Proposal for a Battery to Evaluate Functional Capacity in Older Adults with Disabilities
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Measurement
2.3.1. Neuromuscular Functionality
2.3.2. Functionality in Combined Actions
2.3.3. Functionality in Acceleration
2.3.4. Functionality in Balance
2.3.5. Cardiovascular Functionality
2.4. Statistical Analysis
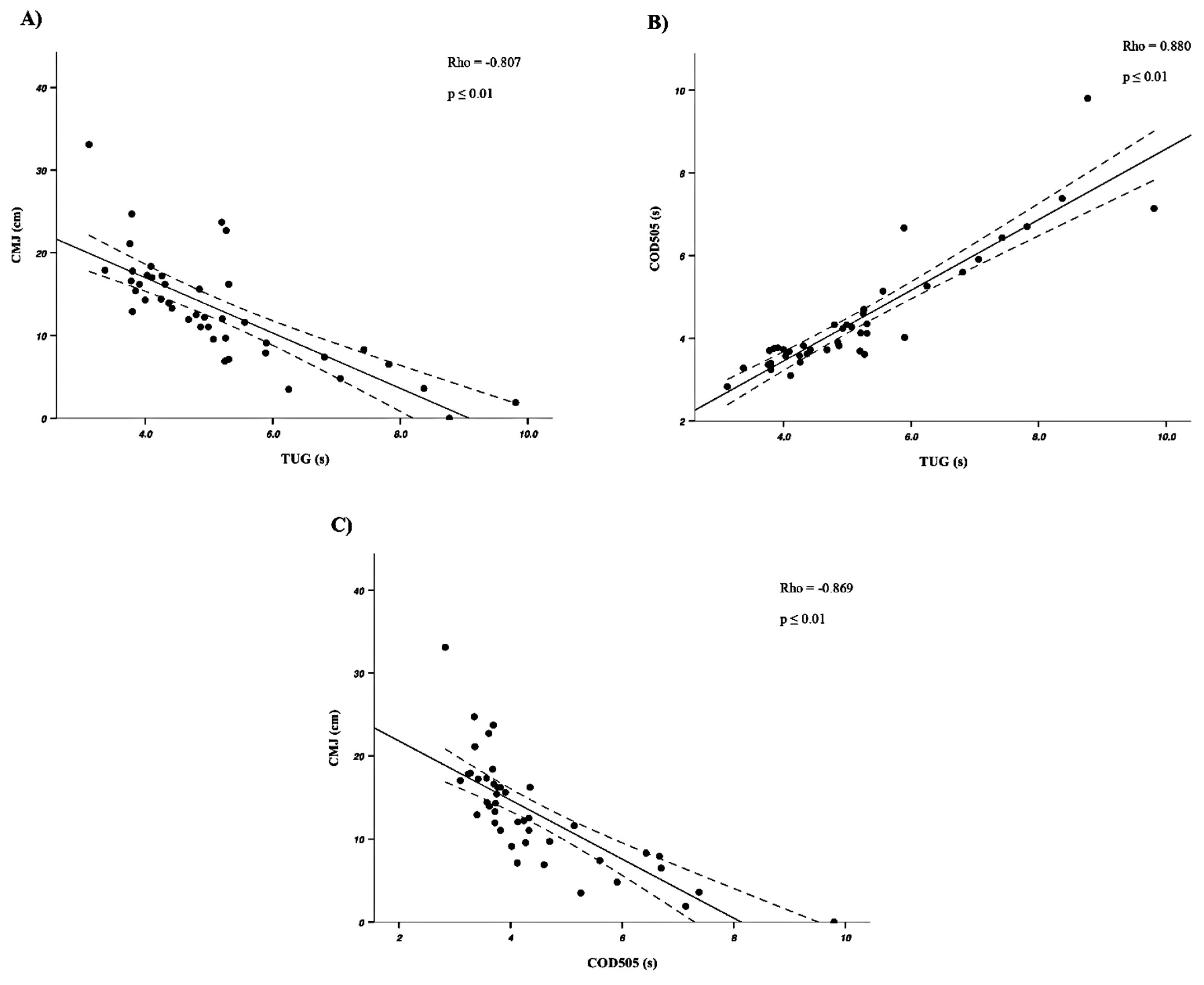
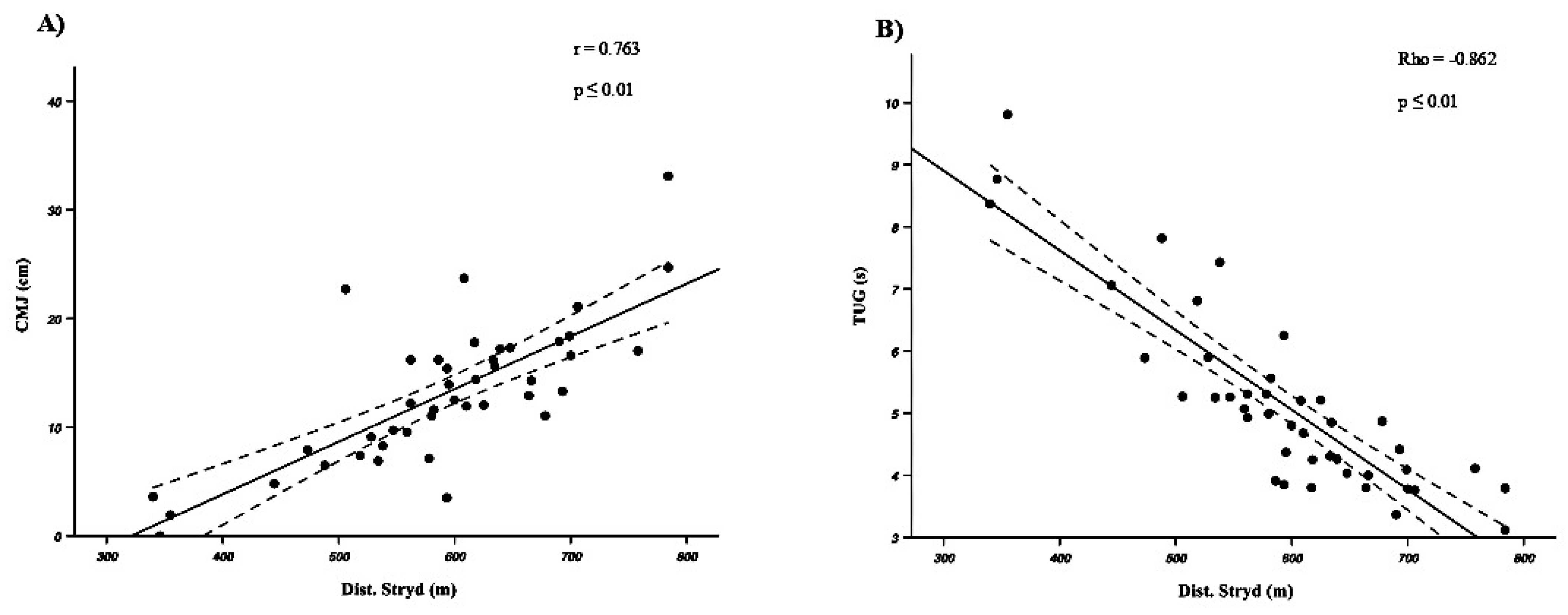
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (Ed.) International Classification of Functioning, Disability and Health: ICF; World Health Organization: Geneva, Switzerland, 2001; ISBN 978-92-4-154542-6. [Google Scholar]
- Disability. Available online: https://www.who.int/news-room/fact-sheets/detail/disability-and-health (accessed on 5 November 2024).
- Eurostat Self-Perceived Long-Standing Limitations in Usual Activities Due to Health Problem by Sex, Age, and Educational Attainment Level. Available online: https://ec.europa.eu/eurostat/databrowser/view/hlth_silc_07/default/table (accessed on 5 November 2024).
- World Health Organization (Ed.) World Report on Disability 2011; World Health Organization: Geneva, Switzerland, 2011; ISBN 978-92-4-156418-2. [Google Scholar]
- Martin Ginis, K.A.; Van Der Ploeg, H.P.; Foster, C.; Lai, B.; McBride, C.B.; Ng, K.; Pratt, M.; Shirazipour, C.H.; Smith, B.; Vásquez, P.M.; et al. Participation of People Living with Disabilities in Physical Activity: A Global Perspective. Lancet 2021, 398, 443–455. [Google Scholar] [CrossRef] [PubMed]
- Carty, C.; Van Der Ploeg, H.P.; Biddle, S.J.H.; Bull, F.; Willumsen, J.; Lee, L.; Kamenov, K.; Milton, K. The First Global Physical Activity and Sedentary Behavior Guidelines for People Living With Disability. J. Phys. Act. Health 2021, 18, 86–93. [Google Scholar] [CrossRef]
- Simón-Siles, S.; Font-Farré, M.; Guerra-Balic, M.; Nishishinya-Aquino, M.B.; Oviedo, G.R. Effects of Exercise on Fitness in Adults with Intellectual Disability: A Protocol of an Overview of Systematic Reviews. BMJ Open 2022, 12, e058053. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, K.; Scott, H.M.; Murthy, S. Associated Risk Factors for Depression and Anxiety in Adults with Intellectual and Developmental Disabilities: Five-Year Follow Up. Am. J. Intellect. Dev. Disabil. 2020, 125, 49–63. [Google Scholar] [CrossRef]
- Jacinto, M.; Oliveira, R.; Brito, J.P.; Martins, A.D.; Matos, R.; Ferreira, J.P. Prescription and Effects of Strength Training in Individuals with Intellectual Disability—A Systematic Review. Sports 2021, 9, 125. [Google Scholar] [CrossRef] [PubMed]
- Liang, Z.; Zhang, M.; Wang, C.; Yuan, Y.; Liang, J. Association between Sedentary Behavior, Physical Activity, and Cardiovascular Disease-Related Outcomes in Adults—A Meta-Analysis and Systematic Review. Front. Public Health 2022, 10, 1018460. [Google Scholar] [CrossRef]
- Muñoz, E.M.; Garrote Rojas, D.; Sánchez Romero, C. La Práctica Deportiva En Personas Con Discapacidad: Motivación Personal, Inclusión y Salud. Rev. INFAD Psicol. 2017, 4, 145. [Google Scholar] [CrossRef]
- Ascondo, J.; Martín-López, A.; Iturricastillo, A.; Granados, C.; Garate, I.; Romaratezabala, E.; Martínez-Aldama, I.; Romero, S.; Yanci, J. Analysis of the Barriers and Motives for Practicing Physical Activity and Sport for People with a Disability: Differences According to Gender and Type of Disability. Int. J. Environ. Res. Public Health 2023, 20, 1320. [Google Scholar] [CrossRef]
- Rosa Guillamón, A.; García Cantó, E.; Pérez Soto, J.J.; Rodríguez García, P.L. Estado de Peso, Condición Física y Satisfacción Con La Vida En Escolares de Educación Primaria. Estudio Piloto. MHSalud: Rev. Cienc. Mov. Hum. Salud 2016, 13, 1–15. [Google Scholar] [CrossRef]
- Boer, P.H. The Effect of 8 Weeks of Freestyle Swim Training on the Functional Fitness of Adults with Down Syndrome. J. Intellect. Disabil. Res. 2020, 64, 770–781. [Google Scholar] [CrossRef]
- Shields, N.; Bennell, K.L.; Radcliffe, J.; Taylor, N.F. Is Strength Training Feasible for Young People with Prader-Willi Syndrome? A Phase I Randomised Controlled Trial. Physiotherapy 2020, 106, 136–144. [Google Scholar] [CrossRef] [PubMed]
- Henríquez, M.; Peña-González, I.; Albaladejo-García, C.; Sadarangani, K.P.; Reina, R. Sex Differences in Change of Direction Deficit and Asymmetries in Footballers with Cerebral Palsy. Scand. Med. Sci. Sports 2023, 33, 1519–1530. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Lopez, S.; Yanci, J.; Granados, C.; Fernandez-Lasa, U.; Iturricastillo, A. Efectos de un programa de ejercicio físico multicomponente en la funcionalidad de personas con la enfermedad de Parkinson. MHSalud Rev. En Cienc. Del Mov. Hum. Y Salud 2023, 20, 63–74. [Google Scholar]
- Alcántara-Cordero, F.J.; Gómez-Píriz, P.T.; Sánchez-López, A.M.; Cabeza-Ruiz, R. Feasibility and Reliability of a Physical Fitness Tests Battery for Adults with Intellectual Disabilities: The SAMU DIS-FIT Battery. Disabil. Health J. 2020, 13, 100886. [Google Scholar] [CrossRef]
- Oppewal, A.; Hilgenkamp, T.I.M. Adding Meaning to Physical Fitness Test Results in Individuals with Intellectual Disabilities. Disabil. Rehabil. 2020, 42, 1406–1413. [Google Scholar] [CrossRef] [PubMed]
- Crotti, M.; Bosio, A.; Invernizzi, P.L. Validity and Reliability of Submaximal Fitness Tests Based on Perceptual Variables. J. Sports Med. Phys. Fit. 2018, 58, 27–53. [Google Scholar] [CrossRef]
- Cabeza-Ruiz, R.; Sánchez-López, A.M.; Trigo, M.E.; Gómez-Píriz, P.T. Feasibility and Reliability of the Assessing Levels of Physical Activity Health-related Fitness Test Battery in Adults with Intellectual Disabilities. J. Intellect. Disabil. Res. 2020, 64, 612–628. [Google Scholar] [CrossRef]
- Huang, J.; Yang, J.; Haegele, J.A.; Wang, L.; Chen, S.; Li, C. Feasibility and Reliability of Health-Related Physical Fitness Tests in Children and Adolescents with Hearing Impairment. Children 2023, 10, 353. [Google Scholar] [CrossRef] [PubMed]
- Gong, H.; Peng, Z.; Liu, Y.; Chen, Z.; Fei, S.; Xu, R.; Liu, K.; Xu, D.; Guo, Y. Fire-retardant braided electronic rope with a hierarchical core-shell structure for fire rescue operations. Compos. Part B Eng. 2023, 271, 111152. [Google Scholar] [CrossRef]
- Eek, M.N.; Augustsson, J.; Zügner, R.; Tranberg, R. Single-Leg Vertical Jumping in Young Adults with Spastic Cerebral Palsy. Gait Posture 2023, 103, 1–5. [Google Scholar] [CrossRef]
- Henríquez, M.; De Campos, L.F.C.; Muñoz-Hinrichsen, F.; Cornejo, M.I.; Yanci, J.; Reina, R. Neuromuscular Fatigue in Cerebral Palsy Football Players after a Competitive Match According to Sport Classification and Playing Position. Int. J. Environ. Res. Public Health 2022, 19, 6070. [Google Scholar] [CrossRef] [PubMed]
- González-Ravé, J.M.; Turner, A.P.; Phillips, S.M. Adaptations to Swimming Training in Athletes with Down’s Syndrome. Int. J. Environ. Res. Public Health 2020, 17, 9175. [Google Scholar] [CrossRef] [PubMed]
- Reina, R.; Iturricastillo, A.; Sabido, R.; Campayo-Piernas, M.; Yanci, J. Vertical and Horizontal Jump Capacity in International Cerebral Palsy Football Players. Int. J. Sports Physiol. Perform. 2018, 13, 597–603. [Google Scholar] [CrossRef]
- Sarabia, J.M.; Roldan, A.; Henríquez, M.; Reina, R. Using Decision Trees to Support Classifiers’ Decision-Making about Activity Limitation of Cerebral Palsy Footballers. Int. J. Environ. Res. Public Health 2021, 18, 4320. [Google Scholar] [CrossRef]
- Yanci, J.; Granados, C.; Otero, M.; Badiola, A.; Olasagasti, J.; Bidaurrazaga-Letona, I.; Iturricastillo, A.; Gil, S. Sprint, Agility, Strength and Endurance Capacity in Wheelchair Basketball Players. Biol. Sport 2014, 32, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Leon-Llamas, J.L.; Villafaina, S.; Murillo-Garcia, A.; Collado-Mateo, D.; Domínguez-Muñoz, F.J.; Sánchez-Gómez, J.; Gusi, N. Strength Assessment Under Dual Task Conditions in Women with Fibromyalgia: A Test–Retest Reliability Study. Int. J. Environ. Res. Public Health 2019, 16, 4971. [Google Scholar] [CrossRef]
- Lee, Y.-C.; Chang, S.-F.; Kao, C.-Y.; Tsai, H.C. Muscle Strength, Physical Fitness, Balance, and Walking Ability at Risk of Fall for Prefrail Older People. BioMed Res. Int. 2022, 2022, 1–12. [Google Scholar] [CrossRef]
- Luarte-Rocha, C.; Castelli Correia De Campos, L.F.; Campos Campos, K.; Alarcón Segura, K.; Henriquez, M.; Pleticosic Ramírez, Y.; Fernández Muñoz, M.; Smith, R.; Muñoz, F.; Duarte, E. Rendimiento Físico de Atletas Varones de Élite de Baloncesto En Silla de Ruedas de La Región Del Biobío-Chile En Inicio Del Período Preparatorio: Estudio Transversal (Physical Performance of Wheelchair Basketball Athletes with Paralympic Projection of Th. Retos 2022, 44, 1027–1036. [Google Scholar] [CrossRef]
- Iturricastillo, A.; Yanci, J.; Granados, C. Neuromuscular Responses and Physiological Changes During Small-Sided Games in Wheelchair Basketball. Adapt. Phys. Act. Q. 2018, 35, 20–35. [Google Scholar] [CrossRef]
- Reina, R.; Iturricastillo, A.; Castillo, D.; Urbán, T.; Yanci, J. Activity Limitation and Match Load in Para-footballers with Cerebral Palsy: An Approach for Evidence-based Classification. Scand. Med. Sci. Sports 2020, 30, 496–504. [Google Scholar] [CrossRef]
- Reina, R.; Barbado, D.; Hernández-Davó, H.; Roldan, A. Dynamic and Static Stability in Para-athletes with Cerebral Palsy Considering Their Impairment Profile. PM&R 2022, 14, 366–376. [Google Scholar] [CrossRef]
- Nasuti, G.; Stuart-Hill, L.; Temple, V.A. The Six-Minute Walk Test for Adults with Intellectual Disability: A Study of Validity and Reliability. J. Intellect. Dev. Disabil. 2013, 38, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Ayán-Pérez, C.; Martínez-Lemos, R.I.; Cancela-Carral, J.M. Reliability and Convergent Validity of the 6-Min Run Test in Young Adults with Down Syndrome. Disabil. Health J. 2017, 10, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Stuart-Hill, L.; Ryan, P.; St. John, L.; Rintala, P.; Temple, V. Heart Rate Responses during the Modified Six-Minute Walk Test among Special Olympics Athletes. Turk. J. Sports Med. 2020, 56, 56–60. [Google Scholar] [CrossRef]
- Pinedo-Jauregi, A.; Garcia-Tabar, I.; Carrier, B.; Navalta, J.W.; Cámara, J. Reliability and Validity of the Stryd Power Meter during Different Walking Conditions. Gait Posture 2022, 92, 277–283. [Google Scholar] [CrossRef]
- Foster, C.; Florhaug, J.A.; Franklin, J.; Gottschall, L.; Hrovatin, L.A.; Parker, S.; Doleshal, P.; Dodge, C. A New Approach to Monitoring Exercise Training. J. Strength Cond. Res. 2001, 15, 109–115. [Google Scholar]
- Iturricastillo Urteaga, A.; Javier, Y.; Granados, C. Rendimiento Físico, Respuestas Fisiológicas Y Percepción Subjetiva del Esfuerzo en El Multi-Stage Fitness Test en Jugadores de Baloncesto en Silla de Ruedas. Rev. Int. Deportes Colect. 2015, in press. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge: Abingdon, UK, 2013; ISBN 978-1-134-74270-7. [Google Scholar]
- Acion, L.; Peterson, J.J.; Temple, S.; Arndt, S. Probabilistic Index: An Intuitive Non-Parametric Approach to Measuring the Size of Treatment Effects. Stat. Med. 2006, 25, 591–602. [Google Scholar] [CrossRef]
- López-Martín, E.; Ardura, D. El Tamaño Del Efecto En La Publicación Científica. EducXX1 2023, 26, 9–17. [Google Scholar] [CrossRef]
- Hopkins, W.G.; Marshall, S.W.; Batterham, A.M.; Hanin, J. Progressive Statistics for Studies in Sports Medicine and Exercise Science. Med. Sci. Sports Exerc. 2009, 41, 3–12. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Martín-Díaz, P.; Carratalá-Tejada, M.; Molina-Rueda, F.; Cuesta-Gómez, A. Reliability and Agreement of the Timed up and Go Test in Children and Teenagers with Autism Spectrum Disorder. Eur. J. Pediatr. 2023, 182, 3577–3585. [Google Scholar] [CrossRef]
- Covain, S.; Baillieul, S.; Nguyen, T.D.; Guinot, M.; Doutreleau, S.; Bricout, V.-A. Gender Differences, Motor Skills and Physical Fitness Heterogeneity in Adults with Down’s Syndrome. J. Clin. Med. 2023, 12, 1367. [Google Scholar] [CrossRef]
- Katajapuu, N.; Laimi, K.; Heinonen, A.; Saltychev, M. Gender-Related Differences in Psychometric Properties of WHO Disability Assessment Schedule 2.0. Int. J. Rehabil. Res. 2019, 42, 316–321. [Google Scholar] [CrossRef]
- Úbeda-Colomer, J.; Devís-Devís, J.; Martin Ginis, K.A. Gender Differences in Theory-Based Predictors of Physical Activity in University Students with Disabilities. Rev. Latinoam. Psicol. 2020, 52, 141–148. [Google Scholar] [CrossRef]
- Wheaton, F.V.; Crimmins, E.M. Female Disability Disadvantage: A Global Perspective on Sex Differences in Physical Function and Disability. Ageing Soc. 2016, 36, 1136–1156. [Google Scholar] [CrossRef]
- Farías-Valenzuela, C.; Alarcón-López, H.; Moraga-Pantoja, M.; Troncoso-Moreno, T.; Vega-Tobar, V.; Rivadeneira-Intriago, M.; Valdivia-Moral, P. Comparación de Medidas Antropométricas de Riesgo Cardiovascular, Fuerza Isométrica Y Funcionalidad Entre Adolescentes Chilenos de Ambos Sexos Con Discapacidad Intelectual. J. Sport Health Res. 2021, 13, 75–86. [Google Scholar]
- Koster, A.; Ding, J.; Stenholm, S.; Caserotti, P.; Houston, D.K.; Nicklas, B.J.; You, T.; Lee, J.S.; Visser, M.; Newman, A.B.; et al. Does the Amount of Fat Mass Predict Age-Related Loss of Lean Mass, Muscle Strength, and Muscle Quality in Older Adults? J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2011, 66A, 888–895. [Google Scholar] [CrossRef]
- Blomqvist, S.; Wester, A.; Sundelin, G.; Rehn, B. Test–Retest Reliability, Smallest Real Difference and Concurrent Validity of Six Different Balance Tests on Young People with Mild to Moderate Intellectual Disability. Physiotherapy 2012, 98, 313–319. [Google Scholar] [CrossRef]
- Winger, M.E.; Caserotti, P.; Cauley, J.A.; Boudreau, R.M.; Piva, S.R.; Cawthon, P.M.; Harris, T.B.; Barrett-Connor, E.; Fink, H.A.; Kado, D.M.; et al. Associations between Novel Jump Test Measures, Grip Strength, and Physical Performance: The Osteoporotic Fractures in Men (MrOS) Study. Aging Clin. Exp. Res. 2020, 32, 587–595. [Google Scholar] [CrossRef]
- Bezodis, N.E.; Willwacher, S.; Salo, A.I.T. The Biomechanics of the Track and Field Sprint Start: A Narrative Review. Sports Med. 2019, 49, 1345–1364. [Google Scholar] [CrossRef]
- Maeda, A.; Yuasa, T.; Nakamura, K.; Higuchi, S.; Motohashi, Y. Physical Performance Tests After Stroke: Reliability and Validity. Am. J. Phys. Med. Rehabil. 2000, 79, 519–525. [Google Scholar] [CrossRef]
- Edgin, J.O.; Mason, G.M.; Allman, M.J.; Capone, G.T.; DeLeon, I.; Maslen, C.; Reeves, R.H.; Sherman, S.L.; Nadel, L. Development and Validation of the Arizona Cognitive Test Battery for Down Syndrome. J. Neurodev. Disord. 2010, 2, 149–164. [Google Scholar] [CrossRef]
- Gavhale, P.; Gunjal, S. Comparison of Functional Capacity among Obese and Non-Obese Young Adults. Int. J. Health Sci. Res. 2022, 12, 225–229. [Google Scholar] [CrossRef]
- Fuentes-Abolafio, I.J.; Trinidad-Fernández, M.; Ricci, M.; Roldán-Jiménez, C.; Gómez-Huelgas, R.; Arjona-Caballero, J.M.; Escriche-Escuder, A.; Bernal-López, M.R.; Pérez-Belmonte, L.M.; Cuesta-Vargas, A.I. Kinematic Parameters Related to Functional Capacity, Fatigue, and Breathlessness during the 6-Min Walk Test in Older Adults with Heart Failure with Preserved Ejection Fraction. Eur. J. Cardiovasc. Nurs. 2024, 23, 69–80. [Google Scholar] [CrossRef] [PubMed]
- Kovarik, M.; Joskova, V.; Patkova, A.; Koblizek, V.; Zadak, Z.; Hronek, M. Hand Grip Endurance Test Relates to Clinical State and Prognosis in COPD Patients Better than 6-Minute Walk Test Distance. Int. J. Chronic Obstr. Pulm. Dis. 2017, 12, 3429–3435. [Google Scholar] [CrossRef]
- Pedrosa, R.; Holanda, G. Correlação entre os testes da caminhada, marcha estacionária e TUG em hipertensas idosas. Rev. Bras. Fisioter. 2009, 13, 252–256. [Google Scholar] [CrossRef]
- Reis, J.D.P.; Martinelli Da Silva, M.; Pavesi, R.O.A.; Vidal, A.P.D.C.; Dias, F.M.V. The Reduction in Grip Strength Is Associated with a Decrease in the Distance Covered in the 6MWT in Elderly People Residing in a Long-Stay Institution. Rev. Cienc. Saude 2022, 12, 41–46. [Google Scholar] [CrossRef]
- Pavon, J.M.; Previll, L.; Woo, M.; Henao, R.; Solomon, M.; Rogers, U.; Olson, A.; Fischer, J.; Leo, C.; Fillenbaum, G.; et al. Machine learning functional impairment classification with electronic health record data. J. Am. Geriatr. Soc. 2023, 71, 2822–2833. [Google Scholar] [CrossRef]

| Best Record | R1 | R2 | CV | Student-T/Wilcoxon p Value | ES d/rb | ICC | r/Rho | ||
|---|---|---|---|---|---|---|---|---|---|
| Neuromuscular functionality | CMJ (cm) | 13.12 ± 6.52 | 12.37 ± 6.81 | 12.71 ± 6.25 | 11.59% ± 0.23% | 0.16 | −0.22 | 0.97 *** | 0.98 *** |
| CMJRight (cm) | 5.58 ± 3.71 | 4.99 ± 3.76 | 5.21 ± 3.52 | 20.27% ± 0.31% | 0.14 | −0.29 | 0.93 *** | 0.94 *** | |
| CMJLeft (cm) | 5.19 ± 3.52 | 4.70 ± 3.28 | 4.89 ± 3.30 | 10.18% ± 0.10% | 0.6 | −0.1 | 0.93 *** | 0.96 *** | |
| SBJ (cm) | 0.92 ± 0.41 | 0.89 ± 0.39 | 0.87 ± 0.39 | 11.36% ± 0.19% | 0.46 | 0.11 | 0.92 *** | 0.92 *** | |
| HGRight (kg) | 29.57 ± 9.62 | 26.97 ± 8.20 | 29.63 ± 9.44 | 6.46% ± 0.04% | <0.001 *** | −0.58 | 0.91 *** | 0.97 *** | |
| HGLeft (kg) | 27.61 ± 8.66 | 26.14 ± 8.44 | 27.27 ± 8.35 | 4.79% ± 0.04% | <0.001 *** | −0.85 | 0.96 *** | 0.97 *** | |
| Functionality in combined actions | TUG (s) | 5.15 ± 1.51 | 5.65 ± 2.02 | 5.34 ± 2.04 | 6.87% ± 0.07% | <0.001 *** | 0.65 | 0.81 *** | 0.96 *** |
| 30CTS (n°) | 14.79 ± 4.08 | 13.76 ± 4.15 | 14.39 ± 3.66 | 7.20% ± 0.07% | <0.001 *** | 0.7 | 0.83 *** | 0.93 *** | |
| Functionality in acceleration | 0–10 m (s) | 3.59 ± 1.62 | 3.79 ± 1.83 | 3.63 ± 1.64 | 4.61% ± 0.05% | 0.01 ** | 0.49 | 0.96 *** | 0.95 *** |
| 0–20 m (s) | 6.94 ± 3.43 | 7.30 ± 3.68 | 7.00 ± 3.49 | 3.66% ± 0.03% | <0.001 *** | 0.6 | 0.98 *** | 0.99 *** | |
| 10–20 m (s) | 3.33 ± 1.81 | 3.51 ± 1.88 | 3.36 ± 1.86 | 4.67% ± 0.05% | <0.001 *** | 0.57 | 0.98 *** | 0.98 *** | |
| COD505 (s) | 4.43 ± 1.41 | 4.68 ± 1.68 | 4.62 ± 1.67 | 5.37% ± 0.06% | 0.04 * | 0.36 | 0.90 *** | 0.91 *** | |
| Functionality in balance | OLSRight (s) | 15.52 ± 6.70 | 13.06 ± 7.60 | 14.81 ± 7.26 | 23.28% ± 0.33% | 0.05 * | −0.63 | 0.71 *** | 0.73 *** |
| OLSLeft (s) | 15.95 ± 6.42 | 12.96 ± 7.21 | 15.48 ± 6.96 | 23.27% ± 0.32% | 0.01 ** | −0.46 | 0.65 *** | 0.67 *** | |
| Cardiovascular functionality | Dist. (m) | 564.91 ± 101.64 | |||||||
| HRmax (pp/m) | 137.55 ± 24.68 | ||||||||
| HRavg (pp/m) | 123.76 ± 24.68 | ||||||||
| RPEmus | 3.46 ± 2.10 | ||||||||
| RPEres | 3.00 ± 1.41 | ||||||||
| Ttimp (C°) | 36.26 ± 0.63 | ||||||||
| Pmaxrel (W/kg) | 2.12 ± 0.85 | ||||||||
| Pminrel (W/kg) | 1.33 ± 0.57 | ||||||||
| Pavgrel (W/kg) | 1.80 ± 0.74 | ||||||||
| Pmaxabs (W) | 147.07 ± 37.88 | ||||||||
| Pminabs (W) | 92.44 ± 29.94 | ||||||||
| Pavgabs (W) | 123.90 ± 32.29 | ||||||||
| Cadence (p/min) | 131.77 ± 13.40 | ||||||||
| Stride length (m) | 0.73 ± 0.10 | ||||||||
| Pace (min:s/km) | 10:55 ± 3:01 | ||||||||
| GCT (ms) | 708.67 ± 308.61 | ||||||||
| Dist.Stryd (m) | 592.163 ± 102.64 |
| Men | Women | CV | Student-T/U-Mann p Value | ES d/PS | ||
|---|---|---|---|---|---|---|
| Neuromuscular functionality | CMJ (cm) | 16.22 ± 8.02 | 12.06 ± 5.67 | 20.77% | 0.07 | 0.66 |
| CMJRight (cm) | 6.76 ± 4.36 | 5.18 ± 3.44 | 18.65% | 0.23 | 0.43 | |
| CMJLeft (cm) | 7.12 ± 3.80 | 4.53 ± 3.21 | 31.43% | 0.03 * | 0.77 | |
| SBJ (cm) | 106.78 ± 51.03 | 86.62 ± 36.11 | 14.74% | 0.16 | 0.50 | |
| HGRight (kg) | 41.56 ± 8.91 | 25.45 ± 5.59 | 34.37% | <0.001 *** | 0.09 | |
| HGLeft (kg) | 38.94 ± 8.49 | 23.71 ± 4.12 | 34.01% | <0.001 *** | 0.09 | |
| Functionality in combined actions | TUG (s) | 5.11 ± 1.32 | 5.17 ± 1.58 | 0.81% | 0.80 | 0.47 |
| 30CTS (n°) | 15.09 ± 5.28 | 14.69 ± 3.67 | 1.92% | 0.78 | 0.10 | |
| Functionality in acceleration | 0–10 m (s) | 3.21 ± 1.12 | 3.72 ± 1.75 | 10.51% | 0.31 | 0.39 |
| 0–20 m (s) | 6.06 ± 2.41 | 7.25 ± 3.70 | 12.57% | 0.30 | 0.39 | |
| 10–20 m (s) | 2.85 ± 1.30 | 3.50 ± 1.94 | 14.35% | 0.30 | 0.39 | |
| COD505 (s) | 4.14 ± 1.10 | 4.53 ± 1.50 | 6.48% | 0.42 | 0.42 | |
| Functionality in balance | OLSRight (s) | 11.22 ± 7.21 | 17.00 ± 5.94 | 28.96% | <0.01 ** | 0.26 |
| OLSLeft (s) | 13.58 ± 8.26 | 16.76 ± 5.58 | 14.82% | 0.20 | 0.39 | |
| Cardiovascular functionality | Dist. (m) | 563.43 ± 111.08 | 565.42 ± 100.08 | 0.25% | 0.78 | 0.47 |
| HRmax (pp/m) | 124.36 ± 26.84 | 142.09 ± 22.58 | 9.41% | 0.04 * | 0.75 | |
| HRavg (pp/m) | 111.54 ± 26.74 | 127.96 ± 20.23 | 9.70% | 0.04 * | 0.75 | |
| RPEmus | 4.27 ± 2.49 | 3.19 ± 1.92 | 20.57% | 0.12 | 0.68 | |
| RPEres | 2.64 ± 1.28 | 3.12 ± 1.45 | 11.99% | 0.35 | 0.41 | |
| Ttimp (C°) | 36.20 ± 0.71 | 36.28 ± 0.61 | 0.14% | 0.71 | 0.56 | |
| Pmaxrel (W/kg) | 1.67 ± 0.48 | 2.28 ± 0.89 | 21.87% | 0.08 | 0.32 | |
| Pminrel (W/kg) | 0.82 ± 0.23 | 1.50 ± 0.55 | 41.67% | <0.001 *** | 1.39 | |
| Pavgrel (W/kg) | 1.32 ± 0.38 | 1.96 ± 0.76 | 27.73% | 0.01 ** | 0.01 | |
| Pmaxabs (W) | 141.51 ± 32.19 | 148.99 ± 39.94 | 3.64% | 0.58 | 0.20 | |
| Pminabs (W) | 70.71 ± 18.93 | 99.92 ± 29.56 | 24.21% | <0.01 ** | 1.07 | |
| Pavgabs (W) | 111.62 ± 25.45 | 128.12 ± 33.64 | 9.73% | 0.15 | 0.52 | |
| Cadence (p/min) | 127.73 ± 12.35 | 133.16 ± 13.66 | 2.94% | 0.18 | 0.41 | |
| Stride length (m) | 0.78 ± 0.11 | 0.72 ± 0.08 | 8.44% | 0.06 | 0.58 | |
| Pace (min:s/km) | 10:18 ± 1:50 | 11:08 ± 3:20 | 5.44% | 0.94 | 0.49 | |
| GCT (ms) | 793.83 ± 293.36 | 679.40 ± 312.76 | 10.98% | 0.26 | 0.61 | |
| Dist.Stryd (m) | 604.22 ± 106.07 | 588.01 ± 102.83 | 1.98% | 1.00 | 0.50 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ascondo, J.; Llodio, I.; Marcos-Rivero, B.; Granados, C.; Romero, S.; Iturricastillo, A.; Yanci, J. Proposal for a Battery to Evaluate Functional Capacity in Older Adults with Disabilities. Sensors 2025, 25, 1813. https://doi.org/10.3390/s25061813
Ascondo J, Llodio I, Marcos-Rivero B, Granados C, Romero S, Iturricastillo A, Yanci J. Proposal for a Battery to Evaluate Functional Capacity in Older Adults with Disabilities. Sensors. 2025; 25(6):1813. https://doi.org/10.3390/s25061813
Chicago/Turabian StyleAscondo, Josu, Iñaki Llodio, Bingen Marcos-Rivero, Cristina Granados, Sheila Romero, Aitor Iturricastillo, and Javier Yanci. 2025. "Proposal for a Battery to Evaluate Functional Capacity in Older Adults with Disabilities" Sensors 25, no. 6: 1813. https://doi.org/10.3390/s25061813
APA StyleAscondo, J., Llodio, I., Marcos-Rivero, B., Granados, C., Romero, S., Iturricastillo, A., & Yanci, J. (2025). Proposal for a Battery to Evaluate Functional Capacity in Older Adults with Disabilities. Sensors, 25(6), 1813. https://doi.org/10.3390/s25061813









