Investigation of Possible Sources of Electrodermal Activity in Surgical Personnel to Assess Workplace Stress Levels
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Hard- and Software
2.3. Experimental Procedure
2.4. Statistical Analysis
3. Results
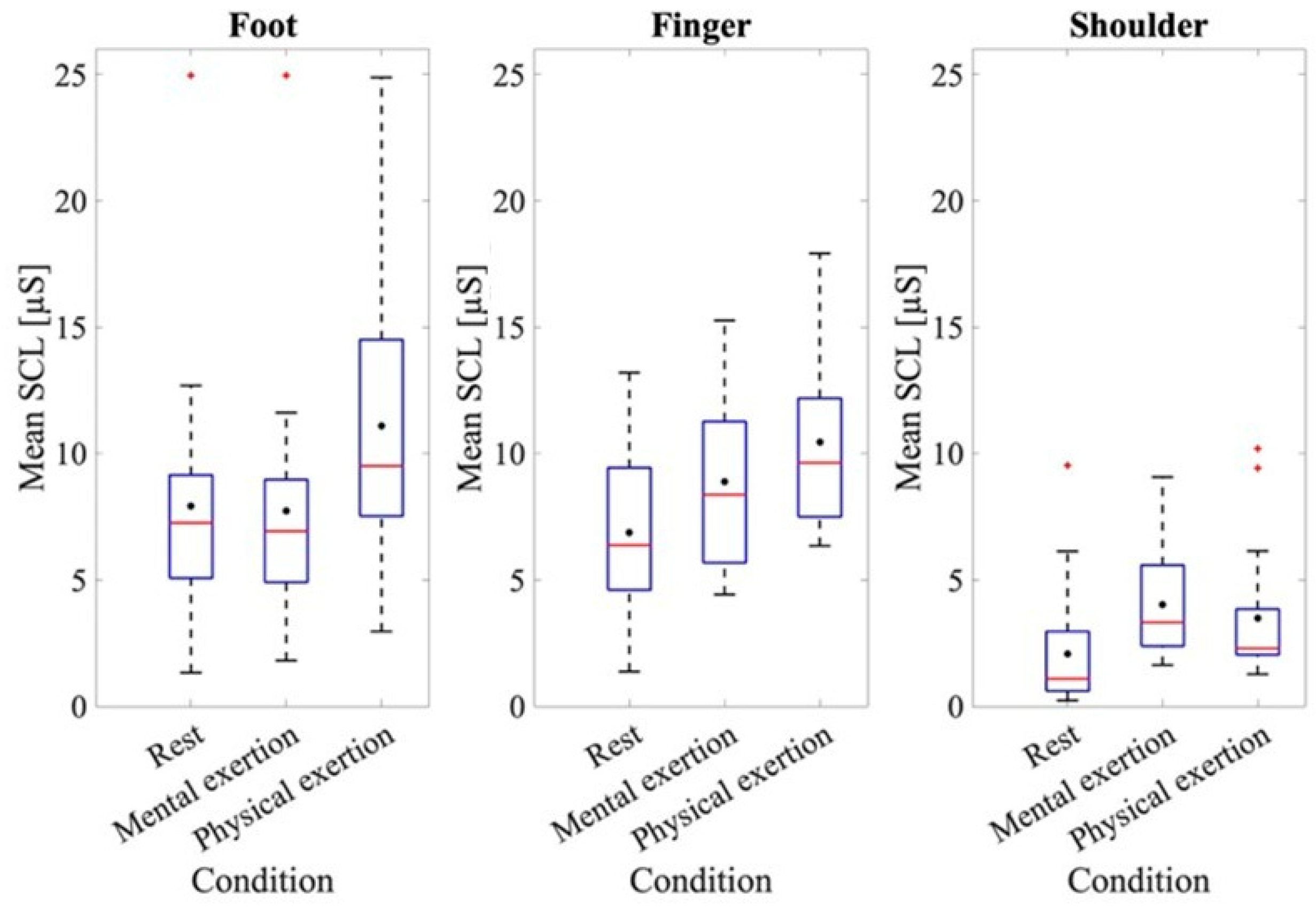
3.1. EDA Data
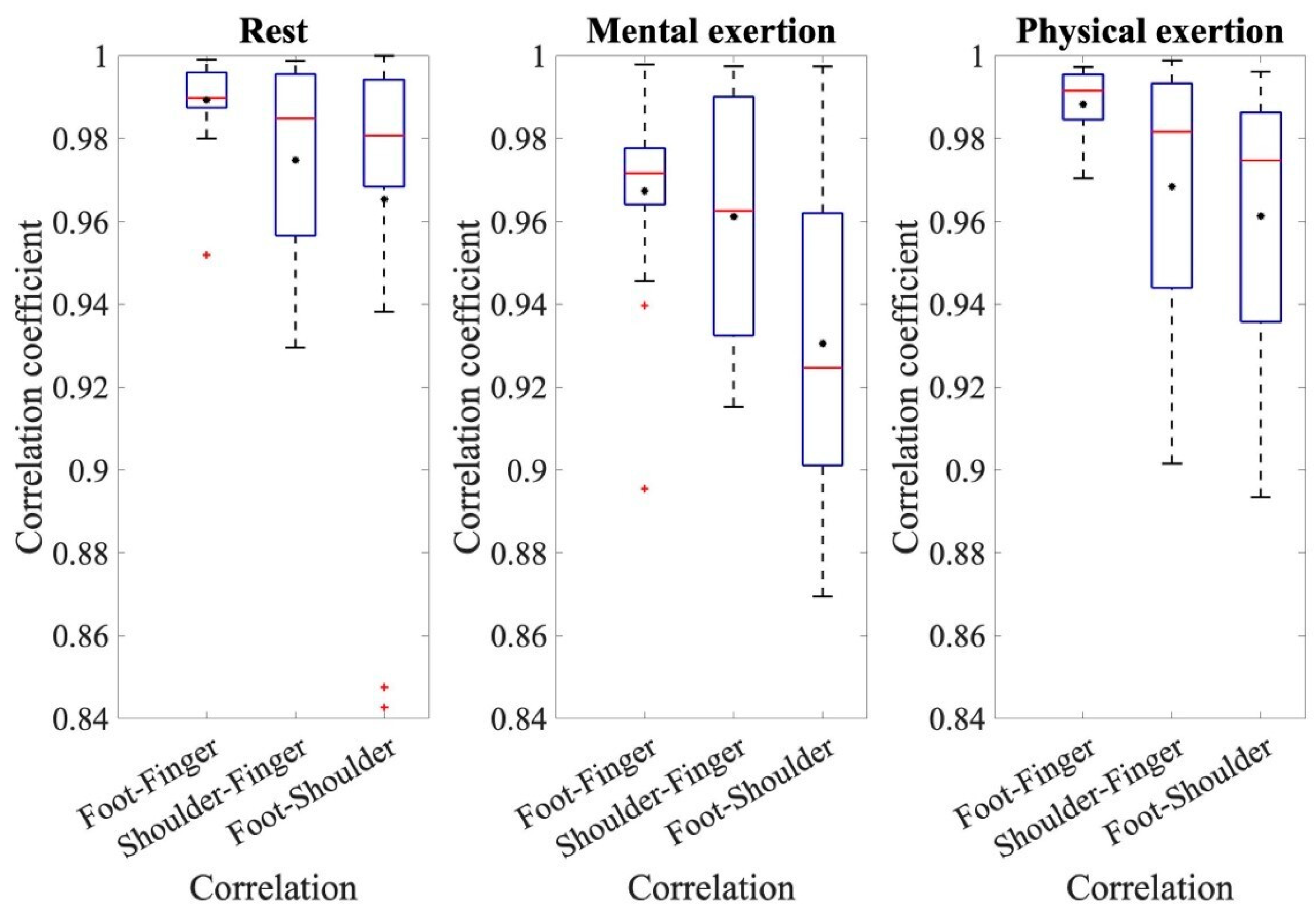
3.2. Correlation Coefficients
3.3. ECG Data
3.4. Comparison of ECG and EDA Data
3.5. Post-Hoc Power Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Arora, S.; Sevdalis, N.; Nestel, D.; Woloshynowych, M.; Darzi, A.; Kneebone, R. The impact of stress on surgical performance: A systematic review of the literature. Surgery 2010, 147, 318–330. [Google Scholar] [CrossRef] [PubMed]
- Anton, N.E.; Montero, P.N.; Howley, L.D.; Brown, C.; Stefanidis, D. What stress coping strategies are surgeons relying upon during surgery? Am. J. Surg. 2015, 210, 846–851. [Google Scholar] [CrossRef] [PubMed]
- Shanafelt, T.D.; Balch, C.M.; Dyrbye, L.; Bechamps, G.; Russell, T.; Satele, D.; Rummans, T.; Swartz, K.; Novotny, P.J.; Sloan, J.; et al. Special report: Suicidal ideation among American surgeons. Arch. Surg. 2011, 146, 54–62. [Google Scholar] [CrossRef] [PubMed]
- So, P. NASA TLX Task Load Index; NASA: Washington, DC, USA, 2020.
- Wilson, M.R.; Poolton, J.M.; Malhotra, N.; Ngo, K.; Bright, E.; Masters, R.S. Development and validation of a surgical workload measure: The surgery task load index (Surg-TLX). World J. Surg. 2011, 35, 1961–1969. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Lowndes, B.; Chrouser, K.; Hallbeck, S.; McCrory, B. Developing a subjective instrument for laparoscopic surgical workload in a high fidelity simulator using the NASA-TLX and Surg-TLX. IISE Trans. Healthc. Syst. Eng. 2020, 11, 161–169. [Google Scholar] [CrossRef]
- Maaoui, C.; Pruski, A.; Abdat, F. Emotion recognition for human-machine communication. In Proceedings of the IEEE/RSJ International Conference on Intelligent Robots and Systems, Nice, France, 22–26 September 2008; pp. 1210–1215. [Google Scholar]
- Camm, A.J.; Malik, M.; Bigger, J.T.; Breithardt, G.; Cerutti, S.; Cohen, R.J.; Coumel, P.; Fallen, E.L.; Kennedy, H.L.; Kleiger, R.E. Heart rate variability: Standards of measurement, physiological interpretation and clinical use. Task force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Ann. Noninvasive Electrocardiol. 1996, 1, 151–181. [Google Scholar]
- Darrow, C.W. The rationale for treating the change in galvanic skin response as a change in conductance. Psychophysiology 1964, 1, 31–38. [Google Scholar] [CrossRef]
- Voss, A.; Schulz, S.; Schroeder, R.; Baumert, M.; Caminal, P. Methods derived from nonlinear dynamics for analysing heart-rate variability. Philos. Trans. R. Soc. A Math. Phys. Eng. Sci. 2009, 367, 277–296. [Google Scholar] [CrossRef]
- Boucsein, W. Electrodermal Activity; Springer Science & Business Media: New York, NY, USA, 2012. [Google Scholar]
- Boucsein, W. Elektrodermale Aktivität: Grundlagen, Methoden und Anwendungen; Springer: Heidelberg, Germany, 2013. [Google Scholar]
- Rahma, O.N.; Putra, A.P.; Rahmatillah, A.; Putri, Y.S.K.A.; Fajriaty, N.D.; Ain, K.; Chai, R. Electrodermal Activity for Measuring Cognitive and Emotional Stress Level. J. Med. Signals Sens. 2022, 12, 155–162. [Google Scholar] [CrossRef]
- Dawson, M.E.; Schell, A.M.; Filion, D.L. The Electrodermal System; Cambridge University Press: Cambridge, UK, 2017. [Google Scholar]
- Venables, P.H.; Christie, M.J. Electrodermal activity. In Techniques in Psychophysiology; Academic Press: London, UK, 1980; p. 54. [Google Scholar]
- Edelberg, R. Electrical properties of the skin. In Methods in Psychophysiology; Williams & Wilkins: Baltimore, MD, USA, 1967. [Google Scholar]
- Edelberg, R. Electrical activity of the skin: Its measurement and uses in psychophysiology. In Handbook of Psychophysiology; Rinehart & Winston: New York, NY, USA, 1972; pp. 367–418. [Google Scholar]
- Harker, M. Psychological Sweating: A Systematic Review Focused on Aetiology and Cutaneous Response. Skin Pharmacol. Physiol. 2013, 26, 92–100. [Google Scholar] [CrossRef]
- Saga, K. Structure and Function of Human Sweat Glands Studied with Histochemistry and Cytochemistry. Prog. Histochem. Cytochem. 2002, 37, 323–386. [Google Scholar] [CrossRef] [PubMed]
- Randall, W.C. Quantitation and Regional Distribution of Sweat Glands in Man. J. Clin. Investig. 1946, 25, 761–767. [Google Scholar] [CrossRef] [PubMed]
- van Dooren, M.; de Vries, J.J.G.; Janssen, J.H. Emotional Sweating across the Body: Comparing 16 Different Skin Conductance Measurement Locations. Physiol. Behav. 2012, 106, 298–304. [Google Scholar] [CrossRef]
- Plewig, G.; Ruzicka, T.; Prinz, J.C.; Kaufmann, R.; Hertl, M. (Eds.) Braun-Falco’s Dermatologie, Venerologie und Allergologie; Springer: Berlin, Germany, 2018. [Google Scholar]
- Freedman, L.W.; Scerbo, A.S.; Dawson, M.E.; Raine, A.; McClure, W.O.; Venables, P.H. The relationship of sweat gland count to electrodermal activity. Psychophysiology 1994, 31, 196–200. [Google Scholar] [CrossRef] [PubMed]
- Hedman, E.; Miller, L.; Schoen, S.; Nielsen, D.; Goodwin, M.; Picard, R. Measuring Autonomic Arousal during Therapy. In Proceedings of the 8th International Design and Emotion Conference, London, UK, 11–14 September 2012; Central Saint Martins College of Art & Design: London, UK, 2012. [Google Scholar]
- Rickles, W., Jr.; Day, J. Electrodermal activity in non-palmer skin sites. Psychophysiology 1968, 4, 421–435. [Google Scholar] [CrossRef] [PubMed]
- Payne, A.F.; Schell, A.M.; Dawson, M.E. Lapses in skin conductance responding across anatomical sites: Comparison of fingers, feet, forehead, and wrist. Psychophysiology 2016, 53, 1984–1992. [Google Scholar] [CrossRef]
- Hossain, M.B.; Kong, Y.; Posada-Quintero, H.F.; Chon, K.H. Comparison of Electrodermal Activity from Multiple Body Locations Based on Standard EDA Indices’ Quality and Robustness Against Motion Artifact. Sensors 2022, 22, 3177. [Google Scholar] [CrossRef]
- Sano, A.; Picard, R.W.; Stickgold, R. Quantitative Analysis of Wrist Electrodermal Activity during Sleep. Int. J. Psychophysiol. 2014, 94, 382–389. [Google Scholar] [CrossRef]
- Poh, M.-Z.; Swenson, N.C.; Picard, R.W. A Wearable Sensor for Unobtrusive, Long-Term Assessment of Electrodermal Activity. IEEE Trans. Biomed. Eng. 2010, 57, 1243–1252. [Google Scholar]
- Van Der Mee, D.J.; Kuhlmann, A.Y.; Veldhuis, J.; Wiegant, V.M. Validity of Electrodermal Activity-Based Measures of Sympathetic Nervous System Activity from a Wrist-Worn Device. Int. J. Psychophysiol. 2021, 168, 52–64. [Google Scholar] [CrossRef]
- Weyn, S.; Poldrack, R.A.; Dorr, A.E.; Cloninger, C.R.; Cuthbert, B.N. Individual Differences in Environmental Sensitivity at Physiological and Phenotypic Level: Two Sides of the Same Coin? Int. J. Psychophysiol. 2022, 176, 36–53. [Google Scholar] [CrossRef] [PubMed]
- Kasos, K.; Kekecs, Z.; Kasos, E.; Szekely, A.; Varga, K. Bilateral Electrodermal Activity in the Active-Alert Hypnotic Induction. Int. J. Clin. Exp. Hypn. 2018, 66, 282–297. [Google Scholar] [CrossRef] [PubMed]
- Kasos, K.; Kekecs, Z.; Kasos, E.; Szekely, A.; Varga, K. Electrodermal activity for measuring cognitive and emotional stress level: A systematic review. J. Clin. Exp. Psychophysiol. 2017, 9, 139–150. [Google Scholar]
- Shields, S.A.; MacDowell, K.A.; Fairchild, S.B.; Campbell, M.L. Is mediation of sweating cholinergic, adrenergic, or both? A comment on the literature. Psychophysiology 1987, 24, 312–319. [Google Scholar] [CrossRef]
- PLUX Wireless Biosignals S.A. Biosignal Acquisition Toolkit for Advanced Research Applications: User Manual. Available online: https://support.pluxbiosignals.com/wp-content/uploads/2021/11/biosignalsplux_User_Manual.pdf (accessed on 6 June 2023).
- PLUX Wireless Biosignals S.A. Electrodermal Activity (EDA) Sensor Datasheet. Available online: https://support.pluxbiosignals.com/wp-content/uploads/2021/11/Electrodermal_Activity_EDA_Datasheet.pdf (accessed on 3 November 2023).
- PLUX Wireless Biosignals S.A. Electrocardiography (ECG) Sensor User Manual. Available online: https://support.pluxbiosignals.com/wp-content/uploads/2021/10/biosignalsplux-Electrocardiography-ECG-User-Manual.pdf (accessed on 6 June 2023).
- Woodrum, D.T.; Andreatta, P.B.; Yellamanchilli, R.K.; Feryus, L.; Gauger, P.G.; Minter, R.M. Construct validity of the LapSim laparoscopic surgical simulator. Am. J. Surg. 2006, 191, 28–32. [Google Scholar] [CrossRef]
- Dean, A.; Voss, D.; Draguljić, D. Design and Analysis of Experiments; Springer International Publishing: Cham, Switzerland, 2017; ISBN 978-3-319-52248-7. [Google Scholar]
- Sato, K.; Kang, W.; Saga, K.; Sato, K. Biology of Sweat Glands and Their Disorders. II. Disorders of Sweat Gland Function. J. Am. Acad. Dermatol. 1989, 20, 713–726. [Google Scholar] [CrossRef]
- Payne, A.F.; Dawson, M.E.; Schell, A.M.; Singh, K.; Courtney, C.G. Can you give me a hand? A comparison of hands and feet as optimal anatomical sites for skin conductance recording. Psychophysiology 2013, 50, 1965–1969. [Google Scholar] [CrossRef]
- Schumm, J.; Bächlin, M.; Setz, C.; Arnrich, B.; Roggen, D.; Tröster, G. Effect of movements on the electrodermal response after a startle event. Methods Inf. Med. 2008, 47, 186–191. [Google Scholar]

| Trial | Heartbeats Per Minute |
|---|---|
| Rest | 74.50 ± 9.58 |
| Mental exertion 1 | 87.09 ± 11.85 |
| Physical exertion 1 | 124.95 ± 20.27 |
| Mental exertion 2 | 88.44 ± 15.33 |
| Physical exertion 2 | 126.06 ± 20.87 |
| Mental exertion 3 | 92.01 ± 13.87 |
| Physical exertion 3 | 127.16 ± 18.67 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schlender, M.; Uslar, V.; Uppenkamp, S.; Tabriz, N.; Weyhe, D.; Cetin, T. Investigation of Possible Sources of Electrodermal Activity in Surgical Personnel to Assess Workplace Stress Levels. Sensors 2024, 24, 7172. https://doi.org/10.3390/s24227172
Schlender M, Uslar V, Uppenkamp S, Tabriz N, Weyhe D, Cetin T. Investigation of Possible Sources of Electrodermal Activity in Surgical Personnel to Assess Workplace Stress Levels. Sensors. 2024; 24(22):7172. https://doi.org/10.3390/s24227172
Chicago/Turabian StyleSchlender, Merle, Verena Uslar, Stefan Uppenkamp, Navid Tabriz, Dirk Weyhe, and Timur Cetin. 2024. "Investigation of Possible Sources of Electrodermal Activity in Surgical Personnel to Assess Workplace Stress Levels" Sensors 24, no. 22: 7172. https://doi.org/10.3390/s24227172
APA StyleSchlender, M., Uslar, V., Uppenkamp, S., Tabriz, N., Weyhe, D., & Cetin, T. (2024). Investigation of Possible Sources of Electrodermal Activity in Surgical Personnel to Assess Workplace Stress Levels. Sensors, 24(22), 7172. https://doi.org/10.3390/s24227172






