1. Introduction
Worldwide, more than 200 million people experience pregnancy annually [
1]. Around 140 million births occur annually. The proportion of births attended by skilled health personnel was less than 81% in 2019 [
2]. Pregnancy is a life stage that involves rapid physiologic and behavioral changes [
3]. During pregnancy, a woman’s lifestyle, behavior, and physical activities can affect her health and that of the fetus [
4]. Hence, constant monitoring is often required if there is risk or complication arises. Pregnancy complications are a severe maternal and infant health risk, leading to adverse outcomes such as miscarriage, preterm birth, stillbirth, and low birth weight [
5]. Around 295,000 women die worldwide due to childbirth complications each year [
2]. There are 23.8 maternal deaths per 100,000 births in the United States and 462 deaths per 100,000 births in low-income countries [
6]. The most common causes of maternal morbidity and mortality are hemorrhage, hypertensive disorders, infection, and sepsis [
7]. Improving maternal health is key to saving the lives of more than half a million women who die each year as a result of complications from pregnancy and childbirth [
8].
There is a clear relationship between lifestyle behaviors, risk factors, and pregnancy complications. Factors affecting maternal health can be external, environmental, risk-based, physical, and behavioral factors [
9]. Careful monitoring of vital signs and physical activities is essential for ensuring the mother’s and fetus’s health and safety during pregnancy. This monitoring is often the first step in the early detection of pregnancy abnormalities and risks, providing an opportunity for prompt and effective intervention to prevent maternal and neonatal morbidity and mortality [
7].
In the traditional medical system, patients make appointments with doctors if symptoms appear and follow their advice until the problem resolves; this is often expensive and time-consuming due to frequent and scheduled visits to the experts [
4,
10]. The current pattern of prenatal care includes 15 face-to-face visits with providers [
11]. The content of these visits includes essential health services, risk assessments, patient education, and the building of trust between patient and provider. In this traditional system, women miss out on important opportunities to monitor and understand their health and the health of their newborns [
11].
With the recent advances in communications and technology, many devices and sensors have been developed to remotely monitor health conditions and track health parameters in daily environments. Wearable sensors, m-health technologies, mobile apps, and other wireless devices such as smartwatches open new possibilities for monitoring behavioral and physiological phenomena [
12,
13,
14]. These devices allow blood glucose level, blood pressure, heart rate, and other biometric data to be consistently measured. The real-time information is then transferred to the healthcare providers. These devices facilitate two-way communication between the doctor and the patient [
15]. In general, identifying physical activity based on wearable sensors is not an easy job and there are many challenges involved. For example, sensor placement on the body affects the physical recognition rate, where a certain physical activity may become more recognizable with sensors worn on specific body parts than others [
4]. Therefore, a clear understanding of sensor principles and proper selection of wearables is essential for effective monitoring.
Several recent research studies have focused on the use of application-specific wearables to monitor maternal health during pregnancy. This review is intended to provide a systematic evaluation of wearable sensors for monitoring maternal health in daily life. The focus is to summarize the effectiveness and limitations of the state-of-the-art methods and to find the scope for future research in this area.
The rest of the paper is organized as follows. First, the review methodology is presented in
Section 2, along with the research questions (RQ) specification.
Section 3 and
Section 4 present a detailed exploration of the review outcome.
Section 5 provides a discussion, and
Section 6 concludes with potential future works.
2. Review Methodology
The goal of this review was to analyze the adequacy of current wearable approaches for monitoring maternal health and fetal conditions and to identify the research gaps in current sensing methodologies. Sensors can be defined as a machine, modules, subsystems, or devices whose purpose is to detect changes and events in the environment [
16]. The current review considers sensors that can collect data, send notifications/alerts (Mobile apps, Smartwatch), ambient sensors (Motion sensors, video camera, microphone), and are those capable of being worn or attached to the body (Belts, suits, wireless and flexible ECG and EEG sensors) as wearable sensors.
The search procedure was conducted according to the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines [
17]. There are several studies that follow PRISMA guidelines for systematic review, such as Imtiaz et al. [
14], Bougea et al. [
18], and Chowdhury et al. [
19]. For this review, we adopted their processes. This methodology used the following four processes: (1) identifying the RQs, (2) recognizing the article sources, (3) searching articles based on the RQs, and (4) analyzing the search outcome.
2.1. Identifying Research Questions
Three research questions (RQs) were chosen to guide this systematic review:
(1) RQ1. What different sensor technologies are employed in prenatal monitoring tasks, how were those sensors placed on body location, and what were the data acquisition processes?
(2) RQ2. How was the acquired data preprocessed regarding noise and artifact removal and prepared for the algorithm development?
(3) RQ3. What specific information was extracted from those sensor signals, how were they extracted, and how was the performance of the sensor evaluated?
2.2. Article Databases Searched
The primary sources for the relevant literature were Google Scholar, IEEE Xplore, MDPI, Science Direct, IOP Science, PubMed, and the ACM Digital library.
Table 1 shows the publication date of the 12 selected articles and their total citations.
2.3. Search Terms
The following free-text search terms were used: ‘wearable sensors’, ‘maternal health’, ‘fetal movement’, ‘fetal heart rate’, and ‘fetal ECG’. The search results were strictly restricted to the English language. The selected full-text articles/references were further analyzed for this review. The selection was further narrowed by applying the eligibility criteria described in
Table 2.
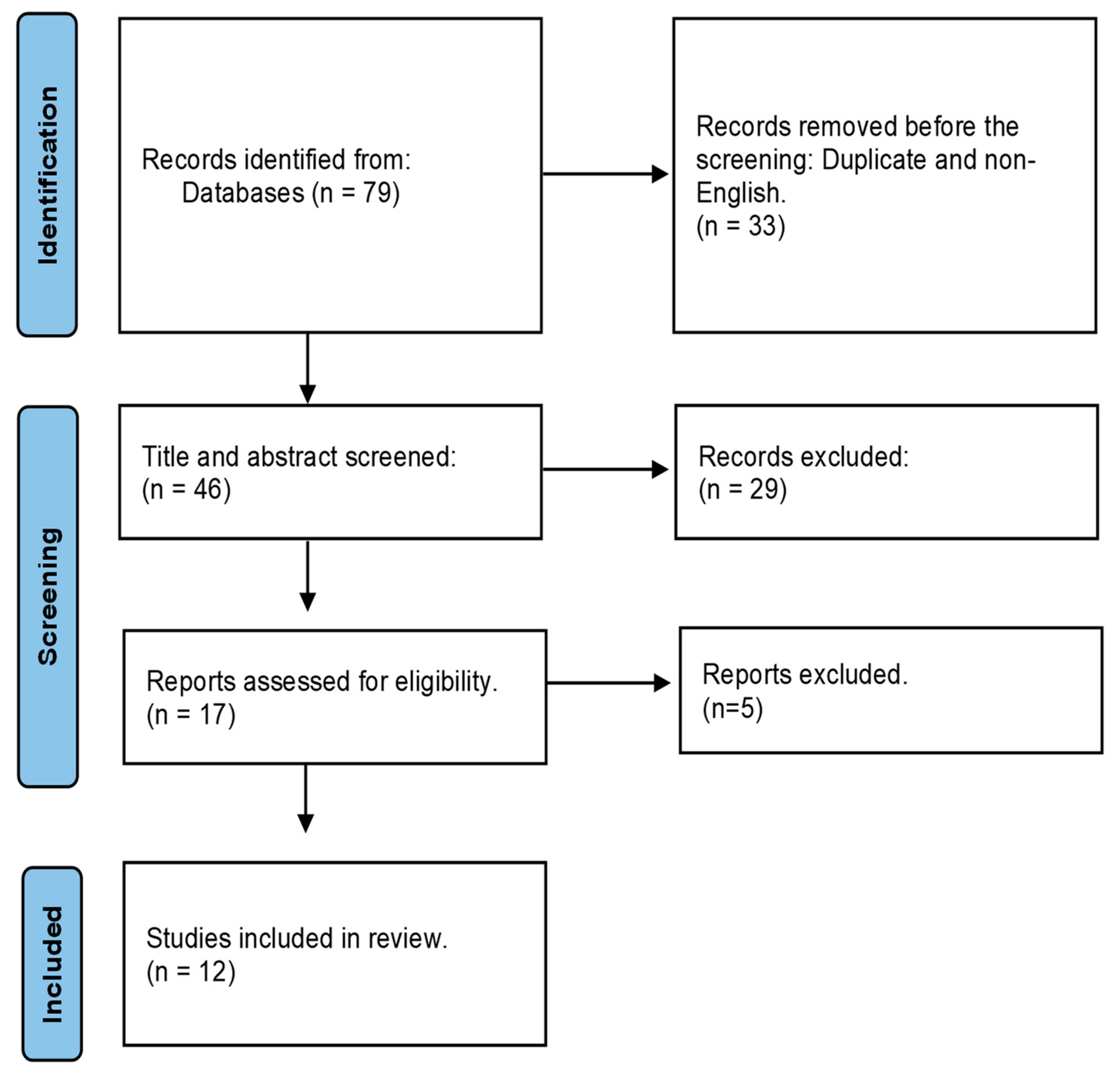
Initially, through the database search, a total of 79 publications were identified, and 46 were chosen for title and abstract screening. 67 articles failed to satisfy the eligibility and were excluded. Finally, 12 articles were selected for the full-text review.
Figure 1 demonstrates the flow diagram of the systematic review strategy.
2.4. Analyzing Review Outcome
A total of 12 publications were found on monitoring fetal and maternal health (including fetal heart rate, fetal movement, maternal physical activities, and stress) using wearable sensors and detecting abnormalities in the early pregnancy stage. The methodologies can broadly be categorized as Seismocardiography (SCG), a technique of measuring the vibrations produced by the beating heart [
29], Gyrocardiography (GCG), a non-invasive technique for assessing heart motions by using a sensor of angular motion–gyroscope–attached to the skin of the chest [
30], FECG (Fetal Electrocardiogram), which is a biomedical signal that gives an electrical representation of FHR (Fetal Heart Rate) to obtain vital information about the condition of the fetus during pregnancy and labor from the recordings on the mother’s body surface [
31], or MECG (Maternal Electrocardiogram), determined by R-R interval and QRS complex measurement of the ECG signal. Fetal position and activity can determine Fetal Movement (FM) and the mother’s heart rate can also indicate the mother’s stress level.
Table 3 outlines the sensor-acquired signals for each study.
4. Data Processing and Algorithm Development
In the comprehensive vital signs monitoring study [
7], the data were filtered by a modified Pan–Tompkins algorithm and the R-peak, which indicates maternal HR, was detected. SpO2 was calculated by filtering the red and infrared channels, detecting peaks, and calculating the pulse amplitudes ratio. RR was recorded using composite chest wall movement data obtained from the x and y-axes of the accelerometer and the ECG signal. Continuous temperature measurements on the chest and limb sensors obtained from direct readings allow the fever curve to be monitored.
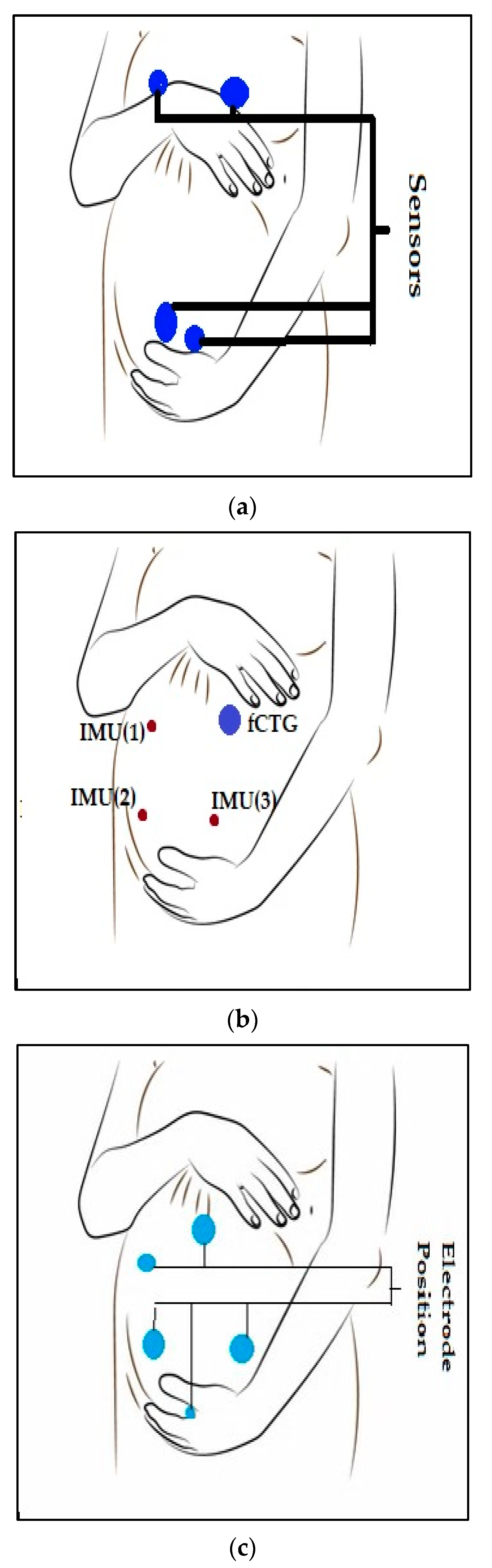
In the fetal heart rate (FHR) detection using seismocardiogram (SCG) and Gyrocardiogram (GCG) study [
24], the readings of the respective axes were first band-pass filtered to focus on the desired frequency components. A zero-phase infinite impulse response (IIR) band-pass filter with cut-off frequencies of 0.8 Hz and 50 Hz was used to pre-filter the SCG waveforms. The observation from GCG was similar to SCG. Therefore, the information from all three sensors was merged to enhance the signal quality of SCG and GCG separately. The preprocessed SCG and GCG signals were converted by CWT with a Morse wavelet [
24].
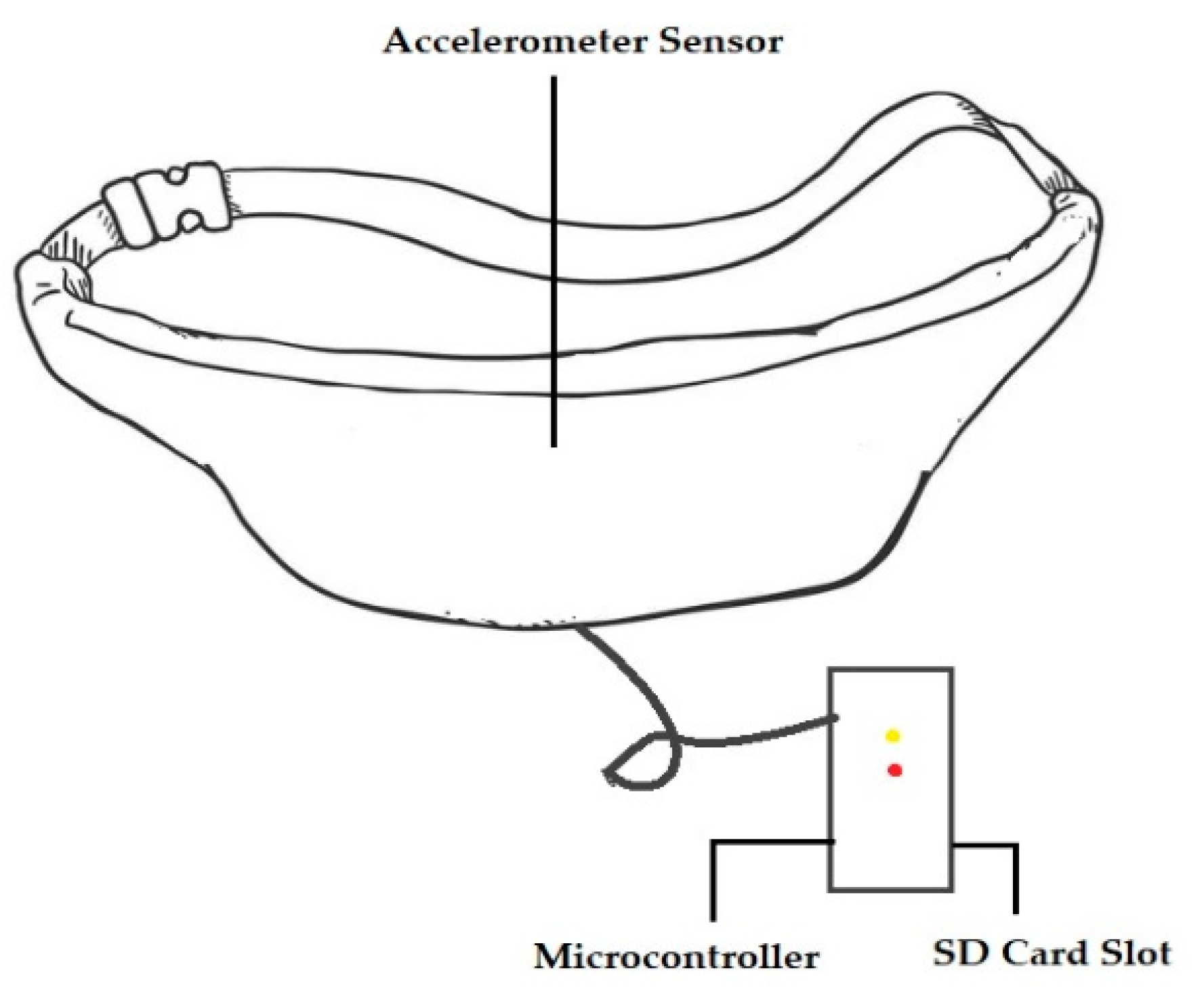
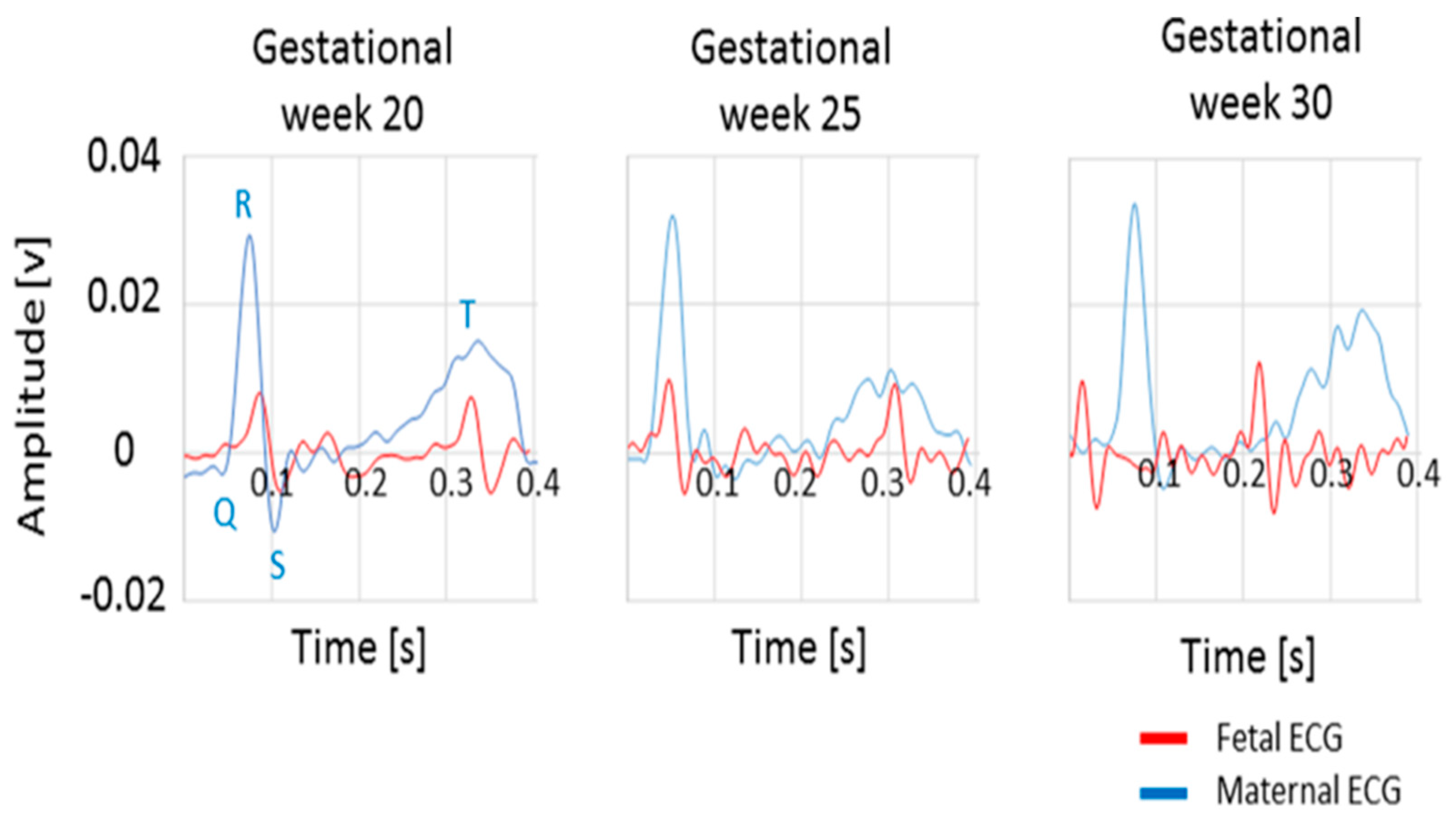
In this study of an electrometer-based amplifier prototype [
59], developed using EPS technology for fECG monitoring, the sensor output voltage was fed to an analog filter with cut-off frequencies of 0.5 Hz and 100 Hz during the amplification stage. This customized version of the sensor was used to record maternal and fetal ECG signals. The low noise levels achieved within the sensor design avoided the use of post-processing stages and allowed visualization of the QRS complex in the raw fetal ECG trace, as shown in
Figure 7 [
20].
The analog output was fed to a commercial National Instruments data acquisition system. The data were acquired using a laptop computer. Display and storage of the data was controlled using a custom-designed graphical interface based on LabVIEW software, including an algorithm for peak detection to determine HR values [
20].
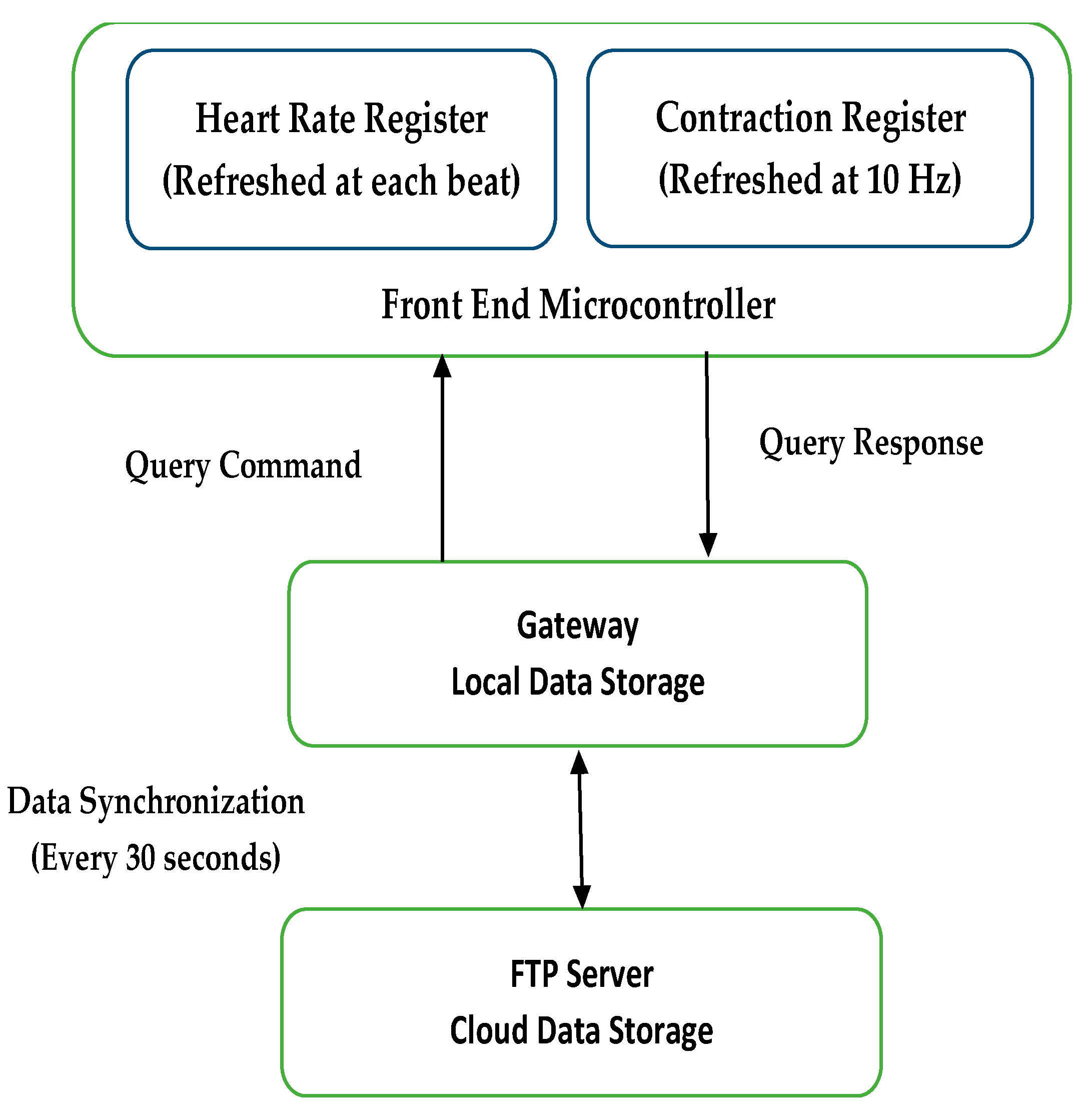
In the study of the toco sensor, an instrumentation amplifier with a gain of 100 amplified the signal to the ADC input range. Further baseline subtraction and gain adjustment were implemented in the gateway software. A gateway was used for local data storage and visualization and to communicate with the mobile data network to transmit data to the server [
21]. Both the wireless gateway and Bluetooth module emitted nonionizing radiation at frequencies ranging from 1 to 2.5 GHz. The FCC limit on the Specific Absorption Rate (SAR), a measure of the rate of energy absorption by the body when exposed to an RF field [
60], for cellular telephones is 1.6 W/kg.
Figure 8 represents various timings for data transmission in the system.
In study [
22], the signal of each channel was divided into six non-overlapping segments (10 s for each segment) and the average of their corresponding SampEn values was returned as the result of the current channel. The signal quality was assessed by comparing the SampEn value in each channel with a constant threshold, that was set to 1.5 for AECG recordings. The average SampEn value was greater than 1.5 for the channels that were regarded as poor quality and subsequently excluded. SampEn less than 1.5 was considered as a good-quality signal and reserved. If less than two channels were of good quality, the two channels with the penultimate and the smallest SampEn values were reserved. The notch filter was applied to remove the power line interference in this work. The combination of the Butterworth filter and median filter was applied to remove baseline drift and impulsive artifacts. The power line interference, baseline drift, and impulsive artifacts of the AECG were mostly removed after the signal noise-canceling step [
22].
Many different types of filters and algorithms were used for data processing in these 12 publications.
Table 7 gives a description of the filters.
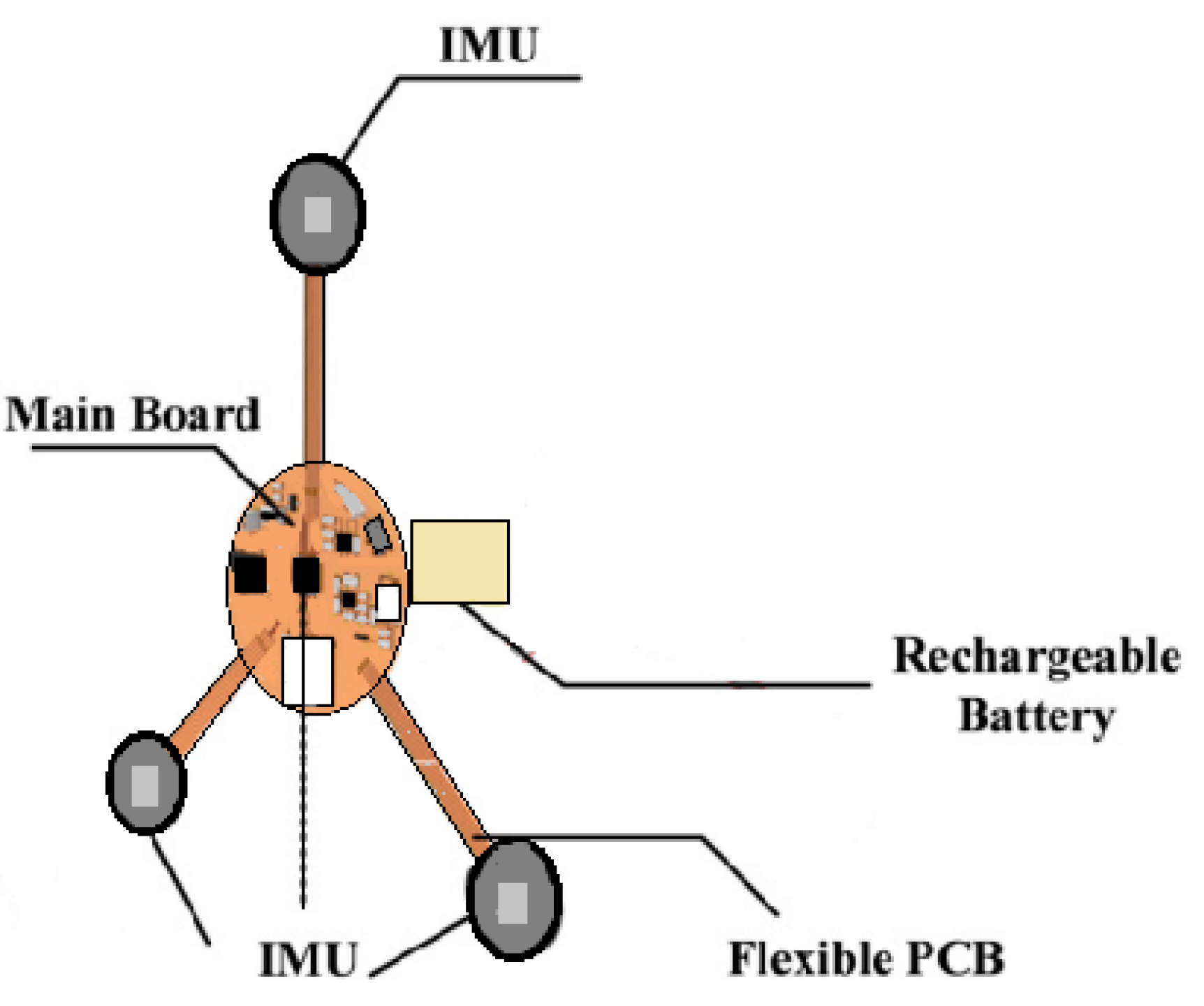
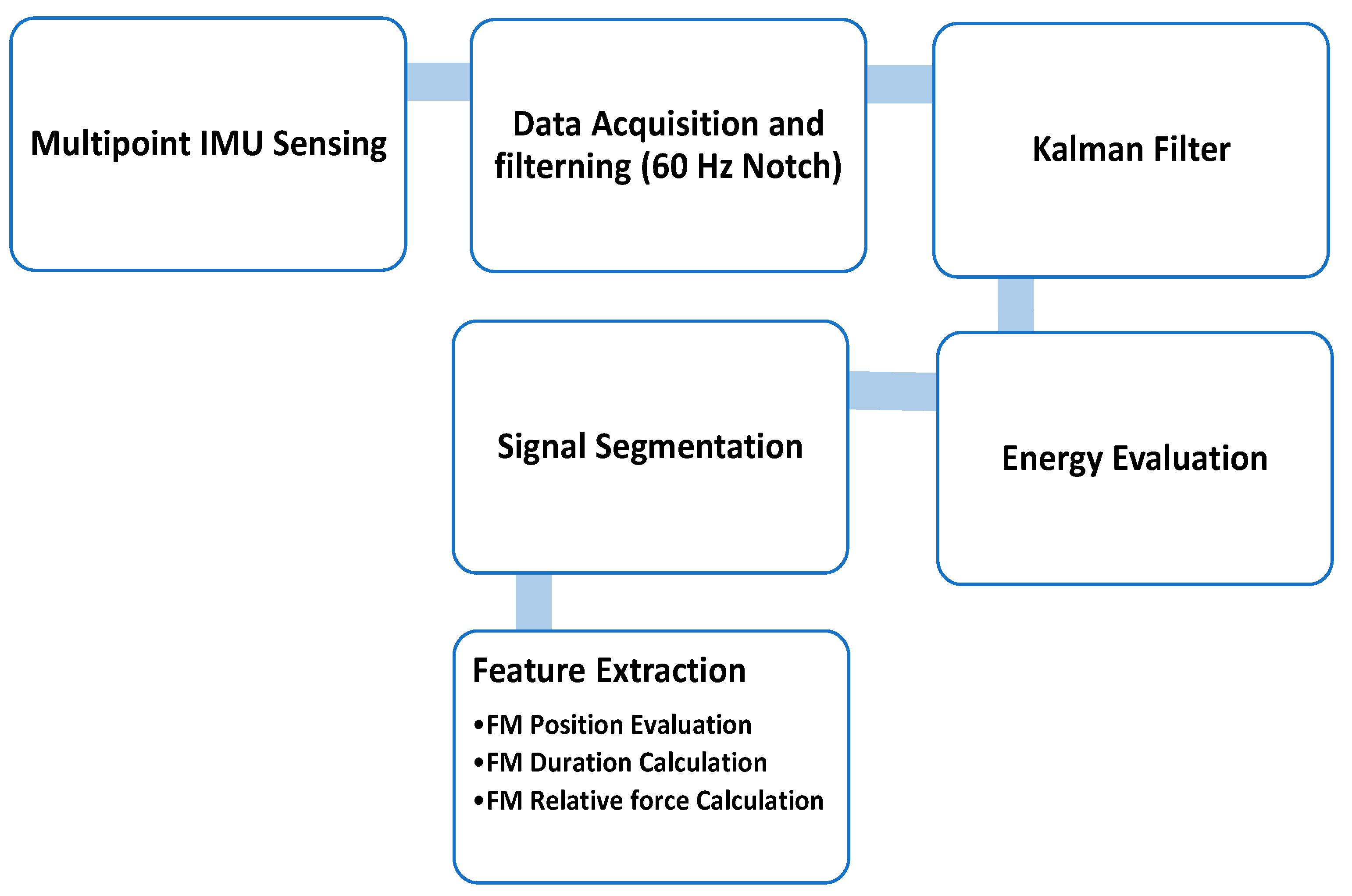
In the IMU sensor study [
25], all the signals received by the IMU went through an Inter-Integrated Circuit, the hardware filter filtered out the 60 Hz noise, and the data were sent to the MCU. The signals from various channels were processed by a Kalman filter to reduce noise and then the position, duration, and Relative Force (RF) of the fetal movement were determined from the signal interval generated by the energy evaluation [
25]. The process of the software is shown in
Figure 9.
Three main features were extracted from the signal to analyze fetal movement [
25]:
In the duo accelerometer study [
26], the denoising process was applied. The model was set as the baseline of the data and subtracted from raw data to remove 0 Hz noise. The Wavelet denoising tool, ‘denoise,’ with the specific parameters ‘Wavelet’, ‘sym2’, ‘Denoising Method’, BlockJS’, ‘NoiseEstimate’, ‘LevelIndpendent’ in MATLAB, was applied. Another tool, ‘hampel’, was applied to detect and remove outliers [
23,
59].
After analyzing the fetal movement waveform, three main groups of features (statistical, morphological, and wavelet features) were selected. Minimum, maximum, standard deviation, mean, and median common statistical features were extracted. Absolute area, relative area, absolute area of the differential, entropy, and kurtosis were also extracted. The ‘Haar’ wavelet was used to decompose the data and extract the approximate coefficients of the discrete wavelet transform. The mean, median, and standard deviation of the wavelet transform were also selected as features for classification. Since each axis had 13 features, the total number of features was 78 [
26].
Predictive models to map X to Y were built using a convolution neural network. The Convolutional Neural Network (CNN) architecture was adopted from [
63].
In the PAR study [
4], two different window sizes (one second and two seconds) and two configurations (overlapping and non-overlapping) were selected. In the one-second window size, the 0.5 s. Mean, SD (Standard Deviation), cosine similarity, RMS (Root Mean Square), Skewness, Kurtosis, Max value, Min value, Frequency Domain Features, Entropy, Zero Crossing, Quartile Range, and Absolute Time Difference between Peaks features were extracted from the data. A total of 43 features were used to represent the sensor data. K-Nearest Neighbors, Decision Tree, Random Forest, Induction rules, and Gradient boosted trees classifiers were used on the proposed MPAR system. Each classifier follows the general rule of supervised machine learning algorithms, where the classifier parameters are trained with the help of a training set and then its classification/recognition performance is evaluated with a completely disjoint test set. The dataset of this study is available upon request [
4].
Table 8 depicts the sensors or devices that were used for monitoring maternal or fetal health. The number of participants in each study and the sensors’ communication technology is also shown.
5. Discussion
This study provides a systematic review of the existing wearable sensors for monitoring maternal health during pregnancy. This review analyzes all twelve available research articles describing wearable sensors and maternal and fetal health. It focuses on three research questions: different sensors module, preprocessing of the signal, and recognition or detection method.
Table 7 and
Table 8 give a summary of the employed sensors and data-obtaining methods.
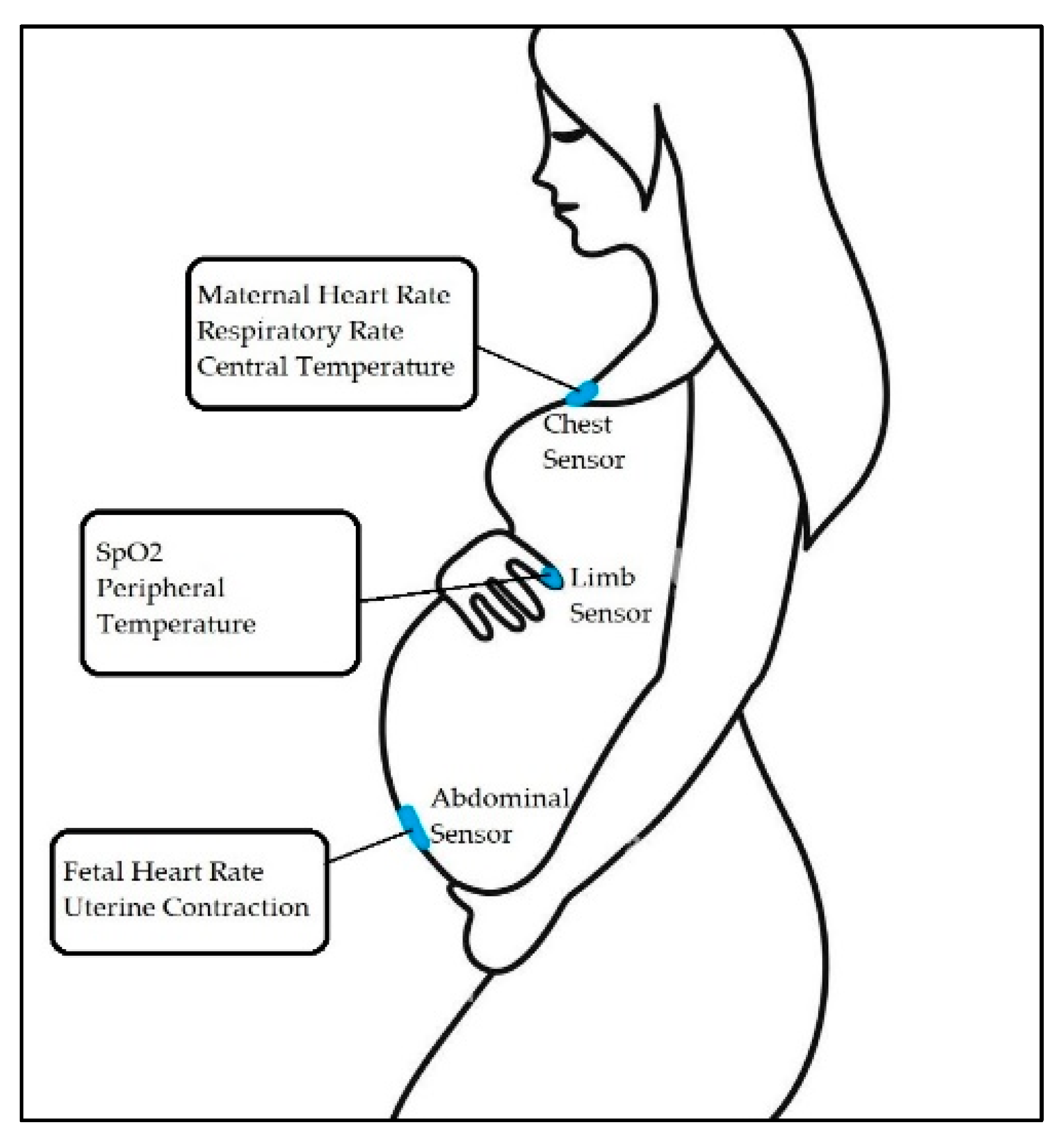
For measuring FECG and FHR-ESP, Toco, prototype, or commercial sensors were used [
7,
20,
21,
22,
23,
24]. These sensors were placed on the abdominal wall and chest of the mother to measure MECG. Maternal heart rate was calculated to determine the stress level. IMU sensors and accelerometer sensors were used to measure fetal movement [
25,
26,
27]. Limb sensors and wearable sensor modules on the wrist measured the mother’s body temperature and physical activities [
4,
7]. The data collected through these sensors were connected to smartphones and laptops, helping to display and store the data.
Data collection time was different for different methodologies. For studies [
25,
26,
27], data collection for fetal movement detection was 1 h, 30 min, and 20 min respectively. For FECG and MECG recording, the participants had to remain in certain positions to ensure uninterrupted recording [
21,
22]. For [
20,
22,
24], the recording was 30 s, 7 min, and 15 min respectively. The data collection was carried out during different stages of pregnancy, with no subject monitored throughout the whole pregnancy period.
Filtering is found to be required to remove external noise or artifacts. Most research studies used a notch filter to remove the power line noise [
65] and an FIR or IIR filter to remove the artifact from the signal. Some devices have built-in filters and so they do not need to perform filtering externally. The study [
23] developed a board employing a microcontroller, sensors, and a shield. This board performs the further processing of the FECG signal after acquiring the signals. In ref. [
20], the study developed a prototype device that amplifies the fetal ECG signal and performs the analog filtering. The other studies primarily use commercially available sensors and perform the data processing and filtering in MATLAB, LabVIEW, Raspberry-PI, and other software. This section also covers the feature extraction methods. Most relevant features were extracted from the data before proceeding to the next step.
Table 6 gives an idea about the extracted features in these studies.
These studies used machine learning and deep learning methods to evaluate or detect the signal.
Table 9 shows the pre-processing methods and performance of the research analysis.
From
Table 8, we can see that only 3 of the studies achieved an accuracy above 90% [
22,
25,
28]. After reviewing the articles, we can propose that further work and development are needed in the field of wearable sensors for monitoring the health of pregnant women. All the wearable sensors mentioned in the articles used in monitoring were tested in a lab environment or clinical trial. Furthermore, the monitoring processes carried out in the papers reviewed here were conducted for a limited time and only during a certain gestational period. The number of participants is also limited and more rigorous testing is required [
4,
7,
20,
21,
22,
23,
24,
25,
26,
27,
28]. Only in study [
7] were bandage sensors implemented; these are more flexible than other sensors. Some pregnant women expressed discomfort wearing these sensors [
25]. Maternal physical activity recognition was conducted for only ten activities [
4]. For continuous monitoring during daily activities throughout the whole pregnancy, there will be many motion artifacts in the acquired signal. These are hard to recognize and remove.
Table 10 describes the pros and cons of the sensor modalities used in the studies.
The sensors or devices used in these studies are safe for both mother and their child and most are commercially available. None of the studies claim any risk in using their sensors for monitoring fetal or mother health. The experiments were supervised by professional doctors [
21,
23,
24,
25]. The subject experimental protocol of studies [
3,
4,
22,
26,
27,
28] were approved by the Ethics Committee. However, it is not mentioned whether these sensors were FDA-approved or not, and no conclusive statement was provided on how rigorously testing was performed by an independent reviewer or institution.
Future work in this field will be focused on developing sensors for continuous monitoring throughout the pregnancy period. The primary focus will be to develop a sensor that can detect any abnormalities in fetal ECG or movement in real-time and give feedback or alert to the patients and the doctor so that the necessary steps can be taken in time and any further complications can be avoided. More flexible sensors, such as the bandage sensors used in the article [
7], need to be developed; they will be more convenient and comfortable for pregnant women. There is a need to increase the number of participants for more accurate results. Addressing the limitations and issues of the wearable device will lead to more opportunities to develop wearable sensors, thereby leading the way in commercializing the sensors.
6. Conclusions
In this systematic review, we focus on three major research questions, including the sensor’s description and processing, data preprocessing, and performance. The existing sensors were thoroughly examined in this review, and their limitation and future scope were identified. The sensors used in these articles help to monitor maternal health (monitoring MECG, body temperature, and stress level) as well as fetal health (FECG, FM). In the study, we found that pregnant women considered wearing a mobile sensor and reported no privacy concerns. According to Runkle et al., seven in ten women agreed to change their behavior or lifestyle during pregnancy after receiving recommendations or messages from a smartphone through wearable sensors. Most of the studies we mentioned applied Machine Learning and Deep Learning methods to the pre-processed signal to detect or evaluate the performance. The accuracy in these studies was around 80% to 90%, which is acceptable according to the articles. So, we can state that wearable sensors significantly contribute to maternal health during pregnancy. Although there is demand and need for wearable healthcare monitors or sensors, there are still some limitations and challenges. Improving accuracy, testing in free-living conditions, enhancing the comfort level of wearable sensors, and continuous and longitudinal monitoring requires the further development of wearable sensors and devices. If these challenges can be addressed, wearable sensors may substantially contribute to reducing the mortality rate due to pregnancy complications or other maternal health issues.