Validity of an Inertial Measurement Unit System to Measure Lower Limb Kinematics at Point of Contact during Incremental High-Speed Running
Abstract
:1. Introduction
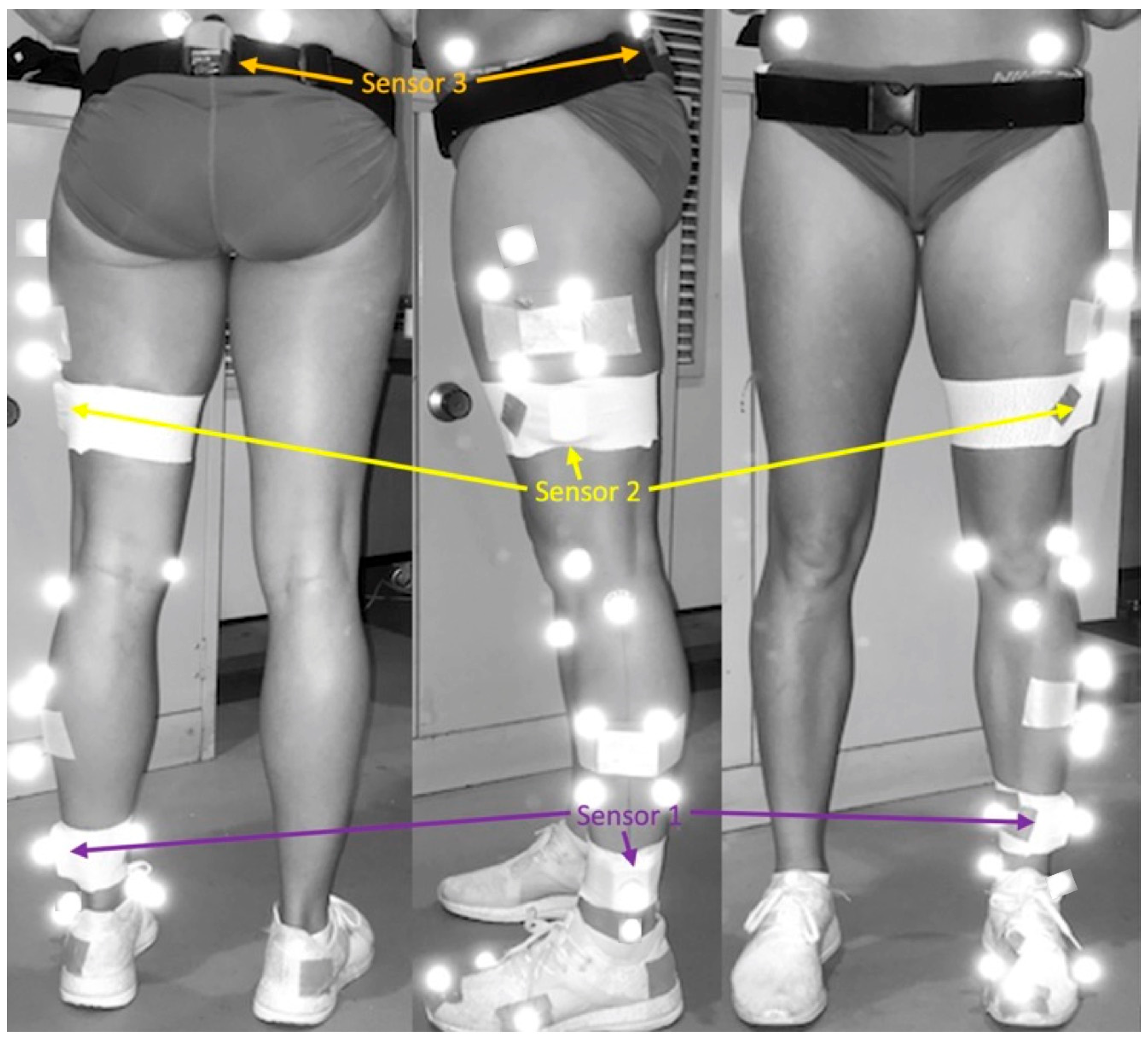
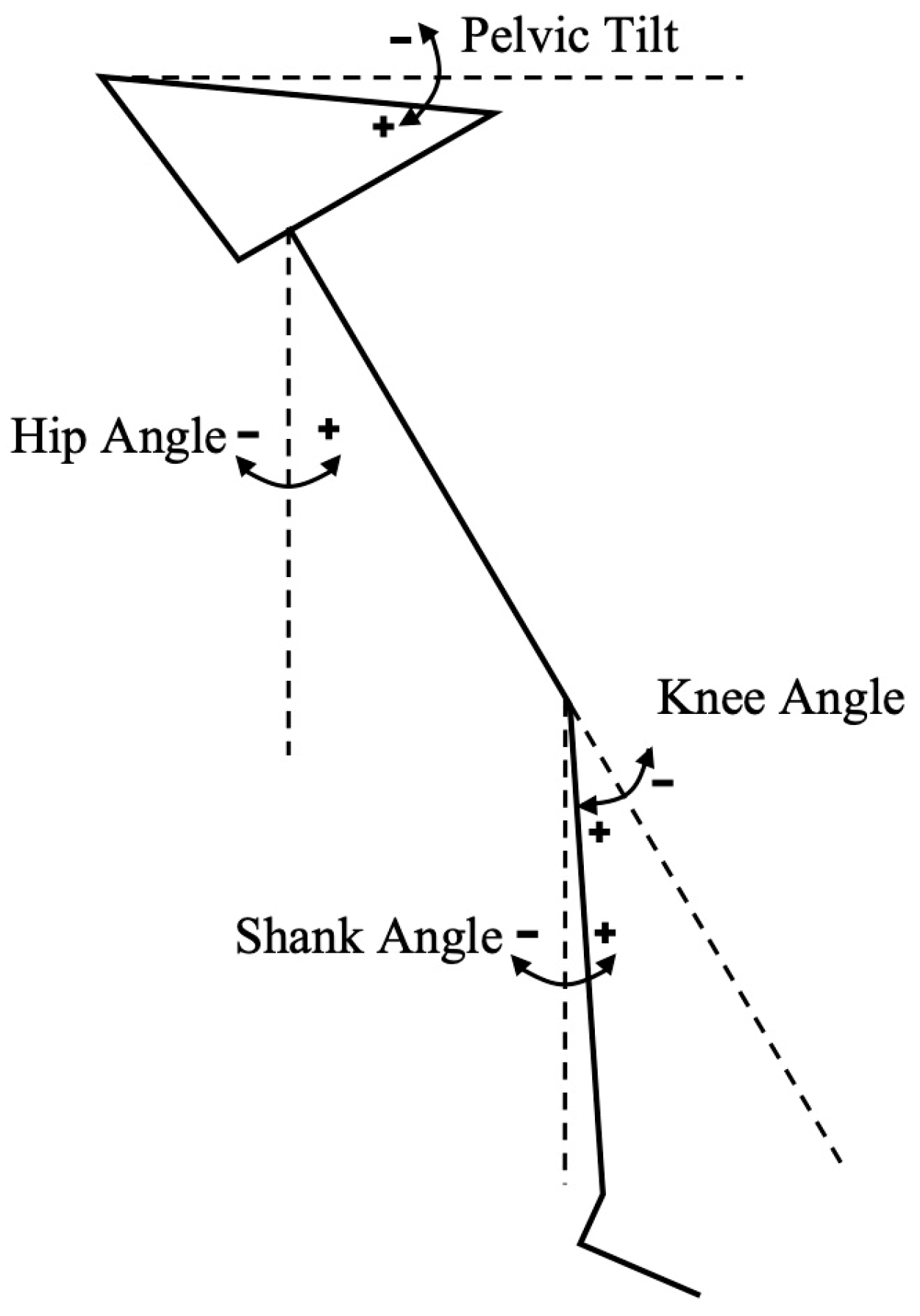
2. Materials and Methods
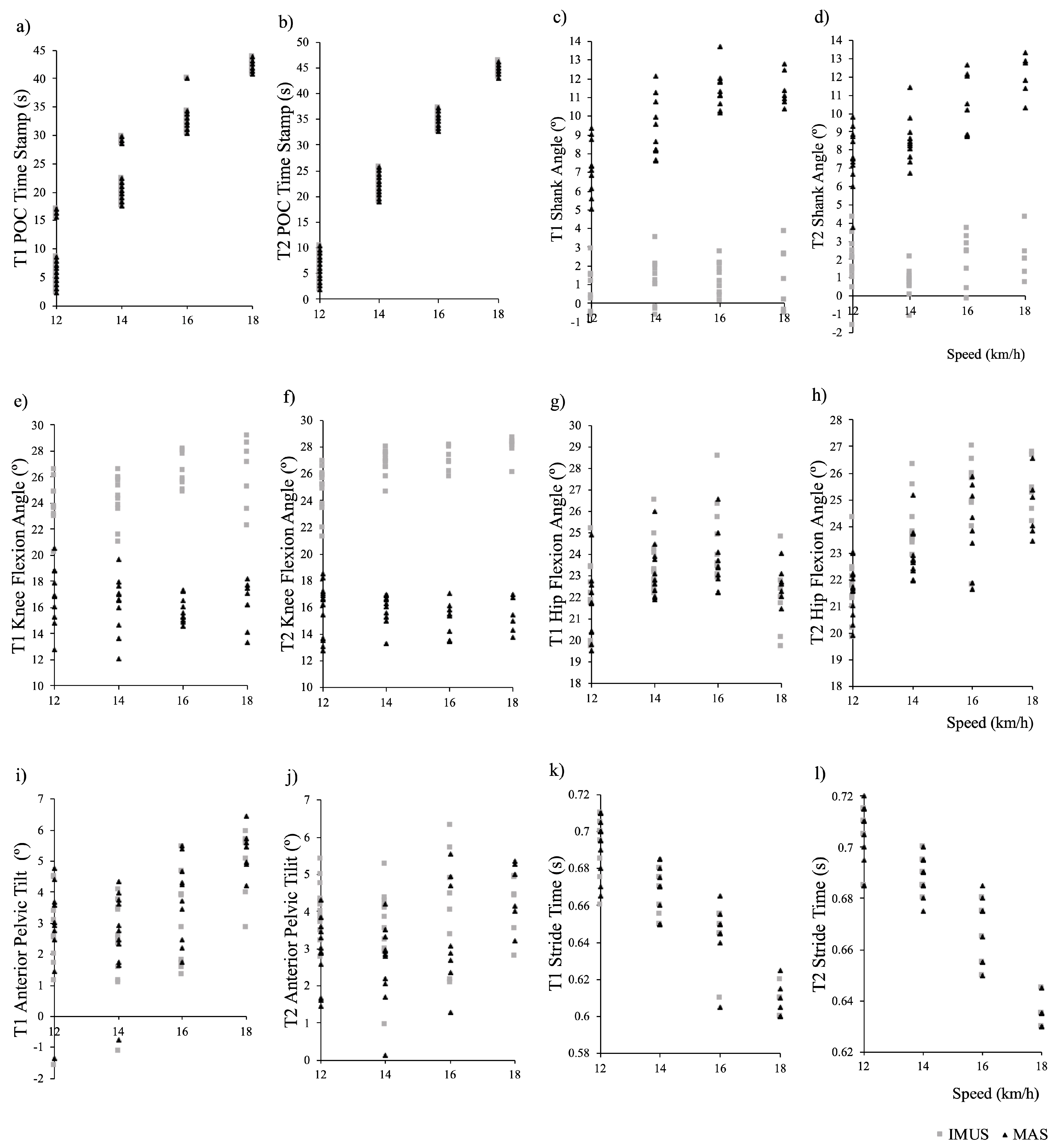
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
References
- Mendiguchia, J.; Castaño-Zambudio, A.; Jiménez-Reyes, P.; Morin, J.B.; Edouard, P.; Conceição, F.; Tawiah-Dodoo, J.; Colyer, S.L. Can we modify maximal speed running posture? Implications for performance and hamstring injury management. Int. J. Sports Physiol. Perform. 2021, 17, 374–383. [Google Scholar] [CrossRef] [PubMed]
- Barton, C.J.; Bonanno, D.R.; Carr, J.; Neal, B.S.; Malliaras, P.; Franklyn-Miller, A.; Menz, H.B. Running retraining to treat lower limb injuries: A mixed-methods study of current evidence synthesised with expert opinion. Br. J. Sports Med. 2016, 50, 513–526. [Google Scholar] [CrossRef] [PubMed]
- Ceyssens, L.; Vanelderen, R.; Barton, C.; Malliaras, P.; Dingenen, B. Biomechanical risk factors associated with running-related injuries: A systematic review. Sports Med. 2019, 49, 1095–1115. [Google Scholar] [CrossRef] [PubMed]
- Weyand, P.G.; Sternlight, D.B.; Bellizzi, M.J.; Wright, S. Faster top running speeds are achieved with greater ground forces not more rapid leg movements. J. Appl. Physiol. 2000, 89, 1991–1999. [Google Scholar] [CrossRef]
- Willy, R. Innovations and pitfalls in the use of wearable devices in the prevention and rehabilitation of running related injuries. Phys. Ther. Sport 2018, 29, 26–33. [Google Scholar] [CrossRef]
- Colyer, S.L.; Evans, M.; Cosker, D.P.; Salo, A.I.T. A review of the evolution of vision-based motion analysis and the integration of advanced computer vision methods towards developing a markerless system. Sports Med. 2018, 4, 24. [Google Scholar] [CrossRef]
- Camomilla, V.; Bergamini, E.; Fantozzi, S.; Vannozzi, G. Trends supporting the in-field use of wearable inertial sensors for sport performance evaluation: A systematic review. Sensors 2018, 18, 873. [Google Scholar] [CrossRef]
- Faisal, A.; Majumder, S.; Mondal, T.; Cowan, D.; Naseh, S.; Deen, M. Monitoring methods of human body joints: State-of-the-art and research challenges. Sensors 2019, 19, 2629. [Google Scholar] [CrossRef]
- Luinge, H.J.; Veltink, P.H. Measuring orientation of human body segments using miniature gyroscopes and accelerometers. Med. Biol. Eng. Comput. 2005, 43, 273–282. [Google Scholar] [CrossRef]
- Potter, M.; Ojeda, L.; Perkins, N.; Cain, S. Effect of IMU Design on IMU-derived stride metrics for running. Sensors 2019, 19, 2601. [Google Scholar] [CrossRef]
- Pacini Panebianco, G.; Bisi, M.C.; Stagni, R.; Fantozzi, S. Analysis of the performance of 17 algorithms from a systematic review: Influence of sensor position, analysed variable and computational approach in gait timing estimation from IMU measurements. Gait Posture 2018, 66, 76–82. [Google Scholar] [CrossRef]
- Kenneally-Dabrowski, C.J.; Serpell, B.G.; Spratford, W. Are accelerometers a valid tool for measuring overground sprinting symmetry? Int. J. Sports Sci. Coach. 2018, 13, 270–277. [Google Scholar] [CrossRef]
- Gurchiek, R.D.; McGinnis, R.S.; Needle, A.R.; McBride, J.M.; van Werkhoven, H. The use of a single inertial sensor to estimate 3-dimensional ground reaction force during accelerative running tasks. J. Biomech. 2017, 61, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Nagahara, R.; Kameda, M.; Neville, J.; Morin, J.-B. Inertial measurement unit-based hip flexion test as an indicator of sprint performance. J. Sports Sci. 2020, 38, 53–61. [Google Scholar] [CrossRef]
- Milner, C.E.; Ferber, R.; Pollard, C.D.; Hamill, J.; Davis, I. Biomechanical factors associated with tibial stress fracture in female runners. Med. Sci. Sports Exerc. 2006, 38, 323–328. [Google Scholar] [CrossRef]
- Struzik, A.; Konieczny, G.; Stawarz, M.; Grzesik, K.; Winiarski, S.; Rokita, A. Relationship between lower limb angular kinematic variables and the effectiveness of sprinting during the acceleration phase. Appl. Bionics Biomech. 2016, 2016, 7480709. [Google Scholar] [CrossRef] [PubMed]
- Toyoshima, R.; Sakurai, S. Kinematic characteristics of high step frequency sprinters and long step length sprinters at top speed phase. Int. J. Sport Health Sci. 2016, 14, 41–50. [Google Scholar] [CrossRef]
- Bergamini, E.; Guillon, P.; Camomilla, V.; Pillet, H.; Skalli, W.; Cappozzo, A. Trunk inclination estimate during the sprint start using an inertial measurement unit: A validation study. J. Appl. Biomech. 2013, 29, 622–627. [Google Scholar] [CrossRef]
- Raper, D.P.; Witchalls, J.; Philips, E.J.; Knight, E.; Drew, M.K.; Waddington, G. Use of a tibial accelerometer to measure ground reaction force in running: A reliability and validity comparison with force plates. J. Sci. Med. Sport 2018, 21, 84–88. [Google Scholar] [CrossRef]
- Mason, R.; Pearson, L.T.; Barry, G.; Young, F.; Lennon, O.; Godfrey, A.; Stuart, S. Wearables for running gait analysis: A systematic review. Sports Med. 2023, 53, 241–268. [Google Scholar] [CrossRef]
- García-Pinillos, F.; Latorre-Román, P.; Soto-Hermoso, V.; Párraga-Montilla, J.; Pantoja-Vallejo, A.; Ramírez-Campillo, R.; Roche-Seruendo, L. Agreement between the spatiotemporal gait parameters from two different wearable devices and high-speed video analysis. PLoS ONE 2019, 14, e0222872. [Google Scholar] [CrossRef] [PubMed]
- Brahms, C.M.; Zhao, Y.; Gerhard, D.; Barden, J.M. Stride length determination during overground running using a single foot-mounted inertial measurement unit. J. Biomech. 2018, 71, 302–305. [Google Scholar] [CrossRef] [PubMed]
- Dideriksen, O.M.; Soegaard, O.C.; Nielsen, O.R. Validity of self-reported running distance. J. Strength Cond. Res. 2016, 30, 1592–1596. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.; Rheinländer, C.; Nolte, K.F.; Wille, S.; Wehn, N.; Jaitner, T. IMU- based determination of stance duration during sprinting. Procedia Eng. 2016, 147, 747–752. [Google Scholar] [CrossRef]
- Agresta, C.E.; Peacock, J.; Housner, J.; Zernicke, R.F.; Zendler, J.D. Experience does not influence injury-related joint kinematics and kinetics in distance runners. Gait Posture 2018, 61, 13–18. [Google Scholar] [CrossRef]
- Brughelli, M.; Cronin, J.; Chaouachi, A. Effects of running velocity on running kinetics and kinematics. J. Strength Cond. Res. 2011, 25, 933–939. [Google Scholar] [CrossRef]
- Fukuchi, R.; Fukuchi, C.; Duarte, M. A public dataset of running biomechanics and the effects of running speed on lower extremity kinematics and kinetics. PeerJ PrePrints 2017, 5, e3298. [Google Scholar] [CrossRef]
- Lebel, K.; Boissy, P.; Hamel, M.; Duval, C. Inertial measures of motion for clinical biomechanics: Comparative assessment of accuracy under controlled conditions—Effect of velocity. PLoS ONE 2013, 8, e79945. [Google Scholar] [CrossRef]
- Provot, T.; Chiementin, X.; Oudin, E.; Bolaers, F.; Murer, S. Validation of a high sampling rate inertial measurement unit for acceleration during running. Sensors 2017, 17, 1958. [Google Scholar] [CrossRef]
- Falbriard, M.; Meyer, F.; Mariani, B.; Millet, G.P.; Aminian, K. Accurate estimation of running temporal parameters using foot-worn inertial sensors. Front. Physiol. 2018, 9, 610. [Google Scholar] [CrossRef]
- Buczek, F.L.; Rainbow, M.J.; Cooney, K.M.; Walker, M.R.; Sanders, J.O. Implications of using hierarchical and six degree-of-freedom models for normal gait analyses. Gait Posture 2010, 31, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Mo, S.; Chow, D.H.K. Accuracy of three methods in gait event detection during overground running. Gait Posture 2018, 59, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Donner, A.; Eliasziw, M. Sample size requirements for reliability studies. Stat. Med. 1987, 6, 441–448. [Google Scholar] [CrossRef] [PubMed]
- Shoukri, M.M.; Asyali, M.H.; Donner, A. Sample size requirements for the design of reliability study: Review and new results. Stat. Methods Med. Res. 2004, 13, 251–271. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Mukaka, M. Statistics corner: A guide to appropriate use of correlation in medical research. Malawi Med. J. 2012, 24, 69–71. [Google Scholar]
- Cuesta-Vargas, A.I.; Galán-Mercant, A.; Williams, J.M. The use of inertial sensors system for human motion analysis. Phys. Ther. Rev. 2010, 15, 462–473. [Google Scholar] [CrossRef]
- Sinclair, J.; Hobbs, S.J.; Protheroe, L.; Edmundson, C.J.; Greenhalgh, A. Determination of gait events using an externally mounted shank accelerometer. J. Appl. Biomech. 2013, 29, 118–122. [Google Scholar] [CrossRef]
- Zrenner, M.; Küderle, A.; Roth, N.; Jensen, U.; Dümler, B.; Eskofier, B.M. Does the position of foot-mounted IMU sensors influence the accuracy of spatio-temporal parameters in endurance running? Sensors 2020, 20, 5705. [Google Scholar] [CrossRef]
- Küderle, A.; Roth, N.; Zlatanovic, J.; Zrenner, M.; Eskofier, B.; Kluge, F. The placement of foot-mounted IMU sensors does affect the accuracy of spatial parameters during regular walking. PLoS ONE 2022, 17, e0269567. [Google Scholar] [CrossRef]
- Macadam, P.; Cronin, J.; Neville, J.; Diewald, S. Quantification of the validity and reliability of sprint performance metrics computed using inertial sensors: A systematic review. Gait Posture 2019, 73, 26–38. [Google Scholar] [CrossRef]
- Zeng, Z.; Liu, Y.; Hu, X.; Tang, M.; Wang, L. Validity and reliability of inertial measurement units on lower extremity kinematics during running: A systematic review and meta-analysis. Sports Med. 2022, 8, 86. [Google Scholar] [CrossRef]
- Nüesch, C.; Roos, E.; Pagenstert, G.; Mündermann, A. Measuring joint kinematics of treadmill walking and running: Comparison between an inertial sensor based system and a camera-based system. J. Biomech. 2017, 57, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.-C.; Price, K.; Carmichael, D.S.; Maniar, N.; Hickey, J.T.; Timmins, R.G.; Heiderscheit, B.C.; Blemker, S.S.; Opar, D.A. Validity of inertial measurement units to measure lower-limb kinematics and pelvic orientation at submaximal and maximal effort running speeds. Sensors 2023, 23, 9599. [Google Scholar] [CrossRef]
- Ruiz-Malagón, E.J.; García-Pinillos, F.; Molina-Molina, A.; Soto-Hermoso, V.M.; Ruiz-Alias, S.A. RunScribe Sacral Gait Lab™ validation for measuring pelvic kinematics during human locomotion at different speeds. Sensors 2023, 23, 2604. [Google Scholar] [CrossRef]
- Lai, Y.-J.; Chou, W.; Chu, I.H.; Wang, Y.-L.; Lin, Y.-J.; Tu, S.J.; Guo, L.-Y. Will the foot strike pattern change at different running speeds with or without wearing shoes? Int. J. Environ. Res. Public Health 2020, 17, 6044. [Google Scholar] [CrossRef] [PubMed]
- Dicharry, J.M.P.T. Kinematics and kinetics of gait: From lab to clinic. Clin. Sports Med. 2010, 29, 347–364. [Google Scholar] [CrossRef] [PubMed]
- Forrester, S.E.; Townend, J. The effect of running velocity on footstrike angle—A curve-clustering approach. Gait Posture 2015, 41, 26–32. [Google Scholar] [CrossRef]
- Lieberman, D.E.; Venkadesan, M.; Werbel, W.A.; Daoud, A.I.; Mang’Eni, R.O.; D’Andrea, S.; Davis, I.S.; Pitsiladis, Y. Foot strike patterns and collision forces in habitually barefoot versus shod runners. Nature 2010, 463, 531–535. [Google Scholar] [CrossRef]
- McKenna, M.; Riches, P.E. A comparison of sprinting kinematics on two types of treadmill and over-ground. Scand. J. Med. Sci. Sports 2007, 17, 649–655. [Google Scholar] [CrossRef]
- Camomilla, V.; Dumas, R.; Cappozzo, A. Human movement analysis: The soft tissue artefact issue. J. Biomech. 2017, 62, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Bélaise, C.; Blache, Y.; Thouzé, A.; Monnet, T.; Begon, M. Effect of wobbling mass modeling on joint dynamics during human movements with impacts. Multibody Syst. Dyn. 2016, 38, 345–366. [Google Scholar] [CrossRef]
- Bergmann, J.H.M.; Mayagoitia, R.E.; Smith, I.C.H. A portable system for collecting anatomical joint angles during stair ascent: A comparison with an optical tracking device. Dyn. Med. 2009, 8, 3. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Z.; Liu, Y.; Li, P.; Wang, L. Validity and reliability of inertial measurement units measurements for running kinematics in different foot strike pattern runners. Front. Bioeng. Biotechnol. 2022, 10, 1005496. [Google Scholar] [CrossRef] [PubMed]



| Trial 1 | Trial 2 | |||||||
|---|---|---|---|---|---|---|---|---|
| ICC (95% CI), p Value | Pearson’s r, p Value | IMU System RMSE (% MAS Mean) | Paired t-Test MAS (SD), IMU System (SD), p Value | ICC (95% CI), p Value | Pearson’s r, p Value | IMU System RMSE (% MAS Mean) | Paired t-Test MAS (SD), IMU System (SD), p Value | |
| POC Detection | ||||||||
| 12 km/h | 1.00 (1.00,1.00), <0.001 * | 1.00, <0.001 * | 0.005 s ^ | 5.44 (2.12), 5.44 (2.13), 0.003 * | 1.00 (1.00,1.00), <0.001 * | 1.00, <0.001 * | 0.0052 s ^ | 6.15 (2.75), 6.15 (2.75), <0.001 * |
| 14 km/h | 1.00 (1.00,1.00), <0.001 * | 1.00, <0.001 * | 0.0043 s ^ | 18.98 (2.23), 18.98 (2.24), <0.001 * | 1.00 (1.00,1.00), <0.001 * | 1.00, <0.001 * | 0.0052 s ^ | 22.33 (2.29), 22.33 (2.29), <0.001 * |
| 16 km/h | 1.00 (1.00,1.00), <0.001 * | 1.00, <0.001 * | 0.0155 s ^ | 31.40 (1.97), 31.40 (1.97), <0.001 * | 1.00 (0.99,1.00), <0.001 * | 1.00, <0.001 * | 0.0047 s ^ | 34.94 (1.63), 34.94 (1.63), <0.001 * |
| 18 km/h | 1.00 (1.00,1.00), <0.001 * | 1.00, <0.001 * | 0.0038 s ^ | 41.94 (1.32), 41.94 (1.32), 0.030 * | 1.00 (0.99,1.00), <0.001 * | 1.00, <0.001 * | 0.0076 s ^ | 44.70 (1.19), 44.70 (1.19), 0.010 * |
| POC Shank Angle | ||||||||
| 12 km/h | 0.04 (−0.01,0.26), 0.024 * | 0.61, 0.060 | 6.84° (94.34%) | 7.25 (1.44), 0.51 (1.28), <0.001* | 0.11 (−0.01,0.44), <0.001 * | 0.89, <0.001 * | 5.81° (76.56%) | 7.59 (1.57), 1.81 (1.46), <0.001 * |
| 14 km/h | 0.03 (−0.01,0.18), 0.037 * | 0.55, 0.08 | 8.20° (88.28%) | 9.29 (1.55), 1.19 (1.21), <0.001* | 0.02 (−0.01,0.14), 0.012 * | 0.71, 0.015 * | 7.83° (91.96%) | 8.51 (1.27), 0.73 (0.81), <0.001 * |
| 16 km/h | 0.01 (−0.00,0.06), 0.680 | 0.48, 0.155 | 10.09° (88.44%) | 11.41 (1.03), 1.36 (0.87), <0.001* | 0.05 (−0.01,0.30), 0.004 * | 0.82, 0.012 * | 8.50° (80.97%) | 10.50 (1.64), 2.05 (1.38), <0.001 * |
| 18 km/h | 0.01 (−0.01,0.12), 0.202 | 0.42, 0.35 | 10.13° (88.71%) | 11.42 (0.89), 1.39 (1.70), <0.001* | −0.00 (−0.01,0.07), 0.580 | −0.09, 0.858 | 10.08° (83.36%) | 12.09 (1.12), 2.12 (1.22), <0.001 * |
| POC Knee Angle | ||||||||
| 12 km/h | 0.08 (−0.03,0.40), 0.030 * | 0.60, 0.067 | 7.30° (43.17%) | 16.90 (2.27), 23.98 (1.78), <0.001 * | 0.06 (−0.01,0.31), <0.001 * | 0.81, <0.001 * | 9.03° (56.98%) | 15.85 (1.96), 24.81 (1.73), <0.001 * |
| 14 km/h | 0.08 (−0.01,0.39), <0.001 * | 0.81, 0.003 * | 8.20° (50.37%) | 16.28 (2.10), 24.39 (1.80), <0.001 * | 0.00 (−0.00,0.04), 0.204 | 0.27, 0.429 | 10.89° (68.21%) | 15.97 (1.10), 26.80 (0.94), <0.001 * |
| 16 km/h | 0.01 (−0.01,0.06), 0.158 | 0.35, 0.324 | 10.83° (68.59%) | 15.79 (0.99), 26.55 (1.32), <0.001 * | 0.00 (−0.00,0.04), 0.338 | 0.17, 0.68 | 12.11° (79.94%) | 15.15 (1.29), 27.18 (0.89), <0.001 * |
| 18 km/h | 0.07 (−0.01,0.42), 0.014 * | 0.81, 0.029 * | 10.07° (61.74%) | 16.31 (1.88), 26.26 (2.65), <0.001 * | −0.01 (−0.01,0.04), 0.915 | −0.61, 0.195 | 12.66° (82.23%) | 15.40 (1.30), 27.92 (0.94), <0.001 * |
| POC Hip Angle | ||||||||
| 12 km/h | 0.87 (0.36,0.97), <0.001 * | 0.92, <0.001 * | 0.86° (3.97%) | 21.61 (1.63), 22.19 (1.62), 0.021 * | 0.88 (0.64,0.96), <0.001 * | 0.88, <0.001 * | 0.52° (2.38%) | 21.61 (0.94), 21.69 (1.12), 0.579 |
| 14 km/h | 0.86 (0.49,0.96), <0.001 * | 0.90, <0.001 * | 0.68° (2.93%) | 23.17 (1.26), 23.58 (1.29), 0.041 * | 0.53 (−0.09,0.87), <0.001 * | 0.84, <0.001 * | 1.20° (5.22%) | 22.95 (0.94), 24.02 (1.02), <0.001 * |
| 16 km/h | 0.69 (0.04,0.92), 0.002 * | 0.84, 0.003 * | 1.34° (5.66%) | 23.66 (1.32), 24.59 (1.81), 0.017 * | 0.70 (−0.09,0.94), <0.001 * | 0.88, 0.004 * | 1.39° (5.82%) | 23.95 (1.60), 25.12 (1.65), 0.005 * |
| 18 km/h | 0.54 (−0.13,0.90), 0.065 | 0.74, 0.055 | 1.31° (5.80%) | 22.61 (0.82), 21.93 (1.69), 0.186 | 0.65 (−0.09,0.94), 0.020 * | 0.78, 0.066 | 1.02° (4.14%) | 24.72 (1.17), 25.49 (1.06), 0.052 |
| POC Pelvis Angle | ||||||||
| 12 km/h | 0.96 (0.43,0.99), <0.001 * | 0.99, <0.001 * | 0.47° (17.11%) | 2.77 (1.74), 2.38 (1.77), 0.002 * | 0.42 (−0.05,0.81), <0.001 * | 0.88, <0.001 * | 1.24° (43.04%) | 2.89 (0.88), 4.06 (0.72), <0.001 * |
| 14 km/h | 0.95 (0.48,0.99), <0.001 * | 0.98, <0.001 * | 0.46° (17.55%) | 2.61 (1.43), 2.26 (1.52), 0.003 * | 0.68 (−0.04,0.93), <0.001 * | 0.96, <0.001 * | 1.04° (39.92%) | 2.61 (1.08), 3.60 (1.11), <0.001 * |
| 16 km/h | 0.82 (0.13,0.96), <0.001 * | 0.91, 0.011 * | 0.86° (22.84%) | 3.77 (1.30), 3.12 (1.46), 0.008 * | 0.84 (0.07,0.97), <0.001 * | 0.92, 0.001 * | 0.89° (25.99%) | 3.44 (1.46), 4.14 (1.54), 0.012 * |
| 18 km/h | 0.72 (0.11,0.94), 0.018 * | 0.82, 0.023 * | 0.73° (13.62%) | 5.33 (0.71), 4.97 (1.14), 0.216 | 0.88 (0.17,0.98), 0.001 * | 0.93, 0.006 | 0.43° (9.58%) | 4.51 (0.85), 4.18 (0.85), 0.048 * |
| Stride Time | ||||||||
| 12 km/h | 0.78 (0.32,0.94), 0.003 * | 0.76, 0.01 * | 0.0047 s (0.68%) | 0.70 (0.01), 0.07 (0.01), 0.758 | 0.94 (0.80,0.98), <0.001 * | 0.94, <0.001 * | 0.0039 s (0.56%) | 0.71 (0.01), 0.71 (0.01), 1.0 |
| 14 km/h | 0.88 (0.60,0.96), <0.001 * | 0.87, <0.001 * | 0.0040 s (0.59%) | 0.67 (0.01), 0.67 (0.01), 0.724 | 0.87 (0.59,0.96), <0.001 * | 0.88, <0.001 * | 0.0034 s (0.49%) | 0.69 (0.01), 0.69 (0.01), 0.676 |
| 16 km/h | 0.72 (0.19,0.92), 0.008 * | 0.76, 0.011 * | 0.0042 s (0.64%) | 0.65 (0.01), 0.65 (0.00), 0.726 | 0.99 (0.96,0.99), <0.001 * | 0.99, <0.001 * | 0.0018 s (0.26%) | 0.67 (0.01), 0.67 (0.01), 0.351 |
| 18 km/h | 0.89 (0.46, 0.98), 0.002 * | 0.90, 0.006 * | 0.0038 s (0.62%) | 0.61 (0.01), 0.61 (0.01), 1.00 | 0.21 (−0.88,0.85), 0.346 | 0.19, 0.725 | 0.0061 s (0.96%) | 0.64 (0.01), 0.64 (0.00), 0.771 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wolski, L.; Halaki, M.; Hiller, C.E.; Pappas, E.; Fong Yan, A. Validity of an Inertial Measurement Unit System to Measure Lower Limb Kinematics at Point of Contact during Incremental High-Speed Running. Sensors 2024, 24, 5718. https://doi.org/10.3390/s24175718
Wolski L, Halaki M, Hiller CE, Pappas E, Fong Yan A. Validity of an Inertial Measurement Unit System to Measure Lower Limb Kinematics at Point of Contact during Incremental High-Speed Running. Sensors. 2024; 24(17):5718. https://doi.org/10.3390/s24175718
Chicago/Turabian StyleWolski, Lisa, Mark Halaki, Claire E. Hiller, Evangelos Pappas, and Alycia Fong Yan. 2024. "Validity of an Inertial Measurement Unit System to Measure Lower Limb Kinematics at Point of Contact during Incremental High-Speed Running" Sensors 24, no. 17: 5718. https://doi.org/10.3390/s24175718
APA StyleWolski, L., Halaki, M., Hiller, C. E., Pappas, E., & Fong Yan, A. (2024). Validity of an Inertial Measurement Unit System to Measure Lower Limb Kinematics at Point of Contact during Incremental High-Speed Running. Sensors, 24(17), 5718. https://doi.org/10.3390/s24175718






