Silica-Based Bioactive Glasses and Their Applications in Hard Tissue Regeneration: A Review
Abstract
1. Introduction
2. Silica-Based Bioactive Glasses (BGs)
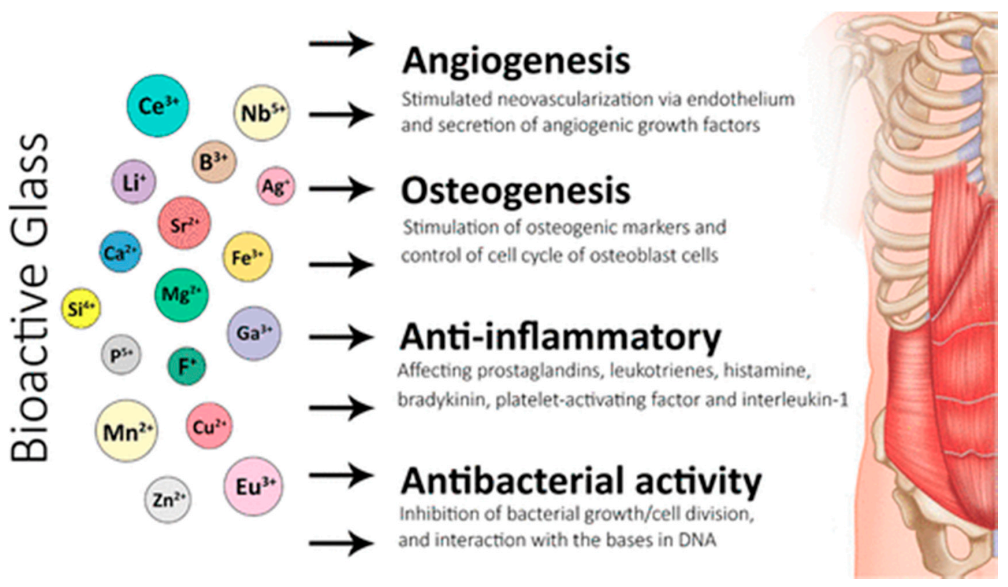
BG Properties
3. Medical Applications of BGs
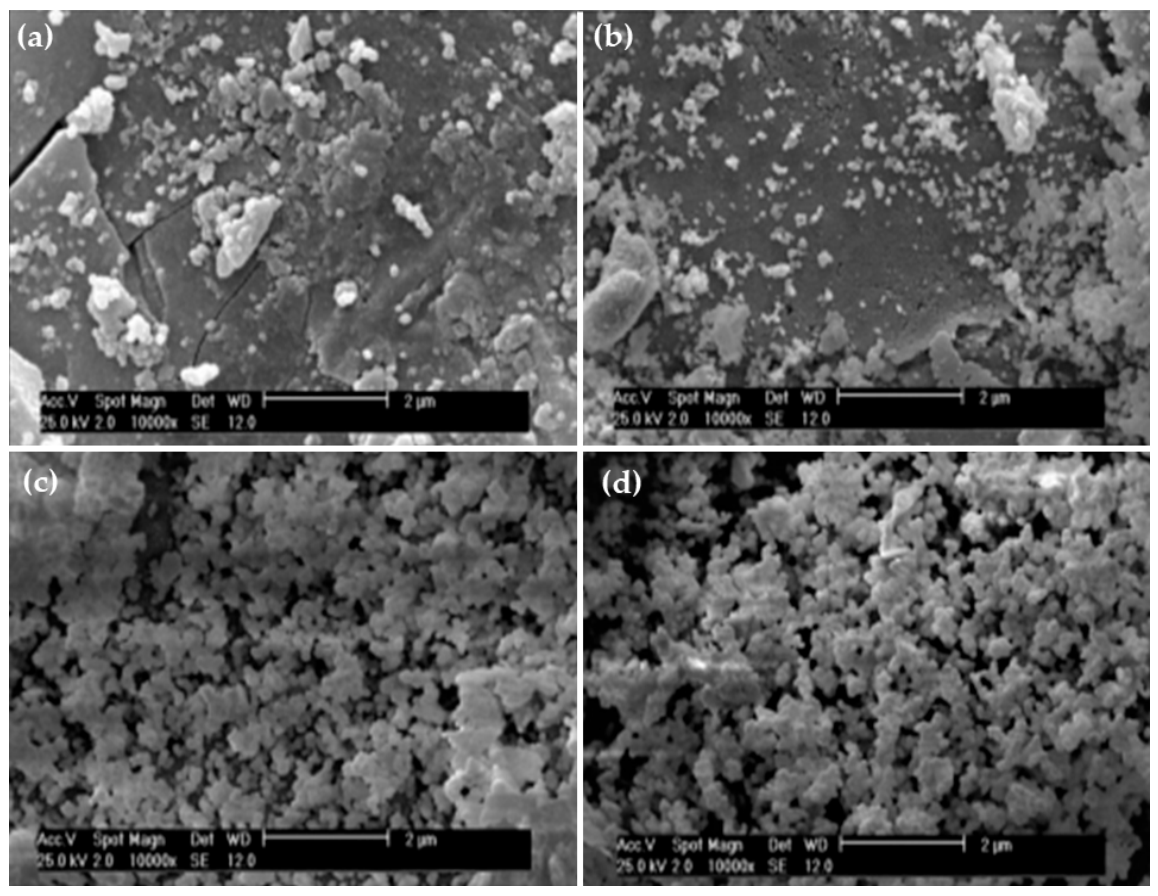
3.1. Bone Regeneration
3.2. Bone Grafts
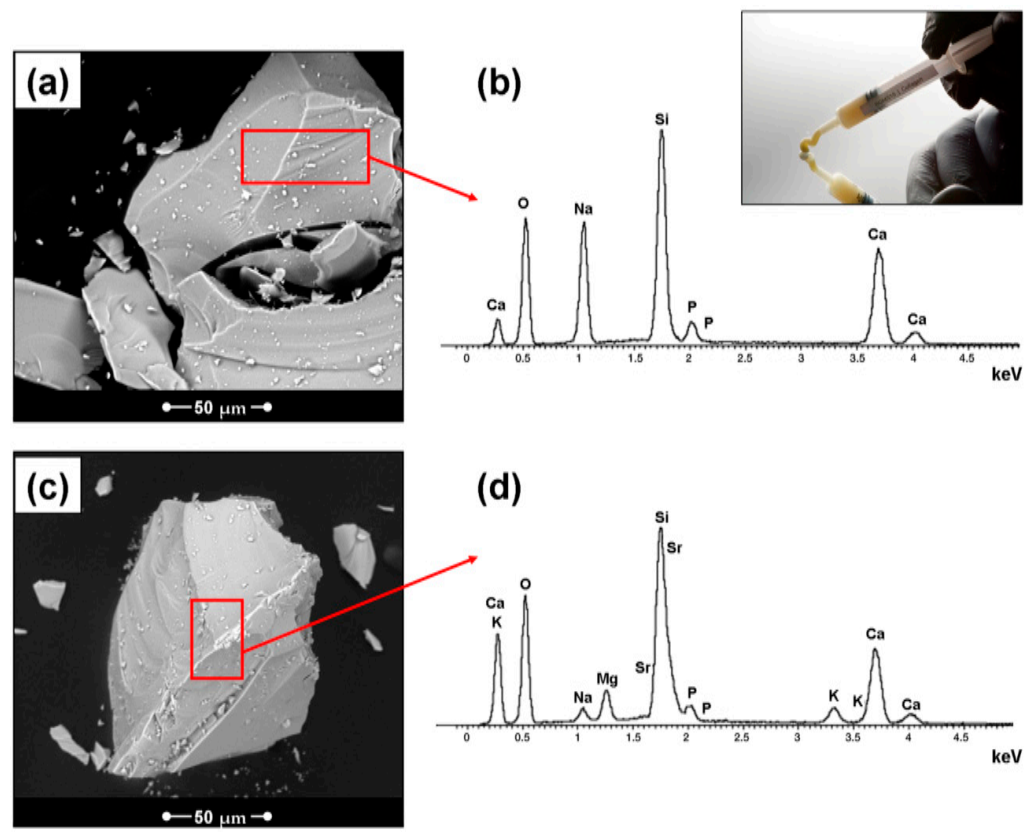
3.3. BG Implant Coatings
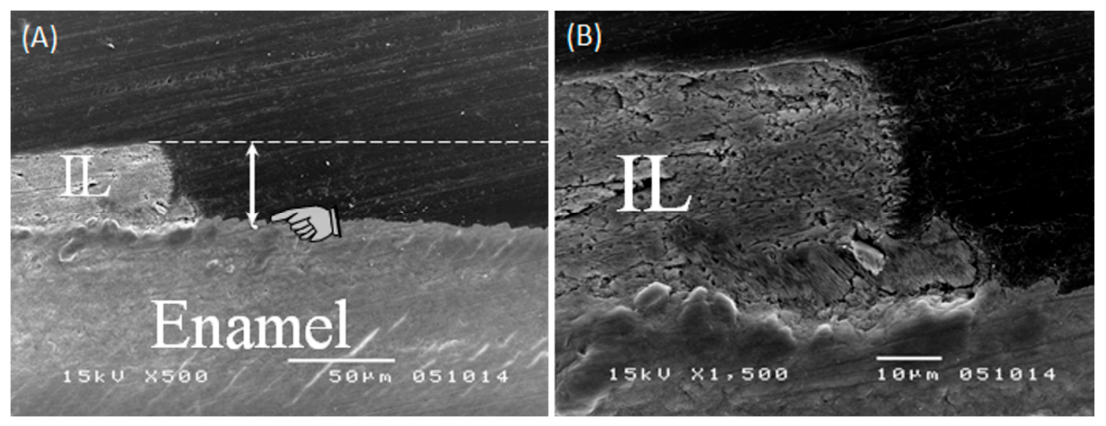
3.4. Enamel Re-Mineralization
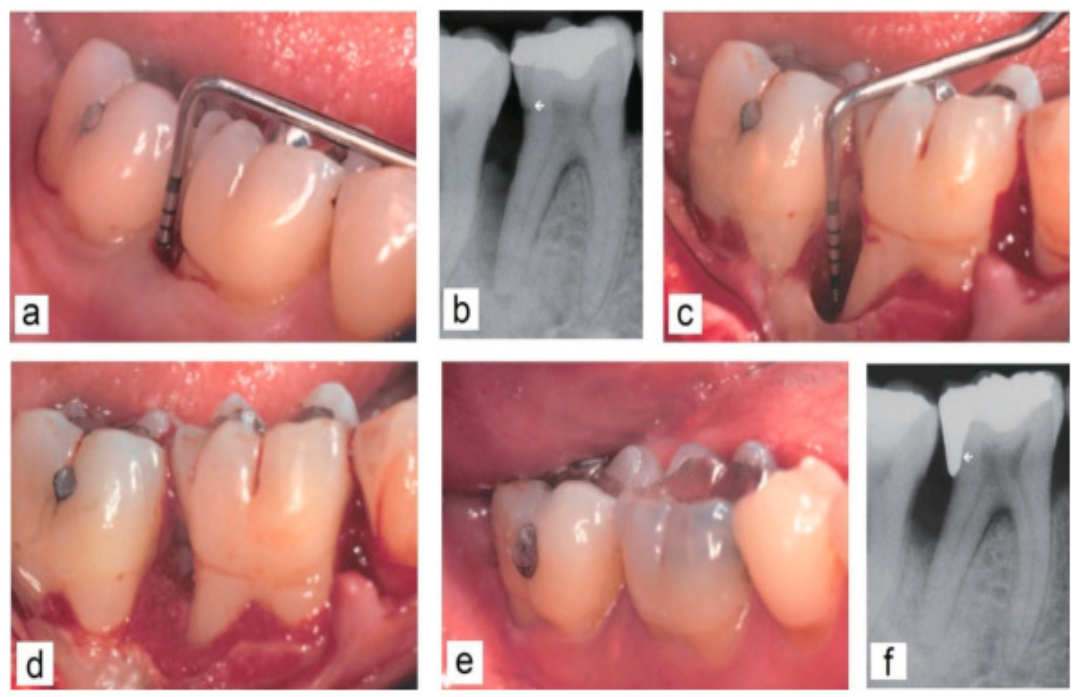
3.5. Treatment of Periodontitis
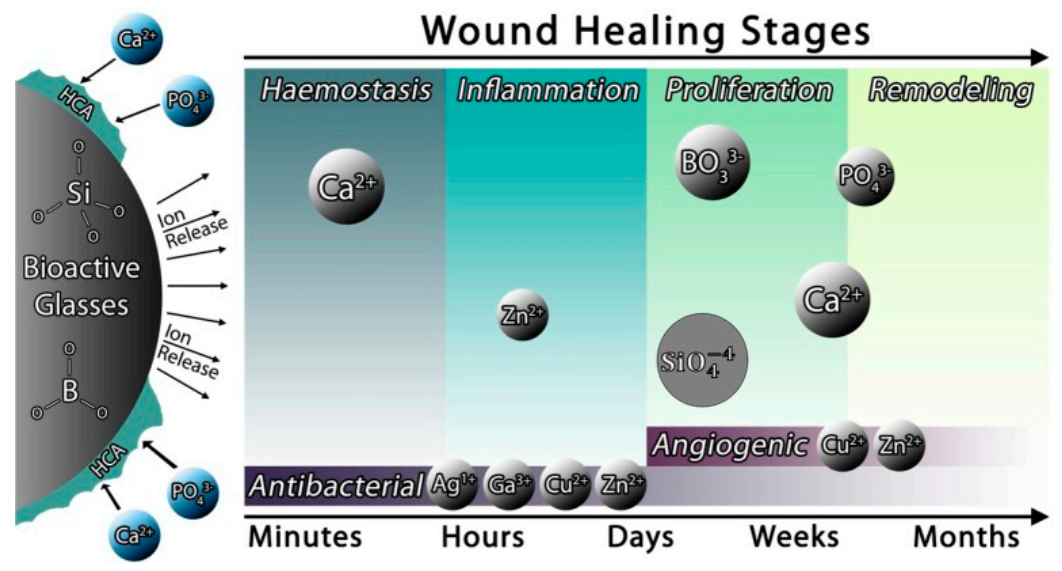
3.6. Wound Healing in Dentistry
3.7. Protection of Dental Pulp
3.8. Bioactive Glass Application in Surgical Sutures
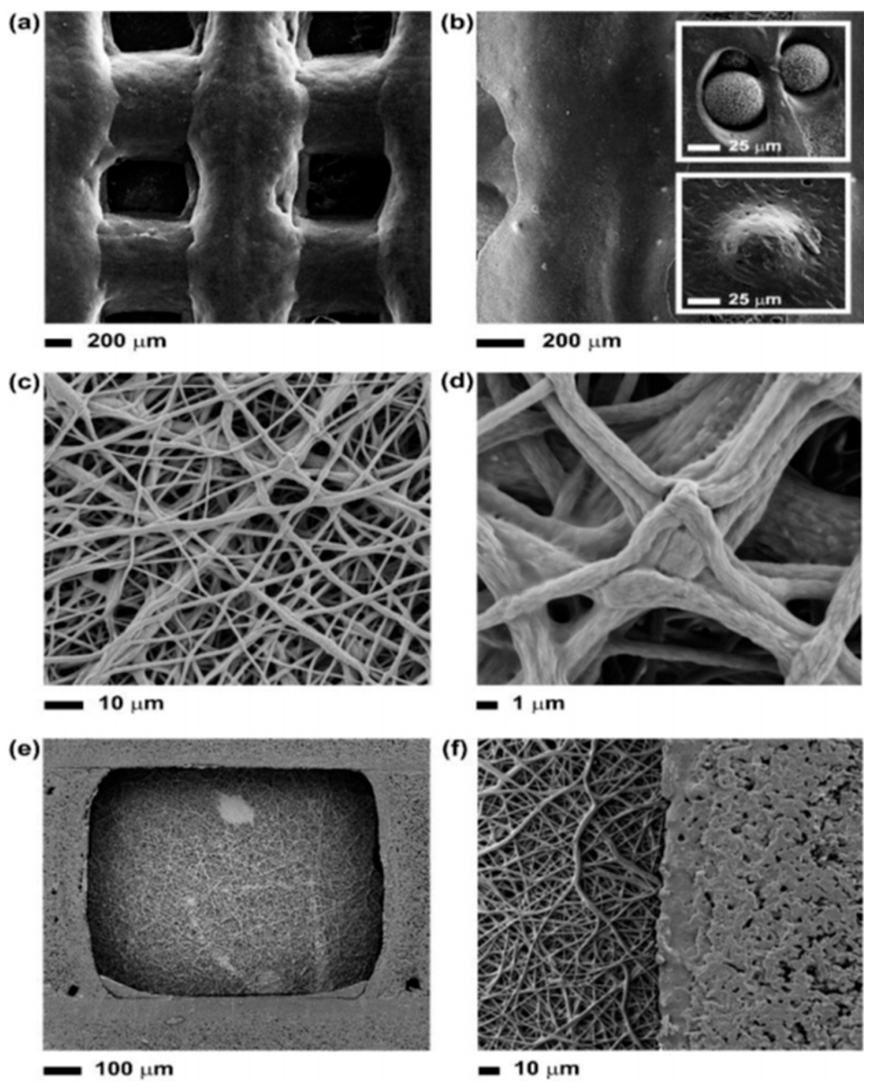
4. 3D Printing of Bioactive Glasses
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Martins, J.P.; Ferreira, M.P.A.; Ezazi, N.Z.; Hirvonen, J.T.; Santos, H.A.; Thrivikraman, G.; Franca, C.M.; Athirasala, A.; Taayeri, A.; Bertassoni, L.E. 3D printing: Prospects and challenges. In Nanotechnologies in Preventive and Regenerative Medicine; Elsevier: Amsterdam, The Netherlands, 2018; pp. 299–379. [Google Scholar] [CrossRef]
- Han, F.; Wang, J.; Ding, L.; Hu, Y.; Li, W.; Yuan, Z.; Guo, Q.; Zhu, C.; Yu, L.; Wang, H.; et al. Tissue Engineering and Regenerative Medicine: Achievements, Future, and Sustainability in Asia. Front. Bioeng. Biotechnol. 2020, 8, 83. [Google Scholar] [CrossRef]
- Li, J.J.; Zreiqat, H. Tissue Response to Biomaterials. In Reference Module in Biomedical Sciences; Elsevier: Amsterdam, The Netherlands, 2018. [Google Scholar] [CrossRef]
- Zhao, X. Introduction to bioactive materials in medicine. In Bioactive Materials in Medicine; Elsevier: Amsterdam, The Netherlands, 2011; pp. 1–13. [Google Scholar] [CrossRef]
- Kaur, G.; Pandey, O.P.; Singh, K.; Homa, D.; Scott, B.; Pickrell, G. A review of bioactive glasses: Their structure, properties, fabrication and apatite formation. J. Biomed. Mater. Res. Part A 2013, 102, 254–274. [Google Scholar] [CrossRef] [PubMed]
- Ducheyne, P. Bioactive ceramics: The effect of surface reactivity on bone formation and bone cell function. Biomaterials 1999, 20, 2287–2303. [Google Scholar] [CrossRef]
- Kokubo, T.; Takadama, H. How useful is SBF in predicting in vivo bone bioactivity? Biomaterials 2006, 27, 2907–2915. [Google Scholar] [CrossRef]
- Bohner, M.; Lemaitre, J. Can bioactivity be tested in vitro with SBF solution? Biomaterials 2009, 30, 2175–2179. [Google Scholar] [CrossRef] [PubMed]
- Marghussian, V. Biomedical Applications of Nano-Glass Ceramics. In Nano-Glass Ceramics; William Andrew Publishing: Oxford, UK, 2015; pp. 225–241. [Google Scholar] [CrossRef]
- Kargozar, S.; Baino, F.; Hamzehlou, S.; Hill, R.G.; Mozafari, M. Bioactive Glasses: Sprouting Angiogenesis in Tissue Engineering. Trends Biotechnol. 2018, 36, 430–444. [Google Scholar] [CrossRef]
- Hench, L.L.; Splinter, R.J.; Allen, W.C.; Greenlee, T.K. Bonding mechanisms at the interface of ceramic prosthetic materials. J. Biomed. Mater. Res. 1971, 5, 117–141. [Google Scholar] [CrossRef]
- Xynos, I.D.; Hukkanen, M.V.J.; Batten, J.J.; Buttery, L.D.; Hench, L.L.; Polak, J.M. Bioglass® 45S5 stimulates osteoblast turnover and enhances bone formation in vitro: Implications and applications for bone tissue engineering. Calcif. Tissue Int. 2000, 67, 321–329. [Google Scholar] [CrossRef]
- Algarni, H.; Alshahrani, I.; Ibrahim, E.H.; Eid, R.A.; Kilany, M.; Ghramh, H.A.; Yousef, E.S. Synthesis, Mechanical, In Vitro and In Vivo Bioactivity and Preliminary Biocompatibility Studies of Bioglasses. Sci. Adv. Mater. 2019, 11, 1458–1466. [Google Scholar] [CrossRef]
- Algarni, H.; Alshahrani, I.; Ibrahim, E.H.; Eid, R.A.; Kilany, M.; Ghramh, H.A.; Yousef, E.S. In-Vitro Bioactivity of Optical Glasses Containing Strontium Oxide (sro). J. Nanoelectron. Optoelectron. 2019, 14, 1105–1112. [Google Scholar] [CrossRef]
- Kargozar, S.; Lotfibakhshaiesh, N.; Ai, J.; Samadikuchaksaraie, A.; Hill, R.G.; Shah, P.A.; Joghataei, M.T. Synthesis, physico-chemical and biological characterization of strontium and cobalt substituted bioactive glasses for bone tissue engineering. J. Non-Cryst. Solids 2016, 449, 133–140. [Google Scholar] [CrossRef]
- Hench, L.L.; Roki, N.; Fenn, M.B. Bioactive glasses: Importance of structure and properties in bone regeneration. J. Mol. Struct. 2014, 1073, 24–30. [Google Scholar] [CrossRef]
- Van Vugt, T.A.; Geurts, J.A.P.; Arts, J.J.; Lindfors, N.C. Biomaterials in treatment of orthopedic infections. In Management of Periprosthetic Joint Infections (PJIs); Elsevier BV: Amsterdam, The Netherlands, 2017; pp. 41–68. [Google Scholar] [CrossRef]
- García-Gareta, E.; Coathup, M.J.; Blunn, G.W. Osteoinduction of bone grafting materials for bone repair and regeneration. Bone 2015, 81, 112–121. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.-Z.; Xie, H.-Q.; Li, X. Scaffolds in Bone Tissue Engineering: Research Progress and Current Applications. In Reference Module in Biomedical Sciences; Elsevier: Amsterdam, The Netherlands, 2020. [Google Scholar] [CrossRef]
- Fiume, E.; Barberi, J.; Verné, E.; Baino, F. Bioactive Glasses: From Parent 45S5 Composition to Scaffold-Assisted Tissue-Healing Therapies. J. Funct. Biomater. 2018, 9, 24. [Google Scholar] [CrossRef] [PubMed]
- Kiran, P.; Ramakrishna, V.; Trebbin, M.; Udayashankar, N.; Shashikala, H. Effective role of CaO/P2O5 ratio on SiO2-CaO-P2O5 glass system. J. Adv. Res. 2017, 8, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Srivatsan, T.S. Processing and Fabrication of Advanced Materials, XVII: Part 8: Polymer-Based Composites and Nano Composites; IK International Publishing House: London, UK, 2009. [Google Scholar]
- Chen, Q.Z.; Xu, J.L.; Yu, L.G.; Fang, X.Y.; Khor, K.A. Spark plasma sintering of sol–gel derived 45S5 Bioglass®-ceramics: Mechanical properties and biocompatibility evaluation. Mater. Sci. Eng. C 2012, 32, 494–502. [Google Scholar] [CrossRef]
- Teodorescu, V.; Matejec, V.; Mrazek, J. Manganese doped sol-gel materials with catalytic properties. J. Optoelectron. Adv. Mater. 2006, 8, 815–819. [Google Scholar]
- Wilson, J.; Pigott, G.H.; Schoen, F.J.; Hench, L.L. Toxicology and biocompatibility of bioglasses. J. Biomed. Mater. Res. 1981, 15, 805–817. [Google Scholar] [CrossRef]
- Wu, C.; Fan, W.; Gelinsky, M.; Xiao, Y.; Simon, P.; Schulze, R.; Doert, T.; Luo, Y.; Cuniberti, G. Bioactive SrO–SiO2 glass with well-ordered mesopores: Characterization, physiochemistry and biological properties. Acta Biomater. 2011, 7, 1797–1806. [Google Scholar] [CrossRef]
- Skallevold, H.E.; Rokaya, D.; Khurshid, Z.; Zafar, M.S. Bioactive Glass Applications in Dentistry. Int. J. Mol. Sci. 2019, 20, 5960. [Google Scholar] [CrossRef]
- Rahmati, M.; Mozafari, M. Selective contribution of bioactive glasses to molecular and cellular pathways. ACS Biomater. Sci. Eng. 2020, 6, 4–20. [Google Scholar] [CrossRef]
- Vichery, C.; Nedelec, J.-M. Bioactive Glass Nanoparticles: From Synthesis to Materials Design for Biomedical Applications. Materials 2016, 9, 288. [Google Scholar] [CrossRef] [PubMed]
- Anitha, D.; Jayashri, P. Nano Structured Bioactive Glass on Dental Disease. Indian J. Public Health Res. Dev. 2019, 10, 3459. [Google Scholar] [CrossRef]
- Mulchandani, N.; Katiyar, V. Bioactive Glasses: Prospects in Bone Tissue Engineering. In Advances in Sustainable Polymers; Springer: Singapore, 2019; pp. 67–83. [Google Scholar]
- Goudarzi, Z.; Ijadi, A.; Bakhriari, A.; Eskandarinezhad, S.; Azizabadi, N.; Asgari Jazi, M. Sr-doped bioactive glasses for biological applications. J. Compos. Compd. 2020, 2, 105–109. [Google Scholar] [CrossRef]
- Zhang, D.; Leppäranta, O.; Munukka, E.; Ylänen, H.; Viljanen, M.K.; Eerola, E.; Hupa, L. Antibacterial effects and dissolution behavior of six bioactive glasses. J. Biomed. Mater. Res. Part A Off. J. Soc. Biomater. Jpn. Soc. Biomater. Aust. Soc. Biomater. Korean Soc. Biomater. 2010, 93, 475–483. [Google Scholar] [CrossRef]
- Krajewski, A.; Ravaglioli, A.; Fabbri, B.; Azzoni, C.B. Doping influence on the interaction between a bioactive glass and a simulated physiological solution: Chemical and EPR tests. J. Mater. Sci. 1987, 22, 1228–1234. [Google Scholar] [CrossRef]
- Balasubramanian, P.; Strobel, L.A.; Kneser, U.; Boccaccini, A.R. Zinccontaining bioactive glasses for bone regeneration, dental and orthopedic applications. Biomed. Glas. 2015, 1, 51–69. [Google Scholar] [CrossRef]
- Bellucci, D.; Cannillo, V.; Anesi, A.; Salvatori, R.; Chiarini, L.; Manfredini, T.; Zaffe, D. Bone regeneration by novel bioactive glasses containing strontium and/or magnesium: A preliminary in-vivo study. Materials 2018, 11, 2223. [Google Scholar] [CrossRef]
- Kapoor, S.; Goel, A.; Tilocca, A.; Dhuna, V.; Bhatia, G.; Dhuna, K.; Ferreira, J.M. Role of glass structure in defining the chemical dissolution behavior, bioactivity and antioxidant properties of zinc and strontium co-doped alkali-free phosphosilicate glasses. Acta Biomater. 2014, 10, 3264–3278. [Google Scholar] [CrossRef]
- Diba, M.; Boccaccini, A.R. Silver-containing bioactive glasses for tissue engineering applications. In Precious Metals for Biomedical Applications; Woodhead Publishing: Amsterdam, The Netherlands, 2014; pp. 177–211. [Google Scholar] [CrossRef]
- Blaker, J.J.; Nazhat, S.N.; Boccaccini, A.R. Development and characterisation of silver-doped bioactive glass-coated sutures for tissue engineering and wound healing applications. Biomaterials 2004, 25, 1319–1329. [Google Scholar] [CrossRef]
- Vernè, E.; Di Nunzio, S.; Bosetti, M.; Appendino, P.; Brovarone, C.V.; Maina, G.; Cannas, M. Surface characterization of silver-doped bioactive glass. Biomaterials 2005, 26, 5111–5119. [Google Scholar] [CrossRef]
- Gholipourmalekabadi, M.; Nezafati, N.; Hajibaki, L.; Mozafari, M.; Moztarzadeh, F.; Hesaraki, S.; Samadikuchaksaraei, A. Detection and qualification of optimum antibacterial and cytotoxic activities of silver-doped bioactive glasses. IET Nanobiotechnol. 2015, 9, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Kaur, G.; Kumar, V.; Baino, F.; Mauro, J.C.; Pickrell, G.; Evans, I.; Bretcanu, O. Mechanical properties of bioactive glasses, ceramics, glass-ceramics and composites: State-of-the-art review and future challenges. Mater. Sci. Eng. C 2019, 104, 109895. [Google Scholar] [CrossRef]
- Nandi, S.K.; Mahato, A.; Kundu, B.; Mukherjee, P. Doped bioactive glass materials in bone regeneration. Adv. Tech. Bone Regen 2016, 13, 276–327. [Google Scholar]
- Hanifi, A.R.; Pomeroy, M.J.; Hampshire, S. Novel Glass Formation in the Ca-Si-Al-O-N-F System. J. Am. Ceram. Soc. 2010, 94, 455–461. [Google Scholar] [CrossRef]
- Gentleman, E.; Fredholm, Y.C.; Jell, G.; Lotfibakhshaiesh, N.; O’Donnell, M.D.; Hill, R.G.; Stevens, M.M. The effects of strontium-substituted bioactive glasses on osteoblasts and osteoclasts in vitro. Biomaterials 2010, 31, 3949–3956. [Google Scholar] [CrossRef] [PubMed]
- Kargozar, S.; Montazerian, M.; Fiume, E.; Baino, F. Multiple and Promising Applications of Strontium (Sr)-Containing Bioactive Glasses in Bone Tissue Engineering. Front. Bioeng. Biotechnol. 2019, 7, 161. [Google Scholar] [CrossRef] [PubMed]
- Erol-Taygun, M.; Unalan, I.; Idris, M.I.B.; Mano, J.F.; Boccaccini, A.R. Bioactıve Glass-Polymer Nanocomposites for Bone Tıssue Regeneration Applicatıons: A Revıew. Adv. Eng. Mater. 2019, 21, 1900287. [Google Scholar] [CrossRef]
- Aina, V.; Perardi, A.; Bergandi, L.; Malavasi, G.; Menabue, L.; Morterra, C.; Ghigo, D. Cytotoxicity of zinc-containing bioactive glasses in contact with human osteoblasts. Chem. Interact. 2007, 167, 207–218. [Google Scholar] [CrossRef]
- Khorami, M.; Hesaraki, S.; Behnamghader, A.; Nazarian, H.; Shahrabi, S. In vitro bioactivity and biocompatibility of lithium substituted 45S5 bioglass. Mater. Sci. Eng. C 2011, 31, 1584–1592. [Google Scholar] [CrossRef]
- Jones, J.R.; Ehrenfried, L.M.; Hench, L.L. Optimising bioactive glass scaffolds for bone tissue engineering. Biomaterials 2006, 27, 964–973. [Google Scholar] [CrossRef] [PubMed]
- Farooq, I.; Moheet, I.A.; Alshwaimi, E. Cavity cutting efficiency of a bioglasstm and alumina powder combination utilized in an air abrasion system. Bull. Mater. Sci. 2016, 39, 1531–1536. [Google Scholar] [CrossRef]
- Jones, J.R.; Gentleman, E.; Polak, J. Bioactive Glass Scaffolds for Bone Regeneration. Elements 2007, 3, 393–399. [Google Scholar] [CrossRef]
- Imran, Z. Bioactive Glass: A Material for the Future. World J. Dent. 2012, 3, 199–201. [Google Scholar] [CrossRef]
- Ravindranadh, K. Bioactive Glasses for Technological and Clinical Applications. Int. J. Chem. Sci. 2016, 14, 1339–1348. [Google Scholar]
- Dimitriou, R.; Jones, E.; Mcgonagle, D.; Giannoudis, P.V. Bone regeneration: Current concepts and future directions. BMC Med. 2011, 9, 66. [Google Scholar] [CrossRef]
- Fernandez de Grado, G.; Keller, L.; Idoux-Gillet, Y.; Wagner, Q.; Musset, A.-M.; Benkirane-Jessel, N.; Offner, D. Bone substitutes: A review of their characteristics, clinical use, and perspectives for large bone defects management. J. Tissue Eng. 2018, 9, 204173141877681. [Google Scholar] [CrossRef]
- Bellucci, D.; Salvatori, R.; Giannatiempo, J.; Anesi, A.; Bortolini, S.; Cannillo, V. A New Bioactive Glass/Collagen Hybrid Composite for Applications in Dentistry. Materials 2019, 12, 2079. [Google Scholar] [CrossRef]
- Sarker, B.; Hum, J.; Nazhat, S.N.; Boccaccini, A.R. Combining Collagen and Bioactive Glasses for Bone Tissue Engineering: A Review. Adv. Healthc. Mater. 2014, 4, 176–194. [Google Scholar] [CrossRef]
- Baino, F.; Novajra, G.; Miguez-Pacheco, V.; Boccaccini, A.R.; Vitale-Brovarone, C. Bioactive glasses: Special applications outside the skeletal system. J. Non Cryst. Solids 2016, 432, 15–30. [Google Scholar] [CrossRef]
- Bellucci, D.; Cannillo, V.; Ciardelli, G.; Gentile, P.; Sola, A. Potassium based bioactive glass for bone tissue engineering. Ceram. Int. 2010, 36, 2449–2453. [Google Scholar] [CrossRef]
- Kumar, P.; Fathima, G.; Vinitha, B. Bone grafts in dentistry. J. Pharm. Bioallied Sci. 2013, 5, 125–127. [Google Scholar] [CrossRef] [PubMed]
- Algarni, H.; AlShahrani, I.; Ibrahim, E.H.; Eid, R.A.; Kilany, M.; Ghramh, H.A.; Ali, A.M.; Yousef, E.S. Fabrication and Biocompatible Characterizations of Bio-Glasses Containing Oxyhalides Ions. J. Nanoelectron. Optoelectron. 2019, 14, 328–334. [Google Scholar] [CrossRef]
- Hench, L.L. Bioactive Glass Bone Grafts: History and Clinical Applications. In Handbook of Bioceramics and Biocomposites; Springer Science and Business Media LLC: Berlin/Heidelberg, Germany, 2016; pp. 23–33. [Google Scholar] [CrossRef]
- Välimäki, V.-V.; Aro, H.T. Molecular Basis for Action of Bioactive Glasses as Bone Graft Substitute. Scand. J. Surg. 2006, 95, 95–102. [Google Scholar] [CrossRef]
- Oonishi, H.; Kushitani, S.; Yasukawa, E.; Iwaki, H.; Hench, L.L.; Wilson, J.; Sugihara, T. Particulate bioglass compared with hydroxyapatite as a bone graft substitute. Clin. Orthop. Relat. Res. 1997, 334, 316–325. [Google Scholar] [CrossRef]
- Khalid, M.D.; Khurshid, Z.; Zafar, M.S.; Farooq, I.; Khan, R.S.; Najmi, A. Bioactive Glasses and their Applications in Dentistry. J. Pak. Dent. Assoc. 2017, 26, 32–38. [Google Scholar] [CrossRef]
- Van Gestel, N.A.P.; Geurts, J.; Hulsen, D.J.W.; Van Rietbergen, B.; Hofmann, S.; Arts, J.J. Clinical Applications of S53P4 Bioactive Glass in Bone Healing and Osteomyelitic Treatment: A Literature Review. BioMed Res. Int. 2015, 2015, 684826. [Google Scholar] [CrossRef]
- Ali, S.; Farooq, I.; Iqbal, K. A review of the effect of various ions on the properties and the clinical applications of novel bioactive glasses in medicine and dentistry. Saudi Dent. J. 2014, 26, 1–5. [Google Scholar] [CrossRef]
- Fetner, A.E.; Hartigan, M.S.; Low, S.B. Periodontal repair using perioglas in nonhuman primates: Clinical and histologic observations. Compendium 1994, 15, 932–935. [Google Scholar]
- Hench, L.L. Bioceramics: From Concept to Clinic. J. Am. Ceram. Soc. 1991, 74, 1487–1510. [Google Scholar] [CrossRef]
- Boccaccini, A.R.; Erol, M.; Stark, W.J.; Mohn, D.; Hong, Z.; Mano, J.F. Polymer/bioactive glass nanocomposites for biomedical applications: A review. Compos. Sci. Technol. 2010, 70, 1764–1776. [Google Scholar] [CrossRef]
- Gerhardt, L.-C.; Boccaccini, A.R. Bioactive Glass and Glass-Ceramic Scaffolds for Bone Tissue Engineering. Materials 2010, 3, 3867–3910. [Google Scholar] [CrossRef] [PubMed]
- Geiger, F.; Beverungen, M.; Lorenz, H.; Wieland, J.; Fehr, M.; Kasten, P. Bone Substitute Effect on Vascularization and Bone Remodeling after Application of phvegf165 Transfected BMSC. J. Funct. Biomater. 2012, 3, 313–326. [Google Scholar] [CrossRef] [PubMed]
- Schmidt-Bleek, K.; Schell, H.; Schulz, N.; Hoff, P.; Perka, C.; Buttgereit, F.; Duda, G.N. Inflammatory phase of bone healing initiates the regenerative healing cascade. Cell Tissue Res. 2011, 347, 567–573. [Google Scholar] [CrossRef] [PubMed]
- Giannoudis, P.V.; Einhorn, T.A.; Schmidmaier, G.; Marsh, D. The diamond concept—Open questions. Injury 2008, 39, S5–S8. [Google Scholar] [CrossRef]
- Nijpanich, S.; Hagio, T.; Kamimoto, Y.; Ichino, R. Floating Adsorbent for Organic Removal Fabricated Through Crystallization of Silicalite-1 on Hollow Glass Microspheres. Sci. Adv. Mater. 2020, 12, 173–179. [Google Scholar] [CrossRef]
- Wennerberg, A.; Bougas, K.; Jimbo, R.; Albrektsson, T. Implant coatings: New modalities for increased osseointegration. Am. J. Dent. 2013, 26, 105–112. [Google Scholar] [PubMed]
- Profeta, A.C.; Prucher, G.M. Bioactive-glass in periodontal surgery and implant dentistry. Dent. Mater. J. 2015, 34, 559–571. [Google Scholar] [CrossRef]
- Oliver, J.N.; Su, Y.; Lu, X.; Kuo, P.-H.; Du, J.; Zhu, D. Bioactive glass coatings on metallic implants for biomedical applications. Bioact. Mater. 2019, 4, 261–270. [Google Scholar] [CrossRef]
- Abbasi, Z.; Bahrololoom, M.E.; Shariat, M.H.; Bagheri, R. Bioactive Glasses in Dentistry: A Review. J. Dent. Biomater. 2015, 2, 1–9. [Google Scholar]
- Stähli, C.; James-Bhasin, M.; Hoppe, A.; Boccaccini, A.R.; Nazhat, S.N. Effect of ion release from Cu-doped 45S5 Bioglass® on 3D endothelial cell morphogenesis. Acta Biomater. 2015, 19, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Stan, G.E.; Pina, S.; Tulyaganov, D.U.; Ferreira, J.M.F.; Pasuk, I.; Morosanu, C.O. Biomineralization capability of adherent bio-glass films prepared by magnetron sputtering. J. Mater. Sci. Mater. Med. 2009, 21, 1047–1055. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Vega, J.M.; Saiz, E.; Tomsia, A.P.; Oku, T.; Suganuma, K.; Marshall, G.W.; Marshall, S.J. Novel Bioactive Functionally Graded Coatings on Ti6Al4V. Adv. Mater. 2000, 12, 894–898. [Google Scholar] [CrossRef]
- Gomez-Vega, J.M.; Saiz, E.; Tomsia, A.P.; Oku, T.; Suganuma, K.; Marshall, G.W.; Marshall, S.J. Bioactive glass coatings with hydroxyapatite and Bioglass® particals on Ti-basedimplants. 1. Processing. Biomaterials 2000, 21, 105–111. [Google Scholar] [CrossRef]
- Moritz, N.; Rossi, S.; Vedel, E.; Tirri, T.; Ylänen, H.; Aro, H.; Närhi, T. Implants coated with bioactive glass by CO2-laser, an in vivo study. J. Mater. Sci. Mater. Electron. 2004, 15, 795–802. [Google Scholar] [CrossRef]
- Bakry, A.S.; Abbassy, M.A. Increasing the efficiency of CPP-ACP to remineralize enamel white spot lesions. J. Dent. 2018, 76, 52–57. [Google Scholar] [CrossRef]
- Bakry, A.S.; Abbassy, M.A. The Efficacy of a Bioglass (45S5) paste temporary filling used to remineralize enamel surfaces prior to bonding procedures. J. Dent. 2019, 85, 33–38. [Google Scholar] [CrossRef]
- Al-Bazi, S.M.; Abbassy, M.A.; Bakry, A.S.; Merdad, L.A.; Hassan, A.H. Effects of chlorhexidine (gel) application on bacterial levels and orthodontic brackets during orthodontic treatment. J. Oral Sci. 2016, 58, 35–42. [Google Scholar] [CrossRef]
- Algarni, H.; Alshahrani, I.; Ibrahim, E.H.; Eid, R.A.; Kilany, M.; Ghramh, H.A.; Sayed, M.A.; Reben, M.; Yousef, E.S. Structural, Thermal Stability and In Vivo Bioactivity Properties of Nanobioglasses Containing zno. Sci. Adv. Mater. 2019, 11, 925–935. [Google Scholar] [CrossRef]
- Bakhsh, T.A.; Bakry, A.S.; Mandurah, M.M.; Abbassy, M.A. Novel evaluation and treatment techniques for white spot lesions. An in vitro study. Orthod. Craniofac. Res. 2017, 20, 170–176. [Google Scholar] [CrossRef]
- Bakry, A.; Abbassy, M.; Alharkan, H.; Basuhail, S.; Al-Ghamdi, K.; Hill, R. A Novel Fluoride Containing Bioactive Glass Paste is Capable of Re-Mineralizing Early Caries Lesions. Materials 2018, 11, 1636. [Google Scholar] [CrossRef] [PubMed]
- Bakry, A.S.; Marghalani, H.Y.; Amin, O.A.; Tagami, J. The effect of a bioglass paste on enamel exposed to erosive challenge. J. Dent. 2014, 42, 1458–1463. [Google Scholar] [CrossRef] [PubMed]
- Bakry, A.S.; Takahashi, H.; Otsuki, M.; Sadr, A.; Yamashita, K.; Tagami, J. CO2 laser improves 45S5 bioglass interaction with dentin. J. Dent. Res. 2011, 90, 246–250. [Google Scholar] [CrossRef] [PubMed]
- Bakry, A.S.; Takahashi, H.; Otsuki, M.; Tagami, J. The durability of phosphoric acid promoted bioglass–dentin interaction layer. Dent. Mater. 2013, 29, 357–364. [Google Scholar] [CrossRef]
- Bakry, A.S.; Takahashi, H.; Otsuki, M.; Tagami, J. Evaluation of new treatment for incipient enamel demineralization using 45S5 bioglass. Dent. Mater. 2014, 30, 314–320. [Google Scholar] [CrossRef]
- Bakry, A.S.; Tamura, Y.; Otsuki, M.; Kasugai, S.; Ohya, K.; Tagami, J. Cytotoxicity of 45S5 bioglass paste used for dentine hypersensitivity treatment. J. Dent. 2011, 39, 599–603. [Google Scholar] [CrossRef]
- Abbassy, M.A.; Bakry, A.S.; Alshehri, N.I.; Alghamdi, T.M.; Rafiq, S.A.; Aljeddawi, D.H.; Hassan, A.H. 45S5 Bioglass paste is capable of protecting the enamel surrounding orthodontic brackets against erosive challenge. J. Orthod. Sci. 2019, 8, 5. [Google Scholar]
- Bae, J.; Son, W.S.; Yoo, K.H.; Yoon, S.Y.; Bae, M.K.; Lee, D.J.; Kim, Y.I. Effects of Poly (Amidoamine) Dendrimer-Coated Mesoporous Bioactive Glass Nanoparticles on Dentin Remineralization. Nanomaterials 2019, 9, 591. [Google Scholar] [CrossRef]
- Tirapelli, C.; Panzeri, H.; Soares, R.G.; Peitl, O.; Zanotto, E.D. A novel bioactive glass-ceramic for treating dentin hypersensitivity. Braz. Oral Res. 2010, 24, 381–387. [Google Scholar]
- Sun, J.; Zhang, Y.; Hu, Y.; Yang, Q. Preparation of Bioactive Glass/Modified Gelatin/Collagen Composite Scaffold and Its Effect on Repair of Sciatic Nerve Defect. Sci. Adv. Mater. 2020, 12, 1814–1823. [Google Scholar] [CrossRef]
- Renvert, S.; Persson, G.R. Periodontitis as a potential risk factor for peri-implantitis. J. Clin. Periodontol. 2009, 36, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Allan, I.; Wilson, M.; Newman, H. Particulate Bioglass® reduces the viability of bacterial biofilms formed on its surface in an in vitro model. Clin. Oral Implant. Res. 2002, 13, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Allan, I.; Newman, H.; Wilson, M. Antibacterial activity of particulate bioglass® against supra-and subgingival bacteria. Biomaterials 2001, 22, 1683–1687. [Google Scholar] [CrossRef]
- Doyon, G.E.; Dumsha, T.; von Fraunhofer, J.A. Fracture resistance of human root dentin exposed to intracanal calcium hydroxide. J. Endod. 2005, 31, 895–897. [Google Scholar] [CrossRef] [PubMed]
- Lovelace, T.B.; Mellonig, J.T.; Me_ert, R.M.; Jones, A.A.; Nummikoski, P.V.; Cochran, D.L. Clinical evaluation of bioactive glass in the treatment of periodontal osseous defects in humans. J. Periodontol. 1998, 69, 1027–1035. [Google Scholar] [CrossRef]
- AbouDeif, Y.M.; Reben, M.; Yousef, E.S.; Al-Salami, A.E.; Al Shehri, A.S. Characterization of Absorption, Emission Cross Section and Gain Coefficient of Tellurite Glasses Doped with Er3+ Ions for Fiber Amplifier. J. Nanoelectron. Optoelectron. 2019, 14, 932–938. [Google Scholar] [CrossRef]
- Profeta, A.C.; Huppa, C. Bioactive-glass in Oral and Maxillofacial Surgery. Craniomaxillofac. Trauma Reconstr. 2016, 9, 001–014. [Google Scholar] [CrossRef]
- Pantchev, A.; Nohlert, E.; Tegelberg, A. Endodontic surgery with and without inserts of bioactive glass PerioGlas—A clinical and radiographic follow-up. Oral Maxillofac. Surg. 2009, 13, 21–26. [Google Scholar] [CrossRef]
- Stanley, H.R.; Hall, M.B.; Clark, A.E.; King, C.J., 3rd; Hench, L.L.; Berte, J.J. Using 45S5 bioglass cones as endosseous ridge maintenance implants to prevent alveolar ridge resorption: A 5-year evaluation. Int. J. Oral Maxillofac. Implants 1997, 12, 95–105. [Google Scholar]
- Mengel, R.; Soffner, M.; Flores-de-Jacoby, L. Bioabsorbable membrane and bioactive glass in the treatment of intrabony defects in patients with generalized aggressive periodontitis: Results of a 12-month clinical and radiological study. J. Periodontol. 2003, 74, 899–908. [Google Scholar] [CrossRef]
- Tai, B.J.; Bian, Z.; Jiang, H.; Greenspan, D.C.; Zhong, J.; Clark, A.E.; Du, M.Q. Anti-gingivitis effect of a dentifrice containing bioactive glass (NovaMin®) particulate. J. Clin. Periodontol. 2006, 33, 86–91. [Google Scholar] [CrossRef]
- Eberhard, J.; Reimers, N.; Dommisch, H.; Hacker, J.; Freitag, S.; Acil, Y.; Jepsen, S. The effect of the topical administration of bioactive glass on inflammatory markers of human experimental gingivitis. Biomaterials 2005, 26, 1545–1551. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Yu, Z.; Long, Y.; Chen, L. Preparation of Porous Titanium Dental Implant by 3D Printing/Composite Coating and Its Biomechanical Properties and Flexural Strength. Sci. Adv. Mater. 2020, 12, 1492–1501. [Google Scholar] [CrossRef]
- Li, M.; Chen, J.; Shi, M.; Zhang, H.; Ma, P.X.; Guo, B. Electroactive anti-oxidant polyurethane elastomers with shape memory property as non-adherent wound dressing to enhance wound healing. Chem. Eng. J. 2019, 375, 121999. [Google Scholar] [CrossRef]
- Naseri, S.; Lepry, W.C.; Nazhat, S.N. Bioactive glasses in wound healing: Hope or hype? J. Mater. Chem. B 2017, 5, 6167–6174. [Google Scholar] [CrossRef] [PubMed]
- Kargozar, S.; Mozafari, M.; Hamzehlou, S.; Baino, F. Using Bioactive Glasses in the Management of Burns. Front. Bioeng. Biotechnol. 2019, 7, 62. [Google Scholar] [CrossRef]
- Dong, X.; Chang, J.; Li, H. Bioglass promotes wound healing through modulating the paracrine effects between macrophages and repairing cells. J. Mater. Chem. B 2017, 5, 5240–5250. [Google Scholar] [CrossRef]
- Krishnan, V.; Lakshmi, T. Bioglass: A novel biocompatible innovation. J. Adv. Pharm. Technol. Res. 2013, 4, 78–83. [Google Scholar] [CrossRef]
- Wang, G.; Lyu, J.; Fang, Y.; Sun, Q.; Ma, P.; Zhang, S.; Xu, B. Preparation of Zirconia-Based Dental Restorative Materials and Exploration on Their Wear Performances on Enamel/Dentine. Sci. Adv. Mater. 2020, 12, 1535–1547. [Google Scholar] [CrossRef]
- Discepoli, N.; Vignoletti, F.; Laino, L.; de Sanctis, M.; Muñoz, F.; Sanz, M. Early healing of the alveolar process after tooth extraction: An experimental study in the beagle dog. J. Clin. Periodontol. 2013, 40, 638–644. [Google Scholar] [CrossRef]
- Stanley, H.R. Pulp capping: Conserving the dental pulp-can it be done? Is it worth it? Oral Surgery Oral Med. Oral Pathol. 1989, 68, 628–639. [Google Scholar] [CrossRef]
- Masterton, J.B. Internal resorption of dentin: A complication arising from unhealed pulp wounds. Br. Dent. J. 1965, 118, 241–249. [Google Scholar] [PubMed]
- Patterson, S.S. Pulp calcifications due to operative procedures pulpotomy. Int. Dent. J. 1967, 17, 490–505. [Google Scholar] [PubMed]
- Reel, D.C.; Lyon, H.E.; Mitchell, R.J. Fracture resistance of amalgam restorations placed over various basing agents. Compendium 1987, 8, 282–286. [Google Scholar] [PubMed]
- Cox, C.F.; Bergenholtz, G.; Fitzgerald, M. Capping of the dental pulp mechanically exposed to the oral microflora-a five week observation of wound healing in the monkey. J. Oral Pathol. Med. 1982, 11, 327–339. [Google Scholar] [CrossRef]
- Oguntebi, B.; Clark, A.; Wilson, J. Pulp Capping with Bioglass® and Autologous Demineralized Dentin in Miniature Swine. J. Dent. Res. 1993, 72, 484–489. [Google Scholar] [CrossRef]
- Frank, R.M.; Wiedemann, P.; Hemmerle, J.; Freymann, M. Pulp capping with synthetic hydroxyapatite in human premolars. J. Appl. Biomater. 1991, 2, 243–250. [Google Scholar] [CrossRef]
- Chu, C.C. Textile-Based Biomaterials for Surgical Applications, In Polymeric Biomaterials, 2nd ed.; Dumitriu, S., Ed.; Marcel Dekker: New York, NY, USA, 2002; pp. 167–186. [Google Scholar]
- Donlan, R.M.; Costerton, J.W. Biofilms: Survival mechanisms of clinically relevant microorganisms. Clin. Microbiol. Rev. 2002, 15, 167–193. [Google Scholar] [CrossRef]
- Mingmalairak, C. Antimicrobial Sutures: New Strategy in Surgical Site Infections. In Science against Microbial Pathogens: Communicating Current Research and Technological Advances; Formatex Research Center: Badajoz, Spain, 2011; pp. 313–323. [Google Scholar]
- Enab, W.; Moataz, M.; Moneim, A. Inducing anti-bacterial activity of commercial PET surgical sutures via silver nanoparticles. In Proceedings of the International Conference on Chemistry, Biomedical and Environment Engineering, Antalya, Turkey, 7–8 October 2014. [Google Scholar]
- Ricco, J.-B.; Assadian, O. Antimicrobial silver grafts for prevention and treatment of vascular graft infection. In Proceedings of the Seminars in Vascular Surgery; WB Saunders: Amsterdam, The Netherlands, 2011; Volume 24, pp. 234–241. [Google Scholar]
- Hameed, A.S.; Al-Warid, R.J.; Obaid, I.A. Anti-bacterial Action of Multi-component Bioactive Glass Coating for Surgical Suture. J. Univ. Babylon 2016, 24, 1395–1400. [Google Scholar]
- Ahmed, I.; Ready, D.; Wilson, M.J.C.; Knowles, J. Antibacterial effect of silver-doped phosphate-based glasses. J. Biomed. Mater. Res. A 2006, 79, 618–626. [Google Scholar] [CrossRef]
- Xie, Z.P.; Zhang, C.Q.; Yi, C.Q.; Qiu, J.J.; Wang, J.Q.; Zhou, J. In Vivo study effect of particulate Bioglass® in the prevention of infection in open fracture fixation. Biomed. Mater. Res. B Appl. Biomater. 2009, 90, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Bergmann, C.; Lindner, M.; Zhang, W.; Koczur, K.; Kirsten, A.; Telle, R.; Fischer, H. 3D printing of bone substitute implants using calcium phosphate and bioactive glasses. J. Eur. Ceram. Soc. 2010, 30, 2563–2567. [Google Scholar] [CrossRef]
- Murphy, C.; Kolan, K.; Li, W.; Semon, J.; Day, D.; Leu, M. 3D bioprinting of stem cells and polymer/bioactive glass composite scaffolds for bone tissue engineering. Int. J. Bioprint. 2017, 3, 54–64. [Google Scholar] [CrossRef] [PubMed]
- Pires, L.S.O.; Fernandes, M.H.F.V.; de Oliviera, J.M.M. Biofabrication of glass scaffolds by 3D printing for tissue engineering. Int. J. Adv. Manuf. Technol. 2018, 98, 2665–2676. [Google Scholar] [CrossRef]
- Qi, X.; Wang, H.; Zhang, Y.; Pang, L.; Xiao, W.; Jia, W.; Wang, Q. Mesoporous bioactive glass-coated 3D printed borosilicate bioactive glass scaffolds for improving repair of bone defects. Int. J. Biol. Sci. 2018, 14, 471. [Google Scholar] [CrossRef]
- Wu, J.; Miao, G.; Zheng, Z.; Li, Z.; Ren, W.; Wu, C.; Guo, L. 3D printing mesoporous bioactive glass/sodium alginate/gelatin sustained release scaffolds for bone repair. J. Biomater. Appl. 2019, 33, 755–765. [Google Scholar] [CrossRef]
- Zhang, Y.; Yu, W.; Ba, Z.; Cui, S.; Wei, J.; Li, H. 3D-printed scaffolds of mesoporous bioglass/gliadin/polycaprolactone ternary composite for enhancement of compressive strength, degradability, cell responses and new bone tissue ingrowth. Int. J. Nanomed. 2018, 13, 5433. [Google Scholar] [CrossRef]
- Montalbano, G.; Fiorilli, S.; Caneschi, A.; Vitale-Brovarone, C. Type I collagen and strontium-containing mesoporous glass particles as hybrid material for 3D printing of bone-like materials. Materials 2018, 11, 700. [Google Scholar] [CrossRef]
- Baino, F.; Barberi, J.; Fiume, E.; Orlygsson, G.; Massera, J.; Verné, E. Robocasting of Bioactive SiO2-P2O5-CaO-MgO-Na2O-K2O Glass Scaffolds. J. Healthc. Eng. 2019, 2019, 5153136. [Google Scholar] [CrossRef]
- Kolan, K.C.; Huang, Y.W.; Semon, J.A.; Leu, M.C. 3D-printed Biomimetic Bioactive Glass Scaffolds for Bone Regeneration in Rat Calvarial Defects. Int. J. Bioprint. 2020, 6, 274. [Google Scholar] [CrossRef] [PubMed]
- Touré, A.B.; Mele, E.; Christie, J.K. Multi-layer Scaffolds of Poly (caprolactone), Poly (glycerol sebacate) and Bioactive Glasses Manufactured by Combined 3D Printing and Electrospinning. Nanomaterials 2020, 10, 626. [Google Scholar] [CrossRef] [PubMed]
| Type | Example of Bioactive Glasses | Composition | ||||||
|---|---|---|---|---|---|---|---|---|
| SiO2 (wt%) | Na2O (wt%) | CaO (wt%) | P2O5 (wt%) | K2O (wt%) | MgO (wt%) | B2O3 (wt%) | ||
| Silicate glass | Bioglass or 45S5 bioactive glass | 45 | 24.5 | 24.5 | 6 | – | – | – |
| Glass ceramic | BonAlive or S53P4 bioactive glass | 53 | 23 | 20 | 4 | – | – | – |
| Silica-based glass | 13-93 bioactive glass | 53 | 6 | 20 | 4 | 12 | 5 | |
| 13-93B1 bioactive glass | 34.4 | 5.8 | 19.5 | 3.8 | 11.7 | 4.9 | 19.9 | |
| Material | Comprehensive Modulus (GPa) | Comprehensive Strength (MPa) | Fracture Toughness (MPa m1/2) | Bending Strength (MPa) | Vickers Hardness (MPa) | Structure |
|---|---|---|---|---|---|---|
| HA | 35–120 | 100–150 | 0.8–1.2 | 60–120 | 90–140 | Ceramic |
| Bioglass 45S5 | 60 | - | 0.6 | 40 | - | Glass |
| Bioglass 52S4.6 | 60 | - | - | 40 | - | Glass |
| Trabecular bone | 0.05–0.6 | 1.5–7.5 | 0.1–0.8 | 10–20 | 40–60 | - |
| Cortical bone | 7–30 | 100–135 | 2–12 | 50–150 | 60–75 | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Harbi, N.; Mohammed, H.; Al-Hadeethi, Y.; Bakry, A.S.; Umar, A.; Hussein, M.A.; Abbassy, M.A.; Vaidya, K.G.; Al Berakdar, G.; Mkawi, E.M.; et al. Silica-Based Bioactive Glasses and Their Applications in Hard Tissue Regeneration: A Review. Pharmaceuticals 2021, 14, 75. https://doi.org/10.3390/ph14020075
Al-Harbi N, Mohammed H, Al-Hadeethi Y, Bakry AS, Umar A, Hussein MA, Abbassy MA, Vaidya KG, Al Berakdar G, Mkawi EM, et al. Silica-Based Bioactive Glasses and Their Applications in Hard Tissue Regeneration: A Review. Pharmaceuticals. 2021; 14(2):75. https://doi.org/10.3390/ph14020075
Chicago/Turabian StyleAl-Harbi, Nuha, Hiba Mohammed, Yas Al-Hadeethi, Ahmed Samir Bakry, Ahmad Umar, Mahmoud Ali Hussein, Mona Aly Abbassy, Karthik Gurunath Vaidya, Ghada Al Berakdar, Elmoiz Merghni Mkawi, and et al. 2021. "Silica-Based Bioactive Glasses and Their Applications in Hard Tissue Regeneration: A Review" Pharmaceuticals 14, no. 2: 75. https://doi.org/10.3390/ph14020075
APA StyleAl-Harbi, N., Mohammed, H., Al-Hadeethi, Y., Bakry, A. S., Umar, A., Hussein, M. A., Abbassy, M. A., Vaidya, K. G., Al Berakdar, G., Mkawi, E. M., & Nune, M. (2021). Silica-Based Bioactive Glasses and Their Applications in Hard Tissue Regeneration: A Review. Pharmaceuticals, 14(2), 75. https://doi.org/10.3390/ph14020075









