Photoacoustic Resonators for Non-Invasive Blood Glucose Detection Through Photoacoustic Spectroscopy: A Systematic Review
Abstract
:1. Introduction
1.1. Invasive Blood Glucose Monitoring
1.2. Non-Invasive Blood Glucose Monitoring
- Sensitivity: This denotes the minimum concentration that a sensor can detect. A blood glucose sensor should be capable of identifying glucose levels as low as 30 mg/dL [11].
- Stability: This pertains to the performance of a measurement device over an extended period. The device should exhibit high precision, ensuring that measurements remain consistent for the same concentration. Additionally, it should offer a high level of accuracy, meaning that measurements should not fluctuate over time.
- Selectivity: The measurement method must be able to distinguish the glucose signal from signals generated by other substances. Since glucose in the human body is present in aqueous solutions that also contain ions or proteins, which could produce interfering signals, the sensor must effectively isolate the glucose signal.
- Portability: The measurement device should be compact and convenient to carry.
2. Principle of Photoacoustic Spectroscopy for Non-Invasive Glucose Detection
2.1. Basic Interaction of IR Light with Human Skin/Tissue
2.2. Principle of Generating and Detecting Photoacoustic Signals
2.3. Amplification Mechanism of Photoacoustic Resonator (PAR)
2.4. Design and Modeling of Photoacoustic Resonator
2.5. Requirements of PAR for Non-Invasive Glucose Detection
- Humidity issue:
- Volume and surface loss:
- Location and position of light source and cylinders:
- Signal-to-noise ratio:
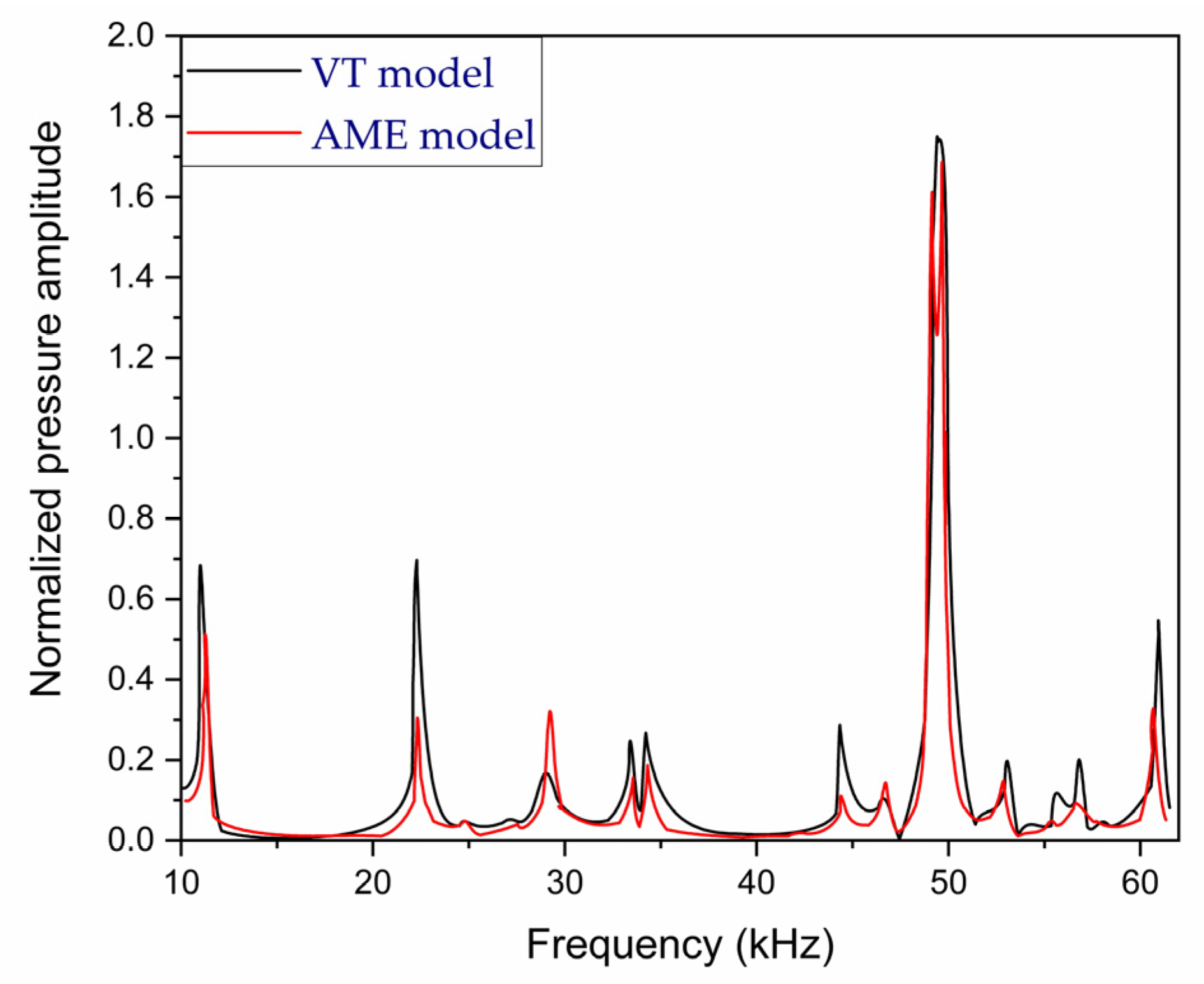
3. History of PA Cells Used in PAS for Non-Invasive Blood Glucose Detection
4. Prospects of PARs for Non-Invasive Glucose Detection
- Finding proper geometry:
- Identifying proper resonant frequency of cell:
- Observation of detection sensitivity and signal-to-noise ratio (SNR):
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Diabetes. Available online: https://www.who.int/health-topics/diabetes?gad_source=1#tab=tab_1 (accessed on 25 July 2024).
- Diabetes Facts and Figures|International Diabetes Federation. Available online: https://idf.org/about-diabetes/diabetes-facts-figures/ (accessed on 25 July 2024).
- Cho, N.H.; Shaw, J.E.; Karuranga, S.; Huang, Y.; da Rocha Fernandes, J.D.; Ohlrogge, A.W.; Malanda, B. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res. Clin. Pract. 2018, 138, 271–281. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Thompson, T.J.; Cheng, Y.J.; Zhuo, X.; Zhang, P.; Gregg, E.; Rolka, D.B. Projection of the future diabetes burden in the United States through 2060. Popul. Health Metr. 2018, 16, 9. [Google Scholar] [CrossRef] [PubMed]
- Standards of Medical Care in Diabetes—2010. Diabetes Care 2010, 33, S11–S61. [CrossRef] [PubMed]
- Clark, L.C.; Lyons, C. ELECTRODE SYSTEMS FOR CONTINUOUS MONITORING IN CARDIOVASCULAR SURGERY. Ann. N. Y. Acad. Sci. 1962, 102, 29–45. [Google Scholar] [CrossRef] [PubMed]
- Villena Gonzales, W.; Mobashsher, A.; Abbosh, A. The Progress of Glucose Monitoring—A Review of Invasive to Minimally and Non-Invasive Techniques, Devices and Sensors. Sensors 2019, 19, 800. [Google Scholar] [CrossRef]
- Phenobarbital—Health Encyclopedia—University of Rochester Medical Center 2017. Available online: https://www.urmc.rochester.edu/encyclopedia/content.aspx?ContentTypeID=167&ContentID=glucose_urine (accessed on 29 July 2024).
- Ross, D.G. Urinalysis. In Imaging and Technology in Urology; Springer International Publishing: Cham, Switzerland, 2023; pp. 171–175. [Google Scholar] [CrossRef]
- Tang, L.; Chang, S.J.; Chen, C.-J.; Liu, J.-T. Non-Invasive Blood Glucose Monitoring Technology: A Review. Sensors 2020, 20, 6925. [Google Scholar] [CrossRef]
- von Lilienfeld-Toal, H.; Weidenmüller, M.; Xhelaj, A.; Mäntele, W. A novel approach to non-invasive glucose measurement by mid-infrared spectroscopy: The combination of quantum cascade lasers (QCL) and photoacoustic detection. Vib. Spectrosc. 2005, 38, 209–215. [Google Scholar] [CrossRef]
- Park, H.D.; Lee, K.J.; Yoon, H.R.; Nam, H.H. Design of a portable urine glucose monitoring system for health care. Comput. Biol. Med. 2005, 35, 275–286. [Google Scholar] [CrossRef]
- Panchbhai, A.S. Correlation of Salivary Glucose Level with Blood Glucose Level in Diabetes Mellitus. J. Oral Maxillofac. Res. 2012, 3, e3. [Google Scholar] [CrossRef]
- Iguchi, S.; Kudo, H.; Saito, T.; Ogawa, M.; Saito, H.; Otsuka, K.; Funakubo, A.; Mitsubayashi, K. A flexible and wearable biosensor for tear glucose measurement. Biomed. Microdevices 2007, 9, 603–609. [Google Scholar] [CrossRef]
- Moyer, J.; Wilson, D.; Finkelshtein, I.; Wong, B.; Potts, R. Correlation Between Sweat Glucose and Blood Glucose in Subjects with Diabetes. Diabetes Technol. Ther. 2012, 14, 398–402. [Google Scholar] [CrossRef] [PubMed]
- Delbeck, S.; Vahlsing, T.; Leonhardt, S.; Steiner, G.; Heise, H.M. Non-invasive monitoring of blood glucose using optical methods for skin spectroscopy—Opportunities and recent advances. Anal. Bioanal. Chem. 2019, 411, 63–77. [Google Scholar] [CrossRef] [PubMed]
- Pleitez, M.; von Lilienfeld-Toal, H.; Mäntele, W. Infrared spectroscopic analysis of human interstitial fluid in vitro and in vivo using FT-IR spectroscopy and pulsed quantum cascade lasers (QCL): Establishing a new approach to non invasive glucose measurement. Spectrochim. Acta Part A Mol. Biomol. Spectrosc. 2012, 85, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Definition of biomarker—NCI Dictionary of Cancer Terms—NCI. Available online: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/biomarker (accessed on 19 August 2024).
- Non-Invasive Blood Glucose Monitoring System Market Size Envisioned at USD 202.73 Million by 2032. Available online: https://www.towardshealthcare.com/insights/non-invasive-blood-glucose-monitoring-system-market (accessed on 21 October 2024).
- Huang, J.; Zhang, Y.; Wu, J. Review of non-invasive continuous glucose monitoring based on impedance spectroscopy. Sens. Actuators A Phys. 2020, 311, 112103. [Google Scholar] [CrossRef]
- Buehler, L.A.; Balasubramanian, V.; Baskerville, S.; Bailey, R.; McCarthy, K.; Rippen, M.; Bena, J.F.; Lansang, M.C. Noninvasive Glucose Monitor Using Dielectric Spectroscopy. Endocr. Pract. 2022, 28, 142–147. [Google Scholar] [CrossRef]
- Sieg, A.; Guy, R.H.; Delgado-Charro, M.B. Noninvasive Glucose Monitoring by Reverse Iontophoresis in Vivo: Application of the Internal Standard Concept. Clin. Chem. 2004, 50, 1383–1390. [Google Scholar] [CrossRef]
- Tang, F.; Wang, X.; Wang, D.; Li, J. Non-Invasive Glucose Measurement by Use of Metabolic Heat Conformation Method. Sensors 2008, 8, 3335–3344. [Google Scholar] [CrossRef]
- Kost, J. Ultrasound-Assisted Insulin Delivery and Noninvasive Glucose Sensing. Diabetes Technol. Ther. 2002, 4, 489–497. [Google Scholar] [CrossRef]
- Kaysir, M.R.; Song, J.; Rassel, S.; Aloraynan, A.; Ban, D. Progress and Perspectives of Mid-Infrared Photoacoustic Spectroscopy for Non-Invasive Glucose Detection. Biosensors 2023, 13, 716. [Google Scholar] [CrossRef]
- Ballerstadt, R.; Evans, C.; Gowda, A.; McNichols, R. In Vivo Performance Evaluation of a Transdermal Near- Infrared Fluorescence Resonance Energy Transfer Affinity Sensor for Continuous Glucose Monitoring. Diabetes Technol. Ther. 2006, 8, 296–311. [Google Scholar] [CrossRef]
- March, W.; Lazzaro, D.; Rastogi, S. Fluorescent Measurement in the Non-Invasive Contact Lens Glucose Sensor. Diabetes Technol. Ther. 2006, 8, 312–317. [Google Scholar] [CrossRef]
- Esenaliev, R.O.; Larin, K.V.; Larina, I.V.; Motamedi, M. Noninvasive monitoring of glucose concentration with optical coherence tomography. Opt. Lett. 2001, 26, 992. [Google Scholar] [CrossRef]
- Enejder, A.M.K.; Scecina, T.G.; Oh, J.; Hunter, M.; Shih, W.-C.; Sasic, S.; Horowitz, G.L.; Feld, M.S. Raman spectroscopy for noninvasive glucose measurements. J. Biomed. Opt. 2005, 10, 031114. [Google Scholar] [CrossRef] [PubMed]
- Lambert, J.L.; Pelletier, C.C.; Borchert, M. Glucose determination in human aqueous humor with Raman spectroscopy. J. Biomed. Opt. 2005, 10, 031110. [Google Scholar] [CrossRef] [PubMed]
- Maruo, K.; Tsurugi, M.; Tamura, M.; Ozaki, Y. In Vivo Noninvasive Measurement of Blood Glucose by Near-Infrared Diffuse-Reflectance Spectroscopy. Appl. Spectrosc. 2003, 57, 1236–1244. [Google Scholar] [CrossRef] [PubMed]
- Marbach, R.; Koschinsky, T.; Gries, F.A.; Heise, H.M. Noninvasive Blood Glucose Assay by Near-Infrared Diffuse Reflectance Spectroscopy of the Human Inner Lip. Appl. Spectrosc. 1993, 47, 875–881. [Google Scholar] [CrossRef]
- Malik, B.H.; Coté, G.L. Real-time, closed-loop dual-wavelength optical polarimetry for glucose monitoring. J. Biomed. Opt. 2010, 15, 017002. [Google Scholar] [CrossRef] [PubMed]
- Purvinis, G.; Cameron, B.D.; Altrogge, D.M. Noninvasive Polarimetric-Based Glucose Monitoring: An in Vivo Study. J. Diabetes Sci. Technol. 2011, 5, 380–387. [Google Scholar] [CrossRef]
- Vrančić, C.; Fomichova, A.; Gretz, N.; Herrmann, C.; Neudecker, S.; Pucci, A.; Petrich, W. Continuous glucose monitoring by means of mid-infrared transmission laser spectroscopy in vitro. Analyst 2011, 136, 1192. [Google Scholar] [CrossRef]
- Spanner, G.; Nießner, R. New concept for the non-invasive determination of physiological glucose concentrations using modulated laser diodes. Anal. Bioanal. Chem. 1996, 354, 306–310. [Google Scholar] [CrossRef]
- Kottmann, J.; Rey, J.M.; Sigrist, M.W. New photoacoustic cell design for studying aqueous solutions and gels. Rev. Sci. Instrum. 2011, 82, 084903. [Google Scholar] [CrossRef] [PubMed]
- Spanner, G.; Niessner, R. Noninvasive determination of blood constituents using an array of modulated laser diodes and a photoacoustic sensor head. Anal. Bioanal. Chem. 1996, 355, 327–328. [Google Scholar] [CrossRef] [PubMed]
- Pai, P.P.; Sanki, P.K.; Banerjee, S. A photoacoustics based continuous non-invasive blood glucose monitoring system. In Proceedings of the 2015 IEEE International Symposium on Medical Measurements and Applications (MeMeA) Proceedings, Torino, Italy, 7–9 May 2015; IEEE: Piscataway, NJ, USA, 2015; pp. 106–111. [Google Scholar]
- Kottmann, J.; Grob, U.; Rey, J.; Sigrist, M. Mid-Infrared Fiber-Coupled Photoacoustic Sensor for Biomedical Applications. Sensors 2013, 13, 535–549. [Google Scholar] [CrossRef] [PubMed]
- Pleitez, M.A.; Lieblein, T.; Bauer, A.; Hertzberg, O.; von Lilienfeld-Toal, H.; Mäntele, W. In Vivo Noninvasive Monitoring of Glucose Concentration in Human Epidermis by Mid-Infrared Pulsed Photoacoustic Spectroscopy. Anal. Chem. 2013, 85, 1013–1020. [Google Scholar] [CrossRef] [PubMed]
- Beard, P. Biomedical photoacoustic imaging. Interface Focus 2011, 1, 602–631. [Google Scholar] [CrossRef]
- Kottmann, J.; Rey, J.M.; Sigrist, M.W. Mid-Infrared Photoacoustic Detection of Glucose in Human Skin: Towards Non-Invasive Diagnostics. Sensors 2016, 16, 1663. [Google Scholar] [CrossRef]
- Christison, G.B.; MacKenzie, H.A. Laser photoacoustic determination of physiological glucose concentrations in human whole blood. Med. Biol. Eng. Comput. 1993, 31, 284–290. [Google Scholar] [CrossRef]
- Fakhlaei, R.; Babadi, A.A.; Sun, C.; Ariffin, N.M.; Khatib, A.; Selamat, J.; Xiaobo, Z. Application, challenges and future prospects of recent nondestructive techniques based on the electromagnetic spectrum in food quality and safety. Food Chem. 2024, 441, 138402. [Google Scholar] [CrossRef]
- Yadav, J.; Rani, A.; Singh, V.; Murari, B.M. Prospects and limitations of non-invasive blood glucose monitoring using near-infrared spectroscopy. Biomed. Signal Process. Control 2015, 18, 214–227. [Google Scholar] [CrossRef]
- Burmeister, J.J.; Arnold, M.A. Evaluation of Measurement Sites for Noninvasive Blood Glucose Sensing with Near-Infrared Transmission Spectroscopy. Clin. Chem. 1999, 45, 1621–1627. [Google Scholar] [CrossRef]
- Olesberg, J.T.; Arnold, M.A.; Mermelstein, C.; Schmitz, J.; Wagner, J. Tunable Laser Diode System for Noninvasive Blood Glucose Measurements. Appl. Spectrosc. 2005, 59, 1480–1484. [Google Scholar] [CrossRef] [PubMed]
- Liakat, S.; Bors, K.A.; Huang, T.-Y.; Michel, A.P.M.; Zanghi, E.; Gmachl, C.F. In vitro measurements of physiological glucose concentrations in biological fluids using mid-infrared light. Biomed. Opt. Express 2013, 4, 1083. [Google Scholar] [CrossRef] [PubMed]
- Rosencwaig, A. Photoacoustic Spectroscopy of Biological Materials. Science 1973, 181, 657–658. [Google Scholar] [CrossRef] [PubMed]
- MacKenzie, H.A.; Ashton, H.S.; Spiers, S.; Shen, Y.; Freeborn, S.S.; Hannigan, J.; Lindberg, J.; Rae, P. Advances in Photoacoustic Noninvasive Glucose Testing. Clin. Chem. 1999, 45, 1587–1595. [Google Scholar] [CrossRef] [PubMed]
- El-Busaidy, S.; Baumann, B.; Wolff, M.; Duggen, L.; Bruhns, H. Experimental and Numerical Investigation of a Photoacoustic Resonator for Solid Samples: Towards a Non-Invasive Glucose Sensor. Sensors 2019, 19, 2889. [Google Scholar] [CrossRef]
- Cox, B.; Laufer, J.G.; Arridge, S.R.; Beard, P.C. Quantitative spectroscopic photoacoustic imaging: A review. J. Biomed. Opt. 2012, 17, 061202. [Google Scholar] [CrossRef]
- Rosenthal, A.; Ntziachristos, V.; Razansky, D. Model-based optoacoustic inversion with arbitrary-shape detectors. Med. Phys. 2011, 38, 4285–4295. [Google Scholar] [CrossRef]
- Nie, L.; Chen, X. Structural and functional photoacoustic molecular tomography aided by emerging contrast agents. Chem. Soc. Rev. 2014, 43, 7132–7170. [Google Scholar] [CrossRef]
- Baumann, B.; Kost, B.; Wolff, M.; Groning, H. Modeling and Numerical Investigation of Photoacoustic Resonators. In Modelling and Simulation; Intech Open Access Publisher: London, UK, 2008. [Google Scholar] [CrossRef]
- Duggen, L.; Lopes, N.; Willatzen, M.; Rubahn, H.-G. Finite Element Simulation of Photoacoustic Pressure in a Resonant Photoacoustic Cell Using Lossy Boundary Conditions. Int. J. Thermophys. 2011, 32, 774–785. [Google Scholar] [CrossRef]
- Glière, A.; Rouxel, J.; Brun, M.; Parvitte, B.; Zéninari, V.; Nicoletti, S. Challenges in the Design and Fabrication of a Lab-on-a-Chip Photoacoustic Gas Sensor. Sensors 2014, 14, 957–974. [Google Scholar] [CrossRef]
- Baumann, B.; Wolff, M.; Kost, B.; Groninga, H. Finite element calculation of photoacoustic signals. Appl. Opt. 2007, 46, 1120. [Google Scholar] [CrossRef] [PubMed]
- Pleitez, M.A.; Lieblein, T.; Bauer, A.; Hertzberg, O.; von Lilienfeld-Toal, H.; Mäntele, W. Windowless ultrasound photoacoustic cell for in vivo mid-IR spectroscopy of human epidermis: Low interference by changes of air pressure, temperature, and humidity caused by skin contact opens the possibility for a non-invasive monitoring of glucose in the interstitial fluid. Rev. Sci. Instrum. 2013, 84, 084901. [Google Scholar] [CrossRef] [PubMed]
- Sim, J.Y.; Ahn, C.-G.; Jeong, E.-J.; Kim, B.K. In vivo Microscopic Photoacoustic Spectroscopy for Non-Invasive Glucose Monitoring Invulnerable to Skin Secretion Products. Sci. Rep. 2018, 8, 1059. [Google Scholar] [CrossRef] [PubMed]
- El-Busaidy, S.; Baumann, B.; Wolff, M.; Duggen, L. Shape optimization of an open photoacoustic resonator. Appl. Sci. 2021, 11, 2571. [Google Scholar] [CrossRef]
- Camou, S.; Haga, T.; Tajima, T.; Tamechika, E. Detection of aqueous glucose based on a cavity size- and optical-wavelength-independent continuous-wave photoacoustic technique. Anal. Chem. 2012, 84, 4718–4724. [Google Scholar] [CrossRef]
- Sensors Council. 2013 IEEE sensors. In Proceedings of the 12th IEEE Sensors Conference, Baltimore, MD, USA, 3–6 November 2013; ISBN 9781467346429. [Google Scholar]
- Wadamori, N. Behavior of long-period measurements using a small-sized photoacoustic cell for aqueous glucose monitoring. In Proceedings of the 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015; IEEE: Piscataway, NJ, USA, 2015; pp. 1267–1270. [Google Scholar] [CrossRef]
- Sim, J.Y.; Ahn, C.; Jeong, E.; Kim, B. Photoacoustic spectroscopy that uses a resonant characteristic of a microphone for in vitro measurements of glucose concentration. In Proceedings of the Engineering in Medicine and Biology Society IEEE, Orlando, FL, USA, 16–20 August 2016. [Google Scholar] [CrossRef]
- Zhao, S.; Tao, W.; He, Q.; Zhao, H.; Yang, H. Glucose solution determination based on liquid photoacoustic resonance. Appl. Opt. 2017, 56, 193. [Google Scholar] [CrossRef]
- El-Busaidy, S.A.S.; Baumann, B.; Wolff, M.; Duggen, L. Modelling of open photoacoustic resonators. Photoacoustics 2020, 18, 100161. [Google Scholar] [CrossRef]
- Yang, L.; Chen, C.; Zhang, Z.; Wei, X. Glucose Determination by a Single 1535 nm Pulsed Photoacoustic Technique: A Multiple Calibration for the External Factors. J. Healthc. Eng. 2022, 2022, 1–10. [Google Scholar] [CrossRef]
- Aloraynan, A.; Rassel, S.; Kaysir, M.R.; Ban, D. Dual quantum cascade lasers for noninvasive glucose detection using photoacoustic spectroscopy. Sci. Rep. 2023, 13, 7927. [Google Scholar] [CrossRef]
- ISHIHARA, Y.; WADAMORI, N. A Study on Enhancement of Sensitivity of a PhotoAcoustic Detector Cell for Non-invasive Measurements Based on Finite Element Method Analysis(Symposium on Biomedical Engineering 2007). Trans. Jpn. Soc. Med. Biol. Eng. BME 2008, 46, 238–245. [Google Scholar]
- Tachibana, K.; Okada, K.; Kobayashi, R.; Ishihara, Y. Development of a high-sensitivity and portable cell using Helmholtz resonance for noninvasive blood glucose-level measurement based on photoacoustic spectroscopy. In Proceedings of the 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 16–20 August 2016; pp. 6477–6480. [Google Scholar] [CrossRef]
- Takamoto, R.; Namba, R.; Matsuoka, M.; Sawada, T. Human in vivo percutaneous absorptiometry using the laser-photoacoustic method. Anal. Chem. 1992, 64, 2661–2663. [Google Scholar] [CrossRef] [PubMed]
- Takamoto, R.; Yamamoto, S.; Namba, R.; Takamatsu, T.; Matsuoka, M.; Sawada, T. In vivo Percutaneous Absorptiometry by a Laser Photoacoustic Method Using a Novel Open-Ended Cell Combined with Light Guide. Anal. Chem. 1994, 66, 2267–2271. [Google Scholar] [CrossRef]





| Year of Publication | Excitation Wavelength (nm) | Type of PA Cell | Frequency Range (kHz) | Q-Factor | Investigated Sample | Glucose Level (mg/dL) | Schematic of PA Cell |
|---|---|---|---|---|---|---|---|
| 2012 [63] | 1382 and 1610 | Cylindrical Fiber-coupled | 300–500 | ----- | Aqueous glucose solution | 50, 100, 150 |  |
| 2012 [41] | 8196 to 10,000 | T-shaped | 50–54 | 102 | Fingertips of healthy and diabetes affected volunteers | <50, and <300 |  |
| 2013 [64] | 1382 to 1610 | Cylindrical Fiber-coupled | 300–500 | ------ | Aqueous glucose solution | 0–100 |  |
| 2013 [40] | 9090 to 9132 | Conical | ------ | ------- | Both in aqueous glucose solution and different body sites of human | 30–500 |  |
| 2013 [60] | 8032 to 10,000 | T-shaped | 50–60 | ------ | Fingertips of healthy and diabetes-affected volunteers | 30–500 |  |
| 2015 [65] | 1550 | T-shaped | 5.05 (resonance frequency of PA cell) | ------ | Aqueous glucose solution | 30–500 | 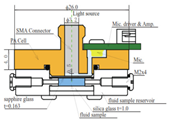 |
| 2016 [66] | 8064 to 11,111 | T-shaped | 51 (resonance frequency of PA cell) | ------ | Carbon black tape as reference sample | 1000 |  |
| 2016 [43] | 8032 to 10,000 | Conical | ------- | ------- | Both aqueous glucose solution and human fingertips | 0–440 |  |
| 2017 [67] | 1064 | Cylindrical | 310 (resonant peak of PZT) | ------ | Aqueous glucose solution | 20–100 |  |
| 2018 [61] | 8000 to 11,111 | T-shaped | 47.5 (resonant peak of PA cell) | ------ | Index fingertip | ------ |  |
| 2020 [68] | ----- | T-shaped | 10–60 | ----- | ------ | ----- |  |
| 2022 [69] | 1535 | Bowl-shaped | 0–5 (for bandpass signal processing) | ------ | Aqueous glucose solution | 30 to 500 | 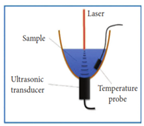 |
| 2023 [70] | 9250 | T-shaped | 10 to 40 (with a frequency step of 0.15 kHz) | ------ | Biomedical skin phantom | 100 to 275 |  |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaysir, M.R.; Zaman, T.M.; Rassel, S.; Wang, J.; Ban, D. Photoacoustic Resonators for Non-Invasive Blood Glucose Detection Through Photoacoustic Spectroscopy: A Systematic Review. Sensors 2024, 24, 6963. https://doi.org/10.3390/s24216963
Kaysir MR, Zaman TM, Rassel S, Wang J, Ban D. Photoacoustic Resonators for Non-Invasive Blood Glucose Detection Through Photoacoustic Spectroscopy: A Systematic Review. Sensors. 2024; 24(21):6963. https://doi.org/10.3390/s24216963
Chicago/Turabian StyleKaysir, Md Rejvi, Thasin Mohammad Zaman, Shazzad Rassel, Jishen Wang, and Dayan Ban. 2024. "Photoacoustic Resonators for Non-Invasive Blood Glucose Detection Through Photoacoustic Spectroscopy: A Systematic Review" Sensors 24, no. 21: 6963. https://doi.org/10.3390/s24216963
APA StyleKaysir, M. R., Zaman, T. M., Rassel, S., Wang, J., & Ban, D. (2024). Photoacoustic Resonators for Non-Invasive Blood Glucose Detection Through Photoacoustic Spectroscopy: A Systematic Review. Sensors, 24(21), 6963. https://doi.org/10.3390/s24216963






