Enhancing Connected Health Ecosystems Through IoT-Enabled Monitoring Technologies: A Case Study of the Monit4Healthy System
Abstract
1. Introduction
2. Literature Review
2.1. IoT Technologies in Health Monitoring
2.1.1. Key Advancements and Applications of IoT in Healthcare
2.1.2. Relevance to Connected Ecosystems
2.2. Challenges in IoT-Based Health Monitoring
- Data accuracy and reliability: ensuring that IoT devices provide accurate and consistent health data for effective decision making;
- Data security and privacy: strong data encryption, authentication mechanisms, secure transmission in IoT health applications, and compliance with healthcare regulations like GDPR (EU) and HIPAA (USA) are required to protect sensitive patient information;
- Infrastructure and connectivity: reliable internet connections (such as Wi-Fi and 5G) and sufficient network capacity are essential for real-time data transmission;
- Energy efficiency: continuous data transmission in wearable devices must be optimized for low power consumption to extend battery life;
- AI and machine learning integration: implementing real-time anomaly detection and predictive analytics necessitates powerful computers and optimized software;
- Interoperability and scalability: the adoption of interoperability frameworks (such as FHIR) is necessary to ensure the seamless integration of various IoT devices and healthcare systems;
- Ethical considerations: addressing issues with patient autonomy, consent, and data ownership is critical for responsible IoT implementation in healthcare;
- Cost and accessibility: removing financial obstacles for smaller healthcare providers and guaranteeing fair access to IoT-enabled healthcare, especially in low-income or vulnerable regions, are important for avoiding a digital divide.
2.3. Communication Technologies for IoT Healthcare
2.3.1. Latency and Bandwidth Challenges
- Wi-Fi’s fast transmission rates make it ideal for sending massive amounts of medical data, including continuous vital sign monitoring or high-resolution imaging. It can be used for high-bandwidth medical image transfers and real-time video consultations, but its high-power consumption limits it from being used in battery-operated devices [37].
- BLE is intended for low-power consumption, making it perfect for wearable health devices and short-range communication between medical sensors and smartphones, yet its short range prevents widespread coverage in hospital settings or remote monitoring scenarios [38].
- LoRaWAN offers long-range connectivity with low power consumption, which makes it ideal for asset tracking in hospitals and rural healthcare applications for sending small health-related data packets over long distances. However, because of its low data rate, LoRaWAN is not appropriate for sending high-resolution medical data [39].
2.3.2. Energy Constraints and the Need for Low-Power IoT Communication
2.3.3. Advances in Low-Power Communication Protocols
2.3.4. Energy Harvesting Techniques
2.3.5. Cloud vs. Edge Computing in Healthcare IoT
2.4. Sensor Fusion and Data Processing in IoT Health Systems
2.4.1. Importance of Sensor Fusion for Accurate Health Monitoring
2.4.2. AI and Machine Learning for Predictive Analytics
2.4.3. Emerging Trends in Multi-Sensor Data Processing
3. Materials and Methods
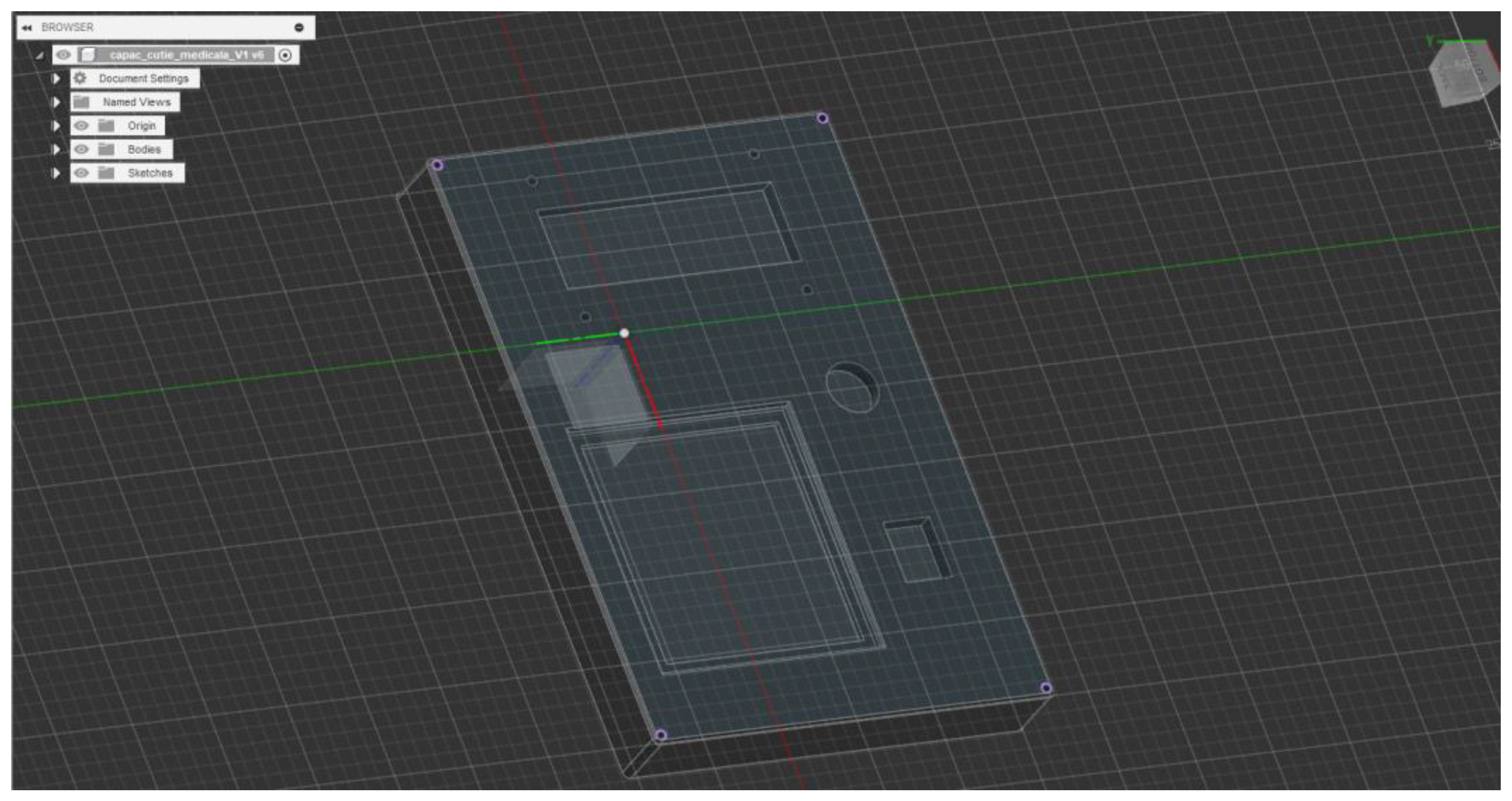
3.1. Monit4Healthy System Architecture and Design
- Data Layer: This layer involves the real-time collection of physiological and environmental data using advanced biomedical sensors integrated into multiple monitoring devices.
- Communication Layer: This layer facilitates efficient and secure data transmission. Wearable devices rely on BLE for short-range communication, while high-bandwidth data transfers occur via Wi-Fi to ensure seamless connectivity with cloud-based storage and processing systems.
- Edge Processing Layer: This layer is responsible for local data processing and initial analysis before transmitting physiological and biomechanical data to the cloud. This layer operates on a Raspberry Pi, which processes raw sensor signals from the Medical Blackbox, AcU Blackbox, EMG Blackbox, and Gaitband IoT-based devices (designed and developed for the Monit4Healthy system). Compared to a cloud-only setup, this approach improves latency, minimizes bandwidth usage by preprocessing data locally, and ensures real-time responsiveness. The implementation of edge computing in IoT systems introduces several significant advantages: (1) reduced latency, by processing data directly at the edge nodes, ensuring fast response times essential for real-time healthcare monitoring; (2) bandwidth efficiency, as only relevant, processed data are transmitted to cloud servers, reducing network congestion; (3) system autonomy and fault tolerance, allowing continued local operation even when cloud services are temporarily unavailable; and (4) enhanced privacy and security, as sensitive patient data are filtered and processed locally, limiting external exposure and improving compliance with data protection standards. Figure 1 highlights the data flow between edge and cloud layers [56].
- Processing and Cloud Layer and Application Sublayer: The Processing and Cloud Layer is responsible for data storage, structured representation, and alerting mechanisms. This layer aggregates sensor data transmitted from the Edge Processing Layer, organizing them for structured analysis and long-term storage. It includes interactive data processing tools, enabling customizable health metric representations and structured reports. A cloud-based alert and notification system operates within this layer, continuously analyzing incoming physiological and biomechanical data. It detects deviations from predefined health thresholds and triggers automated alerts through multi-channel notifications. Secure storage mechanisms are integrated to ensure data encryption, controlled access, and regulatory compliance for sensitive health information. The Application Sublayer acts as the central processing interface for managing sensor data, health alerts, and system configurations. This layer facilitates remote monitoring functionalities, allowing healthcare providers to manage real-time and historical patient data. It is responsible for user authentication, system configuration, and data synchronization across cloud servers and edge devices. It also handles communication between medical professionals and patients, ensuring the seamless integration of monitoring data with personalized medical recommendations.
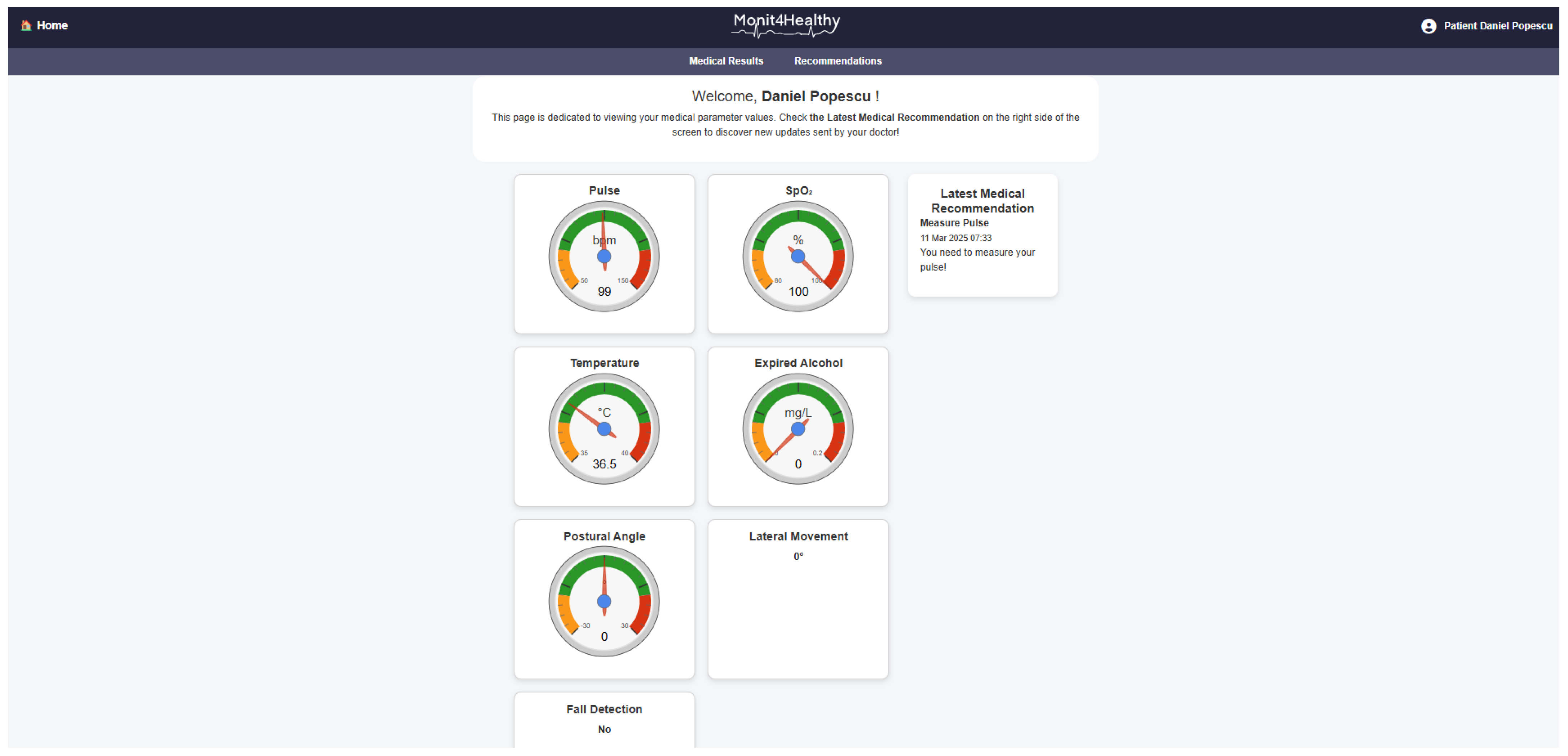
- Visualization Layer: This layer focuses on presenting real-time health insights in a user-friendly format. It provides interactive interfaces for different stakeholders, including patients, clinicians, and researchers, ensuring efficient access to health data. Features include dynamic dashboards, trend graphs, and anomaly detection alerts, ensuring that medical professionals and patients receive timely information.
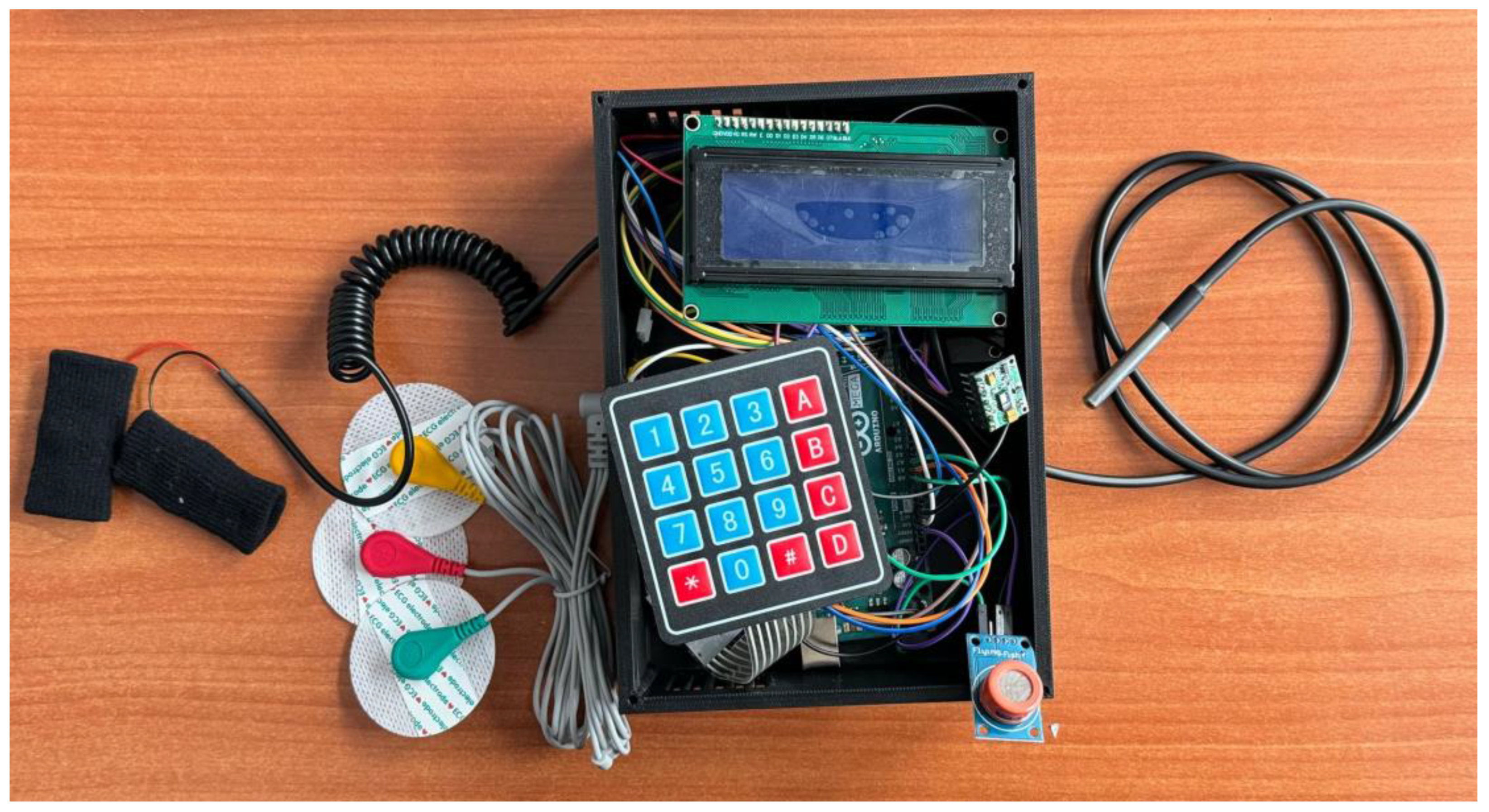
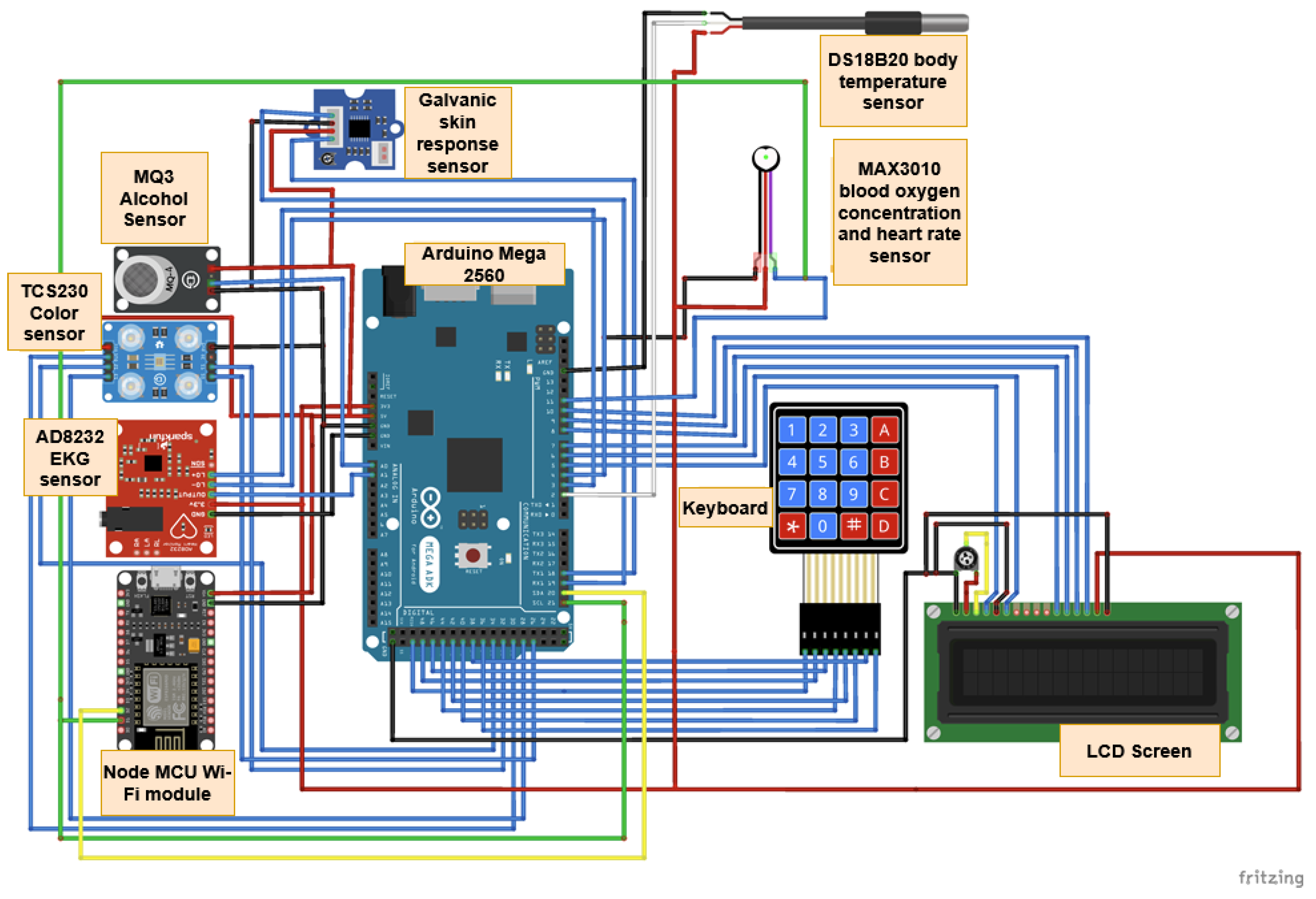
- Medical Blackbox: A multifunctional enclosure that integrates various medical-grade sensors, designed to facilitate efficient data acquisition and processing. It captures and analyzes vital parameters such as heart rate, SpO2, carbon dioxide levels, and GSR. This device integrates high-precision sensors for real-time physiological assessment, ensuring the accurate detection of health anomalies.
- Gaitband: A wearable device designed for real-time gait pattern monitoring, optimized for ergonomic comfort and sensor placement stability. Equipped with an LSM303DLHC magnetometer and accelerometer, the Gaitband continuously monitors gait patterns, posture stability, and movement dynamics. The SAM-M8Q GPS (Global Positioning System) module enhances location tracking and movement analysis, while the HM-10 Bluetooth module and ESP8266 (NodeMCU) facilitate secure wireless data transmission. By analyzing motion data, the device detects irregular walking patterns, potential fall risks, and neuromuscular impairments, providing valuable insights for mobility assessment and rehabilitation.
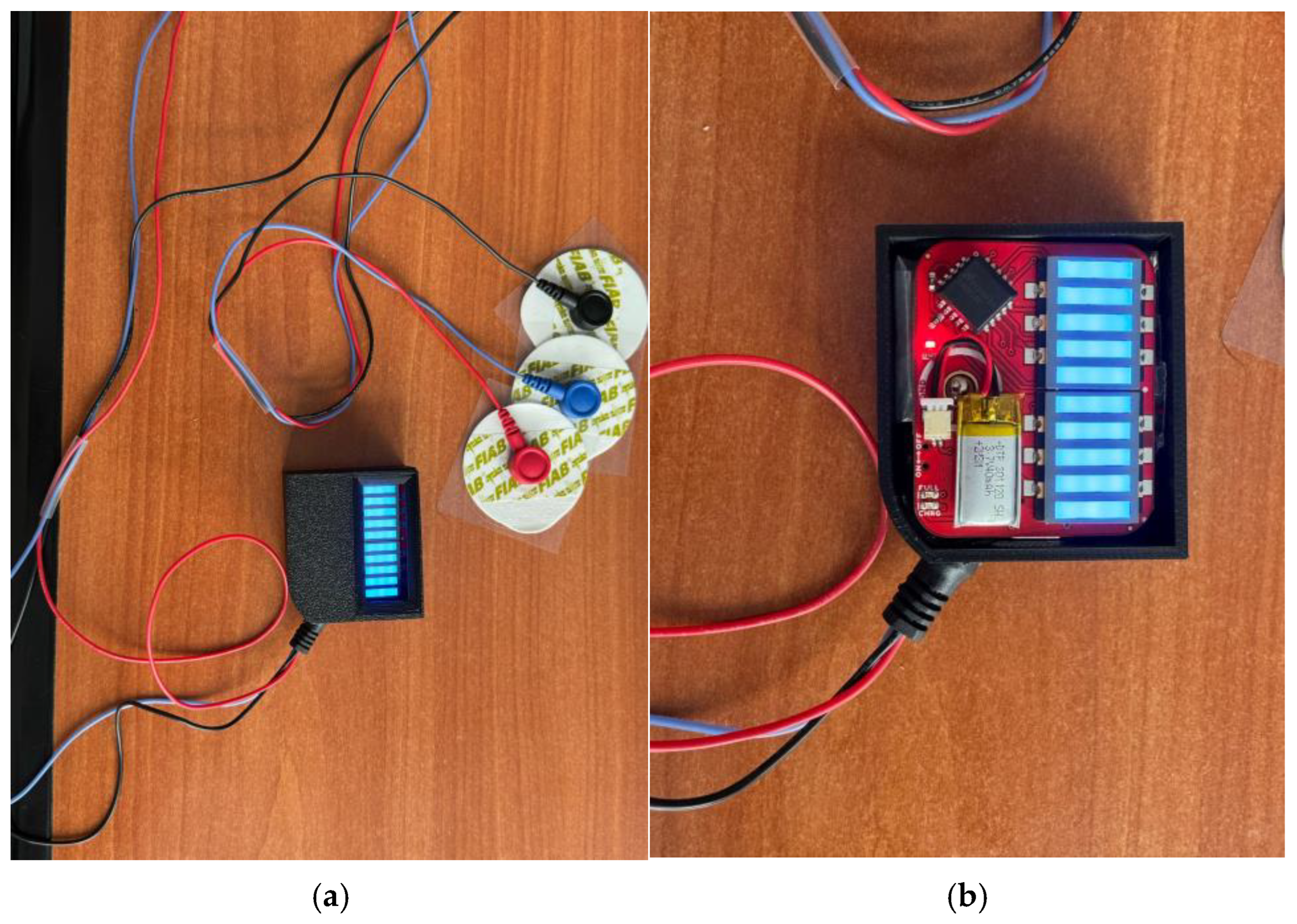
- EMG Blackbox: A specialized enclosure engineered for housing the EMG sensor array, ensuring both signal integrity and protection from external interference. Utilizes surface electromyography (sEMG) sensors for neuromuscular function assessment, measuring electrical muscle activity to monitor conditions such as muscle fatigue and neurodegenerative disorders.
- AcU Blackbox: A device that employs advanced optical spectrometry techniques for non-invasive uric acid monitoring in urine samples. The device provides real-time biochemical analysis, enabling the early detection of metabolic imbalances.
- Patient personal data: Based on personal medical history and previous measured parameters and information from the Monit4Healthy database, clinicians can issue personalized medical recommendations to the patients under their care, in order to communicate clinical or lifestyle actions that the patient should follow. Each recommendation comprises several attributes, such as the title, an optional reference to the medical device that the patient might use in order to complete the action, and the medical recommendation from the physician. The title serves as a brief summary of the action, while the description offers details and guidance for the patient. The medical device is optional, mentioned if the patient needs to use it in order to collect data for ongoing assessment or monitoring, e.g., the Gaitband, for movement analysis. It is a means of communication between clinicians and patients, allowing physicians to remind patients of the necessary clinical or lifestyle actions they should undertake to improve their health. These actions may include tasks such as performing daily exercise, using a medical device to acquire specific data, or scheduling appointments with medical specialists. Each medical recommendation is uniquely associated with the medical professional and their assigned patient, and it is time-stamped and can be easily tracked. The recommendation’s title, associated device, and description are all stored with structured data fields to allow easy retrieval and management.
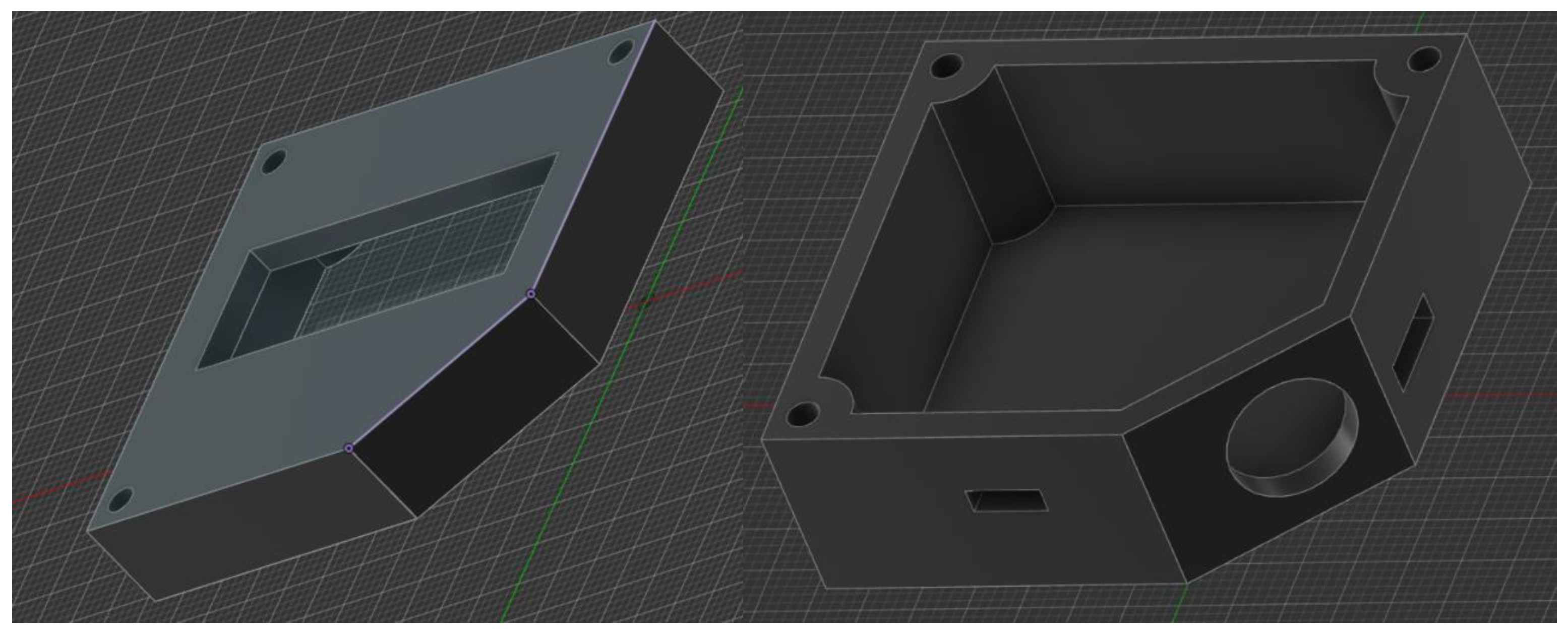
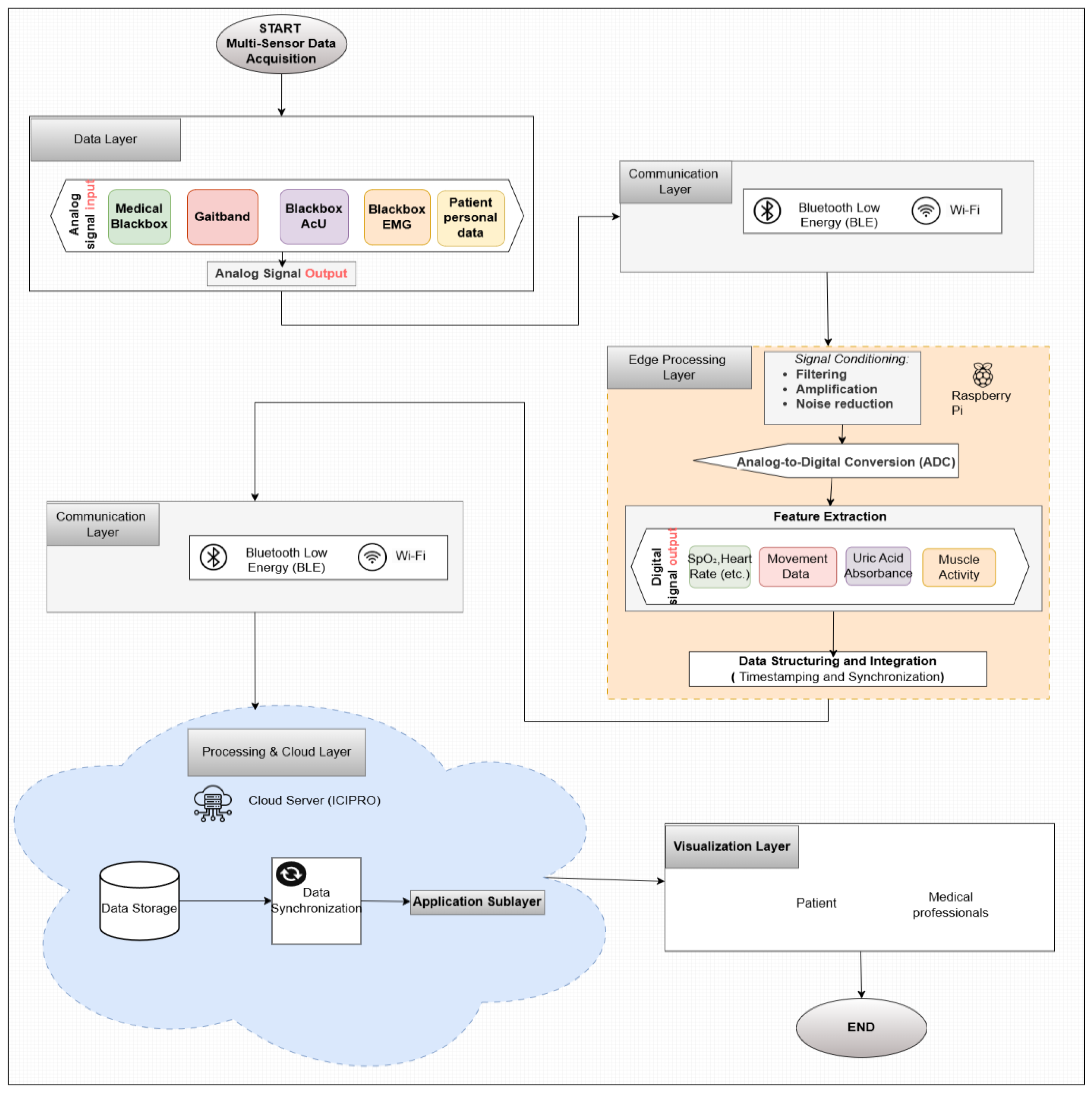
3.2. Blackbox Devices’ Concept and Development
- Corner mounting holes for secure fastening.
- Side cutout ventilation and USB-C connectivity.
- A circular opening on the angled face, for sensor integration.
- Geometric features: Rectangular base with an inclined edge for structural compatibility; the chamfered surface enhances ergonomics and esthetics.
- Mounting points: Four precisely positioned screw holes ensure secure fastening and stability.
- Recessed cavity: Central section accommodates a display, sensor, or functional interface.
- Manufacturing considerations: Optimized for 3D printing, balancing material efficiency and structural integrity.
- Structural optimization: Rigid, lightweight construction ensuring mechanical protection and spatial efficiency.
- Ventilation system: Engineered side slots for effective heat dissipation and sensor accuracy.
- Custom interface openings: Strategically placed cutouts for sensors, power, and data ports, minimizing interference.
- Fastening and accessibility: Predefined mounting holes and alignment guides facilitate secure assembly and maintenance.
- Manufacturing readiness: Optimized for 3D printing, ensuring precision, repeatability, and material efficiency.
- Dimensional accuracy: Defined length/width parameters for precise fit and structural integrity.
- Feature placement: Central cutout for connectors, sensors, or ventilation.
- Alignment and constraints: Geometric symmetry ensures parametric adaptability.
- Manufacturing preparation: Sketch optimized for extrusion, fileting, and fastening integration.
- Component-specific cutouts: Geometrically optimized openings for sensor exposure, display integration, and thermal dissipation.
- Precision fastening: Predefined corner mounting holes ensure secure, vibration-resistant attachment while maintaining accessibility.
- Multi-plane design: Slanted and recessed surfaces enhance ergonomics, esthetics, and mechanical robustness.
- Manufacturing and assembly readiness: Optimized for additive/subtractive manufacturing, ensuring tight tolerance and reliable interlocking with system components.
- Data Layer—Multi-Sensor Data Acquisition: The process starts with the Data Layer, where physiological signals are continuously collected by various sensors integrated within the Monit4Healthy system. The key sensors involved in data acquisition include the Medical Blackbox, Gaitband, Blackbox AcU, and EMG Blackbox.
- Communication Layer—Data Transmission: Once the data are collected by the sensors, they are transmitted through two communication channels:
- ○
- BLE, used for short-range communication, ideal for wearable or portable sensors that require low-power consumption.
- ○
- Wi-Fi, used for higher-bandwidth, long-range data transmission, enabling the system to send large datasets such as high-resolution ECG and other complex signals to the cloud for further processing.
- Edge Processing Layer—Initial Signal Processing: After the data are transmitted, they enter the Edge Processing Layer. Here, the raw signals undergo initial processing, including the following:
- ○
- Signal Conditioning: The filtering and amplification of the data to remove noise and enhance signal quality.
- ○
- Feature Extraction: Relevant features such as heart rate from ECG and PPG signals, muscle activity from EMG, and skin conductance levels from GSR are extracted for further analysis.
- ○
- Analog-to-Digital Conversion: The analog signals from the sensors are converted to digital format to facilitate further computational processing.
A Raspberry Pi or similar edge computing devices are used in this layer to perform the initial processing, reducing the amount of raw data sent to the cloud and ensuring that only essential information is transmitted, thus minimizing bandwidth usage and latency. - Data Structuring and Integration: Once the feature extraction is performed, the processed data are structured and integrated for synchronization across multiple sensors. This step ensures that the data from all sensors are aligned in time by applying timestamps, facilitating multi-sensor data fusion and providing a more comprehensive evaluation of physiological conditions. The integration of data from various sensors such as ECG, EMG, and GSR enhances the system’s ability to detect abnormalities and generate alerts when necessary.
- Data Transmission to the Cloud: After data fusion, the structured data are transmitted using the communication protocols (BLE or Wi-Fi) to the cloud server (ICIPRO). This enables the following:
- ○
- Data Storage: The cloud serves as the repository for the processed data, ensuring they are stored securely and accessible for further analysis.
- ○
- Data Synchronization: The real-time synchronization of the patient’s health data across devices and systems allows healthcare professionals to access the most up-to-date information at any time.
- Application Sublayer—Real-Time Monitoring and Alerts: At this stage, the structured and synchronized data are accessible via an Application Sublayer, where healthcare professionals and patients can view the data in real time through interactive dashboards. These dashboards provide visualizations such as the following:
- ○
- Trend graphs showing the patient’s health metrics over time.
- ○
- Alerts generated when the data deviate from predefined thresholds, indicating potential health risks. This allows for timely interventions, as healthcare providers can receive immediate alerts if a patient’s vital signs indicate a need for attention.
- Visualization Layer—Health Data Visualization: Finally, the processed data are displayed in the Visualization Layer, providing clear and easy-to-interpret health metrics for both patients and medical professionals. This layer facilitates the following:
- ○
- The real-time visualization of key health parameters such as heart rate, SpO2, gait patterns, and muscle activity.
- ○
- Alert notifications that inform healthcare providers about critical changes in the patient’s condition.
- ○
- Access to multiple functionalities that provide real-time, updated data and information related to the patient’s profile, based on the information stored in the system’s database. These functionalities are considered and utilized as part of a personalized, proactive, and preventive health management support system for the patient.
- Bluetooth Module for Real-Time Data Transmission: The Bluetooth module facilitates real-time data transmission, ensuring reliable connectivity. This feature is essential for applications requiring continuous data flow, such as telemetry and remote patient monitoring. Advanced BLE technology ensures low power consumption and reduced latency, making it suitable for wearable health applications. It employs adaptive frequency hopping (AFH) to minimize interference and optimize bandwidth utilization. BLE and Wi-Fi are widely adopted wireless communication technologies for data transmission, each optimized for different application scenarios. BLE is designed for low-power, short-range communication, making it ideal for battery-operated devices such as wearable sensors and IoT nodes. In contrast, Wi-Fi provides higher data throughput and extended coverage, supporting applications that require continuous, high-bandwidth connectivity. Compared to other protocols such as Zigbee and LoRaWan, BLE offers higher data rates but at the cost of a reduced range, while Wi-Fi consumes significantly more power but ensures robust data transmission over greater distances. Although this work does not explicitly analyze the trade-offs in terms of power efficiency, range, and data throughput, it focuses on leveraging both BLE and Wi-Fi to optimize data transmission for specific use cases. BLE has significantly advanced from BLE4 to BLE5, delivering notable enhancements in communication reliability, the data transfer rate, and network scalability—essential elements for contemporary IoT and sensor network applications. Both BLE4 and BLE5 are designed primarily for low-power use—an important feature for battery-powered IoT devices and sensor networks. BLE4, launched with Bluetooth 4.0, utilizes a frequency-hopping spread spectrum technique within the 2.4 GHz ISM band to reach data rates of up to 1 Mbps, featuring a design tailored for energy efficiency and low-power functionality via simplified connection and advertising protocols. Conversely, BLE5 brings substantial improvements, including the adoption of a coded physical layer that boosts range and reliability in environments with high interference, along with a doubling of the nominal data rate to 2 Mbps. BLE5 increases the advertising capability by allowing larger payloads, which enhances detailed device discovery and connectionless communications. These technological advancements not only boost overall network efficiency but also allow for the incorporation of diverse sensors—like GPS units, EMG devices, and environmental sensors such as the DS18B20 and MAX30100—into more intricate and resilient monitoring frameworks. Both BLE and Wi-Fi are prone to interference in high-density environments. This is due to the shared spectrum in the 2.4 GHz ISM band, as well as due to the overlapping channels. To avoid congested channels, BLE utilizes adaptive frequency hopping (AFH). However, AFH’s effectiveness may diminish in dense environments, therefore leading to packet loss and reduced reliability. Wi-Fi networks experience co-channel interference when multiple access points operate on the same or adjacent channels, leading to slower data rates and increased latency, particularly in areas with many overlapping access points [59].
- GPS Module: The GPS module integrates a chip antenna and Qwiic cable connection, ensuring efficient hardware integration. It significantly reduces power consumption while enhancing performance and accuracy. The ability to receive signals from up to four Global Navigation Satellite System constellations simultaneously improves positional accuracy, particularly in environments with limited sky visibility, such as urban canyons or dense foliage. Additionally, Assisted-GPS technology is used to reduce the time-to-first-fix, ensuring faster positioning data. A differential GPS can also be employed to enhance precision, reducing errors to sub-meter accuracy. Based on the u-blox MAX-M10 GNSS platform, the GPS module used in the Monit4Healthy system supports simultaneous reception from up to four GNSS constellations (GPS, Galileo, GLONASS, and BeiDou), improving positioning accuracy and signal availability even in difficult-to-reach places like urban canyons. For power-optimized performance, it makes use of the u-blox Super-E technology, which uses as low as 25 mW while in continuous tracking mode. The Qwiic interface facilitates communication over I2C, allowing for effective data transmission with low latency and simplified wiring. In order to improve energy consumption in wearable health monitoring applications, the module incorporates automated low-power modes, such as power save and periodic tracking, and enables an Assisted Global Navigation Satellite System for an expedited time-to-first-fix. It has anti-jamming and anti-spoofing characteristics, which are essential for preserving data integrity in linked health ecosystems, and enables satellite-based augmentation systems for improved location precision. The MAX-M10 GPS module is a dependable and energy-efficient option for real-time geolocation in the Monit4Healthy system because of these features [60].
- EMG Sensor (Myoware Sparkfun) for Muscle Signal Analysis: This sensor measures EMG signals from muscle activity and features an integrated amplifier with an adjustable gain of up to 1000x. It includes a high-pass filter (0.5 Hz) to eliminate direct current offset and a low-pass filter (125 Hz) to reduce high-frequency noise. The sensor uses three disposable gel electrodes and outputs both raw and envelope signals, making it suitable for applications such as robotics and prosthetics. Signal conditioning is performed to reduce motion artifacts and interference from ambient electrical sources. A notch filter (50/60 Hz) is applied to mitigate power line interference. The Monit4Healthy system’s integrated EMG module uses a multi-stage analog signal conditioning architecture to record and process surface electromyography data with high fidelity. In order to separate the physiological EMG frequencies while reducing low-frequency motion artifacts and high-frequency noise, the signal collection chain starts with an instrumentation amplifier set up for an initial gain of 200× and operating within a passband of 20 Hz to 498 Hz. Signal scaling according to electrode location and specific muscle activation levels is made possible through the following gain stage, which may be adjusted between 1× and 100×. A 3.6 Hz high-pass filter is incorporated into the module to remove DC offset, guaranteeing baseline stability and reducing signal drift over time. After amplification, the signal passes through an envelope detection stage and a full-wave rectification circuit, enabling the recording of both rectified and envelope outputs. A high-resolution analog-to-digital converter digitizes these analog outputs, guaranteeing precise EMG signal sampling for edge processing. In the Monit4Healthy Edge Processing Layer, adaptive feature extraction and threshold-based event detection are made possible through the architecture’s support for the real-time monitoring of both raw and processed EMG data. With a low power consumption appropriate for wearable usage, its modular and adjustable architecture enables the EMG module to be tailored for a variety of health monitoring applications, such as neuromuscular evaluations and rehabilitation situations [61].
- DS18B20 Digital Temperature Sensor: The DS18B20 temperature sensor operates using a 1-wire interface, allowing multiple sensors to share a single data line. It provides accurate temperature readings with a configurable resolution (9–12 bits) and digital transmission to minimize errors compared to analog sensors, making it ideal for biomedical and environmental applications. The sensor includes an integrated temperature compensation feature, ensuring stable readings even under varying environmental conditions. It supports cyclic redundancy check for error detection, enhancing data integrity. The DS18B20 sensor was chosen for its networking advantages, using a 1-wire interface that allows multiple sensors to share a single data line, simplifying wiring in large networks. Data from the sensors were collected with a microcontroller and transmitted via a wireless connection to a cloud platform. The digital transmission of data reduces errors compared to analog sensors, providing accurate and reliable measurements over time [62].
- MAX30100/MAX30102: Pulse Oximetry and Heart Rate Sensors utilize photoplethysmography (PPG) to measure blood SpO2 and heart rate. In our project, the integration of the MAX30102 biosensor with the ESP32 microcontroller utilizes the Inter-Integrated Circuit (I2C) protocol to facilitate seamless data transfer, which is essential for monitoring key health parameters such as heart rate and SpO2 [63]. The sensor includes infrared and red light emitters for dual-wavelength analysis, improving accuracy by compensating for motion artifacts. An integrated ambient light cancelation system enhances signal clarity. The MAX30100 sensor measures PPG signals to determine the SpO2 levels and heart rate. Data are then sent wirelessly (via Bluetooth or Wi-Fi) to cloud storage, enabling real-time remote monitoring. This setup allows healthcare professionals to access patient data remotely and make timely interventions if necessary [64].
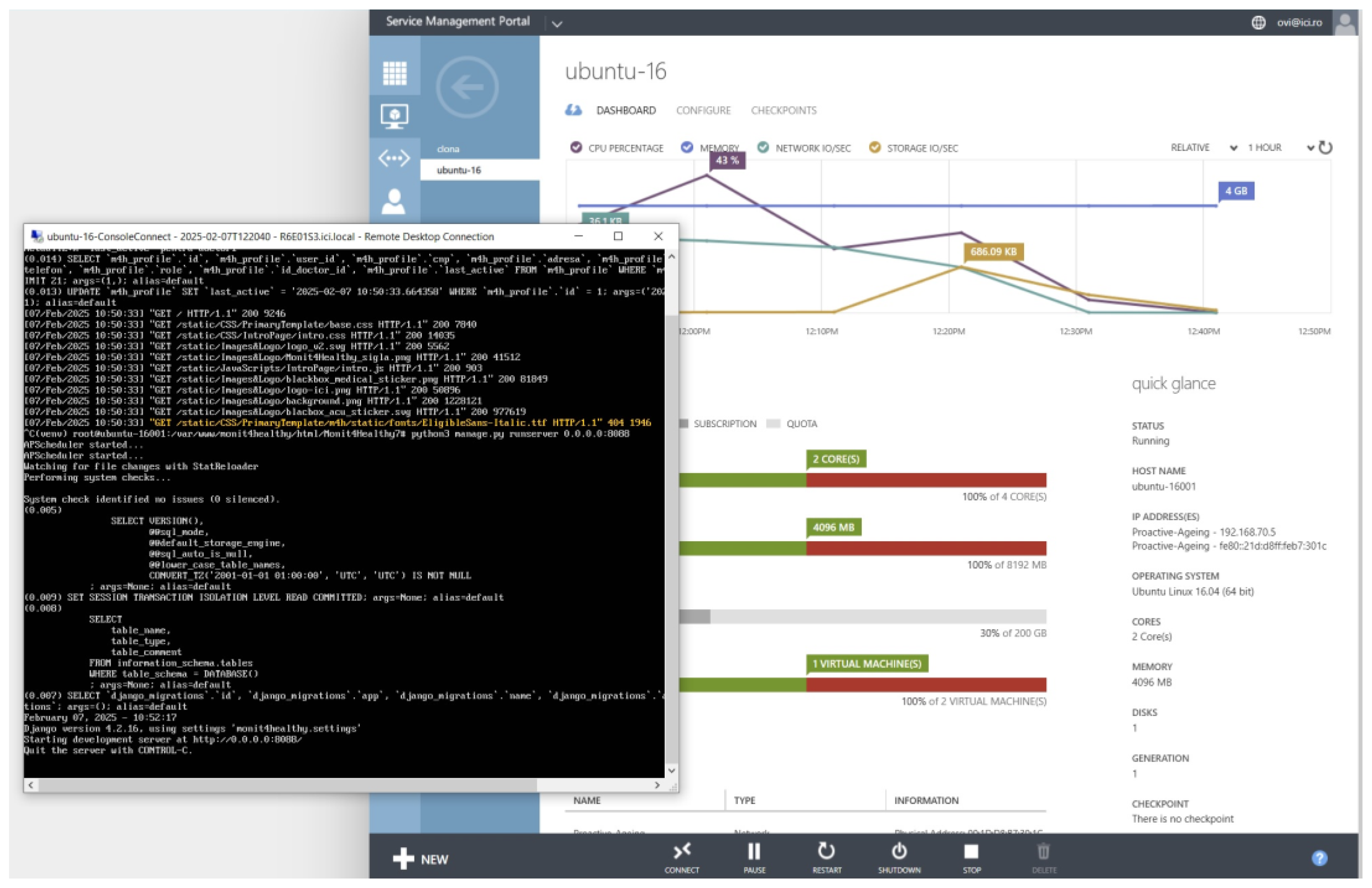
3.3. Development Environment and Tools
3.3.1. Software Frameworks and Programming Environments
- SQL Support: It facilitates the efficient and scalable querying, management, and manipulation of structured data.
- Data Integrity and Security: It implements strong encryption protocols and authentication mechanisms to protect sensitive health information, ensuring compliance with data protection regulations.
- User Authentication and Role-Based Access Control—Django’s built-in authentication system ensures that access to sensitive patient data is restricted to authorized personnel, enforcing strict role-based access policies.
- Patient Management—The framework enables the efficient storage and retrieval of patient data, appointment scheduling, and real-time notifications, ensuring seamless coordination between healthcare providers and patients.
- Medical Professional Management—Django supports the management of medical results, tracking of patient recommendation histories, and coordination of referrals. Additionally, it facilitates the integration of connected medical devices, with automated alert mechanisms notifying healthcare professionals of critical updates, such as abnormal test results or significant changes in a patient’s status.
- Secure Data Handling—The framework incorporates advanced security mechanisms, including built-in protection against SQL injection, cross-site scripting, and cross-site request forgery attacks, ensuring the integrity and confidentiality of medical data.
3.3.2. Hardware Components Used
- ESP32—Chosen for its dual-core architecture, integrated Wi-Fi and Bluetooth capabilities, and ultra-low power consumption, the ESP32 is particularly suited for remote patient monitoring systems that require real-time data transmission over wireless networks. Its deep-sleep functionality minimizes energy usage, ensuring extended operation in battery-powered medical devices [68].
- STM32—These are a family of ARM Cortex-based microcontrollers offering high computational efficiency and low power consumption, making them ideal for embedded medical applications requiring real-time processing. An STM32 microcontroller compresses the digital ECG signals using a basic matrix–vector multiplication technique based on compressed sensing [69].
- Raspberry Pi—Serving as an edge computing node, Raspberry Pi offers high processing power and versatile I/O capabilities, enabling the real-time preprocessing of biomedical signals, anomaly detection, and encrypted data transmission to cloud servers. This reduces network latency and offloads computational tasks from the central cloud infrastructure [70].
- ATmega2560 Microcontroller—Applications requiring extensive firmware storage and multitasking can benefit from the ATmega2560, an 8-bit AVR microcontroller with 256 KB of flash memory, 8 KB of SRAM, and 4 KB of EEPROM. Four UARTs, an SPI, I2C, and sixteen 10-bit analog-to-digital converter channels are among the many peripherals it supports. The AT-mega2560, which runs at a clock speed of 16 MHz, provides dependable performance for activities involving real-time data collection and control while consuming little power, which is crucial for embedded health monitoring applications [71].
- Arduino Mega Board—With 54 digital input/output pins, 16 analog inputs, and various serial communication interfaces, the Arduino Mega board, which is based on the ATmega2560 microcontroller, has extensive I/O capabilities that enable integration with multiple biomedical sensors at once. The Arduino Mega is used in the Medical Blackbox device of the Monit4Healthy system to collect and interpret physiological signals in real time. Strong and scalable health monitoring systems are made possible by its dependable interrupt management, hardware timers, and interoperability with common sensor libraries, which provide effective and coordinated data collection from multi-sensor arrays [72]. Currently, the Medical Blackbox is powered via a regulated 5V DC input, compatible with external USB power adapters and battery packs, ensuring safe and portable operation during laboratory testing.
- Biomedical Sensors—Modules such as MAX30100, for heart rate and SpO2 monitoring via PPG; AD8232, for real-time ECG signal acquisition; a custom EMG module, for electromyography signal capture, designed with adjustable gain, bandpass filtering, and analog signal conditioning tailored for muscle activity monitoring; a GSR sensor, for galvanic skin response measurement, used in stress and autonomic nervous system assessments; and a digital temperature sensor, for continuous body temperature monitoring for real-time ECG signal acquisition, enable continuous physiological monitoring, facilitating the early detection of health anomalies.
3.3.3. Data Processing Frameworks
4. Results
4.1. Selected Illustrations of Implemented Devices
4.1.1. The Medical Blackbox Device
4.1.2. The EMG Blackbox Device
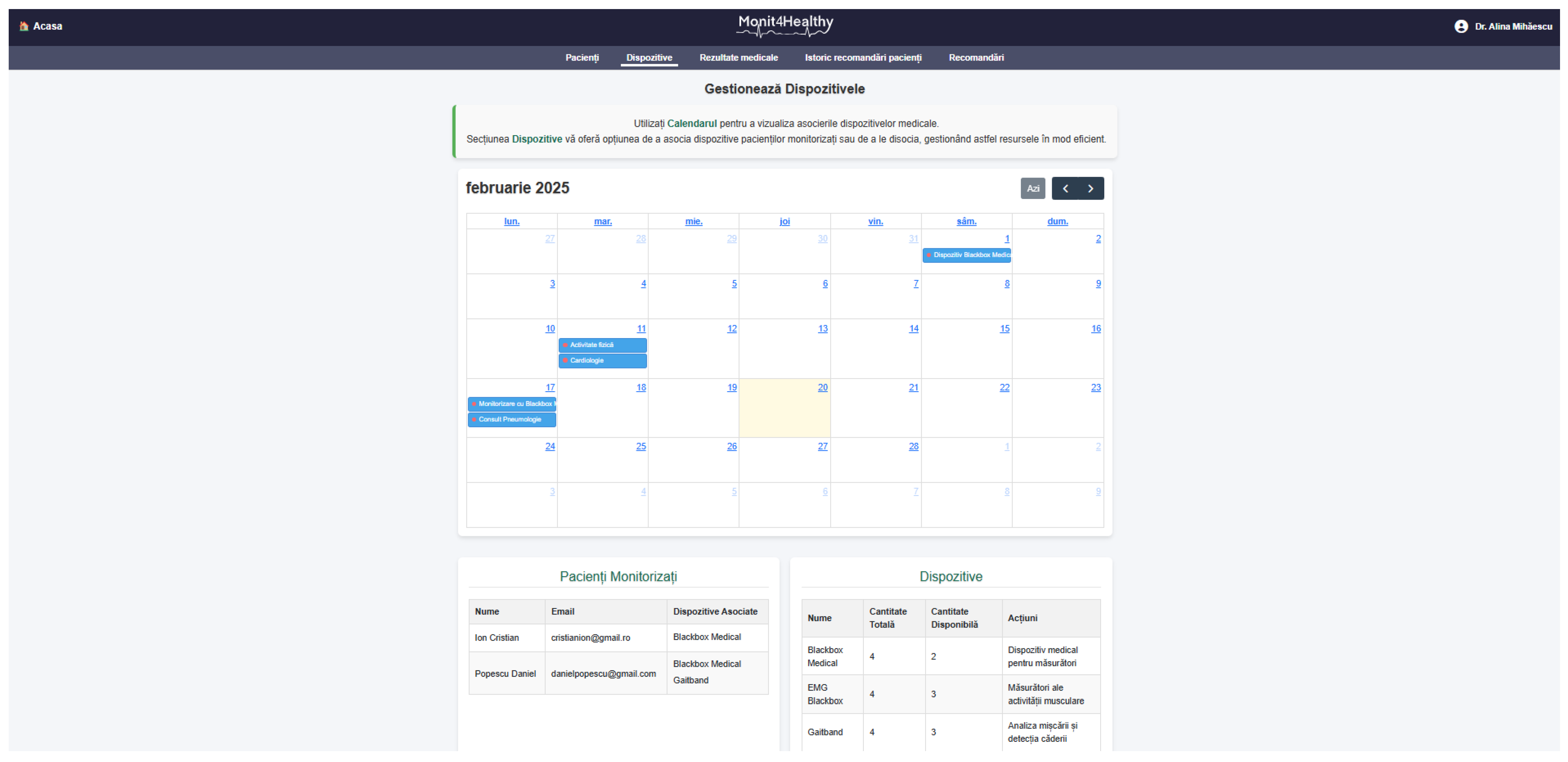
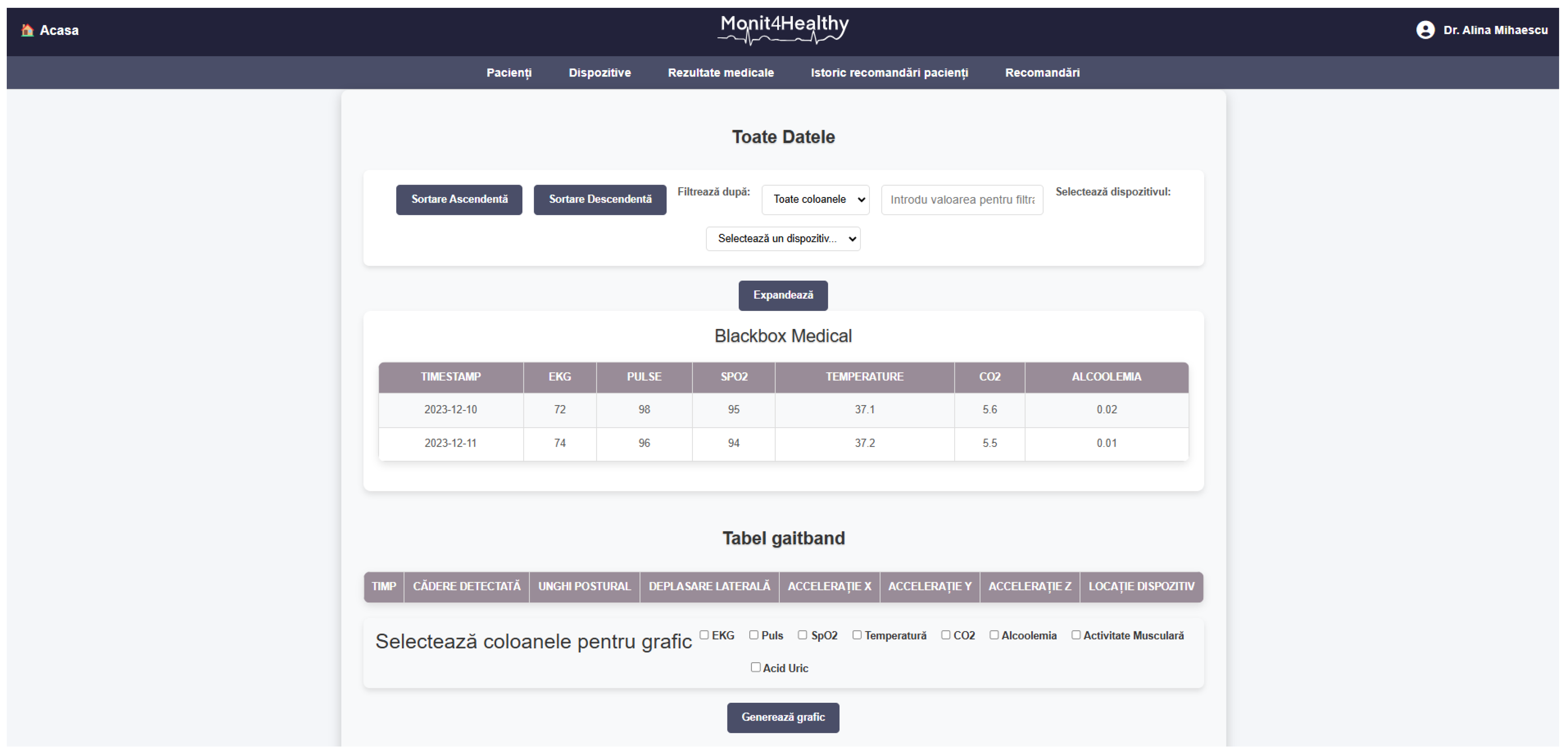
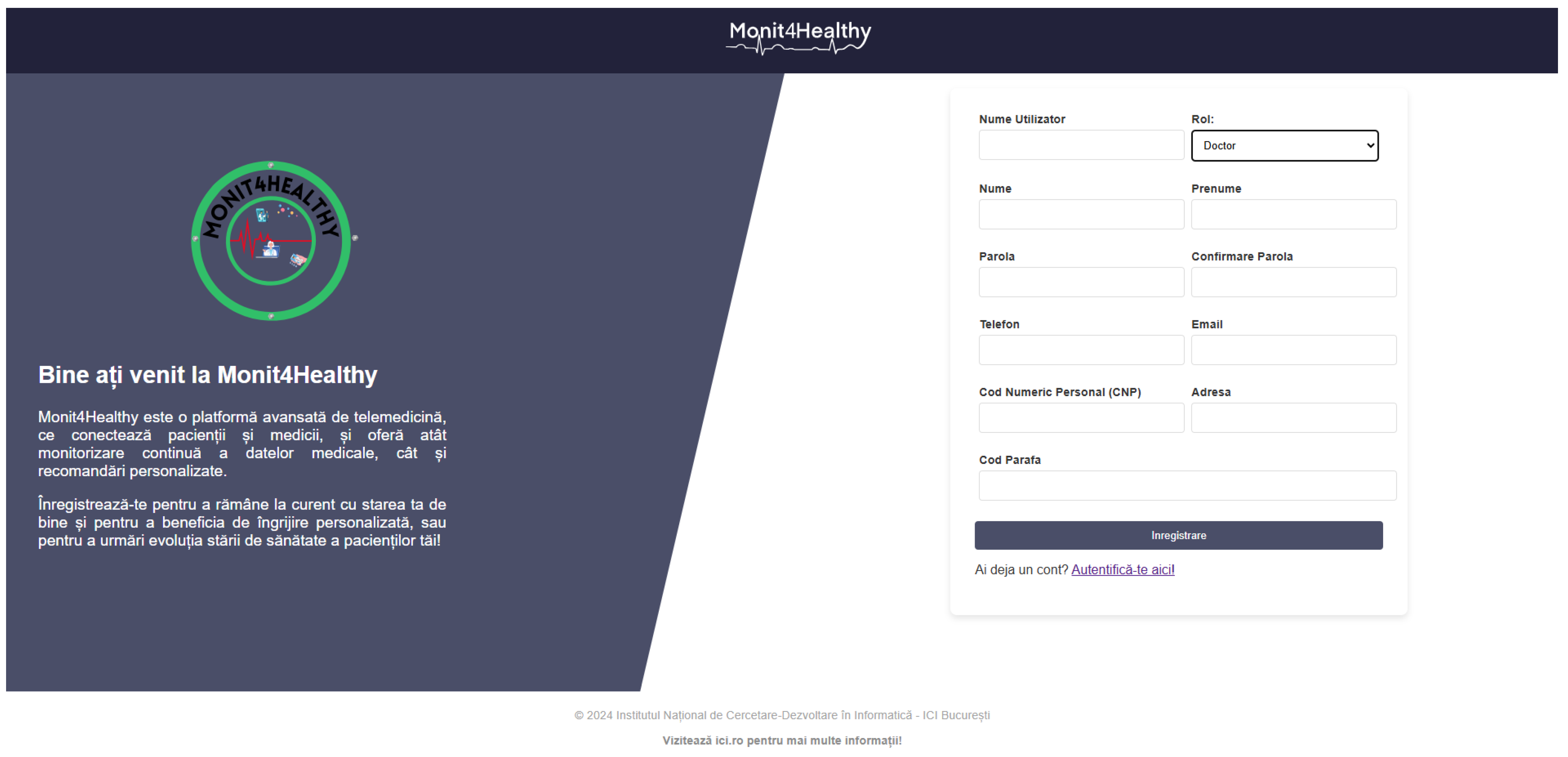
4.2. Monit4Healthy Platform Development
4.2.1. Monit4Healthy Platform Overview
4.2.2. Patient Interface
4.2.3. Medical Professional Interface
- The History of Medical Recommendations section of the Monit4Healthy platform is designed to facilitate the review of past clinical guidance provided to patients. This section provides an interactive interface incorporating a dropdown menu, allowing clinicians to select a specific patient. Upon selection, the platform dynamically displays all previously issued recommendations for the specific patient. This historical overview permits the medical professional to identify trends in patient response to recommendations.
4.2.4. Real-Time Data Transmission and Alerts
4.2.5. Platform Authentication and User Management
4.3. Development Phase Observations
5. Discussion
- Latency optimization: The minimization of transmission delays is accomplished by employing local edge-level preprocessing, therefore reducing the volume of raw biomedical signals being delivered to cloud infrastructures. By substituting the mere reliance on cloud-based processing with real-time physiological filtering and feature extraction occurring at the acquisition level, the system ensures that it is clinically relevant and only transmits well structured data. This approach is expected to reduce latency in scenarios of high-priority health monitoring, such as in detecting arrhythmias based on ECG data, when event-triggered alerts are dire.
- Bandwidth utilization efficiency: The Monit4Healthy system implements adaptive data selection mechanisms, with the purpose of improving network efficiency. To reduce redundant data transmissions, the system replaces the approach of continuously streaming high-frequency signals with periodic reporting and event-triggered alerts. Given that network congestion and resource allocations need to be optimized when designing remote monitoring systems, this design is specifically efficient. The system’s dual-mode communication approach—using BLE for short-range sensor connectivity and Wi-Fi for higher-resolution data transmission when necessary—allows scalable and energy-efficient data exchange.
- Energy consumption considerations: The system improves energy efficiency by implementing a structured power management strategy, minimizing cloud reliance by passing computational tasks to local processing units. To optimize sensor-device interactions, the system utilizes BLE-based communications protocols, which have established low-power characteristics. Further quantitative analysis is required in order to validate the impact of these features in continuous monitoring scenarios, although they are anticipated to enhance energy-efficient operations. The reduction in continuous high-power transmissions, combined with the event-driven adaptive communication is anticipated to lengthen the lifespan of wearable and portable monitoring units. Despite these projections, battery consumption metrics need prolonged real-world evaluation. To additionally improve energy efficiency in extended health monitoring scenarios, future research could focus on duty-cycling mechanisms and machine learning-driven power scheduling.
- Real-world clinical assessments are still unexplored, despite laboratory testing confirming the system’s fundamental functioning. Future research is required to evaluate the Monit4Healthy system’s effectiveness in dynamic real-world settings, especially where network unpredictability, patient mobility, and telemedicine integration are involved.
- Another challenge is scalability, especially when it comes to easy integration with current telemedicine solutions and healthcare IT infrastructures. Even though the system’s modular architecture allows for flexibility, further testing is necessary to guarantee that it can handle extensive medical applications.
- Measurements for the long-term power usage of continuous monitoring have not yet been assessed apart from controlled laboratory settings. Although edge computing decreases redundant data transmission, energy efficiency is expected to be boosted using adaptive power management approaches, especially for wearable and portable applications; future experimental validations need to be performed to identify the practical advantages of these approaches in real-word settings.
- Carrying out extensive experiments to assess system performance in genuine clinical and digital health settings.
- Implementing a full English language option to improve usability for international users.
- Connecting EHRs and other type of healthcare solutions to provide simple interoperability and data sharing.
- Investigating hybrid IoT communication models that provide high-bandwidth, low-latency medical data transmission by integrating 5G-enabled frameworks.
- Future developments focusing on implementing advanced multi-sensor fusion algorithms, enabling the generation of composite health indicators by correlating synchronized ECG, EMG, PPG, and GSR data.
- Developing predictive analytics powered by AI to improve the automated identification of abnormalities and individualized health monitoring.
- To optimize network efficiency, current implementations are targeted toward structured data transmission. Despite ongoing approaches, future research could employ adaptive power management techniques, such as dynamic sensor sampling rate adjustments, to allow the system to reduce data acquisition frequency, and duty-cycling mechanisms, to power down non-essential components during periods of inactivity. To further lengthen the battery life, energy-aware task scheduling could be explored as well.
- Future experimental validations will quantitatively analyze Monit4Healthy’s energy consumption across various operating conditions, assessing the real impact of edge computing and adaptive data transmission on power efficiency.
- Integration with IoT-specific protocols like MQTT is being considered for future development phases, particularly to improve scalability and interoperability in smart city ecosystems or more intricate, dispersed healthcare infrastructures. This will further align the Monit4Healthy system with IoT communication standards by enabling efficient device-to-device and device-to-cloud connection.
- The potential benefits of edge computing will be addressed in more depth. This consists of real-world and simulation-based comparisons of edge-enabled and cloud-only setups, with an emphasis on important performance indicators including power consumption, processing time, data volume, and transmission latency. The findings from these investigations will allow for the additional optimization of the Monit4Healthy system’s edge-cloud integration strategy and quantitatively validate the architectural benefits of the system across various healthcare situations.
- Comprehensive clinical accuracy benchmarking against certified medical equipment is scheduled during real-world deployment phases to validate sensor performance under operational healthcare conditions.
- Adaptive communication strategies that dynamically optimize protocol selection and channel allocation in real time, aiming to enhance transmission reliability and energy efficiency in high-density and variable network environments, will be taken into consideration.
- Miniaturizing the Medical Blackbox by designing a custom PCB to replace the current prototyping board aims to optimize the device’s size, improve power efficiency, and enhance hardware reliability for long-term deployment in both clinical and home-based settings.
- Future research will involve thorough power profiling under a range of operating situations, such as continuous monitoring, event-driven alerts, and inactivity states, in order to comprehensively assess the energy efficiency of the Monit4Healthy system. All system components’ current drawing and consumption trends will be tracked using standardized energy measuring instruments. We will analyze metrics like overall battery duration under particular tasks, energy per transmitted data unit (mWh/MB), and average energy consumption (mW). These parameters will corroborate the system’s energy optimization assertions and direct future hardware and software improvements by enabling comparisons with other IoT-based health monitoring solutions. Future analyses will measure energy consumption per unit of processed biomedical data (e.g., milliwatts per kilobyte transmitted) and energy per monitoring session (e.g., Wh per 1 h operation under standard use settings) in order to assess the system’s energy efficiency. The baseline measurements from cloud-only monitoring systems with comparable sensor configurations but no edge-level preprocessing or structured data transfer will be compared to these measurements. The energy-saving effects of the Monit4Healthy system’s edge computing and adaptive transmission approaches will be measurable through this comparison.
- Phase 1—Pilot Trials in Controlled Clinical Settings
- –
- Objective: Evaluate reliability, usability, and accuracy under supervision of medical professionals.
- –
- Activities: Deploy Monit4Healthy units in medical units for short-term trials; monitor ECG, EMG, and PPG signal acquisition; assess edge–cloud performance in operational conditions.
- –
- Metrics: User feedback, real-time alert responsiveness, signal integrity, data transmission stability, and power consumption profiles.
- –
- Duration: 3–6 months.
- –
- Deliverables: Technical report on system performance; validated integration with EHR platforms and telemedicine systems.
- Phase 2—Multi-Site and Home-Based Testing
- –
- Objective: Assess scalability, adaptability, and long-term reliability in diverse healthcare scenarios.
- –
- Activities: Deploy in multiple sites including home-care environments; focus on patient mobility, variable network conditions, and extended monitoring periods.
- –
- Metrics: Energy consumption trends, battery life in real conditions, network adaptability, anomaly detection rates, data privacy compliance.
- –
- Duration: 6–9 months.
- –
- Deliverables: Comparative performance analysis vs. cloud-only systems; refinement of adaptive power management; user satisfaction studies.
- Phase 3—System Optimization and Hardware Refinement
- –
- Objective: Miniaturize hardware components, improve energy efficiency, and enhance user ergonomics.
- –
- Activities: Design and fabricate custom PCBs for Medical Blackbox and EMG devices; integrate energy-aware scheduling; implement secure boot and firmware updates.
- –
- Metrics: Reduction in form factor, increased battery efficiency (target >12 h), and hardware validation.
- –
- Duration: 6 months (overlapping with Phase 2).
- –
- Deliverables: Optimized prototypes; industrial design for wearable/portable use; regulatory compliance planning (e.g., CE, FDA).
- Phase 4—Integration into Smart Health Ecosystems
- –
- Objective: Align Monit4Healthy system with smart city infrastructure.
- –
- Activities: Pilot integration with municipal health dashboards, emergency services, and AI-powered health trend analytics; implementation of MQTT for scalable IoT communication.
- –
- Metrics: Interoperability benchmarks, real-time data aggregation at population level.
- –
- Duration: 9–12 months.
- –
- Deliverables: Full-scale deployment proposal; partnership reports; scalability studies.
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AFH | Adaptive Frequency Hopping; |
| AI | Artificial Intelligence; |
| BLE | Bluetooth Low Energy; |
| CAD | Computer-Aided Design; |
| CLI | Command Line Interface; |
| ECG | Electrocardiography; |
| EMG | Electromyography; |
| FHIR | Fast Healthcare Interoperability Resources; |
| GDPR | General Data Protection Regulation; |
| GPS | Global Positioning System; |
| GSR | Galvanic Skin Response; |
| HIPAA | Health Insurance Portability and Accountability Act; |
| I2C | Inter-Integrated Circuit; |
| IaaS | Infrastructure as a Service; |
| IoT | Internet of Things; |
| LoRaWAN | Long-Range Wide-Area Network; |
| ORM | Object Relational Mapper; |
| MCU | Microcontroller Unit; |
| PPG | Photoplethysmogram; |
| RPM | Remote Patient Monitoring; |
| SpO2 | Oxygen Saturation; |
| SQL | Structured Query Language; |
| SSL | Secure Sockets Layer; |
| TLS | Transport Layer Security; |
| VM | Virtual Machine; |
| Wi-Fi | Wireless Fidelity. |
References
- Sarkar, M.; Lee, T.-H.; Sahoo, P.K. Smart Healthcare: Exploring the Internet of Medical Things with Ambient Intelligence. Electronics 2024, 13, 2309. [Google Scholar] [CrossRef]
- Copenhagen: WHO Regional Office for Europe Building a Public Health Innovation Ecosystem in the WHO European, Region: Meeting Report. 2024. Available online: https://www.who.int/europe/publications/i/item/WHO-EURO-2024-10102-49874-74930 (accessed on 21 March 2025).
- Băjenaru, L.; Marinescu, I.A.; Tomescu, M.; Drăghici, R. Evaluarea Satisfacției Persoanelor Vârstnice În Utilizarea de Tehnologii Inteligente Asistive: VINCI Studiu de Caz. Rev. Română De Informatică Și Autom. 2022, 32, 19–32. [Google Scholar] [CrossRef]
- Kouchaki, S.; Ding, X.; Sanei, S. AI- and IoT-Enabled Solutions for Healthcare. Sensors 2024, 24, 2607. [Google Scholar] [CrossRef]
- AlAdwani, H.; Zahra. A Systematic Review of IoT Integration on Health Monitoring System. Int. J. Eng. Manag. Res. 2023, 13, 50–59. [Google Scholar] [CrossRef]
- Koulouras, G.; Katsoulis, S.; Zantalis, F. Evolution of Bluetooth Technology: BLE in the IoT Ecosystem. Sensors 2025, 25, 996. [Google Scholar] [CrossRef]
- Safi, H.; Jehangiri, A.I.; Ahmad, Z.; Ala’anzy, M.A.; Alramli, O.I.; Algarni, A. Design and Evaluation of a Low-Power Wide-Area Network (LPWAN)-Based Emergency Response System for Individuals with Special Needs in Smart Buildings. Sensors 2024, 24, 3433. [Google Scholar] [CrossRef]
- Durand, T.G.; Visagie, L.; Booysen, M.J. Evaluation of Next-generation Low-power Communication Technology to Replace GSM in IoT-applications. IET Commun. 2019, 13, 2533–2540. [Google Scholar] [CrossRef]
- Ait Abdelouahid, R.; Debauche, O.; Mahmoudi, S.; Marzak, A. Literature Review: Clinical Data Interoperability Models. Information 2023, 14, 364. [Google Scholar] [CrossRef]
- Azzedin, F.; Alhazmi, T. Secure Data Distribution Architecture in IoT Using MQTT. Appl. Sci. 2023, 13, 2515. [Google Scholar] [CrossRef]
- Shahid, J.; Ahmad, R.; Kiani, A.K.; Ahmad, T.; Saeed, S.; Almuhaideb, A.M. Data Protection and Privacy of the Internet of Healthcare Things (IoHTs). Appl. Sci. 2022, 12, 1927. [Google Scholar] [CrossRef]
- Popoola, O.; Rodrigues, M.; Marchang, J.; Shenfield, A.; Ikpehai, A.; Popoola, J. A Critical Literature Review of Security and Privacy in Smart Home Healthcare Schemes Adopting IoT & Blockchain: Problems, Challenges and Solutions. Blockchain Res. Appl. 2024, 5, 100178. [Google Scholar] [CrossRef]
- da Costa, T.P.; da Costa, D.M.B.; Murphy, F. A Systematic Review of Real-Time Data Monitoring and Its Potential Application to Support Dynamic Life Cycle Inventories. Environ. Impact Assess. Rev. 2024, 105, 107416. [Google Scholar] [CrossRef]
- Al Khatib, I.; Shamayleh, A.; Ndiaye, M. Healthcare and the Internet of Medical Things: Applications, Trends, Key Challenges, and Proposed Resolutions. Informatics 2024, 11, 47. [Google Scholar] [CrossRef]
- Rupanetti, D.; Kaabouch, N. Combining Edge Computing-Assisted Internet of Things Security with Artificial Intelligence: Applications, Challenges, and Opportunities. Appl. Sci. 2024, 14, 7104. [Google Scholar] [CrossRef]
- Bhuiyan, M.N.; Rahman, M.M.; Billah, M.M.; Saha, D. Internet of Things (IoT): A Review of Its Enabling Technologies in Healthcare Applications, Standards Protocols, Security, and Market Opportunities. IEEE Internet Things J. 2021, 8, 10474–10498. [Google Scholar] [CrossRef]
- Wu, X.; Liu, C.; Wang, L.; Bilal, M. Internet of Things-Enabled Real-Time Health Monitoring System Using Deep Learning. Neural Comput. Appl. 2023, 35, 14565–14576. [Google Scholar] [CrossRef]
- Su, M.; Hua, J.; Sun, X.; Liu, Z.; Shi, Y.; Pan, L. Wireless Wearable Devices and Recent Applications in Health Monitoring and Clinical Diagnosis. Biomed. Mater. Devices 2024, 2, 669–694. [Google Scholar] [CrossRef]
- Omaghomi, T.T.; Elufioye, O.A.; Akomolafe, O.; Anyanwu, E.C.; Odilibe, I.P. A Comprehensive Review of Telemedicine Technologies: Past, Present, and Future Prospects. Int. Med. Sci. Res. J. 2024, 4, 183–193. [Google Scholar] [CrossRef]
- Buleje, I.; Siu, V.S.; Hsieh, K.Y.; Hinds, N.; Dang, B.; Bilal, E.; Nguyen, T.; Lee, E.E.; Depp, C.A.; Rogers, J.L. A Versatile Data Fabric for Advanced IoT-Based Remote Health Monitoring. In Proceedings of the 2023 IEEE International Conference on Digital Health (ICDH), Chicago, IL, USA, 2–8 July 2023; IEEE: Piscataway, NJ, USA, 2023; pp. 88–90. [Google Scholar]
- Laska, B.; Xi, P.; Valdés, J.J.; Wallace, B.; Goubran, R. Zero-Shot Multi-Task Cough Sound Analysis with Speech Foundation Model Embeddings. In Proceedings of the 2024 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Eindhoven, The Netherlands, 26–28 June 2024; IEEE: Piscataway, NJ, USA, 2024; pp. 1–6. [Google Scholar]
- Dadkhah, M.; Mehraeen, M.; Rahimnia, F.; Kimiafar, K. Use of Internet of Things for Chronic Disease Management. J. Med. Signals Sens. 2021, 11, 138–157. [Google Scholar] [CrossRef]
- Talpur, M.S.H.; Abro, A.A.; Ebrahim, M.; Kandhro, I.A.; Manickam, S.; Laghari, S.U.A.; Dandoush, A.; Uddin, M. Illuminating Healthcare Management: A Comprehensive Review of IoT-Enabled Chronic Disease Monitoring. IEEE Access 2024, 12, 48189–48209. [Google Scholar] [CrossRef]
- de Farias, F.A.C.; Dagostini, C.M.; de Assunção Bicca, Y.; Falavigna, V.F.; Falavigna, A. Remote Patient Monitoring: A Systematic Review. Telemed. e-Health 2020, 26, 576–583. [Google Scholar] [CrossRef] [PubMed]
- Ianculescu, M.; Paraschiv, E.-A.; Alexandru, A. Addressing Mild Cognitive Impairment and Boosting Wellness for the Elderly through Personalized Remote Monitoring. Healthcare 2022, 10, 1214. [Google Scholar] [CrossRef] [PubMed]
- De Sario Velasquez, G.D.; Borna, S.; Maniaci, M.J.; Coffey, J.D.; Haider, C.R.; Demaerschalk, B.M.; Forte, A.J. Economic Perspective of the Use of Wearables in Health Care: A Systematic Review. Mayo Clin. Proc. Digit. Health 2024, 2, 299–317. [Google Scholar] [CrossRef]
- Lekwijit, S.; Terwiesch, C.; Asch, D.A.; Volpp, K.G. Evaluating the Efficacy of Connected Healthcare: An Empirical Examination of Patient Engagement Approaches and Their Impact on Readmission. Manag. Sci. 2024, 70, 3417–3446. [Google Scholar] [CrossRef]
- Abdulmalek, S.; Nasir, A.; Jabbar, W.A.; Almuhaya, M.A.M.; Bairagi, A.K.; Khan, M.A.-M.; Kee, S.-H. IoT-Based Healthcare-Monitoring System towards Improving Quality of Life: A Review. Healthcare 2022, 10, 1993. [Google Scholar] [CrossRef]
- Hashim, H.; Salihudin, S.F.B.; Saad, P.S.M. Development of IoT Based Healthcare Monitoring System. In Proceedings of the 2022 IEEE International Conference in Power Engineering Application (ICPEA), Shah Alam, Malaysia, 7–8 March 2022; IEEE: Piscataway, NJ, USA, 2022; pp. 1–5. [Google Scholar]
- Dankan Gowda, V.; Chaithra, S.M.; Gujar, S.S.; Firoz Shaikh, S.; Ingole, B.S.; Sudhakar Reddy, N. Scalable AI Solutions for IoT-Based Healthcare Systems Using Cloud Platforms. In Proceedings of the 2024 8th International Conference on I-SMAC (IoT in Social, Mobile, Analytics and Cloud) (I-SMAC), Kirtipur, Nepal, 3–5 October 2024; IEEE: Piscataway, NJ, USA, 2024; pp. 156–162. [Google Scholar]
- Martins, A.; Londral, A.; Nunes, I.L.; Lapão, L.V. Unlocking Human-like Conversations: Scoping Review of Automation Techniques for Personalized Healthcare Interventions Using Conversational Agents. Int. J. Med. Inform. 2024, 185, 105385. [Google Scholar] [CrossRef]
- Navaz, A.N.; Serhani, M.A.; El Kassabi, H.T.; Al-Qirim, N.; Ismail, H. Trends, Technologies, and Key Challenges in Smart and Connected Healthcare. IEEE Access 2021, 9, 74044–74067. [Google Scholar] [CrossRef]
- Ramachandran, G. Creating a Digital Spine for Connected Healthcare Ecosystem: Digitalization for an Effective Supply Chain. In Resilient Health; Academic Press: Cambridge, MA, USA, 2024. [Google Scholar]
- Rehman, A.; Naz, S.; Razzak, I. Leveraging Big Data Analytics in Healthcare Enhancement: Trends, Challenges and Opportunities. Multimed. Syst. 2022, 28, 1339–1371. [Google Scholar] [CrossRef]
- Tian, Y.J.; Felber, N.A.; Pageau, F.; Schwab, D.R.; Wangmo, T. Benefits and Barriers Associated with the Use of Smart Home Health Technologies in the Care of Older Persons: A Systematic Review. BMC Geriatr. 2024, 24, 152. [Google Scholar] [CrossRef]
- Mahmmod, B.M.; Naser, M.A.; Al-Sudani, A.H.S.; Alsabah, M.; Mohammed, H.J.; Alaskar, H.; Almarshad, F.; Hussain, A.; Abdulhussain, S.H. Patient Monitoring System Based on Internet of Things: A Review and Related Challenges with Open Research Issues. IEEE Access 2024, 12, 132444–132479. [Google Scholar] [CrossRef]
- Islam, S.M.R.; Lloret, J.; Zikria, Y. Bin Internet of Things (IoT)-Based Wireless Health: Enabling Technologies and Applications. Electronics 2021, 10, 148. [Google Scholar] [CrossRef]
- Amezquita Garcia, J.A.; Bravo Zanoguera, M.E.; Murrieta-Rico, F.N. Advances and Classification of Autonomous Systems in Biomedical Devices: Integration of Energy Harvesting and Ultra-Low Power Consumption. Electronics 2025, 14, 144. [Google Scholar] [CrossRef]
- Al-Sofi, S.J.; Atroshey, S.M.S.; Ali, I.A. IEEE 802.15.6 and LoRaWAN for WBAN in Healthcare: A Comparative Study on Communication Efficiency and Energy Optimization. Computers 2024, 13, 313. [Google Scholar] [CrossRef]
- Jain, S.; Jain, P.; Upadhyay, P.K.; Moualeu, J.M.; Srivastava, A. An Energy Efficient Health Monitoring Approach with Wireless Body Area Networks. ACM Trans. Comput. Healthc. 2022, 3, 1–22. [Google Scholar] [CrossRef]
- Moreno-Cruz, F.; Toral-López, V.; Escobar-Molero, A.; Ruíz, V.U.; Rivadeneyra, A.; Morales, D.P. TreNch: Ultra-Low Power Wireless Communication Protocol for IoT and Energy Harvesting. Sensors 2020, 20, 6156. [Google Scholar] [CrossRef]
- Rabah, H.; Albasha, L.; Mir, H.; Quadir, N.; Abbas, S.Z. High-Efficiency, Low-Loss, and Wideband 5.8 GHz Energy Harvester Designed Using TSMC 65 nm Process for IoT Self-Powered Nodes. Energies 2025, 18, 862. [Google Scholar] [CrossRef]
- Tohidinejad, Z.; Danyali, S.; Valizadeh, M.; Seepold, R.; TaheriNejad, N.; Haghi, M. Designing a Hybrid Energy-Efficient Harvesting System for Head- or Wrist-Worn Healthcare Wearable Devices. Sensors 2024, 24, 5219. [Google Scholar] [CrossRef]
- Famitafreshi, G.; Afaqui, M.S.; Melià-Seguí, J. A Comprehensive Review on Energy Harvesting Integration in IoT Systems from MAC Layer Perspective: Challenges and Opportunities. Sensors 2021, 21, 3097. [Google Scholar] [CrossRef]
- Dizdarević, J.; Blažević, D.; Grunewald, M.; Jukan, A. An Edge/Cloud Continuum with Wearable Kinetic Energy Harvesting IoT Devices in Remote Areas. In Proceedings of the ICC 2024—IEEE International Conference on Communications, Denver, CO, USA, 9–13 June 2024; IEEE: Piscataway, NJ, USA, 2024; pp. 879–884. [Google Scholar]
- Kurduban, V. Available online: https://Www.Digi.Com/Blog/Post/Edge-Computing-vs-Cloud-Computing (accessed on 22 March 2025).
- Sarangi, A.K.; Mohapatra, A.G.; Mishra, T.C.; Keswani, B. Healthcare 4.0: A Voyage of Fog Computing with IOT, Cloud Computing, Big Data, and Machine Learning. In Fog Computing for Healthcare 4.0 Environments; Springer: Cham, Switzerland, 2021; pp. 177–210. [Google Scholar]
- Al-Marsy, A.; Chaudhary, P.; Rodger, J.A. A Model for Examining Challenges and Opportunities in Use of Cloud Computing for Health Information Systems. Appl. Syst. Innov. 2021, 4, 15. [Google Scholar] [CrossRef]
- Awad, A.I.; Fouda, M.M.; Khashaba, M.M.; Mohamed, E.R.; Hosny, K.M. Utilization of Mobile Edge Computing on the Internet of Medical Things: A Survey. ICT Express 2023, 9, 473–485. [Google Scholar] [CrossRef]
- Issa, M.E.; Helmi, A.M.; Al-Qaness, M.A.A.; Dahou, A.; Abd Elaziz, M.; Damaševičius, R. Human Activity Recognition Based on Embedded Sensor Data Fusion for the Internet of Healthcare Things. Healthcare 2022, 10, 1084. [Google Scholar] [CrossRef]
- Bijalwan, V.; Semwal, V.B.; Mandal, T.K. Fusion of Multi-Sensor-Based Biomechanical Gait Analysis Using Vision and Wearable Sensor. IEEE Sens. J. 2021, 21, 14213–14220. [Google Scholar] [CrossRef]
- Salis, F.; Bertuletti, S.; Scott, K.; Caruso, M.; Bonci, T.; Buckley, E.; Della Croce, U.; Mazza, C.; Cereatti, A. A Wearable Multi-Sensor System for Real World Gait Analysis. In Proceedings of the 2021 43rd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Mexico, 1–5 November 2021; IEEE: Piscataway, NJ, USA, 2021; pp. 7020–7023. [Google Scholar]
- Qiu, S.; Zhao, H.; Jiang, N.; Wang, Z.; Liu, L.; An, Y.; Zhao, H.; Miao, X.; Liu, R.; Fortino, G. Multi-Sensor Information Fusion Based on Machine Learning for Real Applications in Human Activity Recognition: State-of-the-Art and Research Challenges. Inf. Fusion 2022, 80, 241–265. [Google Scholar] [CrossRef]
- John, A.; Cardiff, B.; John, D. A Review on Multisensor Data Fusion for Wearable Health Monitoring. arXiv 2024, arXiv:2412.05895. [Google Scholar]
- Teran-Pineda, D.; Thurnhofer-Hemsi, K.; Dominguez, E. Analysis and Recognition of Human Gait Activity Based on Multimodal Sensors. Mathematics 2023, 11, 1538. [Google Scholar] [CrossRef]
- Zhou, S.; Sun, J.; Xu, K.; Wang, G. AI-Driven Data Processing and Decision Optimization in IoT through Edge Computing and Cloud Architecture. Preprints 2024, 2024100736. [Google Scholar] [CrossRef]
- Still, T. Autodesk Fusion and Cadence: The Power of an Integrated Electromechanical Design Workflow. Available online: https://www.autodesk.com/products/fusion-360/blog/autodesk-fusion-cadence-integrated-workflow-electromechanical-design/ (accessed on 24 March 2025).
- Machine, M.F.G. The Advantages of CAD Software and Why Every Engineer Should Use It. Available online: https://shop.machinemfg.com/the-advantages-of-cad-software-and-why-every-engineer-should-use-it/ (accessed on 24 March 2025).
- Chang, C.-S.; Wu, T.-H.; Wu, Y.-C.; Han, C.-C. Bluetooth-Based Healthcare Information and Medical Resource Management System. Sensors 2023, 23, 5389. [Google Scholar] [CrossRef]
- Specht, C. Maritime DGPS System Positioning Accuracy as a Function of the HDOP in the Context of Hydrographic Survey Performance. Remote Sens. 2022, 15, 10. [Google Scholar] [CrossRef]
- Lee, K.H.; Min, J.Y.; Byun, S. Electromyogram-Based Classification of Hand and Finger Gestures Using Artificial Neural Networks. Sensors 2021, 22, 225. [Google Scholar] [CrossRef]
- Elyounsi, A.; Kalashnikov, A.N. Evaluating Suitability of a DS18B20 Temperature Sensor for Use in an Accurate Air Temperature Distribution Measurement Network. In Proceedings of the 8th International Electronic Conference on Sensors and Applications, Online, 1–15 November 2021; MDPI: Basel, Switzerland, 2021; p. 56. [Google Scholar]
- Uddin, R.; Koo, I. Real-Time Remote Patient Monitoring: A Review of Biosensors Integrated with Multi-Hop IoT Systems via Cloud Connectivity. Appl. Sci. 2024, 14, 1876. [Google Scholar] [CrossRef]
- Heaney, J.; Buick, J.; Hadi, M.U.; Soin, N. Internet of Things-Based ECG and Vitals Healthcare Monitoring System. Micromachines 2022, 13, 2153. [Google Scholar] [CrossRef] [PubMed]
- Divyashree, N.; Prasad, N.K.S. Design and Development of We-CDSS Using Django Framework: Conducing Predictive and Prescriptive Analytics for Coronary Artery Disease. IEEE Access 2022, 10, 119575–119592. [Google Scholar] [CrossRef]
- Alimbayeva, Z.; Alimbayev, C.; Ozhikenov, K.; Bayanbay, N.; Zhikenova, A. Wearable ECG Device and Machine Learning for Heart Monitoring. Sensors 2024, 24, 4201. [Google Scholar] [CrossRef]
- Duart, X.; Quiles, E.; Suay, F.; Chio, N.; García, E.; Morant, F. Evaluating the Effect of Stimuli Color and Frequency on SSVEP. Sensors 2020, 21, 117. [Google Scholar] [CrossRef] [PubMed]
- Ibáñez Castillo, M. Wireless Based Wearable Patient Health Monitoring System Using ESP32. Bachelor’s Thesis, Universitat Politècnica de Catalunya, Barcelona, Spain, 2024. [Google Scholar]
- Cheng, Y.; Ye, Y.; Hou, M.; He, W.; Li, Y.; Deng, X. A Fast and Robust Non-Sparse Signal Recovery Algorithm for Wearable ECG Telemonitoring Using ADMM-Based Block Sparse Bayesian Learning. Sensors 2018, 18, 2021. [Google Scholar] [CrossRef]
- Suresha, P.B.; Hegde, C.; Jiang, Z.; Clifford, G.D. An Edge Computing and Ambient Data Capture System for Clinical and Home Environments. Sensors 2022, 22, 2511. [Google Scholar] [CrossRef]
- Bossard, A. Memory Optimisation on AVR Microcontrollers for IoT Devices’ Minimalistic Displays. Chips 2022, 1, 2–13. [Google Scholar] [CrossRef]
- Ehrmann, G.; Blachowicz, T.; Homburg, S.V.; Ehrmann, A. Measuring Biosignals with Single Circuit Boards. Bioengineering 2022, 9, 84. [Google Scholar] [CrossRef]
- Mathe, S.E.; Kondaveeti, H.K.; Vappangi, S.; Vanambathina, S.D.; Kumaravelu, N.K. A Comprehensive Review on Ap plications of Raspberry Pi. Comput. Sci. Rev. 2024, 52, 100636. [Google Scholar] [CrossRef]
- ICI Bucharest ICIPRO Cloud Computing Services. Available online: https://www.icipro.ro/ (accessed on 25 March 2025).
- Nancy, A.A.; Ravindran, D.; Raj Vincent, P.M.D.; Srinivasan, K.; Gutierrez Reina, D. IoT-Cloud-Based Smart Healthcare Monitoring System for Heart Disease Prediction via Deep Learning. Electronics 2022, 11, 2292. [Google Scholar] [CrossRef]








Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ianculescu, M.; Constantin, V.-Ș.; Gușatu, A.-M.; Petrache, M.-C.; Mihăescu, A.-G.; Bica, O.; Alexandru, A. Enhancing Connected Health Ecosystems Through IoT-Enabled Monitoring Technologies: A Case Study of the Monit4Healthy System. Sensors 2025, 25, 2292. https://doi.org/10.3390/s25072292
Ianculescu M, Constantin V-Ș, Gușatu A-M, Petrache M-C, Mihăescu A-G, Bica O, Alexandru A. Enhancing Connected Health Ecosystems Through IoT-Enabled Monitoring Technologies: A Case Study of the Monit4Healthy System. Sensors. 2025; 25(7):2292. https://doi.org/10.3390/s25072292
Chicago/Turabian StyleIanculescu, Marilena, Victor-Ștefan Constantin, Andreea-Maria Gușatu, Mihail-Cristian Petrache, Alina-Georgiana Mihăescu, Ovidiu Bica, and Adriana Alexandru. 2025. "Enhancing Connected Health Ecosystems Through IoT-Enabled Monitoring Technologies: A Case Study of the Monit4Healthy System" Sensors 25, no. 7: 2292. https://doi.org/10.3390/s25072292
APA StyleIanculescu, M., Constantin, V.-Ș., Gușatu, A.-M., Petrache, M.-C., Mihăescu, A.-G., Bica, O., & Alexandru, A. (2025). Enhancing Connected Health Ecosystems Through IoT-Enabled Monitoring Technologies: A Case Study of the Monit4Healthy System. Sensors, 25(7), 2292. https://doi.org/10.3390/s25072292








