Developing a Portable Autofluorescence Detection System and Its Application in Biological Samples
Abstract
:1. Introduction
2. Materials and Methods
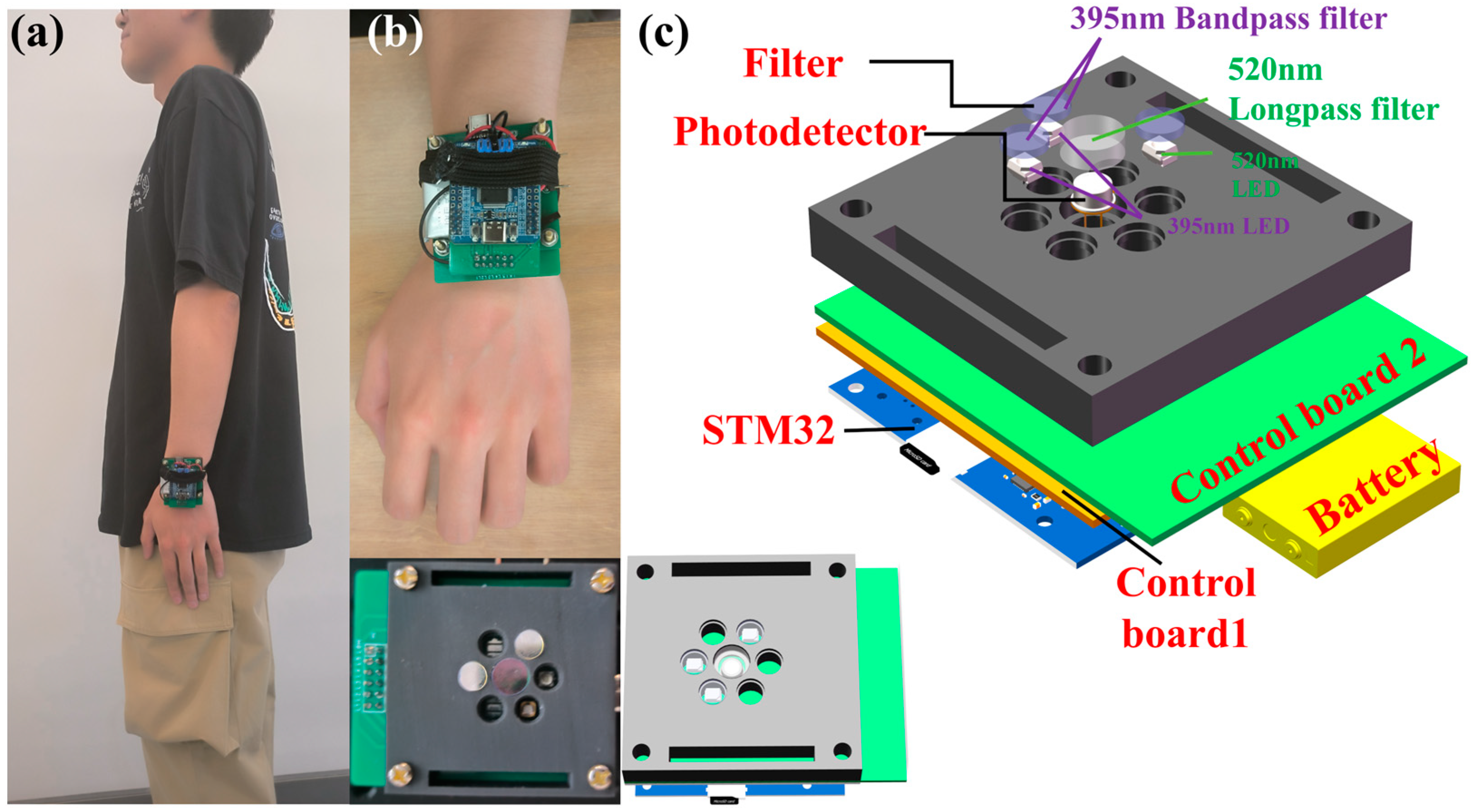
2.1. Structural Design of the Portable Autofluorescence Detection System
2.2. Enhanced Control Module Design for Precision and Portability
2.3. Optimized LED Emission Module for Enhanced Autofluorescence Excitation
2.4. Advanced Detection Module with Precision Filtering and Amplification Circuitry
3. Results
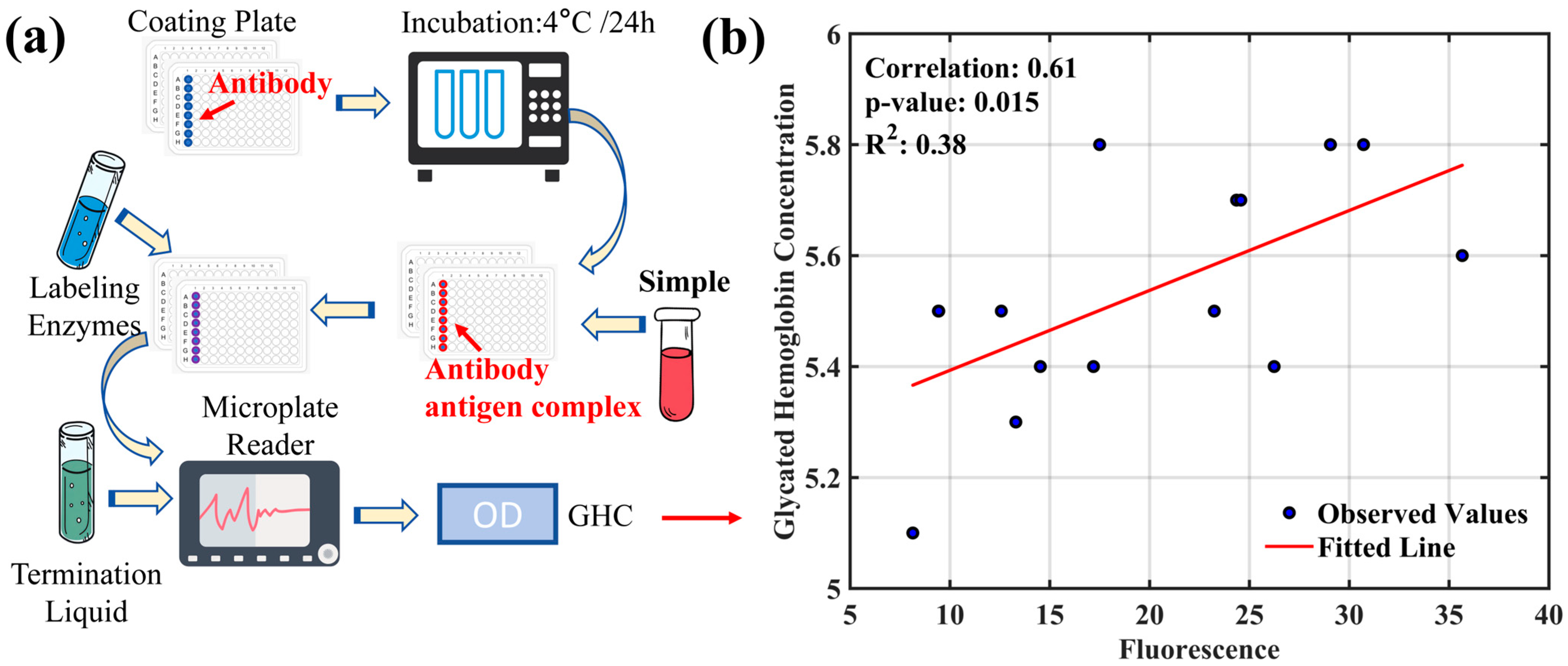
3.1. Study on the Correlation between Glycated Hemoglobin and AGEs’ Fluorescence Intensity
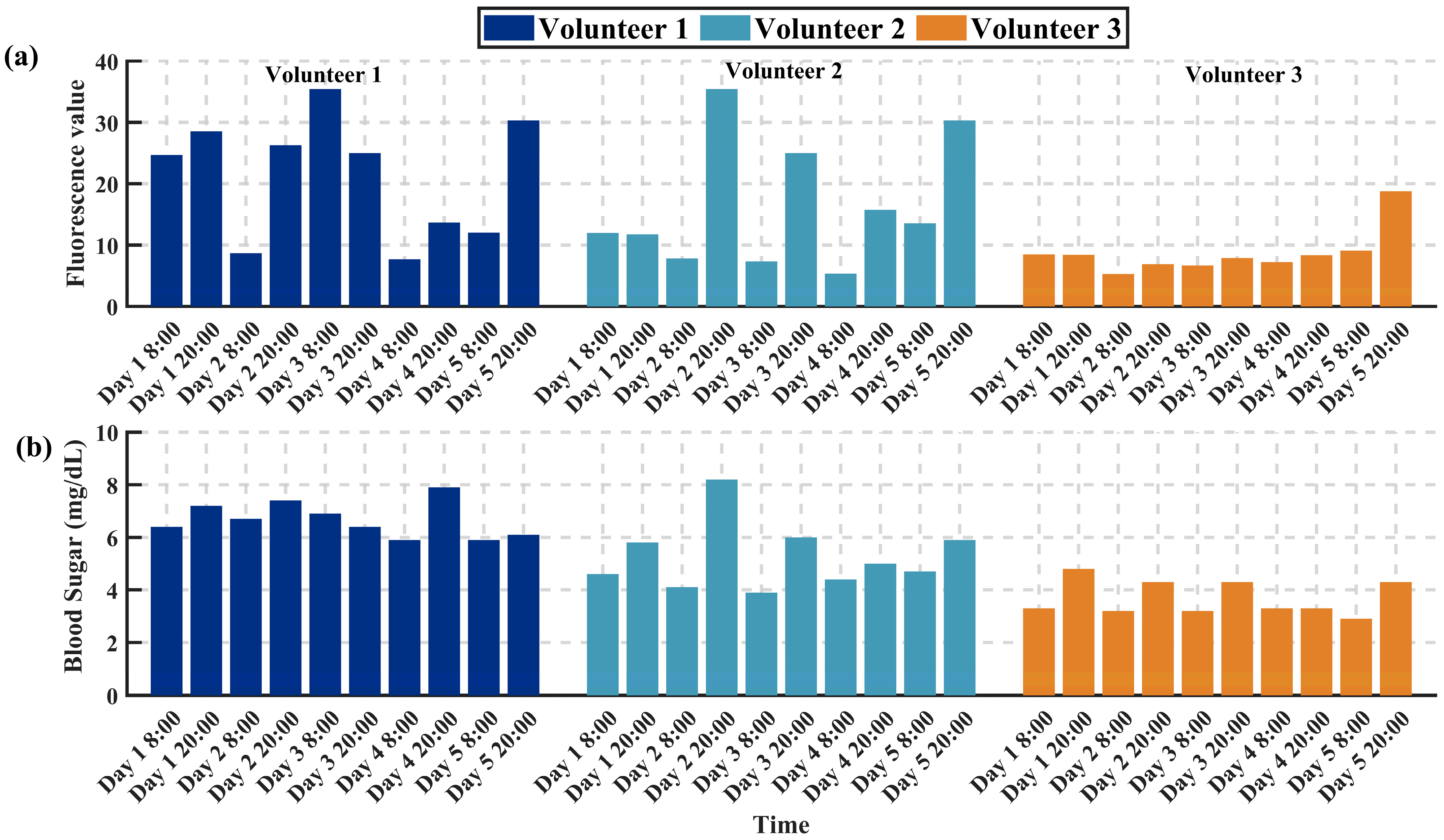
3.2. Study on the Trends of AGEs’ Fluorescence Intensity and Blood Glucose Variation
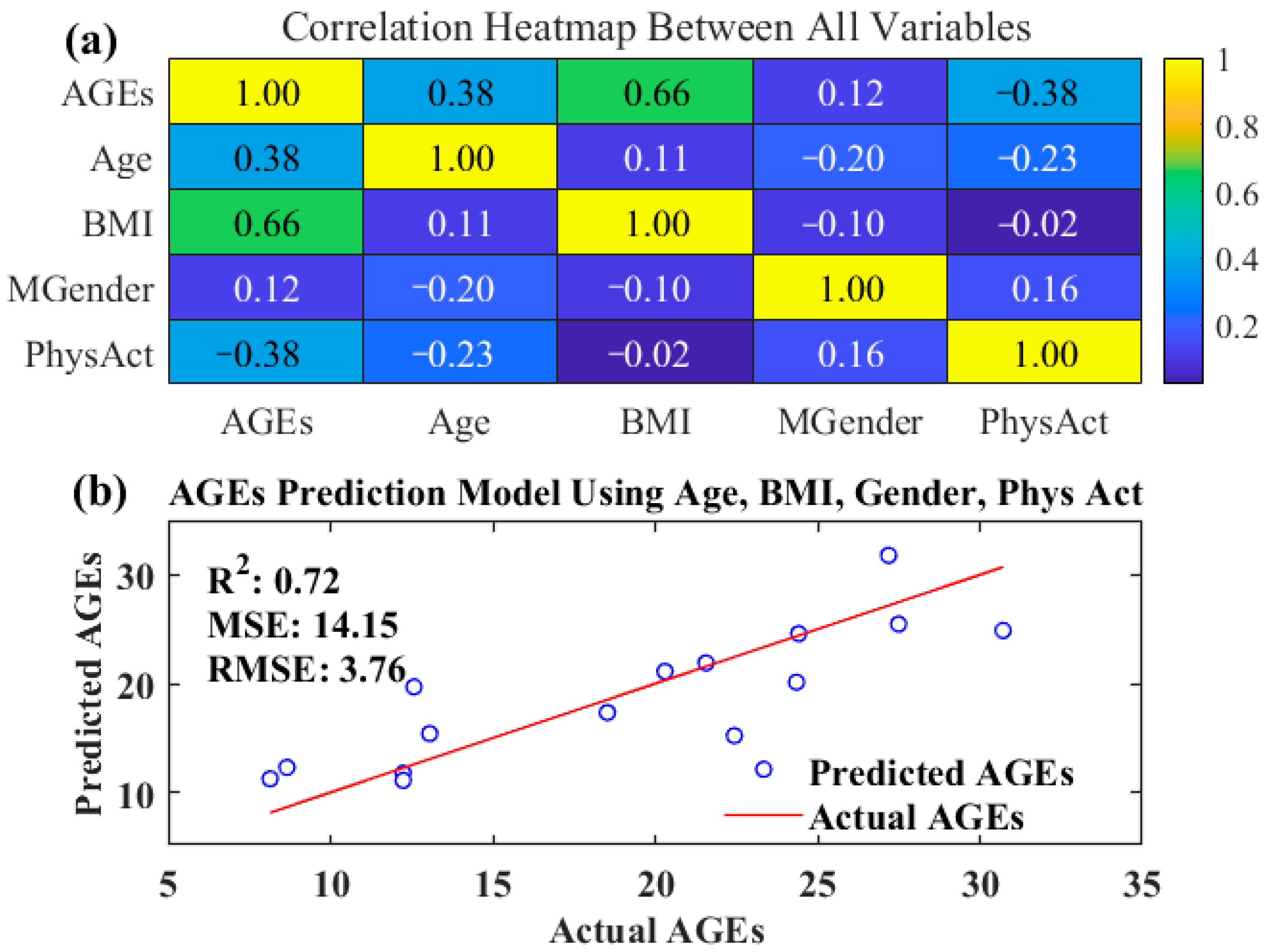
3.3. Validation of a Multivariate Prediction Model Based on Analysis of Factors Influencing Advanced Glycation End-Product Content
4. Conclusions
5. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Itakura, M.; Yamaguchi, K.; Kitazawa, R.; Lim, S.-Y.; Anan, Y.; Yoshitake, J.; Shibata, T.; Negishi, L.; Sugawa, H.; Nagai, R.; et al. Histone Functions as a Cell-Surface Receptor for AGEs. Nat. Commun. 2022, 13, 2974. [Google Scholar] [CrossRef] [PubMed]
- Twarda-Clapa, A.; Olczak, A.; Białkowska, A.M.; Koziołkiewicz, M. Advanced Glycation End-Products (AGEs): Formation, Chemistry, Classification, Receptors, and Diseases Related to AGEs. Cells 2022, 11, 1312. [Google Scholar] [CrossRef] [PubMed]
- Atzeni, I.M.; Van De Zande, S.C.; Westra, J.; Zwerver, J.; Smit, A.J.; Mulder, D.J. The AGE Reader: A Non-Invasive Method to Assess Long-Term Tissue Damage. Methods 2022, 203, 533–541. [Google Scholar] [CrossRef] [PubMed]
- Hegab, Z.; Gibbons, S.; Neyses, L.; Mamas, M.A. Role of Advanced Glycation End Products in Cardiovascular Disease. World J. Cardiol. 2012, 4, 90–102. [Google Scholar] [CrossRef] [PubMed]
- Vistoli, G.; De Maddis, D.; Cipak, A.; Zarkovic, N.; Carini, M.; Aldini, G. Advanced Glycoxidation and Lipoxidation End Products (AGEs and ALEs): An Overview of Their Mechanisms of Formation. Free Radic. Res. 2013, 47, 3–27. [Google Scholar] [CrossRef] [PubMed]
- Perrone, A.; Giovino, A.; Benny, J.; Martinelli, F. Advanced Glycation End Products (AGEs): Biochemistry, Signaling, Analytical Methods, and Epigenetic Effects. Oxidative Med. Cell. Longev. 2020, 2020, e3818196. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.; Cheng, K.-W.; Xiao, J.; Wang, M. The Multifunctional Roles of Flavonoids against the Formation of Advanced Glycation End Products (AGEs) and AGEs-Induced Harmful Effects. Trends Food Sci. Technol. 2020, 103, 333–347. [Google Scholar] [CrossRef]
- Gautieri, A.; Passini, F.S.; Silván, U.; Guizar-Sicairos, M.; Carimati, G.; Volpi, P.; Moretti, M.; Schoenhuber, H.; Redaelli, A.; Berli, M.; et al. Advanced Glycation End-Products: Mechanics of Aged Collagen from Molecule to Tissue. Matrix Biol. 2017, 59, 95–108. [Google Scholar] [CrossRef] [PubMed]
- Loske, C.; Neumann, A.; Cunningham, A.M.; Nichol, K.; Schinzel, R.; Riederer, P.; Münch, G. Cytotoxicity of Advanced Glycation Endproducts Is Mediated by Oxidative Stress. J. Neural Transm. 1998, 105, 1005–1015. [Google Scholar] [CrossRef]
- Meerwaldt, R.; Hartog, J.W.L.; Graaff, R.; Huisman, R.J.; Links, T.P.; den Hollander, N.C.; Thorpe, S.R.; Baynes, J.W.; Navis, G.; Gans, R.O.B.; et al. Skin Autofluorescence, a Measure of Cumulative Metabolic Stress and Advanced Glycation End Products, Predicts Mortality in Hemodialysis Patients. J. Am. Soc. Nephrol. 2005, 16, 3687. [Google Scholar] [CrossRef]
- Wee, B.F.; Sivakumar, S.; Lim, K.H.; Wong, W.K.; Juwono, F.H. Diabetes Detection Based on Machine Learning and Deep Learning Approaches. Multimed. Tools Appl. 2024, 83, 24153–24185. [Google Scholar] [CrossRef]
- Islam, M.M.F.; Ferdousi, R.; Rahman, S.; Bushra, H.Y. Likelihood Prediction of Diabetes at Early Stage Using Data Mining Techniques. In Computer Vision and Machine Intelligence in Medical Image Analysis; Gupta, M., Konar, D., Bhattacharyya, S., Biswas, S., Eds.; Springer: Singapore, 2020; pp. 113–125. [Google Scholar]
- Evans, M.; Morgan, A.R.; Patel, D.; Dhatariya, K.; Greenwood, S.; Newland-Jones, P.; Hicks, D.; Yousef, Z.; Moore, J.; Kelly, B.; et al. Risk Prediction of the Diabetes Missing Million: Identifying Individuals at High Risk of Diabetes and Related Complications. Diabetes Ther. 2021, 12, 87–105. [Google Scholar] [CrossRef] [PubMed]
- Garagliano, J.M.; Katsurada, A.; Miyata, K.; Derbenev, A.V.; Zsombok, A.; Navar, L.G.; Satou, R. Advanced Glycation End Products Stimulate Angiotensinogen Production in Renal Proximal Tubular Cells. Am. J. Med. Sci. 2019, 357, 57–66. [Google Scholar] [CrossRef] [PubMed]
- Noce, A.; Rovella, V.; Marrone, G.; Cattani, G.; Zingaretti, V.; Limongi, D.; D’Agostini, C.; Sorge, R.; Casasco, M.; Di Daniele, N.; et al. Hemodialysis Biomarkers: Total Advanced Glycation End Products (AGEs) against Oxidized Human Serum Albumin (HSAox). Acta Diabetol. 2019, 56, 1323–1331. [Google Scholar] [CrossRef] [PubMed]
- Maasen, K.; Van Greevenbroek, M.M.; Scheijen, J.L.J.; Van Der Kallen, C.J.; Stehouwer, C.D.; Schalkwijk, C.G. High Dietary Glycemic Load Is Associated with Higher Concentrations of Urinary Advanced Glycation Endproducts: The Cohort on Diabetes and Atherosclerosis Maastricht (CODAM) Study. Am. J. Clin. Nutr. 2019, 110, 358–366. [Google Scholar] [CrossRef] [PubMed]
- Corica, D.; Pepe, G.; Currò, M.; Aversa, T.; Tropeano, A.; Ientile, R.; Wasniewska, M. Methods to Investigate Advanced Glycation End-Product and Their Application in Clinical Practice. Methods 2022, 203, 90–102. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Cai, F.; Dong, Y.; Zhu, Z.; Sun, X.; Zhang, H.; He, S. A Portable Confocal Hyperspectral Microscope without Any Scan or Tube Lens and Its Application in Fluorescence and Raman Spectral Imaging. Opt. Commun. 2017, 392, 1–6. [Google Scholar] [CrossRef]
- Cai, F.; He, S. Using Graphics Processing Units to Accelerate Perturbation Monte Carlo Simulation in a Turbid Medium. J. Biomed. Opt. 2012, 17, 040502. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Cai, F.; He, R.; He, S. Experimental Demonstration of Remote and Compact Imaging Spectrometer Based on Mobile Devices. Sensors 2018, 18, 1989. [Google Scholar] [CrossRef]
- Birukov, A.; Cuadrat, R.; Polemiti, E.; Eichelmann, F.; Schulze, M.B. Advanced Glycation End-Products, Measured as Skin Autofluorescence, Associate with Vascular Stiffness in Diabetic, Pre-Diabetic and Normoglycemic Individuals: A Cross-Sectional Study. Cardiovasc. Diabetol. 2021, 20, 110. [Google Scholar] [CrossRef]
- Li, Y.; Shen, F.; Hu, L.; Lang, Z.; Liu, Q.; Cai, F.; Fu, L. A Stare-Down Video-Rate High-Throughput Hyperspectral Imaging System and Its Applications in Biological Sample Sensing. IEEE Sens. J. 2023, 23, 23629–23637. [Google Scholar] [CrossRef]
- Li, Y.; Shen, F.; Lang, Z.; Cai, M.; Zeng, Q.; Liu, Q.; Cai, F. An Underwater Near-Infrared Spectral Continuum Robot as a Tool for in Situ Detection and Classification. Measurement 2023, 216, 112913. [Google Scholar] [CrossRef]
- Li, Y.; Fu, Y.; Lang, Z.; Cai, F. A High-Frequency and Real-Time Ground Remote Sensing System for Obtaining Water Quality Based on a Micro Hyper-Spectrometer. Sensors 2024, 24, 1833. [Google Scholar] [CrossRef] [PubMed]
- Koetsier, M.; Lutgers, H.L.; Smit, A.J.; Links, T.P.; Vries, R.D.; Gans, R.O.B.; Rakhorst, G.; Graaff, R. Skin Autofluorescence for the Risk Assessment of Chronic Complications in Diabetes: A Broad Excitation Range Is Sufficient. Opt. Express OE 2009, 17, 509–519. [Google Scholar] [CrossRef] [PubMed]
- Pohanka, M. Glycated Hemoglobin and Methods for Its Point of Care Testing. Biosensors 2021, 11, 70. [Google Scholar] [CrossRef] [PubMed]
- Zhan, Z.; Li, Y.; Zhao, Y.; Zhang, H.; Wang, Z.; Fu, B.; Li, W.J. A Review of Electrochemical Sensors for the Detection of Glycated Hemoglobin. Biosensors 2022, 12, 221. [Google Scholar] [CrossRef] [PubMed]
- Selvin, E.; Steffes, M.W.; Zhu, H.; Matsushita, K.; Wagenknecht, L.; Pankow, J.; Coresh, J.; Brancati, F.L. Glycated Hemoglobin, Diabetes, and Cardiovascular Risk in Nondiabetic Adults. N. Engl. J. Med. 2010, 362, 800–811. [Google Scholar] [CrossRef] [PubMed]
- Bazaev, N.A.; Pletenev, A.N.; Pozhar, K.V. Classification of Factors Affecting Blood Glucose Concentration Dynamics. Biomed. Eng. 2013, 47, 100–103. [Google Scholar] [CrossRef]
- Nowotny, K.; Jung, T.; Höhn, A.; Weber, D.; Grune, T. Advanced Glycation End Products and Oxidative Stress in Type 2 Diabetes Mellitus. Biomolecules 2015, 5, 194–222. [Google Scholar] [CrossRef]
- Peng, H.; Gao, Y.; Zeng, C.; Hua, R.; Guo, Y.; Wang, Y.; Wang, Z. Effects of Maillard Reaction and Its Product AGEs on Aging and Age-Related Diseases. Food Sci. Hum. Wellness 2024, 13, 1118–1134. [Google Scholar] [CrossRef]
- Semba, R.D.; Nicklett, E.J.; Ferrucci, L. Does Accumulation of Advanced Glycation End Products Contribute to the Aging Phenotype? J. Gerontol. Ser. A 2010, 65A, 963–975. [Google Scholar] [CrossRef] [PubMed]
- Scheijen, J.L.J.M.; Hanssen, N.M.J.; van Greevenbroek, M.M.; Van der Kallen, C.J.; Feskens, E.J.M.; Stehouwer, C.D.A.; Schalkwijk, C.G. Dietary Intake of Advanced Glycation Endproducts Is Associated with Higher Levels of Advanced Glycation Endproducts in Plasma and Urine: The CODAM Study. Clin. Nutr. 2018, 37, 919–925. [Google Scholar] [CrossRef] [PubMed]
- Mo, Y.; Ma, X.; Li, H.; Ran, X.; Yang, W.; Li, Q.; Peng, Y.; Li, Y.; Gao, X.; Luan, X. Relationship between Glycated Albumin and Glycated Hemoglobin According to Glucose Tolerance Status: A Multicenter Study. Diabetes Res. Clin. Pract. 2016, 115, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Koschinsky, T.; He, C.J.; Mitsuhashi, T.; Bucala, R.; Liu, C.; Buenting, C.; Heitmann, K.; Vlassara, H. Orally Absorbed Reactive Glycation Products (Glycotoxins): An Environmental Risk Factor in Diabetic Nephropathy. Proc. Natl. Acad. Sci. USA 1997, 94, 6474–6479. [Google Scholar] [CrossRef] [PubMed]
- Russell, W.R.; Baka, A.; Björck, I.; Delzenne, N.; Gao, D.; Griffiths, H.R.; Hadjilucas, E.; Juvonen, K.; Lahtinen, S.; Lansink, M.; et al. Impact of Diet Composition on Blood Glucose Regulation. Crit. Rev. Food Sci. Nutr. 2016, 56, 541–590. [Google Scholar] [CrossRef] [PubMed]
- Van Galen, K.A.; Ter Horst, K.W.; Serlie, M.J. Serotonin, Food Intake, and Obesity. Obes. Rev. 2021, 22, e13210. [Google Scholar] [CrossRef] [PubMed]
- Han, J.; Sun, Y.; Wu, T.; Hou, X.; Zheng, S.; Zhang, H.; Lin, T.; Liu, H.; Sun, T. Echinacoside-Zinc Nanomaterial Inhibits Skin Glycation by Suppressing the Transcriptional Activation of the Receptor for Advanced Glycation End-Products. ACS Nano 2023, 17, 14123–14135. [Google Scholar] [CrossRef]
- Li, S.; Wang, P.; Ye, M.; Yang, K.; Cheng, D.; Mao, Z.; He, L.; Liu, Z. Cysteine-Activatable Near-Infrared Fluorescent Probe for Dual-Channel Tracking Lipid Droplets and Mitochondria in Epilepsy. Anal. Chem. 2023, 95, 5133–5141. [Google Scholar] [CrossRef]

| Device | Parameters | Cost |
|---|---|---|
| Excitation light | 395 nm\3 W | 0.69$ |
| Calibration light source | 520 nm\1 W | 0.69$ |
| Batteries | 3.7 V\500 mAh | 2.00$ |
| Photodetector | 0.45 A\W | 9.00$ |
| Excitation filter | 10 mm\395 ± 10 nm | 13.00$ |
| Optical emission filter | 10 mm\520 ± 10 nm | 4.80$ |
| Total | 30.18$ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, J.; Li, Y.; Zhang, J.; Cai, F. Developing a Portable Autofluorescence Detection System and Its Application in Biological Samples. Sensors 2024, 24, 3351. https://doi.org/10.3390/s24113351
Zhou J, Li Y, Zhang J, Cai F. Developing a Portable Autofluorescence Detection System and Its Application in Biological Samples. Sensors. 2024; 24(11):3351. https://doi.org/10.3390/s24113351
Chicago/Turabian StyleZhou, Jiaxing, Yunfei Li, Jinfeng Zhang, and Fuhong Cai. 2024. "Developing a Portable Autofluorescence Detection System and Its Application in Biological Samples" Sensors 24, no. 11: 3351. https://doi.org/10.3390/s24113351





