Inertial Measurement Unit and Heart Rate Monitoring to Assess Cardiovascular Fitness of Manual Wheelchair Users during the Six-Minute Push Test
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Hardware
2.3. Study Protocol
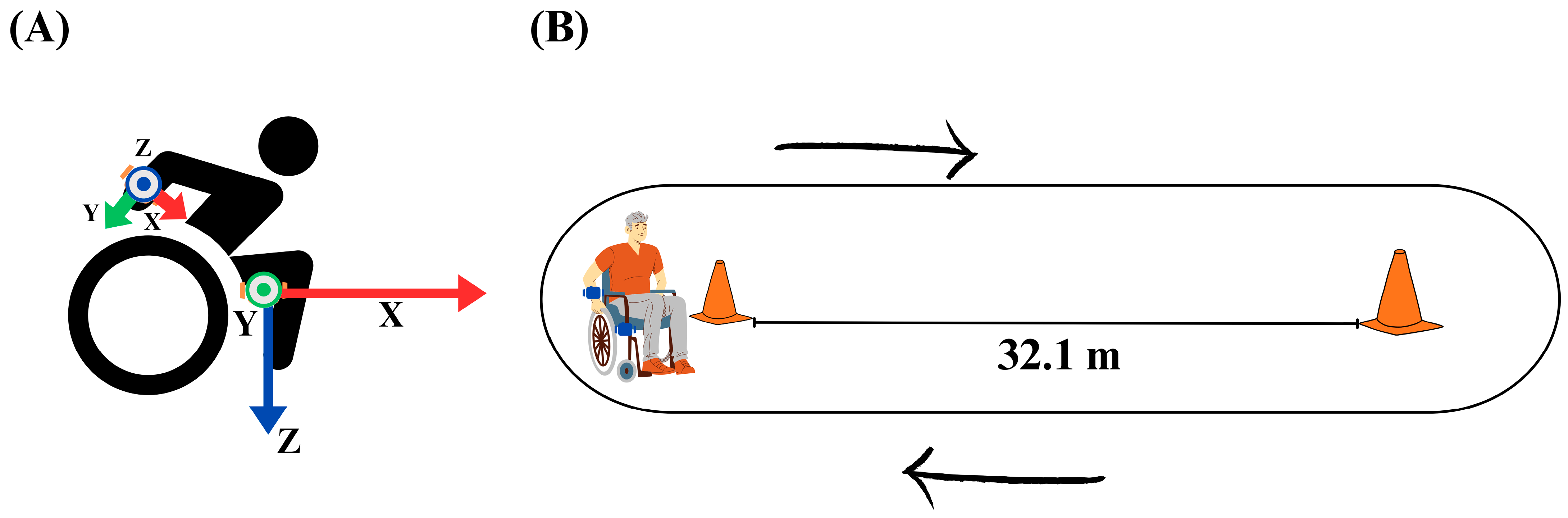
2.3.1. IMU and Heart Rate Monitor Placement
2.3.2. Six-Minute Push Test
2.4. Data Analysis
2.4.1. Number of Laps
2.4.2. Distance
2.4.3. Speed
2.4.4. Propulsion Cycle and Cadence
2.4.5. Heart Rate
2.4.6. Conventional Measurements
2.5. Statistical Analyses
3. Results
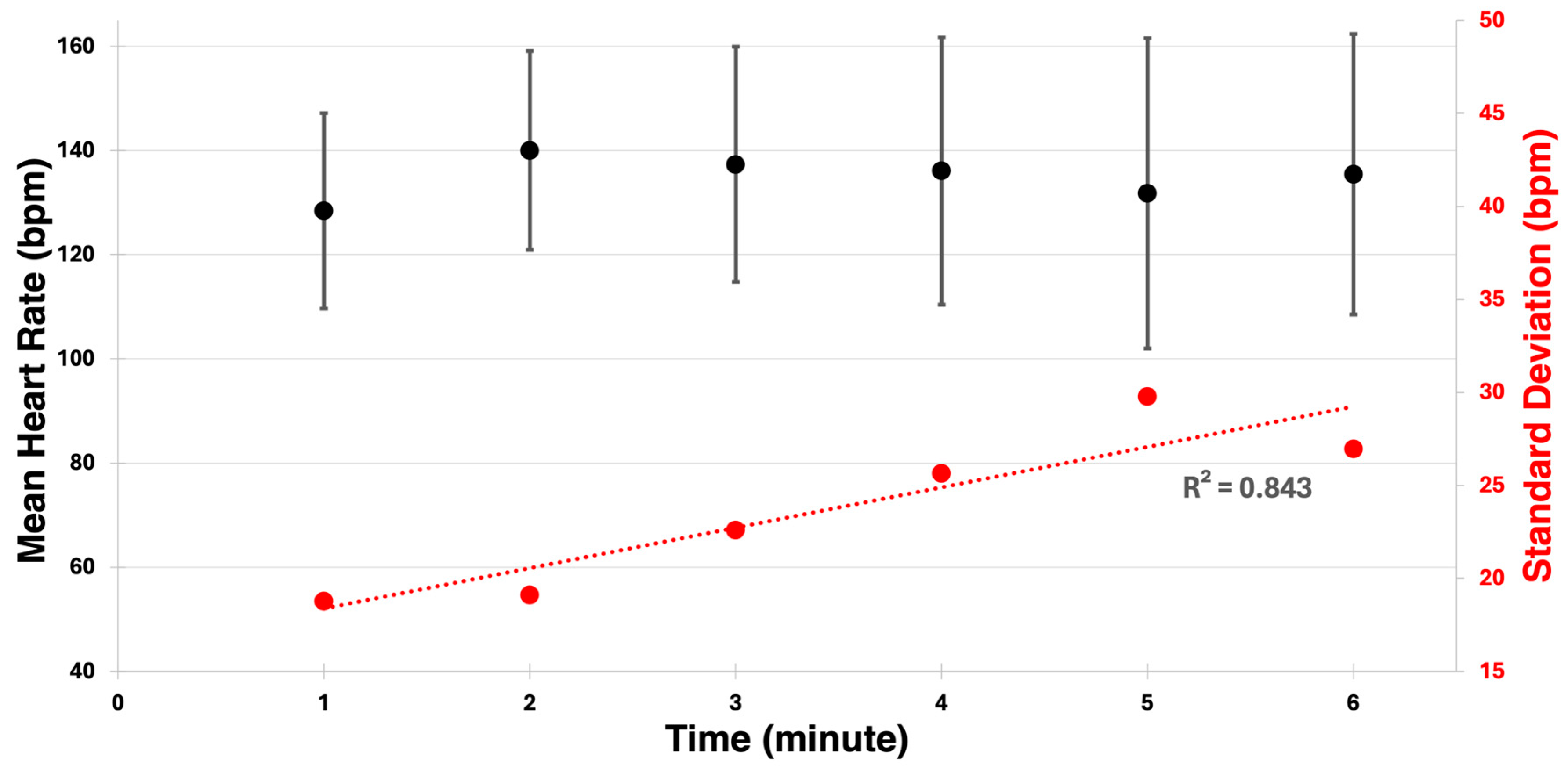
3.1. Six-Minute Push Test Data
3.2. Statistical Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Li, Y.; Li, F.M.; Carrington, P. Breaking the ‘Inescapable’ Cycle of Pain: Supporting Wheelchair Users’ Upper Extremity Health Awareness and Management with Tracking Technologies. In Proceedings of the CHI: Conference on Human Factors in Computing, Hamburg Germany, 23–28 April 2023; pp. 1–17. [Google Scholar]
- Dunstan, D.W.; Dogra, S.; Carter, S.E.; Owen, N. Sit Less and Move More for Cardiovascular Health: Emerging Insights and Opportunities. Nat. Rev. Cardiol. 2021, 18, 637–648. [Google Scholar] [CrossRef] [PubMed]
- Nie, Q.; Rice, L.A.; Sosnoff, J.J.; Shen, S.; Rogers, W.A. Understanding Wheelchair Use in Older Adults from the National Health and Aging Trends Study. Arch. Phys. Med. Rehabil. 2023, 105, 514–524. [Google Scholar] [CrossRef] [PubMed]
- Fasipe, G.; Goršič, M.; Rahman, M.H.; Rammer, J. Community Mobility and Participation Assessment of Manual Wheelchair Users: A Review of Current Techniques and Challenges. Front. Hum. Neurosci. 2024, 17, 1331395. [Google Scholar] [CrossRef] [PubMed]
- Paterson, D.H.; Warburton, D.E. Physical Activity and Functional Limitations in Older Adults: A Systematic Review Related to Canada’s Physical Activity Guidelines. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 38. [Google Scholar] [CrossRef] [PubMed]
- Van der Westhuizen, L.; Mothabeng, D.J.; Nkwenika, T.M. The Relationship between Physical Fitness and Community Participation in People with Spinal Cord Injury. S. Afr. J. Physiother. 2017, 73, a354. [Google Scholar] [CrossRef] [PubMed]
- Damen, K.M.S.; Takken, T.; de Groot, J.F.; Backx, F.J.G.; Radder, B.; Roos, I.C.P.M.; Bloemen, M.A.T. 6-Minute Push Test in Youth Who Have Spina Bifida and Who Self-Propel a Wheelchair: Reliability and Physiologic Response. Phys. Ther. 2020, 100, 1852–1861. [Google Scholar] [CrossRef]
- Beaverson, J.; Beaudreau, L.; Filkowski, J.; Robinson, C.A.; Matsuda, P.N.; Shumway-Cook, A. Assessing Factors Impacting Community Mobility after Stroke: A Pilot Study. J. Neurol. Phys. Ther. 2005, 29, 203. [Google Scholar] [CrossRef]
- Cowan, R.E.; Callahan, M.K.; Nash, M.S. The 6-Min Push Test Is Reliable and Predicts Low Fitness in Spinal Cord Injury. Med. Sci. Sports Exerc. 2012, 44, 1993–2000. [Google Scholar] [CrossRef]
- Solanki, R.; Chaudhari, P.; Bhise, A. Cardio Respiratory Fitness Testing in Spinal Cord Injury Patients Using 6 Minute Push Test. Health J. 2017, 7, 60–63. [Google Scholar]
- Verschuren, O.; Ketelaar, M.; De Groot, J.; Vila Nova, F.; Takken, T. Reproducibility of Two Functional Field Exercise Tests for Children with Cerebral Palsy Who Self-Propel a Manual Wheelchair. Dev. Med. Child Neurol. 2013, 55, 185–190. [Google Scholar] [CrossRef]
- Tsang, K.; Hiremath, S.V.; Crytzer, T.M.; Dicianno, B.E.; Ding, D. Validity of Activity Monitors in Wheelchair Users: A Systematic Review. J. Rehabil. Res. Dev. 2016, 53, 641. [Google Scholar] [CrossRef] [PubMed]
- Kobsar, D.; Charlton, J.M.; Tse, C.T.; Esculier, J.-F.; Graffos, A.; Krowchuk, N.M.; Thatcher, D.; Hunt, M.A. Validity and Reliability of Wearable Inertial Sensors in Healthy Adult Walking: A Systematic Review and Meta-Analysis. J. Neuroeng. Rehabil. 2020, 17, 62. [Google Scholar] [CrossRef] [PubMed]
- Storm, F.A.; Cesareo, A.; Reni, G.; Biffi, E. Wearable Inertial Sensors to Assess Gait during the 6- Minute Walk Test: A Systematic Review. Sensors 2020, 20, 2660. [Google Scholar] [CrossRef] [PubMed]
- Salvi, D.; Poffley, E.; Orchard, E.; Tarassenko, L. The Mobile-Based 6-Minute Walk Test: Usability Study and Algorithm Development and Validation. JMIR MHealth UHealth 2020, 8, 13756. [Google Scholar] [CrossRef] [PubMed]
- Bailo, G.; Saibene, F.L.; Bandini, V.; Arcuri, P.; Salvatore, A.; Meloni, M.; Castagna, A.; Navarro, J.; Lencioni, T.; Ferrarin, M.; et al. Characterization of Walking in Mild Parkinson’s Disease: Reliability, Validity and Discriminant Ability of the Six-Minute Walk Test Instrumented with a Single Inertial Sensor. Sensors 2024, 24, 662. [Google Scholar] [CrossRef] [PubMed]
- Fortune, E.; Cloud-Biebl, B.A.; Madansingh, S.I.; Ngufor, C.G.; Van Straaten, M.G.; Goodwin, B.M.; Murphree, D.H.; Zhao, K.D.; Morrow, M.M. Estimation of Manual Wheelchair-Based Activities in the Free-Living Environment Using a Neural Network Model with Inertial Body-Worn Sensors. J. Electromyogr. Kinesiol. 2022, 62, 102337. [Google Scholar] [CrossRef] [PubMed]
- Vries, W.H.K.; Slikke, R.M.A.; Dijk, M.P.; Arnet, U. Real-Life Wheelchair Mobility Metrics from IMUs. Sensors 2023, 23, 7174. [Google Scholar] [CrossRef] [PubMed]
- Sonenblum, S.E.; Sprigle, S.; Lopez, R.A. Manual Wheelchair Use: Bouts of Mobility in Everyday Life. Rehabil. Res. Pract. 2012, 2012, 753165. [Google Scholar] [CrossRef]
- Sonenblum, S.E.; Sprigle, S.; Caspall, J.; Lopez, R. Validation of an Accelerometer-Based Method to Measure the Use of Manual Wheelchairs. Med. Eng. Phys. 2012, 34, 781–786. [Google Scholar] [CrossRef]
- Marco-Ahulló, A.; Montesinos-Magraner, L.; Gonzalez, L.-M.; Llorens, R.; Segura-Navarro, X.; García-Massó, X. Validation of Using Smartphone Built-In Accelerometers to Estimate the Active Energy Expenditures of Full-Time Manual Wheelchair Users with Spinal Cord Injury. Sensors 2021, 21, 1498. [Google Scholar] [CrossRef]
- Goodwin, B.M.; Jahanian, O.; Van Straaten, M.G.; Fortune, E.; Madansingh, S.I.; Cloud-Biebl, B.A.; Zhao, K.D.; Morrow, M.M. Application and Reliability of Accelerometer-Based Arm Use Intensities in the Free-Living Environment for Manual Wheelchair Users and Able-Bodied Individuals. Sensors 2021, 21, 1236. [Google Scholar] [CrossRef] [PubMed]
- Learmonth, Y.C.; Kinnett-Hopkins, D.; Rice, I.M.; Dysterheft, J.L.; Motl, R.W. Accelerometer Output and Its Association with Energy Expenditure during Manual Wheelchair Propulsion. Spinal Cord 2015, 54, 110–114. [Google Scholar] [CrossRef] [PubMed]
- Kerfeld, C.I.; Hurvitz, P.M.; Bjornson, K.F. Physical Activity Measurement in Children Who Use Mobility Assistive Devices: Accelerometry and Global Positioning System. Pediatr. Phys. Ther. 2021, 33, 92–99. [Google Scholar] [CrossRef] [PubMed]
- Simim, M.A.; de Mello, M.T.; Silva, B.V.; Rodrigues, D.F.; Rosa, J.P.P.; Couto, B.P.; da Silva, A. Load Monitoring Variables in Training and Competition Situations: A Systematic Review Applied to Wheelchair Sports. Adapt. Phys. Act. Q. 2017, 34, 466–483. [Google Scholar] [CrossRef] [PubMed]
- Van Den Berg, R.; De Groot, S.; Swart, K.M.; Van Der Woude, L.H. Physical Capacity after 7 Weeks of Low-Intensity Wheelchair Training. Disabil. Rehabil. 2010, 32, 2244–2252. [Google Scholar] [CrossRef] [PubMed]
- Barfield, J.; Malone, L.A.; Arbo, C.; Jung, A.P. Exercise Intensity during Wheelchair Rugby Training. J. Sports Sci. 2010, 28, 389–398. [Google Scholar] [CrossRef] [PubMed]
- Tolfrey, K.; Goosey-Tolfrey, V.; Campbell, I. Oxygen Uptake-Heart Rate Relationship in Elite Wheelchair Racers. Eur. J. Appl. Physiol. 2001, 86, 174–178. [Google Scholar] [CrossRef] [PubMed]
- Iturricastillo, A.; Yanci, J.; Granados, C.; Goosey-Tolfrey, V. Quantifying Wheelchair Basketball Match Load: A Comparison of Heart-Rate and Perceived-Exertion Methods. Int. J. Sports Physiol. Perform. 2016, 11, 508–514. [Google Scholar] [CrossRef] [PubMed]
- Iturricastillo, A.; Granados, C.; Los Arcos, A.; Yanci, J. Objective and Subjective Methods for Quantifying Training Load in Wheelchair Basketball Small-Sided Games. J. Sports Sci. 2017, 35, 749–755. [Google Scholar] [CrossRef]
- Valent, L.; Zee, W. The Individual Relationship Between Heart Rate And Oxygen Uptake In People With A Tetraplegia: 1909 Board# 48 2: 00 PM-3: 30 PM. Med. Sci. Sports Exerc. 2005, 37, S365–S366. [Google Scholar]
- Calegari, L.; Moreira, I.; Falkowski, A.; Reolão, J.B.C.; Karsten, M.; Deresz, L.F. Agreement between Heart Rate at First Ventilatory Threshold on Treadmill and at 6-Min Walk Test in Coronary Artery Disease Patients on β-Blockers Treatment. J. Exerc. Rehabil. 2021, 17, 362. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Sang, R. Cardiodynamic Variables Measured by Impedance Cardiography during a 6-Minute Walk Test Are Reliable Predictors of Peak Oxygen Consumption in Young Healthy Adults. PLoS ONE 2021, 16, E0252219. [Google Scholar] [CrossRef] [PubMed]
- Lachant, D.J.; Light, A.; Offen, M.; Adams, J.; White, R.J. Heart Rate Monitoring Improves Clinical Assessment during 6-Min Walk. Pulm. Circ. 2020, 10, 2045894020972572. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Jones, A.Y.; Tsang, R.C.; Wang, Y.; Zhou, J.; Zhou, M.; Wang, Y. Noninvasive Investigation of the Cardiodynamic Response to 6MWT in People after Stroke Using Impedance Cardiography. PLoS ONE 2020, 15, E0233000. [Google Scholar] [CrossRef] [PubMed]
- Goršič, M.; Novak, D. Effects of the Auxivo CarrySuit Occupational Exoskeleton When Carrying Front and Side Loads on a Treadmill. J. Biomech. 2023, 156, 111692. [Google Scholar] [CrossRef] [PubMed]
- Nierwińska, K.; Andrzej Myśliwiec, A.K.-R.; Lipowicz, A.; Małecki, A.; Knapik, A. SMART System in the Assessment of Exercise Tolerance in Adults. Sensors 2023, 23, 9624. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Zahradka, N.; Ip, S.; Koneshloo, A.; Roemmich, R.T.; Sehgal, S.; Highland, K.B.; Searson, P.C. Evaluation of Physical Health Status beyond Daily Step Count Using a Wearable Activity Sensor. Npj Digit. Med. 2022, 5, 164. [Google Scholar] [CrossRef] [PubMed]
- Lewis, A.R.; Haydon, D.S.; Phillips, E.J.; Grimshaw, P.N.; Pinder, R.A.; Winter, J.; Robertson, W.S.P.; Portus, M.R. Placement Effects of Inertial Measurement Units on Contact Identification in Wheelchair Racing. Sports Biomech. 2021, 20, 55–70. [Google Scholar] [CrossRef]
- Ramirez Herrera, R.; Momahed Heravi, B.; Barbareschi, G.; Carlson, T.; Holloway, C. Towards a Wearable Wheelchair Monitor: Classification of Push Style Based on Inertial Sensors at Multiple Upper Limb Locations. In Proceedings of the 2018 IEEE International Conference on Systems, Man, and Cybernetics (SMC), Miyazaki, Japan, 7–10 October 2018; pp. 1535–1540. [Google Scholar]
- Nightingale, T.E.; Rouse, P.C.; Thompson, D.; Bilzon, J.L. Measurement of Physical Activity and Energy Expenditure in Wheelchair Users: Methods, Considerations and Future Directions. Sports Med.-Open 2017, 3, 10. [Google Scholar] [CrossRef] [PubMed]
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS Statement: Guidelines for the Six-Minute Walk Test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [Google Scholar] [CrossRef]
- Wheelchair Racing | Maths and Sport. University of Cambridge. Available online: https://sport.maths.org/content/wheelchair-racing?fbclid=IwAR1ySsxV-ddZsM0tR4F2P4OyT42SyHKs3ridzcmH1L0AWIA6lKz22x7j5H8 (accessed on 18 January 2024).
- Uth, N.; Sørensen, H.; Overgaard, K.; Pedersen, P.K. Estimation of VO2max from the Ratio between HR Max and HR Rest—The Heart Rate Ratio Method. Eur. J. Appl. Physiol. 2004, 91, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Castagna, C.; Krustrup, P.; Póvoas, S. Estimation of Maximal Oxygen Uptake Using the Heart Rate Ratio Method in Male Recreational Football Players. Eur. J. Appl. Physiol. 2022, 122, 1421–1428. [Google Scholar] [CrossRef] [PubMed]
- Schober, P.; Boer, C.; Schwarte, L.A. Correlation Coefficients: Appropriate Use and Interpretation. Anesth. Analg. 2018, 126, 1763–1768. [Google Scholar] [CrossRef] [PubMed]
- Pearson’s Correlation Using Stata. Available online: https://statistics.laerd.com/stata-tutorials/pearsons-correlation-using-stata.php (accessed on 28 March 2024).
- Her, Q.L.; Wong, J. Significant Correlation versus Strength of Correlation. Am. J. Health. Syst. Pharm. 2020, 77, 73–75. [Google Scholar] [CrossRef] [PubMed]
- Ratner, B. The Correlation Coefficient: Its Values Range Between +1/−1, or Do They? J. Target. Meas. Anal. Mark. 2009, 17, 139–142. [Google Scholar] [CrossRef]
- Romijnders, R.; Warmerdam, E.; Hansen, C.; Welzel, J.; Schmidt, G.; Maetzler, W. Validation of IMU-Based Gait Event Detection during Curved Walking and Turning in Older Adults and Parkinson’s Disease Patients. J. Neuroeng. Rehabil. 2021, 18, 28. [Google Scholar] [CrossRef] [PubMed]
- Rankin, J.W.; Kwarciak, A.M.; Richter, W.M.; Neptune, R.R. The Influence of Wheelchair Propulsion Technique on Upper Extremity Muscle Demand: A Simulation Study. Clin. Biomech. Bristol Avon 2012, 27, 879–886. [Google Scholar] [CrossRef] [PubMed]
- Jahanian, O.; Van Straaten, M.G.; Goodwin, B.M.; Cain, S.M.; Lennon, R.J.; Barlow, J.D.; Murthy, N.S.; Morrow, M.M.B. Inertial Measurement Unit-Derived Ergonomic Metrics for Assessing Arm Use in Manual Wheelchair Users With Spinal Cord Injury: A Preliminary Report. Top. Spinal Cord Inj. Rehabil. 2021, 27, 12–25. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.-Y.; Lin, C. Developing and Evaluating an Individually Tailored Intervention to Increase Mammography Adherence Among Chinese American Women. Cancer Nurs. 2015, 38, 40–49. [Google Scholar] [CrossRef] [PubMed]
- Durfee, J.; Johnson, T.; Batal, H.; Long, J.; Rinehart, D.; Everhart, R.; Oronce, C.I.; Douglas, I.; Moore, K.; Atherly, A. The Impact of Tailored Intervention Services on Charges and Mortality for Adult Super-Utilizers. Healthcare 2018, 6, 253–258. [Google Scholar] [CrossRef]
- Baker, R.; Camosso-Stefinovic, J.; Gillies, C.; Shaw, E.J.; Cheater, F.; Flottorp, S.; Robertson, N.; Wensing, M.; Fiander, M.; Eccles, M.P.; et al. Tailored Interventions to Address Determinants of Practice. Cochrane Database Syst. Rev. 2015, 2015, CD005470. [Google Scholar] [CrossRef] [PubMed]
- De Fazio, R.; Mastronardi, V.M.; De Vittorio, M.; Visconti, P. Wearable Sensors and Smart Devices to Monitor Rehabilitation Parameters and Sports Performance: An Overview. Sensors 2023, 23, 1856. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Z.; Liu, Y.; Hu, X.; Tang, M.; Wang, L. Validity and Reliability of Inertial Measurement Units on Lower Extremity Kinematics during Running: A Systematic Review and Meta-Analysis. Sports Med.-Open 2022, 8, 86. [Google Scholar] [CrossRef] [PubMed]


| ID | Gender | Age | BMI | Injury Type | Propulsion Pattern |
|---|---|---|---|---|---|
| 1 | Male | 41 | 23.6 | L3 Incomplete Injury | Semicircular |
| 2 | Male | 26 | 32.4 | T10 Incomplete Injury | Semicircular |
| 3 | Male | 32 | 40.8 | Sacral Spina Bifida, Incomplete SCI | Arc |
| 4 | Male | 39 | 29.7 | T8 Complete Injury | Arc |
| 5 | Male | 38 | 19.4 | T6 Complete Injury | Arc |
| 6 | Female | 22 | 23.3 | Neuromuscular Autoimmune Injury | Semicircular |
| 7 | Female | 22 | 39.5 | Spina Bifida L3, 4, 5 | Semicircular |
| 8 | Male | 47 | 28.2 | C6/C7 Incomplete | Arc |
| 9 | Female | 43 | 28.3 | Spina Bifida T12 | Semicircular |
| 10 | Male | 30 | 22.9 | Spinal Cord T10–12 Incomplete | Semicircular |
| ID# | Observer Data | IMU Data | Watch Data | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Counted Laps | Distance (m) | Calculated Completed Laps | Distance with Partial Lap (m) | Mean Speed (m/s) | Cadence (cycles/min) | Mean HR (bpm) | Max HR (bpm) | FMM HR (bpm) | VO2max | |
| 1 | 32 | 1027.2 | 29 | 955.2 | 2.65 | 50.5 | 150.5 | 179 | 170.9 | 28.2 |
| 2 | 27 | 866.7 | 26 | 842.6 | 2.34 | 51.2 | 130.0 | 152 | 134.5 | 27.1 |
| 3 | 28 | 898.8 | 28 | 909.3 | 2.53 | 63.8 | 118.3 | 142 | 125.2 | 25.7 |
| 4 | 25 | 802.5 | 24 | 777.3 | 2.16 | 80.3 | 136 | 172 | 152.9 | 27.9 |
| 5 | 23.5 | 754.4 | 23 | 743.7 | 2.07 | 56.0 | - | - | - | - |
| 6 | 20.5 | 658.1 | 20 | 643.9 | 1.79 | 61.0 | 99.2 | 112 | 106.3 | 23.3 |
| 7 | 22.5 | 722.3 | 22 | 710.3 | 1.97 | 53.5 | 127.2 | 159 | 146.7 | 26.9 |
| 8 | 18 | 577.8 | 17 | 556.3 | 1.55 | 32.3 | 98.6 | 152 | 84.1 | 29.9 |
| 9 | 29 | 930.9 | 29 | 931.0 | 2.59 | 58.8 | 102.6 | 154 | 141.1 | 30.2 |
| 10 | 25.5 | 818.6 | 27 | 879.9 | 2.44 | 69.5 | 127.1 | 159 | 157.9 | 31.6 |
| (σ) | 25.1 (4.2) | 805.8 (133.6) | 25 (4) | 794.0 (130.8) | 2.21 (0.36) | 57.7 (12.7) | 121.1 (17.9) | 153 (19) | 135.5 (27.0) | 27.9 (2.5) |
| Measure | Observer Laps | IMU Laps | Observer Distance (m) | IMU Distance (m) | Mean Speed (m/s) | Mean HR (bpm) | Max HR (bpm) | Final Mean HR (bpm) | VO2max |
|---|---|---|---|---|---|---|---|---|---|
| Observer Laps | 1 | ||||||||
| IMU Laps | 0.947 ** | 1 | |||||||
| Observer Distance (m) | 1.000 ** | 0.947 ** | 1 | ||||||
| IMU Distance (m) | 0.969 ** | 0.997 ** | 0.970 ** | 1 | |||||
| Mean Speed (m/s) | 0.970 ** | 0.997 ** | 0.970 ** | 1.000 ** | 1 | ||||
| Mean HR (bpm) | 0.613 | 0.513 | 0.614 | 0.543 | 0.539 | 1 | |||
| Max HR (bpm) | 0.493 | 0.407 | 0.494 | 0.437 | 0.435 | 0.746 * | 1 | ||
| Final Mean HR (bpm) | 0.754 * | 0.756 * | 0.754 * | 0.762 * | 0.758 * | 0.831 ** | 0.685 * | 1 | |
| VO2max | 0.162 | 0.276 | 0.162 | 0.258 | 0.257 | 0.103 | 0.619 | 0.277 | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fasipe, G.; Goršič, M.; Zabre, E.V.; Rammer, J.R. Inertial Measurement Unit and Heart Rate Monitoring to Assess Cardiovascular Fitness of Manual Wheelchair Users during the Six-Minute Push Test. Sensors 2024, 24, 4172. https://doi.org/10.3390/s24134172
Fasipe G, Goršič M, Zabre EV, Rammer JR. Inertial Measurement Unit and Heart Rate Monitoring to Assess Cardiovascular Fitness of Manual Wheelchair Users during the Six-Minute Push Test. Sensors. 2024; 24(13):4172. https://doi.org/10.3390/s24134172
Chicago/Turabian StyleFasipe, Grace, Maja Goršič, Erika V. Zabre, and Jacob R. Rammer. 2024. "Inertial Measurement Unit and Heart Rate Monitoring to Assess Cardiovascular Fitness of Manual Wheelchair Users during the Six-Minute Push Test" Sensors 24, no. 13: 4172. https://doi.org/10.3390/s24134172
APA StyleFasipe, G., Goršič, M., Zabre, E. V., & Rammer, J. R. (2024). Inertial Measurement Unit and Heart Rate Monitoring to Assess Cardiovascular Fitness of Manual Wheelchair Users during the Six-Minute Push Test. Sensors, 24(13), 4172. https://doi.org/10.3390/s24134172









