Think Big, Start Small: How Nanomedicine Could Alleviate the Burden of Rare CNS Diseases
Abstract
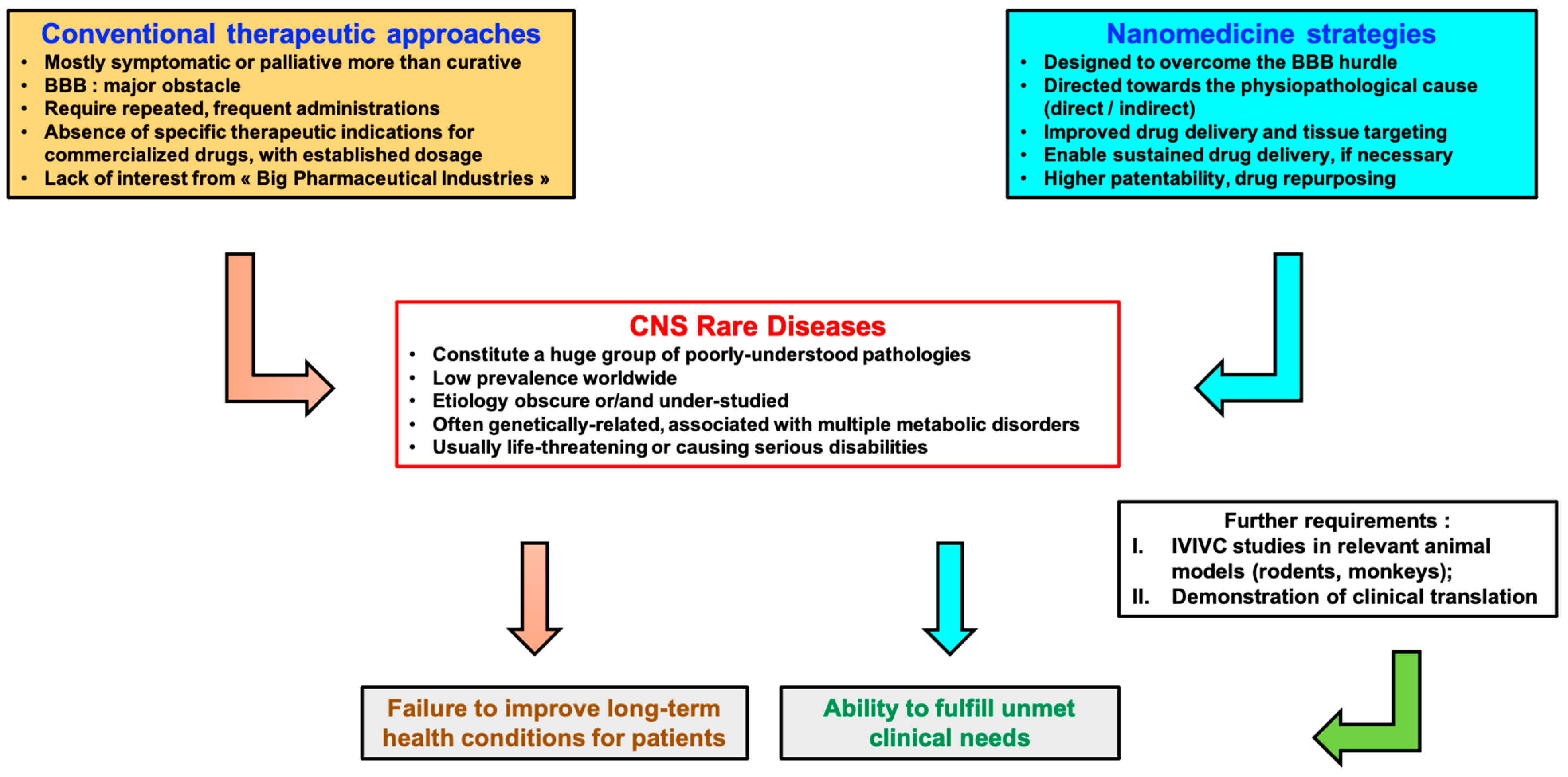
:1. Introduction
2. Nanocarriers Used for the Treatment of CNS Disorders and Strategies to Bypass the BBB
2.1. Parenteral Drug Delivery
2.2. Intranasal Drug Delivery
2.3. Intracarotid Infusion
2.4. Transmucosal Drug Delivery
2.5. Physical or Pharmacological Disruption of the BBB
3. CNS Disorders and Nanotherapeutics
3.1. Niemann–Pick Type C Disease—Nanocapturing Cholesterol
3.2. Spinocerebellar Ataxia—Delivering VEGF-Mimicking Nanoconstructs
3.3. Creatine Transporter Deficiency (CTD)—A Nasal Nanoemulsion for Brain Creatine Shipping
3.4. Mucopolysaccharidosis Type I (MPS I)—A Nano Gene Therapy
3.5. Rare Brain Infectious Diseases—How Nanomedicine Can Repurpose Clinically Approved Drugs
3.6. Primary Central Nervous System Lymphoma (PCNSL)—Enhancing BBB Crossing
4. Future Directions and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Conflicts of Interest
References
- van der Meel, R.; Sulheim, E.; Shi, Y.; Kiessling, F.; Mulder, W.J.M.; Lammers, T. Smart Cancer Nanomedicine. Nat. Nanotechnol. 2019, 14, 1007–1017. [Google Scholar] [CrossRef] [PubMed]
- Spencer, A.P.; Torrado, M.; Custódio, B.; Silva-Reis, S.C.; Santos, S.D.; Leiro, V.; Pêgo, A.P. Breaking Barriers: Bioinspired Strategies for Targeted Neuronal Delivery to the Central Nervous System. Pharmaceutics 2020, 12, 192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, G.; Chen, S.; Zhang, J. Bioinspired and Biomimetic Nanotherapies for the Treatment of Infectious Diseases. Front. Pharmacol. 2019, 10, 751. [Google Scholar] [CrossRef]
- Soares, S.; Sousa, J.; Pais, A.; Vitorino, C. Nanomedicine: Principles, Properties, and Regulatory Issues. Front. Chem. 2018, 6, 360. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Otormin, F.; Duro-Castano, A.; Conejos-Sánchez, I.; Vicent, M.J. Envisioning the Future of Polymer Therapeutics for Brain Disorders. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2019, 11, e1532. [Google Scholar] [CrossRef] [Green Version]
- Pardridge, W.M. The Blood-Brain Barrier: Bottleneck in Brain Drug Development. NeuroRX 2005, 2, 3–14. [Google Scholar] [CrossRef]
- Bernard-Patrzynski, F.; Lécuyer, M.-A.; Puscas, I.; Boukhatem, I.; Charabati, M.; Bourbonnière, L.; Ramassamy, C.; Leclair, G.; Prat, A.; Roullin, V.G. Isolation of Endothelial Cells, Pericytes and Astrocytes from Mouse Brain. PLoS ONE 2019, 14, e0226302. [Google Scholar] [CrossRef] [Green Version]
- De Jong, W.H.; Hagens, W.I.; Krystek, P.; Burger, M.C.; Sips, A.J.A.M.; Geertsma, R.E. Particle Size-Dependent Organ Distribution of Gold Nanoparticles after Intravenous Administration. Biomaterials 2008, 29, 1912–1919. [Google Scholar] [CrossRef]
- Ohta, S.; Kikuchi, E.; Ishijima, A.; Azuma, T.; Sakuma, I.; Ito, T. Investigating the Optimum Size of Nanoparticles for Their Delivery into the Brain Assisted by Focused Ultrasound-Induced Blood–Brain Barrier Opening. Sci. Rep. 2020, 10, 18220. [Google Scholar] [CrossRef]
- Brown, T.D.; Habibi, N.; Wu, D.; Lahann, J.; Mitragotri, S. Effect of Nanoparticle Composition, Size, Shape, and Stiffness on Penetration Across the Blood–Brain Barrier. ACS Biomater. Sci. Eng. 2020, 6, 4916–4928. [Google Scholar] [CrossRef]
- Lombardo, S.M.; Schneider, M.; Türeli, A.E.; Günday Türeli, N. Key for Crossing the BBB with Nanoparticles: The Rational Design. Beilstein J. Nanotechnol. 2020, 11, 866–883. [Google Scholar] [CrossRef] [PubMed]
- Ceña, V.; Játiva, P. Nanoparticle Crossing of Blood–Brain Barrier: A Road to New Therapeutic Approaches to Central Nervous System Diseases. Nanomedcine 2018, 13, 1513–1516. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, Y.; Peng, Z.; Seven, E.S.; Leblanc, R.M. Crossing the Blood-Brain Barrier with Nanoparticles. J. Control. Release 2018, 270, 290–303. [Google Scholar] [CrossRef] [PubMed]
- Commissioner, O. Of the Rare Diseases at FDA. Available online: https://www.fda.gov/patients/rare-diseases-fda (accessed on 10 September 2020).
- Moliner, A.M.; Waligora, J. The European Union Policy in the Field of Rare Diseases. In Rare Diseases Epidemiology: Update and Overview; Posada de la Paz, M., Taruscio, D., Groft, S.C., Eds.; Advances in Experimental Medicine and Biology; Springer International Publishing: Cham, Switzerland, 2017; Volume 1031, pp. 561–587. ISBN 978-3-319-67142-0. [Google Scholar]
- RARE Facts—Global Genes. Available online: https://globalgenes.org/rare-facts/ (accessed on 12 September 2020).
- Nervous System Diseases|Genetic and Rare Diseases Information Center (GARD)—An NCATS Program. Available online: https://rarediseases.info.nih.gov/diseases/diseases-by-category/17/nervous-system-diseases (accessed on 2 November 2020).
- Jones, T.; Townsend, D. History and Future Technical Innovation in Positron Emission Tomography. J. Med. Imaging 2017, 4, 011013. [Google Scholar] [CrossRef]
- Gribkoff, V.K.; Kaczmarek, L.K. The Need for New Approaches in CNS Drug Discovery: Why Drugs Have Failed, and What Can Be Done to Improve Outcomes. Neuropharmacology 2017, 120, 11–19. [Google Scholar] [CrossRef] [Green Version]
- Saunders, N.R.; Dziegielewska, K.M.; Møllgård, K.; Habgood, M.D. Markers for Blood-Brain Barrier Integrity: How Appropriate Is Evans Blue in the Twenty-First Century and What Are the Alternatives? Front. Neurosci. 2015, 9, 385. [Google Scholar] [CrossRef] [Green Version]
- Lockman, P.R.; Koziara, J.M.; Mumper, R.J.; Allen, D.D. Nanoparticle Surface Charges Alter Blood–Brain Barrier Integrity and Permeability. J. Drug Target. 2004, 12, 635–641. [Google Scholar] [CrossRef]
- Pimentel, E.; Sivalingam, K.; Doke, M.; Samikkannu, T. Effects of Drugs of Abuse on the Blood-Brain Barrier: A Brief Overview. Front. Neurosci. 2020, 14, 513. [Google Scholar] [CrossRef]
- Naqvi, S.; Panghal, A.; Flora, S.J.S. Nanotechnology: A Promising Approach for Delivery of Neuroprotective Drugs. Front. Neurosci. 2020, 14, 494. [Google Scholar] [CrossRef]
- Fornaguera, C.; García-Celma, M. Personalized Nanomedicine: A Revolution at the Nanoscale. J. Pers. Med. 2017, 7, 12. [Google Scholar] [CrossRef] [Green Version]
- Morigi, V.; Tocchio, A.; Bellavite Pellegrini, C.; Sakamoto, J.H.; Arnone, M.; Tasciotti, E. Nanotechnology in Medicine: From Inception to Market Domination. J. Drug Deliv. 2012, 2012, 1–7. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Mental Health (NIMH). A Phase I and II Study of PEG-Glucocerebrosidase in Patients with Type 1 or Type 3 Gaucher Disease. 2008. Available online: clinicaltrials.gov (accessed on 10 September 2020).
- Clinical Trial on Gaucher’s Disease: Lysodase—Clinical Trials Registry—ICH GCP. Available online: https://ichgcp.net/clinical-trials-registry/NCT00001410 (accessed on 26 October 2020).
- de Fost, M.; Hollak, C.E.M.; Groener, J.E.M.; Aerts, J.M.F.G.; Maas, M.; Poll, L.W.; Wiersma, M.G.; Häussinger, D.; Brett, S.; Brill, N.; et al. Superior Effects of High-Dose Enzyme Replacement Therapy in Type 1 Gaucher Disease on Bone Marrow Involvement and Chitotriosidase Levels: A 2-Center Retrospective Analysis. Blood 2006, 108, 830–835. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Degnan, A.J.; Ho-Fung, V.M.; Wang, D.-J.; Ficicioglu, C.; Jaramillo, D. Gaucher Disease Status and Treatment Assessment: Pilot Study Using Magnetic Resonance Spectroscopy Bone Marrow Fat Fractions in Pediatric Patients. Clin. Imaging 2020, 63, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Martín-Banderas, L.; Holgado, M.A.; Durán-Lobato, M.; Infante, J.J.; Álvarez-Fuentes, J.; Fernández-Arévalo, M. Role of Nanotechnology for Enzyme Replacement Therapy in Lysosomal Diseases. A Focus on Gaucher’s Disease. Curr. Med. Chem. 2016, 23, 929–952. [Google Scholar] [CrossRef]
- Kaur, I.P.; Sharma, G.; Singh, M.; Sandhu, S.K.; Deol, P.K.; Yadav, M.; Yakhmi, J.V. Nanobiomaterials as gene-delivery vehicles. In Nanobiomaterials in Drug Delivery; Elsevier: Amsterdam, The Netherlands, 2016; pp. 447–486. ISBN 978-0-323-42866-8. [Google Scholar] [CrossRef]
- Elsharkasy, O.M.; Nordin, J.Z.; Hagey, D.W.; de Jong, O.G.; Schiffelers, R.M.; Andaloussi, S.E.; Vader, P. Extracellular Vesicles as Drug Delivery Systems: Why and How? Adv. Drug Deliv. Rev. 2020, 159, 332–343. [Google Scholar] [CrossRef] [PubMed]
- Zylberberg, C.; Matosevic, S. Pharmaceutical Liposomal Drug Delivery: A Review of New Delivery Systems and a Look at the Regulatory Landscape. Drug Deliv. 2016, 23, 3319–3329. [Google Scholar] [CrossRef] [Green Version]
- Talelli, M.; Barz, M.; Rijcken, C.J.F.; Kiessling, F.; Hennink, W.E.; Lammers, T. Core-Crosslinked Polymeric Micelles: Principles, Preparation, Biomedical Applications and Clinical Translation. Nano Today 2015, 10, 93–117. [Google Scholar] [CrossRef] [Green Version]
- Kulkarni, J.A.; Cullis, P.R.; van der Meel, R. Lipid Nanoparticles Enabling Gene Therapies: From Concepts to Clinical Utility. Nucleic Acid Ther. 2018, 28, 146–157. [Google Scholar] [CrossRef] [Green Version]
- Saha, S.; Yakati, V.; Shankar, G.; Jaggarapu, M.M.C.S.; Moku, G.; Madhusudana, K.; Banerjee, R.; Ramkrishna, S.; Srinivas, R.; Chaudhuri, A. Amphetamine Decorated Cationic Lipid Nanoparticles Cross the Blood–Brain Barrier: Therapeutic Promise for Combating Glioblastoma. J. Mater. Chem. B 2020, 8, 4318–4330. [Google Scholar] [CrossRef]
- Duan, Y.; Dhar, A.; Patel, C.; Khimani, M.; Neogi, S.; Sharma, P.; Siva Kumar, N.; Vekariya, R.L. A Brief Review on Solid Lipid Nanoparticles: Part and Parcel of Contemporary Drug Delivery Systems. RSC Adv. 2020, 10, 26777–26791. [Google Scholar] [CrossRef]
- Zeng, Y.; Kurokawa, Y.; Zeng, Q.; Win-Shwe, T.-T.; Nansai, H.; Zhang, Z.; Sone, H. Effects of Polyamidoamine Dendrimers on a 3-D Neurosphere System Using Human Neural Progenitor Cells. Toxicol. Sci. 2016, 152, 128–144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leite, P.E.C.; Pereira, M.R.; Harris, G.; Pamies, D.; dos Santos, L.M.G.; Granjeiro, J.M.; Hogberg, H.T.; Hartung, T.; Smirnova, L. Suitability of 3D Human Brain Spheroid Models to Distinguish Toxic Effects of Gold and Poly-Lactic Acid Nanoparticles to Assess Biocompatibility for Brain Drug Delivery. Part. Fibre Toxicol. 2019, 16, 22. [Google Scholar] [CrossRef]
- Kafa, H.; Wang, J.T.-W.; Rubio, N.; Klippstein, R.; Costa, P.M.; Hassan, H.A.F.M.; Sosabowski, J.K.; Bansal, S.S.; Preston, J.E.; Abbott, N.J.; et al. Translocation of LRP1 Targeted Carbon Nanotubes of Different Diameters across the Blood–Brain Barrier in Vitro and in Vivo. J. Control. Release 2016, 225, 217–229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, S.; Li, C.; Qian, M.; Jiang, H.; Shi, W.; Chen, J.; Lächelt, U.; Wagner, E.; Lu, W.; Wang, Y.; et al. Augmented Glioma-Targeted Theranostics Using Multifunctional Polymer-Coated Carbon Nanodots. Biomaterials 2017, 141, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Paul, W.; Sharma, C.P. Inorganic nanoparticles for targeted drug delivery. In Biointegration of Medical Implant Materials; Elsevier: Amsterdam, The Netherlands, 2010; pp. 204–235. ISBN 978-1-84569-509-5. [Google Scholar] [CrossRef]
- Mulvihill, J.J.; Cunnane, E.M.; Ross, A.M.; Duskey, J.T.; Tosi, G.; Grabrucker, A.M. Drug Delivery across the Blood–Brain Barrier: Recent Advances in the Use of Nanocarriers. Nanomedcine 2020, 15, 205–214. [Google Scholar] [CrossRef] [PubMed]
- Griffith, J.I.; Rathi, S.; Zhang, W.; Zhang, W.; Drewes, L.R.; Sarkaria, J.N.; Elmquist, W.F. Addressing BBB Heterogeneity: A New Paradigm for Drug Delivery to Brain Tumors. Pharmaceutics 2020, 12, 1205. [Google Scholar] [CrossRef]
- Yi, X.; Manickam, D.S.; Brynskikh, A.; Kabanov, A.V. Agile Delivery of Protein Therapeutics to CNS. J. Control. Release 2014, 190, 637–663. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giunchedi, P.; Gavini, E.; Bonferoni, M.C. Nose-to-Brain Delivery. Pharmaceutics 2020, 12, 138. [Google Scholar] [CrossRef] [Green Version]
- Wang, Z.; Xiong, G.; Tsang, W.C.; Schätzlein, A.G.; Uchegbu, I.F. Nose-to-Brain Delivery. J. Pharmacol. Exp. Ther. 2019, 370, 593–601. [Google Scholar] [CrossRef] [Green Version]
- Rhea, E.M.; Logsdon, A.F.; Banks, W.A.; Erickson, M.E. Intranasal Delivery: Effects on the Neuroimmune Axes and Treatment of Neuroinflammation. Pharmaceutics 2020, 12, 1120. [Google Scholar] [CrossRef]
- Joshi, S.; Meyers, P.M.; Ornstein, E. Intracarotid Delivery of Drugs. Anesthesiology 2008, 109, 543–564. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Inamura, T.; Nomura, T.; Bartus, R.T.; Black, K.L. Intracarotid Infusion of RMP-7, a Bradykinin Analog: A Method for Selective Drug Delivery to Brain Tumors. J. Neurosurg. 1994, 81, 752–758. [Google Scholar] [CrossRef] [PubMed]
- Joshi, S.; Emala, C.W.; Pile-Spellman, J. Intra-Arterial Drug Delivery: A Concise Review. J. Neurosurg. Anesthesiol. 2007, 19, 111–119. [Google Scholar] [CrossRef] [PubMed]
- Abhang, P.; Momin, M.; Inamdar, M.; Kar, S. Transmucosal Drug Delivery—An Overview. Drug Deliv. Lett. 2014, 4, 26–37. [Google Scholar] [CrossRef]
- Pandey, P.K.; Sharma, A.K.; Gupta, U. Blood Brain Barrier: An Overview on Strategies in Drug Delivery, Realistic in Vitro Modeling and in Vivo Live Tracking. Tissue Barriers 2016, 4, e1129476. [Google Scholar] [CrossRef] [Green Version]
- Dong, X. Current Strategies for Brain Drug Delivery. Theranostics 2018, 8, 1481–1493. [Google Scholar] [CrossRef]
- Bleier, B.S.; Kohman, R.E.; Feldman, R.E.; Ramanlal, S.; Han, X. Permeabilization of the Blood-Brain Barrier via Mucosal Engrafting: Implications for Drug Delivery to the Brain. PLoS ONE 2013, 8, e61694. [Google Scholar] [CrossRef] [Green Version]
- Xie, J.; Shen, Z.; Anraku, Y.; Kataoka, K.; Chen, X. Nanomaterial-Based Blood-Brain-Barrier (BBB) Crossing Strategies. Biomaterials 2019, 224, 119491. [Google Scholar] [CrossRef]
- Chenthamara, D.; Subramaniam, S.; Ramakrishnan, S.G.; Krishnaswamy, S.; Essa, M.M.; Lin, F.-H.; Qoronfleh, M.W. Therapeutic Efficacy of Nanoparticles and Routes of Administration. Biomater. Res. 2019, 23, 20. [Google Scholar] [CrossRef]
- Marino, A.; Camponovo, A.; Degl’Innocenti, A.; Bartolucci, M.; Tapeinos, C.; Martinelli, C.; De Pasquale, D.; Santoro, F.; Mollo, V.; Arai, S.; et al. Multifunctional Temozolomide-Loaded Lipid Superparamagnetic Nanovectors: Dual Targeting and Disintegration of Glioblastoma Spheroids by Synergic Chemotherapy and Hyperthermia Treatment. Nanoscale 2019, 11, 21227–21248. [Google Scholar] [CrossRef]
- Kariolis, M.S.; Wells, R.C.; Getz, J.A.; Kwan, W.; Mahon, C.S.; Tong, R.; Kim, D.J.; Srivastava, A.; Bedard, C.; Henne, K.R.; et al. Brain Delivery of Therapeutic Proteins Using an Fc Fragment Blood-Brain Barrier Transport Vehicle in Mice and Monkeys. Sci. Transl. Med. 2020, 12, eaay1359. [Google Scholar] [CrossRef] [PubMed]
- Shilo, M.; Motiei, M.; Hana, P.; Popovtzer, R. Transport of Nanoparticles through the Blood–Brain Barrier for Imaging and Therapeutic Applications. Nanoscale 2014, 6, 2146–2152. [Google Scholar] [CrossRef] [PubMed]
- dos Santos Rodrigues, B.; Kanekiyo, T.; Singh, J. ApoE-2 Brain-Targeted Gene Therapy Through Transferrin and Penetratin Tagged Liposomal Nanoparticles. Pharm. Res. 2019, 36, 161. [Google Scholar] [CrossRef] [PubMed]
- Endo-Takahashi, Y.; Ooaku, K.; Ishida, K.; Suzuki, R.; Maruyama, K.; Negishi, Y. Preparation of Angiopep-2 Peptide-Modified Bubble Liposomes for Delivery to the Brain. Biol. Pharm. Bull. 2016, 39, 977–983. [Google Scholar] [CrossRef] [Green Version]
- Hoyos-Ceballos, G.P.; Ruozi, B.; Ottonelli, I.; Da Ros, F.; Vandelli, M.A.; Forni, F.; Daini, E.; Vilella, A.; Zoli, M.; Tosi, G.; et al. PLGA-PEG-ANG-2 Nanoparticles for Blood–Brain Barrier Crossing: Proof-of-Concept Study. Pharmaceutics 2020, 12, 72. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Farrington, G.K.; Caram-Salas, N.; Haqqani, A.S.; Brunette, E.; Eldredge, J.; Pepinsky, B.; Antognetti, G.; Baumann, E.; Ding, W.; Garber, E.; et al. A Novel Platform for Engineering Blood-brain Barrier-crossing Bispecific Biologics. FASEB J. 2014, 28, 4764–4778. [Google Scholar] [CrossRef] [Green Version]
- Gao, H.; Chu, C.; Cheng, Y.; Zhang, Y.; Pang, X.; Li, D.; Wang, X.; Ren, E.; Xie, F.; Bai, Y.; et al. In Situ Formation of Nanotheranostics to Overcome the Blood–Brain Barrier and Enhance Treatment of Orthotopic Glioma. ACS Appl. Mater. Interfaces 2020, 12, 26880–26892. [Google Scholar] [CrossRef]
- National Organization for Rare Disorders (NORD). Niemann Pick Disease Type C. Available online: https://rarediseases.org/rare-diseases/niemann-pick-disease-type-c/ (accessed on 3 November 2020).
- Griffin, L.D.; Gong, W.; Verot, L.; Mellon, S.H. Niemann–Pick Type C Disease Involves Disrupted Neurosteroidogenesis and Responds to Allopregnanolone. Nat. Med. 2004, 10, 704–711. [Google Scholar] [CrossRef]
- Pineda, M.; Walterfang, M.; Patterson, M.C. Miglustat in Niemann-Pick Disease Type C Patients: A Review. Orphanet J. Rare Dis. 2018, 13, 140. [Google Scholar] [CrossRef]
- Farmer, C.A.; Thurm, A.; Farhat, N.; Bianconi, S.; Keener, L.A.; Porter, F.D. Long-Term Neuropsychological Outcomes from an Open-Label Phase I/IIa Trial of 2-Hydroxypropyl-β-Cyclodextrins (VTS-270) in Niemann-Pick Disease, Type C1. CNS Drugs 2019, 33, 677–683. [Google Scholar] [CrossRef]
- Ridler, C. New Drug Slows Niemann–Pick Disease. Nat. Rev. Neurol. 2017, 13, 576–577. [Google Scholar] [CrossRef] [PubMed]
- Brown, A.; Patel, S.; Ward, C.; Lorenz, A.; Ortiz, M.; DuRoss, A.; Wieghardt, F.; Esch, A.; Otten, E.G.; Heiser, L.M.; et al. PEG-Lipid Micelles Enable Cholesterol Efflux in Niemann-Pick Type C1 Disease-Based Lysosomal Storage Disorder. Sci. Rep. 2016, 6, 31750. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klockgether, T.; Mariotti, C.; Paulson, H.L. Spinocerebellar Ataxia. Nat. Rev. Dis. Primer 2019, 5, 24. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, R.; Yau, W.Y.; O’Connor, E.; Houlden, H. Spinocerebellar Ataxia: An Update. J. Neurol. 2019, 266, 533–544. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ruano, L.; Melo, C.; Silva, M.C.; Coutinho, P. The Global Epidemiology of Hereditary Ataxia and Spastic Paraplegia: A Systematic Review of Prevalence Studies. Neuroepidemiology 2014, 42, 174–183. [Google Scholar] [CrossRef]
- Durr, A. Autosomal Dominant Cerebellar Ataxias: Polyglutamine Expansions and Beyond. Lancet Neurol. 2010, 9, 885–894. [Google Scholar] [CrossRef]
- Clarke, J.; Wu, H.-C.; Jayasinghe, L.; Patel, A.; Reid, S.; Bayley, H. Continuous Base Identification for Single-Molecule Nanopore DNA Sequencing. Nat. Nanotechnol. 2009, 4, 265–270. [Google Scholar] [CrossRef]
- Webber, M.J.; Tongers, J.; Newcomb, C.J.; Marquardt, K.-T.; Bauersachs, J.; Losordo, D.W.; Stupp, S.I. Supramolecular Nanostructures That Mimic VEGF as a Strategy for Ischemic Tissue Repair. Proc. Natl. Acad. Sci. USA 2011, 108, 13438–13443. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, Y.-S.; Do, J.; Edamakanti, C.R.; Kini, A.R.; Martina, M.; Stupp, S.I.; Opal, P. Self-Assembling Vascular Endothelial Growth Factor Nanoparticles Improve Function in Spinocerebellar Ataxia Type 1. Brain 2019, 142, 312–321. [Google Scholar] [CrossRef]
- Cvetanovic, M.; Patel, J.M.; Marti, H.H.; Kini, A.R.; Opal, P. Vascular Endothelial Growth Factor Ameliorates the Ataxic Phenotype in a Mouse Model of Spinocerebellar Ataxia Type 1. Nat. Med. 2011, 17, 1445–1447. [Google Scholar] [CrossRef]
- Rafferty, J.; Nagaraj, H.; McCloskey, A.P.; Huwaitat, R.; Porter, S.; Albadr, A.; Laverty, G. Peptide Therapeutics and the Pharmaceutical Industry: Barriers Encountered Translating from the Laboratory to Patients. Curr. Med. Chem. 2016, 23, 4231–4259. [Google Scholar] [CrossRef] [PubMed]
- Storkebaum, E.; Lambrechts, D.; Dewerchin, M.; Moreno-Murciano, M.-P.; Appelmans, S.; Oh, H.; Van Damme, P.; Rutten, B.; Man, W.Y.; De Mol, M.; et al. Treatment of Motoneuron Degeneration by Intracerebroventricular Delivery of VEGF in a Rat Model of ALS. Nat. Neurosci. 2005, 8, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Clark, J.F.; Cecil, K.M. Diagnostic Methods and Recommendations for the Cerebral Creatine Deficiency Syndromes. Pediatr. Res. 2015, 77, 398–405. [Google Scholar] [CrossRef] [PubMed]
- Andres, R.H.; Ducray, A.D.; Schlattner, U.; Wallimann, T.; Widmer, H.R. Functions and Effects of Creatine in the Central Nervous System. Brain Res. Bull. 2008, 76, 329–343. [Google Scholar] [CrossRef]
- National Organization for Rare Disorders (NORD). Cerebral Creatine Deficiency Syndromes. Available online: https://rarediseases.org/rare-diseases/cerebral-creatine-deficiency-syndromes/ (accessed on 5 September 2020).
- Salomons, G.S.; van Dooren, S.J.M.; Verhoeven, N.M.; Cecil, K.M.; Ball, W.S.; Degrauw, T.J.; Jakobs, C. X-Linked Creatine-Transporter Gene (SLC6A8) Defect: A New Creatine-Deficiency Syndrome. Am. J. Hum. Genet. 2001, 68, 1497–1500. [Google Scholar] [CrossRef] [Green Version]
- Ullio-Gamboa, G.; Udobi, K.C.; Dezard, S.; Perna, M.K.; Miles, K.N.; Costa, N.; Taran, F.; Pruvost, A.; Benoit, J.-P.; Skelton, M.R.; et al. Dodecyl Creatine Ester-Loaded Nanoemulsion as a Promising Therapy for Creatine Transporter Deficiency. Nanomed. 2019, 14, 1579–1593. [Google Scholar] [CrossRef]
- Trotier-Faurion, A.; Dézard, S.; Taran, F.; Valayannopoulos, V.; de Lonlay, P.; Mabondzo, A. Synthesis and Biological Evaluation of New Creatine Fatty Esters Revealed Dodecyl Creatine Ester as a Promising Drug Candidate for the Treatment of the Creatine Transporter Deficiency. J. Med. Chem. 2013, 56, 5173–5181. [Google Scholar] [CrossRef]
- Wraith, J.E.; Jones, S. Mucopolysaccharidosis Type I. Pediatr. Endocrinol. Rev. PER 2014, 12 (Suppl. 1), 102–106. [Google Scholar]
- Orphanet: Mucopolysaccharidosis Type 1. Available online: https://www.orpha.net/consor/cgi-bin/OC_Exp.php?lng=en&Expert=579 (accessed on 12 November 2020).
- Scarpa, M.; Orchard, P.J.; Schulz, A.; Dickson, P.I.; Haskins, M.E.; Escolar, M.L.; Giugliani, R. Treatment of Brain Disease in the Mucopolysaccharidoses. Mol. Genet. Metab. 2017, 122, 25–34. [Google Scholar] [CrossRef]
- Beck, M.; Arn, P.; Giugliani, R.; Muenzer, J.; Okuyama, T.; Taylor, J.; Fallet, S. The Natural History of MPS I: Global Perspectives from the MPS I Registry. Genet. Med. 2014, 16, 759–765. [Google Scholar] [CrossRef] [Green Version]
- Wraith, J.E.; Clarke, L.A.; Beck, M.; Kolodny, E.H.; Pastores, G.M.; Muenzer, J.; Rapoport, D.M.; Berger, K.I.; Swiedler, S.J.; Kakkis, E.D.; et al. Enzyme Replacement Therapy for Mucopolysaccharidosis I: A Randomized, Double-Blinded, Placebo-Controlled, Multinational Study of Recombinant Human α-L-Iduronidase (Laronidase). J. Pediatr. 2004, 144, 581–588. [Google Scholar] [CrossRef] [PubMed]
- Yin, H.; Kanasty, R.L.; Eltoukhy, A.A.; Vegas, A.J.; Dorkin, J.R.; Anderson, D.G. Non-Viral Vectors for Gene-Based Therapy. Nat. Rev. Genet. 2014, 15, 541–555. [Google Scholar] [CrossRef] [PubMed]
- Schuh, R.S.; Baldo, G.; Teixeira, H.F. Nanotechnology Applied to Treatment of Mucopolysaccharidoses. Expert Opin. Drug Deliv. 2016, 13, 1709–1718. [Google Scholar] [CrossRef] [PubMed]
- Jayant, R.D.; Sosa, D.; Kaushik, A.; Atluri, V.; Vashist, A.; Tomitaka, A.; Nair, M. Current Status of Non-Viral Gene Therapy for CNS Disorders. Expert Opin. Drug Deliv. 2016, 13, 1433–1445. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fraga, M.; de Carvalho, T.G.; da Silva Diel, D.; Bruxel, F.; Filho, N.A.K.; Teixeira, H.F.; Matte, U. Cationic Nanoemulsions as a Gene Delivery System: Proof of Concept in the Mucopolysaccharidosis I Murine Model. J. Nanosci. Nanotechnol. 2015, 15, 810–816. [Google Scholar] [CrossRef]
- Fraga, M.; Bruxel, F.; Diel, D.; de Carvalho, T.G.; Perez, C.A.; Magalhães-Paniago, R.; Malachias, Â.; Oliveira, M.C.; Matte, U.; Teixeira, H.F. PEGylated Cationic Nanoemulsions Can Efficiently Bind and Transfect PIDUA in a Mucopolysaccharidosis Type I Murine Model. J. Control. Release 2015, 209, 37–46. [Google Scholar] [CrossRef]
- Schuh, R.S.; Poletto, É.; Pasqualim, G.; Tavares, A.M.V.; Meyer, F.S.; Gonzalez, E.A.; Giugliani, R.; Matte, U.; Teixeira, H.F.; Baldo, G. In Vivo Genome Editing of Mucopolysaccharidosis I Mice Using the CRISPR/Cas9 System. J. Control. Release 2018, 288, 23–33. [Google Scholar] [CrossRef]
- Pickar-Oliver, A.; Gersbach, C.A. The next Generation of CRISPR–Cas Technologies and Applications. Nat. Rev. Mol. Cell Biol. 2019, 20, 490–507. [Google Scholar] [CrossRef]
- Yin, H.; Song, C.-Q.; Dorkin, J.R.; Zhu, L.J.; Li, Y.; Wu, Q.; Park, A.; Yang, J.; Suresh, S.; Bizhanova, A.; et al. Therapeutic Genome Editing by Combined Viral and Non-Viral Delivery of CRISPR System Components in Vivo. Nat. Biotechnol. 2016, 34, 328–333. [Google Scholar] [CrossRef]
- Visvesvara, G.S.; Stehr-Green, J.K. Epidemiology of Free-Living Ameba Infections 1. J. Protozool. 1990, 37, 25s–33s. [Google Scholar] [CrossRef]
- Guarner, J.; Bartlett, J.; Shieh, W.-J.; Paddock, C.D.; Visvesvara, G.S.; Zaki, S.R. Histopathologic Spectrum and Immunohistochemical Diagnosis of Amebic Meningoencephalitis. Mod. Pathol. 2007, 20, 1230–1237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Primary Amebic Meningoencephalitis (PAM)—Naegleria Fowleri|Parasites|CDC. Available online: https://www.cdc.gov/parasites/naegleria/index.html (accessed on 18 November 2020).
- CDC—Acanthamoeba Infection. Available online: https://www.cdc.gov/parasites/acanthamoeba/index.html (accessed on 18 November 2020).
- Mungroo, M.R.; Khan, N.A.; Siddiqui, R. Naegleria Fowleri: Diagnosis, Treatment Options and Pathogenesis. Expert Opin. Orphan Drugs 2019, 7, 67–80. [Google Scholar] [CrossRef]
- Samaridou, E.; Alonso, M.J. Nose-to-Brain Peptide Delivery—The Potential of Nanotechnology. Bioorg. Med. Chem. 2018, 26, 2888–2905. [Google Scholar] [CrossRef] [PubMed]
- Matanock, A.; Mehal, J.M.; Liu, L.; Blau, D.M.; Cope, J.R. Estimation of Undiagnosed Naegleria Fowleri Primary Amebic Meningoencephalitis, United States1. Emerg. Infect. Dis. 2018, 24, 162–164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Global Impact. Available online: http://www.cdipd.org/index.php/naegleriasis-global-impact (accessed on 25 December 2020).
- Gharpure, R.; Gleason, M.; Salah, Z.; Blackstock, A.J.; Hess-Homeier, D.; Yoder, J.S.; Ali, I.K.M.; Collier, S.A.; Cope, J.R. Early Release—Geographic Range of Recreational Water-Associated Primary Amebic Meningoencephalitis, United States, 1978–2018. Emerg. Infect. Dis. 2021, 27, 271–274. [Google Scholar] [CrossRef] [PubMed]
- Debnath, A.; Nelson, A.T.; Silva-Olivares, A.; Shibayama, M.; Siegel, D.; McKerrow, J.H. In Vitro Efficacy of Ebselen and BAY 11-7082 Against Naegleria Fowleri. Front. Microbiol. 2018, 9, 414. [Google Scholar] [CrossRef] [Green Version]
- Grace, E.; Asbill, S.; Virga, K. Naegleria Fowleri: Pathogenesis, Diagnosis, and Treatment Options. Antimicrob. Agents Chemother. 2015, 59, 6677–6681. [Google Scholar] [CrossRef] [Green Version]
- Rajendran, K.; Anwar, A.; Khan, N.A.; Siddiqui, R. Brain-Eating Amoebae: Silver Nanoparticle Conjugation Enhanced Efficacy of Anti-Amoebic Drugs against Naegleria fowleri. ACS Chem. Neurosci. 2017, 8, 2626–2630. [Google Scholar] [CrossRef]
- Anwar, A.; Siddiqui, R.; Hussain, M.A.; Ahmed, D.; Shah, M.R.; Khan, N.A. Silver Nanoparticle Conjugation Affects Antiacanthamoebic Activities of Amphotericin B, Nystatin, and Fluconazole. Parasitol. Res. 2018, 117, 265–271. [Google Scholar] [CrossRef]
- Lee, B.; Lee, M.J.; Yun, S.J.; Kim, K.; Choi, I.-H.; Park, S. Silver Nanoparticles Induce Reactive Oxygen Species-Mediated Cell Cycle Delay and Synergistic Cytotoxicity with 3-Bromopyruvate in Candida Albicans, but Not in Saccharomyces Cerevisiae. Int. J. Nanomed. 2019, 14, 4801–4816. [Google Scholar] [CrossRef] [Green Version]
- Anwar, A.; Rajendran, K.; Siddiqui, R.; Raza Shah, M.; Khan, N.A. Clinically Approved Drugs against CNS Diseases as Potential Therapeutic Agents to Target Brain-Eating Amoebae. ACS Chem. Neurosci. 2019, 10, 658–666. [Google Scholar] [CrossRef] [PubMed]
- Zakusov, V.V.; Ostrovskaya, R.U.; Kozhechkin, S.N.; Markovich, V.V.; Molodavkin, G.M.; Voronina, T.A. Further Evidence for GABA-Ergic Mechanisms in the Action of Benzodiazepines. Arch. Int. Pharmacodyn. Ther. 1977, 229, 313–326. [Google Scholar] [PubMed]
- Schwarz, J.R. The Mode of Action of Phenobarbital on the Excitable Membrane of the Node of Ranvier. Eur. J. Pharmacol. 1979, 56, 51–60. [Google Scholar] [CrossRef]
- Yaari, Y.; Selzer, M.E.; Pincus, J.H. Phenytoin: Mechanisms of Its Anticonvulsant Action. Ann. Neurol. 1986, 20, 171–184. [Google Scholar] [CrossRef] [PubMed]
- Rajendran, K.; Anwar, A.; Khan, N.A.; Aslam, Z.; Raza Shah, M.; Siddiqui, R. Oleic Acid Coated Silver Nanoparticles Showed Better in Vitro Amoebicidal Effects against Naegleria Fowleri than Amphotericin B. ACS Chem. Neurosci. 2020, 11, 2431–2437. [Google Scholar] [CrossRef]
- Sales-Campos, H.; de Souza, P.R.; Peghini, B.C.; da Silva, J.S.; Cardoso, C.R. An Overview of the Modulatory Effects of Oleic Acid in Health and Disease. Mini Rev. Med. Chem. 2013, 13, 201–210. [Google Scholar]
- Anwar, A.; Abdalla, S.A.O.; Aslam, Z.; Shah, M.R.; Siddiqui, R.; Khan, N.A. Oleic Acid–Conjugated Silver Nanoparticles as Efficient Antiamoebic Agent against Acanthamoeba Castellanii. Parasitol. Res. 2019, 118, 2295–2304. [Google Scholar] [CrossRef]
- Anwar, A.; Soomaroo, A.; Anwar, A.; Siddiqui, R.; Khan, N.A. Metformin-Coated Silver Nanoparticles Exhibit Anti-Acanthamoebic Activities against Both Trophozoite and Cyst Stages. Exp. Parasitol. 2020, 215, 107915. [Google Scholar] [CrossRef]
- Grommes, C.; DeAngelis, L.M. Primary CNS Lymphoma. J. Clin. Oncol. 2017, 35, 2410–2418. [Google Scholar] [CrossRef]
- Shiels, M.S.; Pfeiffer, R.M.; Besson, C.; Clarke, C.A.; Morton, L.M.; Nogueira, L.; Pawlish, K.; Yanik, E.L.; Suneja, G.; Engels, E.A. Trends in Primary Central Nervous System Lymphoma Incidence and Survival in the U.S. Br. J. Haematol. 2016, 174, 417–424. [Google Scholar] [CrossRef] [Green Version]
- Illerhaus, G.; Schorb, E.; Kasenda, B. Novel Agents for Primary Central Nervous System Lymphoma: Evidence and Perspectives. Blood 2018, 132, 681–688. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Orphanet: Primary Central Nervous System Lymphoma. Available online: https://www.orpha.net/consor/cgi-bin/OC_Exp.php?lng=en&Expert=46135 (accessed on 3 December 2020).
- Chapuy, B.; Stewart, C.; Dunford, A.J.; Kim, J.; Kamburov, A.; Redd, R.A.; Lawrence, M.S.; Roemer, M.G.M.; Li, A.J.; Ziepert, M.; et al. Molecular Subtypes of Diffuse Large B Cell Lymphoma Are Associated with Distinct Pathogenic Mechanisms and Outcomes. Nat. Med. 2018, 24, 679–690. [Google Scholar] [CrossRef] [PubMed]
- Aldape, K.; Brindle, K.M.; Chesler, L.; Chopra, R.; Gajjar, A.; Gilbert, M.R.; Gottardo, N.; Gutmann, D.H.; Hargrave, D.; Holland, E.C.; et al. Challenges to Curing Primary Brain Tumours. Nat. Rev. Clin. Oncol. 2019, 16, 509–520. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alphandéry Nano-Therapies for Glioblastoma Treatment. Cancers 2020, 12, 242. [CrossRef] [Green Version]
- Shi, X.-X.; Miao, W.-M.; Pang, D.-W.; Wu, J.-S.; Tong, Q.-S.; Li, J.-X.; Luo, J.-Q.; Li, W.-Y.; Du, J.-Z.; Wang, J. Angiopep-2 Conjugated Nanoparticles Loaded with Doxorubicin for the Treatment of Primary Central Nervous System Lymphoma. Biomater. Sci. 2020, 8, 1290–1297. [Google Scholar] [CrossRef] [PubMed]
- Xin, H.; Jiang, X.; Gu, J.; Sha, X.; Chen, L.; Law, K.; Chen, Y.; Wang, X.; Jiang, Y.; Fang, X. Angiopep-Conjugated Poly(Ethylene Glycol)-Co-Poly(ε-Caprolactone) Nanoparticles as Dual-Targeting Drug Delivery System for Brain Glioma. Biomaterials 2011, 32, 4293–4305. [Google Scholar] [CrossRef]
- Zhao, Y.; Li, D.; Zhao, J.; Song, J.; Zhao, Y. The Role of the Low-Density Lipoprotein Receptor–Related Protein 1 (LRP-1) in Regulating Blood-Brain Barrier Integrity. Rev. Neurosci. 2016, 27, 623–634. [Google Scholar] [CrossRef]

| Origin | Nanocarrier Designation | Size Range * (nm) | Primary Material | Benefits (+) and Disadvantages (−) | Ref. |
|---|---|---|---|---|---|
| Biological | Viral vectors | <100 | Viral capsid proteins | (+) High transfection efficiency (−) High immunogenicity, high production costs, important adverse effect risks | [31] |
| Extracellular vesicles | 50–500 | Plasma membrane phospholipids | (+) Good safety profile, enhanced specific targeting, controlled pharmacokinetics (−) Very limited data, inadequate in vivo targeting efficiency | [32] | |
| Biologically mimicking | Liposomes | 20–250 | Phospholipids | (+) Drug protection, passive diffusion across the BBB, adapted for both hydrophilic and hydrophobic drugs, possible specific targeting (−) Potential (neuro)toxicity, physicochemical instability, clearance issues | [33] |
| Chemical | Micelles | 10–100 | Surfactants | (+) Absence of neurotoxicity, enhanced drug bioavailability, physicochemical stability, ability to control drug release (−) For lipophilic drugs only, poor drug loading efficiency, physicochemical instability | [34] |
| Lipid nanoparticles (LNPs) | <100 | Cationic lipids | (+) Improved drug loading of genetic material, stability (−) Immunogenicity issues, do not passively target BBB, rapidly cleared from blood | [35,36] | |
| Solid lipid nanoparticles (SLNs) | 50–500 | Solid lipids | (+) Biocompatibility and degradability, absence of neurotoxicity, drug protection, improved control drug release, ability to cross the BBB via passive diffusion (−) Reduced loading efficiency for hydrophilic drugs | [37] | |
| Dendrimers | <10 | Organic dendrons | (+) Adapted for both hydrophilic and hydrophobic drugs, enhanced specific targeting, physicochemical stability (−) Potential (neuro)toxicity, clearance issues, potential organ accumulation | [38] | |
| Polymeric nanoparticles | <500 | Synthetic or natural polymers | (+) Biocompatibility, possible biodegradability, drug protection, ability to control/sustained drug release, enhanced specific targeting (−) Potential (neuro)toxicity (neuroinflammation, neurodegeneration) | [39] | |
| Carbon nanoparticles (nanotubes CNT, quantum dots QD) | <10 (QD) <100 (CNT) | Carbon | (+) Specific chemical, mechanical, and electrical properties, accumulation in brain tissue, enhanced surface functionalization (−) (Neuro)toxicity issues (absence of degradation, accumulation) | [40,41] | |
| Inorganic nanoparticles | 2–100 | Au, Ag, ZnO, Si, ceramic NPs, superparamagnetic iron oxide NPs (SPIONs) | (+) Electrical, mechanical and optical properties, high surface area useful for grafting targeting moieties (−) Established (neuro)toxicity, requires prior functionalization to cross the BBB | [42] |
| Targeting Moiety | Endothelial Target | Examples of ‘Nano’ Applications | Ref. |
|---|---|---|---|
| Transferrin (Tf), lactoferrin (Lf), anti-TfR antibodies or aptamers | Tf receptors (TfR) | Lipid SPION nanovectors loaded functionalized with antibodies against the transferrin receptor | [58] |
| TfR-binding Fc polypeptide | [59] | ||
| Insulin | Insulin receptor | Insulin PEG-coated gold particles | [60] |
| ApoB, ApoE, Angiopep-2 | Low density lipoprotein receptors (LDLR) | ApoE2 loaded brain-targeted functionalized-liposomes | [61] |
| Angiopep-2 Peptide-Modified Bubble Liposomes | [62] | ||
| PLGA-PEG-Ang–2 nanoparticles | [63] | ||
| FC5 | Cell surface α(2,3)-sialoglycoprotein (namely TMEM-30A) | FC5 bivalently fused with human Fc domain | [64] |
| Arginine-Glycine-Aspartic (RGD) peptide | Integrin receptors | RGD peptide-modified ultrasmall Au-ICG nanoparticles | [65] |
| Strategy | Summary | Example(s) of Treated Pathology | Biological Model or Clinical Stage | References | |
|---|---|---|---|---|---|
| Suppress Cause of Disease | Gene therapy | Nanocarriers can deliver genes in a safer, non-viral way. Genes will then express the absent or deficient protein in therapeutic levels. They can also “complex” or “load” excess of substances causing brain damages due to proper physicochemical engineering. | Niemann–Pick type C disease | Phase IIb/III | [70] |
| Capture therapy | Mucopolysacchari-dosis type I (MPS I) | In vivo (mice); ex vivo (MPS I patients fibroblasts) | [96,97,98] | ||
| Target Cell Defect | Nanoencapsulation may allow the delivery of intact peptides or proteins by protecting them against chemical and biological degradations. | Spinocerebellar ataxia | In vivo (mice) and ex vivo (ischemic limb model) | [77,78] | |
| Supplement Deficiency Protein/Peptide Delivery | Nanoconstructs can be engineered to mimic deficient proteins or peptides in order to restore a defective cellular pathway. | Creatine transporter deficiency (CTD) | In vivo (mice) | [86] | |
| Repurpose Clinically Approved Drugs | Many currently approved drugs could be efficient against CNS rare diseases. Nanotechnology enables repurposing their use in such pathological conditions, while improving efficiency and reducing systemic side effects. | Rare brain infectious diseases | In vitro | [112,113,115,119,122] | |
| Enhance BBB Passage | Nanocarriers can be decorated with ligands specifically binding with receptors at the surface of brain endothelial cells. Following ligand–receptor binding, transcytosis is mediated and drugs are delivered to the brain tissue in an enhanced fashion. | Primary central nervous system lymphoma (PCNSL) | In vivo (mice) | [130] | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Faouzi, A.; Roullin, V.G. Think Big, Start Small: How Nanomedicine Could Alleviate the Burden of Rare CNS Diseases. Pharmaceuticals 2021, 14, 109. https://doi.org/10.3390/ph14020109
Faouzi A, Roullin VG. Think Big, Start Small: How Nanomedicine Could Alleviate the Burden of Rare CNS Diseases. Pharmaceuticals. 2021; 14(2):109. https://doi.org/10.3390/ph14020109
Chicago/Turabian StyleFaouzi, Abdelfattah, and Valérie Gaëlle Roullin. 2021. "Think Big, Start Small: How Nanomedicine Could Alleviate the Burden of Rare CNS Diseases" Pharmaceuticals 14, no. 2: 109. https://doi.org/10.3390/ph14020109
APA StyleFaouzi, A., & Roullin, V. G. (2021). Think Big, Start Small: How Nanomedicine Could Alleviate the Burden of Rare CNS Diseases. Pharmaceuticals, 14(2), 109. https://doi.org/10.3390/ph14020109






