Preliminary Characterization of an Active CMOS Pad Detector for Tracking and Dosimetry in HDR Brachytherapy
Abstract
:1. Introduction
2. Materials and Methods
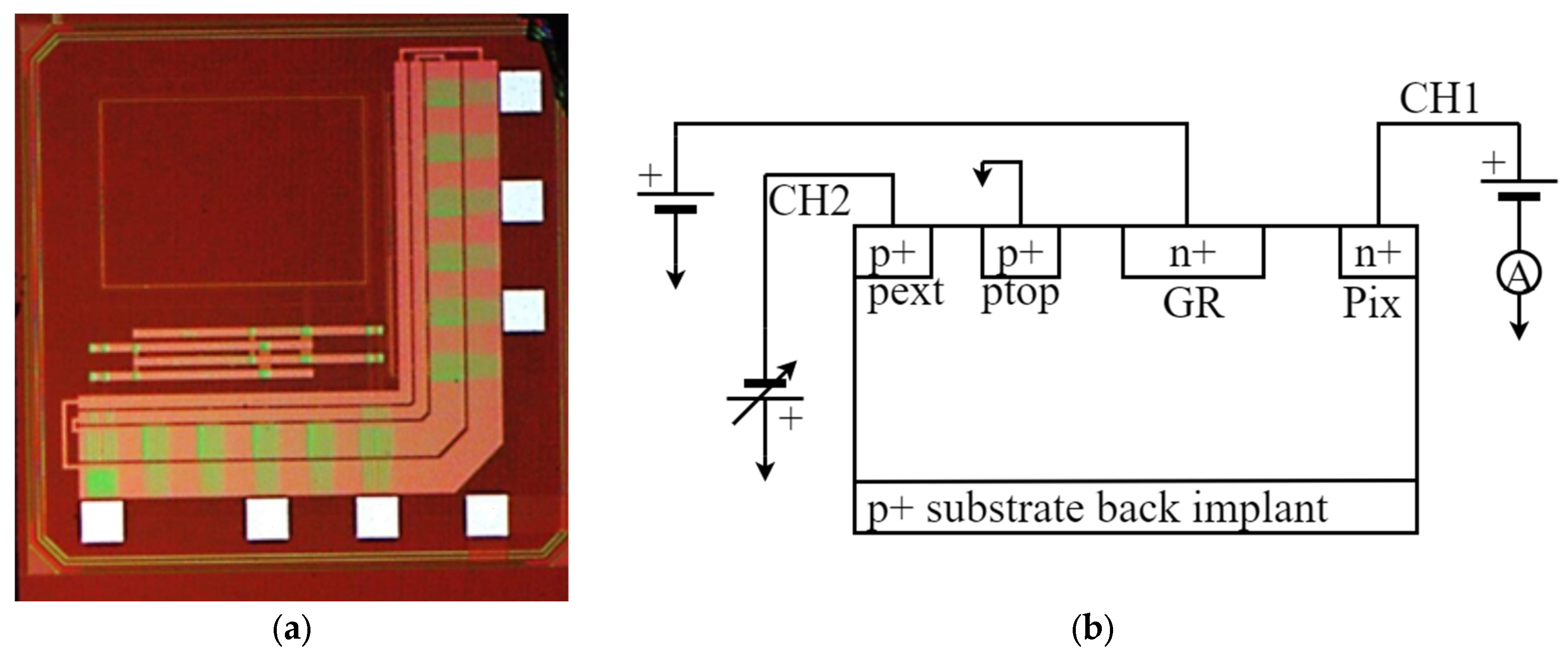
2.1. Detector Architecture
2.2. Active Pad Architecture and Probe Assembling
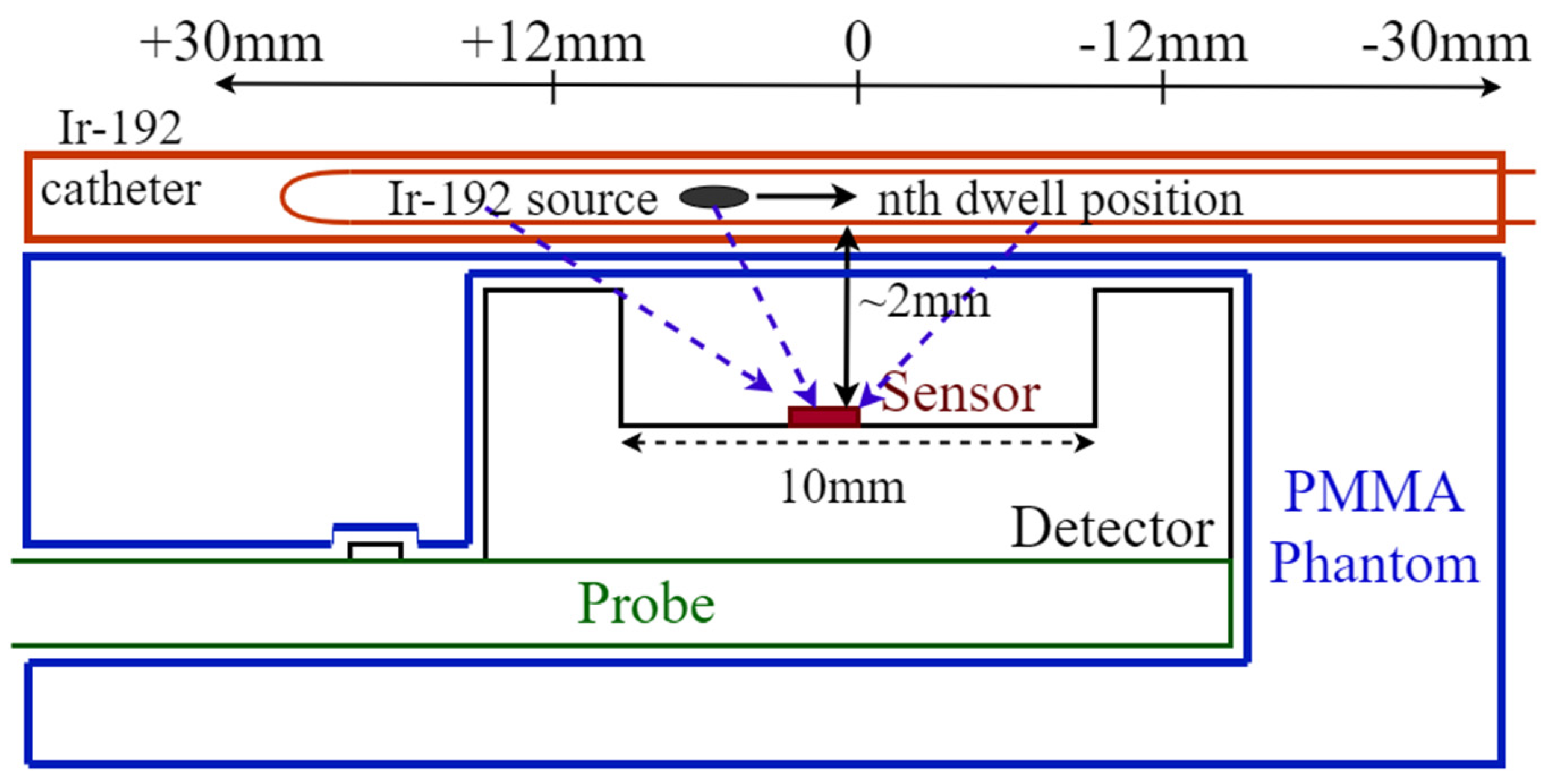
2.3. Phantom
2.4. Electrical Characterization
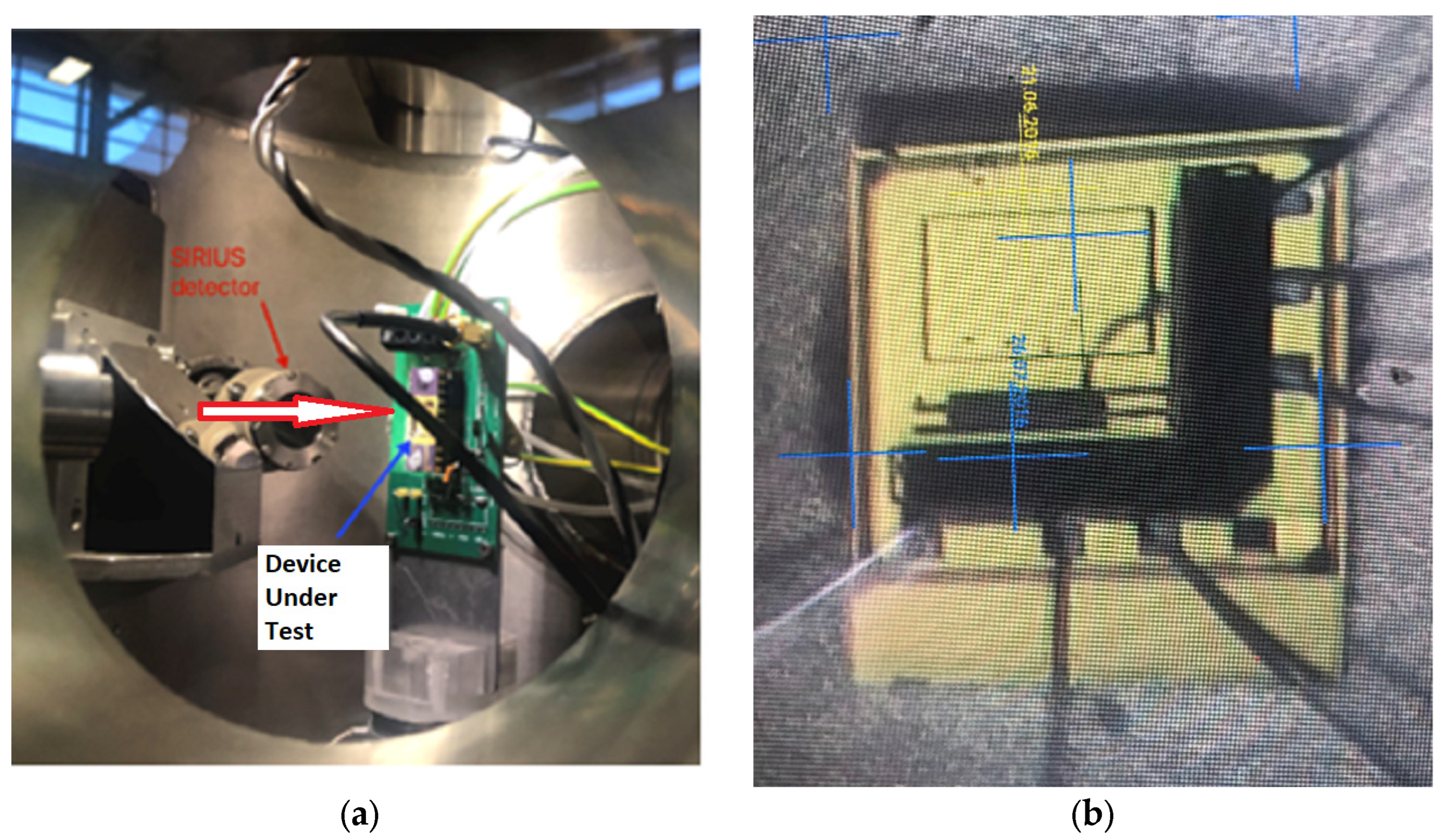
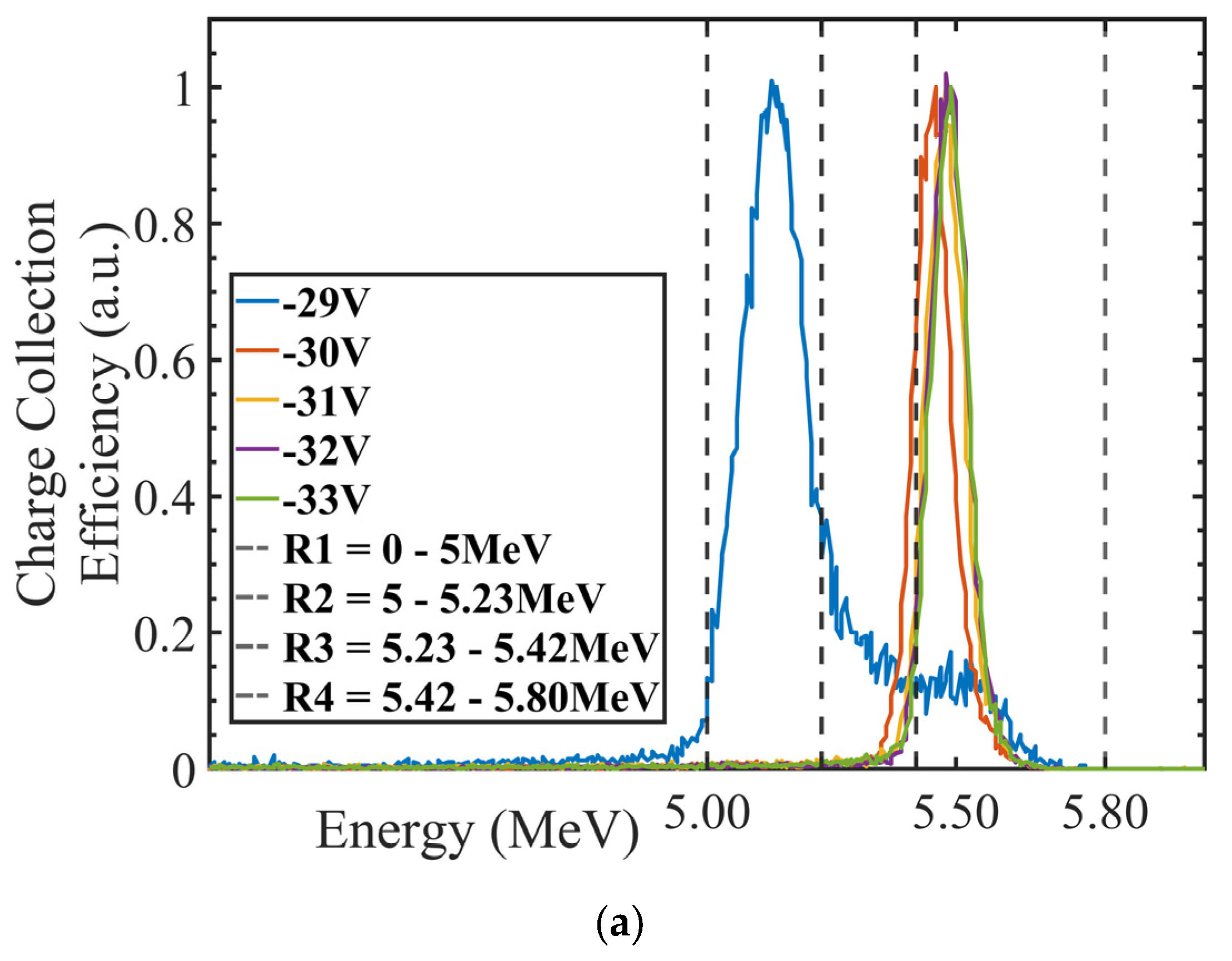
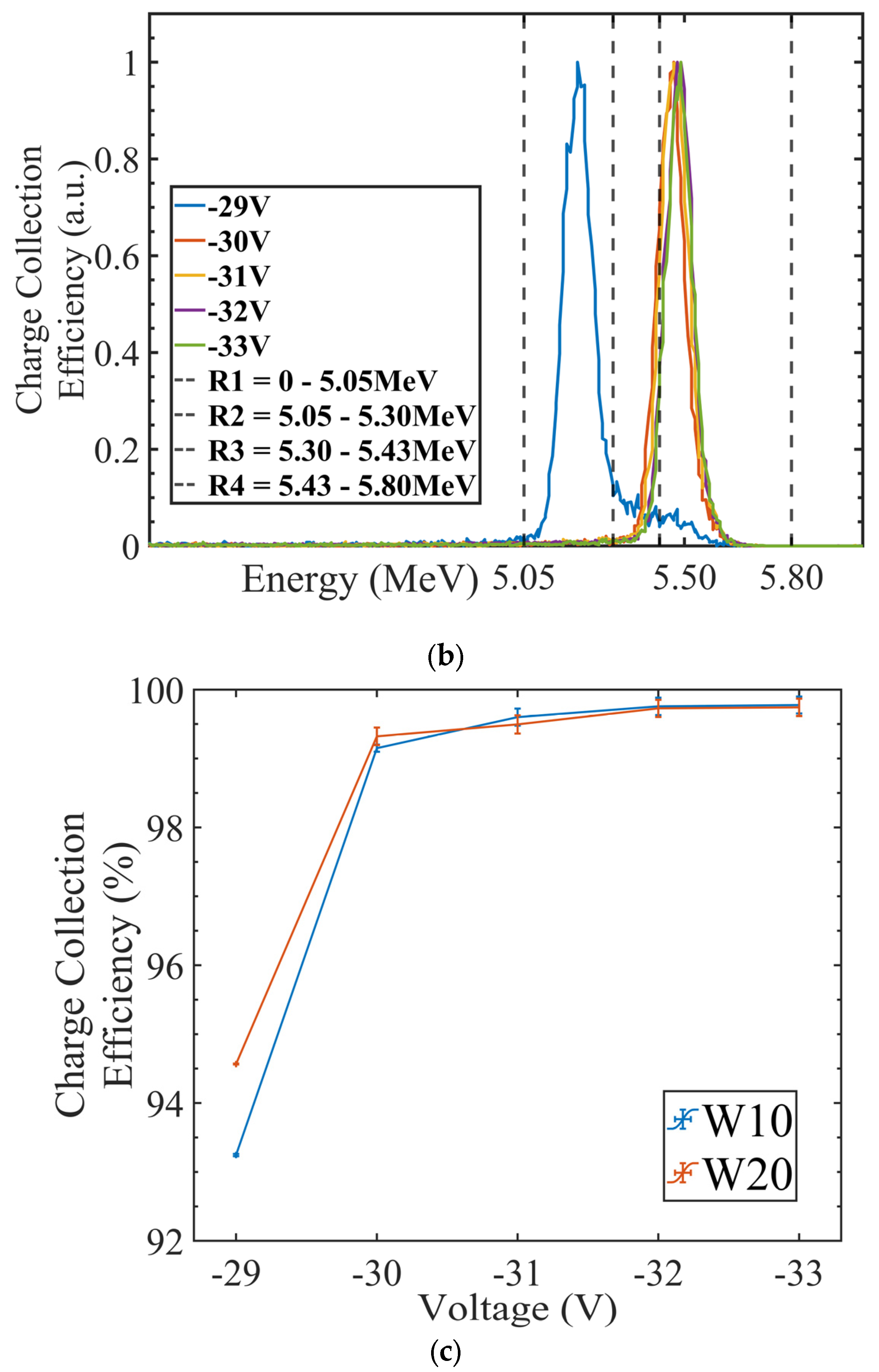
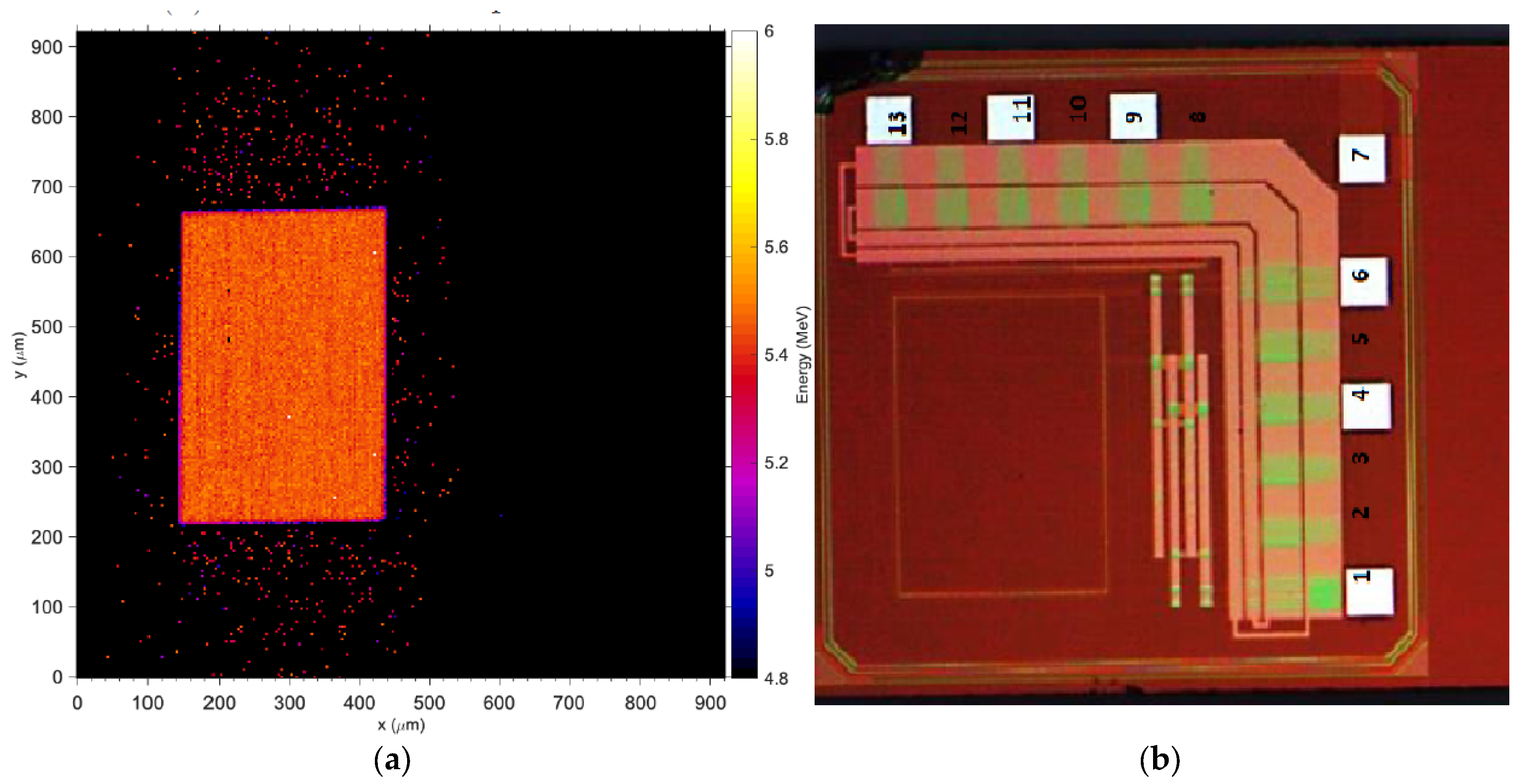
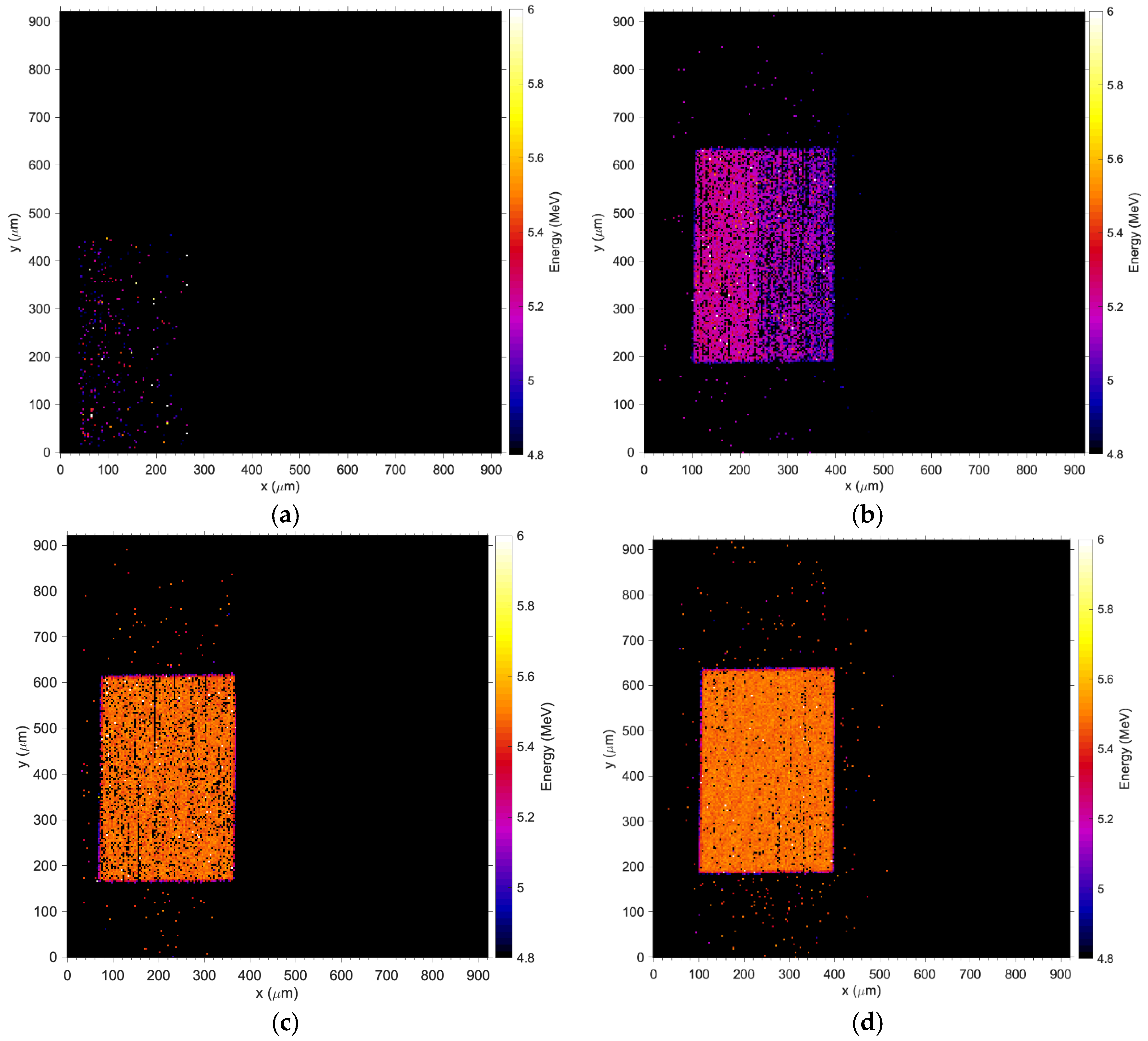
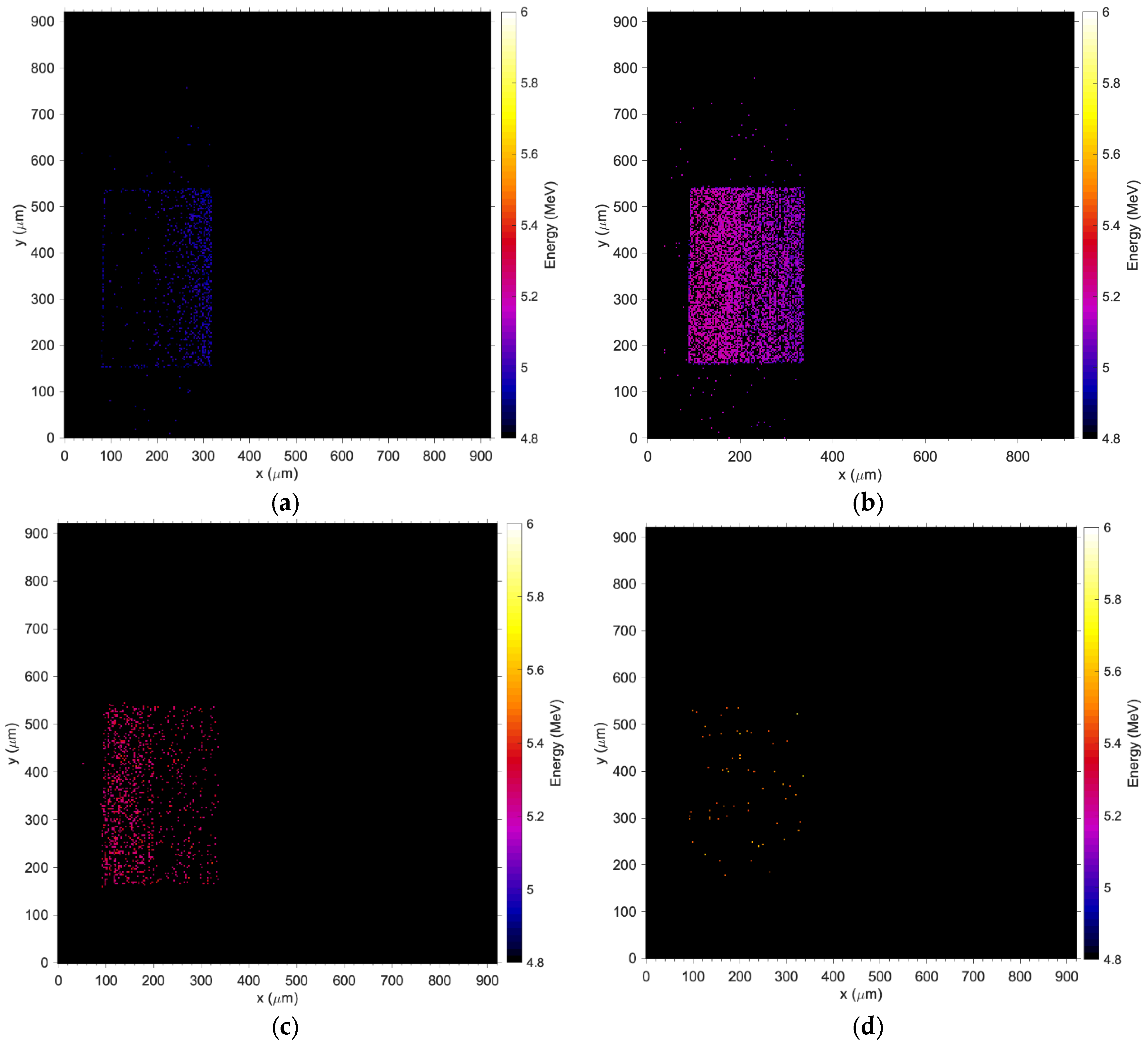
2.5. Charge Collection Imaging by Ion Beam Induced Charge (IBIC) Microscopy
2.6. Characterization of the Detector Response to an Ir-192 Gamma Source for HDR Brachytherapy
2.6.1. Source Localization and Tracking
2.6.2. Sensitivity
2.6.3. Depth Dose
3. Results
3.1. Charge Collection Mapping (IBIC)
3.2. Sensitivity and Calibration with Ir-192
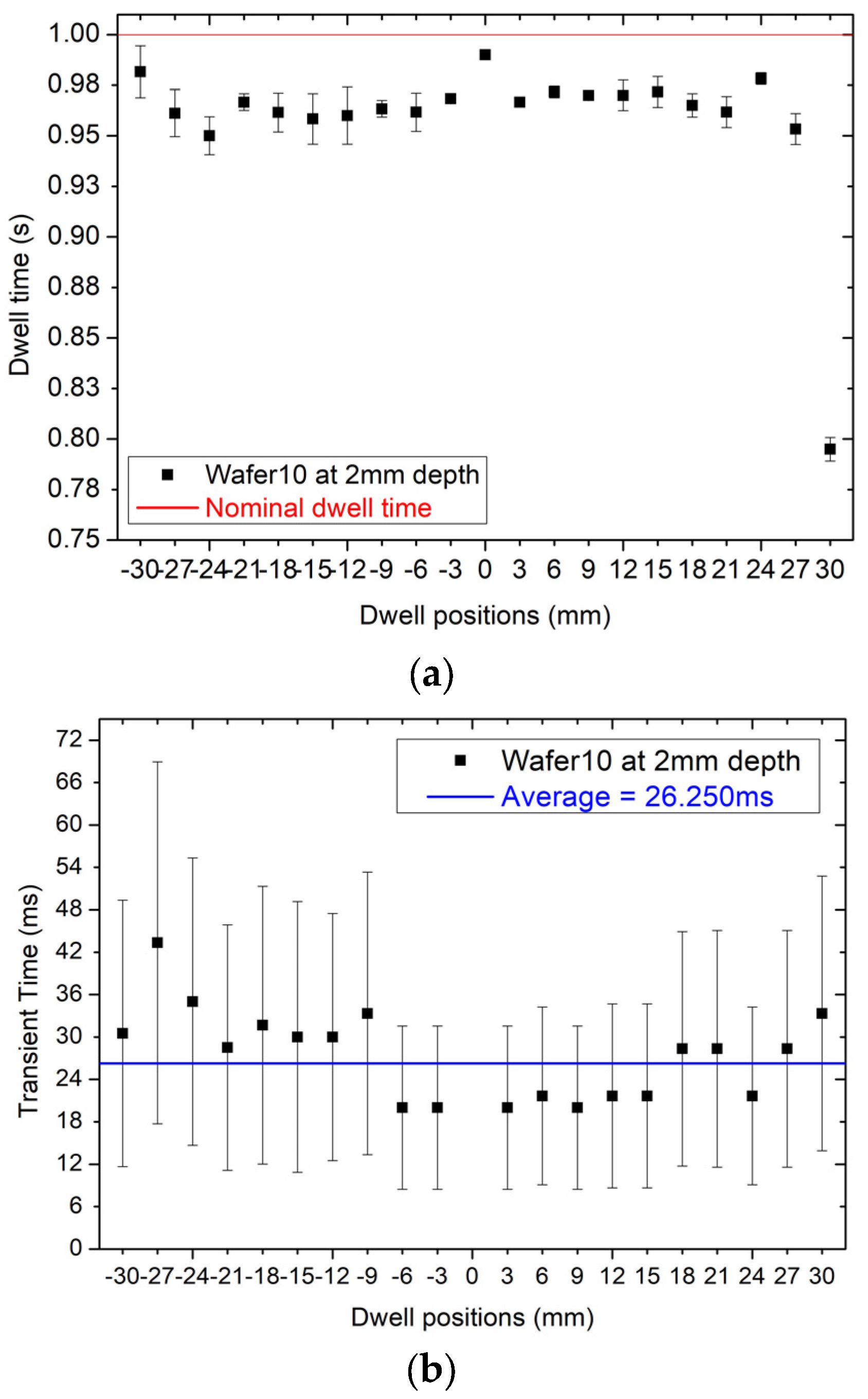
3.3. High Dose Rate (HDR) Source Localization with Ir-192
4. Discussion and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Strouthos, I.; Karagiannis, E.; Zamboglou, N.; Ferentinos, K. High-dose-rate brachytherapy for prostate cancer: Rationale, current applications, and clinical outcome. Cancer Rep. 2022, 5, e1450. [Google Scholar] [CrossRef] [PubMed]
- Valentin, J. Prevention of high-dose-rate brachytherapy accidents. ICRP Publication 97. Ann. ICRP 2005, 35, 1–51. [Google Scholar] [CrossRef] [PubMed]
- Lopez, P.O.; Andrea, P.; Cosset, J.-M.; Dutreix, A.; Landberg, T. Prevention of accidental exposures to patients undergoing radiation therapy. A report of the International Commission on Radiological Protection. Ann. ICRP 2000, 30, 7–70. [Google Scholar] [CrossRef]
- Kubo, H.D.; Glasgow, G.P.; Pethel, T.D.; Thomadsen, B.R.; Williamson, J.F. High dose-rate brachytherapy treatment delivery: Report of the AAPM Radiation Therapy Committee Task Group No. 59. Med. Phys. 1998, 25, 375–403. [Google Scholar] [CrossRef] [PubMed]
- Nath, R.; Anderson, L.L.; Meli, J.A.; Olch, A.J.; Stitt, J.A.; Williamson, J.F. Code of practice for brachytherapy physics: Report of the AAPM radiation therapy committee task group no. 56. Med. Phys. 1997, 24, 1557–1598. [Google Scholar] [CrossRef] [PubMed]
- Fonseca, G.P.; Johansen, J.G.; Smith, R.L.; Beaulieu, L.; Beddar, S.; Kertzscher, G.; Verhaegen, F.; Tanderup, K. In vivo dosimetry in brachytherapy: Requirements and future directions for research, development, and clinical practice. Phys. Imaging Radiat. Oncol. 2020, 16, 1–11. [Google Scholar] [CrossRef]
- Kertzscher, G.; Rosenfeld, A.; Beddar, S.; Tanderup, K.; Cygler, J.E. In vivo dosimetry: Trends and prospects for brachytherapy. Br. J. Radiol. 2014, 87, 20140206. [Google Scholar] [CrossRef]
- Tanderup, K.; Beddar, S.; Andersen, C.E.; Kertzscher, G.; Cygler, J.E. In vivo dosimetry in brachytherapy. Med. Phys. 2013, 40, 070902. [Google Scholar] [CrossRef]
- Jørgensen, E.B.; Kertzscher, G.; Buus, S.; Bentzen, L.; Hokland, S.B.; Rylander, S.; Tanderup, K.; Johansen, J.G. Accuracy of an in vivo dosimetry-based source tracking method for afterloading brachytherapy—A phantom study. Med. Phys. 2021, 48, 2614–2623. [Google Scholar] [CrossRef]
- Smith, R.L.; Hanlon, M.; Panettieri, V.; Millar, J.L.; Matheson, B.; Haworth, A.; Franich, R.D. An integrated system for clinical treatment verification of HDR prostate brachytherapy combining source tracking with pretreatment imaging. Brachytherapy 2018, 17, 111–121. [Google Scholar] [CrossRef]
- Espinoza, A.; Petasecca, M.; Fuduli, I.; Howie, A.; Bucci, J.; Corde, S.; Jackson, M.; Lerch, M.L.F.; Rosenfeld, A.B. The evaluation of a 2D diode array in “magic phantom” for use in high dose rate brachytherapy pretreatment quality assurance. Med. Phys. 2015, 42, 663–673. [Google Scholar] [CrossRef] [PubMed]
- Smith, R.L.; Haworth, A.; Millar, J.; Matheson, B.; Hindson, B.; Taylor, M.; Franich, R. Clinical implementation of in vivo source position verification in high dose rate prostate brachytherapy. Radiother. Oncol. 2015, 115, S87–S88. [Google Scholar] [CrossRef]
- Poder, J.; Cutajar, D.; Guatelli, S.; Petasecca, M.; Howie, A.; Bucci, J.; Rosenfeld, A. HDR brachytherapy in vivo source position verification using a 2D diode array: A Monte Carlo study. J. Appl. Clin. Med. Phys. 2018, 19, 163–172. [Google Scholar] [CrossRef] [PubMed]
- Beld, E.; Moerland, M.A.; Van Der Voort Van Zyp, J.R.N.; Viergever, M.A.; Lagendijk, J.J.W.; Seevinck, P.R. MRI artifact simulation for clinically relevant MRI sequences for guidance of prostate HDR brachytherapy. Phys. Med. Biol. 2019, 64, 095006. [Google Scholar] [CrossRef] [PubMed]
- Romanyukha, A.; Carrara, M.; Mazzeo, D.; Tenconi, C.; Al-Salmani, T.; Poder, J.; Cutajar, D.; Fuduli, I.; Petasecca, M.; Bucci, J.; et al. An innovative gynecological HDR brachytherapy applicator system for treatment delivery and real-time verification. Phys. Medica 2019, 59, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Vasyltsiv, R.; Qian, X.; Xu, Z.; Ryu, S.; Zhao, W.; Howansky, A. Feasibility of 4D HDR brachytherapy source tracking using C-arm tomography: Monte Carlo investigation. In Progress in Biomedical Optics and Imaging—Proceedings of SPIE; SPIE: Bellingham, WA, USA, 2022; Volume 12034. [Google Scholar] [CrossRef]
- Yogo, K.; Tatsuno, Y.; Shimo, T.; Noguchi, Y.; Okudaira, K.; Nozawa, M.; Ishiyama, H.; Yasuda, H.; Oguchi, H.; Yamamoto, S. Real-time tracking of source movement by Cherenkov emission imaging for high-dose-rate brachytherapy. J. Instrum. 2022, 17, T07001. [Google Scholar] [CrossRef]
- Watanabe, Y.; Muraishi, H.; Takei, H.; Hara, H.; Terazaki, T.; Shuto, N.; Shimo, T.; Nozawa, M.; Ishiyama, H.; Hayakawa, K.; et al. Automated source tracking with a pinhole imaging system during high-dose-rate brachytherapy treatment. Phys. Med. Biol. 2018, 63, 145002. [Google Scholar] [CrossRef]
- Smith, R.L.; Haworth, A.; Panettieri, V.; Millar, J.L.; Franich, R.D. A method for verification of treatment delivery in HDR prostate brachytherapy using a flat panel detector for both imaging and source tracking. Med. Phys. 2016, 43, 2435–2442. [Google Scholar] [CrossRef]
- Batič, M.; Burger, J.; Cindro, V.; Kramberger, G.; Mandic, I.; Mikuz, M.; Studen, A.; Zavrtanik, M. Verification of high dose rate 192Ir source position during brachytherapy treatment using silicon pixel detectors. IEEE Trans. Nucl. Sci. 2011, 58, 2250–2256. [Google Scholar] [CrossRef]
- Beddar, A.S.; Suchowerska, N.; Law, S.H. Plastic scintillation dosimetry for radiation therapy: Minimizing capture of Cerenkov radiation noise. Phys. Med. Biol. 2004, 49, 783. [Google Scholar] [CrossRef]
- Wootton, L.; Kudchadker, R.; Lee, A.; Beddar, S. Real-time in vivo rectal wall dosimetry using plastic scintillation detectors for patients with prostate cancer. Phys. Med. Biol. 2014, 59, 647. [Google Scholar] [CrossRef] [PubMed]
- Claus, G.; Colledani, C.; Dulinski, W.; Husson, D.; Turchetta, R.; Riester, J.; Deptuch, G.; Orazi, G.; Winter, M. Particle tracking using CMOS monolithic active pixel sensor. Nucl. Instrum. Methods Phys. Res. A 2001, 465, 120–124. [Google Scholar] [CrossRef]
- Deptuch, G.; Berst, J.D.; Claus, G.; Colledani, C.; Dulinski, W.; Goerlach, U.; Gornoushkin, Y.; Hu, Y.; Husson, D.; Orazi, G.; et al. Design and testing of monolithic active pixel sensors for charged particle tracking. In Proceedings of the IEEE Nuclear Science Symposium and Medical Imaging Conference, Lyon, France, 15–20 October 2000; Volume 1, pp. 3/41–3/48. Available online: https://www.scopus.com/inward/record.uri?eid=2-s2.0-0034593458&partnerID=40&md5=d4418f72f07148a6838ab52bbad160d8 (accessed on 2 January 2024).
- Passeri, D.; Placidi, P.; Verducci, L.; Ciampolini, P.; Matrella, G.; Marras, A.; Bilei, G.M. RAPS: An innovative active pixel for particle detection integrated in CMOS technology. Nucl. Instrum. Methods Phys. Res. Sect. A 2004, 518, 482–485. [Google Scholar] [CrossRef]
- Turchetta, R.; Allport, P.P.; Casse, G.; Clark, A.; Crooks, J.; Evans, A.; Fant, A.; Faruqi, A.; French, M.; Henderson, R.; et al. CMOS Monolithic Active Pixel Sensors (MAPS): New “eyes” for science. Nucl. Instrum. Methods Phys. Res. A 2006, 560, 139–142. [Google Scholar] [CrossRef]
- Turchetta, R.; French, M.; Manolopoulos, S.; Tyndel, M.; Allport, P.; Bates, R.; O’shea, V.; Hall, G.; Raymond, M. Monolithic active pixel sensors (MAPS) in a VLSI CMOS technology. Nucl. Instrum. Methods Phys. Res. Sect. A Accel. Spectrometers Detect. Assoc. Equip. 2003, 501, 251–259. [Google Scholar] [CrossRef]
- Contin, G.; Anderssen, E.; Greiner, L.; Schambach, J.; Silber, J.; Stezelberger, T.; Sun, X.; Szelezniak, M.; Vu, C.; Wieman, H.; et al. The STAR Heavy Flavor Tracker (HFT): Focus on the MAPS based PXL detector. Nucl. Part. Phys. Proc. 2016, 273–275, 1155–1159. [Google Scholar] [CrossRef]
- Heymes, J.; Ivory, J.; Stefanov, K.; Buggey, T.; Hetherington, O.; Soman, M.; Holland, A. Characterisation of a soft X-ray optimised CMOS Image Sensor. J. Instrum. 2022, 17, P05003. [Google Scholar] [CrossRef]
- Mager, M. ALPIDE, the Monolithic Active Pixel Sensor for the ALICE ITS upgrade. Nucl. Instrum. Methods Phys. Res. A 2016, 824, 434–438. [Google Scholar] [CrossRef]
- Servoli, L.; Fabiani, S.; Casale, M.; Devo, A.; Placidi, P.; Italiani, M. Use of CMOS image sensor to characterize brachytherapy HDR afterloader. Phys. Medica 2021, 92, S130. [Google Scholar] [CrossRef]
- Golshan, M.; Spadinger, I.; Chng, N. Source strength verification and quality assurance of preloaded brachytherapy needles using a CMOS flat panel detector. Med. Phys. 2016, 43, 3008–3018. [Google Scholar] [CrossRef]
- Pancheri, L.; Giampaolo, R.; Salvo, A.; Mattiazzo, S.; Corradino, T.; Giubilato, P.; Santoro, R.; Caccia, M.; Margutti, G.; Olave, J.E.; et al. Fully Depleted MAPS in 110-nm CMOS Process With 100–300-μm Active Substrate. IEEE Trans. Electron. Devices 2020, 67, 2393–2399. [Google Scholar] [CrossRef]
- Rosenfeld, A.B.; Cutajar, D.L.; Lerch, M.L.F.; Takacs, G.; Brady, J.; Braddock, T.; Perevertaylo, V.; Bucci, J.; Kearsley, J.; Zaider, M.; et al. In vivo dosimetry and seed localization in prostate brachytherapy with permanent implants. IEEE Trans. Nucl. Sci. 2004, 51, 3013–3018. [Google Scholar] [CrossRef]
- Fuduli, I.; Newall, M.K.; Espinoza, A.A.; Porumb, C.; Carolan, M.; Lerch, M.; Metcalfe, P.; Rosenfeld, A.; Petasecca, M. Multichannel Data Acquisition System comparison for Quality Assurance in external beam radiation therapy. Radiat. Meas. 2014, 71, 338–341. [Google Scholar] [CrossRef]
- Breese, M.B.H.; Vittone, E.; Vizkelethy, G.; Sellin, P.J. A review of ion beam induced charge microscopy. Nucl. Instrum. Meth. B 2007, 264, 345. [Google Scholar] [CrossRef]
- Pastuovic, Z.; Davis, J.; Linh Tran, T.; Paino, J.R.; Dipuglia, A.; James, B.; Povoli, M.; Kok, A.; Perevertaylo, V.L.; Siegele, R.; et al. IBIC microscopy—The powerful tool for testing micron—Sized sensitive volumes in segmented radiation detectors used in synchrotron microbeam radiation and hadron therapies. Nucl. Instrum. Methods Phys. Res. B 2019, 458, 90–96. [Google Scholar] [CrossRef]
- Pastuovic, Z.; Siegele, R.; Cohen, D.D.; Mann, M.; Ionescu, M.; Button, D.; Long, S. The new confocal heavy ion microprobe beamline at ANSTO: The first microprobe resolution tests and applications for elemental imaging and analysis. Nucl. Instrum. Methods Phys. Res. B 2017, 404, 1–8. [Google Scholar] [CrossRef]
- NIST. ASTAR: Stopping Power and Range Tables for Alpha Particles. NIST. Available online: https://physics.nist.gov/cgi-bin/Star/ap_table.pl (accessed on 21 August 2023).
- Granero, D.; Pérez-Calatayud, J.; Casal, E.; Ballester, F.; Venselaar, J. A dosimetric study on the high dose rate Flexisource. Med. Phys. 2006, 33, 4578–4582. [Google Scholar] [CrossRef]
- Rivard, M.J.; Coursey, B.M.; DeWerd, L.A.; Hanson, W.F.; Huq, M.S.; Ibbott, G.S.; Mitch, M.G.; Nath, R.; Williamson, J.F. Update of AAPM Task Group No. 43 Report: A revised AAPM protocol for brachytherapy dose calculations. Med. Phys. 2004, 31, 633–674. [Google Scholar] [CrossRef]




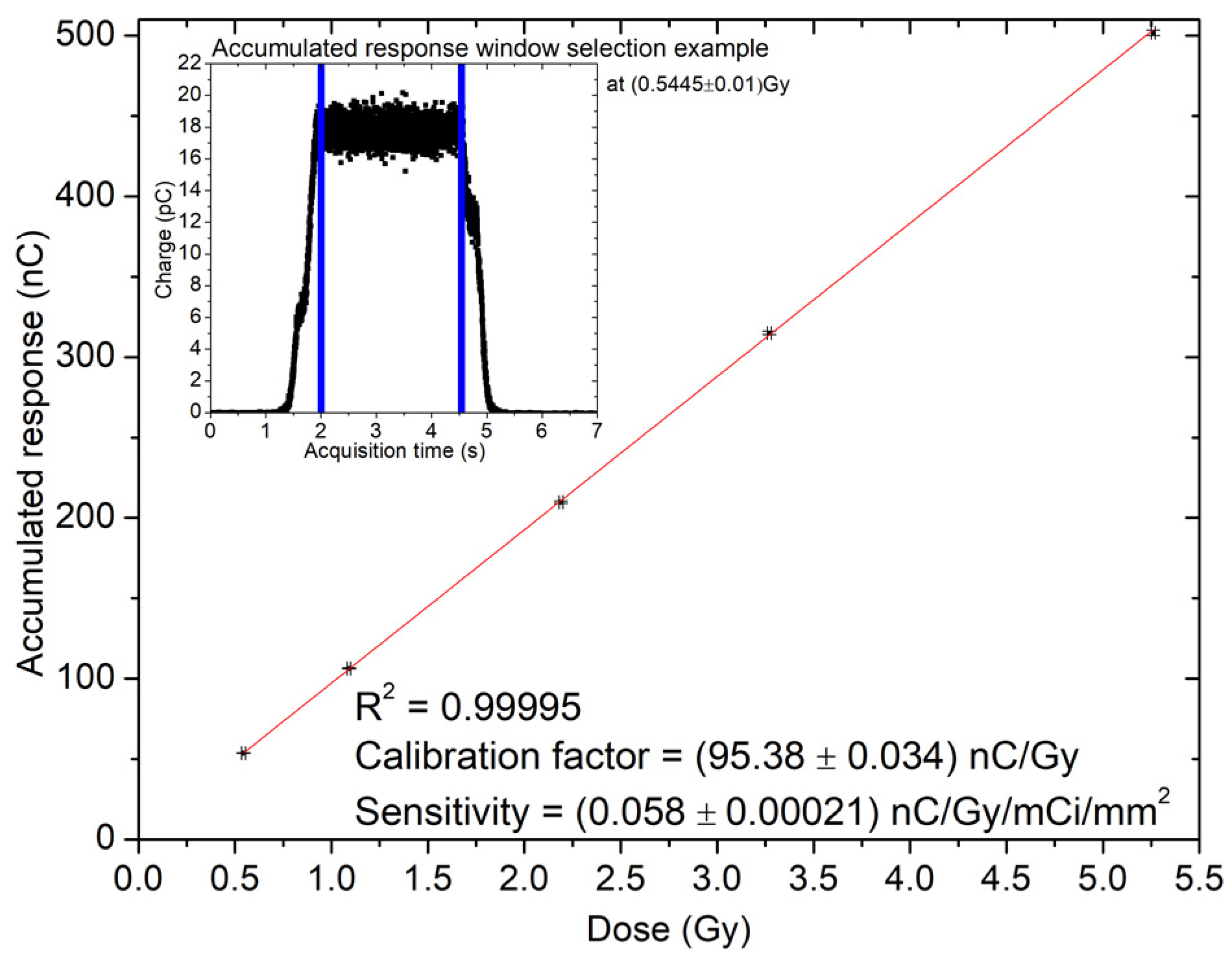


| Dwell Time (s) | Dose (Gy) | Integral Response (nC) |
|---|---|---|
| 3 | 0.54 ± 0.01 | 53.69 ± 1.00 |
| 6 | 1.09 ± 0.01 | 106.37 ± 1.04 |
| 12 | 2.18 ± 0.01 | 209.86 ± 1.21 |
| 18 | 3.27 ± 0.01 | 315.09 ± 1.48 |
| 29 | 5.26 ± 0.01 | 501.81 ± 2.02 |
| Wafer | Sensitivity (nC Gy−1 mCi−1 mm−2) |
|---|---|
| W10 | (58 ± 0.21) × 10−3 |
| W20 | (36 ± 1.4) × 10−3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bui, T.N.H.; Large, M.; Poder, J.; Bucci, J.; Bianco, E.; Giampaolo, R.A.; Rivetti, A.; Da Rocha Rolo, M.; Pastuovic, Z.; Corradino, T.; et al. Preliminary Characterization of an Active CMOS Pad Detector for Tracking and Dosimetry in HDR Brachytherapy. Sensors 2024, 24, 692. https://doi.org/10.3390/s24020692
Bui TNH, Large M, Poder J, Bucci J, Bianco E, Giampaolo RA, Rivetti A, Da Rocha Rolo M, Pastuovic Z, Corradino T, et al. Preliminary Characterization of an Active CMOS Pad Detector for Tracking and Dosimetry in HDR Brachytherapy. Sensors. 2024; 24(2):692. https://doi.org/10.3390/s24020692
Chicago/Turabian StyleBui, Thi Ngoc Hang, Matthew Large, Joel Poder, Joseph Bucci, Edoardo Bianco, Raffaele Aaron Giampaolo, Angelo Rivetti, Manuel Da Rocha Rolo, Zeljko Pastuovic, Thomas Corradino, and et al. 2024. "Preliminary Characterization of an Active CMOS Pad Detector for Tracking and Dosimetry in HDR Brachytherapy" Sensors 24, no. 2: 692. https://doi.org/10.3390/s24020692
APA StyleBui, T. N. H., Large, M., Poder, J., Bucci, J., Bianco, E., Giampaolo, R. A., Rivetti, A., Da Rocha Rolo, M., Pastuovic, Z., Corradino, T., Pancheri, L., & Petasecca, M. (2024). Preliminary Characterization of an Active CMOS Pad Detector for Tracking and Dosimetry in HDR Brachytherapy. Sensors, 24(2), 692. https://doi.org/10.3390/s24020692







