Opioid Dosage Levels, Concurrent Risk Factors and Self-Perceptions among Chronic Pain, Opioid-Managed Individuals at Elevated Risk for Opioid Overdose
Abstract
:1. Introduction
2. Results
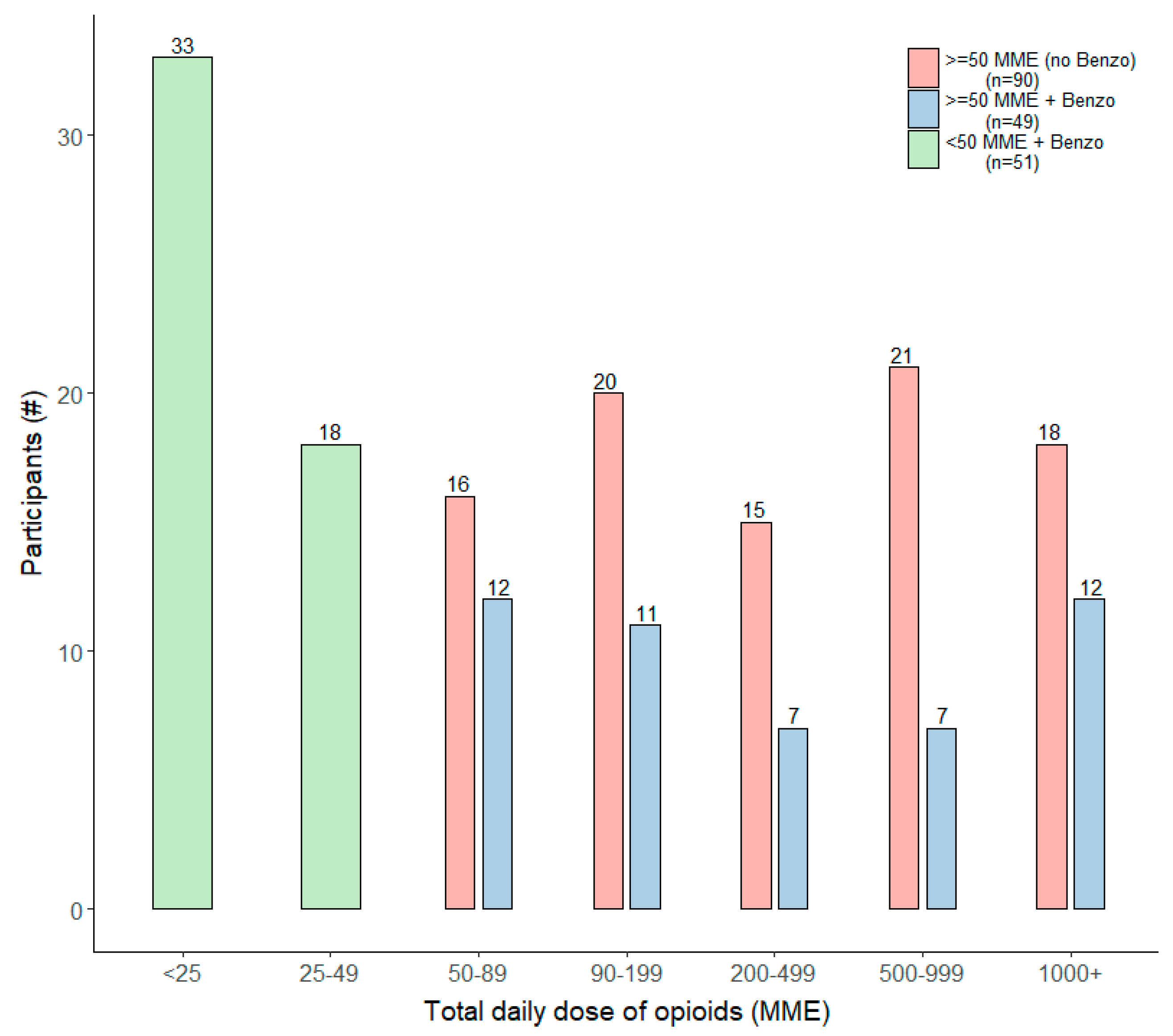
2.1. Distribution of Daily MME and Concomitant Benzodiazepine Use
2.2. Demographics of CPOM Sample
2.3. Prescription Drug Use and Opioid Overdose Risk Factors
2.4. Perceptions and Provider Communication about Opioid Dosage Level and Risks
2.5. Median Daily MME and Self-Perceptions
3. Discussion
4. Materials and Methods
4.1. Sample Development
4.2. Data Collection and Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Centers for Disease Control and Prevention. Drug Overdose Deaths in the U.S. up 30% in 2020. Available online: https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2021/20210714.htm (accessed on 31 October 2021).
- Centers for Disease Control and Prevention. Prescription Opioid Overdose Death Maps. Available online: https://www.cdc.gov/drugoverdose/deaths/prescription/maps.html (accessed on 31 October 2021).
- Dowell, D.; Haegerich, T.M.; Chou, R. CDC Guideline for Prescribing Opioids for Chronic Pain—United States, 2016. JAMA 2016, 315, 1624–1645. [Google Scholar] [CrossRef] [Green Version]
- Reuben, D.B.; Alvanzo, A.A.; Ashikaga, T.; Bogat, G.A.; Callahan, C.M.; Ruffing, V.; Steffens, D.C. National Institutes of Health Pathways to Prevention Workshop: The role of opioids in the treatment of chronic pain. Ann. Intern. Med. 2015, 162, 295–300. [Google Scholar] [CrossRef] [Green Version]
- Bohnert, A.S.B.; Guy, G.P., Jr.; Losby, J.L. Opioid Prescribing in the United States Before and after the Centers for Disease Control and Prevention’s 2016 Opioid Guideline. Ann. Intern. Med. 2018, 169, 367–375. [Google Scholar] [CrossRef]
- Encinosa, W.; Bernard, D.; Selden, T.M. Opioid and non-opioid analgesic prescribing before and after the CDC’s 2016 opioid guideline. Int. J. Health Econ. Manag. 2021, 1–52. [Google Scholar] [CrossRef]
- Goldstick, J.E.; Guy, G.P.; Losby, J.L.; Baldwin, G.; Myers, M.; Bohnert, A.S.B. Changes in Initial Opioid Prescribing Practices After the 2016 Release of the CDC Guideline for Prescribing Opioids for Chronic Pain. JAMA Netw. Open 2021, 4, e2116860. [Google Scholar] [CrossRef]
- Sutherland, T.N.; Wunsch, H.; Pinto, R.; Newcomb, C.; Brensinger, C.; Gaskins, L.; Bateman, B.T.; Neuman, M.D. Association of the 2016 US Centers for Disease Control and Prevention Opioid Prescribing Guideline With Changes in Opioid Dispensing After Surgery. JAMA Netw. Open 2021, 4, e2111826. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. U.S. Opioid Dispensing Rate Maps. Available online: https://www.cdc.gov/drugoverdose/rxrate-maps/index.html (accessed on 21 October 2021).
- Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results from the 2019 National Survey on Drug Use and Health (HHS Publication No. PEP20-07-01-001, NSDUH Series H-55); Rockville, M.D., Ed.; Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration: Rockville, MD, USA, 2020.
- Gomes, T.; Mamdani, M.M.; Dhalla, I.A.; Paterson, J.M.; Juurlink, D.N. Opioid dose and drug-related mortality in patients with nonmalignant pain. Arch. Intern. Med. 2011, 171, 686–691. [Google Scholar] [CrossRef] [Green Version]
- Dunn, K.M.; Saunders, K.W.; Rutter, C.M.; Banta-Green, C.J.; Merrill, J.O.; Sullivan, M.D.; Weisner, C.M.; Silverberg, M.J.; Campbell, C.I.; Psaty, B.M.; et al. Opioid prescriptions for chronic pain and overdose: A cohort study. Ann. Intern. Med. 2010, 152, 85–92. [Google Scholar] [CrossRef]
- Bohnert, A.S.; Valenstein, M.; Bair, M.J.; Ganoczy, D.; McCarthy, J.F.; Ilgen, M.A.; Blow, F.C. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA 2011, 305, 1315–1321. [Google Scholar] [CrossRef] [Green Version]
- Algera, M.H.; Olofsen, E.; Moss, L.; Dobbins, R.L.; Niesters, M.; van Velzen, M.; Groeneveld, G.J.; Heuberger, J.; Laffont, C.M.; Dahan, A. Tolerance to Opioid-Induced Respiratory Depression in Chronic High-Dose Opioid Users: A Model-Based Comparison With Opioid-Naive Individuals. Clin. Pharmacol. Ther. 2021, 109, 637–645. [Google Scholar] [CrossRef]
- Higgins, C.; Smith, B.H.; Matthews, K. Evidence of opioid-induced hyperalgesia in clinical populations after chronic opioid exposure: A systematic review and meta-analysis. Br. J. Anaesth. 2019, 122, e114–e126. [Google Scholar] [CrossRef] [Green Version]
- Jones, C.M.; McAninch, J.K. Emergency Department Visits and Overdose Deaths From Combined Use of Opioids and Benzodiazepines. Am. J. Prev. Med. 2015, 49, 493–501. [Google Scholar] [CrossRef]
- Chua, K.P.; Brummett, C.M.; Ng, S.; Bohnert, A.S.B. Association Between Receipt of Overlapping Opioid and Benzodiazepine Prescriptions From Multiple Prescribers and Overdose Risk. JAMA Netw. Open 2021, 4, e2120353. [Google Scholar] [CrossRef]
- Gladden, R.M.; O’Donnell, J.; Mattson, C.L.; Seth, P. Changes in Opioid-Involved Overdose Deaths by Opioid Type and Presence of Benzodiazepines, Cocaine, and Methamphetamine—25 States, July–December 2017 to January–June 2018. MMWR Morb. Mortal. Wkly. Rep. 2019, 68, 737–744. [Google Scholar] [CrossRef] [Green Version]
- Hernandez, I.; He, M.; Brooks, M.M.; Zhang, Y. Exposure-Response Association Between Concurrent Opioid and Benzodiazepine Use and Risk of Opioid-Related Overdose in Medicare Part D Beneficiaries. JAMA Netw. Open 2018, 1, e180919. [Google Scholar] [CrossRef] [Green Version]
- Park, T.W.; Saitz, R.; Ganoczy, D.; Ilgen, M.A.; Bohnert, A.S. Benzodiazepine prescribing patterns and deaths from drug overdose among US veterans receiving opioid analgesics: Case-cohort study. BMJ 2015, 350, h2698. [Google Scholar] [CrossRef] [Green Version]
- Sun, E.C.; Dixit, A.; Humphreys, K.; Darnall, B.D.; Baker, L.C.; Mackey, S. Association between concurrent use of prescription opioids and benzodiazepines and overdose: Retrospective analysis. BMJ 2017, 356, j760. [Google Scholar] [CrossRef] [Green Version]
- Liu, S.; O’Donnell, J.; Gladden, R.M.; McGlone, L.; Chowdhury, F. Trends in Nonfatal and Fatal Overdoses Involving Benzodiazepines—38 States and the District of Columbia, 2019–2020. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1136–1141. [Google Scholar] [CrossRef]
- Bair, M.J.; Robinson, R.L.; Katon, W.; Kroenke, K. Depression and pain comorbidity: A literature review. Arch. Intern. Med. 2003, 163, 2433–2445. [Google Scholar] [CrossRef] [Green Version]
- Fendrich, M.; Becker, J.; Hernandez-Meier, J. Psychiatric symptoms and recent overdose among people who use heroin or other opioids: Results from a secondary analysis of an intervention study. Addict. Behav. Rep. 2019, 10, 100212. [Google Scholar] [CrossRef]
- Nadpara, P.A.; Joyce, A.R.; Murrelle, E.L.; Carroll, N.W.; Carroll, N.V.; Barnard, M.; Zedler, B.K. Risk Factors for Serious Prescription Opioid-Induced Respiratory Depression or Overdose: Comparison of Commercially Insured and Veterans Health Affairs Populations. Pain Med. 2018, 19, 79–96. [Google Scholar] [CrossRef] [Green Version]
- Richards, G.C.; Mahtani, K.R.; Muthee, T.B.; DeVito, N.J.; Koshiaris, C.; Aronson, J.K.; Goldacre, B.; Heneghan, C.J. Factors associated with the prescribing of high-dose opioids in primary care: A systematic review and meta-analysis. BMC Med. 2020, 18, 68. [Google Scholar] [CrossRef] [Green Version]
- Scherrer, J.F.; Salas, J.; Copeland, L.A.; Stock, E.M.; Ahmedani, B.K.; Sullivan, M.D.; Burroughs, T.; Schneider, F.D.; Bucholz, K.K.; Lustman, P.J. Prescription Opioid Duration, Dose, and Increased Risk of Depression in 3 Large Patient Populations. Ann. Fam. Med. 2016, 14, 54–62. [Google Scholar] [CrossRef]
- Scherrer, J.F.; Salas, J.; Lustman, P.J.; Burge, S.; Schneider, F.D. Change in opioid dose and change in depression in a longitudinal primary care patient cohort. Pain 2015, 156, 348–355. [Google Scholar] [CrossRef]
- McCormick, C.D.; Dadiomov, D.; Trotzky-Sirr, R.; Qato, D.M. Prevalence and distribution of high-risk prescription opioid use in the United States, 2011–2016. Pharmacoepidemiol. Drug Saf. 2021, 30, 1532–1540. [Google Scholar] [CrossRef]
- Chau, D.L.; Walker, V.; Pai, L.; Cho, L.M. Opiates and elderly: Use and side effects. Clin. Interv. Aging 2008, 3, 273–278. [Google Scholar] [CrossRef] [Green Version]
- Fox, L.M.; Hoffman, R.S.; Vlahov, D.; Manini, A.F. Risk factors for severe respiratory depression from prescription opioid overdose. Addiction 2018, 113, 59–66. [Google Scholar] [CrossRef]
- Rubin, R. Limits on Opioid Prescribing Leave Patients With Chronic Pain Vulnerable. JAMA 2019, 321, 2059–2062. [Google Scholar] [CrossRef]
- Elabd, S. Mixed Reaction from Professional Groups on CDC Opioid Guideline. Top. Pain Manag. 2016, 32, 7–10. [Google Scholar] [CrossRef]
- Gray, B.M.; Vandergrift, J.L.; Weng, W.; Lipner, R.S.; Barnett, M.L. Clinical Knowledge and Trends in Physicians’ Prescribing of Opioids for New Onset Back Pain, 2009-2017. JAMA Netw. Open 2021, 4, e2115328. [Google Scholar] [CrossRef]
- Markovic, T.; Pedersen, C.E.; Massaly, N.; Vachez, Y.M.; Ruyle, B.; Murphy, C.A.; Abiraman, K.; Shin, J.H.; Garcia, J.J.; Yoon, H.J.; et al. Pain induces adaptations in ventral tegmental area dopamine neurons to drive anhedonia-like behavior. Nat. Neurosci. 2021, 24, 1601–1613. [Google Scholar] [CrossRef]
- Salas, J.; Li, X.; Xian, H.; Sullivan, M.D.; Ballantyne, J.C.; Lustman, P.J.; Grucza, R.; Scherrer, J.F. Opioid dosing among patients with 3 or more years of continuous prescription opioid use before and after the CDC opioid prescribing guideline. Int. J. Drug Policy 2021, 97, 103308. [Google Scholar] [CrossRef] [PubMed]
- Agnoli, A.; Xing, G.; Tancredi, D.J.; Magnan, E.; Jerant, A.; Fenton, J.J. Association of Dose Tapering With Overdose or Mental Health Crisis Among Patients Prescribed Long-term Opioids. JAMA 2021, 326, 411–419. [Google Scholar] [CrossRef]
- Green, T.C.; Davis, C.; Xuan, Z.; Walley, A.Y.; Bratberg, J. Laws Mandating Coprescription of Naloxone and Their Impact on Naloxone Prescription in Five US States, 2014-2018. Am. J. Public Health 2020, 110, 881–887. [Google Scholar] [CrossRef] [PubMed]
- Sohn, M.; Talbert, J.C.; Huang, Z.; Lofwall, M.R.; Freeman, P.R. Association of Naloxone Coprescription Laws With Naloxone Prescription Dispensing in the United States. JAMA Netw. Open 2019, 2, e196215. [Google Scholar] [CrossRef]

| TOTAL | ≥50 MME | BZD | |||
|---|---|---|---|---|---|
| (N = 190) | (n = 139, 73.2%) | (n = 100, 52.6%) | |||
| ≥50 MME + No BZD (n = 90, 47.4%) | ≥50 MME + BZD (n = 49, 25.8%) | <50 MME + BZD (n = 51, 26.8%) | sig. (χ2/F) | ||
| Gender | 0.735 | ||||
| Female | 120 (63.2%) | 54 (60%) | 31 (63.3%) | 35 (68.6%) | |
| Male | 69 (36.3%) | 35 (38.9%) | 18 (36.7%) | 16 (31.4%) | |
| Non-binary/third gender | 1 (0.5%) | 1 (1.1%) | 0 (0%) | 0 (0%) | |
| Age [Mean (±SE)] | 57 (±1.0) | 59.6 (±1.5) | 49.9 (±2.1) | 59.1 (±1.8) | <0.001 * |
| Race/Ethnicity | 0.402 | ||||
| Caucasian or white | 165 (86.8%) | 77 (85.6%) | 41 (83.7%) | 47 (92.2%) | |
| Non-white | 25 (13.2%) | 13 (14.4%) | 8 (16.3%) | 4 (7.8%) | |
| Educational Attainment | |||||
| High school graduate or less | 46 (24.2%) | 29 (32.2%) | 7 (14.3%) | 10 (19.6%) | 0.041 * |
| Vocational/trade school | 13 (6.8%) | 4 (4.4%) | 5 (10.2%) | 4 (7.8%) | 0.415 |
| Some college | 56 (29.5%) | 30 (33.3%) | 11 (22.4%) | 15 (29.4%) | 0.405 |
| College graduate or more | 75 (39.5%) | 27 (30%) | 26 (53.1%) | 22 (43.1%) | 0.024 * |
| Marital Status | |||||
| Married or living as married | 112 (58.9%) | 57 (63.3%) | 30 (61.2%) | 25 (49%) | 0.235 |
| Separated or divorced | 33 (17.4%) | 14 (15.6%) | 5 (10.2%) | 14 (27.5%) | 0.062 |
| Single, never been married | 27 (14.2%) | 10 (11.1%) | 10 (20.4%) | 7 (13.7%) | 0.323 |
| Widowed | 18 (9.5%) | 9 (10%) | 4 (8.2%) | 5 (9.8%) | 0.935 |
| Employment Status | |||||
| Retired | 82 (43.2%) | 47 (52.2%) | 15 (30.6%) | 20 (39.2%) | 0.039 * |
| Full-time employment | 58 (30.5%) | 21 (23.3%) | 22 (44.9%) | 15 (29.4%) | 0.030 * |
| Not employed | 22 (11.6%) | 11 (12.2%) | 5 (10.2%) | 6 (11.8%) | 0.938 |
| Homemaker | 17 (8.9%) | 6 (6.7%) | 6 (12.2%) | 5 (9.8%) | 0.529 |
| Part-time employment | 6 (3.2%) | 3 (3.3%) | 0 (0%) | 3 (5.9%) | 0.241 |
| Employment changed recently due to COVID-19 | 5 (2.6%) | 2 (2.2%) | 1 (2%) | 2 (3.9%) | 0.796 |
| Coverage for Prescription Medication | |||||
| Medicare Part D | 70 (36.8%) | 33 (36.7%) | 11 (22.4%) | 26 (51.0%) | 0.013 * |
| Insurance w/co-pay obtained through work or another organization | 44 (23.2%) | 21 (23.3%) | 13 (26.5%) | 10 (19.6%) | 0.713 |
| Private insurance-purchased directly from the insurance company | 33 (17.4%) | 12 (13.3%) | 15 (30.6%) | 6 (11.8%) | 0.017 * |
| Medicaid | 27 (14.2%) | 12 (13.3%) | 8 (16.3%) | 7 (13.7%) | 0.884 |
| Purchased all out of pocket/cash | 17 (8.9%) | 7 (7.8%) | 5 (10.2%) | 5 (9.8%) | 0.864 |
| Prescription discount card | 12 (6.3%) | 5 (5.6%) | 4 (8.2%) | 3 (5.9%) | 0.824 |
| VA or Military Insurance/Tricare | 8 (4.2%) | 5 (5.6%) | 3 (6.1%) | 0 (0%) | 0.213 |
| TOTAL | ≥50 MME | BZD | |||
|---|---|---|---|---|---|
| (N = 190) | (n = 139, 73.2%) | (n = 100, 52.6%) | |||
| ≥50 MME + No BZD (n = 90, 47.4%) | ≥50 MME + BZD (n = 49, 25.8%) | <50 MME + BZD (n = 51, 26.8%) | sig. (χ2/F) | ||
| Mean/Median daily dose of opioids (MME) [Mean (±SE)/Median] | 469.7 (±50.7)/120 | 596 (±69.5)/325 | 705.4 (±129)/301.2 | 20.2 (±1.7)/15 | <0.001 * |
| Prescription opioids taken daily for chronic pain | |||||
| Hydrocodone | 104 (54.7%) | 53 (58.9%) | 32 (65.3%) | 19 (37.3%) | 0.010 * |
| Oxycodone | 57 (30%) | 32 (35.6%) | 15 (30.6%) | 10 (19.6%) | 0.138 |
| Tramadol | 39 (20.5%) | 9 (10%) | 9 (18.4%) | 21 (41.2%) | <0.001 * |
| Morphine | 11 (5.8%) | 8 (8.9%) | 3 (6.1%) | 0 (0%) | 0.094 |
| Buprenorphine | 9 (4.7%) | 4 (4.4%) | 4 (8.2%) | 1 (2%) | 0.339 |
| Hydromorphone | 6 (3.2%) | 4 (4.4%) | 2 (4.1%) | 0 (0%) | 0.319 |
| Fentanyl | 5 (2.6%) | 1 (1.1%) | 3 (6.1%) | 1 (2%) | 0.199 |
| Oxymorphone | 1 (0.5%) | 1 (1.1%) | 0 (0%) | 0 (0%) | 0.572 |
| Other(s) | 14 (7.4%) | 4 (4.4%) | 4 (8.2%) | 6 (11.8%) | 0.270 |
| Number of prescription opioids taken daily for chronic pain | |||||
| One | 137 (72.1%) | 64 (71.1%) | 29 (59.2%) | 44 (86.3%) | 0.010 * |
| Two | 43 (22.6%) | 22 (24.4%) | 15 (30.6%) | 6 (11.8%) | 0.068 |
| Three | 6 (3.2%) | 1 (1.1%) | 4 (8.2%) | 1 (2%) | 0.064 |
| Four or more | 4 (2.1%) | 3 (3.3%) | 1 (2%) | 0 (0%) | 0.416 |
| Concomitant benzodiazepine use | |||||
| Alprazolam | 39 (39.0%) | - | 17 (34.7%) | 22 (43.1%) | 0.387 |
| Lorazepam | 28 (28.0%) | - | 13 (26.5%) | 15 (29.4%) | 0.748 |
| Clonazepam | 26 (26.0%) | - | 15 (30.6%) | 11 (21.6%) | 0.303 |
| Diazepam) | 22 (22.0%) | - | 13 (26.5%) | 9 (17.6%) | 0.284 |
| Clorazepate | 3 (3.0%) | - | 2 (4.1%) | 1 (2%) | 0.614 |
| Clobazam | 1 (1.0%) | - | 1 (2%) | 0 (0%) | 0.305 |
| Chlordiazepoxide | 1 (1.0%) | - | 1 (2%) | 0 (0%) | 0.490 |
| Lifetime history of diagnosis/treatment | |||||
| Anxiety, depression, or other mental health disorder | 100 (52.6%) | 30 (33.3%) | 33 (67.3%) | 37 (72.5%) | <0.001 * |
| Sleep breathing disorder (e.g., sleep apnea) | 55 (28.9%) | 24 (26.7%) | 18 (36.7%) | 13 (25.5%) | 0.374 |
| COPD | 38 (20.0%) | 16 (17.8%) | 12 (24.5%) | 10 (19.6%) | 0.638 |
| Kidney/liver disease | 15 (7.9%) | 8 (8.9%) | 4 (8.2%) | 3 (5.9%) | 0.814 |
| Any | 128 (67.4%) | 47 (52.2%) | 39 (79.6%) | 42 (82.4%) | <0.001 * |
| Number of days (in past month) ≥ 1 alcoholic drink was consumed | |||||
| One | 115 (61.8%) | 58 (65.2%) | 28 (57.1%) | 29 (60.4%) | 0.632 |
| Two | 19 (10.2%) | 6 (6.7%) | 9 (18.4%) | 4 (8.3%) | 0.086 |
| 3–4 | 25 (13.4%) | 10 (11.2%) | 6 (12.2%) | 9 (18.8%) | 0.450 |
| 5–9 | 14 (7.5%) | 7 (7.9%) | 2 (4.1%) | 5 (10.4%) | 0.490 |
| 10–20 | 7 (3.8%) | 2 (2.2%) | 4 (8.2%) | 1 (2.1%) | 0.169 |
| 20+ | 6 (3.2%) | 6 (6.7%) | 0 (0%) | 0 (0%) | 0.034 * |
| TOTAL | ≥50 MME | BZD | |||
|---|---|---|---|---|---|
| (N = 190) | (n = 139, 73.2%) | (n = 100, 52.6%) | |||
| Dosage | ≥50 MME + No BZD (n = 90, 47.4%) | ≥50 MME + BZD (n = 49, 25.8%) | <50 MME + BZD (n = 51, 26.8%) | sig. (χ2/F) | |
| Pharmacist/healthcare provider talked with you the dosage level of your prescribed opioid medication | 82 (43.2%) | 34 (37.8%) | 26 (53.1%) | 22 (43.1%) | 0.221 |
| What dose range do you consider your opioid pain medication to be? | |||||
| Low dose | 75 (39.5%) | 35 (38.9%) | 12 (24.5%) | 28 (54.9%) | 0.086 †,* |
| Moderate dose | 88 (46.3%) | 42 (46.7%) | 31 (63.3%) | 15 (29.4%) | 0.061 †,* |
| High dose | 11 (5.8%) | 6 (6.7%) | 4 (8.2%) | 1 (2%) | 0.742 † |
| Don’t know | 16 (8.4%) | 7 (7.8%) | 2 (4.1%) | 7 (13.7%) | 0.493 † |
| Overdose risk | |||||
| Pharmacist/healthcare provider talked with you about the risks, other than side effects, associated with your prescribed opioid medication | 111 (58.4%) | 46 (51.1%) | 36 (73.5%) | 29 (56.9%) | 0.037 * |
| Pharmacist/healthcare provider talked to you about the risks associated with taking an opioid and benzodiazepines at the same time | 64 (64.0%) | - | 34 (69.4%) | 30 (58.8%) | 0.271 |
| Is your opioid medication for chronic pain associated with a risk for overdose? | |||||
| Yes | 110 (57.9%) | 56 (62.2%) | 30 (61.2%) | 24 (47.1%) | 0.185 |
| No | 36 (18.9%) | 13 (14.4%) | 11 (22.4%) | 12 (23.5%) | 0.320 |
| Don’t know | 44 (23.2%) | 21 (23.3%) | 8 (16.3%) | 15 (29.4%) | 0.300 |
| Perceived risk of overdose when using opioids | |||||
| No risk | 118 (62.1%) | 61 (67.8%) | 27 (55.1%) | 30 (58.8%) | 0.289 |
| Slight risk | 44 (23.2%) | 15 (16.7%) | 14 (28.6%) | 15 (29.4%) | 0.131 |
| Moderate risk | 25 (13.2%) | 14 (15.6%) | 6 (12.2%) | 5 (9.8%) | 0.609 |
| High risk | 3 (1.6%) | 0 (0%) | 2 (4.1%) | 1 (2%) | 0.177 |
| Perceived concern of overdose when using opioids | |||||
| Not at all concerned | 114 (60.0%) | 57 (63.3%) | 28 (57.1%) | 29 (56.9%) | 0.673 |
| Not very concerned | 27 (14.2%) | 14 (15.6%) | 6 (12.2%) | 7 (13.7%) | 0.861 |
| Somewhat concerned | 25 (13.2%) | 8 (8.9%) | 11 (22.4%) | 6 (11.8%) | 0.073 |
| Very concerned | 19 (10.0%) | 8 (8.9%) | 4 (8.2%) | 7 (13.7%) | 0.579 |
| Extremely concerned | 5 (2.6%) | 3 (3.3%) | 0(0%) | 2 (3.9%) | 0.401 |
| Which of the following increases your risk of overdosing from an opioid? | |||||
| Taking more than prescribed at one time because one built up a tolerance and needed more for it to be effective | 130 (68.4%) | 58 (64.4%) | 35 (71.4%) | 37 (72.5%) | 0.531 |
| Using prescribed opioids more often or in larger amounts than directed or prescribed by a healthcare provider | 130 (68.4%) | 61 (67.8%) | 35 (71.4%) | 34 (66.7%) | 0.863 |
| Use of alcohol at the same time as a prescribed opioid | 125 (65.8%) | 57 (63.3%) | 33 (67.3%) | 35 (68.6%) | 0.788 |
| Taking someone else’s prescribed opioid | 106 (55.8%) | 53 (58.9%) | 25 (51%) | 28 (54.9%) | 0.664 |
| Forgetting to take a prescribed dose and then doubling up the next time | 101 (53.2%) | 50 (55.6%) | 26 (53.1%) | 25 (49%) | 0.756 |
| Taking prescribed opioids in combination with benzodiazepines | 89 (46.8%) | 40 (44.4%) | 26 (53.1%) | 23 (45.1%) | 0.597 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ellis, M.S.; Kasper, Z.A.; Gold, M.; Cicero, T.J. Opioid Dosage Levels, Concurrent Risk Factors and Self-Perceptions among Chronic Pain, Opioid-Managed Individuals at Elevated Risk for Opioid Overdose. Pharmaceuticals 2021, 14, 1279. https://doi.org/10.3390/ph14121279
Ellis MS, Kasper ZA, Gold M, Cicero TJ. Opioid Dosage Levels, Concurrent Risk Factors and Self-Perceptions among Chronic Pain, Opioid-Managed Individuals at Elevated Risk for Opioid Overdose. Pharmaceuticals. 2021; 14(12):1279. https://doi.org/10.3390/ph14121279
Chicago/Turabian StyleEllis, Matthew S., Zachary A. Kasper, Mark Gold, and Theodore J. Cicero. 2021. "Opioid Dosage Levels, Concurrent Risk Factors and Self-Perceptions among Chronic Pain, Opioid-Managed Individuals at Elevated Risk for Opioid Overdose" Pharmaceuticals 14, no. 12: 1279. https://doi.org/10.3390/ph14121279
APA StyleEllis, M. S., Kasper, Z. A., Gold, M., & Cicero, T. J. (2021). Opioid Dosage Levels, Concurrent Risk Factors and Self-Perceptions among Chronic Pain, Opioid-Managed Individuals at Elevated Risk for Opioid Overdose. Pharmaceuticals, 14(12), 1279. https://doi.org/10.3390/ph14121279







