Quantifying States and Transitions of Emerging Postural Control for Children Not Yet Able to Sit Independently
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
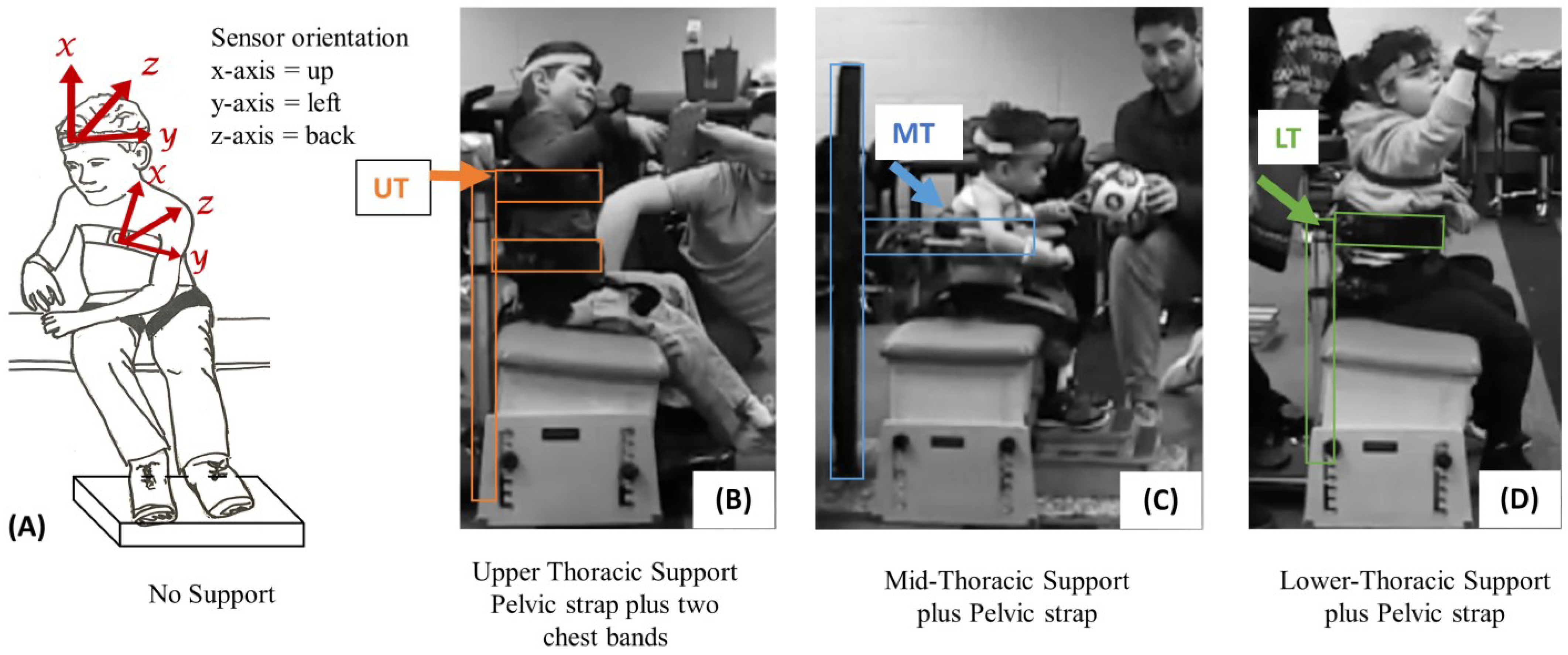
2.2. Experimental Methods
2.3. Algorithm Development
2.4. Data Processing
3. Results
4. Discussion
4.1. Limitations
4.2. Future Studies
5. Clinical and Research Relevance
6. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rosenbaum, P.L.; Walter, S.D.; Hanna, S.E.; Palisano, R.J.; Russell, D.J.; Raina, P.; Wood, E.; Bartlett, D.J.; Galuppi, B.E. Prognosis for Gross Motor Function in Cerebral Palsy: Creation of Motor Development Curves. JAMA J. Am. Med. Assoc 2003, 288, 1357–1363. [Google Scholar] [CrossRef] [Green Version]
- Hanna, S.E.; Rosenbaum, P.L.; Bartlett, D.J.; Palisano, R.J.; Walter, S.D.; Avery, L.; Russell, D.J. Stability and decline in gross motor function among children and youth with cerebral palsy aged 2 to 21 years. Dev. Med. Child Neurol. 2009, 51, 295–302. [Google Scholar] [CrossRef]
- Beckung, E.; Hagberg, G.; Uldall, P.; Cans, C.; Europe, F.S.O.C.P.I. Probability of Walking in Children with Cerebral Palsy in Europe. Pediatrics 2008, 121, e187–e192. [Google Scholar] [CrossRef] [Green Version]
- Cloake, T.; Gardner, A. The management of scoliosis in children with cerebral palsy: A review. J. Spine Surg. 2016, 2, 299–309. [Google Scholar] [CrossRef] [Green Version]
- Soo, B.; Howard, J.J.; Boyd, R.N.; Reid, S.M.; Lanigan, A.; Wolfe, R.; Graham, H.K. Hip displacement in cerebral palsy. J. Bone Jt. Surg. 2006, 88A, 121–129. [Google Scholar]
- Henderson, R.C.; Kairalla, J.; Abbas, A.; Stevenson, R.D. Predicting low bone density in children and young adults with quadriplegic cerebral palsy. Dev. Med. Child Neurol. 2004, 46, 416–419. [Google Scholar] [CrossRef]
- Henderson, R.C. Bone density and other possible predictors of fracture risk in children and adolescents with spastic quadri-plegia. Dev. Med. Child Neurol. 1997, 39, 224–227. [Google Scholar] [CrossRef]
- Da Silva, D.C.G.; da Cunha, M.D.S.B.; de Oliveira Santana, A.; dos Santos Alves, A.M.; Santos, M.P. Malnutrition and nutritional deficiencies in children with cerebral palsy: A systematic review and meta-analysis. Public Health 2022, 205, 192–201. [Google Scholar] [CrossRef]
- Boel, L.; Pernet, K.; Toussaint, M.; Ides, K.; Leemans, G.; Haan, J.; Van Hoorenbeeck, K.; Verhulst, S. Respiratory morbidity in children with cerebral palsy: An overview. Dev. Med. Child Neurol. 2019, 61, 646–653. [Google Scholar] [CrossRef]
- Marpole, R.; Blackmore, A.M.; Gibson, N.; Cooper, M.S.; Langdon, K.; Wilson, A.C. Evaluation and Management of Respiratory Illness in Children With Cerebral Palsy. Front. Pediatr. 2020, 8, 333. [Google Scholar] [CrossRef]
- Blackmore, A.M.; Bear, N.; Blair, E.; Gibson, N.; Jalla, C.; Langdon, K.; Moshovis, L.; Steer, K.; Wilson, A.C. Factors Associated with Respiratory Illness in Children and Young Adults with Cerebral Palsy. J. Pediatr. 2016, 168, 151–157.e1. [Google Scholar] [CrossRef]
- McInnes, E.; Jammali-Blasi, A.; Bell-Syer, S.E.; Dumville, J.C.; Middleton, V.; Cullum, N. Support surfaces for pressure ulcer prevention. Cochrane Database Syst. Rev. 2015, 2015, CD001735. [Google Scholar] [CrossRef] [Green Version]
- Schlüer, A.-B.; Schols, J.M.G.A.; Halfens, R.J.G. Pressure Ulcer Treatment in Pediatric Patients. Adv. Ski. Wound Care 2013, 26, 504–510. [Google Scholar] [CrossRef]
- Lieber, R.L.; Fridén, J. Muscle contracture and passive mechanics in cerebral palsy. J. Appl. Physiol. 2019, 126, 1492–1501. [Google Scholar] [CrossRef]
- Hägglund, G.; Andersson, S.; Düppe, H.; Pedertsen, H.L.; Nordmark, E.; Westbom, L. Prevention of severe contractures might replace multilevel surgery in cerebral palsy: Results of a population-based health care programme and new techniques to reduce spasticity. J. Pediatr. Orthop. B 2005, 14, 269–273. [Google Scholar] [CrossRef]
- Davids, J.R. Management of Neuromuscular Hip Dysplasia in Children with Cerebral Palsy: Lessons and Challenges. J. Pediatr. Orthop. 2018, 38, S21–S27. [Google Scholar] [CrossRef]
- Imms, C.; Reilly, S.; Carlin, J.; Dodd, K.J. Characteristics influencing participation of Australian children with cerebral palsy. Disabil. Rehabil. 2009, 31, 2204–2215. [Google Scholar] [CrossRef]
- Harbourne, R.T.; Deffeyes, J.E.; Kyvelidou, A.; Stergiou, N. Complexity of postural control in infants: Linear and nonlinear features revealed by principal component analysis. Nonlinear Dyn. Psychol. Life Sci. 2009, 13, 123–144. [Google Scholar]
- Harbourne, R.T.; Stergiou, N. Nonlinear analysis of the development of sitting postural control. Dev. Psychobiol. 2003, 42, 368–377. [Google Scholar] [CrossRef]
- Hedberg, Å.; Carlberg, E.B.; Forssberg, H.; Hadders-Algra, M. Development of postural adjustments in sitting position during the first half year of life. Dev. Med. Child Neurol. 2005, 47, 312–320. [Google Scholar] [CrossRef]
- Brogren, E.; Hadders-Algra, M.; Forssberg, H. Postural Control in Sitting Children with Cerebral Palsy. Neurosci. Biobehav. Rev. 1998, 22, 591–596. [Google Scholar] [CrossRef]
- Chen, L.C.; Metcalfe, J.S.; Chang, T.Y.; Jeka, J.J.; Clark, J.E. The development of infant upright posture: Sway less or sway differently? Exp. Brain Res. 2008, 186, 293–303. [Google Scholar] [CrossRef]
- Russell, D.J.; Rosenbaum, P.L.; Cadman, D.T.; Gowland, C.; Hardy, S.; Jarvis, S. The gross motor function measure—A means to evaluate the effects of physical therapy. Dev. Med. Child Neurol. 1989, 31, 341–352. [Google Scholar] [CrossRef]
- Wang, H.-H.; Liao, H.-F.; Hsieh, C.-L. Reliability, sensitivity to change, and responsiveness of the Peabody Developmental Motor Scales—Second edition for children with cerebral palsy. Phys. Ther. 2006, 86, 1351–1359. [Google Scholar] [CrossRef] [Green Version]
- Pousada, M.; Guillamón, N.; Hernández-Encuentra, E.; Munoz, E.; Redolar, D.; Boixadós, M.; Gómez-Zúñiga, B.; Redolar-Ripoll, D. Impact of Caring for a Child with Cerebral Palsy on the Quality of Life of Parents: A Systematic Review of the Literature. J. Dev. Phys. Disabil. 2013, 25, 545–577. [Google Scholar] [CrossRef]
- Butler, P.; Saavedra, M.S.; Sofranac, M.M.; Jarvis, M.S.; Woollacott, M. Refinement, Reliability, and Validity of the Segmental Assessment of Trunk Control (SATCo). Pediatr. Phys. Ther. 2010, 22, 246–257. [Google Scholar] [CrossRef] [Green Version]
- Woollacott, M.H.; Shumway-Cook, A. Changes in Posture Control Across the Life Span—A Systems Approach. Phys. Ther. 1990, 70, 799–807. [Google Scholar] [CrossRef] [Green Version]
- Assaiante, C.; Amblard, B. An Ontogenic Model for the Sensorimotor Organization of Balance Control in Humans. Dev. Med. Child Neurol. 1995, 14, 13–43. [Google Scholar]
- Novak, I.; McIntyre, S.; Morgan, C.; Campbell, L.; Dark, L.; Morton, N.; Stumbles, E.; Wilson, S.-A.; Goldsmith, S. A systematic review of interventions for children with cerebral palsy: State of the evidence. Dev. Med. Child Neurol. 2013, 55, 885–910. [Google Scholar] [CrossRef]
- Novak, I.; Morgan, C.; Fahey, M.; Finch-Edmondson, M.; Galea, C.; Hines, A.; Langdon, K.; Mc Namara, M.; Paton, M.C.; Popat, H.; et al. State of the Evidence Traffic Lights 2019: Systematic Review of Interventions for Preventing and Treating Children with Cerebral Palsy. Curr. Neurol. Neurosci. Rep. 2020, 20, 3. [Google Scholar] [CrossRef] [Green Version]
- Prieto, T.; Myklebust, J.; Hoffmann, R.; Lovett, E.; Myklebust, B. Measures of postural steadiness: Differences between healthy young and elderly adults. IEEE Trans. Biomed. Eng. 1996, 43, 956–966. [Google Scholar] [CrossRef]
- Goodworth, A.; Saavedra, S. Postural mechanisms in moderate-to-severe cerebral palsy. J. Neurophysiol. 2021, 125, 1698–1719. [Google Scholar] [CrossRef]
- Peterka, R.J. Sensorimotor Integration in Human Postural Control. J. Neurophysiol. 2002, 88, 1097–1118. [Google Scholar] [CrossRef] [Green Version]
- Spain, R.I.; Mancini, M.; Horak, F.B.; Bourdette, D. Body-worn sensors capture variability, but not decline, of gait and balance measures in multiple sclerosis over 18 months. Gait Posture 2014, 39, 958–964. [Google Scholar] [CrossRef] [Green Version]
- Forssberg, H.; Hadders-Algra, M. Postural adjustments due to external perturbations during sitting in 1-month-old infants: Evidence for the innate origin of direction specificity. Exp. Brain Res. 2004, 157, 10–17. [Google Scholar] [CrossRef]
- Chen, L.-C.; Metcalfe, J.S.; Jeka, J.J.; Clark, J.E. Two steps forward and one back: Learning to walk affects infants’ sitting posture. Infant Behav. Dev. 2007, 30, 16–25. [Google Scholar] [CrossRef]
- Bertenthal, B.I.; Bai, D.L. Infants Sensitivity to Optical-Flow for Controlling Posture. Dev. Psychol. 1989, 25, 936–945. [Google Scholar] [CrossRef]
- Woollacott, M.; Debu, B.; and Mowatt, M. Neuromuscular Control of Posture in the Infant and Child—Is Vision Dominant. J. Mot. Behav. 1987, 19, 167–186. [Google Scholar] [CrossRef]
- Saavedra, S.L.; Van Donkelaar, P.; Woollacott, M.H. Learning about gravity: Segmental assessment of upright control as infants develop independent sitting. J. Neurophysiol. 2012, 108, 2215–2229. [Google Scholar] [CrossRef]
- Saavedra, S.L.; Woollacott, M.H. Segmental Contributions to Trunk Control in Children with Moderate-to-Severe Cerebral Palsy. Arch. Phys. Med. Rehabil. 2015, 96, 1088–1097. [Google Scholar] [CrossRef] [Green Version]
- Goodworth, A.D.; Wu, Y.-H.; Felmlee, D.; Dunklebarger, E.; Saavedra, S. A Trunk Support System to Identify Posture Control Mechanisms in Populations Lacking Independent Sitting. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 25, 22–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Da Costa, C.S.N.; Saavedra, S.L.; Rocha, N.A.C.F.; Woollacott, M.H. Effect of Biomechanical Constraints on Neural Control of Head Stability in Children with Moderate to Severe Cerebral Palsy. Phys. Ther. 2017, 97, 374–385. [Google Scholar] [CrossRef] [Green Version]
- Hanna, S.E.; Bartlett, D.J.; Rivard, L.M.; Russell, D.J. Reference Curves for the Gross Motor Function Measure: Percentiles for Clinical Description and Tracking Over Time Among Children with Cerebral Palsy. Phys. Ther. 2008, 88, 596–607. [Google Scholar] [CrossRef]
- Palisano, R.; Rosenbaum, P.; Walter, S.; Russell, D.; Wood, E.; Galuppi, B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev. Med. Child Neurol. 2008, 39, 214–223. [Google Scholar] [CrossRef]
- Vitrikas, K.; Dalton, H.; Breish, D. Cerebral Palsy: An Overview. Am. Fam. Physician 2020, 101, 213–220. [Google Scholar]
- Cans, C.; Dolk, H.; Platt, M.J.; Colver, A.; Prasauskene, A.; Rägeloh-Mann, I.K. Recommendations from the SCPE collaborative group for defining and classifying cerebral palsy. Dev. Med. Child Neurol. 2007, 49, 35–38. [Google Scholar] [CrossRef]
- Jethwa, A.; Mink, J.; MacArthur, C.; Knights, S.; Fehlings, T.; Fehlings, D. Development of the Hypertonia Assessment Tool (HAT): A discriminative tool for hypertonia in children. Dev. Med. Child Neurol. 2010, 52, e83–e87. [Google Scholar] [CrossRef]
- Rachwani, J.; Santamaria, V.; Saavedra, S.L.; Wood, S.; Porter, F.; Woollacott, M.H. Segmental trunk control acquisition and reaching in typically developing infants. Exp. Brain Research. Exp. Hirnforschung. Exp. Cereb. 2013, 228, 131–139. [Google Scholar] [CrossRef] [Green Version]
- Rachwani, J.; Santamaria, V.; Saavedra, S.L.; Woollacott, M.H. The development of trunk control and its relation to reaching in infancy: A longitudinal study. Front. Hum. Neurosci. 2015, 9, 94. [Google Scholar]
- Santamaria, V.; Rachwani, J.; Saavedra, S.; Woollacott, M. Effect of Segmental Trunk Support on Posture and Reaching in Children with Cerebral Palsy. Pediatr. Phys. Ther. 2016, 28, 285–293. [Google Scholar] [CrossRef] [Green Version]
- Saavedra, S.L.; Goodworth, A.D. Postural Control in Children and Youth with Cerebral Palsy. In Cerebral Palsy; Miller, F., Bachrach, S., Lennon, N., O’Neil, M., Eds.; Springer International Publishing: Cham, Switzerland, 2019; pp. 1–21. [Google Scholar]
- Peterka, R.J.; Loughlin, P.J. Dynamic Regulation of Sensorimotor Integration in Human Postural Control. J. Neurophysiol. 2004, 91, 410–423. [Google Scholar] [CrossRef] [Green Version]
- Russell, D.J.; Avery, L.M.; Rosenbaum, P.L.; Raina, P.S.; Walter, S.D.; Palisano, R.J. Improved Scaling of the Gross Motor Function Measure for Children with Cerebral Palsy: Evidence of Reliability and Validity. Phys. Ther. 2000, 80, 873–885. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Russell, D.J.; Avery, L.; Walter, S.D.; Hanna, S.E.; Bartlett, D.J.; Rosenbaum, P.L.; Palisano, R.J.; Gorter, J.W. Development and validation of item sets to improve efficiency of administration of the 66-item Gross Motor Function Measure in children with cerebral palsy. Dev. Med. Child Neurol. 2010, 52, e48–e54. [Google Scholar] [CrossRef] [PubMed]
- Smith, B.A.; Trujillo-Priego, I.A.; Lane, C.J.; Finley, J.M.; Horak, F.B. Daily Quantity of Infant Leg Movement: Wearable Sensor Algorithm and Relationship to Walking Onset. Sensors 2015, 15, 19006–19020. [Google Scholar] [CrossRef] [Green Version]
- Franchak, J.M.; Scott, V.; Luo, C. A Contactless Method for Measuring Full-Day, Naturalistic Motor Behavior Using Wearable Inertial Sensors. Front. Psychol. 2021, 12, 701343. [Google Scholar] [CrossRef] [PubMed]
- Saboor, A.; Kask, T.; Kuusik, A.; Alam, M.M.; Le Moullec, Y.; Niazi, I.K.; Zoha, A.; Ahmad, R. Latest Research Trends in Gait Analysis Using Wearable Sensors and Machine Learning: A Systematic Review. IEEE Access 2020, 8, 167830–167864. [Google Scholar] [CrossRef]
- Peake, J.M.; Kerr, G.; Sullivan, J.P. A Critical Review of Consumer Wearables, Mobile Applications, and Equipment for Providing Biofeedback, Monitoring Stress, and Sleep in Physically Active Populations. Front. Physiol. 2018, 9, 743. [Google Scholar] [CrossRef] [PubMed]
- Brogioli, M.; Popp, W.L.; Schneider, S.; Albisser, U.; Brust, A.K.; Frotzler, A.; Gassert, R.; Curt, A.; Starkey, M.L. Multi-Day Recordings of Wearable Sensors Are Valid and Sensitive Measures of Function and Independence in Human Spinal Cord Injury. J. Neurotrauma 2017, 34, 1141–1148. [Google Scholar] [CrossRef]
- Schneider, S.; Popp, W.L.; Brogioli, M.; Albisser, U.; Demkó, L.; Debecker, I.; Velstra, I.-M.; Gassert, R.; Curt, A. Reliability of Wearable-Sensor-Derived Measures of Physical Activity in Wheelchair-Dependent Spinal Cord Injured Patients. Front. Neurol. 2018, 9, 1039. [Google Scholar] [CrossRef] [Green Version]
- Rast, F.M.; Labruyère, R. Systematic review on the application of wearable inertial sensors to quantify everyday life motor activity in people with mobility impairments. J. Neuroeng. Rehabil. 2020, 17, 125. [Google Scholar] [CrossRef]
- Adolph, K.E.; Cole, W.G.; Komati, M.; Garciaguirre, J.S.; Badaly, D.; Lingeman, J.M.; Chan, G.L.Y.; Sotsky, R.B. How Do You Learn to Walk? Thousands of Steps and Dozens of Falls per Day. Psychol. Sci. 2012, 23, 1387–1394. [Google Scholar] [CrossRef] [PubMed] [Green Version]












| ID | Age (Years) | Gestational Age (Weeks) | Sex | Etiology | Diagnosis | SATCo Level | GMFCS Level | HAT |
|---|---|---|---|---|---|---|---|---|
| 01DK | 5.5 | 31 | Male | Intrauterine asphyxia Apgar 4, respiratory insufficiency, hydrocephalus post hemorrhagic, cerebral ventricle leukomalacia, hyperbilirubinemia | Prematurity, spastic bilateral CP | Mid Thoracic | V | spasticity |
| 02KJ | 3.5 | 25 | Male | Unknown | CP | Mid Thoracic | IV | spasticity |
| 03JP | 1.9 | 34 | Male | Stopped moving in utero | Prematurity | Mid Thoracic | IV | spasticity |
| 04SD | 4.8 | 34 | Female | Three small bleeds in the brainstem, apnea, low Apgar score | Prematurity, bilateral sensorineural hearing loss, dyskinetic CP | Upper Thoracic | V | dystonia |
| 05BS | 5 | 40 | Male | Agenesis of corpus callosum | CP | Upper Thoracic | IV | spasticity |
| 06ML | 13 | Overdue | Male | Unknown | Athetoid CP with dystonic movements | Upper Thoracic | V | dystonia |
| 07WB | 13 | 33 | Male | Schizencephaly | CP | Lower Thoracic | IV | spasticity |
| 08AC | 7 | 23 | Female | Ischemic brain injury to cerebellum, bilateral intraventricular hemorrhage (IVH) | CP | Lower Thoracic | IV | hypotonia ataxia |
| Behavior | Functional Description |
|---|---|
| Trunk Upright | The trunk (T) is considered upright if it is within a cone with respect to the vertical axis. |
| Head Upright | The head (H) is considered upright if it is within a cone with respect to the trunk axis. |
| Trunk Stationary | The trunk was considered stationary at any given time if there was small variation of movement in both the ML and AP directions for an interval leading up to the current time. (Variance over 1 s < 10°) |
| Trunk Angle Magnitude Increasing/Decreasing/Stable | The trunk was considered to have its angle magnitude increasing or decreasing if the angular speed in the most prominent direction (ML or AP) was large. It was increasing if the angle magnitude was positive and decreasing if the velocity was negative. (Stable if slope of best fit line over 1 s < 5°/s) |
| Next State | |||||||
|---|---|---|---|---|---|---|---|
| Stable | Head | Wobble | Rise | Fall | Collapse | ||
| Current State | Stable | 0 | 1 | 2 | 0 | 1 | 0 |
| Head | 0 | 15 | 11 | 1 | 3 | 0 | |
| Wobble | 3 | 7 | 122 | 44 | 82 | 0 | |
| Rise | 1 | 7 | 90 | 77 | 63 | 0 | |
| Fall | 0 | 0 | 33 | 37 | 46 | 78 | |
| Collapse | 0 | 0 | 0 | 79 | 0 | 148 | |
| 01DK | 02KJ | 03JP | 04SD | |||||
|---|---|---|---|---|---|---|---|---|
| noSup | MT sup | noSup | MT sup | noSup | LT sup | noSup | UT sup | |
| Stable | 6.5% | 41.1% | 0.6% | 34.6% | 4.0% | 18.5% | 7.2% | 10.9% |
| Head | 18.5% | 17.8% | 1.3% | 48.0% | 22.8% | 8.5% | 9.6% | 66.8% |
| Wobble | 33.4% | 14.0% | 25.2% | 6.7% | 27.7% | 33.0% | 37.7% | 8.5% |
| Rise | 15.6% | 8.4% | 25.1% | 3.6% | 17.5% | 7.9% | 21.6% | 3.2% |
| Fall | 14.2% | 7.0% | 17.1% | 3.3% | 17.0% | 6.9% | 19.3% | 3.6% |
| Collapse | 11.7% | 11.6% | 30.7% | 3.9% | 11.0% | 25.2% | 4.6% | 7.0% |
| 05BS | 06ML | 07WB | 08AC | |||||
| noSup | UT sup | noSup | UT sup | noSup | LT sup | noSup | LT sup | |
| Stable | 5.3% | 43.3% | 0.4% | 2.6% | 7.9% | 29.5% | 4.9% | 7.3% |
| Head | 11.6% | 35.0% | 3.2% | 49.6% | 5.8% | 18.6% | 37.1% | 37.5% |
| Wobble | 26.2% | 5.7% | 27.1% | 18.6% | 22.0% | 21.7% | 31.8% | 25.7% |
| Rise | 23.5% | 5.1% | 25.0% | 1.6% | 22.8% | 7.1% | 10.0% | 9.3% |
| Fall | 18.5% | 6.0% | 20.5% | 3.6% | 20.2% | 8.3% | 11.2% | 9.9% |
| Collapse | 14.9% | 4.9% | 23.8% | 24.0% | 21.3% | 14.9% | 5.0% | 10.3% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mellodge, P.; Saavedra, S.; Tran Poit, L.; Pratt, K.A.; Goodworth, A.D. Quantifying States and Transitions of Emerging Postural Control for Children Not Yet Able to Sit Independently. Sensors 2023, 23, 3309. https://doi.org/10.3390/s23063309
Mellodge P, Saavedra S, Tran Poit L, Pratt KA, Goodworth AD. Quantifying States and Transitions of Emerging Postural Control for Children Not Yet Able to Sit Independently. Sensors. 2023; 23(6):3309. https://doi.org/10.3390/s23063309
Chicago/Turabian StyleMellodge, Patricia, Sandra Saavedra, Linda Tran Poit, Kristamarie A. Pratt, and Adam D. Goodworth. 2023. "Quantifying States and Transitions of Emerging Postural Control for Children Not Yet Able to Sit Independently" Sensors 23, no. 6: 3309. https://doi.org/10.3390/s23063309
APA StyleMellodge, P., Saavedra, S., Tran Poit, L., Pratt, K. A., & Goodworth, A. D. (2023). Quantifying States and Transitions of Emerging Postural Control for Children Not Yet Able to Sit Independently. Sensors, 23(6), 3309. https://doi.org/10.3390/s23063309




