Prospects of Topoisomerase Inhibitors as Promising Anti-Cancer Agents
Abstract
:1. Introduction
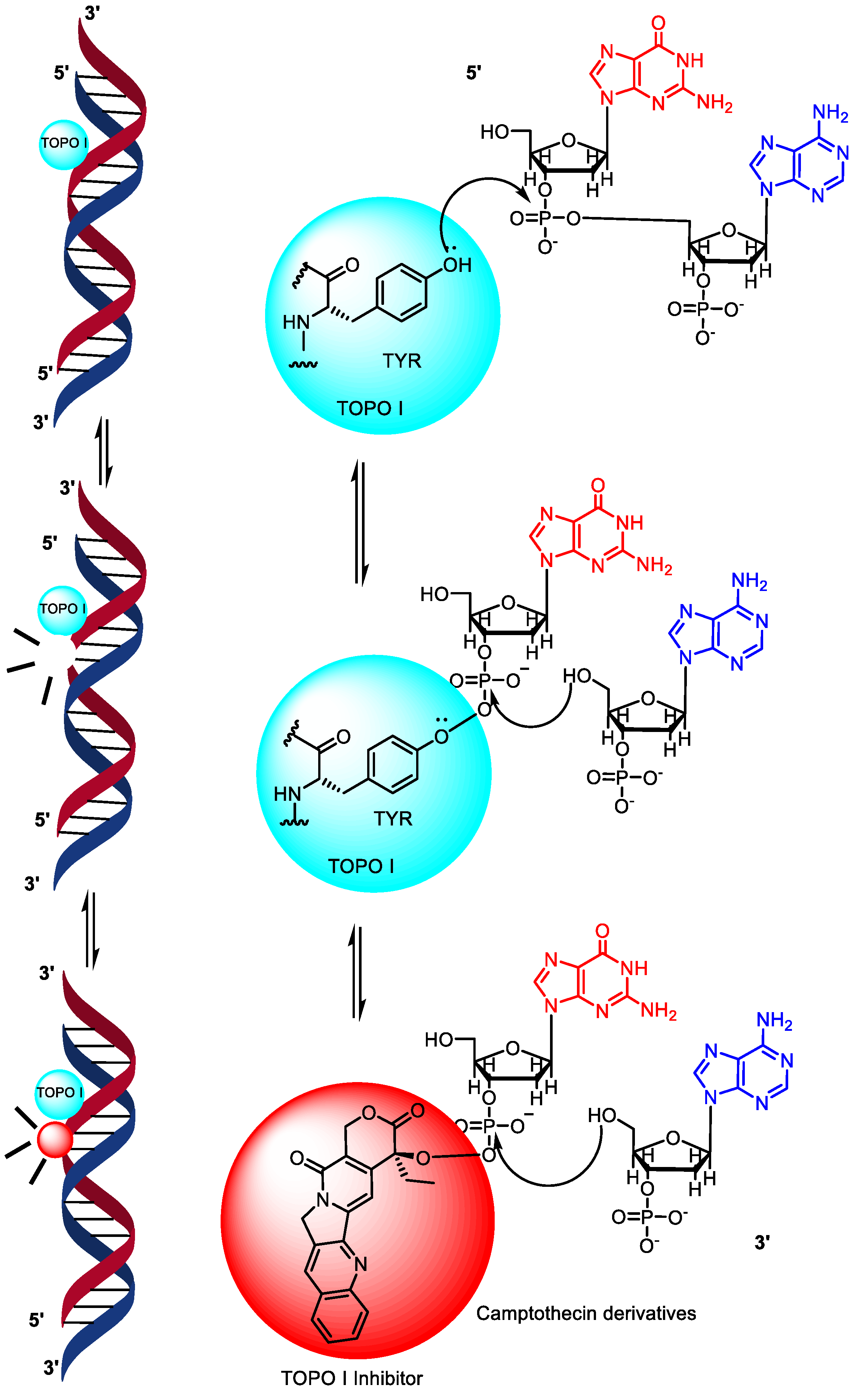
1.1. Topoisomerase I Mechanism of Action
1.2. Mechanism of Action of Topoisomerase II
2. Drugs in Clinical Usage
2.1. Anthracycline-Based Clinically Used DNA-Topoisomerase Inhibitors
2.2. Anthracenedione and Acridine Derivatives
2.3. Camptothecin Analogues
2.4. Epipodophyllotoxin Derivatives
| Sl. | Drug | Class | Mechanism/Target | Indications | Adverse Drug Reactions | Ref. |
|---|---|---|---|---|---|---|
| 1 | Doxorubicin | Anthracycline | Topoisomerase IIα and IIβ poison, intercalation, free radicals | Various cancers | Cardiotoxicity, myelosuppression, nausea, potential for cumulative toxicity | [53,54] |
| 2 | Epirubicin | Anthracycline | Topoisomerase IIα and IIβ poison, intercalation, free radicals | Breast cancer | Cardiotoxicity, myelosuppression, nausea, potential for cumulative toxicity | [36] |
| 3 | Valrubicin | Anthracycline | Topoisomerase IIα and IIβ poison, intercalation, free radicals | Urinary bladder carcinoma | Local irritation, urinary symptoms, myelosuppression | [55] |
| 4 | Daunorubicin | Anthracycline | Topoisomerase IIα and IIβ poison, intercalation, free radicals | Leukemia | Cardiotoxicity, myelosuppression, nausea, potential for cumulative toxicity | [56] |
| 5 | Idarubicin | Anthracycline | Topoisomerase IIα and IIβ poison, intercalation, free radicals | Leukemia | Cardiotoxicity, myelosuppression, nausea, potential for cumulative toxicity | [57] |
| 6 | Mitoxantrone | Anthracenedione | Topoisomerase II poison, intercalation | Leukemia, prostate cancer, MS | Myelosuppression, potential for cumulative toxicity, potential for myelosuppression | [58] |
| 7 | Pixantrone | Anthracenedione | Topoisomerase II poison, intercalation | Non-Hodgkin B-cell lymphoma | Myelosuppression, potential for cumulative toxicity | [43] |
| 8 | Amsacrine | Acridine | Topoisomerase II poison, intercalation | Acute leukemia | Myelosuppression, potential for cumulative toxicity | |
| 9 | Camptothecin | Camptothecin | Topoisomerase I inhibitor, DNA strand breaks | Not specified | Gastrointestinal toxicity, myelosuppression, potential for cumulative toxicity | [59] |
| 10 | Topotecan | Camptothecin | Topoisomerase I inhibitor, DNA strand breaks | Small-cell lung cancer | Myelosuppression, gastrointestinal toxicity, potential for cumulative toxicity | [60,61] |
| 11 | Irinotecan | Camptothecin | Topoisomerase I inhibitor, DNA strand breaks | Colon and rectal carcinoma | Diarrhea, myelosuppression, potential for cumulative toxicity | [62] |
| 12 | Belotecan | Camptothecin | Topoisomerase I inhibitor, DNA strand breaks | Non-small-cell lung cancer, ovarian cancer | Myelosuppression, gastrointestinal toxicity, potential for cumulative toxicity | [50] |
| 13 | Etoposide | Epipodophyllotoxin | Topoisomerase II poison, intercalation | Testicular tumors, small-cell lung cancer | Myelosuppression, gastrointestinal toxicity, potential for cumulative toxicity | [63] |
| 14 | Teniposide | Epipodophyllotoxin | Topoisomerase II poison, intercalation | Childhood acute lymphoblastic leukemia | Myelosuppression, gastrointestinal toxicity, potential for cumulative toxicity | [64] |
3. TOPO Inhibitors in Clinical Trials
3.1. Topoisomerase Inhibitors in Phase 1 Clinical Trials
3.2. Topoisomerase Inhibitors in Phase 2 Clinical Trials
3.3. Topoisomerase Inhibitors in Phase 3 Clinical Trials
4. Topoisomerase Inhibitors in Preclinical Studies
4.1. Naphthalimide–Benzothiazole Derivatives
4.2. β-Carboline Hybrids as Topoisomerase Inhibitors
4.3. Imidazopyridinyl-1,3,4-Oxadiazole Derivatives
4.4. Pyrazole-Linked Benzothiazole-β-Naphthol Derivatives
4.5. Podophyllotoxin Congeners
4.6. Benzimidazoles Congeners
5. Conclusions
6. Recent Advances in the Discovery of New and Novel Topoisomerase Inhibitors
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Delgado, J.L.; Hsieh, C.M.; Chan, N.L.; Hiasa, H. Topoisomerases as Anticancer Targets. Biochem. J. 2018, 475, 373–398. [Google Scholar] [CrossRef] [PubMed]
- Jain, C.K.; Pradhan, B.S.; Banerjee, S.; Mondal, N.B.; Majumder, S.S.; Bhattacharyya, M.; Chakrabarti, S.; Roychoudhury, S.; Majumder, H.K. Sulfonoquinovosyl Diacylglyceride Selectively Targets Acute Lymphoblastic Leukemia Cells and Exerts Potent Anti-Leukemic Effects In Vivo. Sci. Rep. 2015, 5, 12082. [Google Scholar] [CrossRef] [PubMed]
- Jang, J.Y.; Kim, D.; Kim, N.D. Recent Developments in Combination Chemotherapy for Colorectal and Breast Cancers with Topoisomerase Inhibitors. Int. J. Mol. Sci. 2023, 24, 8457. [Google Scholar] [CrossRef]
- Capranico, G.; Marinello, J.; Chillemi, G. Type I DNA Topoisomerases. J. Med. Chem. 2017, 60, 2169–2192. [Google Scholar] [CrossRef] [PubMed]
- Rajan, R.; Osterman, A.K.; Gast, A.T.; Mondragón, A. Biochemical Characterization of the Topoisomerase Domain of Methanopyrus Kandleri Topoisomerase V. J. Biol. Chem. 2014, 289, 28898–28909. [Google Scholar] [CrossRef]
- Nitiss, J.L. DNA Topoisomerase II and Its Growing Repertoire of Biological Functions. Nat. Rev. Cancer 2009, 9, 327. [Google Scholar] [CrossRef]
- Wang, Y.; Rakela, S.; Chambers, J.W.; Hua, Z.C.; Muller, M.T.; Nitiss, J.L.; Tse-Dinh, Y.C.; Leng, F. Kinetic Study of DNA Topoisomerases by Supercoiling-Dependent Fluorescence Quenching. ACS Omega 2019, 4, 18413–18422. [Google Scholar] [CrossRef]
- Oppegard, L.M.; Delgado, J.L.; Kulkarni, C.A.; Towle, T.R.; Hart, D.E.; Williams, B.P.; Lentz, S.R.C.; Norris, B.J.; Flory, C.M.; Schumacher, R.J.; et al. Novel N-1 Substituted Fluoroquinolones Inhibit Human Topoisomerase I Activity and Exhibit Anti-Proliferative Activity. Investig. New Drugs 2019, 37, 378–383. [Google Scholar] [CrossRef]
- Sooryakumar, D.; Dexheimer, T.S.; Teicher, B.A.; Pommier, Y. Molecular and Cellular Pharmacology of the Novel Noncamptothecin Topoisomerase I Inhibitor Genz-644282. Mol. Cancer Ther. 2011, 10, 1490–1499. [Google Scholar] [CrossRef]
- McKie, S.J.; Neuman, K.C.; Maxwell, A. DNA Topoisomerases: Advances in Understanding of Cellular Roles and Multi-Protein Complexes via Structure-Function Analysis. Bioessays 2021, 43, e2000286. [Google Scholar] [CrossRef]
- Buzun, K.; Bielawska, A.; Bielawski, K.; Gornowicz, A. DNA Topoisomerases as Molecular Targets for Anticancer Drugs. J. Enzym. Inhib. Med. Chem. 2020, 35, 1781–1799. [Google Scholar] [CrossRef] [PubMed]
- Singh, B.N.; Mudgil, Y.; Sopory, S.K.; Reddy, M.K. Molecular Characterization of a Nuclear Topoisomerase II from Nicotiana Tabacum That Functionally Complements a Temperature-Sensitive Topoisomerase II Yeast Mutant. Plant Mol. Biol. 2003, 52, 1063–1076. [Google Scholar] [CrossRef] [PubMed]
- Dasgupta, T.; Ferdous, S.; Tse-Dinh, Y.C. Mechanism of Type IA Topoisomerases. Molecules 2020, 25, 4769. [Google Scholar] [CrossRef] [PubMed]
- Berney, D.M.; Shamash, J.; Gaffney, J.; Jordan, S.; Oliver, R.T.D. DNA Topoisomerase I and II Expression in Drug Resistant Germ Cell Tumours. Br. J. Cancer 2002, 87, 624–629. [Google Scholar] [CrossRef]
- Marini, V.; Nikulenkov, F.; Samadder, P.; Juul, S.; Knudsen, B.R.; Krejci, L. MUS81 Cleaves TOP1-Derived Lesions and Other DNA–Protein Cross-Links. BMC Biol. 2023, 21, 110. [Google Scholar] [CrossRef]
- Pommier, Y.; Barcelo, J.M.; Rao, V.A.; Sordet, O.; Jobson, A.G.; Thibaut, L.; Miao, Z.H.; Seiler, J.A.; Zhang, H.; Marchand, C.; et al. Repair of Topoisomerase I-Mediated DNA Damage. Prog. Nucleic Acid. Res. Mol. Biol. 2006, 81, 179. [Google Scholar] [CrossRef]
- Yildizhan, H.; Barkan, N.P.; Turan, S.K.; Demiralp, Ö.; Demiralp, F.D.Ö.; Uslu, B.; Ōzkan, S.A. Treatment Strategies in Cancer from Past to Present. In Drug Targeting and Stimuli Sensitive Drug Delivery Systems; William Andrew Publishing: Norwich, NY, USA, 2018; pp. 1–37. [Google Scholar] [CrossRef]
- Martin, S.A. The DNA Mismatch Repair Pathway. In DNA Repair in Cancer Therapy: Molecular Targets and Clinical Applications: Second Edition; Academic Press: Cambridge, MA, USA, 2016; pp. 151–177. [Google Scholar] [CrossRef]
- Bjornsti, M.A.; Kaufmann, S.H. Topoisomerases and Cancer Chemotherapy: Recent Advances and Unanswered Questions. F1000Research 2019, 8, 1704. [Google Scholar] [CrossRef]
- Radaeva, M.; Dong, X.; Cherkasov, A. The Use of Methods of Computer-Aided Drug Discovery in the Development of Topoisomerase II Inhibitors: Applications and Future Directions. J. Chem. Inf. Model. 2020, 60, 3703–3721. [Google Scholar] [CrossRef]
- Pommier, Y. Topoisomerase I Inhibitors: Camptothecins and Beyond. Nat. Rev. Cancer 2006, 6, 789–802. [Google Scholar] [CrossRef]
- Hu, W.; Huang, X.S.; Wu, J.F.; Yang, L.; Zheng, Y.T.; Shen, Y.M.; Li, Z.Y.; Li, X. Discovery of Novel Topoisomerase II Inhibitors by Medicinal Chemistry Approaches. J. Med. Chem. 2018, 61, 8947–8980. [Google Scholar] [CrossRef]
- Bailly, C. Contemporary Challenges in the Design of Topoisomerase II Inhibitors for Cancer Chemotherapy. Chem. Rev. 2012, 112, 3611–3640. [Google Scholar] [CrossRef] [PubMed]
- Deweese, J.E.; Osheroff, N. The DNA Cleavage Reaction of Topoisomerase II: Wolf in Sheep’s Clothing. Nucleic Acids Res. 2009, 37, 738. [Google Scholar] [CrossRef] [PubMed]
- Goffart, S.; Hangas, A.; Pohjoismäki, J.L.O. Twist and Turn—Topoisomerase Functions in Mitochondrial DNA Maintenance. Int. J. Mol. Sci. 2019, 20, 2041. [Google Scholar] [CrossRef] [PubMed]
- McClendon, A.K.; Osheroff, N. DNA Topoisomerase II, Genotoxicity, and Cancer. Mutat. Res. 2007, 623, 83. [Google Scholar] [CrossRef] [PubMed]
- El-Husseiny, W.M.; El-Sayed, M.A.-A.; El-Azab, A.S.; AlSaif, N.A.; Alanazi, M.M.; Abdel-Aziz, A.A.-M. Synthesis of New Polycyclic Systems with Potential Antitumor Activity and Angiogenic Biological Studies. J. Enzym. Inhib. Med. Chem. 2012, 35, 744–758. [Google Scholar] [CrossRef]
- Ketron, A.C.; Osheroff, N. Phytochemicals as Anticancer and Chemopreventive Topoisomerase II Poisons. Phytochem. Rev. 2014, 13, 19–35. [Google Scholar] [CrossRef]
- Ganga Reddy, V.; Srinivasa Reddy, T.; Privér, S.H.; Bai, Y.; Mishra, S.; Wlodkowic, D.; Mirzadeh, N.; Bhargava, S. Synthesis of Gold(I) Complexes Containing Cinnamide: In Vitro Evaluation of Anticancer Activity in 2D and 3D Spheroidal Models of Melanoma and In Vivo Angiogenesis. Inorg. Chem. 2019, 58, 5988–5999. [Google Scholar] [CrossRef]
- Schoeffler, A.J.; Berger, J.M. DNA Topoisomerases: Harnessing and Constraining Energy to Govern Chromosome Topology. Q. Rev. Biophys. 2008, 41, 41–101. [Google Scholar] [CrossRef]
- Jian, J.Y.; Osheroff, N. Telling Your Right Hand from Your Left: The Effects of DNA Supercoil Handedness on the Actions of Type II Topoisomerases. Int. J. Mol. Sci. 2023, 24, 11199. [Google Scholar] [CrossRef]
- Hevener, K.E.; Verstak, T.A.; Lutat, K.E.; Riggsbee, D.L.; Mooney, J.W. Recent Developments in Topoisomerase-Targeted Cancer Chemotherapy. Acta Pharm. Sin. B 2018, 8, 844–861. [Google Scholar] [CrossRef]
- Pommier, Y.; Leo, E.; Zhang, H.; Marchand, C. DNA Topoisomerases and Their Poisoning by Anticancer and Antibacterial Drugs. Chem. Biol. 2010, 17, 421–433. [Google Scholar] [CrossRef] [PubMed]
- Johnson-Arbor, K.; Dubey, R. Doxorubicin. In xPharm: The Comprehensive Pharmacology Reference; Elsevier: Amsterdam, The Netherlands, 2022; pp. 1–5. [Google Scholar] [CrossRef]
- Wang, H.; Xiao, X.; Xiao, Q.; Lu, Y.; Wu, Y. The Efficacy and Safety of Daunorubicin versus Idarubicin Combined with Cytarabine for Induction Therapy in Acute Myeloid Leukemia: A Meta-Analysis of Randomized Clinical Trials. Medicine 2020, 99, E20094. [Google Scholar] [CrossRef] [PubMed]
- Ghorbani-Abdi-Saedabad, A.; Hanafi-Bojd, M.Y.; Parsamanesh, N.; Tayarani-Najaran, Z.; Mollaei, H.; Hoshyar, R. Anticancer and Apoptotic Activities of Parthenolide in Combination with Epirubicin in Mda-Mb-468 Breast Cancer Cells. Mol. Biol. Rep. 2020, 47, 5807–5815. [Google Scholar] [CrossRef] [PubMed]
- Miyoshi, Y.; Kurosumi, M.; Kurebayashi, J.; Matsuura, N.; Takahashi, M.; Tokunaga, E.; Egawa, C.; Masuda, N.; Kim, S.J.; Okishiro, M.; et al. Topoisomerase IIalpha-Positive and BRCA1-Negative Phenotype: Association with Favorable Response to Epirubicin-Based Regimens for Human Breast Cancers. Cancer Lett. 2008, 264, 44–53. [Google Scholar] [CrossRef]
- Kuznetsov, D.D.; Alsikafi, N.F.; O’Connor, R.C.; Steinberg, G.D. Intravesical Valrubicin in the Treatment of Carcinoma in Situ of the Bladder. Expert. Opin. Pharmacother. 2001, 2, 1009–1013. [Google Scholar] [CrossRef]
- Nitiss, J.L.; Kiianitsa, K.; Sun, Y.; Nitiss, K.C.; Maizels, N. Topoisomerase Assays. Curr. Protoc. 2021, 1, e250. [Google Scholar] [CrossRef]
- Chan, M.K.; Fadzil, N.A.; Chew, A.L.; Khoo, B.Y. New Molecular Biologist Perspective and Insight: DNA Topoisomerases Production by Recombinant DNA Technology for Medical Laboratory Application and Pharmaceutical Industry. Electron. J. Biotechnol. 2013, 16, 18. [Google Scholar] [CrossRef]
- Sawyer, D.B.; Peng, X.; Chen, B.; Pentassuglia, L.; Lim, C.C. Mechanisms of Anthracycline Cardiac Injury: Can We Identify Strategies for Cardio-Protection? Prog. Cardiovasc. Dis. 2010, 53, 105. [Google Scholar] [CrossRef]
- Dempke, W.C.M.; Zielinski, R.; Winkler, C.; Silberman, S.; Reuther, S.; Priebe, W. Anthracycline-Induced Cardiotoxicity—Are We about to Clear This Hurdle? Eur. J. Cancer 2023, 185, 94–104. [Google Scholar] [CrossRef]
- Zinzani, P.L.; Corradini, P.; Martelli, M.; Minotti, G.; Oliva, S.; Spina, M.; Barosi, G.; Tura, S. Critical Concepts, Practice Recommendations, and Research Perspectives of Pixantrone Therapy in Non-Hodgkin Lymphoma: A SIE, SIES, and GITMO Consensus Paper. Eur. J. Haematol. 2016, 97, 554–561. [Google Scholar] [CrossRef]
- Yakkala, P.A.; Panda, S.R.; Naidu, V.G.M.; Shafi, S.; Kamal, A. Pyridine-Based 1,2,4-Triazolo-Tethered Indole Conjugates Potentially Affecting TNKS and PI3K in Colorectal Cancer. ACS Med. Chem. Lett. 2023, 14, 260–269. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Jiang, T.; Li, Q.; Ling, X. Camptothecin (CPT) and Its Derivatives Are Known to Target Topoisomerase I (Top1) as Their Mechanism of Action: Did We Miss Something in CPT Analogue Molecular Targets for Treating Human Disease Such as Cancer? Am. J. Cancer Res. 2017, 7, 2350. [Google Scholar] [PubMed]
- Robati, M.; Holtz, D.; Dunton, C.J. A Review of Topotecan in Combination Chemotherapy for Advanced Cervical Cancer. Ther. Clin. Risk Manag. 2008, 4, 213. [Google Scholar] [CrossRef] [PubMed]
- Goto, K.; Ohe, Y.; Shibata, T.; Seto, T.; Takahashi, T.; Nakagawa, K.; Tanaka, H.; Takeda, K.; Nishio, M.; Mori, K.; et al. Combined Chemotherapy with Cisplatin, Etoposide, and Irinotecan versus Topotecan Alone as Second-Line Treatment for Patients with Sensitive Relapsed Small-Cell Lung Cancer (JCOG0605): A Multicentre, Open-Label, Randomised Phase 3 Trial. Lancet Oncol. 2016, 17, 1147–1157. [Google Scholar] [CrossRef]
- Fujita, K.I.; Kubota, Y.; Ishida, H.; Sasaki, Y. Irinotecan, a Key Chemotherapeutic Drug for Metastatic Colorectal Cancer. World J. Gastroenterol. 2015, 21, 12234. [Google Scholar] [CrossRef]
- Kim, J.H.; Kim, H.S.; Han, A.R.; Moh, I.H.; Chung, D.C.; Choi, D.R.; Jang, H.J.; Kim, J.B.; Yang, D.H.; Lee, S.I.; et al. Irinotecan, Leucovorin and 5-Fluorouracil (Modified FOLFIRI) as Salvage Chemotherapy for Frail or Elderly Patients with Advanced Gastric Cancer. Oncol. Lett. 2012, 4, 751. [Google Scholar] [CrossRef]
- Kim, Y.M.; Lee, S.W.; Kim, D.Y.; Kim, J.H.; Nam, J.H.; Kim, Y.T. The Efficacy and Toxicity of Belotecan (CKD-602), a Camptothericin Analogue Topoisomerase I Inhibitor, in Patients with Recurrent or Refractory Epithelial Ovarian Cancer. J. Chemother. 2010, 22, 197–200. [Google Scholar] [CrossRef]
- Bethesda LiverTox. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury; National Institute of Diabetes and Digestive and Kidney Diseases: Bethesda, MD, USA, 2012. [Google Scholar]
- Agrawal, K. Teniposide. In xPharm: The Comprehensive Pharmacology Reference; Elsevier: Amsterdam, The Netherlands, 2007; pp. 1–4. [Google Scholar] [CrossRef]
- Kollárová-Brázdová, P.; Jirkovská, A.; Karabanovich, G.; Pokorná, Z.; Piskáčková, H.B.; Jirkovský, E.; Kubeš, J.; Lenčová-Popelová, O.; Mazurová, Y.; Adamcová, M.; et al. Investigation of Structure-Activity Relationships of Dexrazoxane Analogs Reveals Topoisomerase IIβ Interaction as a Prerequisite for Effective Protection against Anthracycline Cardiotoxicity. J. Pharmacol. Exp. Ther. 2020, 373, 402–415. [Google Scholar] [CrossRef]
- Deng, S.; Yan, T.; Jendrny, C.; Nemecek, A.; Vincetic, M.; Gödtel-Armbrust, U.; Wojnowski, L. Dexrazoxane May Prevent Doxorubicin-Induced DNA Damage via Depleting Both Topoisomerase II Isoforms. BMC Cancer 2014, 14, 842. [Google Scholar] [CrossRef]
- Marinello, J.; Delcuratolo, M.; Capranico, G. Anthracyclines as Topoisomerase II Poisons: From Early Studies to New Perspectives. Int. J. Mol. Sci. 2018, 19, 3480. [Google Scholar] [CrossRef]
- Saleem, T.; Kasi, A. Daunorubicin. In xPharm: The Comprehensive Pharmacology Reference; Elsevier: Amsterdam, The Netherlands, 2022; pp. 1–4. [Google Scholar] [CrossRef]
- Volkova, M.; Raymond Russell, I. Anthracycline Cardiotoxicity: Prevalence, Pathogenesis and Treatment. Curr. Cardiol. Rev. 2011, 7, 214. [Google Scholar] [CrossRef] [PubMed]
- Evison, B.J.; Sleebs, B.E.; Watson, K.G.; Phillips, D.R.; Cutts, S.M. Mitoxantrone, More than Just Another Topoisomerase II Poison. Med. Res. Rev. 2016, 36, 248–299. [Google Scholar] [CrossRef] [PubMed]
- Rose, W.C.; Marathe, P.H.; Jang, G.R.; Monticello, T.M.; Balasubramanian, B.N.; Long, B.; Fairchild, C.R.; Wall, M.E.; Wani, M.C. Novel Fluoro-Substituted Camptothecins: In Vivo Antitumor Activity, Reduced Gastrointestinal Toxicity and Pharmacokinetic Characterization. Cancer Chemother. Pharmacol. 2006, 58, 73–85. [Google Scholar] [CrossRef] [PubMed]
- Lv, C.; Liu, X.; Zheng, Q.; Chen, H.; Yang, X.; Zhong, J.; Wang, Y.; Duan, J.; Wang, Z.; Bai, H.; et al. Analysis of Topoisomerase I Expression and Identification of Predictive Markers for Efficacy of Topotecan Chemotherapy in Small Cell Lung Cancer. Thorac. Cancer 2018, 9, 1166–1173. [Google Scholar] [CrossRef] [PubMed]
- Vennepureddy, A.; Atallah, J.-P.; Terjanian, T. Role of Topotecan in Non-Small Cell Lung Cancer: A Review of Literature. World J. Oncol. 2015, 6, 429. [Google Scholar] [CrossRef]
- Tsavaris, N.; Ziras, N.; Kosmas, C.; Giannakakis, T.; Gouveris, P.; Vadiaka, M.; Dimitrakopoulos, A.; Karadima, D.; Rokana, S.; Papalambros, E.; et al. Two Different Schedules of Irinotecan (CPT-11) in Patients with Advanced Colorectal Carcinoma Relapsing after a 5-Fluorouracil and Leucovorin Combination. A Randomized Study. Cancer Chemother. Pharmacol. 2003, 52, 514–519. [Google Scholar] [CrossRef]
- Smith, N.A.; Byl, J.A.W.; Mercer, S.L.; Deweese, J.E.; Osheroff, N. Etoposide Quinone Is a Covalent Poison of Human Topoisomerase IIβ. Biochemistry 2014, 53, 3229–3236. [Google Scholar] [CrossRef]
- Fraser, J.; Wills, L.; Fardus-Reid, F.; Irvine, L.; Elliss-Brookes, L.; Fern, L.; Cameron, A.L.; Pritchard-Jones, K.; Feltbower, R.G.; Shelton, J.; et al. Oral Etoposide as a Single Agent in Childhood and Young Adult Cancer in England: Still a Poorly Evaluated Palliative Treatment. Pediatr. Blood Cancer 2021, 68, e29204. [Google Scholar] [CrossRef]
- Cushman, M. Design and Synthesis of Indenoisoquinolines Targeting Topoisomerase I and Other Biological Macromolecules for Cancer Chemotherapy. J. Med. Chem. 2021, 64, 17572–17600. [Google Scholar] [CrossRef]
- Pommier, Y.; Cushman, M. The Indenoisoquinolines Non-Camptothecin Topoisomerase I Inhibitors: Update and Perspectives. Mol. Cancer Ther. 2009, 8, 1008. [Google Scholar] [CrossRef]
- Zuco, V.; Supino, R.; Favini, E.; Tortoreto, M.; Cincinelli, R.; Croce, A.C.; Bucci, F.; Pisano, C.; Zunino, F. Efficacy of ST1968 (Namitecan) on a Topotecan-Resistant Squamous Cell Carcinoma. Biochem. Pharmacol. 2010, 79, 535–541. [Google Scholar] [CrossRef] [PubMed]
- Benton, C.B.; Ravandi, F. Targeting Acute Myeloid Leukemia with TP53-Independent Vosaroxin. Future Oncol. 2017, 13, 125–133. [Google Scholar] [CrossRef]
- Faruqi, A.; Tadi, P. Cytarabine. In xPharm: The Comprehensive Pharmacology Reference; Elsevier: Amsterdam, The Netherlands, 2022; pp. 1–5. [Google Scholar] [CrossRef]
- Gadade, D.D.; Pekamwar, S.S. Cyclodextrin Based Nanoparticles for Drug Delivery and Theranostics. Adv. Pharm. Bull. 2020, 10, 166. [Google Scholar] [CrossRef]
- Pettengell, R.; Długosz-Danecka, M.; Andorsky, D.; Belada, D.; Georgiev, P.; Quick, D.; Singer, J.W.; Singh, S.B.; Pallis, A.; Egorov, A.; et al. Pixantrone plus Rituximab versus Gemcitabine plus Rituximab in Patients with Relapsed Aggressive B-Cell Non-Hodgkin Lymphoma Not Eligible for Stem Cell Transplantation: A Phase 3, Randomized, Multicentre Trial (PIX306). Br. J. Haematol. 2020, 188, 240–248. [Google Scholar] [CrossRef] [PubMed]
- Chamberlain, F.E.; Jones, R.L.; Chawla, S.P. Aldoxorubicin in Soft Tissue Sarcomas. Future Oncol. 2019, 15, 1429–1435. [Google Scholar] [CrossRef] [PubMed]
- Lazareva, N.F.; Baryshok, V.P.; Lazarev, I.M. Silicon-Containing Analogs of Camptothecin as Anticancer Agents. Arch. Pharm. 2018, 351, 1700297. [Google Scholar] [CrossRef]
- Van Arnam, E.B.; Ruzzini, A.C.; Sit, C.S.; Currie, C.R.; Clardy, J. A Rebeccamycin Analog Provides Plasmid-Encoded Niche Defense. J. Am. Chem. Soc. 2015, 137, 14272–14274. [Google Scholar] [CrossRef]
- Robey, R.W.; Obrzut, T.; Shukla, S.; Polgar, O.; MacAlou, S.; Bahr, J.C.; Di Pietro, A.; Ambudkar, S.V.; Bates, S.E. Becatecarin (Rebeccamycin Analog, NSC 655649) Is a Transport Substrate and Induces Expression of the ATP-Binding Cassette Transporter, ABCG2, in Lung Carcinoma Cells. Cancer Chemother. Pharmacol. 2009, 64, 575. [Google Scholar] [CrossRef]
- Sankara Rao, N.; Nagesh, N.; Lakshma Nayak, V.; Sunkari, S.; Tokala, R.; Kiranmai, G.; Regur, P.; Shankaraiah, N.; Kamal, A. Design and Synthesis of DNA-Intercalative Naphthalimide-Benzothiazole/Cinnamide Derivatives: Cytotoxicity Evaluation and Topoisomerase-IIα Inhibition. Medchemcomm 2019, 10, 72–79. [Google Scholar] [CrossRef]
- Kamal, A.; Srinivasulu, V.; Nayak, V.L.; Sathish, M.; Shankaraiah, N.; Bagul, C.; Reddy, N.V.S.; Rangaraj, N.; Nagesh, N. Design and Synthesis of C3-Pyrazole/Chalcone-Linked Beta-Carboline Hybrids: Antitopoisomerase I, DNA-Interactive, and Apoptosis-Inducing Anticancer Agents. ChemMedChem 2014, 9, 2084–2098. [Google Scholar] [CrossRef]
- Kamal, A.; Sathish, M.; Nayak, V.L.; Srinivasulu, V.; Kavitha, B.; Tangella, Y.; Thummuri, D.; Bagul, C.; Shankaraiah, N.; Nagesh, N. Design and Synthesis of Dithiocarbamate Linked β-Carboline Derivatives: DNA Topoisomerase II Inhibition with DNA Binding and Apoptosis Inducing Ability. Bioorg. Med. Chem. 2015, 23, 5511–5526. [Google Scholar] [CrossRef] [PubMed]
- Sathish, M.; Chetan Dushantrao, S.; Nekkanti, S.; Tokala, R.; Thatikonda, S.; Tangella, Y.; Srinivas, G.; Cherukommu, S.; Hari Krishna, N.; Shankaraiah, N.; et al. Synthesis of DNA Interactive C3-Trans-Cinnamide Linked β-Carboline Conjugates as Potential Cytotoxic and DNA Topoisomerase I Inhibitors. Bioorg. Med. Chem. 2018, 26, 4916–4929. [Google Scholar] [CrossRef] [PubMed]
- Jadala, C.; Sathish, M.; Reddy, T.S.; Reddy, V.G.; Tokala, R.; Bhargava, S.K.; Shankaraiah, N.; Nagesh, N.; Kamal, A. Synthesis and in Vitro Cytotoxicity Evaluation of β-Carboline-Combretastatin Carboxamides as Apoptosis Inducing Agents: DNA Intercalation and Topoisomerase-II Inhibition. Bioorg. Med. Chem. 2019, 27, 3285–3298. [Google Scholar] [CrossRef]
- Kovvuri, J.; Nagaraju, B.; Nayak, V.L.; Akunuri, R.; Rao, M.P.N.; Ajitha, A.; Nagesh, N.; Kamal, A. Design, Synthesis and Biological Evaluation of New β-Carboline-Bisindole Compounds as DNA Binding, Photocleavage Agents and Topoisomerase I Inhibitors. Eur. J. Med. Chem. 2018, 143, 1563–1577. [Google Scholar] [CrossRef] [PubMed]
- Subba Rao, A.V.; Vishnu Vardhan, M.V.P.S.; Subba Reddy, N.V.; Srinivasa Reddy, T.; Shaik, S.P.; Bagul, C.; Kamal, A. Synthesis and Biological Evaluation of Imidazopyridinyl-1,3,4-Oxadiazole Conjugates as Apoptosis Inducers and Topoisomerase IIα Inhibitors. Bioorg. Chem. 2016, 69, 7–19. [Google Scholar] [CrossRef] [PubMed]
- Nagaraju, B.; Kovvuri, J.; Kumar, C.G.; Routhu, S.R.; Shareef, M.A.; Kadagathur, M.; Adiyala, P.R.; Alavala, S.; Nagesh, N.; Kamal, A. Synthesis and Biological Evaluation of Pyrazole Linked Benzothiazole-β-Naphthol Derivatives as Topoisomerase I Inhibitors with DNA Binding Ability. Bioorg. Med. Chem. 2019, 27, 708–720. [Google Scholar] [CrossRef]
- Kamal, A.; Kumar, B.A.; Suresh, P.; Agrawal, S.K.; Chashoo, G.; Singh, S.K.; Saxena, A.K. Synthesis of 4β-N-Polyaromatic Substituted Podophyllotoxins: DNA Topoisomerase Inhibition, Anticancer and Apoptosis-Inducing Activities. Bioorg. Med. Chem. 2010, 18, 8493–8500. [Google Scholar] [CrossRef]
- Kamal, A.; Suresh, P.; Ramaiah, M.J.; Mallareddy, A.; Imthiajali, S.; Pushpavalli, S.N.C.V.L.; Lavanya, A.; Pal-Bhadra, M. Synthesis and Biological Evaluation of 4β-Sulphonamido and 4β-[(4′-Sulphonamido)Benzamide]Podophyllotoxins as DNA Topoisomerase-IIα and Apoptosis Inducing Agents. Bioorg. Med. Chem. 2012, 20, 2054–2066. [Google Scholar] [CrossRef]
- Kamal, A.; Suresh, P.; Ramaiah, M.J.; Srinivasa Reddy, T.; Kapavarapu, R.K.; Rao, B.N.; Imthiajali, S.; Lakshminarayan Reddy, T.; Pushpavalli, S.N.C.V.L.; Shankaraiah, N.; et al. 4β-[4′-(1-(Aryl)Ureido)Benzamide]Podophyllotoxins as DNA Topoisomerase i and IIα Inhibitors and Apoptosis Inducing Agents. Bioorg. Med. Chem. 2013, 21, 5198–5208. [Google Scholar] [CrossRef]
- Kamal, A.; Kumar, B.A.; Suresh, P.; Shankaraiah, N.; Kumar, M.S. An Efficient One-Pot Synthesis of Benzothiazolo-4β-Anilino-Podophyllotoxin Congeners: DNA Topoisomerase-II Inhibition and Anticancer Activity. Bioorg. Med. Chem. Lett. 2011, 21, 350–353. [Google Scholar] [CrossRef]
- Shankaraiah, N.; Kumar, N.P.; Amula, S.B.; Nekkanti, S.; Jeengar, M.K.; Naidu, V.G.M.; Reddy, T.S.; Kamal, A. One-Pot Synthesis of Podophyllotoxin-Thiourea Congeners by Employing NH2SO3H/NaI: Anticancer Activity, DNA Topoisomerase-II Inhibition, and Apoptosis Inducing Agents. Bioorg. Med. Chem. Lett. 2015, 25, 4239–4244. [Google Scholar] [CrossRef] [PubMed]
- Reddy, V.G.; Bonam, S.R.; Reddy, T.S.; Akunuri, R.; Naidu, V.G.M.; Nayak, V.L.; Bhargava, S.K.; Kumar, H.M.S.; Srihari, P.; Kamal, A. 4β-Amidotriazole Linked Podophyllotoxin Congeners: DNA Topoisomerase-IIα Inhibition and Potential Anticancer Agents for Prostate Cancer. Eur. J. Med. Chem. 2018, 144, 595–611. [Google Scholar] [CrossRef] [PubMed]
- Sathish, M.; Kavitha, B.; Nayak, V.L.; Tangella, Y.; Ajitha, A.; Nekkanti, S.; Alarifi, A.; Shankaraiah, N.; Nagesh, N.; Kamal, A. Synthesis of Podophyllotoxin Linked β-Carboline Congeners as Potential Anticancer Agents and DNA Topoisomerase II Inhibitors. Eur. J. Med. Chem. 2018, 144, 557–571. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.S.; Gatto, B.; Yu, C.; Liu, A.; Liu, L.F.; LaVoie, E.J. Substituted 2,5′-Bi-1H-Benzimidazoles: Topoisoraerase I Inhibition and Cytotoxicity. J. Med. Chem. 1996, 39, 992–998. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.S.; Yu, C.; Liu, A.; Liu, L.F.; LaVoie, E.J. Terbenzimidazoles: Influence of 2″-, 4-, and 5-Substituents on Cytotoxicity and Relative Potency as Topoisomerase I Poisons. J. Med. Chem. 1997, 40, 2818–2824. [Google Scholar] [CrossRef]
- Coban, G.; Zencir, S.; Zupkó, I.; Réthy, B.; Gunes, H.S.; Topcu, Z. Synthesis and Biological Activity Evaluation of 1H-Benzimidazoles via Mammalian DNA Topoisomerase I and Cytostaticity Assays. Eur. J. Med. Chem. 2009, 44, 2280–2285. [Google Scholar] [CrossRef]
- Singh, M.; Tandon, V. Synthesis and Biological Activity of Novel Inhibitors of Topoisomerase I: 2-Aryl-Substituted 2-Bis-1H-Benzimidazoles. Eur. J. Med. Chem. 2011, 46, 659–669. [Google Scholar] [CrossRef]
- Talukdar, A.; Kundu, B.; Sarkar, D.; Goon, S.; Mondal, M.A. Topoisomerase I Inhibitors: Challenges, Progress and the Road Ahead. Eur. J. Med. Chem. 2022, 236, 114304. [Google Scholar] [CrossRef]
- Majumdar, A.G.; Shree, S.; Das, A.; Kumar, B.K.; Dey, P.; Subramanian, M.; Patro, B.S. Design, Synthesis and Development of a Dual Inhibitor of Topoisomerase 1 and Poly (ADP-Ribose) Polymerase 1 for Efficient Killing of Cancer Cells. Eur. J. Med. Chem. 2023, 258, 115598. [Google Scholar] [CrossRef]
- Idowu, T.; Schweizer, F. Ubiquitous Nature of Fluoroquinolones: The Oscillation between Antibacterial and Anticancer Activities. Antibiotics 2017, 6, 26. [Google Scholar] [CrossRef]
- Beberok, A.; Wrześniok, D.; Rok, J.; Rzepka, Z.; Respondek, M.; Buszman, E. Ciprofloxacin Triggers the Apoptosis of Human Triple-Negative Breast Cancer MDA-MB-231 Cells via the P53/Bax/Bcl-2 Signaling Pathway. Int. J. Oncol. 2018, 52, 1727–1737. [Google Scholar] [CrossRef]
- Ma, Y.C.; Wang, Z.X.; Jin, S.J.; Zhang, Y.X.; Hu, G.Q.; Cui, D.T.; Wang, J.S.; Wang, M.; Wang, F.Q.; Zhao, Z.J. Dual Inhibition of Topoisomerase II and Tyrosine Kinases by the Novel Bis-Fluoroquinolone Chalcone-Like Derivative HMNE3 in Human Pancreatic Cancer Cells. PLoS ONE 2016, 11, e0162821. [Google Scholar] [CrossRef]
- Skok, Ž.; Zidar, N.; Kikelj, D.; Ilaš, J. Dual Inhibitors of Human DNA Topoisomerase II and Other Cancer-Related Targets. J. Med. Chem. 2020, 63, 884–904. [Google Scholar] [CrossRef]
















| Sl. | Drug | Class | Mechanism/Target | Study Phase | NCT Number |
|---|---|---|---|---|---|
| 1 | Indenoisoquinolines 15, 16, 17 | Non-camptothecin type I inhibitors | Stabilize DNA–topoisomerase cleavage complex, preferential DNA cleavage sites | Phase 1 | NCT-01794104 |
| 2 | Namitecan (ST1968) | Topoisomerase I inhibitor | Inhibits topoisomerase I, demonstrated anti-tumor activity | Phase 1 | Not specified |
| 3 | Vosaroxin | Anti-cancer quinolone derivative (AQD) | Targets type II topoisomerases, induces DNA damage and apoptosis | Phase 2 | NCT-02658487 |
| 4 | Cytarabine | Nucleoside analogue | Incorporates into DNA, inhibits DNA synthesis | Phase 2 | NCT-02658487 |
| 5 | CRLX101 | Camptothecin nanoparticle conjugate | Increases tumor cell exposure to camptothecin, tumor-specific targeting | Phase 2 | NCT-01380769 |
| 6 | Pixantrone | Anthracenedione | Induces DNA damage, anti-tumor activity | Phase 3 | NCT-01321541 |
| 7 | Aldoxorubicin | Pro-drug of doxorubicin | Delivers doxorubicin directly to tumor tissue | Phase 3 | NCT-02049905 |
| 8 | Silatecan | Silicon-containing camptothecin derivative | Inhibits topoisomerase I, being evaluated for gliosarcoma | Phase 2 | NCT-01124539 |
| 9 | Becatecarin | Rebeccamycin analogue | Dual topoisomerase I and II poison, clinical development ceased | Phase 2 | NCT-00132600 |
| 10 | Edotecarin | Rebeccamycin analogue | Dual topoisomerase I and II poison, clinical development ceased | Phase 2 | NCT-02310763 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yakkala, P.A.; Penumallu, N.R.; Shafi, S.; Kamal, A. Prospects of Topoisomerase Inhibitors as Promising Anti-Cancer Agents. Pharmaceuticals 2023, 16, 1456. https://doi.org/10.3390/ph16101456
Yakkala PA, Penumallu NR, Shafi S, Kamal A. Prospects of Topoisomerase Inhibitors as Promising Anti-Cancer Agents. Pharmaceuticals. 2023; 16(10):1456. https://doi.org/10.3390/ph16101456
Chicago/Turabian StyleYakkala, Prasanna Anjaneyulu, Naveen Reddy Penumallu, Syed Shafi, and Ahmed Kamal. 2023. "Prospects of Topoisomerase Inhibitors as Promising Anti-Cancer Agents" Pharmaceuticals 16, no. 10: 1456. https://doi.org/10.3390/ph16101456
APA StyleYakkala, P. A., Penumallu, N. R., Shafi, S., & Kamal, A. (2023). Prospects of Topoisomerase Inhibitors as Promising Anti-Cancer Agents. Pharmaceuticals, 16(10), 1456. https://doi.org/10.3390/ph16101456






