Levator Scapulae Stiffness Measurement Reliability in Individuals with and without Chronic Neck Pain by Experienced and Novel Examiners
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Sample Size Calculation
2.4. Examiners
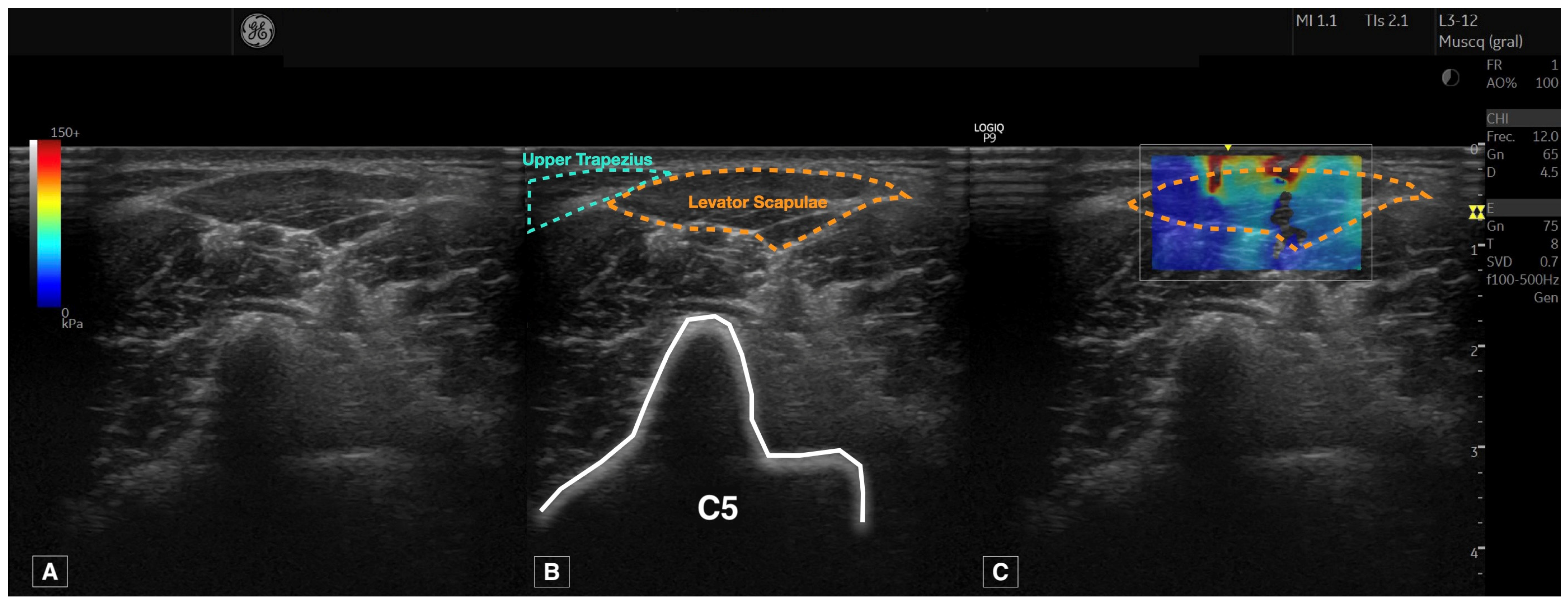
2.5. Ultrasound Imaging Acquisition Protocol
2.6. Measurement of Muscle Stiffness
2.7. Statistical Analyses
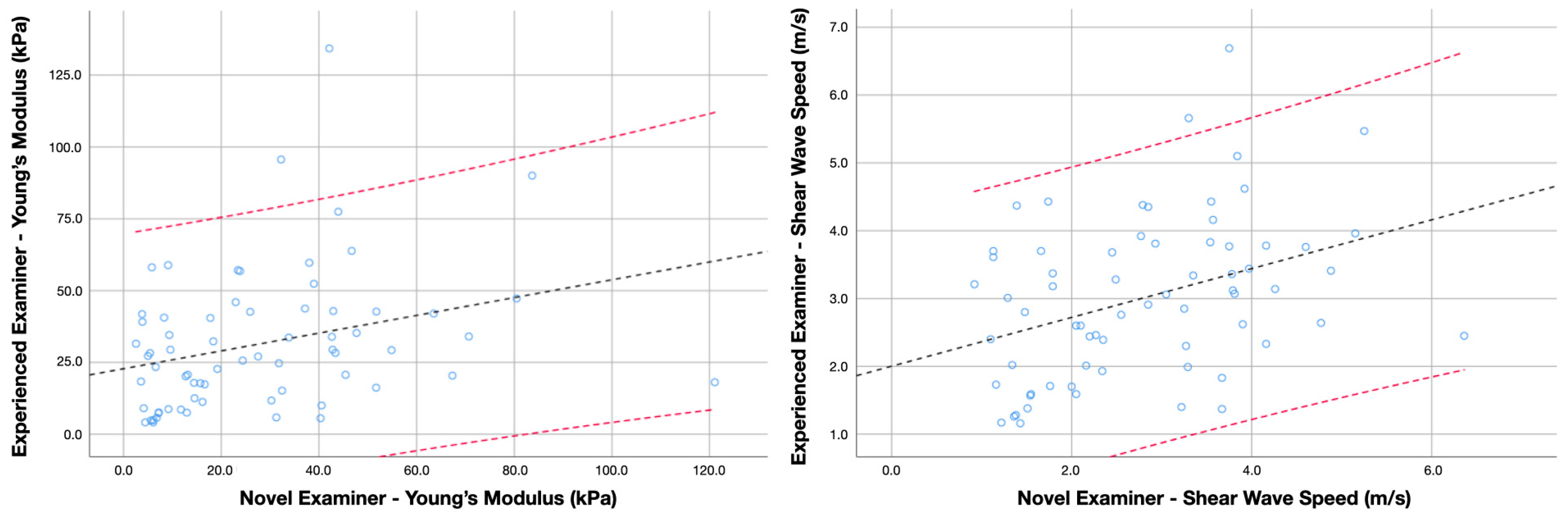
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schünke, M.; Schulte, E.; Schumacher, U. Prometheus. Texto y Atlas de Anatomia. Tomo 3: Cabeza, Cuello y Neuroanatomía, 3rd ed.; Editorial Médica Panamericana: Madrid, Spain, 2015. [Google Scholar]
- Beger, O.; Dinç, U.; Beger, B.; Uzmansel, D.; Kurtoğlu, Z. Morphometric properties of the levator scapulae, rhomboid major, and rhomboid minor in human fetuses. Surg. Radiol. Anat. 2018, 40, 449–455. [Google Scholar] [CrossRef] [PubMed]
- Au, J.; Webb, A.L.; Buirski, G.; Smith, P.N.; Pickering, M.R.; Perriman, D.M. Anatomic variations of levator scapulae in a normal cohort: An MRI study. Surg. Radiol. Anat. 2017, 39, 337–343. [Google Scholar] [CrossRef] [PubMed]
- Chotai, P.N.; Loukas, M.; Tubbs, R.S. Unusual origin of the levator scapulae muscle from mastoid process. Surg. Radiol. Anat. 2015, 37, 1277–1281. [Google Scholar] [CrossRef] [PubMed]
- Eliot, D.J. Electromyography of levator scapulae: New findings allow tests of a head stabilization model. J. Manip. Physiol. Ther. 1996, 19, 19–25. [Google Scholar]
- Kendall, F.; McCreary, E. Muscles Testing and Function, 5th ed.; Williams and Wilkins: Baltimore, MD, USA, 2005. [Google Scholar]
- Navarro-Ledesma, S.; Fernandez-Sanchez, M.; Struyf, F.; Martinez-Calderon, J.; Miguel Morales-Asencio, J.; Luque-Suarez, A. Differences in scapular upward rotation, pectoralis minor and levator scapulae muscle length between the symptomatic, the contralateral asymptomatic shoulder and control subjects: A cross-sectional study in a Spanish primary care setting. BMJ Open 2019, 9, e023020. [Google Scholar] [CrossRef] [PubMed]
- Navarro-Ledesma, S.; Fernandez-Sanchez, M.; Struyf, F.; Luque Suarez, A. Association of Both Scapular Upward Rotation and Scapulothoracic Muscle Lengths With Shoulder Pain, Function, and Range of Movement. J. Manip. Physiol. Ther. 2020, 43, 824–831. [Google Scholar] [CrossRef] [PubMed]
- Snodgrass, S.J.; Croker, C.; Yerrapothu, M.; Shepherd, S.; Stanwell, P.; Holder, C.; Oldmeadow, C.; Elliott, J. Cervical muscle volume in individuals with idiopathic neck pain compared to asymptomatic controls: A cross-sectional magnetic resonance imaging study. Musculoskelet. Sci. Pract. 2019, 44, 102050. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, H.; Muraki, T.; Morise, S.; Yamamoto, N.; Itoi, E.; Izumi, S.I. Differences in scapular motion and parascapular muscle activities among patients with symptomatic and asymptomatic rotator cuff tears, and healthy individuals. JSES Int. 2020, 5, 238–246. [Google Scholar] [CrossRef]
- Behrsin, J.F.; Maguire, K. Levator Scapulae Action during Shoulder Movement: A Possible Mechanism for Shoulder Pain of Cervical Origin. Aust. J. Physiother. 1986, 32, 101–106. [Google Scholar] [CrossRef]
- Chiarotto, A.; Clijsen, R.; Fernandez-de-Las-Penas, C.; Barbero, M. Prevalence of myofascial trigger points in spinal disorders: A systematic review and meta-analysis. Arch. Phys. Med. Rehabil. 2016, 97, 316–337. [Google Scholar] [CrossRef]
- Sari, H.; Akarirmak, U.; Uludag, M. Active myofascial trigger points might be more frequent in patients with cervical radiculopathy. Eur. J. Phys. Rehabil. Med. 2012, 48, 237–244. [Google Scholar]
- Ettlin, T.; Schuster, C.; Stoffel, R.; Brüderlin, A.; Kischka, U. A distinct pattern of myofascial findings in patients after whiplash injury. Arch. Phys. Med. Rehabil. 2008, 89, 1290–1293. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Pérez, A.M.; Villaverde-Gutiérrez, C.; Mora-Sánchez, A.; Alonso-Blanco, C.; Sterling, M.; Fernández-de-Las-Peñas, C. Muscle trigger points, pressure pain threshold, and cervical range of motion in patients with high level of disability related to acute whiplash injury. J. Orthop. Sports Phys. Ther. 2012, 42, 634–641. [Google Scholar] [CrossRef] [PubMed]
- Cao, Q.W.; Peng, B.G.; Wang, L.; Huang, Y.Q.; Jia, D.L.; Jiang, H.; Lv, Y.; Liu, X.G.; Liu, R.G.; Li, Y.; et al. Expert consensus on the diagnosis and treatment of myofascial pain syndrome. World J. Clin. Cases 2021, 9, 2077–2089. [Google Scholar] [CrossRef] [PubMed]
- Valera-Calero, J.A.; Ojedo-Martín, C.; Fernández-de-Las-Peñas, C.; Cleland, J.A.; Arias-Buría, J.L.; Hervás-Pérez, J.P. Reliability and Validity of Panoramic Ultrasound Imaging for Evaluating Muscular Quality and Morphology: A Systematic Review. Ultrasound Med. Biol. 2021, 47, 185–200. [Google Scholar] [CrossRef] [PubMed]
- Varol, U.; Sánchez-Jiménez, E.; Leloup, E.A.A.; Navarro-Santana, M.J.; Fernández-De-Las-Peñas, C.; Sánchez-Jorge, S.; Valera-Calero, J.A. Correlation between Body Composition and Inter-Examiner Errors for Assessing Lumbar Multifidus Muscle Size, Shape and Quality Metrics with Ultrasound Imaging. Bioengineering 2023, 10, 133. [Google Scholar] [CrossRef] [PubMed]
- Varol, U.; Navarro-Santana, M.J.; Valera-Calero, J.A.; Antón-Ramírez, S.; Álvaro-Martínez, J.; Díaz-Arribas, M.J.; Fernández-De-Las-Peñas, C.; Plaza-Manzano, G. Convergent Validity between Electromyographic Muscle Activity, Ultrasound Muscle Thickness and Dynamometric Force Measurement for Assessing Muscle. Sensors 2023, 23, 2030. [Google Scholar] [CrossRef] [PubMed]
- Valera-Calero, J.A.; Fernández-de-Las-Peñas, C.; Varol, U.; Ortega-Santiago, R.; Gallego-Sendarrubias, G.M.; Arias-Buría, J.L. Ultrasound Imaging as a Visual Biofeedback Tool in Rehabilitation: An Updated Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 7554. [Google Scholar] [CrossRef]
- Diep, D.; Chen, K.J.Q.; Kumbhare, D. Ultrasound-guided interventional procedures for myofascial trigger points: A systematic review. Reg. Anesth. Pain Med. 2021, 46, 73–80. [Google Scholar] [CrossRef]
- Ozturk, A.; Grajo, J.R.; Dhyani, M.; Anthony, B.W.; Samir, A.E. Principles of ultrasound elastography. Abdom. Radiol. 2018, 43, 773–785. [Google Scholar] [CrossRef]
- Valera-Calero, J.A.; Sánchez-Jorge, S.; Buffet-García, J.; Varol, U.; Gallego-Sendarrubias, G.M.; Álvarez-González, J. Is Shear-Wave Elastography a Clinical Severity Indicator of Myofascial Pain Syndrome? An Observational Study. J. Clin. Med. 2021, 10, 2895. [Google Scholar] [CrossRef] [PubMed]
- Kottner, J.; Audigé, L.; Brorson, S.; Donner, A.; Gajewski, B.J.; Hróbjartsson, A.; Roberts, C.; Shoukri, M.; Streiner, D.L. Guidelines for Reporting Reliability and Agreement Studies (GRRAS) were proposed. J. Clin. Epidemiol. 2011, 64, 96–106. [Google Scholar] [CrossRef] [PubMed]
- Faggion, C.M., Jr. EQUATOR reporting guidelines should also be used by clinicians. J. Clin. Epidemiol. 2020, 117, 149–150. [Google Scholar] [CrossRef] [PubMed]
- Boonstra, A.M.; Schiphorst Preuper, H.R.; Balk, G.A.; Stewart, R.E. Cut-off points for mild, moderate, and severe pain on the visual analogue scale for pain in patients with chronic musculoskeletal pain. Pain 2014, 155, 2545–2550. [Google Scholar] [CrossRef]
- Walter, S.D.; Eliasziw, M.; Donner, A. Sample size and optimal designs for reliability studies. Stat. Med. 1998, 17, 101–110. [Google Scholar] [CrossRef]
- Valera-Calero, J.A.; Gallego-Sendarrubias, G.; Fernández-de-Las-Peñas, C.; Cleland, J.A.; Ortega-Santiago, R.; Arias-Buría, J.L. Cross-sectional area of the cervical extensors assessed with panoramic ultrasound imaging: Preliminary data in healthy people. Musculoskelet. Sci. Pract. 2020, 50, 102257. [Google Scholar] [CrossRef] [PubMed]
- Valera-Calero, J.A.; Gallego-Sendarrubias, G.M.; Fernández-de-Las-Peñas, C.; Cleland, J.A.; Ortega-Santiago, R.; Arias-Buría, J.L. Panoramic Ultrasound Examination of Posterior Neck Extensors in Healthy Subjects: Intra-Examiner Reliability Study. Diagnostics 2020, 10, 740. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Ten Hove, D.; Jorgensen, T.D.; van der Ark, L.A. Updated guidelines on selecting an intraclass correlation coefficient for interrater reliability, with applications to incomplete observational designs. Psychol. Methods 2022. [Google Scholar] [CrossRef]
- Kozinc, Ž.; Šarabon, N. Shear-wave elastography for assessment of trapezius muscle stiffness: Reliability and association with low-level muscle activity. PLoS ONE 2020, 15, e0234359. [Google Scholar] [CrossRef]
- Money, S. Pathophysiology of Trigger Points in Myofascial Pain Syndrome. J. Pain Palliat. Care Pharmacother. 2017, 31, 158–159. [Google Scholar] [CrossRef] [PubMed]
- Guzmán Pavón, M.J.; Cavero Redondo, I.; Martínez Vizcaíno, V.; Ferri Morales, A.; Lorenzo García, P.; Álvarez Bueno, C. Comparative Effectiveness of Manual Therapy Interventions on Pain and Pressure Pain Threshold in Patients With Myofascial Trigger Points: A Network Meta-analysis. Clin. J. Pain 2022, 38, 749–760. [Google Scholar] [CrossRef] [PubMed]
- Valera-Calero, J.A.; Sánchez-Jorge, S.; Buffet-García, J.; Varol, U. Fernández-de-Las-Peñas, C., Álvarez-González, J. Changes in stiffness at active myofascial trigger points of the upper trapezius after dry needling in patients with chronic neck pain: A randomized controlled trial. Acupunct. Med. 2023, 41, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Kuo, W.H.; Jian, D.W.; Wang, T.G.; Wang, Y.C. Neck muscle stiffness quantified by sonoelastography is correlated with body mass index and chronic neck pain symptoms. Ultrasound Med. Biol. 2013, 39, 1356–1361. [Google Scholar] [CrossRef]
- Yanase, K.; Ikezoe, T.; Nakamura, M.; Saeki, J.; Yagi, M.; Hirono, T.; Tamezawa, T.; Motomura, Y.; Ibuki, S.; Ichihashi, N. Effective muscle elongation positions for the neck extensor muscles: An ultrasonic shear wave elastography study. J. Electromyogr. Kinesiol. 2021, 60, 102569. [Google Scholar] [CrossRef]
- Taş, S.; Korkusuz, F.; Erden, Z. Neck Muscle Stiffness in Participants With and Without Chronic Neck Pain: A Shear-Wave Elastography Study. J. Manip. Physiol. Ther. 2018, 41, 580–588. [Google Scholar] [CrossRef]
- Akagi, R.; Kusama, S. Comparison Between Neck and Shoulder Stiffness Determined by Shear Wave Ultrasound Elastography and a Muscle Hardness Meter. Ultrasound Med. Biol. 2015, 41, 2266–2271. [Google Scholar] [CrossRef]
- Varol, U.; Navarro-Santana, M.J.; Gómez-Sánchez, S.; Plaza-Manzano, G.; Sánchez-Jiménez, E.; Valera-Calero, J.A. Inter-Examiner Disagreement for Assessing Cervical Multifidus Ultrasound Metrics Is Associated with Body Composition Features. Sensors 2023, 23, 1213. [Google Scholar] [CrossRef]
- Weber, B.R.; Uhlig, Y.; Grob, D.; Dvorák, J.; Müntener, M. Duration of pain and muscular adaptations in patients with dysfunction of the cervical spine. J. Orthop. Res. 1993, 11, 805–810. [Google Scholar] [CrossRef]
- Yamasaki, M.; Sasaki, Y. Determining Young’s modulus of timber on the basis of a strength database and stress wave propagation velocity I: An estimation method for Young’s modulus employing Monte Carlo simulation. J. Wood Sci. 2010, 56, 269–275. [Google Scholar] [CrossRef]

| Sociodemographic Characteristics | Levator Scapulae SWE a | |||||
|---|---|---|---|---|---|---|
| Age (y) | Height (m) | Weight (kg) | BMI (kg/m2) | Young’s Modulus (kPa) | Shear Wave Speed (m/s) | |
| Gender | ||||||
| Males (n = 35) | 22.2 ± 4.7 | 1.77 ± 0.07 | 74.8 ± 13.3 | 23.9 ± 3.6 | 29.6 ± 19.4 | 2.92 ± 0.99 |
| Females (n = 32) | 20.6 ± 2.6 | 1.64 ± 0.06 | 65.1 ± 12.5 | 24.3 ± 4.7 | 28.4 ± 21.2 | 2.78 ± 1.10 |
| Difference | 1.6 (−0.31; 3.5) p = 0.101 | 0.13 (0.09; 0.16) p < 0.001 | 9.7 (3.3; 16.1) p = 0.003 | 0.4 (−1.6; 2.4) p = 0.707 | 1.1 (−5.9; 8.1) p = 0.747 | 0.14 (−0.21; 0.50) p = 0.436 |
| Cases and controls | ||||||
| Asymptomatic subjects (n = 33) | 21.4 ± 4.8 | 1.72 ± 0.08 | 72.4 ± 14.4 | 24.3 ± 4.0 | 27.8 ± 21.4 | 2.78 ± 1.10 |
| Patients with neck pain (n = 34) | 21.5 ± 2.8 | 1.69 ± 0.10 | 68.3 ± 13.1 | 23.8 ± 4.3 | 29.6 ± 19.1 | 2.90 ± 1.00 |
| Difference | 0.0 (−1.9; 2.0) p = 0.973 | 0.03 (−0.01; 0.08) p = 0.133 | 4.1 (−2.7; 10.8) p = 0.231 | 0.4 (−1.6; 2.5) p = 0.667 | 1.8 (−5.1; 8.7) p = 0.605 | 0.11 (−0.24; 0.47) p = 0.525 |
| Variables | Asymptomatic Individuals (n = 33) | Patients with Neck Pain (n = 34) | ||
|---|---|---|---|---|
| Young’s Modulus (kPa) | Shear Wave Speed (m/s) | Young’s Modulus (kPa) | Shear Wave Speed (m/s) | |
| Mean (n = 268 images) | 27.8 ± 21.4 | 2.78 ± 1.10 | 29.6 ± 19.1 | 2.90 ± 1.00 |
| Experienced examiner (n = 134 images) | 30.7 ± 28.4 | 2.89 ± 1.32 | 31.4 ± 24.0 | 3.00 ± 1.17 |
| Novel examiner (n = 134 images) | 24.9 ± 19.3 | 2.67 ± 1.09 | 27.8 ± 23.3 | 2.79 ± 1.23 |
| Absolute difference | 14.7 ± 8.4 | 0.72 ± 0.36 | 19.5 ± 10.2 | 1.01 ± 0.50 |
| ICC3,2 (95% CI) | 0.714 (0.533; 0.825) | 0.779 (0.639; 0.865) | 0.461 (0.127; 0.668) | 0.546 (0.265; 0.720) |
| SEM | 11.4 | 0.51 | 14.0 | 0.67 |
| MDC95 | 31.7 | 1.43 | 38.9 | 1.86 |
| CV (%) | 52.8 | 25.9 | 65.9 | 34.8 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Varol, U.; Valera-Calero, J.A.; Sánchez-Jiménez, E.; Fernández-de-las-Peñas, C.; Ortega-Santiago, R.; Kobylarz, M.D.; Navarro-Santana, M.J. Levator Scapulae Stiffness Measurement Reliability in Individuals with and without Chronic Neck Pain by Experienced and Novel Examiners. Sensors 2024, 24, 277. https://doi.org/10.3390/s24010277
Varol U, Valera-Calero JA, Sánchez-Jiménez E, Fernández-de-las-Peñas C, Ortega-Santiago R, Kobylarz MD, Navarro-Santana MJ. Levator Scapulae Stiffness Measurement Reliability in Individuals with and without Chronic Neck Pain by Experienced and Novel Examiners. Sensors. 2024; 24(1):277. https://doi.org/10.3390/s24010277
Chicago/Turabian StyleVarol, Umut, Juan Antonio Valera-Calero, Elena Sánchez-Jiménez, César Fernández-de-las-Peñas, Ricardo Ortega-Santiago, Mateusz D. Kobylarz, and Marcos José Navarro-Santana. 2024. "Levator Scapulae Stiffness Measurement Reliability in Individuals with and without Chronic Neck Pain by Experienced and Novel Examiners" Sensors 24, no. 1: 277. https://doi.org/10.3390/s24010277
APA StyleVarol, U., Valera-Calero, J. A., Sánchez-Jiménez, E., Fernández-de-las-Peñas, C., Ortega-Santiago, R., Kobylarz, M. D., & Navarro-Santana, M. J. (2024). Levator Scapulae Stiffness Measurement Reliability in Individuals with and without Chronic Neck Pain by Experienced and Novel Examiners. Sensors, 24(1), 277. https://doi.org/10.3390/s24010277








