Dose Response of Bumetanide on Aquaporins and Angiogenesis Biomarkers in Human Retinal Endothelial Cells Exposed to Intermittent Hypoxia
Abstract
:1. Introduction
2. Results
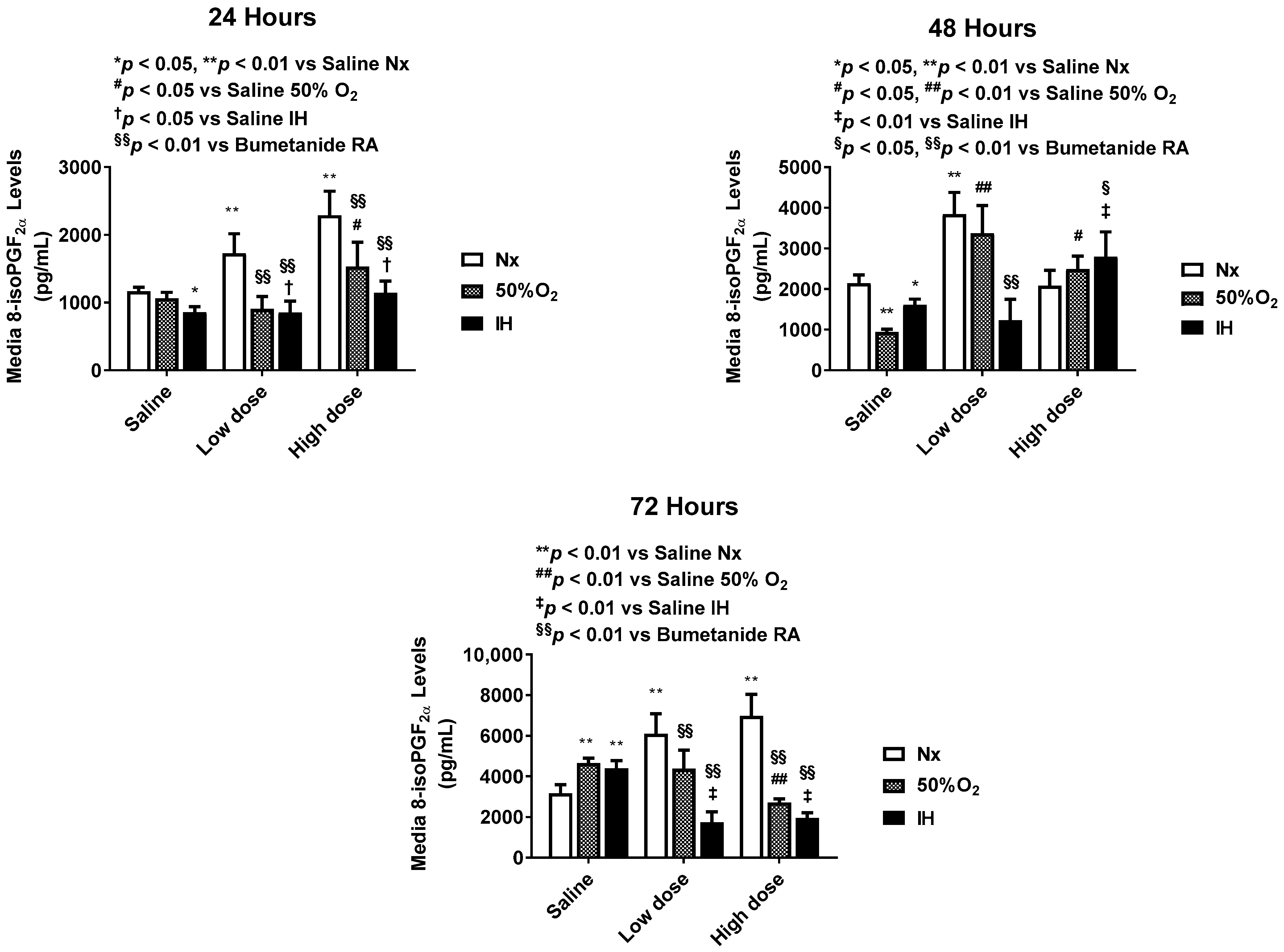
2.1. Effect of Bumetanide on Oxidative Stress
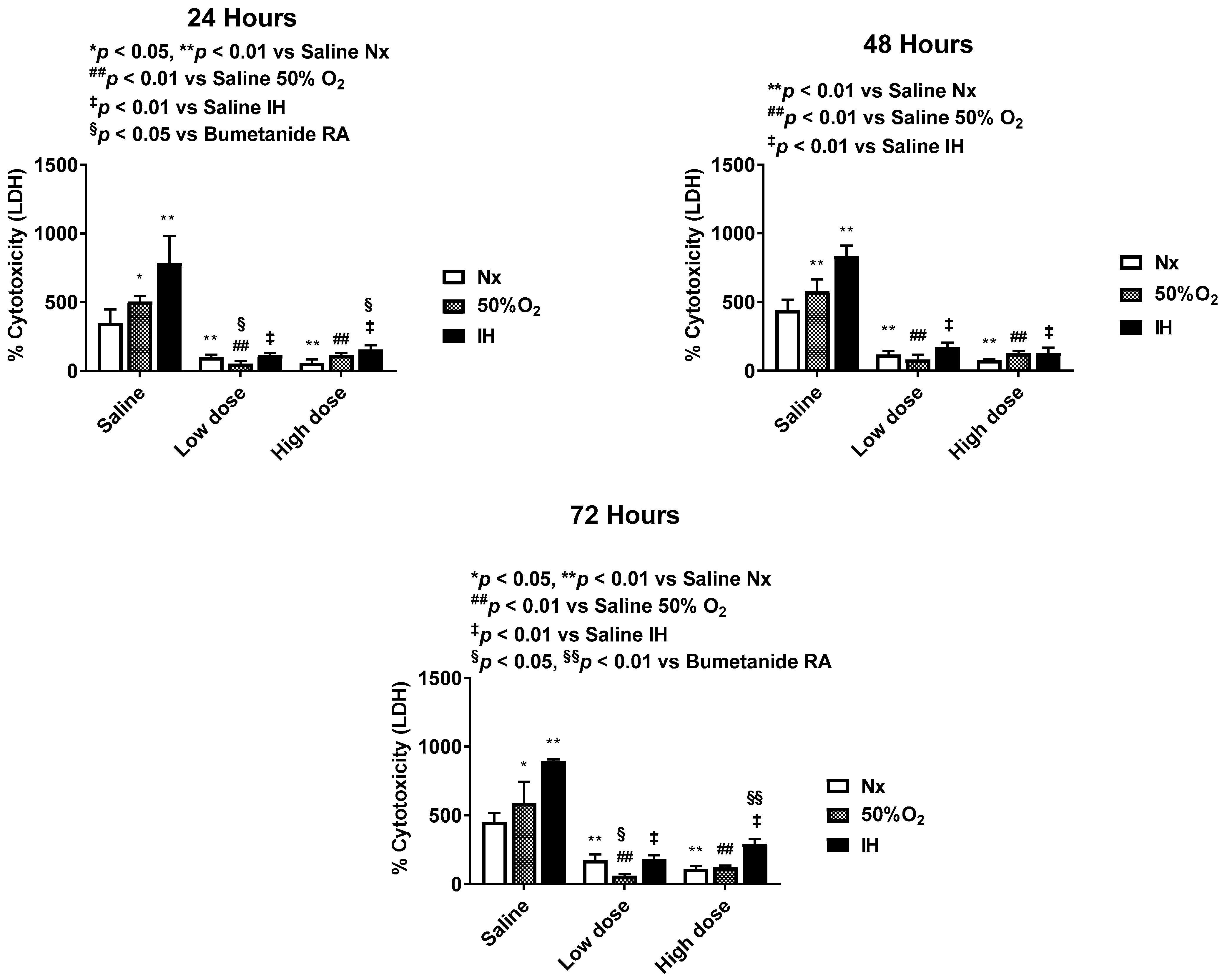
2.2. Effect of Bumetanide on Percentage (%) Cytotoxicity
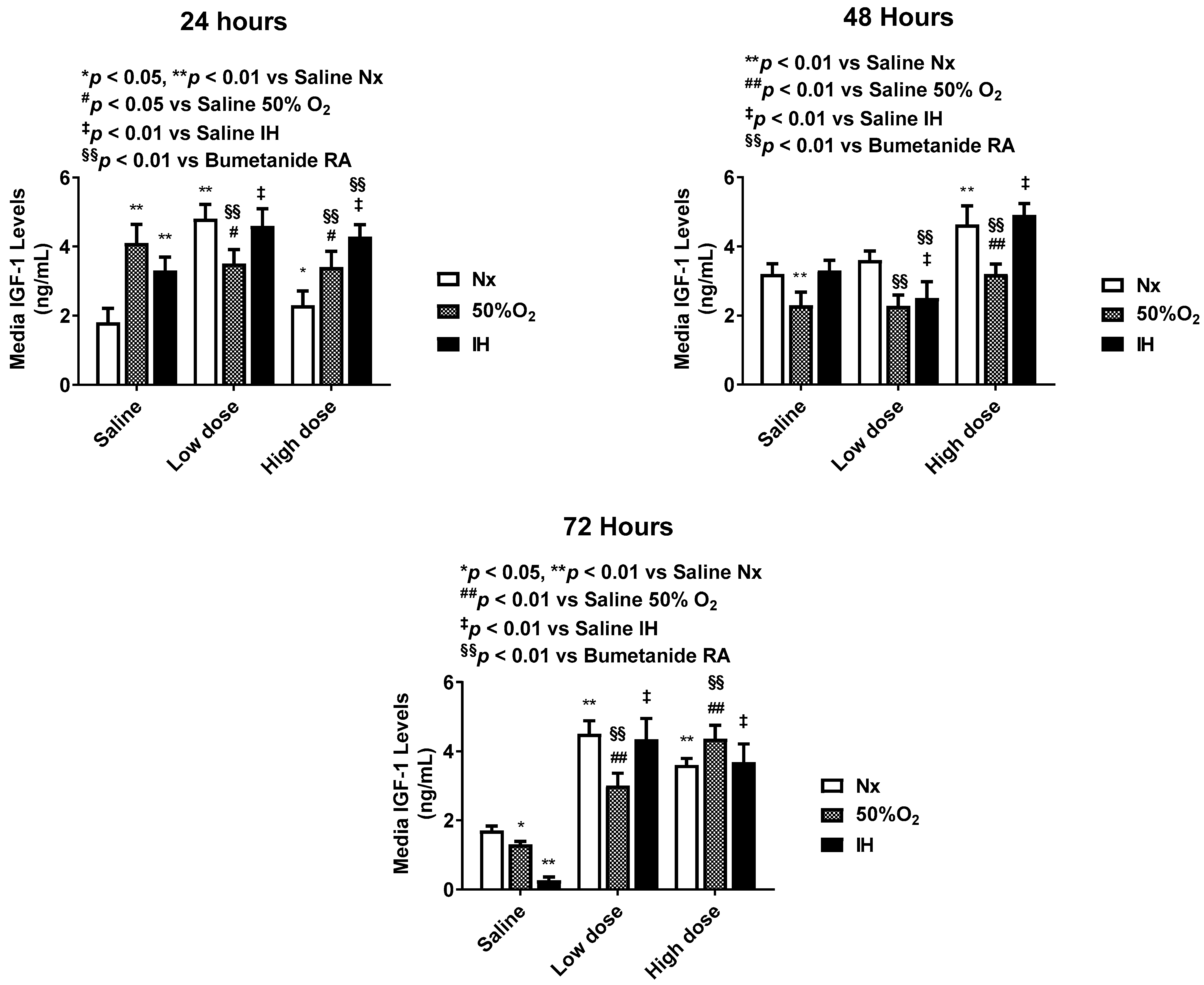
2.3. Effect of Bumetanide on Angiogenesis
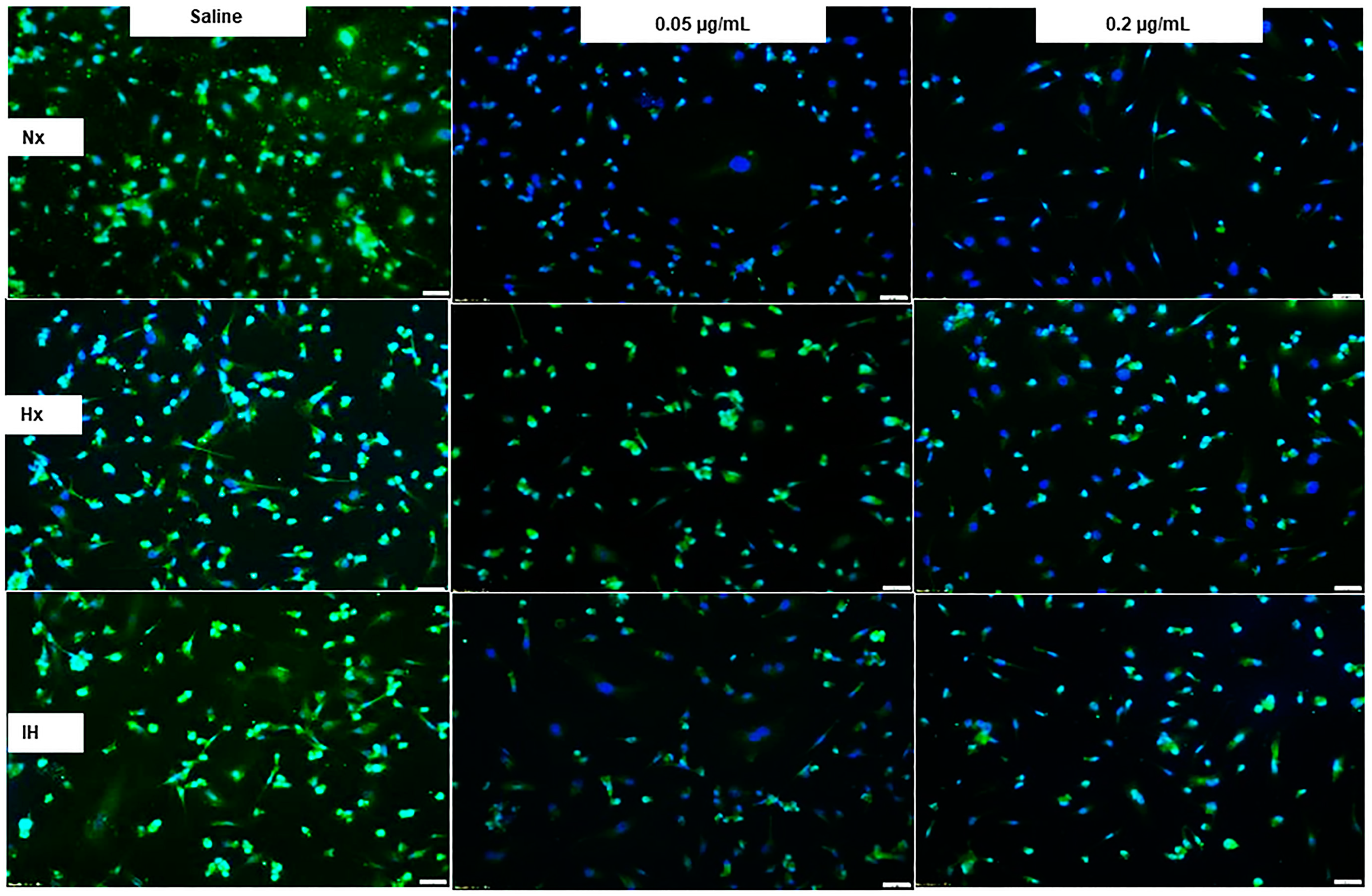
2.4. Effect of Bumetanide on AQP Immunoreactivity
2.5. Effects of Bumetanide on Tube Formation Capacity
2.6. Quantitative Analysis
2.7. Effect of Bumetanide on AQP Gene Expression in HMRECs
3. Discussion
4. Materials and Methods
4.1. Cells
4.2. Experimental Design
4.3. Hx and IH Profiles
4.4. Assay of 8-isoPGF2α
4.5. Assay of Cytotoxicity
4.6. Assay of Angiogenesis Biomarkers
4.7. Tube Formation Assay
4.8. Immunoreactivity Assays
4.9. Real Time PCR
4.10. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gilbert, C.; Foster, A. Childhood blindness in the context of VISION 2020-The Right to Sight. Bull. World Health Organ. 2001, 79, 227–232. [Google Scholar] [PubMed]
- Sharma, M.; Vanderveen, D.K. Identification and Treatment of Retinopathy of Prematurity: Update. NeoReviews 2017, 18, e84–e90. [Google Scholar] [CrossRef] [Green Version]
- News NIH, National Eye Institute. Early Treatment of Blinding Eye Disease in Infants Can Prevent Severe Vision Loss. Available online: www.nei.nih.gov/rop (accessed on 8 December 2003).
- Chen, J.; Smith, L.E. Retinopathy of prematurity. Angiogenesis 2007, 10, 133–140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heidary, G.; Vanderveen, D.; Smith, L.E. Retinopathy of prematurity: Current concepts in molecular pathogenesis. Semin. Ophthalmol. 2009, 24, 77–81. [Google Scholar] [CrossRef]
- Stone, J.; Itin, A.; Alon, T.; Pe’er, J.; Gnessin, H.; Chan-Ling, T.; Keshet, E. Development of retinal vasculature is mediated by hypoxia-induced vascular endothelial growth factor (VEGF) expression by neuroglia. J. Neurosci. 1995, 15, 4738–4747. [Google Scholar] [CrossRef] [PubMed]
- Silva, R.A.; Moshfeghi, D.M. Interventions in retinopathy of prematurity. NeoReviews 2012, 13, e476–e485. [Google Scholar] [CrossRef]
- Raghuveer, T.S.; Zackula, R. Strategies to prevent severe retinopathy of prematurity. NeoReviews 2020, 21, e249–e263. [Google Scholar] [CrossRef] [PubMed]
- Blumenkranz, M. Optimal current and future treatments for diabetic macular oedema. Eye 2010, 24, 428–434. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, Q.; Gillies, M.; Wong, T. Management of diabetic retinopathy: A systematic review. JAMA 2007, 298, 902–916. [Google Scholar] [CrossRef] [Green Version]
- Nicolò, M.; Ghiglione, D.; Calabria, G. Retinal pigment epithelial tear following intravitreal injection of bevacizumab (Avastin). Eur. J. Ophthalmol. 2006, 16, 770–773. [Google Scholar] [CrossRef]
- Shah, C.P.; Hsu, J.; Garg, S.J.; Fischer, D.H.; Kaiser, R. Retinal pigment epithelial tear after intravitreal bevacizumab injection. Am. J. Ophthalmol. 2006, 142, 1070–1072. [Google Scholar] [CrossRef] [PubMed]
- Morin, J.; Luu, T.M.; Superstein, R.; Ospina, L.H.; Lefebvre, F.; Simard, M.N.; Shah, V.; Shah, P.S.; Kelly, E.N. Canadian Neonatal Network and the Canadian Neonatal Follow-Up Network Investigators. Neurodevelopmental outcomes following bevacizumab injections for retinopathy of prematurity. Pediatrics 2016, 137, e20153218. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suk, K.K.; Berrocal, A.M.; Murray, T.G.; Rich, R.; Major, J.C.; Hess, D.; Johnson, R.A. Retinal detachment despite aggressive management of aggressive posterior retinopathy of prematurity. J. Pediatr. Ophthalmol. Strabismus 2010, 47, e1–e4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, J.; Blair, M.P.; Shapiro, M.J.; Lichtenstein, S.J.; Galasso, J.M.; Kapur, R. Reactivation of retinopathy of prematurity after bevacizumab injection. Arch. Ophthalmol. 2012, 130, 1000–1006. [Google Scholar] [CrossRef] [PubMed]
- Karaca, C.; Oner, A.O.; Mirza, E.; Polat, O.A.; Sahiner, M. Bilateral effect of unilateral bevacizumab injection in retinopathy of prematurity. JAMA Ophthalmol. 2013, 131, 1099–1101. [Google Scholar] [CrossRef] [PubMed]
- Andreoli, C.M.; Miller, J.W. Anti-vascular endothelial growth factor therapy for ocular neovascular disease. Curr. Opin. Ophthalmol. 2007, 18, 502–508. [Google Scholar] [CrossRef]
- Byeon, S.H.; Lee, S.C.; Choi, S.H.; Lee, H.K.; Lee, J.H.; Chu, Y.K.; Kwon, O.W. Vascular endothelial growth factor as an autocrine survival factor for retinal pigment epithelial cells under oxidative stress via the VEGF-R2/PI3K/Akt. Investig. Ophthalmol. Vis. Sci. 2010, 51, 1190–1197. [Google Scholar] [CrossRef] [Green Version]
- Inan, U.U.; Avci, B.; Kusbeci, T.; Kaderli, B.; Avci, R.; Temel, S.G. Preclinical safety evaluation of intravitreal injection of full-length humanized vascular endothelial growth factor antibody in rabbit eyes. Investig. Ophthalmol. Vis. Sci. 2007, 48, 1773–1781. [Google Scholar] [CrossRef] [Green Version]
- Aiello, L.P. Targeting intraocular neovascularization and edema—One drop at a time. N. Engl. J. Med. 2008, 359, 967–969. [Google Scholar] [CrossRef] [Green Version]
- Nishijima, K.; Ng, Y.S.; Zhong, L.; Bradley, J.; Schubert, W.; Jo, N.; Akita, J.; Samuelsson, S.J.; Robinson, G.S.; Adamis, A.P.; et al. Vascular endothelial growth factor-A is a survival factor for retinal neurons and a critical neuroprotectant during the adaptive response to ischemic injury. Am. J. Pathol. 2007, 171, 53–67. [Google Scholar] [CrossRef] [Green Version]
- Saint-Geniez, M.; Kurihara, T.; Sekiyama, E.; Maldonado, A.E.; D’Amore, P.A. An essential role for RPE-derived soluble VEGF in the maintenance of the choriocapillaris. Proc. Natl. Acad. Sci. USA 2009, 106, 18751–18756. [Google Scholar] [CrossRef] [Green Version]
- Saint-Geniez, M.; Maharaj, A.S.; Walshe, T.E.; Tucker, B.A.; Sekiyama, E.; Kurihara, T.; Darland, D.C.; Young, M.J.; D’Amore, P.A. Endogenous VEGF is required for visual function: Evidence for a survival role on müller cells and photoreceptors. PLoS ONE 2008, 3, e3554. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tan, J.; Cai, C.; Shrier, E.; McNally, L.; Lazzaro, D.; Aranda, J.V.; Beharry, K.D. Ocular adverse effects of intravitreal bevacizumab are potentiated by intermittent hypoxia in a rat model of oxygen-induced retinopathy. J. Ophthalmol. 2017, 2017, 4353129. [Google Scholar] [CrossRef] [PubMed]
- Valencia, A.M.; Cai, C.; Tan, J.; Duggan, T.; Valencia, G.B.; Aranda, J.V.; Beharry, K.D. Intravitreal Bevacizumab Alters Type IV Collagenases and Exacerbates Arrested Alveologenesis in the Neonatal Rat Lungs. Exp. Lung Res. 2017, 43, 120–133. [Google Scholar] [CrossRef]
- Papadopoulos, M.C.; Saadoun, S.; Verkman, A.S. Aquaporins and Cell Migration. Pflugers Arch. 2008, 456, 693–700. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patil, R.; Wang, H.; Sharif, N.A.; Mitra, A. Aquaporins: Novel Targets for Age-Related Ocular Disorders. J. Ocul. Pharmacol. Ther. 2018, 34, 177–187. [Google Scholar] [CrossRef] [PubMed]
- Schey, K.L.; Wang, Z.L.; Wenke, J.; Qi, Y. Aquaporins in the eye: Expression, function, and roles in ocular disease. Biochim. Biophys. Acta 2014, 1840, 1513–1523. [Google Scholar] [CrossRef] [Green Version]
- Verkman, A.S. Aquaporins in endothelia. Kidney Int. 2006, 69, 1120–1123. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bringmann, A.; Uckermann, O.; Pannicke, T.; Iandiev, I.; Reichenbach, A.; Wiedemann, P. Neuronal versus glial cell swelling in the ischaemic retina. Acta Ophthalmol. Scand. 2005, 83, 528–538. [Google Scholar] [CrossRef]
- Russell, J.M. Sodium-potassium-chloride cotransport. Physiol. Rev. 2000, 80, 211–276. [Google Scholar] [CrossRef]
- Sullivan, J.E.; Witte, M.K.; Yamashita, T.S.; Myers, C.M.; Blumer, J.L. Pharmacokinetics of bumetanide in critically ill infants. Clin. Pharmacol. Ther. 1996, 60, 405–413. [Google Scholar] [CrossRef]
- Pressler, R.M.; Boylan, G.B.; Marlow, N.; Blennow, M.; Chiron, C.; Cross, J.H.; de Vries, L.S.; Hallberg, B.; Hellström-Westas, L.; Jullien, V.; et al. Bumetanide for the treatment of seizures in newborn babies with hypoxic ischaemic encephalopathy (NEMO): An open-label, dose finding, and feasibility phase 1/2 trial. Lancet Neurol. 2015, 14, 469–477. [Google Scholar] [CrossRef]
- Zhang, L.L.; Pathak, H.R.; Coulterm, D.A.; Freed, M.A.; Vardi, N. Shift of intracellular chloride concentration in ganglion and amacrine cells of developing mouse retina. J. Neurophysiol. 2006, 95, 2404–2416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Migliati, E.; Meurice, N.; DuBois, P.; Fang, J.S.; Somasekharan, S.; Beckett, E.; Flynn, G.; Yool, A.J. Inhibition of aquaporin-1 and aquaporin-4 water permeability by a derivative of the loop diuretic bumetanide acting at an internal pore-occluding binding site. Mol. Pharmacol. 2009, 76, 105–112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yan, X.; Liu, J.; Wang, X.; Li, W.; Chen, J.; Sun, H. Pretreatment with AQP4 and NKCC1 Inhibitors Concurrently Attenuated Spinal Cord Edema and Tissue Damage after Spinal Cord Injury in Rats. Front. Physiol. 2018, 9, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malamas, A.S.; Jin, E.; Zhang, Q.; Haaga, J.; Lu, Z.R. Anti-angiogenic effects of bumetanide revealed by DCE-MRI with a biodegradable macromolecular contrast agent in a colon cancer model. Pharm. Res. 2015, 32, 3029–3043. [Google Scholar] [CrossRef] [Green Version]
- Guzel, S.; Cai, C.; Taimur, A.; Quan, M.; Valencia, G.B.; Aranda, J.V.; Beharry, K.D. Bumetanide suppression of angiogenesis in a rat model of oxygen-induced retinopathy. Int. J. Mol. Sci. 2020, 21, 987. [Google Scholar] [CrossRef] [Green Version]
- Di Fiore, J.M.; Vento, M. Intermittent hypoxemia and oxidative stress in preterm infants. Respir. Physiol. Neurobiol. 2019, 266, 121–129. [Google Scholar] [CrossRef]
- Di Fiore, J.M.; Bloom, J.N.; Orge, F.; Schutt, A.; Schluchter, M.; Cheruvu, V.K.; Walsh, M.; Finer, N.; Martin, R.J. A higher incidence of intermittent hypoxemic episodes is associated with severe retinopathy of prematurity. J. Pediatr. 2010, 157, 69–73. [Google Scholar] [CrossRef] [Green Version]
- Di Fiore, J.M.; Kaffashi, F.; Loparo, K.; Sattar, A.; Schluchter, M.; Foglyano, R.; Martin, R.J.; Wilson, C.G. The relationship between patterns of intermittent hypoxia and retinopathy of prematurity in preterm infants. Pediatr. Res. 2012, 72, 606–612. [Google Scholar] [CrossRef] [Green Version]
- Poets, C.F.; Roberts, R.S.; Schmidt, B.; Whyte, R.K.; Asztalos, E.V.; Bader, D.; Bairam, A.; Moddemann, D.; Peliowski, A.; Rabi, Y.; et al. Association Between Intermittent Hypoxemia or Bradycardia and Late Death or Disability in Extremely Preterm Infants. JAMA 2015, 14, 595–603. [Google Scholar] [CrossRef] [PubMed]
- Perrone, S.; Laschi, E.; Buonocore, G. Oxidative stress biomarkers in the perinatal period: Diagnostic and prognostic value. Semin. Fetal Neonatal Med. 2020, 25, 101087. [Google Scholar] [CrossRef] [PubMed]
- Milne, G.L.; Morrow, J.D. Isoprostanes and related compounds: Update 2006. Antioxid. Redox Signal. 2006, 8, 1379–1384. [Google Scholar] [CrossRef]
- Morrow, J.D. The isoprostanes-unique products of arachidonate peroxidation: Their role as mediators of oxidant stress. Curr. Pharm. Des. 2006, 12, 895–902. [Google Scholar] [CrossRef]
- Milne, G.L.; Yin, H.; Brooks, J.D.; Sanchez, S.; Roberts, L.J., 2nd; Morrow, J.D. Quantification of F2isoprostanes in biological fluids and tissues as a measure of oxidant stress. Methods Enzymol. 2007, 433, 113–126. [Google Scholar] [PubMed]
- Morrow, J.D.; Hill, K.E.; Burk, R.F.; Nammour, T.M.; Badr, K.F.; Roberts, L.J., 2nd. A series of prostaglandin F2-like compounds are produced in vivo in humans by a non-cyclooxygenase, free radical-catalyzed mechanism. Proc. Natl. Acad. Sci. USA 1990, 87, 9383–9387. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kadiiska, M.B.; Gladen, B.C.; Baird, D.D.; Graham, L.B.; Parker, C.E.; Ames, B.N.; Basu, S.; Fitzgerald, G.A.; Lawson, J.A.; Marnett, L.J.; et al. Biomarkers of oxidative stress study III. Effects of the nonsteroidal anti-inflammatory agents indomethacin and meclofenamic acid on measurements of oxidative products of lipids in CCl4 poisoning. Free Radic. Biol. Med. 2005, 38, 711–718. [Google Scholar] [CrossRef] [PubMed]
- Korzeniewski, C.; Callewaert, D. An enzyme-release assay for natural cytotoxicity. J. Immunol. Methods 1983, 64, 313–320. [Google Scholar] [CrossRef]
- Jacobs, E.; Hissin, P.J.; Propper, W.; Mayer, L.; Sarkozi, L. Stability of lactate dehydrogenase at different storage temperatures. Clin. Biochem. 1986, 19, 183–188. [Google Scholar] [CrossRef]
- Marklund, L.; Henriksson, R.; Grankvist, K. Amphotericin B-induced apoptosis and cytotoxicity is prevented by the Na+, K+, 2Cl(−)-cotransport blocker bumetanide. Life Sci. 2000, 66, PL319–PL324. [Google Scholar] [CrossRef]
- Jamieson, D.; Chance, B.; Cadenas, E.; Boveris, A. The relation of free radical production to hyperoxia. Annu. Rev. Physiol. 1986, 48, 703–719. [Google Scholar] [CrossRef] [PubMed]
- Beharry, K.D.; Cai, C.L.; Valencia, G.B.; Valencia, A.M.; Lazzaro, D.R.; Bany-Mohammed, F.; Aranda, J.V. Neonatal Intermittent hypoxia, Reactive Oxygen Species, and Oxygen-induced Retinopathy. React. Oxyg. Species (Apex.) 2017, 3, 12–25. [Google Scholar] [CrossRef] [PubMed]
- Haas, M. The Na–K–Cl cotransporters. Am. J. Physiol. 1994, 267, C869–C885. [Google Scholar] [CrossRef]
- Jayakumar, A.R.; Panickar, K.S.; Curtis, K.M.; Tong, X.Y.; Moriyama, M.; Norenberg, M.D. Na-K-Cl cotransporter-1 in the mechanism of cell swelling in cultured astrocytes after fluid percussion injury. J. Neurochem. 2011, 117, 437–448. [Google Scholar] [CrossRef] [PubMed]
- Panet, R.; Marcus, M.; Atlan, H. Overexpression of the Na(+)/K(+)/Cl(−) cotransporter gene induces cell proliferation and phenotypic transformation in mouse fibroblasts. J. Cell. Physiol. 2000, 182, 109–118. [Google Scholar] [CrossRef]
- Yan, Y.; Dempsey, R.J.; Flemmer, A.; Forbush, B.; Sun, D. Inhibition of Na(+)-K(+)-Cl(−) cotransporter during focal cerebral ischemia decreases edema and neuronal damage. Brain Res. 2003, 961, 22–31. [Google Scholar] [CrossRef]
- Verkman, A.S. Aquaporins water channels and endothelial function. J. Anat. 2002, 200, 617–627. [Google Scholar] [CrossRef] [PubMed]
- Galán-Cobo, A.; Ramírez-Lorca, R.; Echevarría, M. Role of aquaporins in cell proliferation: What else beyond water permeability? Channels 2016, 10, 185–201. [Google Scholar] [CrossRef] [Green Version]
- Echevarría, M.; Muñoz-Cabello, A.M.; Sánchez-Silva, R.; Toledo-Aral, J.J.; López-Barneo, J. Development of cytosolic hypoxia and hypoxia-inducible factor stabilization are facilitated by aquaporin-1 expression. J. Biol. Chem. 2007, 282, 30207–30215. [Google Scholar] [CrossRef] [Green Version]
- Ruiz-Ederra, J.; Verkman, A.S. Aquaporin-1 independent microvessel proliferation in a neonatal mouse model of oxygen-induced retinopathy. Investig. Ophthalmol. Vis. Sci. 2007, 48, 4802–4810. [Google Scholar] [CrossRef] [Green Version]
- Verkman, A.S. Aquaporins. Curr. Biol. 2013, 23, R52–R55. [Google Scholar] [CrossRef] [Green Version]
- Habela, C.W.; Ernest, N.J.; Swindall, A.F.; Sontheimer, H. Chloride accumulation drives volume dynamics underlying cell proliferation and migration. J. Neurophysiol. 2009, 101, 750–757. [Google Scholar] [CrossRef] [Green Version]
- Tomita, Y.; Palethorpe, H.M.; Smith, E.; Nakhjavani, M.; Townsend, A.R.; Price, T.J.; Yool, A.J.; Hardingham, J.E. Bumetanide-derived aquaporin 1 inhibitors, AqB013 and AqB050 inhibit tube formation of endothelial cells through induction of apoptosis and impaired migration in vitro. Int. J. Mol. Sci. 2019, 20, 1818. [Google Scholar] [CrossRef] [Green Version]
- Semenza, G.L. Hypoxia-inducable factor 1: Oxygen homeostasis and disease pathophysiology. Trends Mol. Med. 2001, 7, 345–350. [Google Scholar] [CrossRef]
- Gerber, H.P.; McMurtrey, A.; Kowalski, J.; Yan, M.; Keyt, B.A.; Dixit, V.; Ferrara, N. Vascular endothelial growth factor regulates endothelial cell survival through the phosphatidylinositol 3′-kinase/Akt signal transduction pathway. Requirement for Flk-1/KDR activation. J. Biol. Chem. 1998, 273, 30336–30343. [Google Scholar] [CrossRef] [Green Version]
- Wikenheiser, J.; Wolfram, J.A.; Gargesha, M.; Yang, K.; Karunamuni, G.; Wilson, D.L.; Semenza, G.L.; Agani, F.; Fisher, S.A.; Ward, N.; et al. Altered hypoxia-inducible factor-1 alpha expression levels correlate with coronary vessel anomalies. Dev. Dyn. 2009, 238, 2688–2700. [Google Scholar] [CrossRef] [Green Version]
- Terraneo, L.; Virgili, E.; Caretti, A.; Bianciardi, P.; Samaja, M. In vivo hyperoxia induces hypoxia-inducible factor-1α overexpression in LNCaP tumors without affecting the tumor growth rate. Int. J. Biochem. Cell Biol. 2014, 51, 65–74. [Google Scholar] [CrossRef]
- Laughner, E.; Taghavi, P.; Chiles, K.; Mahon, P.C.; Semenza, G.L. HER2 (neu) signaling increases the rate of hypoxia-inducible factor 1α (HIF-1α) synthesis: Novel mechanism for HIF- 1-mediated vascular endothelial growth factor expression. Mol. Cell. Biol. 2001, 21, 3995–4004. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dumont, D.J.; Fong, G.H.; Puri, M.C.; Gradwohl, G.; Alitalo, K.; Breitman, M.L. Vascularization of the mouse embryo: A study of flk-1, tek, tie, and vascular endothelial growth factor expression during development. Dev. Dyn. 1995, 203, 80–92. [Google Scholar] [CrossRef] [PubMed]
- Fong, G.H.; Rossant, J.; Gertsenstein, M.; Breitman, M.L. Role of the Flt-1 receptor tyrosine kinase in regulating the assembly of vascular endothelium. Nature 1995, 376, 66–70. [Google Scholar] [CrossRef] [PubMed]
- Shibuya, M. Vascular endothelial growth factor (VEGF) and its receptor (VEGFR) signaling in angiogenesis: A crucial target for anti- and pro-angiogenic therapies. Genes Cancer 2011, 2, 1097–1105. [Google Scholar] [CrossRef]
- Jakimiuk, A.J.; Nowicka, M.A.; Zagozda, M.; Koziol, K.; Lewandowski, P.; Issat, T. High levels of soluble vascular endothelial growth factor receptor1/SFLT1and low levels of vascular endothelial growth factor in follicular fluid on the day of oocyte retrieval correlate with ovarian hyperstimulation syndrome regardless of the stimulation protocol. J. Physiol. Pharmacol. 2017, 68, 477–484. [Google Scholar]
- Kendall, R.L.; Thomas, K.A. Inhibition of vascular endothelial cell growth factor activity by an endogenously encoded soluble receptor. Proc. Natl. Acad. Sci. USA 1993, 90, 10705–10709. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chappell, J.C.; Taylor, S.M.; Ferrara, N.; Bautch, V.L. Local guidance of emerging vessel sprouts requires soluble Flt-1. Dev. Cell 2009, 17, 377–386. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kearney, J.B.; Ambler, C.; Monaco, K.A.; Johnson, N.; Rapoport, R.G.; Bautch, V.L. Vascular endothelial growth factor receptor Flt-1 negatively regulates developmental blood vessel formation by modulating endothelial cell division. Blood 2002, 99, 2397–2407. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olmos, A.; Díaz, L.; Avila, E.; Barrera, D.; López-Marure, R.; Biruete, B.; Larrea, F.; Halhali, A. Associations between insulin-like growth factor I, vascular endothelial growth factor and its soluble receptor 1 in umbilical serum and endothelial cells obtained from normotensive and preeclamptic pregnancies. Growth Factors 2013, 31, 123–129. [Google Scholar] [CrossRef]
- Bou Khalil, R. Is insulin growth factor-1 the future for treating autism spectrum disorder and/or schizophrenia? Med. Hypotheses 2017, 99, 23–25. [Google Scholar] [CrossRef]
- Baroncelli, L.; Cenni, M.C.; Melani, R.; Deidda, G.; Landi, S.; Narducci, R.; Cancedda, L.; Maffei, L.; Berardi, N. Early IGF-1 primes visual cortex maturation and accelerates developmental switch between NKCC1 and KCC2 chloride transporters in enriched animals. Neuropharmacology 2017, 113 (Pt A), 167–177. [Google Scholar] [CrossRef]
- Nakao-Hayashi, J.; Ito, H.; Kanayasu, T.; Morita, I.; Murota, S. Stimulatory effects of insulin and insulin-like growth factor I on migration and tube formation by vascular endothelial cells. Atherosclerosis 1992, 92, 141–149. [Google Scholar] [CrossRef]
- Smith, L.E.; Kopchick, J.J.; Chen, W.; Knapp, J.; Kinose, F.; Daley, D.; Foley, E.; Smith, R.G.; Schaeffer, J.M. Essential role of growth hormone in ischemia-induced retinal neovascularization. Science 1997, 276, 1706–1709. [Google Scholar] [CrossRef]
- Rutkovskiy, A.; Bliksøen, M.; Hillestad, V.; Amin, M.; Czibik, G.; Valen, G.; Vaage, J.; Amiry-Moghaddam, M.; Stensløkken, K.O. Aquaporin-1 in cardiac endothelial cells is downregulated in ischemia, hypoxia and cardioplegia. J. Mol. Cell. Cardiol. 2013, 56, 22–33. [Google Scholar] [CrossRef]
- Au, C.G.; Cooper, S.T.; Lo, H.P.; Compton, A.G.; Yang, N.; Wintour, E.M.; North, K.N.; Winlaw, D.S. Expression of aquaporin 1 in human cardiac and skeletal muscle. J. Mol. Cell. Cardiol. 2004, 36, 655–662. [Google Scholar] [CrossRef] [PubMed]
- Saadoun, S.; Papadopoulos, M.C.; Davies, D.C.; Bell, B.A.; Krishna, S. Increased aquaporin 1 water channel expression in human brain tumours. Br. J. Cancer 2002, 87, 621–623. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dorward, H.S.; Du, A.; Bruhn, M.A.; Wrin, J.; Pei, J.V.; Evdokiou, A.; Price, T.J.; Yool, A.J.; Hardingham, J.E. Pharmacological blockade of aquaporin-1 water channel by AqB013 restricts migration and invasiveness of colon cancer cells and prevents endothelial tube formation in vitro. J. Exp. Clin. Cancer Res. 2016, 35, 36. [Google Scholar] [CrossRef] [Green Version]
- Nagelhus, E.A.; Ottersen, O.P. Physiological roles of aquaporin-4 in brain. Physiol. Rev. 2013, 93, 1543–1562. [Google Scholar] [CrossRef] [Green Version]
- Goodyear, M.J.; Crewther, S.G.; Junghans, B.M. A role for aquaporin-4 in fluid regulation in the inner retina. Vis. Neurosci. 2009, 26, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Tenckhoff, S.; Hollborn, M.; Kohen, L.; Wolf, S.; Wiedemann, P.; Bringmann, A. Diversity of aquaporin mRNA expressed by rat and human retinas. NeuroReport 2005, 16, 53–56. [Google Scholar] [CrossRef]
- Nagelhus, E.A.; Veruki, M.L.; Torp, R.; Haug, F.M.; Laake, J.H.; Nielsen, S.; Agre, P.; Ottersen, O.P. Aquaporin-4 water channel protein in the rat retina and optic nerve: Polarized expression in muller cells and fibrous astrocytes. J. Neurosci. 1998, 18, 2506–2519. [Google Scholar] [CrossRef]
- Kida, T.; Oku, H.; Horie, T.; Fukumoto, M.; Okuda, Y.; Morishita, S.; Ikeda, T. Implication of VEGF and aquaporin 4 mediating Müller cell swelling to diabetic retinal edema. Graefes Arch. Clin. Exp. Ophthalmol. 2017, 255, 1149–1157. [Google Scholar] [CrossRef]
- Pisani, F.; Cammalleri, M.; Dal Monte, M.; Locri, F.; Mola, M.G.; Nicchia, G.P.; Frigeri, A.; Bagnoli, P.; Svelto, M. Potential role of the methylation of VEGF gene promoter in response to hypoxia in oxygen-induced retinopathy: Beneficial effect of the absence of AQP4. J. Cell. Mol. Med. 2018, 22, 613–627. [Google Scholar] [CrossRef]
- Quan, M.; Cai, C.; Valencia, G.B.; Aranda, J.V.; Beharry, K.D. MnTBAP or catalase is more protective against oxidative stress in human retinal endothelial cells exposed to intermittent hypoxia than their co-administration (EUK-134). React. Oxygen Species 2017, 397, 47–65. [Google Scholar] [CrossRef] [Green Version]
- Coleman, R.J.; Beharry, K.D.; Brock, R.S.; Abad-Santos, P.; Abad-Santos, M.; Modanlou, H.D. Effects of brief clustered versus dispersed hypoxia episodes on systemic and ocular growth factors in a rat model of OIR. Pediatr. Res. 2008, 64, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Brock, R.S.; Gebrekristos, B.H.; Kuniyoshi, K.M.; Modanlou, H.D.; Falcao, M.C.; Beharry, K.D. Biomolecular effects of JB1 (an IGF-I peptide analog) in a rat model of oxygen-induced retinopathy. Pediatr. Res. 2011, 69, 35–41. [Google Scholar] [CrossRef] [Green Version]
- Beharry, K.D.; Cai, C.L.; Sharma, P.; Bronshtein, V.; Valencia, G.B.; Lazzaro, D.R.; Aranda, J.V. Hydrogen peroxide accumulation in the choroid during intermittent hypoxia increases risk of severe oxygen-induced retinopathy in neonatal rats. Investig. Ophthalmol. Vis. Sci. 2013, 54, 7644–7657. [Google Scholar] [CrossRef] [Green Version]
- Jivabhai-Patel, S.; Bany-Mohammed, F.; McNally, L.; Valencia, G.B.; Lazzaro, D.R.; Aranda, J.V.; Beharry, K.D. Exogenous superoxide dismutase mimetic without scavenging H2O2 causes photoreceptor damage in a rat model for oxygen-induced retinopathy. Investig. Ophthalmol. Vis. Sci. 2015, 56, 1665–1677. [Google Scholar] [CrossRef] [Green Version]
- Tu, C.; Beharry, K.D.; Shen, X.; Li, J.; Wang, L.; Aranda, J.V.; Qu, J. Proteomic profiling of the retinas in a neonatal rat model of oxygen-induced retinopathy with a reproducible ion-current-based MS1 approach. J. Proteome Res. 2015, 14, 2109–2120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aranda, J.V.; Cai, C.L.; Ahmad, T.; Bronshtein, V.; Sadeh, J.; Valencia, G.B.; Lazzaro, D.R.; Beharry, K.D. Pharmacologic synergism of ocular ketorolac and systemic caffeine citrate in rat oxygen-induced retinopathy. Pediatr. Res. 2016, 80, 554–565. [Google Scholar] [CrossRef] [PubMed] [Green Version]






| Normoxia (Nx) | Hyperoxia (Hx, 50% O2) | Intermittent Hypoxia (IH) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Saline | Low Dose | High Dose | Saline | Low Dose | High Dose | Saline | Low Dose | High Dose | |
| No. Cells | 537.6 ± 105.1 | 208.4 ± 17.3 ** | 138.5 ± 15.0 ** | 289.6 ± 25.8 | 217.5 ± 11.1 **,# | 149.8 ± 14.8 ** | 477.5 ± 32.8 | 331.0 ± 58.5 # | 240.0 ± 26.0 **,## |
| VEGF | 949.0 ± 174.4 | 306.0 ± 24.0 ** | 254.0 ± 29.1 ** | 419.8 ± 69.8 # | 398.5 ± 20.1 | 240.5 ± 18.4 * | 1132.0 ± 178.4 | 367.8 ± 68.9 ** | 260.0 ± 29.8 ** |
| VEGFR-1 | 504.3 ± 36.1 | 345.8 ± 46.6 * | 368.5 ± 33.0 * | 617.3 ± 113.7 | 158.3 ± 14.3 **,# | 234.8 ± 47.0 ** | 1196.8 ± 127.4 ## | 447.8 ± 68.0 ** | 583.5 ± 72.7 **,# |
| AQP-1 | 560.8 ± 76.5 | 470.7 ± 111 | 318.8 ± 105.5 | 550.9 ± 96.6 | 583.0 ± 45.1 | 407.3 ± 58.3 | 504.2 ± 110.3 | 432.0 ± 67.1 | 388.5 ± 53.2 |
| AQP-4 | 1236.6 ± 110 | 388.6 ± 90.9 ** | 277.3 ± 52.7 ** | 1153.0 ± 118 | 673.0 ± 108 * | 771.8 ± 89.7 *,## | 1623.8 ± 111.1 | 482.5 ± 66.4 ** | 1021.5 ± 74.6 **,## |
| No. Tubes | 90.3 ± 12.5 | 38.3 ± 8.9 ** | 44.9 ± 15.6 * | 29.6 ± 8.0 ## | 16.6 ± 1.0 ## | 10.2 ± 2.0 **,# | 45.5 ± 11.0 ## | 0 ± 0 **,## | 6.6 ± 2.0 **,## |
| Genes | Saline Hx | Saline IH | Low Dose Nx | Low Dose Hx | Low Dose IH | High Dose Nx | High Dose Hx | High Dose IH |
|---|---|---|---|---|---|---|---|---|
| AQP-1 | −1.5 ± 0.09 | 4.3 ± 0.3 | −72.5 ± 17.4 ** | 1.5 ± 0.2 | −41.1 ± 1.8 ** | −4.5 ± 3.9 | −3.8 ± 2.5 | −4.5 ± 1.2 |
| AQP-2 | −2.0 ± 4.2 | −0.2 ± 1.7 | −15.2 ± 2.7 ** | −11.7 ± 0.9 ** | −12.3 ± 1.8 ** | −10.0 ± 0.9 ** | −10.6 ± 0.9 ** | −16.1 ± 1.5 ** |
| AQP-3 | 1.4 ± 4.2 | 2.6 ± 1.7 | −4.9 ± 1.3 | 1.1 ± 0.13 | −2.7 ± 1.2 | 0.01 ± 1.8 | −3.4 ± 0.5 | −3.2 ± 0.3 |
| AQP-4 | 1.7 ± 0.9 | 1.0 ± 2.9 | −249.1 ± 95 ** | −0.3 ± 3.1 | −152.1 ± 19.3 ** | −6.1 ± 0.7 | −2.5 ± 0.01 | −1.7 ± 1.0 |
| AQP-5 | −0.3 ± 2.3 | 13.2 ± 2.5 | −243.0 ± 86 ** | −8.5 ± 1.7 * | −131.0 ± 10.2 * | −24.5 ± 10.2 ** | −6.8 ± 2.8 | −35.9 ± 14.6 ** |
| AQP-6 | 3.6 ± 1.4 | −6.9 ± 0.91 | −260.3 ± 71.1 ** | −24.2 ± 8.8 ** | −215.4 ± 34.6 ** | −423.2 ± 18.7 ** | −18.2 ± 1.6 ** | −245.4 ± 65.6 ** |
| AQP-7 | 1.2 ± 0.3 | 9.2 ± 1.1 ** | −50.7 ± 1.3 ** | 3.0 ± 0.03 | −31.6 ± 2.6 ** | −2.0 ± 1.6 | −11.2 ± 0.3 ** | −1.2 ± 0.3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guzel, S.; Cai, C.L.; Aranda, J.V.; Beharry, K.D. Dose Response of Bumetanide on Aquaporins and Angiogenesis Biomarkers in Human Retinal Endothelial Cells Exposed to Intermittent Hypoxia. Pharmaceuticals 2021, 14, 967. https://doi.org/10.3390/ph14100967
Guzel S, Cai CL, Aranda JV, Beharry KD. Dose Response of Bumetanide on Aquaporins and Angiogenesis Biomarkers in Human Retinal Endothelial Cells Exposed to Intermittent Hypoxia. Pharmaceuticals. 2021; 14(10):967. https://doi.org/10.3390/ph14100967
Chicago/Turabian StyleGuzel, Sibel, Charles L. Cai, Jacob V. Aranda, and Kay D. Beharry. 2021. "Dose Response of Bumetanide on Aquaporins and Angiogenesis Biomarkers in Human Retinal Endothelial Cells Exposed to Intermittent Hypoxia" Pharmaceuticals 14, no. 10: 967. https://doi.org/10.3390/ph14100967
APA StyleGuzel, S., Cai, C. L., Aranda, J. V., & Beharry, K. D. (2021). Dose Response of Bumetanide on Aquaporins and Angiogenesis Biomarkers in Human Retinal Endothelial Cells Exposed to Intermittent Hypoxia. Pharmaceuticals, 14(10), 967. https://doi.org/10.3390/ph14100967







