Efficacy of Wearable Single-Lead ECG Monitoring during Exercise Stress Testing: A Comparative Study
Abstract
:1. Introduction
2. Methods
2.1. Wearable Single-Lead ECG Device
2.2. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Comparison of ECG Monitoring Methods
3.3. HR Agreement across Exercise Test Stages
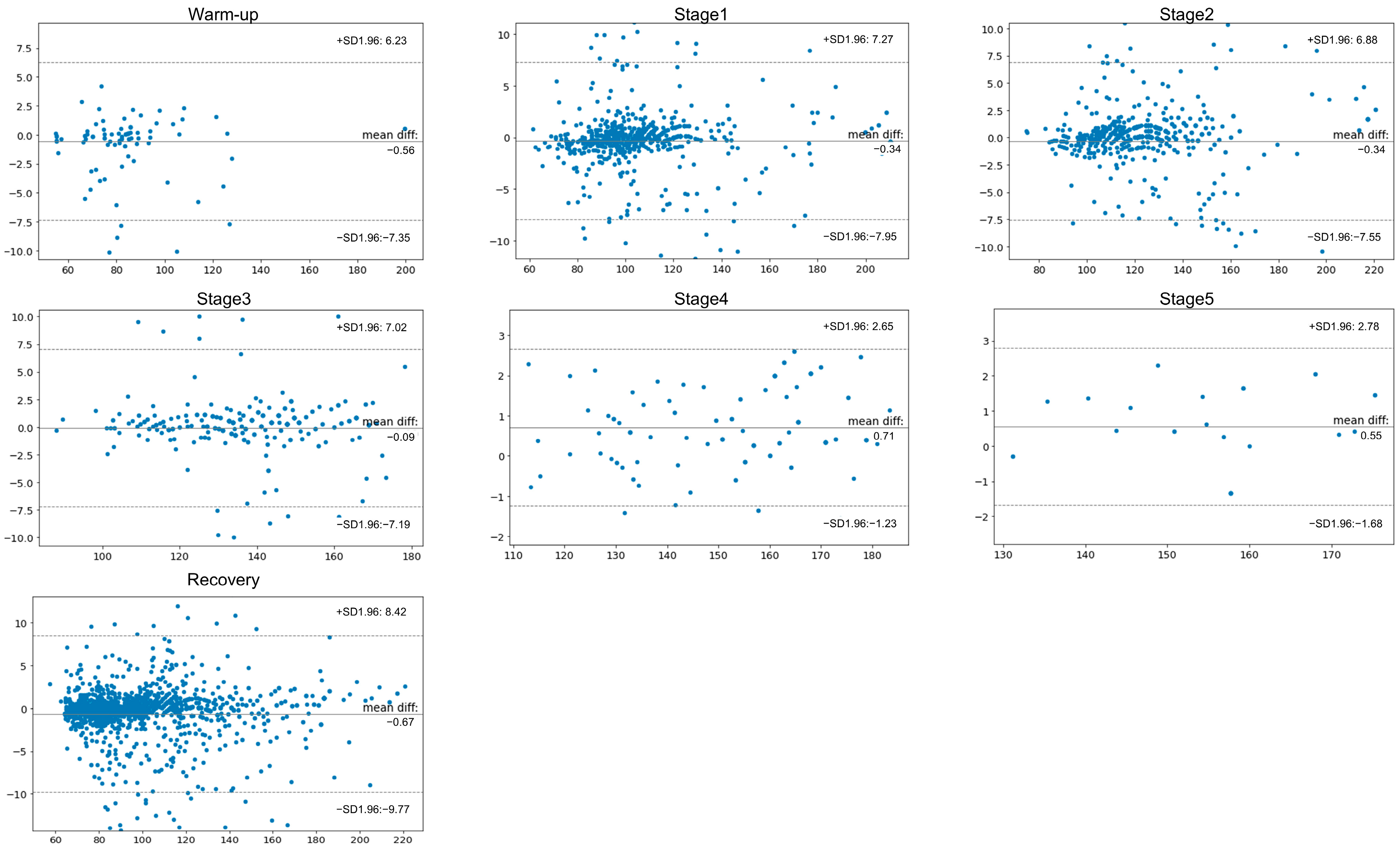
4. Discussion
5. Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tsao, C.W.; Aday, A.W.; Almarzooq, Z.I.; Alonso, A.; Beaton, A.Z.; Bittencourt, M.S.; Boehme, A.K.; Buxton, A.E.; Carson, A.P.; Commodore-Mensah, Y.; et al. Heart Disease and Stroke Statistics-2022 Update: A Report From the American Heart Association. Circulation 2022, 145, e153–e639. [Google Scholar] [PubMed]
- Beatty, A.L.; Beckie, T.M.; Dodson, J.; Goldstein, C.M.; Hughes, J.W.; Kraus, W.E.; Martin, S.S.; Olson, T.P.; Pack, Q.R.; Stolp, H.; et al. A New Era in Cardiac Rehabilitation Delivery: Research Gaps, Questions, Strategies, and Priorities. Circulation 2023, 147, 254–266. [Google Scholar] [CrossRef] [PubMed]
- Dibben, G.O.; Faulkner, J.; Oldridge, N.; Rees, K.; Thompson, D.R.; Zwisler, A.D.; Taylor, R.S. Exercise-based cardiac rehabilitation for coronary heart disease: A meta-analysis. Eur. Heart J. 2023, 44, 452–469. [Google Scholar] [CrossRef] [PubMed]
- Hansen, D.; Abreu, A.; Ambrosetti, M.; Cornelissen, V.; Gevaert, A.; Kemps, H.; Laukkanen, J.A.; Pedretti, R.; Simonenko, M.; Wilhelm, M.; et al. Exercise intensity assessment and prescription in cardiovascular rehabilitation and beyond: Why and how: A position statement from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology. Eur. J. Prev. Cardiol. 2022, 29, 230–245. [Google Scholar] [CrossRef]
- Stracina, T.; Ronzhina, M.; Redina, R.; Novakova, M. Golden standard or obsolete method? Review of ECG applications in clinical and experimental context. Front. Physiol. 2022, 13, 867033. [Google Scholar] [CrossRef]
- Abreu, A.; Frederix, I.; Dendale, P.; Janssen, A.; Doherty, P.; Piepoli, M.F.; Voeller, H.; Davos, C.H.; Secondary Prevention and Rehabilitation Section of EAPC Reviewers: Ambrosetti Marco. Standardization and quality improvement of secondary prevention through cardiovascular rehabilitation programmes in Europe: The avenue towards EAPC accreditation programme: A position statement of the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology (EAPC). Eur. J. Prev. Cardiol. 2020, 28, 496–509. [Google Scholar]
- Wong, K.C.; Klimis, H.; Lowres, N.; von Huben, A.; Marschner, S.; Chow, C.K. Diagnostic accuracy of handheld electrocardiogram devices in detecting atrial fibrillation in adults in community versus hospital settings: A systematic review and meta-analysis. Heart 2020, 106, 1211–1217. [Google Scholar] [CrossRef]
- Reddy, R.K.; Pooni, R.; Zaharieva, D.P.; Senf, B.; El Youssef, J.; Dassau, E.; Doyle, F.J., III; Clements, M.A.; Rickels, M.R.; Patton, S.R.; et al. Accuracy of Wrist-Worn Activity Monitors during Common Daily Physical Activities and Types of Structured Exercise: Evaluation Study. JMIR mHealth uHealth 2018, 6, e10338. [Google Scholar] [CrossRef]
- Sana, F.; Isselbacher, E.M.; Singh, J.P.; Heist, E.K.; Pathik, B.; Armoundas, A.A. Wearable Devices for Ambulatory Cardiac Monitoring: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2020, 75, 1582–1592. [Google Scholar] [CrossRef]
- Kwon, S.; Lee, S.R.; Choi, E.K.; Ahn, H.J.; Song, H.S.; Lee, Y.S.; Oh, S.; Lip, G.Y. Comparison Between the 24-h Holter Test and 72-h Single-Lead Electrocardiogram Monitoring with an Adhesive Patch-Type Device for Atrial Fibrillation Detection: Prospective Cohort Study. J. Med. Internet Res. 2022, 24, e37970. [Google Scholar] [CrossRef]
- Gibbons, R.J.; Balady, G.J.; Bricker, J.T.; Chaitman, B.R.; Fletcher, G.F.; Froelicher, V.F.; Mark, D.B.; McCallister, B.D.; Mooss, A.N.; O’Reilly, M.G.; et al. ACC/AHA 2002 guideline update for exercise testing: Summary article. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines). J. Am. Coll. Cardiol. 2002, 40, 1531–1540. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; Pan, Y.; Wu, F.; Huan, R. Optimized Electrode Locations for Wearable Single-Lead ECG Monitoring Devices: A Case Study Using WFEES Modules Based on the LANS Method. Sensors 2019, 19, 4458. [Google Scholar] [CrossRef]
- Lehnert, B. BlandAltmanLeh: Plots (Slightly Extended) Bland-Altman Plots. 2015. Available online: https://cran.r-project.org/web/packages/BlandAltmanLeh/BlandAltmanLeh.pdf (accessed on 1 March 2024).
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef]
- Taylor, R.S.; Dalal, H.M.; McDonagh, S.T.J. The role of cardiac rehabilitation in improving cardiovascular outcomes. Nat. Rev. Cardiol. 2022, 19, 180–194. [Google Scholar] [CrossRef] [PubMed]
- Ades, P.A.; Khadanga, S.; Savage, P.D.; Gaalema, D.E. Enhancing participation in cardiac rehabilitation: Focus on underserved populations. Prog. Cardiovasc. Dis. 2022, 70, 102–110. [Google Scholar] [CrossRef] [PubMed]
- Snoek, J.A.; Prescott, E.I.; van der Velde, A.E.; Eijsvogels, T.M.H.; Mikkelsen, N.; Prins, L.F.; Bruins, W.; Meindersma, E.; González-Juanatey, J.R.; Peña-Gil, C.; et al. Effectiveness of Home-Based Mobile Guided Cardiac Rehabilitation as Alternative Strategy for Nonparticipation in Clinic-Based Cardiac Rehabilitation Among Elderly Patients in Europe: A Randomized Clinical Trial. JAMA Cardiol. 2021, 6, 463–468. [Google Scholar] [CrossRef]
- Thomas, R.J.; Beatty, A.L.; Beckie, T.M.; Brewer, L.C.; Brown, T.M.; Forman, D.E.; Franklin, B.A.; Keteyian, S.J.; Kitzman, D.W.; Regensteiner, J.G.; et al. Home-Based Cardiac Rehabilitation: A Scientific Statement From the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. Circulation 2019, 140, e69–e89. [Google Scholar] [CrossRef]
- Ramachandran, H.J.; Jiang, Y.; Tam, W.W.S.; Yeo, T.J.; Wang, W. Effectiveness of home-based cardiac telerehabilitation as an alternative to Phase 2 cardiac rehabilitation of coronary heart disease: A systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2022, 29, 1017–1043. [Google Scholar] [CrossRef]
- Stefanakis, M.; Batalik, L.; Antoniou, V.; Pepera, G. Safety of home-based cardiac rehabilitation: A systematic review. Heart Lung 2022, 55, 117–126. [Google Scholar] [CrossRef]
- Bayoumy, K.; Gaber, M.; Elshafeey, A.; Mhaimeed, O.; Dineen, E.H.; Marvel, F.A.; Martin, S.S.; Muse, E.D.; Turakhia, M.P.; Tarakji, K.G.; et al. Smart wearable devices in cardiovascular care: Where we are and how to move forward. Nat. Rev. Cardiol. 2021, 18, 581–599. [Google Scholar] [CrossRef]
- Li, X.; Dunn, J.; Salins, D.; Zhou, G.; Zhou, W.; Schüssler-Fiorenza Rose, S.M.; Perelman, D.; Colbert, E.; Runge, R.; Rego, S.; et al. Digital health: Tracking physiomes and activity using wearable biosensors reveals useful health-related information. PLoS Biol. 2017, 15, e2001402. [Google Scholar] [CrossRef] [PubMed]
- Dafny, H.A.; Champion, S.; Gebremichael, L.G.; Pearson, V.; Hendriks, J.M.; Clark, R.A.; Pinero de Plaza, M.A.; Gulyani, A.; Hines, S.; Beleigoli, A. Cardiac rehabilitation, physical activity, and the effectiveness of activity monitoring devices on cardiovascular patients: An umbrella review of systematic reviews. Eur. Heart J. Qual. Care Clin. Outcomes 2023, 9, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Etiwy, M.; Akhrass, Z.; Gillinov, L.; Alashi, A.; Wang, R.; Blackburn, G.; Gillinov, S.M.; Phelan, D.; Gillinov, A.M.; Houghtaling, P.L.; et al. Accuracy of wearable heart rate monitors in cardiac rehabilitation. Cardiovasc. Diagn. Ther. 2019, 9, 262. [Google Scholar] [CrossRef] [PubMed]
- Shumate, T.; Link, M.; Furness, J.; Kemp-Smith, K.; Simas, V.; Climstein, M. Validity of the Polar Vantage M watch when measuring heart rate at different exercise intensities. PeerJ 2021, 9, e10893. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Yan, B.P.-Y.; Dai, W.-X.; Ding, X.-R.; Zhang, Y.-T.; Zhao, N. Multi-wavelength photoplethysmography method for skin arterial pulse extraction. Biomed. Opt. Express 2016, 7, 4313–4326. [Google Scholar] [CrossRef]
- Martín-Escudero, P.; Cabanas, A.M.; Dotor-Castilla, M.L.; Galindo-Canales, M.; Miguel-Tobal, F.; Fernández-Pérez, C.; Fuentes-Ferrer, M.; Giannetti, R. Are activity wrist-worn devices accurate for determining heart rate during intense exercise? Bioengineering 2023, 10, 254. [Google Scholar] [CrossRef]



| Value | |
|---|---|
| Demographics | |
| Age, year | 57.8 ± 11.2 |
| Male, % | 32 (64.0) |
| Height, cm | 164.3 ± 10.0 |
| Weight, kg | 66.2 ± 15.6 |
| Body mass index, kg/m2 | 24.3 ± 4.2 |
| Comorbidity | |
| Hypertension | 22 (44.0) |
| Diabetes mellitus | 15 (30.0) |
| Coronary artery disease | 27 (54.0) |
| Atrial fibrillation | 11 (22.0) |
| Heart failure | 13 (26.0) |
| Peripheral artery disease | 1 (2.0) |
| Chronic kidney disease | 3 (6.0) |
| Chronic obstructive pulmonary disease | 1 (2.0) |
| Cerebrovascular accident | 0 (0.0) |
| Indication for exercise test | |
| Suspected coronary artery disease | 9 (18.0) |
| Known patients with coronary artery disease | 25 (50.0) |
| Suspected arrhythmia | 4 (8.0) |
| Evaluation of exercise capacity | 6 (12.0) |
| Evaluation of heart failure | 6 (12.0) |
| Medications | |
| Beta blocker | 18 (36.0) |
| Calcium channel blocker | 14 (28.0) |
| Antiarrhythmic drug | 7 (14.0) |
| Exercise test results | |
| Maximal METs | 9.1 ± 3.3 |
| Exercise duration, mins | 6.5 ± 3.1 |
| Maximal heart rate, bpm | 149.5 ± 27.2 |
| 12-Lead ECG | Wearable Single-Lead ECG | p-Value for Reliability (Correlation) | Corrcoef | p-Value for Difference | |
|---|---|---|---|---|---|
| Total QRS | 1405.9 ± 540.7 | 1419.3 ± 542.5 | <0.001 | >0.9 | 0.19 |
| VEB | 15.2 ± 66.1 | 15.4 ± 66.1 | <0.001 | 1.0 | 0.0078 |
| VEB burden, % | 0.01 ± 0.06 | 0.01 ± 0.06 | <0.001 | 1.0 | >0.9 |
| SVEB | 3.6 ± 8.6 | 3.6 ± 8.6 | <0.001 | 1.0 | >0.9 |
| SVEB burden, % | 0.004 ± 0.009 | 0.004 ± 0.009 | <0.001 | 1.0 | >0.9 |
| Max RR, ms | 931 ± 250 | 931 ± 245 | <0.001 | >0.9 | >0.9 |
| Average RR, ms | 570 ± 93 | 569 ± 92 | <0.001 | >0.9 | 0.34 |
| Min RR, ms | 357 ± 73 | 357 ± 73 | <0.001 | 1.0 | >0.9 |
| Noise ratio, % | 1.3 ± 3.7 | 0.6 ± 2.1 | <0.001 | 0.41 | 0.13 |
| Stage | Conventional 12-Lead ECG | Wearable Single-Lead ECG | N | ICC | p-Value for Difference | |||
|---|---|---|---|---|---|---|---|---|
| Mean in HR (bpm) | SD | Mean in HR (bpm) | SD | N | r | p-Value | p-Value | |
| Warm-up | 85 | 23.7 | 86 | 23.5 | 90 | 0.990 | <0.001 | 0.45 |
| Stage1 | 107 | 24.0 | 107 | 24.3 | 826 | 0.987 | <0.001 | 0.29 |
| Stage2 | 124 | 23.0 | 124 | 23.2 | 645 | 0.987 | <0.001 | 0.31 |
| Stage3 | 137 | 17.1 | 137 | 17.2 | 335 | 0.976 | <0.001 | 0.25 |
| Stage4 | 153 | 17.4 | 153 | 17.2 | 123 | 0.998 | <0.001 | 0.45 |
| Stage5 | 156 | 12.1 | 155 | 11.9 | 26 | 0.995 | <0.001 | 0.45 |
| Recovery | 101 | 27.9 | 101 | 28.4 | 1695 | 0.986 | <0.001 | 0.37 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, H.-I.; Lee, S.J.; Choi, J.D.; Kim, G.; Lee, Y.-S.; Lee, J.-Y. Efficacy of Wearable Single-Lead ECG Monitoring during Exercise Stress Testing: A Comparative Study. Sensors 2024, 24, 6394. https://doi.org/10.3390/s24196394
Choi H-I, Lee SJ, Choi JD, Kim G, Lee Y-S, Lee J-Y. Efficacy of Wearable Single-Lead ECG Monitoring during Exercise Stress Testing: A Comparative Study. Sensors. 2024; 24(19):6394. https://doi.org/10.3390/s24196394
Chicago/Turabian StyleChoi, Hyo-In, Seung Jae Lee, Jong Doo Choi, GyungChul Kim, Young-Shin Lee, and Jong-Young Lee. 2024. "Efficacy of Wearable Single-Lead ECG Monitoring during Exercise Stress Testing: A Comparative Study" Sensors 24, no. 19: 6394. https://doi.org/10.3390/s24196394





