Wearing WHOOP More Frequently Is Associated with Better Biometrics and Healthier Sleep and Activity Patterns
Abstract
1. Introduction
2. Materials and Methods
2.1. Participant Eligibility
2.2. Data Collection
2.3. Categorizing Participants by Wear Frequency
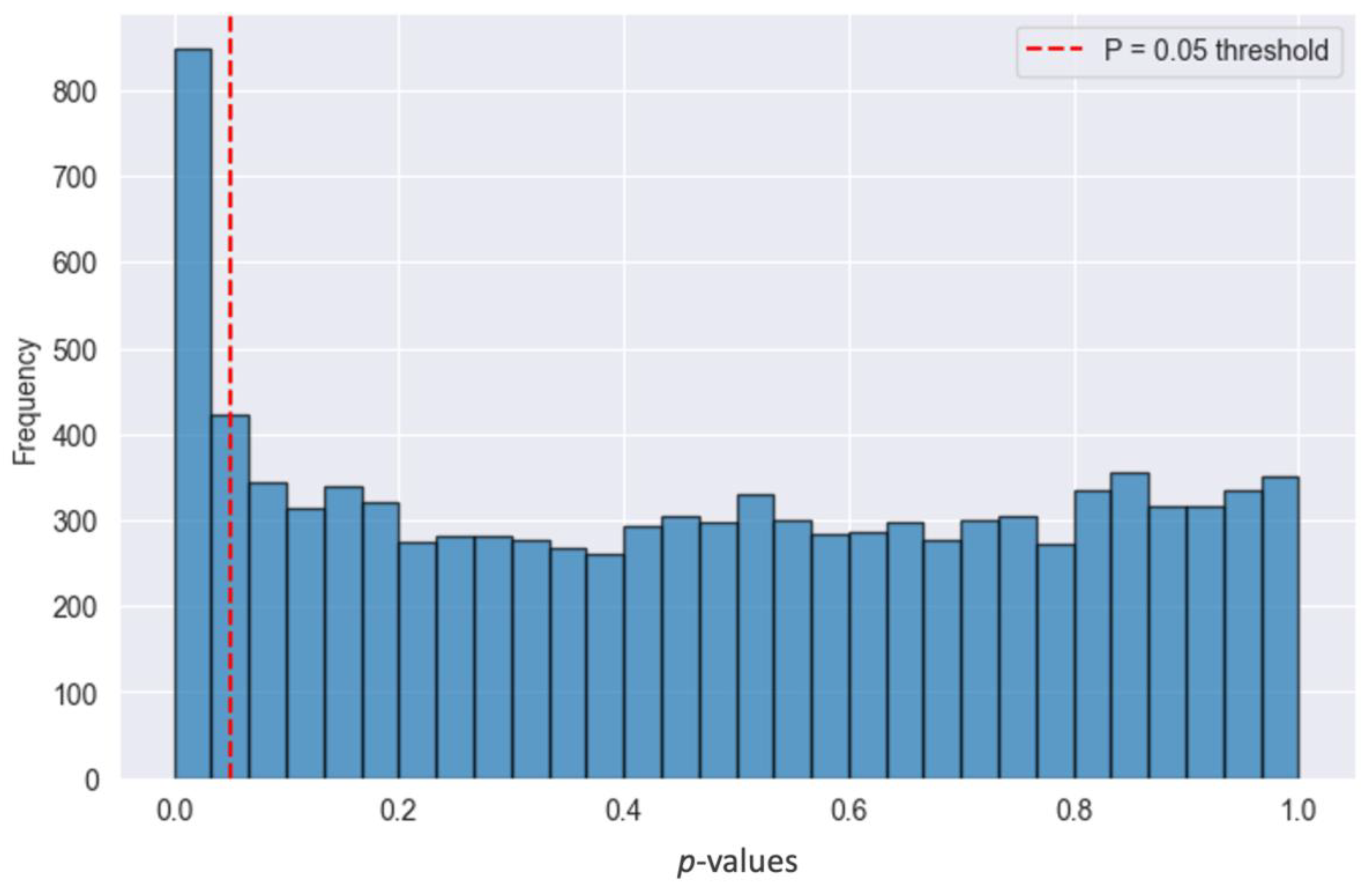
2.4. Statistical Analysis
3. Results
3.1. Higher Wear Frequency and Week-to-Week Increases in Wear Associated with Better Biometrics
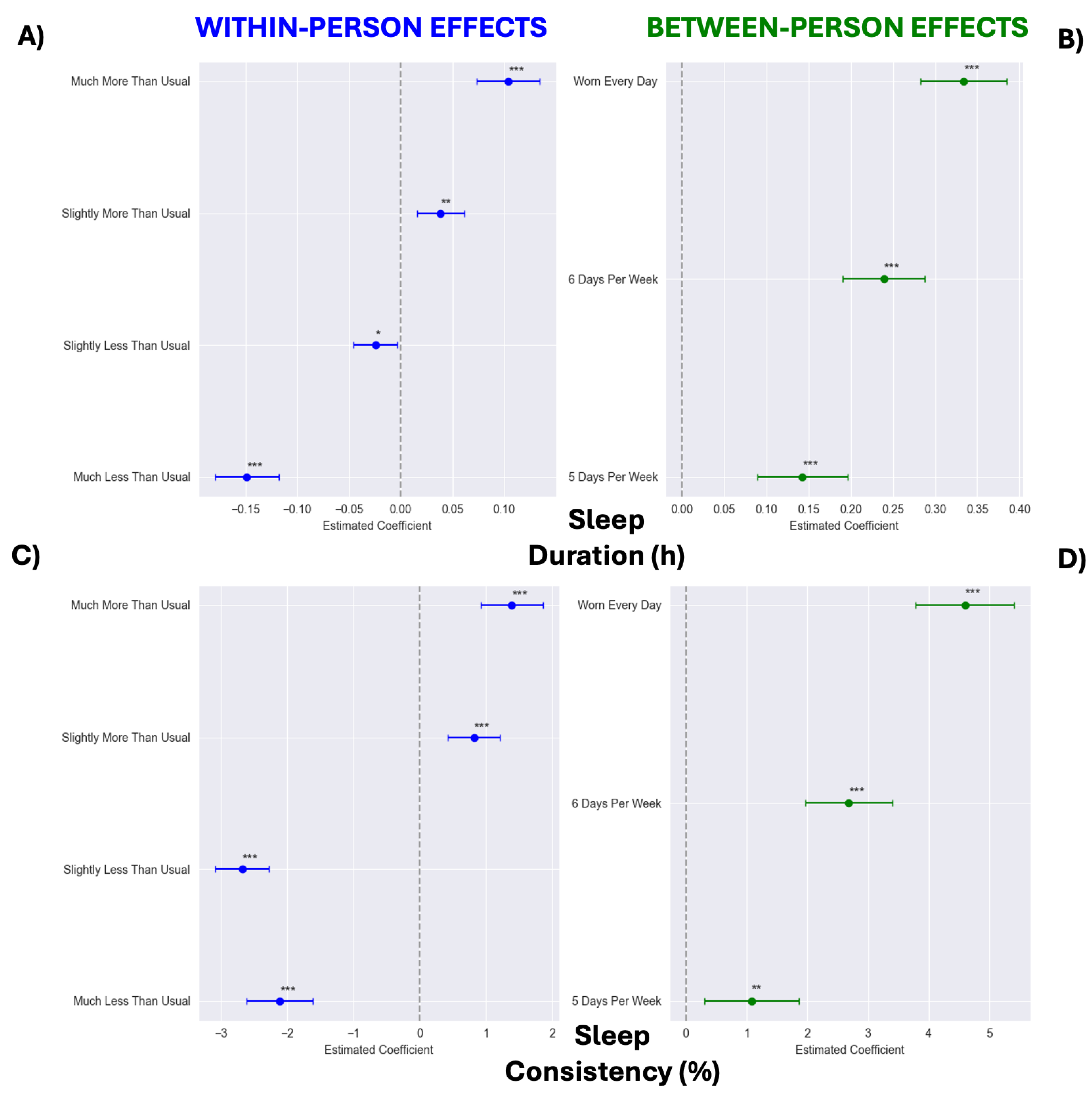
3.2. Sleep Consistency Improves over Time, and Higher Wear Frequency and Week-to-Week Increases in Wear Are Associated with Longer and More Consistent Sleep
3.3. Physical Activity Increases over Time, and Higher Wear Frequency and Week-to-Week Increases in Wear Are Associated with More Activity
3.4. Sleep Duration Partially Mediates the Association Between Wear Frequency and RHR
3.5. Past Wear Frequency Predicts Future Resting Heart Rate
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BMI | Body mass index |
| HRV | Heart rate variability |
| RHR | Resting heart rate |
References
- Dhingra, L.S.; Aminorroaya, A.; Oikonomou, E.K.; Nargesi, A.A.; Wilson, F.P.; Krumholz, H.M.; Khera, R. Use of Wearable Devices in Individuals With or at Risk for Cardiovascular Disease in the US, 2019 to 2020. JAMA Netw. Open 2023, 6, e2316634. [Google Scholar] [CrossRef] [PubMed]
- Piwek, L.; Ellis, D.A.; Andrews, S.; Joinson, A. The Rise of Consumer Health Wearables: Promises and Barriers. PLoS Med. 2016, 13, e1001953. [Google Scholar] [CrossRef]
- Paolillo, E.W.; Lee, S.Y.; VandeBunte, A.; Djukic, N.; Fonseca, C.; Kramer, J.H.; Casaletto, K.B. Wearable Use in an Observational Study Among Older Adults: Adherence, Feasibility, and Effects of Clinicodemographic Factors. Front. Digit. Health 2022, 4, 884208. [Google Scholar] [CrossRef]
- Alam, S.; Zhang, M.; Harris, K.; Fletcher, L.M.; Reneker, J.C. The Impact of Consumer Wearable Devices on Physical Activity and Adherence to Physical Activity in Patients with Cardiovascular Disease: A Systematic Review of Systematic Reviews and Meta-Analyses. Telemed. J. E Health 2023, 29, 986–1000. [Google Scholar] [CrossRef] [PubMed]
- Au, W.W.; Recchia, F.; Fong, D.Y.; Wong, S.H.S.; Chan, D.K.C.; Capio, C.M.; Yu, C.C.W.; Wong, S.W.S.; Sit, C.H.P.; Ip, P.; et al. Effect of wearable activity trackers on physical activity in children and adolescents: A systematic review and meta-analysis. Lancet Digit. Health 2024, 6, e625–e639. [Google Scholar] [CrossRef] [PubMed]
- Szeto, K.; Arnold, J.; Singh, B.; Gower, B.; Simpson, C.E.M.; Maher, C. Interventions Using Wearable Activity Trackers to Improve Patient Physical Activity and Other Outcomes in Adults Who Are Hospitalized: A Systematic Review and Meta-analysis. JAMA Netw. Open 2023, 6, e2318478. [Google Scholar] [CrossRef]
- Mizuno, A.; Changolkar, S.; Patel, M.S. Wearable Devices to Monitor and Reduce the Risk of Cardiovascular Disease: Evidence and Opportunities. Annu. Rev. Med. 2021, 72, 459–471. [Google Scholar] [CrossRef]
- Heizmann, A.N.; Chapelle, C.; Laporte, S.; Roche, F.; Hupin, D.; Le Hello, C. Impact of wearable device-based interventions with feedback for increasing daily walking activity and physical capacities in cardiovascular patients: A systematic review and meta-analysis of randomised controlled trials. BMJ Open 2023, 13, e069966. [Google Scholar] [CrossRef]
- Berryhill, S.; Morton, C.J.; Dean, A.; Berryhill, A.; Provencio-Dean, N.; Patel, S.I.; Estep, L.; Combs, D.; Mashaqi, S.; Gerald, L.B.; et al. Effect of wearables on sleep in healthy individuals: A randomized crossover trial and validation study. J. Clin. Sleep Med. 2020, 16, 775–783. [Google Scholar] [CrossRef]
- Moore, S.L.; Carey, E.P.; Finikiotis, K.; Ford, K.L.; Zane, R.D.; Green, K.K. Use of a wearable device to improve sleep quality. Front. Digit. Health 2024, 6, 1384173. [Google Scholar] [CrossRef]
- Reilly, T.; Peiser, B. Seasonal variations in health-related human physical activity. Sports Med. 2006, 36, 473–485. [Google Scholar] [CrossRef]
- Brandenberger, G.; Buchheit, M.; Ehrhart, J.; Simon, C.; Piquard, F. Is slow wave sleep an appropriate recording condition for heart rate variability analysis? Auton. Neurosci. 2005, 121, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Mejía-Mejía, E.; Budidha, K.; Abay, T.Y.; May, J.M.; Kyriacou, P.A. Heart Rate Variability (HRV) and Pulse Rate Variability (PRV) for the Assessment of Autonomic Responses. Front. Physiol. 2020, 11, 779. [Google Scholar] [CrossRef] [PubMed]
- Shaffer, F.; Ginsberg, J.P. An Overview of Heart Rate Variability Metrics and Norms. Front. Public Health 2017, 5, 258. [Google Scholar] [CrossRef] [PubMed]
- Gellish, R.L.; Goslin, B.R.; Olson, R.E.; McDonald, A.; Russi, G.D.; Moudgil, V.K. Longitudinal modeling of the relationship between age and maximal heart rate. Med. Sci. Sports Exerc. 2007, 39, 822–829. [Google Scholar] [CrossRef]
- Grosicki, G.J.; Kim, J.; Fielding, F.; Jasinski, S.R.; Chapman, C.; Hippel, W.V.; Holmes, K.E. Heart and health behavior responses to GLP-1 receptor agonists: A 12-wk study using wearable technology and causal inference. Am. J. Physiol. Heart Circ. Physiol. 2025, 328, H235–H241. [Google Scholar] [CrossRef]
- Holmes, K.E.; Fox, N.; King, J.; Presby, D.M.; Kim, J. Connection Between Sleep and Psychological Well-Being in U.S. Army Soldiers. Mil. Med. 2024, 189, e40–e48. [Google Scholar] [CrossRef]
- Miller, D.J.; Sargent, C.; Roach, G.D. A Validation of Six Wearable Devices for Estimating Sleep, Heart Rate and Heart Rate Variability in Healthy Adults. Sensors 2022, 22, 6317. [Google Scholar] [CrossRef]
- Miller, D.J.; Lastella, M.; Scanlan, A.T.; Bellenger, C.; Halson, S.L.; Roach, G.D.; Sargent, C. A validation study of the WHOOP strap against polysomnography to assess sleep. J. Sports Sci. 2020, 38, 2631–2636. [Google Scholar] [CrossRef]
- WHO Guidelines on Physical Activity and Sedentary Behaviour; WHO: Geneva, Switzerland, 2020.
- Chen, X.J.; Barywani, S.B.; Hansson, P.O.; Östgärd Thunström, E.; Rosengren, A.; Ergatoudes, C.; Mandalenakis, Z.; Caidahl, K.; Fu, M.L. Impact of changes in heart rate with age on all-cause death and cardiovascular events in 50-year-old men from the general population. Open Heart 2019, 6, e000856. [Google Scholar] [CrossRef]
- Jin, Q.; Yang, N.; Dai, J.; Zhao, Y.; Zhang, X.; Yin, J.; Yan, Y. Association of Sleep Duration With All-Cause and Cardiovascular Mortality: A Prospective Cohort Study. Front. Public Health 2022, 10, 880276. [Google Scholar] [CrossRef] [PubMed]
- Windred, D.P.; Burns, A.C.; Lane, J.M.; Saxena, R.; Rutter, M.K.; Cain, S.W.; Phillips, A.J.K. Sleep regularity is a stronger predictor of mortality risk than sleep duration: A prospective cohort study. Sleep 2024, 47, zsad253. [Google Scholar] [CrossRef] [PubMed]
- Hoopes, E.K.; Berube, F.R.; D’Agata, M.N.; Patterson, F.; Farquhar, W.B.; Edwards, D.G.; Witman, M.A.H. Sleep duration regularity, but not sleep duration, is associated with microvascular function in college students. Sleep 2021, 44, zsaa175. [Google Scholar] [CrossRef] [PubMed]
- Lloyd-Jones, D.M.; Allen, N.B.; Anderson, C.A.M.; Black, T.; Brewer, L.C.; Foraker, R.E.; Grandner, M.A.; Lavretsky, H.; Perak, A.M.; Sharma, G.; et al. Life’s Essential 8: Updating and Enhancing the American Heart Association’s Construct of Cardiovascular Health: A Presidential Advisory From the American Heart Association. Circulation 2022, 146, e18–e43. [Google Scholar] [CrossRef]
- Ferguson, T.; Olds, T.; Curtis, R.; Blake, H.; Crozier, A.J.; Dankiw, K.; Dumuid, D.; Kasai, D.; O’Connor, E.; Virgara, R.; et al. Effectiveness of wearable activity trackers to increase physical activity and improve health: A systematic review of systematic reviews and meta-analyses. Lancet Digit. Health 2022, 4, e615–e626. [Google Scholar] [CrossRef]
- Reimers, A.K.; Knapp, G.; Reimers, C.D. Effects of Exercise on the Resting Heart Rate: A Systematic Review and Meta-Analysis of Interventional Studies. J. Clin. Med. 2018, 7, 503. [Google Scholar] [CrossRef]
- Eser, P.; Jaeger, E.; Marcin, T.; Herzig, D.; Trachsel, L.D.; Wilhelm, M. Acute and chronic effects of high-intensity interval and moderate-intensity continuous exercise on heart rate and its variability after recent myocardial infarction: A randomized controlled trial. Ann. Phys. Rehabil. Med. 2022, 65, 101444. [Google Scholar] [CrossRef]
- Bouton, M.E. Why behavior change is difficult to sustain. Prev. Med. 2014, 68, 29–36. [Google Scholar] [CrossRef]
- Wong, J.S.; Lu, W.A.; Wu, K.T.; Liu, M.; Chen, G.Y.; Kuo, C.D. A comparative study of pulse rate variability and heart rate variability in healthy subjects. J. Clin. Monit. Comput. 2012, 26, 107–114. [Google Scholar] [CrossRef]



| <5 Days/Week | 5 Days/Week | 6 Days/Week | Worn Every Day | |
|---|---|---|---|---|
| Descriptives | ||||
| Criteria (days/week) | <5 | 5.0–5.99 | 6.0–6.99 | 7.0 |
| Weekday percentage (%) | 73.77 ± 22.84 * | 72.74 ± 14.58 * | 71.74 ± 6.56 * | 71.30 ± 1.71 * |
| Number of members (n) | 677 | 1316 | 5570 | 4351 |
| Percent male (%) | 45.9 | 47.4 | 50.9 * | 50.2 * |
| Age (yrs) | 31.83 ± 11.02 | 31.59 ± 10.82 | 32.76 ± 10.97 ^ | 33.47 ± 11.06 * |
| BMI (kg/m2) | 25.62 ± 4.91 | 25.67 ± 5.10 | 25.49 ± 4.84 | 25.27 ± 4.59 ^ |
| Baseline Biometrics | ||||
| Resting heart rate (bpm) | 64.09 ± 9.48 | 63.44 ± 9.19 | 61.80 ± 9.00 * | 60.47 ± 8.63 * |
| Heart rate variability (ms) | 56.52 ± 27.73 | 56.36 ± 28.44 | 57.02 ± 28.70 | 58.08 ± 29.58 |
| Baseline Sleep Characteristics | ||||
| Sleep duration (hrs) | 6.18 ± 1.38 * | 6.44 ± 1.26 * | 6.58 ± 1.13 * | 6.79 ± 1.04 * |
| Sleep consistency (%) | 57.74 ± 15.66 * | 60.69 ± 15.68 * | 64.34 ± 14.18 * | 69.10 ± 11.9 * |
| Baseline Physical Activity Variables | ||||
| Total weekly activity (min) | 151.1 ± 197.5 * | 175.3 ± 197.9 * | 207.4 ± 210.6 * | 237.5 ± 213.5 * |
| Daily activity (min) | 28.21 ± 36.00 * | 30.42 ± 34.25 * | 34.49 ± 34.95 * | 38.37 ± 34.55 * |
| Predictor | β | 95% CI | p-Value |
|---|---|---|---|
| RHR | |||
| Intercept | 9.467 | [8.787, 10.147] | <0.001 |
| Sex [T.Male] | −0.620 | [−0.724, −0.515] | <0.001 |
| Time (Weeks) | 0.144 | [0.071, 0.216] | <0.001 |
| Average Days Worn (Between-Person) | −0.441 | [−0.515, −0.368] | <0.001 |
| Time × Average Days Worn | −0.018 | [−0.029, −0.007] | 0.001 |
| Person-Mean Days Worn (Within-Person) | −0.369 | [−0.391, −0.347] | <0.001 |
| Baseline RHR | 0.896 | [0.890, 0.902] | <0.001 |
| Age | 0.006 | [0.002, 0.011] | 0.005 |
| BMI | 0.030 | [0.019, 0.041] | <0.001 |
| Season [T.Spring] | 0.074 | [−0.013, 0.161] | 0.094 |
| Season [T.Summer] | −0.139 | [−0.218, −0.061] | <0.001 |
| Season [T.Winter] | 0.226 | [0.149, 0.302] | <0.001 |
| Weekday Percentage | −0.014 | [−0.016, −0.012] | <0.001 |
| HRV | |||
| Intercept | 3.251 | [1.737, 4.765] | <0.001 |
| Sex [T.Male] | 0.345 | [0.089, 0.601] | 0.008 |
| Time (Weeks) | −0.032 | [−0.213, 0.148] | 0.727 |
| Average Days Worn (Between-Person) | 0.289 | [0.108, 0.471] | 0.002 |
| Time × Average Days Worn | 0.002 | [−0.026, 0.029] | 0.902 |
| Person-Mean Days Worn (Within-Person) | 0.252 | [0.201, 0.303] | <0.001 |
| Baseline HRV | 0.934 | [0.929, 0.939] | <0.001 |
| Age | −0.085 | [−0.097, −0.072] | <0.001 |
| BMI | 0.011 | [−0.016, 0.038] | 0.409 |
| Season [T.Spring] | −0.215 | [−0.425, −0.004] | 0.046 |
| Season [T.Summer] | 0.469 | [0.278, 0.661] | <0.001 |
| Season [T.Winter] | −0.436 | [−0.621, −0.251] | <0.001 |
| Weekday Percentage | 0.018 | [0.012, 0.023] | <0.001 |
| Predictor | β | 95% CI | p-Value |
|---|---|---|---|
| Sleep Duration | |||
| Intercept | 2.425 | [2.299, 2.551] | <0.0001 |
| Sex [T.Male] | −0.134 | [−0.153, −0.116] | <0.001 |
| Time (Weeks) | 0.000 | [−0.013, 0.013] | 0.956 |
| Average Days Worn (Between-Person) | 0.111 | [0.097, 0.126] | <0.001 |
| Time × Average Days Worn | −0.000 | [−0.002, 0.002] | 0.920 |
| Person-Mean Days Worn (Within-Person) | 0.050 | [0.045, 0.055] | <0.001 |
| Baseline Sleep Duration | 0.590 | [0.581, 0.598] | <0.001 |
| Age | −0.004 | [−0.004, −0.003] | <0.001 |
| BMI | −0.009 | [−0.011, −0.007] | <0.001 |
| Season [T.Spring] | −0.005 | [−0.022, 0.012] | 0.577 |
| Season [T.Summer] | −0.010 | [−0.025, 0.006] | 0.230 |
| Season [T.Winter] | 0.033 | [0.017, 0.048] | <0.001 |
| Weekday Percentage | −0.000 | [−0.001, 0.000] | 0.759 |
| Sleep Consistency | |||
| Intercept | 2.835 | [1.168, 4.502] | 0.001 |
| Sex [T.Male] | −0.676 | [−0.902, −0.449] | <0.001 |
| Time (Weeks) | 0.288 | [0.080, 0.497] | 0.007 |
| Average Days Worn (Between-Person) | 2.036 | [1.823, 2.250] | <0.001 |
| Time × Average Days Worn | −0.051 | [−0.083, −0.019] | 0.002 |
| Person-Mean Days Worn (Within-Person) | 1.144 | [1.074, 1.214] | <0.001 |
| Baseline Sleep Consistency | 0.674 | [0.665, 0.682] | <0.001 |
| Age | 0.074 | [0.064, 0.084] | <0.001 |
| BMI | −0.084 | [−0.108, −0.060] | <0.001 |
| Season [T.Spring] | 0.087 | [−0.137, 0.311] | 0.446 |
| Season [T.Summer] | 0.007 | [−0.194, 0.207] | 0.949 |
| Season [T.Winter] | −0.006 | [−0.207, 0.195] | 0.955 |
| Weekday Percentage | 0.066 | [0.059, 0.074] | <0.001 |
| Predictor | β | 95% CI | p-Value |
|---|---|---|---|
| Total Weekly Activity Minutes | |||
| Intercept | −80.035 | [−102.882, 57.188] | <0.001 |
| Sex [T.Male] | 6.938 | [3.093, 10.784] | <0.001 |
| Time (Weeks) | 3.471 | [0.852, 6.089] | 0.009 |
| Average Days Worn (Between-Person) | 33.944 | [31.009, 36.880] | <0.001 |
| Time × Average Days Worn | −1.121 | [−1.522, −0.719] | <0.001 |
| Person-Mean Days Worn (Within-Person) | 26.183 | [25.386, 26.979] | <0.001 |
| Baseline Weekly Activity Minutes | 0.695 | [0.685, 0.705] | <0.001 |
| Age | −0.055 | [−0.228, 0.119] | 0.539 |
| BMI | −2.422 | [−2.829, −2.016] | <0.001 |
| Season [T.Spring] | −3.832 | [−7.143, −0.520] | 0.023 |
| Season [T.Summer] | 0.991 | [−2.022, 4.003] | 0.519 |
| Season [T.Winter] | −34.438 | [−37.341, −31.535] | <0.001 |
| Weekday Percentage | −0.057 | [−0.141, 0.027] | 0.185 |
| Daily Activity Minutes | |||
| Intercept | 2.626 | [−1.944, 7.195] | 0.260 |
| Sex [Male] | 1.310 | [0.633, 1.986] | <0.001 |
| Time (Weeks) | 0.632 | [0.186, 1.077] | 0.005 |
| Average Days Worn (Between-Person) | 3.525 | [2.909, 4.140] | <0.001 |
| Time × Average Days Worn | −0.169 | [−0.238, −0.101] | <0.001 |
| Person-Mean Days Worn (Within-Person) | 1.007 | [0.876, 1.137] | <0.001 |
| Baseline Daily Activity Minutes | 0.527 | [0.517, 0.537] | <0.001 |
| Age | 0.000 | [−0.031, 0.031] | 1.000 |
| BMI | −0.467 | [−0.538, −0.396] | <0.001 |
| Season [T.Spring] | 0.183 | [−0.385, 0.750] | 0.528 |
| Season [T.Summer] | 1.149 | [0.638, 1.660] | <0.001 |
| Season [T.Winter] | −5.088 | [−5.573, −4.602] | <0.001 |
| Weekday Percentage | −0.006 | [−0.019, 0.008] | 0.401 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grosicki, G.J.; Fielding, F.; Kim, J.; Chapman, C.J.; Olaru, M.; Hippel, W.v.; Holmes, K.E. Wearing WHOOP More Frequently Is Associated with Better Biometrics and Healthier Sleep and Activity Patterns. Sensors 2025, 25, 2437. https://doi.org/10.3390/s25082437
Grosicki GJ, Fielding F, Kim J, Chapman CJ, Olaru M, Hippel Wv, Holmes KE. Wearing WHOOP More Frequently Is Associated with Better Biometrics and Healthier Sleep and Activity Patterns. Sensors. 2025; 25(8):2437. https://doi.org/10.3390/s25082437
Chicago/Turabian StyleGrosicki, Gregory J., Finnbarr Fielding, Jeongeun Kim, Christopher J. Chapman, Maria Olaru, William von Hippel, and Kristen E. Holmes. 2025. "Wearing WHOOP More Frequently Is Associated with Better Biometrics and Healthier Sleep and Activity Patterns" Sensors 25, no. 8: 2437. https://doi.org/10.3390/s25082437
APA StyleGrosicki, G. J., Fielding, F., Kim, J., Chapman, C. J., Olaru, M., Hippel, W. v., & Holmes, K. E. (2025). Wearing WHOOP More Frequently Is Associated with Better Biometrics and Healthier Sleep and Activity Patterns. Sensors, 25(8), 2437. https://doi.org/10.3390/s25082437






