A Comprehensive Review of HLA and Severe Cutaneous Adverse Drug Reactions: Implication for Clinical Pharmacogenomics and Precision Medicine
Abstract
:1. Introduction
2. HLA Molecular Biology
3. HLA Genomic Organization and Inheritance
4. HLA Polymorphisms and HLA Nomenclature
5. HLA Genotyping: Methods for Identification
6. Severe Cutaneous Adverse Drug Reactions (SCARs)
6.1. Stevens–Johnson Syndrome/Toxic Epidermal Necrolysis (SJS/TEN)
6.2. Drug Reaction with Eosinophilia and Systemic Symptom (DRESS)
6.3. Acute Generalized Exanthematous Pustulosis (AGEP)
7. Potential Mechanism of HLA-Associated Drug Hypersensitivity
7.1. Hapten/Pro-Hapten Theory
7.2. The Pharmacological-Interaction (P-I) Theory
7.3. Repertoire Alteration Theory
8. HLA and CD8+T-Cells Provide the Immunogenetics Basis of Systemic Drug Hypersensitivity
9. Pharmacogenomics and HLA Research across the World
10. Drug Hypersensitivity and HLA Alleles: Translational Research into Clinical Practices
10.1. Association of Abacavir Hypersensitivity with HLA-B*57:01
10.2. Association of Carbamazepine Hypersensitivity with HLA-B*15:02
10.3. Association of Allopurinol Hypersensitivity with HLA-B*58:01
11. International Clinical Recommendations for HLA Genotyping
12. Approach to the HLA Genotype Screening in Clinical Implementation
13. Reimbursement and Cost Effectiveness Screening of HLA
14. Drug Hypersensitivity and HLA: Clinical Implementation in Thailand
14.1. Genomics Thailand
14.2. From Research into the National Policy: A Model of HLA-B*15:02
14.2.1. Carbamazepine
14.2.2. Allopurinol
14.2.3. Abacavir
14.2.4. Cotrimoxazole
14.2.5. Dapsone
14.3. Cost-Effective Analysis
14.4. Pharmacogenomics Laboratory Distribution and Local Accessibility
14.5. Workflow
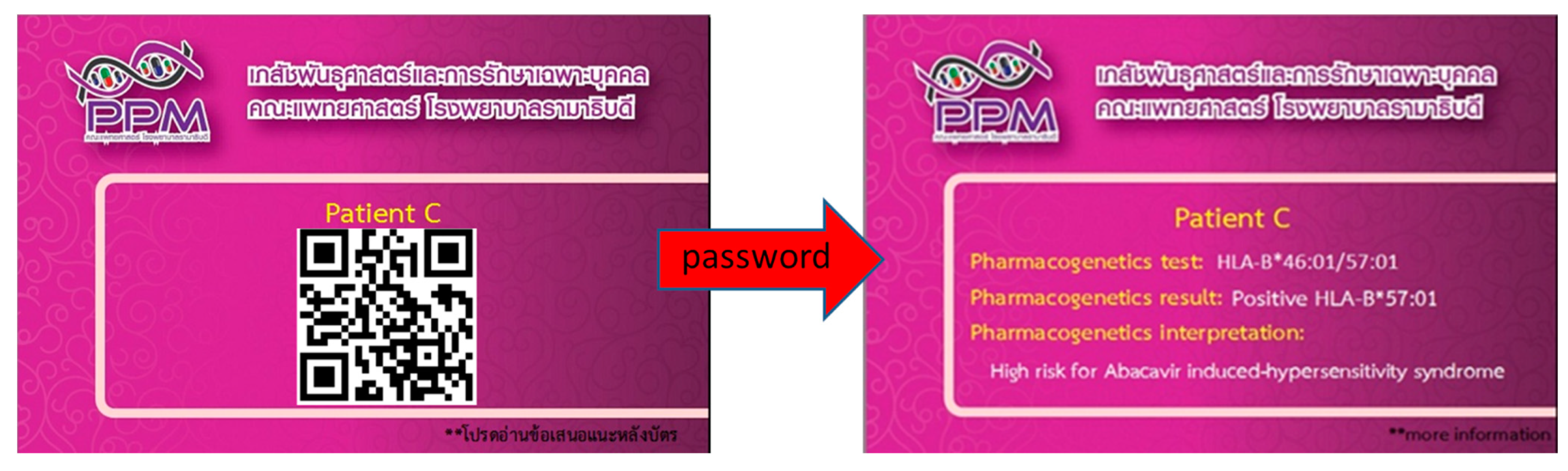
14.6. PPM CARD
14.7. Multidisciplinary Team
14.8. Electronic Health Record
14.9. Counseling
14.10. Knowledge and Education
15. Expert Opinion
- (A)
- Introduce appropriate HLA test such as screening of family members for risk genes of CBZ, e.g., HLA-B75 serotype, i.e., HLA-B*15:02, HLA-B*15:08, HLA-B*15:11, HLA-B*15:21.
- (B)
- Introduce relevant HLA test for all population in the settings. For example, HLA-B*15:02 test only for Han Chinese, Thai, Indian, Malaysian and Singaporean population. In contrast, HLA-A*31:01 test only for Caucasian, European, Japanese and Korean population.
- (C)
- Prepare alternative drugs for those patients who may be at HLA associated risk of SCARs and incorporated these into the local prescribing guidelines.
- (D)
- Caution should be taken for interpreting and reporting PGx test results, as some biomarkers are phenotype specific while others are universal markers as discussed in this review.
16. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dendrou, C.A.; Petersen, J.; Rossjohn, J.; Fugger, L. HLA variation and disease. Nat. Rev. Immunol. 2018, 18, 325–339. [Google Scholar] [CrossRef] [PubMed]
- Tiercy, J.M. Molecular basis of HLA polymorphism: Implications in clinical transplantation. Transpl. Immunol. 2002, 9, 173–180. [Google Scholar] [CrossRef]
- Gao, J.; Zhu, C.; Zhu, Z.; Tang, L.; Liu, L.; Wen, L.; Sun, L. The human leukocyte antigen and genetic susceptibility in human diseases. J. Bio-X Res. 2019, 2, 112–120. [Google Scholar] [CrossRef]
- Charron, D. HLA, immunogenetics, pharmacogenetics and personalized medicine. Vox Sang. 2011, 100, 163–166. [Google Scholar] [CrossRef]
- Howell, W.M.; Carter, V.; Clark, B. The HLA system: Immunobiology, HLA typing, antibody screening and crossmatching techniques. J. Clin. Pathol. 2010, 63, 387–390. [Google Scholar] [CrossRef]
- Madden, K.; Chabot-Richards, D. HLA testing in the molecular diagnostic laboratory. Virchows Arch. Int. J. Pathol. 2019, 474, 139–147. [Google Scholar] [CrossRef]
- Choo, S.Y. The HLA system: Genetics, immunology, clinical testing, and clinical implications. Yonsei Med. J. 2007, 48, 11–23. [Google Scholar] [CrossRef] [Green Version]
- Mahdi, B.M. Introductory Chapter: Concept of Human Leukocyte Antigen (HLA). In Human Leukocyte Antigen (HLA); Mahdi, B.M., Ed.; IntechOpen: London, UK, 2019; pp. 1–8. ISBN 978-1-78985-762-7. [Google Scholar]
- Lam, T.H.; Shen, M.; Chia, J.M.; Chan, S.H.; Ren, E.C. Population-specific recombination sites within the human MHC region. Heredity 2013, 111, 131–138. [Google Scholar] [CrossRef] [Green Version]
- Williams, T.M. Human leukocyte antigen gene polymorphism and the histocompatibility laboratory. J. Mol. Diagn. JMD 2001, 3, 98–104. [Google Scholar] [CrossRef] [Green Version]
- Duke, J.L.; Lind, C.; Mackiewicz, K.; Ferriola, D.; Papazoglou, A.; Gasiewski, A.; Heron, S.; Huynh, A.; McLaughlin, L.; Rogers, M.; et al. Determining performance characteristics of an NGS-based HLA typing method for clinical applications. HLA 2016, 87, 141–152. [Google Scholar] [CrossRef]
- Bharadwaj, M.; Illing, P.; Theodossis, A.; Purcell, A.W.; Rossjohn, J.; McCluskey, J. Drug hypersensitivity and human leukocyte antigens of the major histocompatibility complex. Annu. Rev. Pharmacol. Toxicol. 2012, 52, 401–431. [Google Scholar] [CrossRef]
- White, K.D.; Gaudieri, S.; Phillips, E.J. HLA and the Pharmacogenomics of Drug Hypersensitivity. In Handbook of Pharmacogenomics and Stratified Medicine; Elsevier-Hanley and Belfus Inc.: London, UK, 2014; pp. 437–465. ISBN 978-0-12386-883-1. [Google Scholar]
- Arbitrio, M.; Scionti, F.; Di Martino, M.T.; Caracciolo, D.; Pensabene, L.; Tassone, P.; Tagliaferri, P. Pharmacogenomics Biomarker Discovery and Validation for Translation in Clinical Practice. Clin. Transl. Sci. 2021, 14, 113–119. [Google Scholar] [CrossRef]
- European Bioinformatics Institute. Statistics < IMGT/HLA <IPD <EMBL-EBI. Available online: https://www.ebi.ac.uk/ipd/imgt/hla/stats.html (accessed on 14 May 2021).
- Robinson, J.; Guethlein, L.A.; Cereb, N.; Yang, S.Y.; Norman, P.J.; Marsh, S.G.E.; Parham, P. Distinguishing functional polymorphism from random variation in the sequences of >10,000 HLA-A, -B and -C alleles. PLoS Genet. 2017, 13, e1006862. [Google Scholar] [CrossRef] [PubMed]
- Robinson, J.; Barker, D.J.; Georgiou, X.; Cooper, M.A.; Flicek, P.; Marsh, S.G.E. IPD-IMGT/HLA Database. Nucleic Acids Res. 2020, 48, D948–D955. [Google Scholar] [CrossRef] [PubMed]
- Illing, P.T.; Purcell, A.W.; McCluskey, J. The role of HLA genes in pharmacogenomics: Unravelling HLA associated adverse drug reactions. Immunogenetics 2017, 69, 617–630. [Google Scholar] [CrossRef] [PubMed]
- Marsh, S.G.; Albert, E.D.; Bodmer, W.F.; Bontrop, R.E.; Dupont, B.; Erlich, H.A.; Fernández-Viña, M.; Geraghty, D.E.; Holdsworth, R.; Hurley, C.K.; et al. Nomenclature for factors of the HLA system, 2010. Tissue Antigens 2010, 75, 291–455. [Google Scholar] [CrossRef]
- Mayor, N.P.; Robinson, J.; McWhinnie, A.J.; Ranade, S.; Eng, K.; Midwinter, W.; Bultitude, W.P.; Chin, C.S.; Bowman, B.; Marks, P.; et al. HLA Typing for the Next Generation. PLoS ONE 2015, 10, e0127153. [Google Scholar] [CrossRef] [Green Version]
- Dunckley, H. HLA typing by SSO and SSP methods. In Immunogenetics; Christiansen, F., Tait, B., Eds.; Springer: New York, NY, USA, 2012; pp. 9–25. [Google Scholar] [CrossRef]
- Gabriel, C.; Fürst, D.; Faé, I.; Wenda, S.; Zollikofer, C.; Mytilineos, J.; Fischer, G.F. HLA typing by next-generation sequencing—Getting closer to reality. Tissue Antigens 2014, 83, 65–75. [Google Scholar] [CrossRef]
- Erlich, H. HLA DNA typing: Past, present, and future. Tissue Antigens 2012, 80, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Stocchi, L.; Cascella, R.; Zampatti, S.; Pirazzoli, A.; Novelli, G.; Giardina, E. The Pharmacogenomic HLA Biomarker Associated to Adverse Abacavir Reactions: Comparative Analysis of Different Genotyping Methods. Curr. Genom. 2012, 13, 314–320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fowler, T.; Bansal, A.S.; Lozsádi, D. Risks and management of antiepileptic drug induced skin reactions in the adult out-patient setting. Seizure 2019, 72, 61–70. [Google Scholar] [CrossRef] [Green Version]
- Fan, W.L.; Shiao, M.S.; Hui, R.C.; Su, S.C.; Wang, C.W.; Chang, Y.C.; Chung, W.H. HLA Association with Drug-Induced Adverse Reactions. J. Immunol. Res. 2017, 2017, 3186328. [Google Scholar] [CrossRef]
- Fricke-Galindo, I.; LLerena, A.; López-López, M. An update on HLA alleles associated with adverse drug reactions. Drug Metab. Pers. 2017, 32, 73–87. [Google Scholar] [CrossRef]
- Kaniwa, N.; Saito, Y. Pharmacogenomics of severe cutaneous adverse reactions and drug-induced liver injury. J. Hum. Genet. 2013, 58, 317–326. [Google Scholar] [CrossRef] [Green Version]
- Yang, S.C.; Chen, C.B.; Lin, M.Y.; Zhang, Z.Y.; Jia, X.Y.; Huang, M.; Zou, Y.F.; Chung, W.H. Genetics of Severe Cutaneous Adverse Reactions. Front. Med. 2021, 8, 652091. [Google Scholar] [CrossRef]
- Yip, V.L.; Alfirevic, A.; Pirmohamed, M. Genetics of immune-mediated adverse drug reactions: A comprehensive and clinical review. Clin. Rev. Allergy Immunol. 2015, 48, 165–175. [Google Scholar] [CrossRef]
- Chung, W.H.; Hung, S.I. Recent advances in the genetics and immunology of Stevens-Johnson syndrome and toxic epidermal necrosis. J. Dermatol. Sci. 2012, 66, 190–196. [Google Scholar] [CrossRef] [PubMed]
- Chung, W.H.; Hung, S.I.; Yang, J.Y.; Su, S.C.; Huang, S.P.; Wei, C.Y.; Chin, S.W.; Chiou, C.C.; Chu, S.C.; Ho, H.C.; et al. Granulysin is a key mediator for disseminated keratinocyte death in Stevens-Johnson syndrome and toxic epidermal necrolysis. Nat. Med. 2008, 14, 1343–1350. [Google Scholar] [CrossRef]
- Schwartz, R.A.; McDonough, P.H.; Lee, B.W. Toxic epidermal necrolysis: Part I. Introduction, history, classification, clinical features, systemic manifestations, etiology, and immunopathogenesis. J. Am. Acad. Dermatol. 2013, 69, 173-e1. [Google Scholar] [CrossRef]
- Ferrandiz-Pulido, C.; Garcia-Patos, V. A review of causes of Stevens-Johnson syndrome and toxic epidermal necrolysis in children. Arch. Dis. Child. 2013, 98, 998–1003. [Google Scholar] [CrossRef]
- Frey, N.; Jossi, J.; Bodmer, M.; Bircher, A.; Jick, S.S.; Meier, C.R.; Spoendlin, J. The Epidemiology of Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis in the UK. J. Investig. Dermatol. 2017, 137, 1240–1247. [Google Scholar] [CrossRef] [Green Version]
- Hsu, D.Y.; Brieva, J.; Silverberg, N.B.; Silverberg, J.I. Morbidity and Mortality of Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis in United States Adults. J. Investig. Dermatol. 2016, 136, 1387–1397. [Google Scholar] [CrossRef] [Green Version]
- Halevy, S.; Ghislain, P.D.; Mockenhaupt, M.; Fagot, J.P.; Bouwes Bavinck, J.N.; Sidoroff, A.; Naldi, L.; Dunant, A.; Viboud, C.; Roujeau, J.C. Allopurinol is the most common cause of Stevens-Johnson syndrome and toxic epidermal necrolysis in Europe and Israel. J. Am. Acad. Dermatol. 2008, 58, 25–32. [Google Scholar] [CrossRef]
- Kunimi, Y.; Hirata, Y.; Aihara, M.; Yamane, Y.; Ikezawa, Z. Statistical analysis of Stevens-Johnson syndrome caused by Mycoplasma pneumonia infection in Japan. Allergol. Int. 2011, 60, 525–532. [Google Scholar] [CrossRef]
- Forman, R.; Koren, G.; Shear, N.H. Erythema multiforme, Stevens-Johnson syndrome and toxic epidermal necrolysis in children: A review of 10 years' experience. Drug Saf. 2002, 25, 965–972. [Google Scholar] [CrossRef]
- Sukasem, C.; Katsila, T.; Tempark, T.; Patrinos, G.P.; Chantratita, W. Drug-Induced Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis Call for Optimum Patient Stratification and Theranostics via Pharmacogenomics. Annu. Rev. Genom. Hum. Genet. 2018, 19, 329–353. [Google Scholar] [CrossRef]
- Husain, Z.; Reddy, B.Y.; Schwartz, R.A. DRESS syndrome: Part I. Clinical perspectives. J. Am. Acad. Dermatol. 2013, 68, 693-e1. [Google Scholar] [CrossRef]
- Bocquet, H.; Bagot, M.; Roujeau, J.C. Drug-induced pseudolymphoma and drug hypersensitivity syndrome (Drug Rash with Eosinophilia and Systemic Symptoms: DRESS). Semin. Cutan. Med. Surg. 1996, 15, 250–257. [Google Scholar] [CrossRef]
- Cacoub, P.; Musette, P.; Descamps, V.; Meyer, O.; Speirs, C.; Finzi, L.; Roujeau, J.C. The DRESS syndrome: A literature review. Am. J. Med. 2011, 124, 588–597. [Google Scholar] [CrossRef]
- Kim, G.Y.; Anderson, K.R.; Davis, D.M.R.; Hand, J.L.; Tollefson, M.M. Drug reaction with eosinophilia and systemic symptoms (DRESS) in the pediatric population: A systematic review of the literature. J. Am. Acad. Dermatol. 2020, 83, 1323–1330. [Google Scholar] [CrossRef]
- Spriet, S.; Banks, T.A. Drug reaction with eosinophilia and systemic symptoms syndrome. Allergy Asthma. Proc. 2015, 36, 501–505. [Google Scholar] [CrossRef]
- Descamps, V.; Valance, A.; Edlinger, C.; Fillet, A.M.; Grossin, M.; Lebrun-Vignes, B.; Belaich, S.; Crickx, B. Association of human herpesvirus 6 infection with drug reaction with eosinophilia and systemic symptoms. Arch. Dermatol. 2001, 137, 301–304. [Google Scholar] [PubMed]
- Shiohara, T.; Mizukawa, Y. Drug-induced hypersensitivity syndrome (DiHS)/drug reaction with eosinophilia and systemic symptoms (DRESS): An update in 2019. Allergol. Int. 2019, 68, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Shear, N.H.; Spielberg, S.P. Anticonvulsant hypersensitivity syndrome. In vitro assessment of risk. J. Clin. Investig. 1988, 82, 1826–1832. [Google Scholar] [CrossRef] [PubMed]
- Sidoroff, A.; Halevy, S.; Bavinck, J.N.; Vaillant, L.; Roujeau, J.C. Acute generalized exanthematous pustulosis (AGEP)—A clinical reaction pattern. J. Cutan. Pathol. 2001, 28, 113–119. [Google Scholar] [CrossRef] [Green Version]
- Sidoroff, A.; Dunant, A.; Viboud, C.; Halevy, S.; Bavinck, J.N.; Naldi, L.; Mockenhaupt, M.; Fagot, J.P.; Roujeau, J.C. Risk factors for acute generalized exanthematous pustulosis (AGEP)-results of a multinational case-control study (EuroSCAR). Br. J. Dermatol. 2007, 157, 989–996. [Google Scholar] [CrossRef]
- Davidovici, B.; Dodiuk-Gad, R.; Rozenman, D.; Halevy, S. Profile of acute generalized exanthematous pustulosis in Israel during 2002–2005: Results of the RegiSCAR Study. Isr. Med. Assoc. J. 2008, 10, 410–412. [Google Scholar]
- Halevy, S. Acute generalized exanthematous pustulosis. Curr. Opin. Allergy Clin. Immunol. 2009, 9, 322–328. [Google Scholar] [CrossRef]
- Szatkowski, J.; Schwartz, R.A. Acute generalized exanthematous pustulosis (AGEP): A review and update. J. Am. Acad. Dermatol. 2015, 73, 843–848. [Google Scholar] [CrossRef] [PubMed]
- Hadavand, M.A.; Kaffenberger, B.; Cartron, A.M.; Trinidad, J.C. Clinical Presentation and Management of Atypical and Recalcitrant Acute Generalized Exanthematous Pustulosis (AGEP). J. Am. Acad. Dermatol. 2020. [Google Scholar] [CrossRef]
- Koga, C.; Kabashima, K.; Shiraishi, N.; Kobayashi, M.; Tokura, Y. Possible pathogenic role of Th17 cells for atopic dermatitis. J. Investig. Dermatol. 2008, 128, 2625–2630. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Britschgi, M.; Steiner, U.C.; Schmid, S.; Depta, J.P.; Senti, G.; Bircher, A.; Burkhart, C.; Yawalkar, N.; Pichler, W.J. T-cell involvement in drug-induced acute generalized exanthematous pustulosis. J. Clin. Investig. 2001, 107, 1433–1441. [Google Scholar] [CrossRef] [Green Version]
- Kakeda, M.; Schlapbach, C.; Danelon, G.; Tang, M.M.; Cecchinato, V.; Yawalkar, N.; Uguccioni, M. Innate immune cells express IL-17A/F in acute generalized exanthematous pustulosis and generalized pustular psoriasis. Arch. Dermatol. Res. 2014, 306, 933–938. [Google Scholar] [CrossRef] [PubMed]
- Navarini, A.A.; Valeyrie-Allanore, L.; Setta-Kaffetzi, N.; Barker, J.N.; Capon, F.; Creamer, D.; Roujeau, J.C.; Sekula, P.; Simpson, M.A.; Trembath, R.C.; et al. Rare variations in IL36RN in severe adverse drug reactions manifesting as acute generalized exanthematous pustulosis. J. Investig. Dermatol. 2013, 133, 1904–1907. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meier-Schiesser, B.; Feldmeyer, L.; Jankovic, D.; Mellett, M.; Satoh, T.K.; Yerly, D.; Navarini, A.; Abe, R.; Yawalkar, N.; Chung, W.H.; et al. Culprit Drugs Induce Specific IL-36 Overexpression in Acute Generalized Exanthematous Pustulosis. J. Investig. Dermatol. 2019, 139, 848–858. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chung, W.H.; Wang, C.W.; Dao, R.L. Severe cutaneous adverse drug reactions. J. Dermatol. 2016, 43, 758–766. [Google Scholar] [CrossRef]
- Verma, R.; Vasudevan, B.; Pragasam, V. Severe cutaneous adverse drug reactions. Med. J. Armed Forces India 2013, 69, 375–383. [Google Scholar] [CrossRef] [Green Version]
- Martin, T.; Li, H. Severe cutaneous adverse drug reactions: A review on epidemiology, etiology, clinical manifestation and pathogenesis. Chin. Med. J. 2008, 121, 756–761. [Google Scholar] [PubMed]
- Yun, J.; Cai, F.; Lee, F.J.; Pichler, W.J. T-cell-mediated drug hypersensitivity: Immune mechanisms and their clinical relevance. Asia Pac. Allergy 2016, 6, 77–89. [Google Scholar] [CrossRef] [Green Version]
- Watkins, S.; Pichler, W. Activating interactions of sulfanilamides with T cell receptors. Open J. Immunol. 2013, 3, 139–157. [Google Scholar] [CrossRef] [Green Version]
- Adam, J.; Wuillemin, N.; Watkins, S.; Jamin, H.; Eriksson, K.K.; Villiger, P.; Fontana, S.; Pichler, W.J.; Yerly, D. Abacavir induced T cell reactivity from drug naïve individuals shares features of allo-immune responses. PLoS ONE 2014, 9, e95339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burkhart, C.; Britschgi, M.; Strasser, I.; Depta, J.P.; von Greyerz, S.; Barnaba, V.; Pichler, W.J. Non-covalent presentation of sulfamethoxazole to human CD4+ T cells is independent of distinct human leucocyte antigen-bound peptides. Clin. Exp. Allergy 2002, 32, 1635–1643. [Google Scholar] [CrossRef] [PubMed]
- Zanni, M.P.; von Greyerz, S.; Schnyder, B.; Wendland, T.; Pichler, W.J. Allele-unrestricted presentation of lidocaine by HLA-DR molecules to specific alphabeta+ T cell clones. Int. Immunol. 1998, 10, 507–515. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, P.; Zhang, S.; Wang, Y.; Yang, C.; Huang, J. Structural modeling of HLA-B*1502/peptide/carbamazepine/T-cell receptor complex architecture: Implication for the molecular mechanism of carbamazepine-induced Stevens-Johnson syndrome/toxic epidermal necrolysis. J. Biomol. Struct. Dyn. 2016, 34, 1806–1817. [Google Scholar] [CrossRef] [PubMed]
- Mockenhaupt, M. Stevens-Johnson syndrome and toxic epidermal necrolysis: Clinical patterns, diagnostic considerations, etiology, and therapeutic management. Semin. Cutan. Med. Surg. 2014, 33, 10–16. [Google Scholar] [CrossRef] [PubMed]
- Olson, D.; Abbott, J.; Lin, C.; Prok, L.; Dominguez, S.R. Characterization of Children With Recurrent Episodes of Stevens Johnson Syndrome. J. Pediatr.Infect. Dis. Soc. 2017, 6, e140–e143. [Google Scholar] [CrossRef]
- Roujeau, J.C.; Kelly, J.P.; Naldi, L.; Rzany, B.; Stern, R.S.; Anderson, T.; Auquier, A.; Bastuji-Garin, S.; Correia, O.; Locati, F.; et al. Medication use and the risk of Stevens-Johnson syndrome or toxic epidermal necrolysis. N. Engl. J. Med. 1995, 333, 1600–1607. [Google Scholar] [CrossRef]
- Levi, N.; Bastuji-Garin, S.; Mockenhaupt, M.; Roujeau, J.C.; Flahault, A.; Kelly, J.P.; Martin, E.; Kaufman, D.W.; Maison, P. Medications as risk factors of Stevens-Johnson syndrome and toxic epidermal necrolysis in children: A pooled analysis. Pediatrics 2009, 123, e297–e304. [Google Scholar] [CrossRef] [PubMed]
- Sassolas, B.; Haddad, C.; Mockenhaupt, M.; Dunant, A.; Liss, Y.; Bork, K.; Haustein, U.F.; Vieluf, D.; Roujeau, J.C.; Le Louet, H. ALDEN, an algorithm for assessment of drug causality in Stevens-Johnson Syndrome and toxic epidermal necrolysis: Comparison with case-control analysis. Clin. Pharmacol. Ther. 2010, 88, 60–68. [Google Scholar] [CrossRef]
- Dodiuk-Gad, R.P.; Chung, W.H.; Valeyrie-Allanore, L.; Shear, N.H. Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis: An Update. Am. J. Clin. Dermatol. 2015, 16, 475–493. [Google Scholar] [CrossRef]
- Sorrell, J.; Anthony, L.; Rademaker, A.; Belknap, S.M.; Callahan, S.; West, D.P.; Paller, A.S. Score of Toxic Epidermal Necrosis Predicts the Outcomes of Pediatric Epidermal Necrolysis. Pediatr. Dermatol. 2017, 34, 433–437. [Google Scholar] [CrossRef]
- Fernando, S.L. Drug-reaction eosinophilia and systemic symptoms and drug-induced hypersensitivity syndrome. Australas. J. Dermatol. 2014, 55, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Kano, Y.; Hirahara, K.; Mitsuyama, Y.; Takahashi, R.; Shiohara, T. Utility of the lymphocyte transformation test in the diagnosis of drug sensitivity: Dependence on its timing and the type of drug eruption. Allergy 2007, 62, 1439–1444. [Google Scholar] [CrossRef] [PubMed]
- Tang, Y.H.; Mockenhaupt, M.; Henry, A.; Bounoua, M.; Naldi, L.; Le Gouvello, S.; Bensussan, A.; Roujeau, J.C. Poor relevance of a lymphocyte proliferation assay in lamotrigine-induced Stevens-Johnson syndrome or toxic epidermal necrolysis. Clin. Exp. Allergy 2012, 42, 248–254. [Google Scholar] [CrossRef]
- Porebski, G.; Pecaric-Petkovic, T.; Groux-Keller, M.; Bosak, M.; Kawabata, T.T.; Pichler, W.J. In vitro drug causality assessment in Stevens-Johnson syndrome—Alternatives for lymphocyte transformation test. Clin. Exp. Allergy 2013, 43, 1027–1037. [Google Scholar] [CrossRef] [PubMed]
- Wolkenstein, P.; Chosidow, O.; Fléchet, M.L.; Robbiola, O.; Paul, M.; Dumé, L.; Revuz, J.; Roujeau, J.C. Patch testing in severe cutaneous adverse drug reactions, including Stevens-Johnson syndrome and toxic epidermal necrolysis. Contact Dermatol. 1996, 35, 234–236. [Google Scholar] [CrossRef]
- Hassoun-Kheir, N.; Bergman, R.; Weltfriend, S. The use of patch tests in the diagnosis of delayed hypersensitivity drug eruptions. Int. J. Dermatol. 2016, 55, 1219–1224. [Google Scholar] [CrossRef] [PubMed]
- Pinho, A.; Coutinho, I.; Gameiro, A.; Gouveia, M.; Gonçalo, M. Patch testing—A valuable tool for investigating non-immediate cutaneous adverse drug reactions to antibiotics. J. Eur. Acad. Dermatol. Venereol. 2017, 31, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Shanbhag, S.S.; Chodosh, J.; Fathy, C.; Goverman, J.; Mitchell, C.; Saeed, H.N. Multidisciplinary care in Stevens-Johnson syndrome. Adv. Chronic Dis. 2020, 11, 2040622319894469. [Google Scholar] [CrossRef]
- Schwartz, R.A.; McDonough, P.H.; Lee, B.W. Toxic epidermal necrolysis: Part II. Prognosis, sequelae, diagnosis, differential diagnosis, prevention, and treatment. J. Am. Acad. Dermatol. 2013, 69, e1–e16. [Google Scholar] [CrossRef]
- Palmieri, T.L.; Greenhalgh, D.G.; Saffle, J.R.; Spence, R.J.; Peck, M.D.; Jeng, J.C.; Mozingo, D.W.; Yowler, C.J.; Sheridan, R.L.; Ahrenholz, D.H.; et al. A multicenter review of toxic epidermal necrolysis treated in U.S. burn centers at the end of the twentieth century. J. Burn Care Rehabil. 2002, 23, 87–96. [Google Scholar] [CrossRef]
- Zimmermann, S.; Sekula, P.; Venhoff, M.; Motschall, E.; Knaus, J.; Schumacher, M.; Mockenhaupt, M. Systemic Immunomodulating Therapies for Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis: A Systematic Review and Meta-analysis. JAMA Dermatol. 2017, 153, 514–522. [Google Scholar] [CrossRef]
- Huang, Y.C.; Li, Y.C.; Chen, T.J. The efficacy of intravenous immunoglobulin for the treatment of toxic epidermal necrolysis: A systematic review and meta-analysis. Br. J. Dermatol. 2012, 167, 424–432. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, S.; Tang, S.; Li, S.; Pan, Y.; Ding, Y. Biologic TNF-alpha inhibitors in the treatment of Stevens-Johnson syndrome and toxic epidermal necrolysis: A systemic review. J. Dermatol. Treat. 2020, 31, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.Y.; Walsh, S.A.; Creamer, D. Long-term complications of Stevens-Johnson syndrome/toxic epidermal necrolysis (SJS/TEN): The spectrum of chronic problems in patients who survive an episode of SJS/TEN necessitates multidisciplinary follow-up. Br. J. Dermatol. 2017, 177, 924–935. [Google Scholar] [CrossRef] [PubMed]
- Olteanu, C.; Shear, N.H.; Chew, H.F.; Hashimoto, R.; Alhusayen, R.; Whyte-Croasdaile, S.; Finkelstein, Y.; Burnett, M.; Ziv, M.; Sade, S.; et al. Severe Physical Complications among Survivors of Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis. Drug Saf. 2018, 41, 277–284. [Google Scholar] [CrossRef] [PubMed]
- Yun, J.; Adam, J.; Yerly, D.; Pichler, W.J. Human leukocyte antigens (HLA) associated drug hypersensitivity: Consequences of drug binding to HLA. Allergy 2012, 67, 1338–1346. [Google Scholar] [CrossRef] [PubMed]
- Martin, A.M.; Almeida, C.A.; Cameron, P.; Purcell, A.W.; Nolan, D.; James, I.; McCluskey, J.; Phillips, E.; Landay, A.; Mallal, S. Immune responses to abacavir in antigen-presenting cells from hypersensitive patients. AIDS 2007, 21, 1233–1244. [Google Scholar] [CrossRef]
- Hetherington, S.; McGuirk, S.; Powell, G.; Cutrell, A.; Naderer, O.; Spreen, B.; Lafon, S.; Pearce, G.; Steel, H. Hypersensitivity reactions during therapy with the nucleoside reverse transcriptase inhibitor abacavir. Clin. Ther. 2001, 23, 1603–1614. [Google Scholar] [CrossRef]
- Mallal, S.; Phillips, E.; Carosi, G.; Molina, J.M.; Workman, C.; Tomazic, J.; Jägel-Guedes, E.; Rugina, S.; Kozyrev, O.; Cid, J.F.; et al. HLA-B*5701 screening for hypersensitivity to abacavir. N. Engl. J. Med. 2008, 358, 568–579. [Google Scholar] [CrossRef] [Green Version]
- Small, C.B.; Margolis, D.A.; Shaefer, M.S.; Ross, L.L. HLA-B*57:01 allele prevalence in HIV-infected North American subjects and the impact of allele testing on the incidence of abacavir-associated hypersensitivity reaction in HLA-B*57:01-negative subjects. BMC Infect. Dis. 2017, 17, 256. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mounzer, K.; Hsu, R.; Fusco, J.S.; Brunet, L.; Henegar, C.E.; Vannappagari, V.; Stainsby, C.M.; Shaefer, M.S.; Ragone, L.; Fusco, G.P. HLA-B*57:01 screening and hypersensitivity reaction to abacavir between 1999 and 2016 in the OPERA(®) observational database: A cohort study. AIDS Res. Ther. 2019, 16, 1. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Krebs, K.; Milani, L.; Lauschke, V.M. Global Frequencies of Clinically Important HLA Alleles and Their Implications for the Cost-Effectiveness of Preemptive Pharmacogenetic Testing. Clin. Pharmacol. Ther. 2021, 109, 160–174. [Google Scholar] [CrossRef] [PubMed]
- Stainsby, C.M.; Perger, T.M.; Vannappagari, V.; Mounzer, K.C.; Hsu, R.K.; Henegar, C.E.; Oyee, J.; Urbaityte, R.; Lane, C.E.; Carter, L.M.; et al. Abacavir Hypersensitivity Reaction Reporting Rates During a Decade of HLA-B*5701 Screening as a Risk-Mitigation Measure. Pharmacotherapy 2019, 39, 40–54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Puthanakit, T.; Bunupuradah, T.; Kosalaraksa, P.; Vibol, U.; Hansudewechakul, R.; Ubolyam, S.; Suwanlerk, T.; Kanjanavanit, S.; Ngampiyaskul, C.; Wongsawat, J.; et al. Prevalence of human leukocyte antigen-B*5701 among HIV-infected children in Thailand and Cambodia: Implications for abacavir use. Pediatric Infect. Dis. J. 2013, 32, 252–253. [Google Scholar] [CrossRef] [Green Version]
- Young, B.; Squires, K.; Patel, P.; Dejesus, E.; Bellos, N.; Berger, D.; Sutherland-Phillips, D.H.; Liao, Q.; Shaefer, M.; Wannamaker, P. First large, multicenter, open-label study utilizing HLA-B*5701 screening for abacavir hypersensitivity in North America. AIDS 2008, 22, 1673–1675. [Google Scholar] [CrossRef]
- Martin, M.A.; Hoffman, J.M.; Freimuth, R.R.; Klein, T.E.; Dong, B.J.; Pirmohamed, M.; Hicks, J.K.; Wilkinson, M.R.; Haas, D.W.; Kroetz, D.L. Clinical Pharmacogenetics Implementation Consortium Guidelines for HLA-B Genotype and Abacavir Dosing: 2014 update. Clin. Pharmacol. Ther. 2014, 95, 499–500. [Google Scholar] [CrossRef] [PubMed]
- Aberg, J.A.; Kaplan, J.E.; Libman, H.; Emmanuel, P.; Anderson, J.R.; Stone, V.E.; Oleske, J.M.; Currier, J.S.; Gallant, J.E. Primary care guidelines for the management of persons infected with human immunodeficiency virus: 2009 update by the HIV medicine Association of the Infectious Diseases Society of America. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2009, 49, 651–681. [Google Scholar] [CrossRef] [Green Version]
- ICH Topic E15 Definitions for Genomic Biomarkers, Pharmacogenomics, Pharmacogenetics, Genomic Data and Sample Coding Categories. Available online: docs/en_GB/document_library/Scientific_guideline/2009/09/WC500002880.pdf (accessed on 25 June 2021).
- U.S. Food and Drug Administration. Information for Healthcare Professionals: Abacavir (Marketed as Ziagen) and Abacavir-Containing Medications. Available online: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm123927.htm (accessed on 21 May 2021).
- Sukasem, C.; Chaichan, C.; Nakkrut, T.; Satapornpong, P.; Jaruthamsophon, K.; Jantararoungtong, T.; Koomdee, N.; Sririttha, S.; Medhasi, S.; Oo-Puthinan, S.; et al. Association between HLA-B Alleles and Carbamazepine-Induced Maculopapular Exanthema and Severe Cutaneous Reactions in Thai Patients. J. Immunol. Res. 2018, 2018, 2780272. [Google Scholar] [CrossRef] [Green Version]
- Phillips, E.J.; Sukasem, C.; Whirl-Carrillo, M.; Müller, D.J.; Dunnenberger, H.M.; Chantratita, W.; Goldspiel, B.; Chen, Y.T.; Carleton, B.C.; George, A.L., Jr.; et al. Clinical Pharmacogenetics Implementation Consortium Guideline for HLA Genotype and Use of Carbamazepine and Oxcarbazepine: 2017 Update. Clin. Pharmacol. Ther. 2018, 103, 574–581. [Google Scholar] [CrossRef] [Green Version]
- Sukasem, C.; Sririttha, S.; Chaichan, C.; Nakkrut, T.; Satapornpong, P.; Jaruthamsophon, K.; Jantararoungtong, T.; Koomdee, N.; Medhasi, S.; Oo-Puthinan, S.; et al. Spectrum of cutaneous adverse reactions to aromatic antiepileptic drugs and human leukocyte antigen genotypes in Thai patients and meta-analysis. Pharm. J. 2021. [Google Scholar] [CrossRef]
- Jaruthamsophon, K.; Tipmanee, V.; Sangiemchoey, A.; Sukasem, C.; Limprasert, P. HLA-B*15:21 and carbamazepine-induced Stevens-Johnson syndrome: Pooled-data and in silico analysis. Sci. Rep. 2017, 7, 45553. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tangamornsuksan, W.; Chaiyakunapruk, N.; Somkrua, R.; Lohitnavy, M.; Tassaneeyakul, W. Relationship between the HLA-B*1502 allele and carbamazepine-induced Stevens-Johnson syndrome and toxic epidermal necrolysis: A systematic review and meta-analysis. JAMA Dermatol. 2013, 149, 1025–1032. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grover, S.; Kukreti, R. HLA alleles and hypersensitivity to carbamazepine: An updated systematic review with meta-analysis. Pharm. Genom. 2014, 24, 94–112. [Google Scholar] [CrossRef]
- Yuliwulandari, R.; Kristin, E.; Prayuni, K.; Sachrowardi, Q.; Suyatna, F.D.; Menaldi, S.L.; Wichukchinda, N.; Mahasirimongkol, S.; Cavallari, L.H. Association of the HLA-B alleles with carbamazepine-induced Stevens-Johnson syndrome/toxic epidermal necrolysis in the Javanese and Sundanese population of Indonesia: The important role of the HLA-B75 serotype. Pharmacogenomics 2017, 18, 1643–1648. [Google Scholar] [CrossRef] [PubMed]
- Sun, D.; Yu, C.H.; Liu, Z.S.; He, X.L.; Hu, J.S.; Wu, G.F.; Mao, B.; Wu, S.H.; Xiang, H.H. Association of HLA-B*1502 and *1511 allele with antiepileptic drug-induced Stevens-Johnson syndrome in central China. J. Huazhong Univ. Sci. Technol. Med. Sci. 2014, 34, 146–150. [Google Scholar] [CrossRef]
- Kaniwa, N.; Saito, Y.; Aihara, M.; Matsunaga, K.; Tohkin, M.; Kurose, K.; Furuya, H.; Takahashi, Y.; Muramatsu, M.; Kinoshita, S.; et al. HLA-B*1511 is a risk factor for carbamazepine-induced Stevens-Johnson syndrome and toxic epidermal necrolysis in Japanese patients. Epilepsia 2010, 51, 2461–2465. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Lee, K.W.; Song, W.J.; Kim, S.H.; Jee, Y.K.; Lee, S.M.; Kang, H.R.; Park, H.W.; Cho, S.H.; Park, S.H.; et al. Carbamazepine-induced severe cutaneous adverse reactions and HLA genotypes in Koreans. Epilepsy Res. 2011, 97, 190–197. [Google Scholar] [CrossRef] [PubMed]
- Capule, F.; Tragulpiankit, P.; Mahasirimongkol, S.; Jittikoon, J.; Wichukchinda, N.; Theresa Alentajan-Aleta, L.; James Barit, J.V.; Casanova-Gutierrez, J.; Cabral-Lim, L.; Baltazar Reyes, J.P.; et al. Association of carbamazepine-induced Stevens-Johnson syndrome/toxic epidermal necrolysis with the HLA-B75 serotype or HLA-B*15:21 allele in Filipino patients. Pharm. J. 2020, 20, 533–541. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.B.; Hsiao, Y.H.; Wu, T.; Hsih, M.S.; Tassaneeyakul, W.; Jorns, T.P.; Sukasem, C.; Hsu, C.N.; Su, S.C.; Chang, W.C.; et al. Risk and association of HLA with oxcarbazepine-induced cutaneous adverse reactions in Asians. Neurology 2017, 88, 78–86. [Google Scholar] [CrossRef] [PubMed]
- Sukasem, C.; Jantararoungtong, T.; Koomdee, N. Pharmacogenomics research and its clinical implementation in Thailand: Lessons learned from the resource-limited settings. Drug Metab. Pharmacokinet. 2021, 39, 100399. [Google Scholar] [CrossRef]
- Koomdee, N.; Pratoomwun, J.; Jantararoungtong, T.; Theeramoke, V.; Tassaneeyakul, W.; Klaewsongkram, J.; Rerkpattanapipat, T.; Santon, S.; Puangpetch, A.; Intusoma, U.; et al. Association of HLA-A and HLA-B Alleles with Lamotrigine-Induced Cutaneous Adverse Drug Reactions in the Thai Population. Front. Pharmacol. 2017, 8, 879. [Google Scholar] [CrossRef] [PubMed]
- Sukasem, C.; Sririttha, S.; Tempark, T.; Klaewsongkram, J.; Rerkpattanapipat, T.; Puangpetch, A.; Boongird, A.; Chulavatnatol, S. Genetic and clinical risk factors associated with phenytoin-induced cutaneous adverse drug reactions in Thai population. Pharmacoepidemiol. Drug Saf. 2020, 29, 565–574. [Google Scholar] [CrossRef] [PubMed]
- Tassaneeyakul, W.; Prabmeechai, N.; Sukasem, C.; Kongpan, T.; Konyoung, P.; Chumworathayi, P.; Tiamkao, S.; Khunarkornsiri, U.; Kulkantrakorn, K.; Saksit, N.; et al. Associations between HLA class I and cytochrome P450 2C9 genetic polymorphisms and phenytoin-related severe cutaneous adverse reactions in a Thai population. Pharm. Genom. 2016, 26, 225–234. [Google Scholar] [CrossRef] [PubMed]
- Genin, E.; Chen, D.P.; Hung, S.I.; Sekula, P.; Schumacher, M.; Chang, P.Y.; Tsai, S.H.; Wu, T.L.; Bellón, T.; Tamouza, R.; et al. HLA-A*31:01 and different types of carbamazepine-induced severe cutaneous adverse reactions: An international study and meta-analysis. Pharm. J. 2014, 14, 281–288. [Google Scholar] [CrossRef]
- Su, S.-C.; Hung, S.-I.; Fan, W.-L.; Dao, R.-L.; Chung, W.-H. Severe Cutaneous Adverse Reactions: The Pharmacogenomics from Research to Clinical Implementation. Int. J. Mol. Sci. 2016, 17, 1890. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Satapornpong, P.; Jinda, P.; Jantararoungtong, T.; Koomdee, N.; Chaichan, C.; Pratoomwun, J.; Na Nakorn, C.; Aekplakorn, W.; Wilantho, A.; Ngamphiw, C.; et al. Genetic Diversity of HLA Class I and Class II Alleles in Thai Populations: Contribution to Genotype-Guided Therapeutics. Front. Pharmacol. 2020, 11, 78. [Google Scholar] [CrossRef] [PubMed]
- Cao, K.; Hollenbach, J.; Shi, X.; Shi, W.; Chopek, M.; Fernández-Viña, M.A. Analysis of the frequencies of HLA-A, B, and C alleles and haplotypes in the five major ethnic groups of the United States reveals high levels of diversity in these loci and contrasting distribution patterns in these populations. Hum. Immunol. 2001, 62, 1009–1030. [Google Scholar] [CrossRef]
- Chang, C.C.; Too, C.L.; Murad, S.; Hussein, S.H. Association of HLA-B*1502 allele with carbamazepine-induced toxic epidermal necrolysis and Stevens-Johnson syndrome in the multi-ethnic Malaysian population. Int. J. Dermatol. 2011, 50, 221–224. [Google Scholar] [CrossRef]
- Cristallo, A.F.; Schroeder, J.; Citterio, A.; Santori, G.; Ferrioli, G.M.; Rossi, U.; Bertani, G.; Cassano, S.; Gottardi, P.; Ceschini, N.; et al. A study of HLA class I and class II 4-digit allele level in Stevens-Johnson syndrome and toxic epidermal necrolysis. Int. J. Immunogenet. 2011, 38, 303–309. [Google Scholar] [CrossRef]
- Lonjou, C.; Borot, N.; Sekula, P.; Ledger, N.; Thomas, L.; Halevy, S.; Naldi, L.; Bouwes-Bavinck, J.N.; Sidoroff, A.; de Toma, C.; et al. A European study of HLA-B in Stevens-Johnson syndrome and toxic epidermal necrolysis related to five high-risk drugs. Pharm. Genom. 2008, 18, 99–107. [Google Scholar] [CrossRef] [Green Version]
- Jung, J.W.; Kim, J.Y.; Park, I.W.; Choi, B.W.; Kang, H.R. Genetic markers of severe cutaneous adverse reactions. Korean J. Intern. Med. 2018, 33, 867–875. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- U.S. Food and Drug Administration. Able of Pharmacogenomic Biomarkers in Drug Labeling. Available online: http://www.fda.gov/Drugs/ScienceResearch/ResearchAreas/Pharmacogenetics/ucm083378.htm (accessed on 29 June 2021).
- Lee, M.H.; Stocker, S.L.; Anderson, J.; Phillips, E.J.; Nolan, D.; Williams, K.M.; Graham, G.G.; Sullivan, J.R.; Day, R.O. Initiating allopurinol therapy: Do we need to know the patient's human leucocyte antigen status? Intern. Med. J. 2012, 42, 411–416. [Google Scholar] [CrossRef] [PubMed]
- Jung, J.W.; Song, W.J.; Kim, Y.S.; Joo, K.W.; Lee, K.W.; Kim, S.H.; Park, H.W.; Chang, Y.S.; Cho, S.H.; Min, K.U.; et al. HLA-B58 can help the clinical decision on starting allopurinol in patients with chronic renal insufficiency. Nephrol. Dial. Transpl. 2011, 26, 3567–3572. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jung, J.W.; Kim, D.K.; Park, H.W.; Oh, K.H.; Joo, K.W.; Kim, Y.S.; Ahn, C.; Lee, K.W.; Cho, S.H.; Min, K.U.; et al. An effective strategy to prevent allopurinol-induced hypersensitivity by HLA typing. Genet. Med. 2015, 17, 807–814. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dean, L.; Kane, M. Allopurinol Therapy and HLA-B*58:01 Genotype. In Medical Genetics Summaries; Pratt, V.M., Scott, S.A., Pirmohamed, M., Esquivel, B., Kane, M.S., Kattman, B.L., Malheiro, A.J., Eds.; National Center for Biotechnology Information: Bethesda, MD, USA, 2012; pp. 1–11. [Google Scholar]
- Kaniwa, N.; Saito, Y.; Aihara, M.; Matsunaga, K.; Tohkin, M.; Kurose, K.; Sawada, J.; Furuya, H.; Takahashi, Y.; Muramatsu, M.; et al. HLA-B locus in Japanese patients with anti-epileptics and allopurinol-related Stevens-Johnson syndrome and toxic epidermal necrolysis. Pharmacogenomics 2008, 9, 1617–1622. [Google Scholar] [CrossRef] [PubMed]
- Keller, S.F.; Lu, N.; Blumenthal, K.G.; Rai, S.K.; Yokose, C.; Choi, J.W.J.; Kim, S.C.; Zhang, Y.; Choi, H.K. Racial/ethnic variation and risk factors for allopurinol-associated severe cutaneous adverse reactions: A cohort study. Ann. Rheum. Dis. 2018, 77, 1187–1193. [Google Scholar] [CrossRef] [PubMed]
- Lu, N.; Rai, S.K.; Terkeltaub, R.; Kim, S.C.; Menendez, M.E.; Choi, H.K. Racial disparities in the risk of Stevens-Johnson Syndrome and toxic epidermal necrolysis as urate-lowering drug adverse events in the United States. Semin. Arthritis Rheum. 2016, 46, 253–258. [Google Scholar] [CrossRef] [Green Version]
- Ko, T.-M.; Tsai, C.-Y.; Chen, S.-Y.; Chen, K.-S.; Yu, K.-H.; Chu, C.-S.; Huang, C.-M.; Wang, C.-R.; Weng, C.-T.; Yu, C.-L.; et al. Use of HLA-B*58:01 genotyping to prevent allopurinol induced severe cutaneous adverse reactions in Taiwan: National prospective cohort study. BMJ Br. Med. J. 2015, 351, h4848. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gonçalo, M.; Coutinho, I.; Teixeira, V.; Gameiro, A.R.; Brites, M.M.; Nunes, R.; Martinho, A. HLA-B*58:01 is a risk factor for allopurinol-induced DRESS and Stevens-Johnson syndrome/toxic epidermal necrolysis in a Portuguese population. Br. J. Dermatol. 2013, 169, 660–665. [Google Scholar] [CrossRef]
- Sukasem, C.; Jantararoungtong, T.; Kuntawong, P.; Puangpetch, A.; Koomdee, N.; Satapornpong, P.; Supapsophon, P.; Klaewsongkram, J.; Rerkpattanapipat, T. HLA-B*58:01 for Allopurinol-Induced Cutaneous Adverse Drug Reactions: Implication for Clinical Interpretation in Thailand. Front. Pharmacol. 2016, 7, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kang, H.R.; Jee, Y.K.; Kim, Y.S.; Lee, C.H.; Jung, J.W.; Kim, S.H.; Park, H.W.; Chang, Y.S.; Jang, I.J.; Cho, S.H.; et al. Positive and negative associations of HLA class I alleles with allopurinol-induced SCARs in Koreans. Pharm. Genom. 2011, 21, 303–307. [Google Scholar] [CrossRef] [PubMed]
- FitzGerald, J.D.; Dalbeth, N.; Mikuls, T.; Brignardello-Petersen, R.; Guyatt, G.; Abeles, A.M.; Gelber, A.C.; Harrold, L.R.; Khanna, D.; King, C.; et al. 2020 American College of Rheumatology Guideline for the Management of Gout. Arthritis Care Res. 2020, 72, 744–760. [Google Scholar] [CrossRef]
- Saksit, N.; Tassaneeyakul, W.; Nakkam, N.; Konyoung, P.; Khunarkornsiri, U.; Chumworathayi, P.; Sukasem, C.; Suttisai, S.; Piriyachananusorn, N.; Tiwong, P.; et al. Risk factors of allopurinol-induced severe cutaneous adverse reactions in a Thai population. Pharm. Genom. 2017, 27, 255–263. [Google Scholar] [CrossRef] [PubMed]
- Sato, T.; Cheng, C.-L.; Park, H.-W.; Kao Yang, Y.-H.; Yang, M.-S.; Fujita, M.; Kumagai, Y.; Tohkin, M.; Saito, Y.; Sai, K. Real-world evidence of population differences in allopurinol-related severe cutaneous adverse reactions in East Asians: A population-based cohort study. Clin. Transl. Sci. 2021, 14, 1002–1014. [Google Scholar] [CrossRef] [PubMed]
- Hung, S.I.; Chung, W.H.; Liou, L.B.; Chu, C.C.; Lin, M.; Huang, H.P.; Lin, Y.L.; Lan, J.L.; Yang, L.C.; Hong, H.S.; et al. HLA-B*5801 allele as a genetic marker for severe cutaneous adverse reactions caused by allopurinol. Proc. Natl. Acad. Sci. USA 2005, 102, 4134–4139. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, H.-W.; Kim, D.K.; Kim, S.-H.; Kim, S.; Chae, D.-W.; Yang, M.-S.; Oh, Y.K.; Lee, J.P.; Jung, J.-W.; Shin, J.; et al. Efficacy of the HLA-B∗58:01 Screening Test in Preventing Allopurinol-Induced Severe Cutaneous Adverse Reactions in Patients with Chronic Renal Insufficiency—A Prospective Study. J. Allergy Clin. Immunol. Pract. 2019, 7, 1271–1276. [Google Scholar] [CrossRef] [PubMed]
- Stamp, L.K.; Day, R.O.; Yun, J. Allopurinol hypersensitivity: Investigating the cause and minimizing the risk. Nat. Rev. Rheumatol. 2016, 12, 235–242. [Google Scholar] [CrossRef]
- Thurston, M.M.; Phillips, B.B.; Bourg, C.A. Safety and efficacy of allopurinol in chronic kidney disease. Ann. Pharm. 2013, 47, 1507–1516. [Google Scholar] [CrossRef]
- Abdullah-Koolmees, H.; van Keulen, A.M.; Nijenhuis, M.; Deneer, V.H.M. Pharmacogenetics Guidelines: Overview and Comparison of the DPWG, CPIC, CPNDS, and RNPGx Guidelines. Front. Pharmacol. 2020, 11, 595219. [Google Scholar] [CrossRef]
- Caudle, K.E.; Dunnenberger, H.M.; Freimuth, R.R.; Peterson, J.F.; Burlison, J.D.; Whirl-Carrillo, M.; Scott, S.A.; Rehm, H.L.; Williams, M.S.; Klein, T.E.; et al. Standardizing terms for clinical pharmacogenetic test results: Consensus terms from the Clinical Pharmacogenetics Implementation Consortium (CPIC). Genet. Med. 2017, 19, 215–223. [Google Scholar] [CrossRef] [PubMed]
- Thorn, C.F.; Klein, T.E.; Altman, R.B. PharmGKB: The Pharmacogenomics Knowledge Base. Methods Mol. Biol. (Clifton N. J.) 2013, 1015, 311–320. [Google Scholar] [CrossRef] [Green Version]
- PharmGKB. PharmGKB Website. Prescr. Info. 2020. Available online: https://www.pharmgkb.org/ (accessed on 21 July 2021).
- The Clinical Pharmacogenetics Implementation Consortium (CPIC®). Available online: https://cpicpgx.org/guidelines/ (accessed on 21 July 2021).
- Amstutz, U.; Shear, N.H.; Rieder, M.J.; Hwang, S.; Fung, V.; Nakamura, H.; Connolly, M.B.; Ito, S.; Carleton, B.C. Recommendations for HLA-B*15:02 and HLA-A*31:01 genetic testing to reduce the risk of carbamazepine-induced hypersensitivity reactions. Epilepsia 2014, 55, 496–506. [Google Scholar] [CrossRef]
- Picard, N.; Boyer, J.C.; Etienne-Grimaldi, M.C.; Barin-Le Guellec, C.; Thomas, F.; Loriot, M.A. Pharmacogenetics-based personalized therapy: Levels of evidence and recommendations from the French Network of Pharmacogenetics (RNPGx). Therapie 2017, 72, 185–192. [Google Scholar] [CrossRef]
- The Dutch Pharmacogenomic Working Group. Hamacogenomic Recommendations, Farmacogenetica-Update. 2020. Available online: www.knmp.nl/ (accessed on 5 July 2021).
- Dean, L. Carbamazepine Therapy and HLA Genotype. In Medical Genetics Summaries; Pratt, V.M., Scott, S.A., Pirmohamed, M., Esquivel, B., Kane, M.S., Kattman, B.L., Malheiro, A.J., Eds.; National Center for Biotechnology Information: Bethesda, MD, USA, 2012; pp. 1–18. [Google Scholar]
- Chen, Z.; Liew, D.; Kwan, P. Effects of a HLA-B*15:02 screening policy on antiepileptic drug use and severe skin reactions. Neurology 2014, 83, 2077–2084. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, D.V.; Vidal, C.; Chu, H.C.; van Nunen, S. Developing pharmacogenetic screening methods for an emergent country: Vietnam. World Allergy Organ. J. 2019, 12, 100037. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mushiroda, T.; Takahashi, Y.; Onuma, T.; Yamamoto, Y.; Kamei, T.; Hoshida, T.; Takeuchi, K.; Otsuka, K.; Okazaki, M.; Watanabe, M.; et al. Association of HLA-A*31:01 Screening with the Incidence of Carbamazepine-Induced Cutaneous Adverse Reactions in a Japanese Population. JAMA Neurol. 2018, 75, 842–849. [Google Scholar] [CrossRef] [PubMed]
- Tiamkao, S.; Jitpimolmard, J.; Sawanyawisuth, K.; Jitpimolmard, S. Cost minimization of HLA-B*1502 screening before prescribing carbamazepine in Thailand. Int. J. Clin. Pharm. 2013, 35, 608–612. [Google Scholar] [CrossRef] [PubMed]
- Dong, D.; Sung, C.; Finkelstein, E.A. Cost-effectiveness of HLA-B*1502 genotyping in adult patients with newly diagnosed epilepsy in Singapore. Neurology 2012, 79, 1259–1267. [Google Scholar] [CrossRef] [PubMed]
- Saokaew, S.; Tassaneeyakul, W.; Maenthaisong, R.; Chaiyakunapruk, N. Cost-effectiveness analysis of HLA-B*5801 testing in preventing allopurinol-induced SJS/TEN in Thai population. PLoS ONE 2014, 9, e94294. [Google Scholar] [CrossRef] [Green Version]
- Park, D.J.; Kang, J.H.; Lee, J.W.; Lee, K.E.; Wen, L.; Kim, T.J.; Park, Y.W.; Park, S.H.; Lee, S.S. Cost-effectiveness analysis of HLA-B5801 genotyping in the treatment of gout patients with chronic renal insufficiency in Korea. Arthritis Care Res. (Hoboken) 2015, 67, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Finding the Right Drug. C.F.M. Genomics. Available online: https://www.nature.com/articles/d42473–020–00207–8 (accessed on 25 July 2021).
- Chong, H.Y.; Allotey, P.A.; Chaiyakunapruk, N. Current landscape of personalized medicine adoption and implementation in Southeast Asia. BMC Med. Genom. 2018, 11, 94. [Google Scholar] [CrossRef] [PubMed]
- Esmaeilzadeh, H.; Farjadian, S.; Alyasin, S.; Nemati, H.; Nabavizadeh, H.; Esmaeilzadeh, E. Epidemiology of Severe Cutaneous Adverse Drug Reaction and Its HLA Association among Pediatrics. Iran. J. Pharm. Res. 2019, 18, 506–522. [Google Scholar] [PubMed]
- Locharernkul, C.; Loplumlert, J.; Limotai, C.; Korkij, W.; Desudchit, T.; Tongkobpetch, S.; Kangwanshiratada, O.; Hirankarn, N.; Suphapeetiporn, K.; Shotelersuk, V. Carbamazepine and phenytoin induced Stevens-Johnson syndrome is associated with HLA-B*1502 allele in Thai population. Epilepsia 2008, 49, 2087–2091. [Google Scholar] [CrossRef] [PubMed]
- Tassaneeyakul, W.; Tiamkao, S.; Jantararoungtong, T.; Chen, P.; Lin, S.Y.; Chen, W.H.; Konyoung, P.; Khunarkornsiri, U.; Auvichayapat, N.; Pavakul, K.; et al. Association between HLA-B*1502 and carbamazepine-induced severe cutaneous adverse drug reactions in a Thai population. Epilepsia 2010, 51, 926–930. [Google Scholar] [CrossRef] [PubMed]
- Sukasem, C.; Chantratita, W. A success story in pharmacogenomics: Genetic ID card for SJS/TEN. Pharmacogenomics 2016, 17, 455–458. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tassaneeyakul, W.; Jantararoungtong, T.; Chen, P.; Lin, P.Y.; Tiamkao, S.; Khunarkornsiri, U.; Chucherd, P.; Konyoung, P.; Vannaprasaht, S.; Choonhakarn, C.; et al. Strong association between HLA-B*5801 and allopurinol-induced Stevens-Johnson syndrome and toxic epidermal necrolysis in a Thai population. Pharm. Genom. 2009, 19, 704–709. [Google Scholar] [CrossRef]
- Hershfield, M.S.; Callaghan, J.T.; Tassaneeyakul, W.; Mushiroda, T.; Thorn, C.F.; Klein, T.E.; Lee, M.T. Clinical Pharmacogenetics Implementation Consortium guidelines for human leukocyte antigen-B genotype and allopurinol dosing. Clin. Pharmacol. Ther. 2013, 93, 153–158. [Google Scholar] [CrossRef] [Green Version]
- Hughes, A.R.; Spreen, W.R.; Mosteller, M.; Warren, L.L.; Lai, E.H.; Brothers, C.H.; Cox, C.; Nelsen, A.J.; Hughes, S.; Thorborn, D.E.; et al. Pharmacogenetics of hypersensitivity to abacavir: From PGx hypothesis to confirmation to clinical utility. Pharm. J. 2008, 8, 365–374. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mallal, S.; Nolan, D.; Witt, C.; Masel, G.; Martin, A.M.; Moore, C.; Sayer, D.; Castley, A.; Mamotte, C.; Maxwell, D.; et al. Association between presence of HLA-B*5701, HLA-DR7, and HLA-DQ3 and hypersensitivity to HIV-1 reverse-transcriptase inhibitor abacavir. Lancet 2002, 359, 727–732. [Google Scholar] [CrossRef]
- Sousa-Pinto, B.; Pinto-Ramos, J.; Correia, C.; Gonçalves-Costa, G.; Gomes, L.; Gil-Mata, S.; Araújo, L.; Delgado, L. Pharmacogenetics of abacavir hypersensitivity: A systematic review and meta-analysis of the association with HLA-B*57:01. J. Allergy Clin. Immunol. 2015, 136, 1092–1094.e1093. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hughes, A.R.; Mosteller, M.; Bansal, A.T.; Davies, K.; Haneline, S.A.; Lai, E.H.; Nangle, K.; Scott, T.; Spreen, W.R.; Warren, L.L.; et al. Association of genetic variations in HLA-B region with hypersensitivity to abacavir in some, but not all, populations. Pharmacogenomics 2004, 5, 203–211. [Google Scholar] [CrossRef] [PubMed]
- Hetherington, S.; Hughes, A.R.; Mosteller, M.; Shortino, D.; Baker, K.L.; Spreen, W.; Lai, E.; Davies, K.; Handley, A.; Dow, D.J.; et al. Genetic variations in HLA-B region and hypersensitivity reactions to abacavir. Lancet 2002, 359, 1121–1122. [Google Scholar] [CrossRef]
- Saag, M.; Balu, R.; Phillips, E.; Brachman, P.; Martorell, C.; Burman, W.; Stancil, B.; Mosteller, M.; Brothers, C.; Wannamaker, P.; et al. High sensitivity of human leukocyte antigen-b*5701 as a marker for immunologically confirmed abacavir hypersensitivity in white and black patients. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2008, 46, 1111–1118. [Google Scholar] [CrossRef] [Green Version]
- Martin, M.A.; Klein, T.E.; Dong, B.J.; Pirmohamed, M.; Haas, D.W.; Kroetz, D.L. Clinical pharmacogenetics implementation consortium guidelines for HLA-B genotype and abacavir dosing. Clin. Pharmacol. Ther. 2012, 91, 734–738. [Google Scholar] [CrossRef] [PubMed]
- Sukasem, C.; Tempark, T. Pharmacogenomics: A New Approach for Preventing Severe Cutaneous Adverse Drug Reactions. In Genomics-Driven Healthcare; Adis: Singapore, 2018; pp. 373–409. [Google Scholar] [CrossRef]
- Guo, Y.; Shi, L.; Hong, H.; Su, Z.; Fuscoe, J.; Ning, B. Studies on abacavir-induced hypersensitivity reaction: A successful example of translation of pharmacogenetics to personalized medicine. Sci. China Life Sci. 2013, 56, 119–124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, C.W.; Tassaneeyakul, W.; Chen, C.B.; Chen, W.T.; Teng, Y.C.; Huang, C.Y.; Sukasem, C.; Lu, C.W.; Lee, Y.S.; Choon, S.E.; et al. Whole genome sequencing identifies genetic variants associated with co-trimoxazole hypersensitivity in Asians. J. Allergy Clin. Immunol. 2021, 147, 1402–1412. [Google Scholar] [CrossRef] [PubMed]
- Sukasem, C.; Pratoomwun, J.; Satapornpong, P.; Klaewsongkram, J.; Rerkpattanapipat, T.; Rerknimitr, P.; Lertpichitkul, P.; Puangpetch, A.; Nakkam, N.; Konyoung, P.; et al. Genetic Association of Co-Trimoxazole-Induced Severe Cutaneous Adverse Reactions Is Phenotype-Specific: HLA Class I Genotypes and Haplotypes. Clin. Pharmacol. Ther. 2020, 108, 1078–1089. [Google Scholar] [CrossRef] [PubMed]
- Kongpan, T.; Mahasirimongkol, S.; Konyoung, P.; Kanjanawart, S.; Chumworathayi, P.; Wichukchinda, N.; Kidkeukarun, R.; Preechakul, S.; Khunarkornsiri, U.; Bamrungram, W.; et al. Candidate HLA genes for prediction of co-trimoxazole-induced severe cutaneous reactions. Pharm. Genom. 2015, 25, 402–411. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Satapornpong, P.; Pratoomwun, J.; Rerknimitr, P.; Klaewsongkram, J.; Nakkam, N.; Rungrotmongkol, T.; Konyoung, P.; Saksit, N.; Mahakkanukrauh, A.; Amornpinyo, W.; et al. HLA-B*13: 01 Is a Predictive Marker of Dapsone-Induced Severe Cutaneous Adverse Reactions in Thai Patients. Front. Immunol. 2021, 12, 661135. [Google Scholar] [CrossRef]
- Tempark, T.; Satapornpong, P.; Rerknimitr, P.; Nakkam, N.; Saksit, N.; Wattanakrai, P.; Jantararoungtong, T.; Koomdee, N.; Mahakkanukrauh, A.; Tassaneeyakul, W.; et al. Dapsone-induced severe cutaneous adverse drug reactions are strongly linked with HLA-B*13: 01 allele in the Thai population. Pharm. Genom. 2017, 27, 429–437. [Google Scholar] [CrossRef] [PubMed]
- Park, H.J.; Park, J.W.; Kim, S.H.; Choi, S.Y.; Kim, H.K.; Jung, C.G.; Yang, M.S.; Kang, D.Y.; Cho, M.K.; Kwon, H.S.; et al. The HLA-B*13:01 and the dapsone hypersensitivity syndrome in Korean and Asian populations: Genotype- and meta-analyses. Expert Opin. Drug. Saf. 2020, 19, 1349–1356. [Google Scholar] [CrossRef]
- Liu, H.; Wang, Z.; Bao, F.; Wang, C.; Sun, L.; Zhang, H.; Yu, G.; Mi, Z.; Li, J.; Li, L.; et al. Evaluation of Prospective HLA-B*13:01 Screening to Prevent Dapsone Hypersensitivity Syndrome in Patients with Leprosy. JAMA Dermatol. 2019, 155, 666–672. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tangamornsuksan, W.; Lohitnavy, M. Association between HLA-B*1301 and Dapsone-Induced Cutaneous Adverse Drug Reactions: A Systematic Review and Meta-analysis. JAMA Dermatol. 2018, 154, 441–446. [Google Scholar] [CrossRef] [Green Version]
- Krismawati, H.; Irwanto, A.; Pongtiku, A.; Irwan, I.D.; Maladan, Y.; Sitanggang, Y.A.; Wahyuni, T.; Tanjung, R.; Sun, Y.; Liu, H.; et al. Validation study of HLA-B*13:01 as a biomarker of dapsone hypersensitivity syndrome in leprosy patients in Indonesia. PLoS Negl. Trop. Dis. 2020, 14, e0008746. [Google Scholar] [CrossRef] [PubMed]
- Bank, P.C.D.; Swen, J.J.; Guchelaar, H.J. Implementation of Pharmacogenomics in Everyday Clinical Settings. Adv. Pharm. 2018, 83, 219–246. [Google Scholar] [CrossRef]
- Rios-Santos, F.; Magno, L.A.V. Pharmacogenetics and metabolism: Past, present and future. In Topics on Drug Metabolism; Paxton, J., Ed.; IntechOpen: Rijeka, Croatia, 2012; pp. 61–86. ISBN 978-953-51-0099-7. [Google Scholar]
- Wong, C.S.; Yeung, C.K.; Chan, C.Y.; Yap, D.Y.; Tang, S.C.; Cheung, B.M.; Kwok, J.S.; Chan, H.H. HLA-B*58:01 screening to prevent allopurinol-induced severe cutaneous adverse reactions in Chinese patients with chronic kidney disease. Arch. Dermatol. Res. 2021, 1–9. [Google Scholar] [CrossRef]
- Rattanavipapong, W.; Koopitakkajorn, T.; Praditsitthikorn, N.; Mahasirimongkol, S.; Teerawattananon, Y. Economic evaluation of HLA-B*15:02 screening for carbamazepine-induced severe adverse drug reactions in Thailand. Epilepsia 2013, 54, 1628–1638. [Google Scholar] [CrossRef] [PubMed]
- Levy, K.D.; Decker, B.S.; Carpenter, J.S.; Flockhart, D.A.; Dexter, P.R.; Desta, Z.; Skaar, T.C. Prerequisites to implementing a pharmacogenomics program in a large health-care system. Clin. Pharmacol. Ther. 2014, 96, 307–309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mills, R.; Haga, S.B. Clinical delivery of pharmacogenetic testing services: A proposed partnership between genetic counselors and pharmacists. Pharmacogenomics 2013, 14, 957–968. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caraballo, P.J.; Hodge, L.S.; Bielinski, S.J.; Stewart, A.K.; Farrugia, G.; Schultz, C.G.; Rohrer-Vitek, C.R.; Olson, J.E.; St Sauver, J.L.; Roger, V.L.; et al. Multidisciplinary model to implement pharmacogenomics at the point of care. Genet. Med. 2017, 19, 421–429. [Google Scholar] [CrossRef] [Green Version]
- Hoffman, J.M.; Dunnenberger, H.M.; Kevin Hicks, J.; Caudle, K.E.; Whirl Carrillo, M.; Freimuth, R.R.; Williams, M.S.; Klein, T.E.; Peterson, J.F. Developing knowledge resources to support precision medicine: Principles from the Clinical Pharmacogenetics Implementation Consortium (CPIC). J. Am. Med. Inf. Assoc. 2016, 23, 796–801. [Google Scholar] [CrossRef] [Green Version]
- Arwood, M.J.; Chumnumwat, S.; Cavallari, L.H.; Nutescu, E.A.; Duarte, J.D. Implementing Pharmacogenomics at Your Institution: Establishment and Overcoming Implementation Challenges. Clin. Transl. Sci. 2016, 9, 233–245. [Google Scholar] [CrossRef]
- O’Connor, S.K.; Ferreri, S.P.; Michaels, N.M.; Chater, R.W.; Viera, A.J.; Faruki, H.; McLeod, H.L.; Roederer, M. Making pharmacogenetic testing a reality in a community pharmacy. J. Am. Pharm. Assoc. 2012, 52, e259–e265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mital, S.; Musunuru, K.; Garg, V.; Russell, M.W.; Lanfear, D.E.; Gupta, R.M.; Hickey, K.T.; Ackerman, M.J.; Perez, M.V.; Roden, D.M.; et al. Enhancing Literacy in Cardiovascular Genetics: A Scientific Statement from the American Heart Association. Circ. Cardiovasc. Genet. 2016, 9, 448–467. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Padgett, L.; O’Connor, S.; Roederer, M.; McLeod, H.; Ferreri, S. Pharmacogenomics in a community pharmacy: ACT now. J. Am. Pharm. Assoc. 2011, 51, 189–193. [Google Scholar] [CrossRef] [PubMed]
- McCullough, K.B.; Formea, C.M.; Berg, K.D.; Burzynski, J.A.; Cunningham, J.L.; Ou, N.N.; Rudis, M.I.; Stollings, J.L.; Nicholson, W.T. Assessment of the pharmacogenomics educational needs of pharmacists. Am. J. Pharm. Educ. 2011, 75, 51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McMahon, T.; Tucci, J. The perceptions of pharmacists in Victoria, Australia on pharmacogenetics and its implications. Pharm. Pract. (Granada) 2011, 9, 141–147. [Google Scholar] [PubMed]
- Tuteja, S.; Haynes, K.; Zayac, C.; Sprague, J.E.; Bernhardt, B.; Pyeritz, R. Community pharmacists' attitudes towards clinical utility and ethical implications of pharmacogenetic testing. Pers. Med. 2013, 10, 793–800. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alexander, K.M.; Divine, H.S.; Hanna, C.R.; Gokun, Y.; Freeman, P.R. Implementation of personalized medicine services in community pharmacies: Perceptions of independent community pharmacists. J. Am. Pharm. Assoc. 2014, 54, 510–517. [Google Scholar] [CrossRef]
- Giri, J.; Curry, T.B.; Formea, C.M.; Nicholson, W.T.; Rohrer Vitek, C.R. Education and Knowledge in Pharmacogenomics: Still a Challenge? Clin. Pharmacol. Ther. 2018, 103, 752–755. [Google Scholar] [CrossRef] [PubMed]
- Weitzel, K.W.; Duong, B.Q.; Arwood, M.J.; Owusu-Obeng, A.; Abul-Husn, N.S.; Bernhardt, B.A.; Decker, B.; Denny, J.C.; Dietrich, E.; Gums, J.; et al. A stepwise approach to implementing pharmacogenetic testing in the primary care setting. Pharmacogenomics 2019, 20, 1103–1112. [Google Scholar] [CrossRef] [PubMed]






| Method | Advantage | Disadvantage | Medical Applications |
|---|---|---|---|
| rSSO |
|
|
|
| SSP |
|
|
|
| Real-time PCR |
|
|
|
| SBT |
|
|
|
| RegiSCAR | Bocquet et al. | J-SCAR. |
|---|---|---|
| Criteria: Diagnosis when all 3 items +3/4 of all of the following clinical signs | Criteria: All 3 is required, 1 of each clinical signs | Criteria: Typical—all 7 clinical signs/criteria Atypical—5 first clinical signs |
| 1. Acute skin eruption 2. Reaction suspected to drug-related 3. Hospitalization | 1. Cutaneous drug eruption | 1. Maculopapular rash develop > 3 weeks after starting offending drug 2. Prolonged clinical symptoms 2 weeks after discontinuation of the causative drug 3. Fever > 38 °C 4. ALT > 100 U/L or other organ involvement 5. Lymphocyte abnormalities ≤ 1 present -Leukocytosis > 11 × 109/L -Atypical lymphocytes > 5% -Eosinophilia > 1.5 × 109/L 6. Lymphadenopathy 7. HHV-6 reactivation |
| 1. Fever > 38 °C 2. Enlarged lymph nodes ≤ 2 sites 3. Involvement ≤ 1 internal organ 4. Blood count abnormalities -Lymphocytes above or below normal limit -Eosinophils above normal limit -Platelets under normal limit | 2. Hematologic abnormalities -Eosinophil > 1.5 × 109/L -Atypical lymphocytes | |
| 3. Systemic involvement -Lymphadenopathy ≤ 2 cm -Hepatitis: transaminase ≤ 2X -Interstitial nephritis -Interstitial pneumonitis -Carditis |
| HLA Pharmacogenetics Marker | Allele Frequency (%) | Drug | ADR Type | |||||
|---|---|---|---|---|---|---|---|---|
| Thai Population (n = 470) [25] | African Americans (n = 252) [26] | North American (n = 187) [26] | Caucasians (n = 265) [26] | Hispanics (n = 234) [26] | Asians (n = 358) [26] | |||
| HLA-A*01:01 | 2.23 | 5.56 | 7.49 | 15.09 | 5.98 | 1.53 | Phenobarbital | SCARs, MPE [32] |
| HLA-A*24:02 | 11.49 | 2.78 | 22.73 | 6.6 | 12.18 | 18.94 | Carbamazepine | SJS/TEN [33] |
| Phenytoin | SJS/TEN [33] | |||||||
| Lamotrigine | SJS/TEN, MPE [33] | |||||||
| HLA-A*30:02 | 0 | 4.96 | 1.87 | 0.57 | 3.42 | 0.14 | Amoxicillin-Clavulanate | DILI [34] |
| HLA-A*31:01 | 0.85 | 0.79 | 7.75 | 3.21 | 4.91 | 3.06 | Carbamazepine | CADRs, SJS/TEN, DRESS, MPE [35,69,70] |
| 0.85 | 0.79 | 7.75 | 3.21 | 4.91 | 3.06 | Lamotrigine | SCARs [36] | |
| HLA-A*33:03 | 11.17 | 3.97 | 0.53 | 0.57 | 1.07 | 11.7 | Allopurinol | SJS/TEN [71,72] |
| Ticlopidine | DILI [73] | |||||||
| HLA-A*68:01 | 0.96 | 2.58 | 5.62 | 3.02 | 2.56 | 0.28 | Lamotrigine | SCARs [37] |
| HLA-B*13:01 | 5.96 | 0 | 0 | 0 | 0 | 3.34 | Phenytoin | SCARs [38] |
| Phenobarbital | DRESS [32] | |||||||
| Dapsone | DRESS [39] | |||||||
| Salazosulfa-pyridine | DRESS [40] | |||||||
| HLA-B*15:02 | 7.66 | 0.2 | 0 | 0 | 0 | 4.87 | Carbamazepine | SJS/TEN [35,69,70] |
| Oxcarbazepine | MPE, SJS [35] | |||||||
| Phenytoin | SJS/TEN [35] | |||||||
| Cotrimoxazole | SJS/TEN [74] | |||||||
| HLA-B*15:11 | 0.21 | 0 | 0 | 0 | 0 | 0.28 | Carbamazepine | SJS/TEN [35,69] |
| HLA-B*15:13 | 0.96 | 0 | 0 | 0 | 0 | 0.28 | Phenytoin | SJS/TEN, DRESS [33,75,76] |
| HLA-B*35:05 | 1.91 | 0 | 0 | 0.38 | 0.85 | 0.14 | Nevirapine | SJS/TEN, DRESS [69,77] |
| HLA-B*38:01 | 0 | 0.4 | 1.07 | 2.45 | 1.71 | 0.42 | Co-trimoxazole | SJS/TEN [78] |
| HLA-B*38:02 | 4.26 | 0 | 0 | 0.19 | 0 | 6.55 | Oxcarbazepine | MPE [79] |
| Co-trimoxazole | SJS/TEN [78] | |||||||
| HLA-B*51:01 | 4.26 | 1.2 | 11.23 | 5.66 | 6.2 | 6.69 | Phenobarbital | SJS/TEN [32] |
| HLA-B*56:02 | 0.11 | 0 | 0 | 0 | 0 | 0.28 | Phenytoin | DRESS [38] |
| HLA-B*57:01 | 1.17 | 2.39 | 2.14 | 4.15 | 1.92 | 0.97 | Abacavir | AHS [35,69,80] |
| Flucloxacillin | DILI [81] | |||||||
| HLA-B*58:01 | 6.38 | 6.37 | 0.8 | 1.13 | 1.07 | 7.38 | Allopurinol | CADRs, SCARs, MPE, SJS/TEN, DRESS [35,69,71,82] |
| HLA-B*59:01 | 0 | 0 | 0 | 0 | 0 | 0.56 | Methazolamide | SJS/TEN [83] |
| HLA-C*03:02 | 7.77 | 2.78 | 0.27 | 0.38 | 1.07 | 7.66 | Allopurinol | SJS/TEN [71,72] |
| HLA-C*06:02 | 4.26 | 11.31 | 5.62 | 8.68 | 6.84 | 3.62 | Co-trimoxazole | SJS/TEN [74] |
| HLA-C*08:01 | 10.32 | 0.2 | 2.41 | 0 | 1.71 | 11.28 | Carbamazepine | SJS/TEN [33] |
| Phenytoin | SJS/TEN [84] | |||||||
| Allopurinol | SJS/TEN [84] | |||||||
| Co-trimoxazole | SJS/TEN [74] | |||||||
| HLA Pharmacogenetics Markers | Allele Frequency (%) | Drug | ADR Type | ||||
|---|---|---|---|---|---|---|---|
| Thai Population (n = 470) [25] | African Americans (n = 241) [85] | Caucasians (n = 265) [86] | Japanese (n = 371) [87] | Han Chinese (n = 358) [88] | |||
| HLA-DRB1*12:02 | 15.32 | 0.4 | 0 | 1.5 | 13.3 | Carbamazepine | SJS/TEN [33] |
| HLA-DRB1*13:02 | 1.38 | 8.5 | 3.4 | 7.7 | 2.8 | Allopurinol | SJS/TEN [71] |
| HLA-DRB1*15:01 | 8.09 | 16 | 15.8 | 8.5 | 10.8 | Amoxicillin- Clavulanate | DILI [34,89] |
| HLA-DRB1*15:02 | 14.47 | 0 | 0.8 | 10 | 5.3 | Allopurinol | SJS/TEN [71] |
| HLA-DRB1*16:02 | 5.96 | 0 | 0 | 0.9 | 5.3 | Phenytoin | SJS/TEN [84] |
| HLA-DQB1*06:02 | 1.49 | 23.2 | 15.8 | 8.2 | 3.8 | Amoxicillin- Clavulanate | DILI [34,89] |
| HLA-DQA1*02:01 | 8.72 | 9.1 | 13.2 | N/A | 5.7 | Lapatinib | DILI [90] |
| Drug | Gene | Phenotype | Clinical Recommendations | Recom. Authority | Level of Evidence | Genotyping Recommendations |
|---|---|---|---|---|---|---|
| Carbamazepine | HLA | HLA-B*15:02 negative and HLA-A*31:01 negative | Use standard dose as per guidelines | CPIC | 1A | Strong |
| HLA-B*15:02 negative and HLA-A*31:01 positive | If patient is CBZ-naïve and alternative agents are available, do not use CBZ | CPIC | 1A | Strong | ||
| HLA-B*15:02 positive and any HLA-A*31:01 genotype | If patient is CBZ-naïve, do not use CBZ | CPIC | 1A | Strong | ||
| HLA-B*15:02, HLA-A*31:01 and HLA-B*15:11 carriers | Choose an alternative | DPWG | 4E | Essential | ||
| HLA-B*15:02 positive | Alternative medication should be used as first-line therapy. | CPNDS | +++ | B-Moderate | ||
| HLA-A*31:01 positive | Alternative medication should be used as first-line therapy | CPNDS | +++ | B-Moderate | ||
| HLA-B*15:02 positive | CBZ is not recommended unless the benefits clearly outweigh the risks | FDA | - | - | ||
| HLA-A*31:01 positive | Risks and benefits should be weighed before prescription of CBZ | FDA | - | - | ||
| Oxcarbazepine | HLA-B | HLA-B*15:02 negative | Use OXC per standard dosing guidelines | CPIC | 1A | Strong |
| HLA-B*15:02 positive | If patient is oxcarbazepine naïve, do not use oxcarbazepine. | CPIC | 1A | Strong | ||
| HLA-B*15:02 positive | An alternative is recommended. If not possible, it is recommended to advise the patient to report any rash immediately. | DPWG | 4D | Beneficial (patients of Asian, not-Japanese and not-Korean, descent) | ||
| HLA-B*15:02 positive | Patients are at higher risk of SCARs. Genotyping is not a substitute for clinical vigilance | FDA | - | - | ||
| Abacavir | HLA-B | HLA-B*57:01 negative | Use abacavir per standard dosing guidelines | CPIC | 1A | Strong |
| HLA-B*57:01 positive | Abacavir is not recommended | CPIC | 1A | Strong | ||
| HLA-B*57:01 positive | Abacavir is contra-indicated. | DPWG | 4E | Essential | ||
| HLA-B*57:01 positive | Do not use abacavir | FDA | - | - | ||
| Allopurinol | HLA-B | HLA-B*58:01 negative | Use allopurinol per standard dosing guidelines | CPIC | 1A | Strong |
| HLA-B*58:01 positive | Allopurinol is contraindicated. | CPIC | 1A | Strong | ||
| HLA-B*58:01 positive | Choose an alternative, e.g., febuxostat or to precede treatment with allopurinol tolerance induction. | DPWG | 4F | - | ||
| HLA-B*58:01 positive | Results in higher severe skin reactions | FDA | - | - | ||
| Phenytoin | HLA-B | HLA-B*15:02 negative | Initiate therapy with recommended maintenance dose | CPIC | 1A | Strong |
| HLA-B*15:02 positive | If patient is phenytoin naive, do not use phenytoin | CPIC | 1A | Strong | ||
| HLA-B*15:02 positive | Phenytoin can induce the life-threatening cutaneous adverse events | DPWG | 4E | Beneficial (patients of Asian, but not Japanese and Korean descent) | ||
| Lamotrigine | HLA-B | HLA-B*15:02 | Considers genotyping of patients to be beneficial for drug safety. Avoided lamotrigine if possible, even if both the incidence and the risk increase are low | DPWG | 4E | Beneficial (patients of Asian but not Japanese and Korean descent) |
| Flucloxacillin | HLA-B | HLA-B*57:01 | Regularly monitor the patient’s liver function. Choose an alternative if liver enzymes and/or bilirubin levels are elevated | DPWG | 4F | - |
| Lamotrigine | HLA-B | HLA-B*15:02 | Considers genotyping of patients to be beneficial for drug safety. Avoided lamotrigine if possible, even if both the incidence and the risk increase are low | DPWG | 4E | Beneficial (patients of Asian but not Japanese and Korean descent) |
| Flucloxacillin | HLA-B | HLA-B*57:01 | Regularly monitor the patient’s liver function. Choose an alternative if liver enzymes and/or bilirubin levels are elevated | DPWG | 4F | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kloypan, C.; Koomdee, N.; Satapornpong, P.; Tempark, T.; Biswas, M.; Sukasem, C. A Comprehensive Review of HLA and Severe Cutaneous Adverse Drug Reactions: Implication for Clinical Pharmacogenomics and Precision Medicine. Pharmaceuticals 2021, 14, 1077. https://doi.org/10.3390/ph14111077
Kloypan C, Koomdee N, Satapornpong P, Tempark T, Biswas M, Sukasem C. A Comprehensive Review of HLA and Severe Cutaneous Adverse Drug Reactions: Implication for Clinical Pharmacogenomics and Precision Medicine. Pharmaceuticals. 2021; 14(11):1077. https://doi.org/10.3390/ph14111077
Chicago/Turabian StyleKloypan, Chiraphat, Napatrupron Koomdee, Patompong Satapornpong, Therdpong Tempark, Mohitosh Biswas, and Chonlaphat Sukasem. 2021. "A Comprehensive Review of HLA and Severe Cutaneous Adverse Drug Reactions: Implication for Clinical Pharmacogenomics and Precision Medicine" Pharmaceuticals 14, no. 11: 1077. https://doi.org/10.3390/ph14111077
APA StyleKloypan, C., Koomdee, N., Satapornpong, P., Tempark, T., Biswas, M., & Sukasem, C. (2021). A Comprehensive Review of HLA and Severe Cutaneous Adverse Drug Reactions: Implication for Clinical Pharmacogenomics and Precision Medicine. Pharmaceuticals, 14(11), 1077. https://doi.org/10.3390/ph14111077







