Williams, G.C.; Resnicow, K. Toward systematic integration between self-determination theory and motivational interviewing as examples of top-down and bottom-up intervention development: Autonomy or volition as a fundamental theoretical principle. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 23. [Google Scholar] [CrossRef] [Green Version]
- Dunton, G.F.; Kawabata, K.; Intille, S.; Wolch, J.; Pentz, M.A. Assessing the social and physical contexts of children’s leisure-time physical activity: An ecological momentary assessment study. Am. J. Health Promot. 2012, 26, 135–142. [Google Scholar] [CrossRef]
- Dunton, G.F.; Liao, Y.; Intille, S.S.; Spruijt-Metz, D.; Pentz, M. Investigating children’s physical activity and sedentary behavior using ecological momentary assessment with mobile phones. Obesity 2011, 19, 1205–1212. [Google Scholar] [CrossRef]
- Intille, S.S. Technological innovations enabling automatic, context-sensitive ecological momentary assessment. In The Science of Real-Time Data Capture: Self-Reports in Health Research; Caldeira, V.R.B.G., Rombach, H.D., Eds.; Oxford University Press: Oxford, UK, 2007; pp. 308–337. [Google Scholar]
- Troiano, R.; Intille, S.; John, D.; Thapa-Chhetry, B.; Tang, Q. NHANES and NNYFS wrist accelerometer data: Processing 7 TB of data for public access. J. Phys. Act. Health 2018, 15, S19. [Google Scholar]
- John, D.; Thompson, D.L.; Raynor, H.; Bielak, K.; Rider, B.; Bassett, D.R. Treadmill workstations: A worksite physical activity intervention in overweight and obese office workers. J. Phys. Act. Health 2011, 8, 1034–1043. [Google Scholar] [CrossRef]
- Boerema, S.T.; van Velsen, L.; Vollenbroek, M.M.; Hermens, H.J. Pattern measures of sedentary behaviour in adults: A literature review. Digit. Health 2020, 6, 2055207620905418. [Google Scholar] [CrossRef]
- Chastin, S.F.M.; Winkler, E.A.H.; Eakin, E.G.; Gardiner, P.; Dunstan, D.; Owen, N.; Healy, G. Sensitivity to Change of Objectively-Derived Measures of Sedentary Behavior. Meas. Phys. Educ. Exerc. Sci. 2015, 19, 138–147. [Google Scholar] [CrossRef]
- Healy, G.N.; Eakin, E.G.; Owen, N.; Lamontagne, A.D.; Moodie, M.; Winkler, E.A.; Wiesner, G.; Willenberg, L.; Dunstan, D.W. A Cluster Randomized Controlled Trial to Reduce Office Workers’ Sitting Time: Effect on Activity Outcomes. Med. Sci. Sport. Exerc. 2016, 48, 1787–1797. [Google Scholar] [CrossRef]
- Sawilowsky, S.S. New Effect Size Rules of Thumb. J. Mod. Appl. Stat. Methods 2009, 8, 467–474. [Google Scholar] [CrossRef]
- Rubin, D.B. Multiple Imputation for Nonresponse in Surveys; John Wiley & Sons, Inc.: New York, NY, USA, 1987. [Google Scholar]
- McNeish, D. Missing data methods for arbitrary missingness with small samples. J. Appl. Stat. 2016, 44, 24–39. [Google Scholar] [CrossRef] [Green Version]
- Thabane, L.; Mbuagbaw, L.; Zhang, S.; Samaan, Z.; Marcucci, M.; Ye, C.; Thabane, M.; Giangregorio, L.; Dennis, B.; Kosa, D.; et al. A tutorial on sensitivity analyses in clinical trials: The what, why, when and how. BMC Med. Res. Methodol. 2013, 13, 92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Felt, J.M.; Depaoli, S.; Tiemensma, J. Latent Growth Curve Models for Biomarkers of the Stress Response. Front. Neurosci. 2017, 11, 315. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Diallo, T.M.O.; Morin, A.J.S. Power of Latent Growth Curve Models to Detect Piecewise Linear Trajectories. Struct. Equ. Model. A Multidiscip. J. 2014, 22, 449–460. [Google Scholar] [CrossRef]
- Duncan, T.E.; Duncan, S.C. The ABC’s of LGM: An Introductory Guide to Latent Variable Growth Curve Modeling. Soc. Pers. Psychol. Compass 2009, 3, 979–991. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kunzler, F.; Mishra, V.; Kramer, J.N.; Kotz, D.; Fleisch, E.; Kowatsch, T. Exploring the State-of-Receptivity for mHealth Interventions. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 2019, 3, 1–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mishra, V.; Kunzler, F.; Kramer, J.N.; Fleisch, E.; Kowatsch, T.; Kotz, D. Detecting Receptivity for mHealth Interventions in the Natural Environment. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 2021, 5, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Schwebel, F.; Larimer, M.E. Text message reminders as an adjunct to a substance use intervention for adoslescents and young adults: Pilot feasibility and acceptability findings. Digit. Health 2020, 6, 11. [Google Scholar]
- Kramer, J.-N.; Künzler, F.; Mishra, V.; Smith, S.N.; Kotz, D.; Scholz, U.; Fleisch, E.; Kowatsch, T. Which Components of a Smartphone Walking App Help Users to Reach Personalized Step Goals? Results from an Optimization Trial. Ann. Behav. Med. 2020, 54, 518–528. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martin, G.; Pear, J.J. Increasing a Behavior with Positive Reinforcement. In Behavior Modification, 10th ed.; Psychology Press: New York, NY, USA, 2014. [Google Scholar]
- Tan, X.; Shiyko, M.P.; Li, R.; Li, Y.; Dierker, L. A time-varying effect model for intensive longitudinal data. Psychol. Methods 2012, 17, 61–77. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trail, J.B.; Collins, L.M.; Rivera, D.E.; Li, R.; Piper, M.E.; Baker, T.B. Functional data analysis for dynamical system identification of behavioral processes. Psychol. Methods 2014, 19, 175–187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lanza, S.T.; Vasilenko, S.A.; Liu, X.; Li, R.; Piper, M.E. Advancing the understanding of craving during smoking cessation attempts: A demonstration of the time-varying effect model. Nicotine Tob. Res. 2014, 16 (Suppl. S2), S127–S134. [Google Scholar] [CrossRef] [Green Version]
- Dziak, J.J.; Li, R.; Tan, X.; Shiffman, S.; Shiyko, M.P. Modeling intensive longitudinal data with mixtures of nonparametric trajectories and time-varying effects. Psychol. Methods 2015, 20, 444–469. [Google Scholar] [CrossRef]
- Bickmore, T.W.; Mauer, D.; Brown, T. Context Awareness in a Handheld Exercise Agent. Pervasive Mob. Comput. 2009, 5, 226–235. [Google Scholar] [CrossRef] [Green Version]
- Brouwer, W.; Kroeze, W.; Crutzen, R.; de Nooijer, J.; de Vries, N.K.; Brug, J.; Oenema, A. Which intervention characteristics are related to more exposure to internet-delivered healthy lifestyle promotion interventions? A systematic review. J. Med. Internet. Res. 2011, 13, e2. [Google Scholar] [CrossRef] [PubMed]
- Schubart, J.R.; Stuckey, H.L.; Ganeshamoorthy, A.; Sciamanna, C.N. Chronic health conditions and internet behavioral interventions: A review of factors to enhance user engagement. Comput. Inf. Nurs. 2011, 29, 81–92. [Google Scholar] [CrossRef] [PubMed]
- Fischer, G. User modeling in human–computer interaction. User Model. User-Adapt. Interact. 2001, 11, 65–86. [Google Scholar] [CrossRef]
- Direito, A.; Carraça, E.; Rawstorn, J.; Whittaker, R.; Maddison, R. mHealth technologies to influence physical activity and sedentary behaviors: Behavior change techniques, systematic review and meta-analysis of randomized controlled trials. Ann. Behav. Med. 2016, 51, 226–239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Reilly, G.A.; Spruijt-Metz, D. Current mHealth technologies for physical activity assessment and promotion. Am. J. Prev. Med. 2013, 45, 501–507. [Google Scholar] [CrossRef] [Green Version]
- Vandelanotte, C.; Müller, A.M.; Short, C.E.; Hingle, M.; Nathan, N.; Williams, S.L.; Lopez, M.L.; Parekh, S.; Maher, C.A. Past, present, and future of eHealth and mHealth research to improve physical activity and dietary behaviors. J. Nutr. Educ. Behav. 2016, 48, 219–228.e1. [Google Scholar] [CrossRef]
- Fogg, B.J. Persuasive Technology: Using Computers to Change What We Think and Do, 1st ed.; Morgan and Kauffman Publishers: SanFrancisco, CA, USA, 2002. [Google Scholar]
- Blake, H.; Mo, P.; Malik, S.; Thomas, S. How effective are physical activity interventions for alleviating depressive symptoms in older people? A systematic review. Clin. Rehabil. 2009, 23, 873–887. [Google Scholar] [CrossRef]
- Conn, V.S.; Minor, M.A.; Burks, K.J.; Rantz, M.J.; Pomeroy, S.H. Integrative review of physical activity intervention research with aging adults. J. Am. Geriatr. Soc. 2003, 51, 1159–1168. [Google Scholar] [CrossRef]
- Faverio, M. Share of Those 65 and Older Who Are Tech Users Has Grown in the Past Decade; Pew Research Center: Washington, DC, USA, 2022; Available online: https://www.pewresearch.org/fact-tank/2022/01/13/share-of-those-65-and-older-who-are-tech-users-has-grown-in-the-past-decade/ (accessed on 4 December 2022).
- World Population Ageing. Highlights; United Nations, Department of Economic and Social Affairs: New York, NY, USA, 2019; Available online: https://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2019-Highlights.pdf (accessed on 4 December 2022).
- Looije, R.; Neerincx, M.A.; Cnossen, F. Persuasive robotic assistant for health self-management of older adults: Design and evaluation of social behaviors. Int. J. Hum. Comput. Stud. 2010, 68, 386–397. [Google Scholar] [CrossRef]
- Kemperman, A.; van den Berg, P.; Weijs-Perree, M.; Uijtdewillegen, K. Loneliness of Older Adults: Social Network and the Living Environment. Int. J. Environ. Res. Public Health 2019, 16, 406. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pels, F.; Kleinert, J. Loneliness and physical activity: A systematic review. Int. Rev. Sport. Exerc. Psychol. 2016, 9, 231–260. [Google Scholar] [CrossRef]
- Rico-Uribe, L.A.; Caballero, F.F.; Martin-Maria, N.; Cabello, M.; Ayuso-Mateos, J.L.; Miret, M. Association of loneliness with all-cause mortality: A meta-analysis. PLoS ONE 2018, 13, e0190033. [Google Scholar] [CrossRef] [PubMed]
- Park, C.; Majeed, A.; Gill, H.; Tamura, J.; Ho, R.C.; Mansur, R.B.; Nasri, F.; Lee, Y.; Rosenblat, J.D.; Wong, E.; et al. The Effect of Loneliness on Distinct Health Outcomes: A Comprehensive Review and Meta-Analysis. Psychiatry Res. 2020, 294, 113514. [Google Scholar] [CrossRef]
- Steptoe, A.; Kivimaki, M. Stress and cardiovascular disease: An update on current knowledge. Annu. Rev. Public Health 2013, 34, 337–354. [Google Scholar] [CrossRef]
- Duggan, M.; Ellison, N.B.; Lampe, C.; Lenhart, A.; Madden, M. Social Media Update 2014. Pew Research Center: Internet Project January Omnibus Survey, January, 2015. Available online: https://www.pewresearch.org/internet/2015/01/09/social-media-update-2014/ (accessed on 4 December 2022).
- Duggan, A., Jr. RLS. Interpersonal Communication in Health and Illness. In Health Behavior Theory, Research, and Practice, 5th ed.; Glanz, K., Rimer, B.K., Viswanath, K., Eds.; Jossey-Bass: SanFrancisco, CA, USA, 2015; pp. 243–267. [Google Scholar]
- Putnam, R. Bowling Alone: The Collapse and Revival of American Community; Simon & Schuster: New York, NY, USA, 2000. [Google Scholar]
- He, Z.; Bian, J.; Carretta, H.J.; Lee, J.; Hogan, W.R.; Shenkman, E.; Charness, N. Prevalence of Multiple Chronic Conditions Among Older Adults in Florida and the United States: Comparative Analysis of the OneFlorida Data Trust and National Inpatient Sample. J. Med. Internet Res. 2018, 20, e137. [Google Scholar] [CrossRef]
- Heidenreich, P.A.; Trogdon, J.G.; Khavjou, O.A.; Butler, J.; Dracup, K.; Ezekowitz, M.D.; Finkelstein, E.A.; Hong, Y.; Johnston, S.J.; Khera, A.; et al. Forecasting the future of cardiovascular disease in the United States: A policy statement from the American Heart Association. Circulation 2011, 123, 933–944. [Google Scholar] [CrossRef] [Green Version]
- Alzheimer’s Association. Alzheimer’s Disease Facts and Figures. 2018. Available online: https://www.alz.org/media/homeoffice/facts%20and%20figures/facts-and-figures.pdf (accessed on 4 December 2022).
- Kowal, S.L.; Dall, T.M.; Chakrabarti, R.; Storm, M.V.; Jain, A. The current and projected economic burden of Parkinson’s disease in the United States. Mov. Disord. Off. J. Mov. Disord. Soc. 2013, 28, 311–318. [Google Scholar] [CrossRef]
- Physical Activity Guidelines Advisory Committee Report, 2008 to the Secretary of Health and Human Services; United States Department of Health and Human Services: Washington, DC, USA, 2008. Available online: https://health.gov/sites/default/files/2019-10/CommitteeReport_7.pdf (accessed on 4 December 2022).
- Exercise Attitudes and Behaviors: A Survey of Midlife and Older Adults; AARP: Washington, DC, USA, 2022; Available online: https://assets.aarp.org/rgcenter/health/exercise.pdf (accessed on 4 December 2022).
- Tudor-Locke, C.; Jones, R.; Myers, A.M.; Paterson, D.H.; Ecclestone, N.A. Contribution of structured exercise class participation and informal walking for exercise to daily physical activity in community-dwelling older adults. Res. Q. Exerc. Sport 2002, 73, 350–356. [Google Scholar] [CrossRef]
- Dunstan, D.W.; Daly, R.M.; Owen, N.; Jolley, D.; Vulikh, E.; Shaw, J.; Zimmet, P. Home-based resistance training is not sufficient to maintain improved glycemic control following supervised training in older individuals with type 2 diabetes. Diabetes Care 2005, 28, 3–9. [Google Scholar] [CrossRef] [Green Version]
- Dunstan, D.W.; Vulikh, E.; Owen, N.; Jolley, D.; Shaw, J.; Zimmet, P. Community center-based resistance training for the maintenance of glycemic control in adults with type 2 diabetes. Diabetes Care 2006, 29, 2586–2591. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schmitz, K.H.; Hannan, P.J.; Stovitz, S.D.; Bryan, C.J.; Warren, M.; Jensen, M.D. Strength training and adiposity in premenopausal women: Strong, healthy, and empowered study. Am. J. Clin. Nutr. 2007, 86, 566–572. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Katz, P.; Julian, L.; Tonner, M.C.; Yazdany, J.; Trupin, L.; Yelin, E.; Criswell, L.A. Physical activity, obesity, and cognitive impairment among women with systemic lupus erythematosus. Arthritis Care Res. 2012, 64, 502–510. [Google Scholar] [CrossRef] [PubMed]
- Napoli, N.; Shah, K.; Waters, D.L.; Sinacore, D.R.; Qualls, C.; Villareal, D.T. Effect of weight loss, exercise, or both on cognition and quality of life in obese older adults. Am. J. Clin. Nutr. 2014, 100, 189–198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Medalia, A.; Revheim, N. Dealing with Cognitive Dysfunction Associaed with Psychiatric Disabilities: A Handbook for Families and Friends of Individuals with Psychiatric Disorders; New York State Office of Mental Health Family Liaison Bureau: New York, NY, USA, 2022. Available online: https://omh.ny.gov/omhweb/cogdys_manual/cogdyshndbk.pdf (accessed on 21 January 2021).




| Weeks 1–3 | Introduction, core component education, technique boot camp, and strength foundation |
| Weeks 4–10 | Incorporation of learned exercises into routines and establishing practical progression benchmarks |
| Weeks 11–16 | Increasing intensity of routines with a focus on high-interval training and appropriate overloading techniques for power and muscle mass |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arguello, D.; Rogers, E.; Denmark, G.H.; Lena, J.; Goodro, T.; Anderson-Song, Q.; Cloutier, G.; Hillman, C.H.; Kramer, A.F.; Castaneda-Sceppa, C.; et al. Companion: A Pilot Randomized Clinical Trial to Test an Integrated Two-Way Communication and Near-Real-Time Sensing System for Detecting and Modifying Daily Inactivity among Adults >60 Years—Design and Protocol. Sensors 2023, 23, 2221. https://doi.org/10.3390/s23042221
Arguello D, Rogers E, Denmark GH, Lena J, Goodro T, Anderson-Song Q, Cloutier G, Hillman CH, Kramer AF, Castaneda-Sceppa C, et al. Companion: A Pilot Randomized Clinical Trial to Test an Integrated Two-Way Communication and Near-Real-Time Sensing System for Detecting and Modifying Daily Inactivity among Adults >60 Years—Design and Protocol. Sensors. 2023; 23(4):2221. https://doi.org/10.3390/s23042221
Chicago/Turabian StyleArguello, Diego, Ethan Rogers, Grant H. Denmark, James Lena, Troy Goodro, Quinn Anderson-Song, Gregory Cloutier, Charles H. Hillman, Arthur F. Kramer, Carmen Castaneda-Sceppa, and et al. 2023. "Companion: A Pilot Randomized Clinical Trial to Test an Integrated Two-Way Communication and Near-Real-Time Sensing System for Detecting and Modifying Daily Inactivity among Adults >60 Years—Design and Protocol" Sensors 23, no. 4: 2221. https://doi.org/10.3390/s23042221
APA StyleArguello, D., Rogers, E., Denmark, G. H., Lena, J., Goodro, T., Anderson-Song, Q., Cloutier, G., Hillman, C. H., Kramer, A. F., Castaneda-Sceppa, C., & John, D. (2023). Companion: A Pilot Randomized Clinical Trial to Test an Integrated Two-Way Communication and Near-Real-Time Sensing System for Detecting and Modifying Daily Inactivity among Adults >60 Years—Design and Protocol. Sensors, 23(4), 2221. https://doi.org/10.3390/s23042221






