Handgrip Strength in Health Applications: A Review of the Measurement Methodologies and Influencing Factors
Abstract
1. Introduction
- The primary focus of the study was methodological, encompassing the development of an HGS device, the examination of measurement procedures and the investigation of methodological aspects related to data processing.
- The proposed device, measurement procedure or processing methodology was subjected to testing in real experimental conditions.
2. Issues and Measurement Techniques for Handgrip Strength
2.1. Traditional Measurement Devices
2.2. Innovative Measurement Devices
2.3. Alternative Methods for Force Measurement
3. Methodological Aspects
3.1. Measurement Protocols
3.2. Parameters of Interest and Force Signal Analysis
3.3. Device Grip
3.4. Arm and Elbow Positions
3.5. Calibration
4. Endogenous Factors Influencing Handgrip Strength Value
4.1. Hand Dominance
4.2. Hand Size
4.3. Body Mass
4.4. Gender and Age
5. Exogenous Factors Influencing Handgrip Strength
5.1. Moments of the Day
5.2. Job/Occupation
5.3. Smoking
5.4. Psychological Sphere
6. Discussion and Conclusions
- (1)
- Issues and measurement techniques—This paper covers several devices, from traditional to novel, highlighting the importance of methodological rigor and technological advancement in the accurate assessment of HGS. Although traditional dynamometers lack a standard geometric shape, as highlighted in Section 2, they all have a fixed handle, a sliding handle, a load cell and a display or indicator. The working modes are similar: the patient rests their palm against the fixed handle, while their fingers wrap around the sliding handle and exert the grip that is measured by the load cell and shown on the display or indicator. From a purely geometric perspective, the discrepancies between devices from multiple manufacturers are mainly attributable to the widths of the individual handles, the distance between two handles, the shaping for the palm on the fixed handle and for the fingers on the sliding handle, and the overall volume. However, the weight of the handgrip device can also vary depending on the materials used and the construction stiffness adopted. These parameters are of significant importance for the suitable handling of the device, but more prominently, they can largely influence the correct execution of the test. Indeed, in the case of subjects with either small or large hand sizes, not all handgrip devices are adaptable and only a limited number of fit levels can be selected. Moreover, for patients who have functional limitations or impairments of one or more fingers or even parts of the hand, it is necessary to consider specific customized devices. Finally (see Table 1), from a purely measurement point of view, there is a limited variability within the measurement range (±10 kg, 80 kg to 100 kg except for MAP, mod. 130K1, for which the maximum measurable value is 130 kg). However, the differences in accuracy (up to 400%, from ±0.5 kg to ±2.0 kg) and especially in resolution (up to 10 times, from 0.1 kg to 1 kg) become more significant. These metrological properties should be carefully considered since they are responsible for the adequacy of the measurement and are difficult to distinguish by an inexperienced operator and the patient. Finally, each manufacturer adopts its own design, which can significantly differ from others, leading to variations in measurement results even under similar test conditions. This diversity makes it difficult to establish universal measurement protocols and compromises the consistency of data collection and analysis across studies and applications.
- (2)
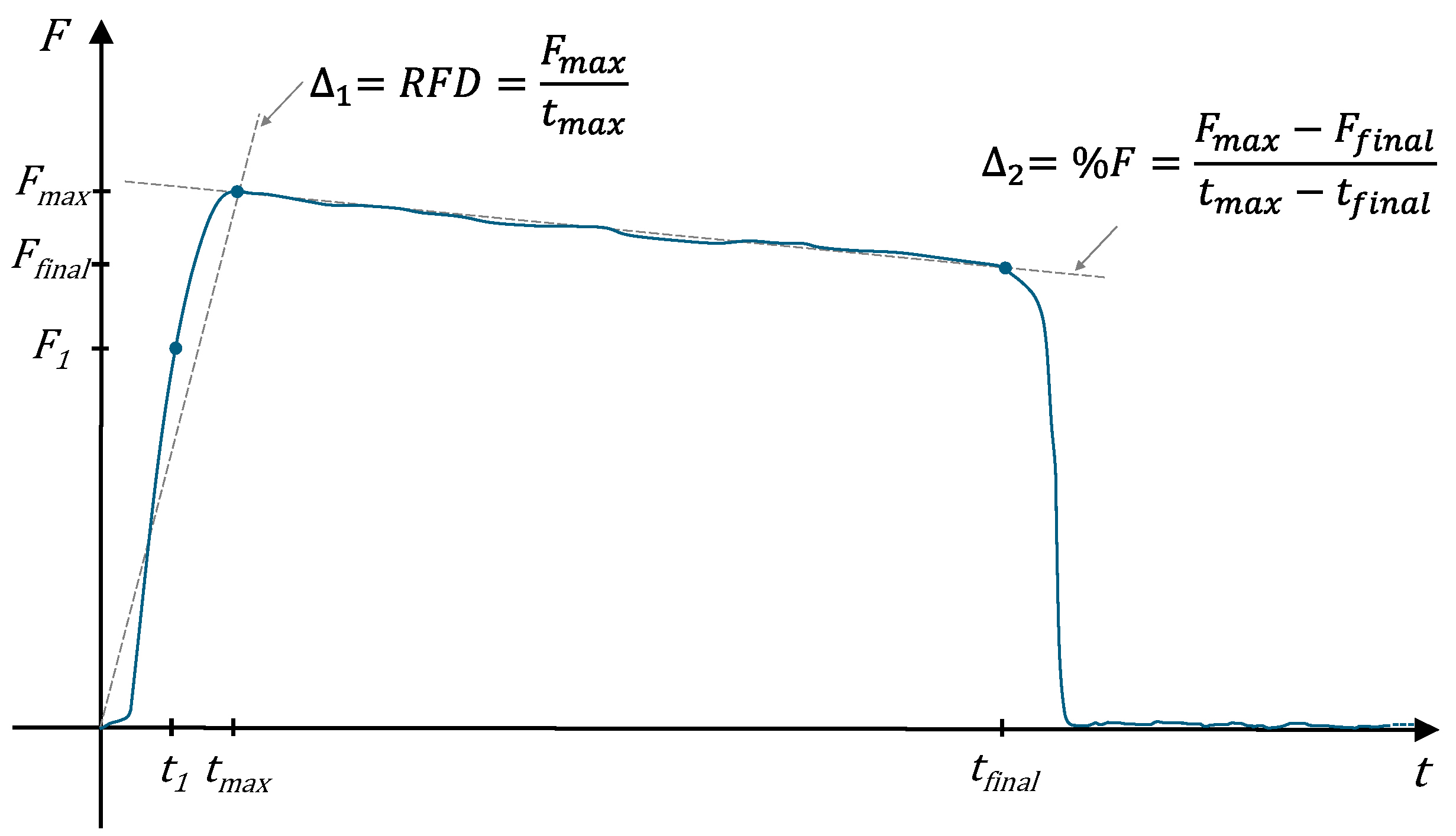
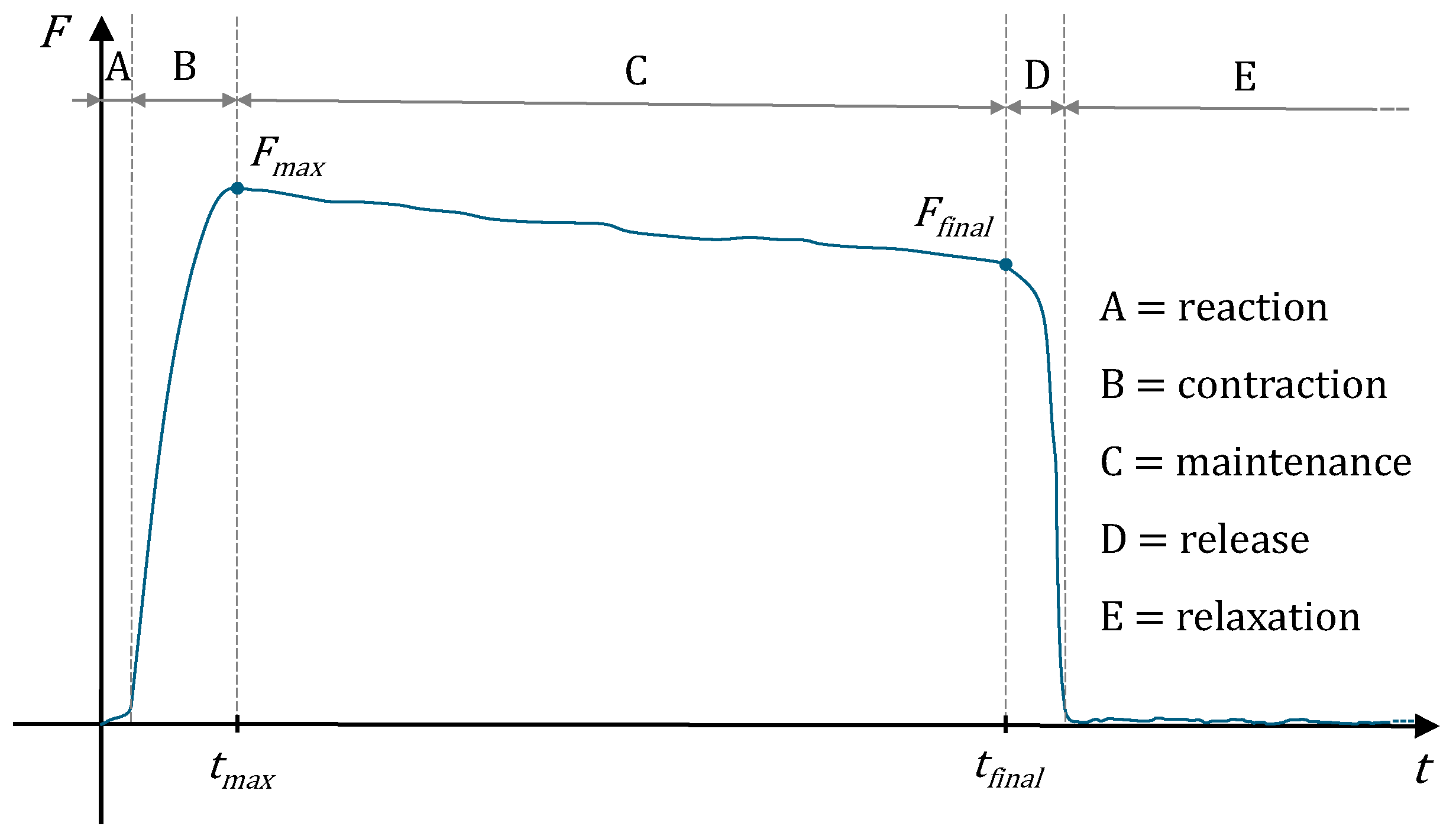
- Methodological aspects—This study has emphasized some limitations of current HGS measurement practices. The choice of a representative parameter for the measurement of HGS is therefore a topic of considerable discussion in the literature, and a common and objective strategy has not yet been identified. Although the maximal isometric force Fmax (see Figure 2) is relatively straightforward to consider, this value tends to exhibit a rapid decay and frequently differs significantly from its final value Ffinal. Similarly, the evaluation of a fraction of Fmax does not ensure a broadly agreeable outcome. It could be really interesting to estimate a generalized parameter that takes into account Fmax, i.e., an impulsive force, and the duration of the measurement, i.e., a muscular endurance. For these reasons, although it is rarely considered in the field of sports and medicine, the rate of decay Δ2 could be configured as a valid alternative, thereby enhancing the representativeness of the measurement result. Hence, the current methods neglect the dynamic profile of force application over time, which could provide deeper insights into neuromuscular health, fatigue resistance and recovery. Although testing under dynamic conditions is desirable, this type of measurement is more complex and less straightforward than a static evaluation. The devices that perform this function are more technologically complex, have a higher cost and, above all, require sufficient experience in use and the processing procedure. The main protocols and most of the works in the literature are focused only on the static aspect of this measurement and on the determinations of a single descriptive parameter for HGS. Such dynamics are particularly valuable in clinical settings where they can offer diagnostic and prognostic insights. Moreover, this review has identified a significant gap in the literature concerning the metrological validation of these devices. Few studies ensure measurement traceability to international standards, raising concerns about the accuracy and reliability of the data, especially when such measurements are used to support clinical decisions or to design rehabilitation protocols. This lack of standardization can lead to inconsistencies in data interpretation and affect the comparability of studies, thereby limiting the scientific rigor of research in this field.
- (3)
- Endogenous and exogenous factors of influence—There is also a critical need to define standardized testing protocols, which should be universally applicable, yet adaptable to account for variability among different populations and clinical conditions. Adapting measurement protocols to account for endogenous factors such as age, gender, hand size and body mass, as well as exogenous factors such as job occupation and circadian influences, will improve the accuracy of HGS assessments and may better reflect individual capabilities and limitations, providing a more accurate basis for therapeutic or training interventions. Indeed, all measurements, involving living creatures and specifically humans, require a sufficient degree of individuality to be considered valid. Moreover, the procedure of measurement could better reflect individual capabilities and limitations, thereby providing a more accurate basis for therapeutic or training interventions. Specifically, the sport area is characterized by a significant degree of individuality for its athletes, whereas this orientation tends to be limited in the medical field. Thus, the introduction of some corrective parameters, acting on the attributable HGS, could be desirable. In this regard, it could be suggested that first patients be classified as healthy or pathological. Subsequently, a corrective scale could be implemented in accordance with the physiological characteristics and, if applicable, the specific disease of the subject. Certainly, such an effort should require the collaborative efforts of several professionals and the processing of a considerable amount of data.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Landsmeer, J. Power grip and precision handling. Ann. Rheum. Dis. 1962, 21, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Long, C.I.I.; Conrad, P.W.; Hall, E.A.; Furler, S.L. Intrinsic-extrinsic muscle control of the hand in power grip and precision handling: An electromyographic study. J. Bone Jt. Surg. Am. 1970, 52, 853–867. [Google Scholar] [CrossRef]
- Shahimi, N.H.; Goh, C.H.; Mat, S.; Lim, R.; Koh, V.C.A.; Nyman, S.R.; Tan, P.M.; Lim, E. Psychological status and physical performance are independently associated with autonomic function. Biomed. Eng. Online 2022, 21, 28. [Google Scholar] [CrossRef] [PubMed]
- Buendía-Romero, Á.; Hernández-Belmonte, A.; Franco-López, F.; Romero-Borrego, E.; Cava, A.M.; Pallarés, J.G.; Courel-Ibáñez, J. A sensitive and practical evaluation to detect lower-limb strength changes in geriatrics: The isometric knee extension test. Appl. Sci. 2023, 13, 2946. [Google Scholar] [CrossRef]
- Van Lummel, R.C.; Evers, J.; Niessen, M.; Beek, P.J.; Van Dieën, J.H. Older adults with weaker muscle strength stand up from a sitting position with more dynamic trunk use. Sensors 2018, 18, 1235. [Google Scholar] [CrossRef] [PubMed]
- Eckman, M.; Gigliotti, C.; Sutermaster, S.; Butler, P.J.; Mehta, K. Using handgrip strength to screen for diabetes in developing countries. J. Med. Eng. Technol. 2016, 40, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Roman-Liu, D. Upper limb load as a function of repetitive task parameters: Part 1—A model of upper limb load. Int. J. Occup. Saf. Ergon. 2005, 11, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Matveev, M.; Prokopova, R.; Nachev, C. Time-related heart autonomic balance characteristics in healthy subjects. Physiol. Meas. 2003, 24, 727–743. [Google Scholar] [CrossRef] [PubMed]
- Korte, J.; Rauwolf, T.; Thiel, J.N.; Mitrasch, A.; Groschopp, P.; Neidlin, M.; Schmeibser, A.; Braun-Dillaeus, R.; Berg, P. Hemodynamic assessment of the pathological left ventricle function under rest and exercise conditions. Fluids 2023, 8, 71. [Google Scholar] [CrossRef]
- Gil, A.W.; da Silva, R.A.; Pereira, C.; Nascimento, V.B.; Amorim, C.F.; Imaizumi, M.; Teixeira, D.C. Reproducibility of dynamometers in handrail format in evaluating handgrip strength and traction in young and older adults. Med. Eng. Phys. 2022, 100, 103749. [Google Scholar] [CrossRef]
- Urbano, D.; Restivo, M.T.; Barbosa, M.R.; Fernandes, Â.; Abreu, P.; Chousal, M.D.F.; Coelho, T. Handgrip strength time profile and frailty: An exploratory study. Appl. Sci. 2021, 11, 5134. [Google Scholar] [CrossRef]
- Tyagi, O.; Mehta, R.K. Mind over body: A neuroergonomic approach to assessing motor performance under stress in older adults. Appl. Ergon. 2022, 101, 103691. [Google Scholar] [CrossRef] [PubMed]
- Fuss, F.K.; Niegl, G. Finger load distribution in different types of climbing grips. Sports Technol. 2012, 5, 151–155. [Google Scholar] [CrossRef]
- Martínez-Rodríguez, A.; Alacid, F.; Cuestas-Calero, B.J.; Matłosz, P.; López-Plaza, D. Physical and morphological differences between young elite taekwondo and karate players. Appl. Sci. 2023, 13, 10109. [Google Scholar] [CrossRef]
- Bajkowski, D.S.; Cynarski, W.J. Handgrip strength as a distinguishing factor of people training martial arts. Appl. Sci. 2023, 13, 9900. [Google Scholar] [CrossRef]
- Pawlik, D.; Dziubek, W.; Rogowski, Ł.; Struzik, A.; Rokita, A. Strength abilities and serve reception efficiency of youth female volleyball players. Appl. Bionics Biomech. 2022, 2022, 4328761. [Google Scholar] [CrossRef] [PubMed]
- Majstorović, N.; Dopsaj, M.; Grbić, V.; Savić, Z.; Vićentijević, A.; Aničić, Z.; Zadražnik, M.; Toskić, L.; Nešić, G. Isometric strength in volleyball players of different age: A multidimensional model. Appl. Sci. 2020, 10, 4107. [Google Scholar] [CrossRef]
- Nowak, A.; Molik, B.; Kosmol, A.; Szczepaniak, M.; Marszałek, J. Application of the arm-cranking 30-second Wingate Anaerobic Test (the WAnT) to assess power in amputee football players. Acta Bioeng. Biomech. 2021, 23, 13–23. [Google Scholar] [CrossRef] [PubMed]
- de Jesus, K.; Mourão, L.; Roesler, H.; Viriato, N.; de Jesus, K.; Vaz, M.; Fernandes, R.; Vilas-Boas, J.P. 3D device for forces in swimming starts and turns. Appl. Sci. 2019, 9, 3559. [Google Scholar] [CrossRef]
- Kaplan, Ö. Evaluating the relation between dominant and non-dominant hand perimeters and handgrip strength of basketball, volleyball, badminton and handball athletes. Int. J. Environ. Sci. Educ. 2016, 11, 3297–3309. [Google Scholar]
- Tanikawa, Y.; Gao, F.; Miyakawa, M.; Kiryu, T.; Kizuka, T.; Endo, Y.; Okawa, S.; Yamada, Y. Evaluation of muscle activities in human forearms under exercises by diffuse optical tomography. IEEJ Trans. Electron. Inf. Syst. 2012, 132, 374–383. [Google Scholar]
- Lee, S.I.; Mortazavi, B.; Hoffman, H.A.; Lu, D.S.; Li, C.; Paak, B.H.; Garst, J.H.; Razaghy, M.; Espinal, M.; Park, E.; et al. A prediction model for functional outcomes in spinal cord disorder patients using gaussian process regression. IEEE J. Biomed. Health Inf. 2014, 20, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Durand, S.; Ripamonti, M.; Rahmani, A.; Beaune, B. Is handgrip force changed following a 45-min kart driving session in competition? Comput. Methods Biomech. Biomed. Eng. 2013, 16, 112–113. [Google Scholar] [CrossRef] [PubMed]
- Kharb, S.S.; Belokar, R.M.; Kant, S.; Sharma, M. Measurement of handgrip strength of north indian male farmers and its implications in design of farm equipment. Instrum. Mes. Metrol. 2020, 19, 385–389. [Google Scholar] [CrossRef]
- Zhang, F.; Momeni, K.; Ramanujam, A.; Ravi, M.; Carnahan, J.; Kirshblum, S.; Forrest, G.F. Cervical spinal cord transcutaneous stimulation improves upper extremity and hand function in people with complete tetraplegia: A case study. IEEE Trans. Neural Syst. Rehabil. Eng. 2020, 28, 3167–3174. [Google Scholar] [CrossRef] [PubMed]
- Olczak, A.; Truszczyńska-Baszak, A. Assessment of the impact of the Tipstim® device application and the study position on motor coordination and grip strength of the affected upper limb post-ischemic stroke—A randomized parallel crossover trial. Appl. Sci. 2022, 12, 2761. [Google Scholar] [CrossRef]
- Khanicheh, A.; Mintzopoulos, D.; Weinberg, B.; Tzika, A.A.; Mavroidis, C. MR_CHIROD v. 2: Magnetic resonance compatible smart hand rehabilitation device for brain imaging. IEEE Trans. Neural Syst. Rehabil. Eng. 2008, 16, 91–98. [Google Scholar] [CrossRef]
- Garcia-Hernandez, N.; Garza-Martinez, K.; Parra-Vega, V.; Alvarez-Sanchez, A.; Conchas-Arteaga, L. Development of an EMG-based exergaming system for isometric muscle training and its effectiveness to enhance motivation, performance and muscle strength. Int. J. Hum. Comput. Stud. 2019, 124, 44–55. [Google Scholar] [CrossRef]
- Celik, D.; AnaforogluKulunkoglu, B. Photobiomodulation therapy versus extracorporeal shock wave therapy in the treatment of lateral epicondylitis. Photobiomodulation Photomed. Laser Surg. 2019, 37, 269–275. [Google Scholar] [CrossRef]
- Jiang, F.L.; Tang, S.; Eom, S.H.; Lee, J.Y.; Chae, J.H.; Kim, C.H. Distribution of bioelectrical impedance vector analysis and phase angle in korean elderly and sarcopenia. Sensors 2023, 23, 7090. [Google Scholar] [CrossRef]
- Olczak, A.; Truszczyńska-Baszak, A.; Stępień, A. The use of Armeo® Spring device to assess the effect of trunk stabilization exercises on the functional capabilities of the upper limb—An observational study of patients after stroke. Sensors 2022, 22, 4336. [Google Scholar] [CrossRef] [PubMed]
- Straudi, S.; Tramontano, M.; Russo, E.F.; Perrero, L.; Agostini, M.; Gandolfi, M.; Aprile, I.; Paci, M.; Casanova, E.; Marino, D.; et al. Robot-assisted upper limb training for patients with multiple sclerosis: An evidence-based review of clinical applications and effectiveness. Appl. Sci. 2021, 12, 222. [Google Scholar] [CrossRef]
- Kotzian, S.T.; Haider, S.; Grabovac, I.; Schubert, N.; Josef, S. Successful performance of basic gestures in tablet technology in post stroke patients: A feasibility study. Technol. Health Care 2019, 27, 613–622. [Google Scholar] [CrossRef] [PubMed]
- Qamruddin, A.A.; Husain, N.R.N.; Sidek, M.Y.; Hanafi, M.H.; Ripin, Z.M.; Ali, N. Musculoskeletal complications of hand–arm vibration syndrome among tyre shop workers in Kelantan, Malaysia. Int. J. Occup. Saf. Ergon. 2022, 28, 213–222. [Google Scholar] [CrossRef] [PubMed]
- Arjunan, S.P.; Kumar, D.K.; Jayadeva, J. Fractal and twin SVM-based handgrip recognition for healthy subjects and trans-radial amputees using myoelectric signal. Biomed. Eng. 2016, 61, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Zhu, Y.; Ju, Y.; Long, T.; Jin, L.; Zhang, J.; Zhao, Y.; Wang, H.; Wu, R. Changes in nutritional status of cancer patients undergoing proton radiation therapy based on real-world data. J. Health Eng. 2023, 2023, 9260747. [Google Scholar] [CrossRef] [PubMed]
- Khader, A.; Almashaqbeh, S. Handgrip strength and its association with anthropometric measurements at different anatomical positions of arm among young individuals. J. Biomim. Biomater. Biomed. Eng. 2023, 60, 97–107. [Google Scholar] [CrossRef]
- Lopes, M.B.; Silva, L.F.; Dantas, M.A.; Matos, C.M.; Lopes, G.B.; Lopes, A.A. Sex-age-specific handgrip strength and mortality in an incident hemodialysis cohort: The risk explained by nutrition and comorbidities. Int. J. Artif. Organs 2018, 41, 825–832. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Siemionow, V.; Yao, W.; Sahgal, V.; Yue, G.H. Single-trial EEG-EMG coherence analysis reveals muscle fatigue-related progressive alterations in corticomuscular coupling. IEEE Trans. Neural Syst. Rehabil. Eng. 2010, 18, 97–106. [Google Scholar] [CrossRef]
- Hsu, L.I.; Lim, K.W.; Lai, Y.H.; Chen, C.S.; Chou, L.W. Effects of muscle fatigue and recovery on the neuromuscular network after an intermittent handgrip fatigue task: Spectral analysis of electroencephalography and electromyography signals. Sensors 2023, 23, 2440. [Google Scholar] [CrossRef]
- Işik, E.İ.; Soygun, K.; Kahraman, Ö.C.; Koçak, E.F. The effect of the menstrual cycle on the sense of touch, grip strength and manual dexterity of dental students. Int. J. Occup. Saf. Ergon. 2022, 28, 1167–1175. [Google Scholar] [CrossRef]
- Shibuya, K. The activity of the primary motor cortex ipsilateral to the exercising hand decreases during repetitive handgrip exercise. Physiol. Meas. 2011, 32, 1929. [Google Scholar] [CrossRef]
- Huynh, T.H.; Jafari, R.; Chung, W.Y. Noninvasive cuffless blood pressure estimation using pulse transit time and impedance plethysmography. IEEE Trans. Biomed. Eng. 2018, 66, 967–976. [Google Scholar] [CrossRef]
- Sola, J.; Proença, M.; Ferrario, D.; Porchet, J.A.; Falhi, A.; Grossenbacher, O.; Allemann, Y.; Rimoldi, S.F.; Sartori, C. Noninvasive and nonocclusive blood pressure estimation via a chest sensor. IEEE Trans. Biomed. Eng. 2013, 60, 3505–3513. [Google Scholar] [CrossRef]
- Chin, K.Y.; Panerai, R.B. A new noninvasive device for continuous arterial blood pressure monitoring in the superficial temporal artery. Physiol. Meas. 2013, 34, 407. [Google Scholar] [CrossRef]
- Gurley, K.; Shang, Y.; Yu, G. Noninvasive optical quantification of absolute blood flow, blood oxygenation, and oxygen consumption rate in exercising skeletal muscle. J. Biomed. Opt. 2012, 17, 075010. [Google Scholar]
- Shimura, M.; Ueda, T.; Choi, G.M.; Tanahashi, M.; Miyauchi, T. Simultaneous dual-plane CH PLIF, single-plane OH PLIF and dual-plane stereoscopic PIV measurements in methane-air turbulent premixed flames. Proc. Comb. Inst. 2011, 33, 775–782. [Google Scholar] [CrossRef]
- Bowers, E.J.; Murray, A. Effects on baroreflex sensitivity measurements when different protocols are used to induce regular changes in beat-to-beat intervals and systolic pressure. Physiol. Meas. 2004, 25, 523. [Google Scholar] [CrossRef] [PubMed]
- Butterworth, E.J.; Evanochko, W.T.; Pohost, G.M. The 31 P–NMR stress test: An approach for detecting myocardial ischemia. Ann. Biomed. Eng. 2000, 28, 930–933. [Google Scholar] [CrossRef] [PubMed]
- Landry, C.; Hedge, E.T.; Hughson, R.L.; Peterson, S.D.; Arami, A. Accurate blood pressure estimation during activities of daily living: A wearable cuffless solution. IEEE J. Biomed. Health Inf. 2021, 25, 2510–2520. [Google Scholar] [CrossRef]
- Park, S.C.; Saiphoklang, N.; Jung, D.; Gomez, D.; Phillips, J.E.; Dolezal, B.A.; Tashkin, D.P.; Barjaktarevic, I.; Cooper, C.B. Use of a wearable biosensor to study heart rate variability in chronic obstructive pulmonary disease and its relationship to disease severity. Sensors 2022, 22, 2264. [Google Scholar] [CrossRef] [PubMed]
- Di Rienzo, M.; Avolio, A.; Rizzo, G.; Zeybek, Z.M.I.; Cucugliato, L. Multi-site pulse transit times, beat-to-beat blood pressure, and isovolumic contraction time at rest and under stressors. IEEE J. Biomed. Health Inf. 2021, 26, 561–571. [Google Scholar] [CrossRef]
- Phillips, D.A.; Del Vecchio, A.R.; Carroll, K.; Matthews, E.L. Developing a practical application of the isometric squat and surface electromyography. Biomechanics 2021, 1, 145–151. [Google Scholar] [CrossRef]
- Rojek, A.M.; Wood, R.E.; Stewart, I.B. The effect of changing limb position on the validity of venous occlusion plethysmography. Physiol. Meas. 2007, 28, 861. [Google Scholar] [CrossRef] [PubMed]
- Soller, B.R.; Hagan, R.D.; Shear, M.; Walz, J.M.; Landry, M.; Anunciacion, D.; Orquiola, A.; Heard, S.O. Comparison of intramuscular and venous blood pH, PCO2 and PO2 during rhythmic handgrip exercise. Physiol. Meas. 2007, 28, 639. [Google Scholar] [CrossRef]
- Raamat, R.; Talts, J.; Jagomägi, K. Application of amplitude-based and slope-based algorithms to determine beat-to-beat finger arterial compliance during handgrip exercise. Med. Eng. Phys. 2008, 30, 67–74. [Google Scholar] [CrossRef]
- Raamat, R.; Jagomägi, K.; Talts, J.; Toska, K.; Walløe, L. Recording of short-term finger blood pressure changes induced by an arterial occlusive thigh cuff: Comparison between the modified oscillometric and Finapres techniques. Physiol. Meas. 2001, 22, 13. [Google Scholar] [CrossRef]
- Wolff, C.; Steinheimer, P.; Warmerdam, E.; Dahmen, T.; Slusallek, P.; Schlinkmann, C.; Chen, F.; Orth, M.; Pohlemann, T.; Ganse, B. Effects of age, body height, body weight, body mass index and handgrip strength on the trajectory of the plantar pressure stance-phase curve of the gait cycle. Front. Bioeng. Biotechnol. 2023, 11, 1110099. [Google Scholar] [CrossRef]
- Hsieh, P.C.; Chang, C.J.; Lin, C.Y. Effect of resistance exercise training combined with plant-based protein supplementation on the prevention of sarcopenia in the middle-aged and elderly. Gerontechnology 2022, 21, 1. [Google Scholar] [CrossRef]
- Hunter, H.H.; Sorbie, G.G.; Grace, F.M.; Gu, Y.; Lam, W.K.; Baker, J.S.; Dutheil, F.; Dias, T.; Ugbolue, U.C. An electromyographic assessment pilot study on the reliability of the forearm muscles during multi-planar maximum voluntary contraction grip and wrist articulation in young males. Technol. Health Care 2022, 30, 713–724. [Google Scholar] [CrossRef]
- Yusopa, Z.M.; Zain, M.M.; Hussein, M.; Musa, A.R. Tremorx: An assistive device to improve tremor patient writing capability. J. Teknol. 2016, 78, 103–108. [Google Scholar] [CrossRef]
- Le, T.; Shim, A.L.; Newman, D. Does a relationship between handgrip strength and coincidence anticipation timing exist among young adults: A pilot study. Int. J. Occup. Saf. Ergon. 2022, 28, 2546–2550. [Google Scholar] [CrossRef]
- Wu, Y.; Chen, Y.; Ye, Y.; Yan, T.; Song, R. Age-related differences in complexity during handgrip control using multiscale entropy. IEEE Access 2018, 6, 45552–45561. [Google Scholar] [CrossRef]
- de Mathelin, M.; Nageotte, F.; Zanne, P.; Dresp-Langley, B. Sensors for expert grip force profiling: Towards benchmarking manual control of a robotic device for surgical tool movements. Sensors 2019, 19, 4575. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://lafayetteevaluation.com/ (accessed on 24 June 2024).
- Available online: https://www.vernier.com/product/hand-dynamometer/ (accessed on 24 June 2024).
- Patel, T.; Sanjog, J.; Karmakar, S. Isometric handgrip strength of agricultural workers from northeast region of India. Agric. Eng. Int. CIGR J. 2015, 17, 130–140. [Google Scholar]
- Wang, Y.; Zheng, L.; Yang, J.; Wang, S. A grip strength estimation method using a novel flexible sensor under different wrist angles. Sensors 2022, 22, 2002. [Google Scholar] [CrossRef]
- Manto, M.; Van DenBraber, N.; Grimaldi, G.; Lammertse, P. A new myohaptic instrument to assess wrist motion dynamically. Sensors 2010, 10, 3180–3194. [Google Scholar] [CrossRef] [PubMed]
- Takanokura, M. Optimal handgrip height of four-wheeled walker on various road conditions to reduce muscular load for elderly users with steady walking. J. Biomech. 2010, 43, 843–848. [Google Scholar] [CrossRef] [PubMed]
- Allégue, H.; Turki, O.; Oranchuk, D.J.; Khemiri, A.; Schwesig, R.; Chelly, M.S. The effect of combined isometric and plyometric training versus contrast strength training on physical performance in male junior handball players. Appl. Sci. 2023, 13, 9069. [Google Scholar] [CrossRef]
- Legg, H.S.; Arnold, C.M.; Farthing, J.P.; Lanovaz, J.L. Age differences in upper extremity joint moments and strength during a laboratory-based tether-release forward fall arrest in older women. J. Biomech. 2022, 138, 111107. [Google Scholar] [CrossRef]
- Borg, E.; Borg, G. A demonstration of level-anchored ratio scaling for prediction of grip strength. Appl. Ergon. 2013, 44, 835–840. [Google Scholar] [CrossRef]
- Hwang, Y.; Hong, G.R.S. Predictors of driving cessation in community-dwelling older adults: A 3-year longitudinal study. Transp. Res. F Traffic Psychol. Behav. 2018, 52, 202–209. [Google Scholar] [CrossRef]
- Maikala, R.V.; Bhambhani, Y.N. Functional changes in cerebral and paraspinal muscle physiology of healthy women during exposure to whole-body vibration. Accid. Anal. Prev. 2008, 40, 943–953. [Google Scholar] [CrossRef] [PubMed]
- Nikodelis, T.; Savvoulidis, S.; Athanasakis, P.; Chalitsios, C.; Loizidis, T. Comparative study of validity and reliability of two handgrip dynamometers: K-force grip and Jamar. Biomechanics 2021, 1, 73–82. [Google Scholar] [CrossRef]
- Available online: https://www.artisantg.com/Scientific/72187-1/Performance-Health-Jamar-5030J1-Hydraulic-Hand-Dynamometer (accessed on 24 June 2024).
- Available online: https://www.performancehealth.ca/amfile/file/download/file/5365/product/48337/ (accessed on 24 June 2024).
- Available online: https://www.si-instruments.com/download-centre/lafayette/jamar-plus-digital-dynamometer.html (accessed on 24 June 2024).
- Jeon, Y.J.; Lee, S.K.; Shin, C. Relative hand grip and back muscle strength, but not mean muscle strength, as risk factors for incident metabolic syndrome and its metabolic components: 16 years of follow-up in a population-based cohort study. Appl. Sci. 2021, 11, 5198. [Google Scholar] [CrossRef]
- Available online: https://www.takei-si.co.jp/products/product_type/health-promotion/physical-fitness-test/muscle-strength-physical-fitness-test/ (accessed on 24 June 2024).
- Kotoh, Y.; Saeki, I.; Yamasaki, T.; Sasaki, R.; Tanabe, N.; Oono, T.; Matsuda, T.; Hisanaga, T.; Matsumoto, T.; Hidaka, I.; et al. Effect of handgrip strength on clinical outcomes of patients with hepatocellular carcinoma treated with Lenvatinib. Appl. Sci. 2020, 10, 5403. [Google Scholar] [CrossRef]
- Available online: https://www.takei-si.co.jp/products/1208/ (accessed on 24 June 2024).
- Roman-Liu, D.; Tokarski, T.; Mazur-Różycka, J. Is the grip force measurement suitable for assessing overall strength regardless of age and gender? Measurement 2021, 176, 109093. [Google Scholar] [CrossRef]
- Available online: https://www.kern-sohn.com/cgi-bin/cosmoshop/lshop.cgi?action=showdetail&ls=en&rubnum=260804&artnum=MAP%20130K1 (accessed on 24 June 2024).
- Available online: https://www.kern-sohn.com/cgi-bin/cosmoshop/lshop.cgi?action=showdetail&ls=en&rubnum=260804&artnum=MAP%2080K1 (accessed on 24 June 2024).
- Available online: https://www.camryscalestore.com/products/camry-digital-hand-dynamometer-grip-strength-measurement-meter-auto-capturing-hand-grip-power (accessed on 24 June 2024).
- Fiorini, L.; Coviello, L.; Sorrentino, A.; Sancarlo, D.; Ciccone, F.; D’Onofrio, G.; Mancioppi, G.; Rovini, E.; Cavallo, F. User profiling to enhance clinical assessment and human–robot interaction: A feasibility study. Int. J. Soc. Robot. 2023, 15, 501–516. [Google Scholar] [CrossRef]
- Available online: https://www.camry.cn/product/electroni-hand-dynamometer.html (accessed on 24 June 2024).
- Available online: https://www.fab-ent.com/evaluation/strength/baseline-hydraulic-hand-dynamometers/ (accessed on 24 June 2024).
- Available online: https://www.sport-thieme.com/Therapy-psychomotricity/Exercising-improving-mobility/Measuring-devices/art=2775803 (accessed on 24 June 2024).
- Mehta, R.K.; Cavuoto, L.A. The effects of obesity, age, and relative workload levels on handgrip endurance. Appl. Ergon. 2015, 46, 91–95. [Google Scholar] [CrossRef]
- Available online: https://hogganscientific.com/product/microfet-handgrip-dynamometer/ (accessed on 24 June 2024).
- Mohaini, M.A.; Nor, N.S.M.; Mohamad, M.; Ghazali, N.E.; Saputra, H.M. IoT-based instrumented bicycle handlebar for children with autism spectrum disorder. J. Adv. Res. Appl. Mech. 2023, 105, 12–27. [Google Scholar] [CrossRef]
- Kaidi, H.M.; Izhar, M.A.M.; Ahmad, N.; Dziyauddin, R.A.; Sarip, S.; Mashudi, N.A.; Mohamed, N.; Jalil, S.Z.A.; Khan, M.A.A. A smart IoT-based prototype system for rehabilitation monitoring. Int. J. Integr. Eng. 2023, 15, 104–111. [Google Scholar]
- Jahan, M.I.; Chethana, K.; Honnungar, R.V.; Asokan, S. Design and development of optical fiber Bragg grating based device for measurement of handgrip force. Opt. Quantum Electron. 2022, 54, 68. [Google Scholar] [CrossRef]
- Van Drongelen, S.; van den Berg, J.; Arnet, U.; Veeger, D.H.; van der Woude, L.H. Development and validity of an instrumented handbike: Initial results of propulsion kinetics. Med. Eng. Phys. 2011, 33, 1167–1173. [Google Scholar] [CrossRef] [PubMed]
- Ab Rahman, M.H.; Maidin, N.A.; Ahmad, M.N.; Osman, M.H.; Wahid, M.K.; Wahid, M.F.I.; Firdaus, N.S.; Yassim, H.M.; Damanhuri, A.A.M.; Abd Sukor, S.M. The comparison study of handgrip pressure on steering wheel national cars. J. Mech. Eng. 2018, 4, 89–105. [Google Scholar]
- Mohd Fa’iz, W.; Ahamad Aiman, C.Z.; Seri Rahayu, K. Handgrip pressure study on Perodua Car’s steering wheel among male drivers. ARPN J. Eng. Appl. Sci. 2017, 12, 4837–48401. [Google Scholar]
- Yokoyama, M.; Koyama, R.; Yanagisawa, M. An evaluation of hand-force prediction using artificial neural-network regression models of surface EMG signals for handwear devices. J. Sens. 2017, 2017, 3980906. [Google Scholar] [CrossRef]
- Santos Borges, L.; Fernandes, M.H.; Schettino, L.; da Coqueiro, R.S.; Pereira, R. Handgrip explosive force is correlated with mobility in the elderly women. Acta Bioeng. Biomech. 2015, 17, 145–149. [Google Scholar]
- Pylatiuk, C.; Kargov, A.; Schulz, S.; Döderlein, L. Distribution of grip force in three different functional prehension patterns. J. Med. Eng. Technol. 2006, 30, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Paul, J.; Zhao, L.; Ngoi, B.K. Fiber-optic sensor for handgrip-strength monitoring: Conception and design. Appl. Opt. 2005, 44, 3696–3704. [Google Scholar] [CrossRef]
- Fess, E.E.; Moran, C.A. Clinical Assessment Recommendations; American Society of Hand Therapists: Mt. Laurel, NJ, USA, 1981. [Google Scholar]
- Sisneros, K.; Maurya, P.; Johnson, E.; Ford, B.; Palmer, T. Age-related differences in vertical jump height and handgrip strength measurements. Acta Bioeng. Biomech. 2023, 25, 19–26. [Google Scholar] [CrossRef]
- Bani, N.A.; Hassan, M.Z.; Kaidi, H.M.; Hashim, N.F.M.; Dziyauddin, R.A.; Musa, R.; Suhot, M.A.; Usman, S.; Muhammad-Sukki, F.; Abu-Bakar, S.; et al. Assessment of health status of the elderly and pre-elderly at a Malaysia elderly care Centre. Int. J. Integr. Eng. 2018, 10, 10–22. [Google Scholar] [CrossRef]
- Florianovicz, V.C.; Ferraresi, C.; Kuriki, H.U.; Marcolino, A.M.; Barbosa, R.I. Effects of photobiomodulation therapy and restriction of wrist extensor blood flow on grip: Randomized clinical trial. Photobiomodulation Photomed. Laser Surg. 2020, 38, 743–749. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.A.; Sundaraj, K.; Ahmad, R.B.; Ahamed, N.U.; Islam, M.A.; Sundaraj, S. Evaluation of repetitive isometric contractions on the heads of triceps brachii muscle during grip force exercise. Technol. Health Care 2014, 22, 617–625. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Mehta, R.K.; Erraguntla, M.; Sasangohar, F.; Qaraqe, K. Quantifying accelerometer-based tremor features of neuromuscular fatigue in healthy and diabetic adults. IEEE Sens. J. 2020, 20, 11183–11190. [Google Scholar] [CrossRef]
- Schibye, B.; Hansen, A.F.; Søgaard, K.; Christensen, H. Aerobic power and muscle strength among young and elderly workers with and without physically demanding work tasks. Appl. Ergon. 2001, 32, 425–431. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, T.; Bjarnason-Wehrens, B.; Mommertz, S.; Schulte-Eistrup, S.; Willemsen, D.; Sindermann, J.; Predel, H.G.; Reiss, N. Development of exercise-related values in heart failure patients supported with a left ventricular assist device. Int. J. Artif. Organs 2019, 42, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, C.K.; Tu, Y.K.; Tsai, Y.J.; Yang, C.Y.; Lu, C.W. Forearm muscular strength and performance fatigability in orthopaedic surgeons when performing bone screw fixations. Appl. Ergon. 2020, 87, 103135. [Google Scholar] [CrossRef]
- Haddix, C.; Al-Bakri, A.F.; Sunderam, S. Prediction of isometric handgrip force from graded event-related desynchronization of the sensorimotor rhythm. J. Neural Eng. 2021, 18, 056033. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.K.; Liu, L.K.; Woo, J.; Assantachai, P.; Auyeung, T.W.; Bahyah, K.S.; Chou, M.Y.; Chen, L.Y.; Hsu, P.S.; Krairit, O.; et al. Sarcopenia in Asia: Consensus report of the Asian working group for Sarcopenia. J. Am. Med. Dir. Assoc. 2014, 15, 95–101. [Google Scholar] [CrossRef]
- Maris, A.; Coninx, K.; Seelen, H.; Truyens, V.; De Weyer, T.; Geers, R.; Lemmens, M.; Coolen, J.; Stupar, S.; Lamers, I.; et al. The impact of robot-mediated adaptive I-TRAVLE training on impaired upper limb function in chronic stroke and multiple sclerosis. Disabil. Rehabil. Assist. Technol. 2018, 13, 1–9. [Google Scholar] [CrossRef]
- Myers, D.B.; Grennan, D.M.; Palmer, D.G. Hand grip function in patients with rheumatoid arthritis. Arch. Phys. Med. Rehabil. 1980, 61, 369–373. [Google Scholar] [PubMed]
- Andria, G.; Attivissimo, F.; Giaquinto, N.; Lanzolla, A.M.L.; Quagliarella, L.; Sasanelli, N. Functional evaluation of handgrip signals for parkinsonian patients. IEEE Trans. Instrum. Meas. 2006, 55, 1467–1473. [Google Scholar] [CrossRef]
- Saremi, M.; Rostamzadeh, S.; Nasr Esfahani, M. Hand functionality in dentists: The effect of anthropometric dimensions and specialty. Int. J. Occup. Saf. Ergon. 2022, 28, 1473–1481. [Google Scholar] [CrossRef] [PubMed]
- Żyliński, M.; Niewiadomski, W.; Cybulski, G.; Gąsiorowska, A. Device for controlling stimulus self-application during autonomic nervous system tests. Med. Devices Evid. Res. 2021, 1, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Nataraj, R.; Sanford, S. Control modification of grasp force covaries agency and performance on rigid and compliant surfaces. Front. Bioeng. Biotechnol. 2021, 8, 574006. [Google Scholar] [CrossRef] [PubMed]
- Restrepo-Correa, J.H.; Hernández-Arellano, J.L.; Ochoa-Ortiz, C.A.; Maldonado-Macías, A.A. Influence of an armrest support on handgrip strength in different arm and shoulder flexion angles in overhead postures. Int. J. Occup. Saf. Ergon. 2023, 29, 90–98. [Google Scholar] [CrossRef] [PubMed]
- Marković, S.; Dopsaj, M.; Veljković, V. Reliability of sports medical solutions handgrip and Jamar handgrip dynamometer. Meas. Sci. Rev. 2020, 20, 59–64. [Google Scholar] [CrossRef]
- Aziz, A.N.U.; Osman, N.; Rosman, N.A.; Talip, N.K.A.; Chinnasee, C.; Nadzalan, A.M. The effects of elbow flexion angles on handgrip force production among trained women. Int. J. Innov. Technol. Expl Eng. 2019, 8, 730–732. [Google Scholar] [CrossRef]
- Hou, W.; Zheng, X.; Jiang, Y.; Zheng, J.; Peng, C.; Xu, R. A study of models for handgrip force prediction from surface electromyography of extensor muscle. Biomed. Eng. Appl. Basis Commun. 2009, 21, 81–88. [Google Scholar] [CrossRef]
- Bechtol, C.O. Grip test: The use of a dynamometer with adjustable handle spacings. J. Bone Jt. Surg. Am. 1954, 36-A, 820–832. [Google Scholar]
- Kharb, S.S.; Kumar, P.; Malik, A. Anthropometric measurement of haryana male farmers and its implications in design of agricultural tools and equipment. J. Inst. Eng. Ser. C 2023, 104, 925–939. [Google Scholar] [CrossRef]
- Ramos, M.; Palmeira, L.; Oliveira, T.; Melo, R.; Lopes, C.; Carvalho, I.; Chagas, D.; Batista, L.A. Association of handgrip strength with anthropometry of a Brazilian healthy adolescent sample. Int. J. Occup. Saf. Ergon. 2023, 29, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Krzysztoszek, J.; Maciaszek, J.; Bronikowski, M.; Karasiewicz, M.; Laudańska-Krzemińska, I. Comparison of fitness and physical activity levels of obese people with hypertension. Appl. Sci. 2021, 11, 10330. [Google Scholar] [CrossRef]
- Vanderburgh, P.M.; Mahar, M.T.; Chou, C.H. Allometric scaling of grip strength by body mass in college-age men and women. Res. Q. Exerc. Sport. 1995, 66, 80–84. [Google Scholar] [CrossRef]
- Godziuk, K.; Prado, C.M.; Woodhouse, L.J.; Forhan, M. Prevalence of sarcopenic obesity in adults with end-stage knee osteoarthritis. Osteoarthr. Cartil. 2019, 27, 1735–1745. [Google Scholar] [CrossRef] [PubMed]
- Usman, S.; Rusli, F.A.; Bani, N.A.; Muhtazaruddin, M.N.; Muhammad-Sukki, F. A study on the correlation between hand grip and age using statistical and machine learning analysis. Int. J. Integr. Eng. 2023, 15, 84–93. [Google Scholar] [CrossRef]
- Wen, W.L.; Lin, H.C.; Yu, H.C.; Chen, Y.P.; Liang, C.C.; Hsu, W.H.; Hsu, J.S.; Shih, M.C.; Lee, M.Y.; Chen, S.C. Appendicular skeletal muscle mass index and physiological performance in post-menopausal women with total thyroidectomy. Appl. Sci. 2021, 11, 7555. [Google Scholar] [CrossRef]
- Campo-Prieto, P.; Cancela-Carral, J.M.; Rodríguez-Fuentes, G. Feasibility and effects of an immersive virtual reality exergame program on physical functions in institutionalized older adults: A randomized clinical trial. Sensors 2022, 22, 6742. [Google Scholar] [CrossRef] [PubMed]
- Schubert, P.; Liebherr, M.; Kersten, S.; Haas, C.T. Biomechanical demand analysis of older passengers in a standing position during bus transport. J. Transp. Health 2017, 4, 226–236. [Google Scholar] [CrossRef]
- McGarvey, S.R.; Morrey, B.F.; Askew, L.J. An KN Reliability of isometric strength testing: Temporal factors and strength variation. Clin. Orthop. Relat. Res. 1984, 185, 301–305. [Google Scholar] [CrossRef]
- Jain, R.; Rana, K.B.; Meena, M.L. Effect of work experience and upper-limb muscle activity on grip strength of manual workers. Int. J. Occup. Saf. Ergon. 2023, 29, 315–320. [Google Scholar] [CrossRef]
- Tokarski, T.; Roman-Liu, D.; Kamińska, J. The influence of age and type of force on muscle strength capabilities in women. Int. J. Occup. Saf. Ergon. 2012, 18, 47–57. [Google Scholar] [CrossRef] [PubMed]
- Chandra, A.M.; Ghosh, S.; Iqbal, R.; Sadhu, N. A comparative assessment of the impact of different occupations on workers’ static musculoskeletal fitness. Int. J. Occup. Saf. Ergon. 2007, 13, 271–278. [Google Scholar] [CrossRef] [PubMed]
| Name, Model | Manufacturer, Country | Measurement Range | Accuracy | Resolution | Size | Weight | References |
|---|---|---|---|---|---|---|---|
| Jamar, 5030J1 | Patterson Medical | 0 to 90 kg | ±1% | 1 kg | 102 mm × 216 mm × 318 mm | 0.4 kg | [72,77] |
| Jamar, Smart | Patterson Medical | 0 to 90.0 kg | ±1% | 0.1 kg | 102 mm × 267 mm × 356 mm | 1 kg | [11,78] |
| Jamar, Plus + | Patterson Medical | 0 to 90.0 kg | ±1% | 0.1 kg | 102 mm × 267 mm × 356 mm | 1 kg | [28,79] |
| T.K.K., 5102 | Takei Scientific Instruments (Niigata, Japan) | 0 to 100.0 kg | ±2.0 kg | 0.5 kg | 59 mm × 154 mm × 235 mm | 0.6 kg | [80,81] |
| T.K.K., 5401 | Takei Scientific Instruments | 0 to 100.0 kg | ±2.0 kg | 0.1 kg | 62 mm × 154 mm × 235 mm | 0.6 kg | [82,83] |
| MAP, 130K1 | Kern & Sohn (Baden-Württemberg, Germany) | 0 to 130.0 kg | - | 0.1 kg | 55 mm × 102 mm × 212 mm | 0.4 kg | [84,85] |
| MAP, 80K1 | Kern & Sohn | 0 to 80.0 kg | - | 0.1 kg | 55 mm × 102 mm × 212 mm | 0.4 kg | [23,86] |
| Camry, EH101 | Camry Electronic (Zhaoqing, China) | 0 to 90.0 kg | ±0.5 kg | 0.1 kg | 30 mm × 125 mm × 195 mm | - | [26,87] |
| Camry, EH201R | Camry Electronic | 0 to 90.0 kg | - | 0.1 kg | 78 mm × 139 mm × 227 mm | 0.2 kg | [88,89] |
| Baseline, lite 12-0241 | Baseline Instruments (White Plains, NY, USA) | 0 to 90 kg | ±2% | 1 kg | 30 mm × 152 mm × 254 mm | 1.3 kg | [16,90] |
| Saehan, SH5001 | Saehan (Yongin-si, Republic of Korea) | 0 to 90 kg | ±1% | 1 kg | 72 mm × 130 mm × 250 mm | 0.7 kg | [18,91] |
| MicroFET, 4 | Hoggan Scientific (Salt Lake City, UT, USA) | 0 to 90.72 kg | ±1% | 0.45 kg | 102 mm × 305 mm × 356 mm | 1.8 kg | [92,93] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Quattrocchi, A.; Garufi, G.; Gugliandolo, G.; De Marchis, C.; Collufio, D.; Cardali, S.M.; Donato, N. Handgrip Strength in Health Applications: A Review of the Measurement Methodologies and Influencing Factors. Sensors 2024, 24, 5100. https://doi.org/10.3390/s24165100
Quattrocchi A, Garufi G, Gugliandolo G, De Marchis C, Collufio D, Cardali SM, Donato N. Handgrip Strength in Health Applications: A Review of the Measurement Methodologies and Influencing Factors. Sensors. 2024; 24(16):5100. https://doi.org/10.3390/s24165100
Chicago/Turabian StyleQuattrocchi, Antonino, Giada Garufi, Giovanni Gugliandolo, Cristiano De Marchis, Domenicantonio Collufio, Salvatore Massimiliano Cardali, and Nicola Donato. 2024. "Handgrip Strength in Health Applications: A Review of the Measurement Methodologies and Influencing Factors" Sensors 24, no. 16: 5100. https://doi.org/10.3390/s24165100
APA StyleQuattrocchi, A., Garufi, G., Gugliandolo, G., De Marchis, C., Collufio, D., Cardali, S. M., & Donato, N. (2024). Handgrip Strength in Health Applications: A Review of the Measurement Methodologies and Influencing Factors. Sensors, 24(16), 5100. https://doi.org/10.3390/s24165100











