Combination of Bacteriophages and Antibiotics for Prevention of Vascular Graft Infections—An In Vitro Study
Abstract
:1. Introduction
2. Results
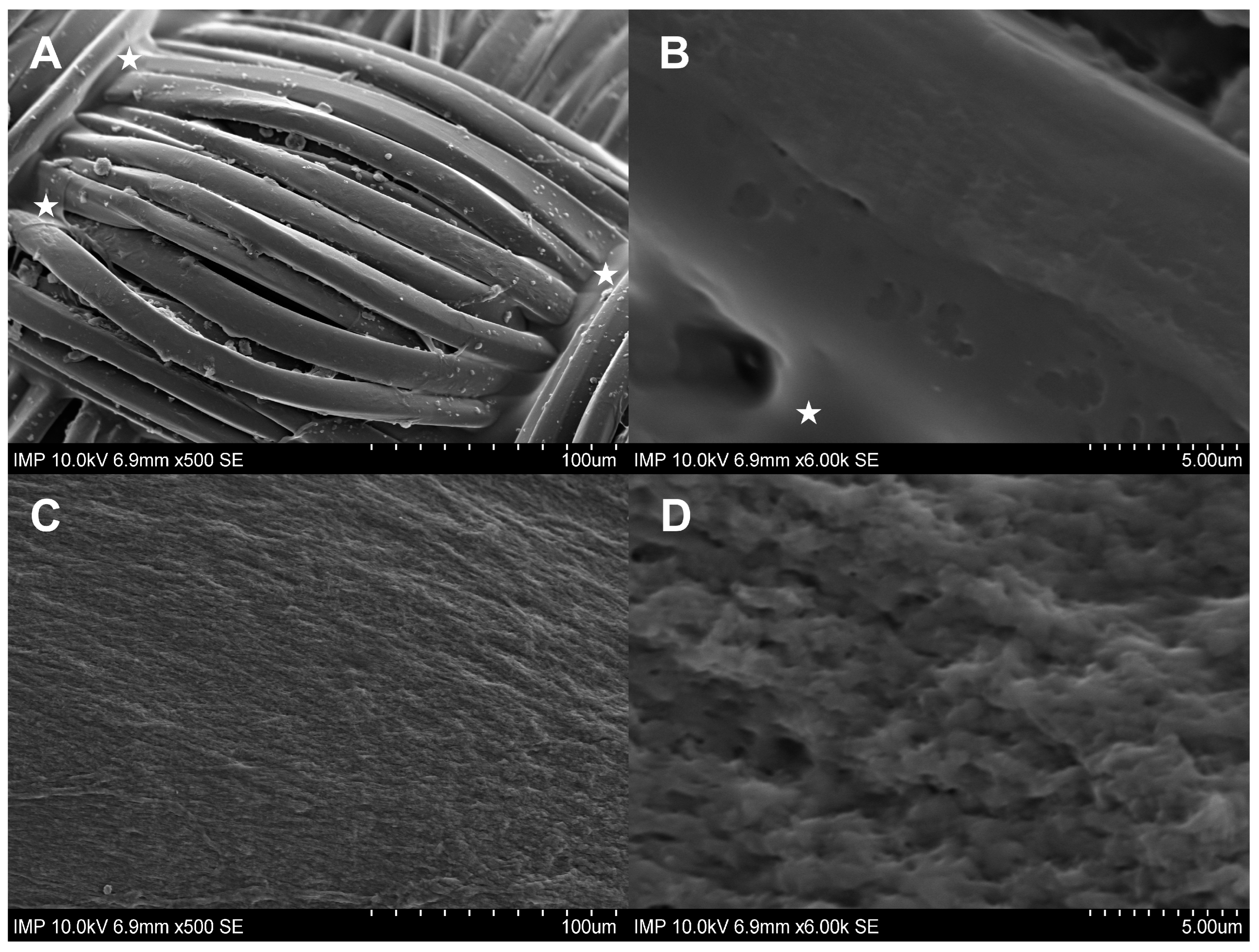
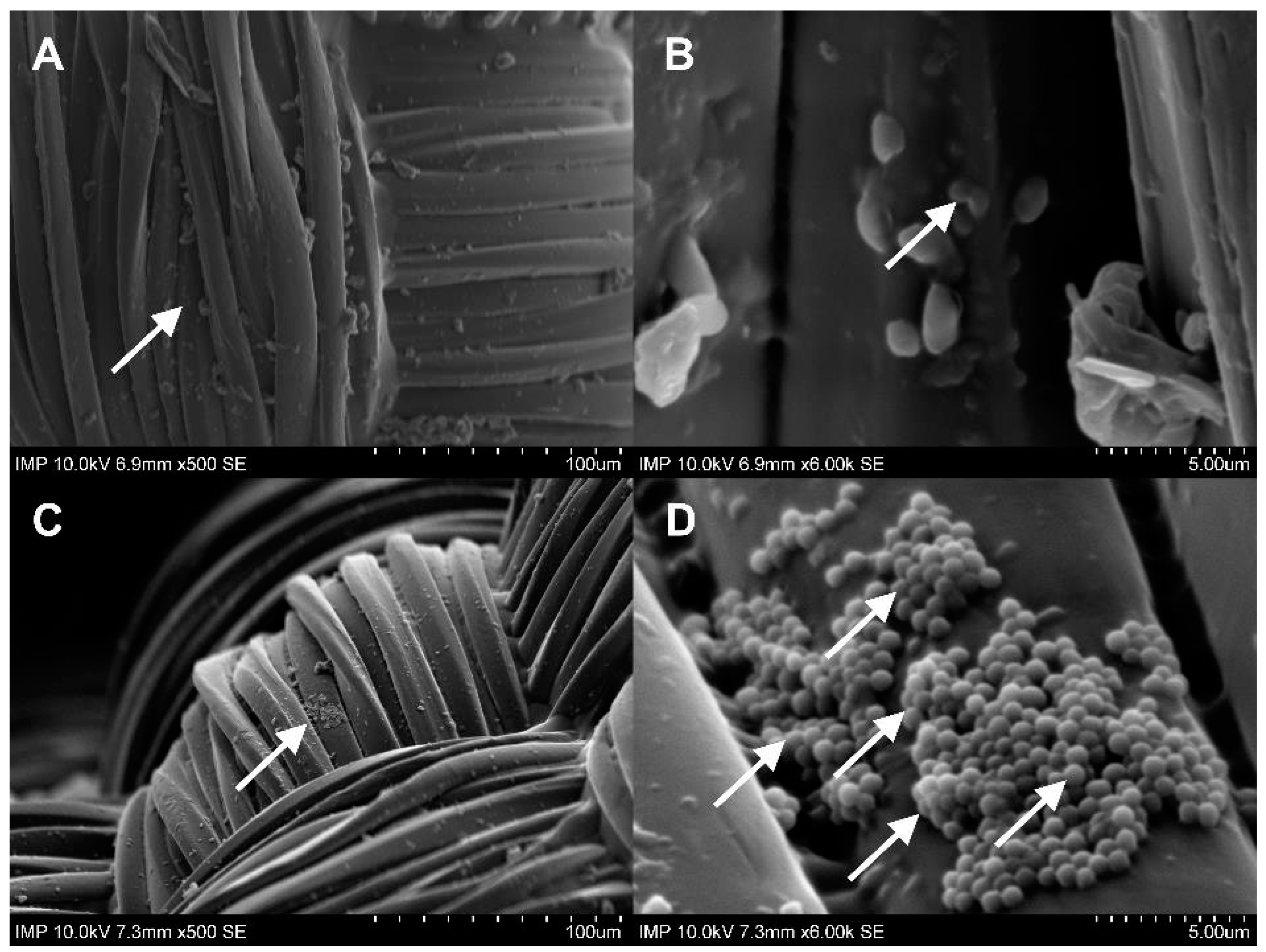
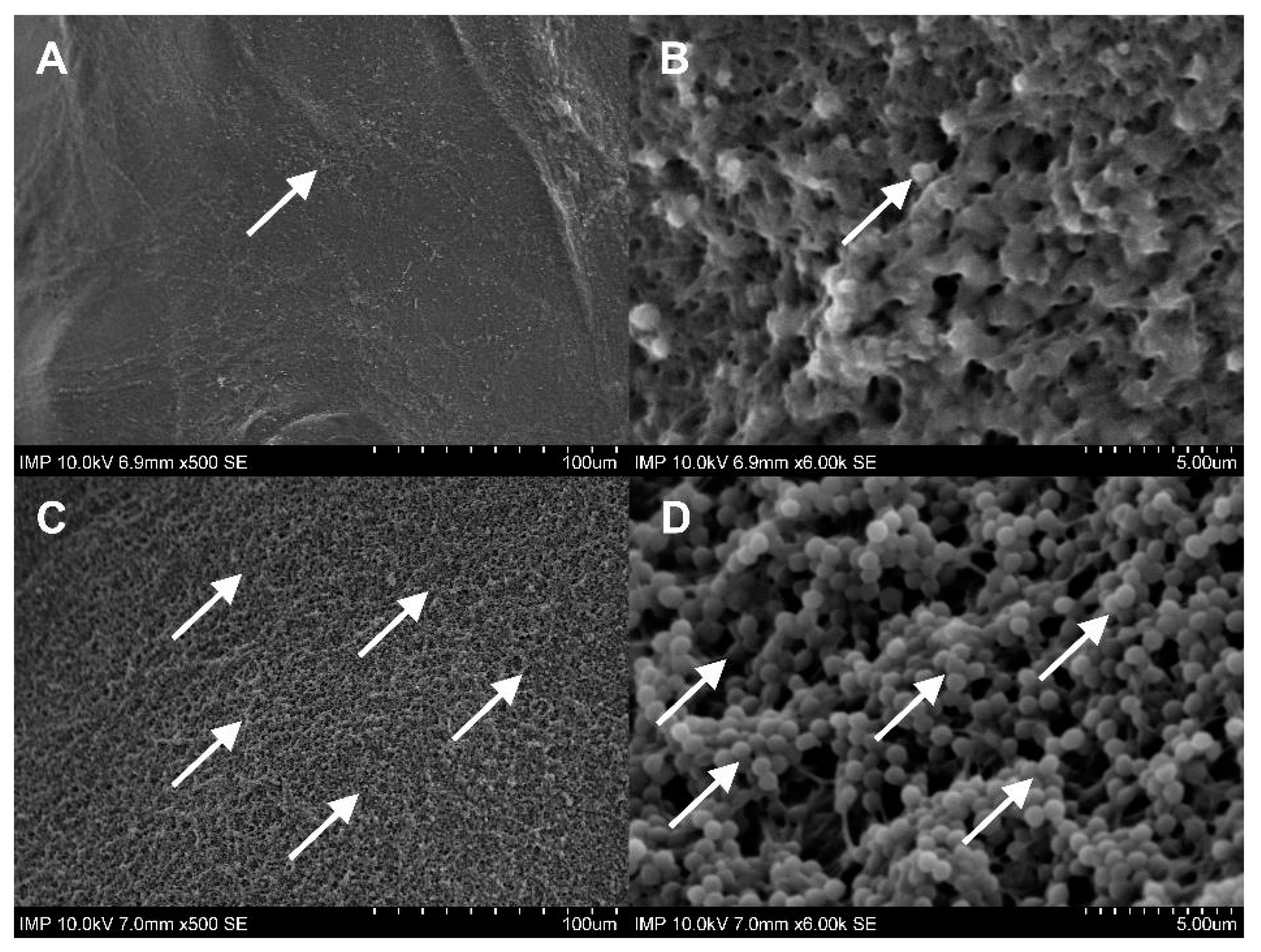
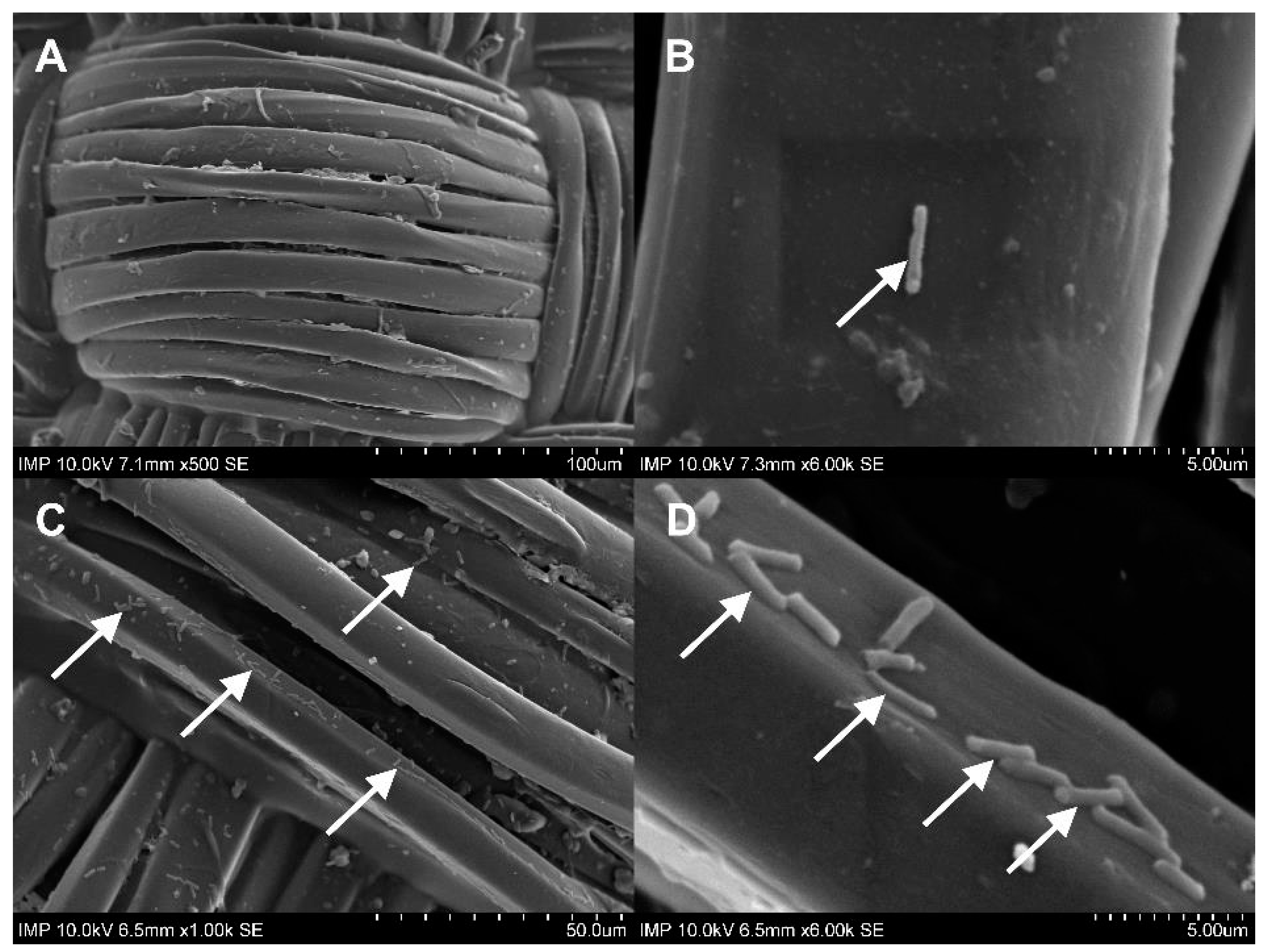
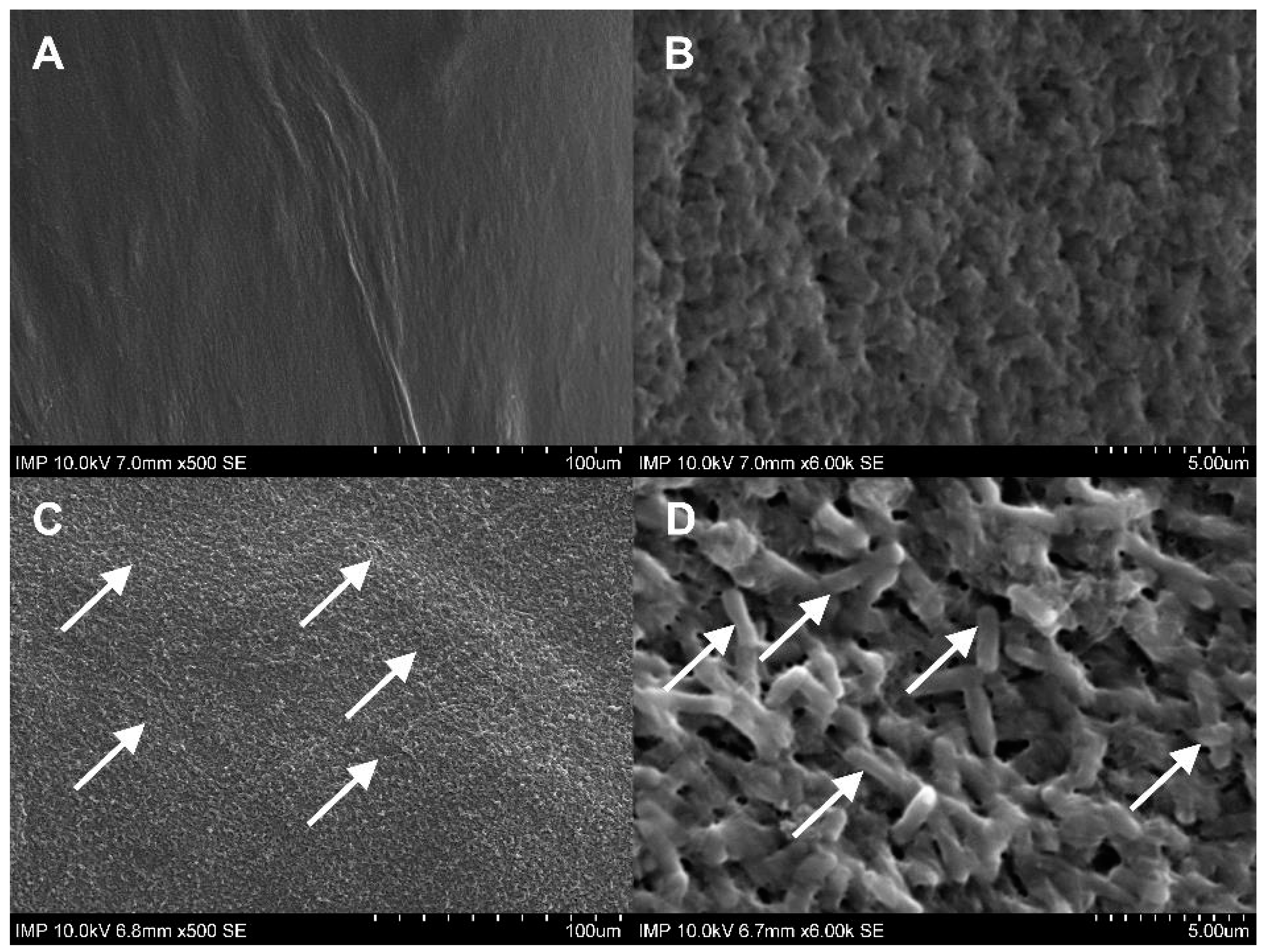
2.1. Surface Coating of the Grafts
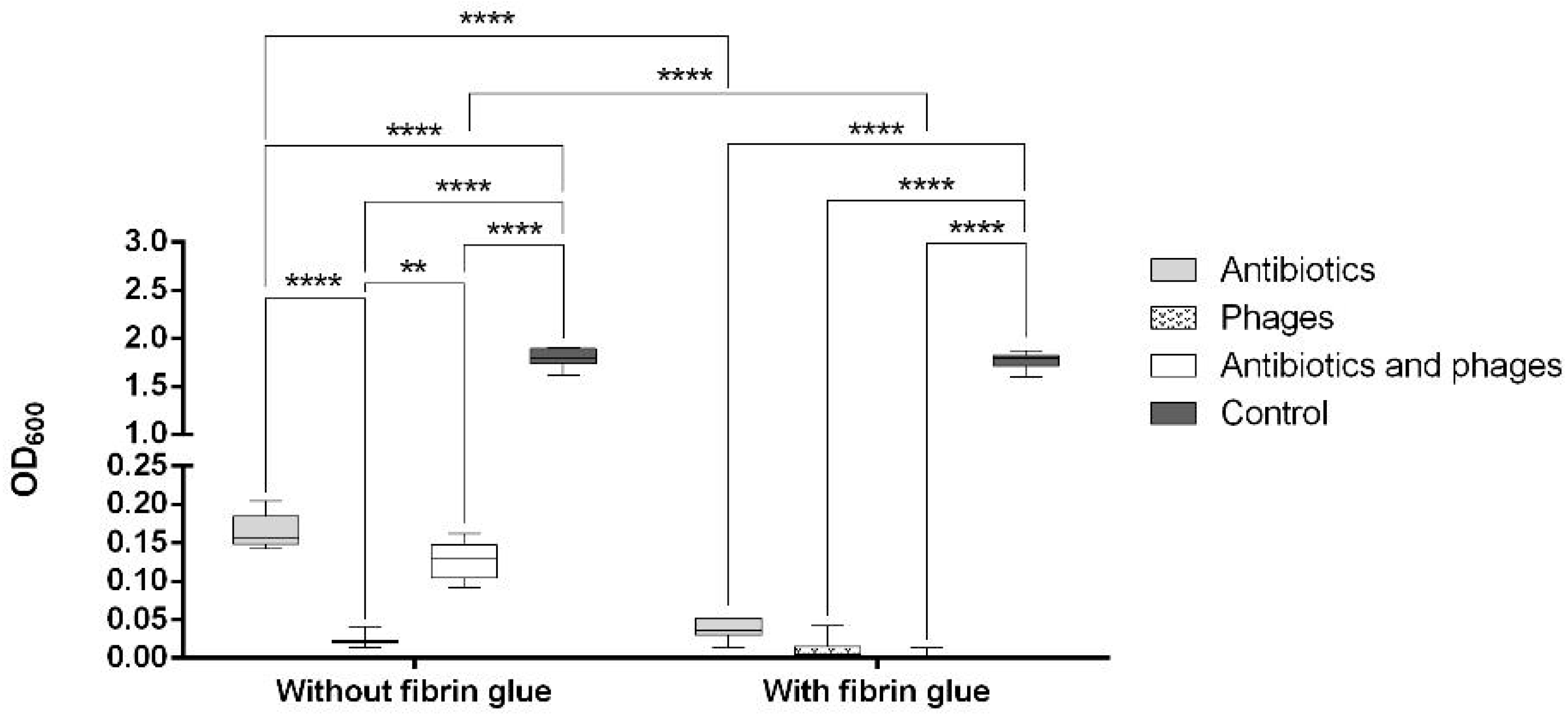
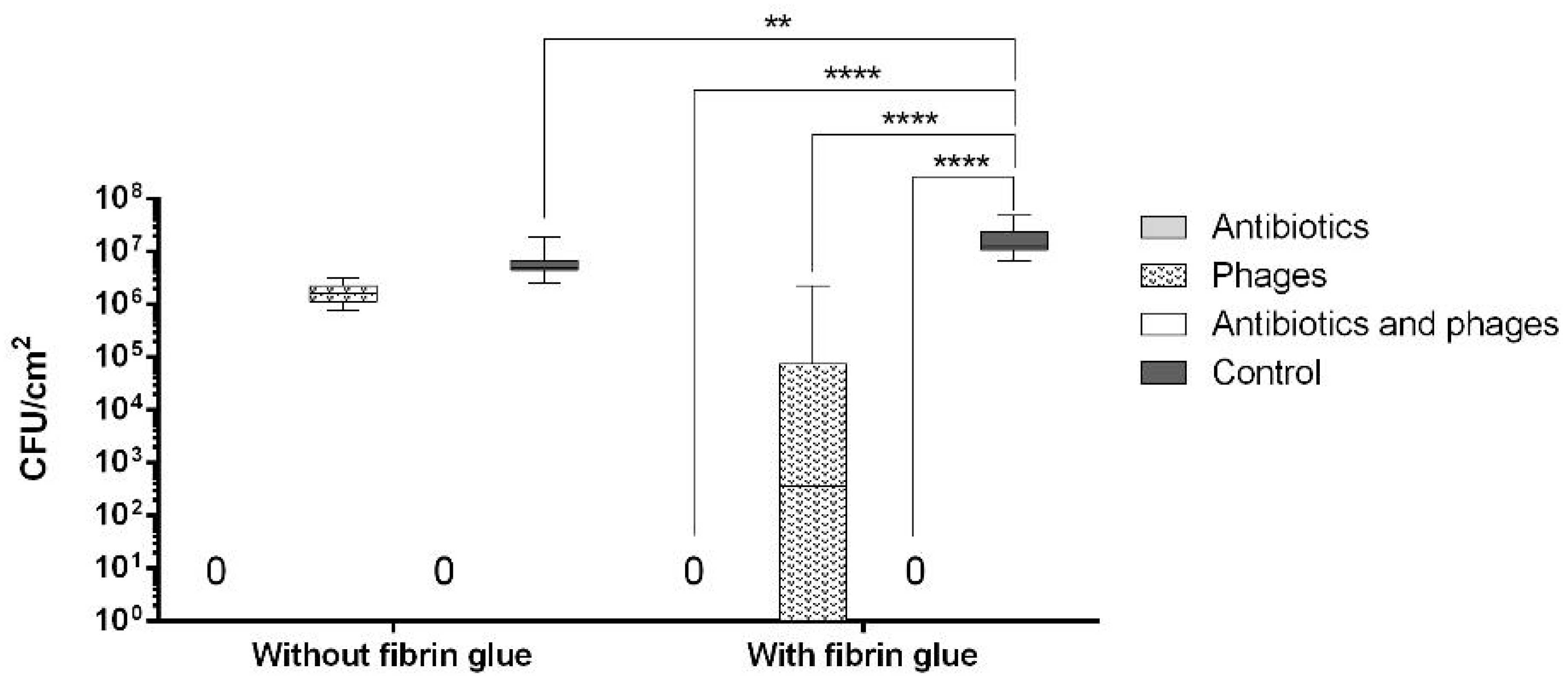
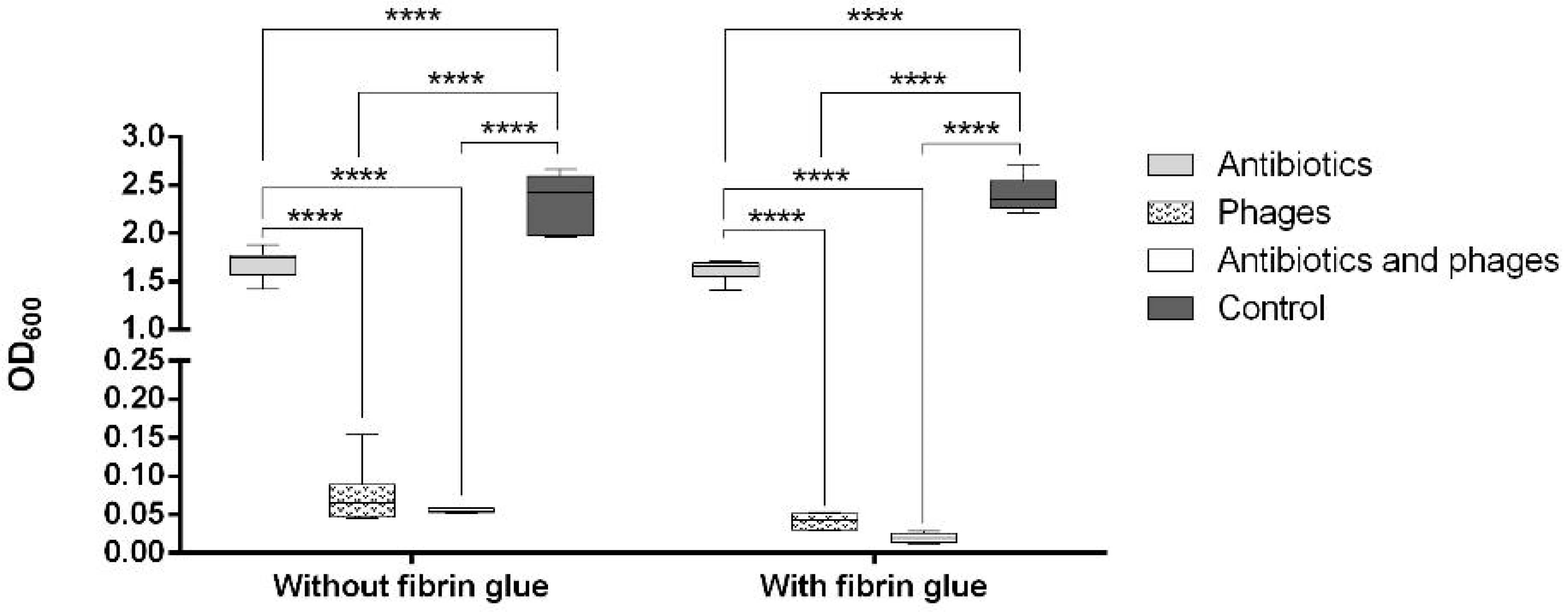
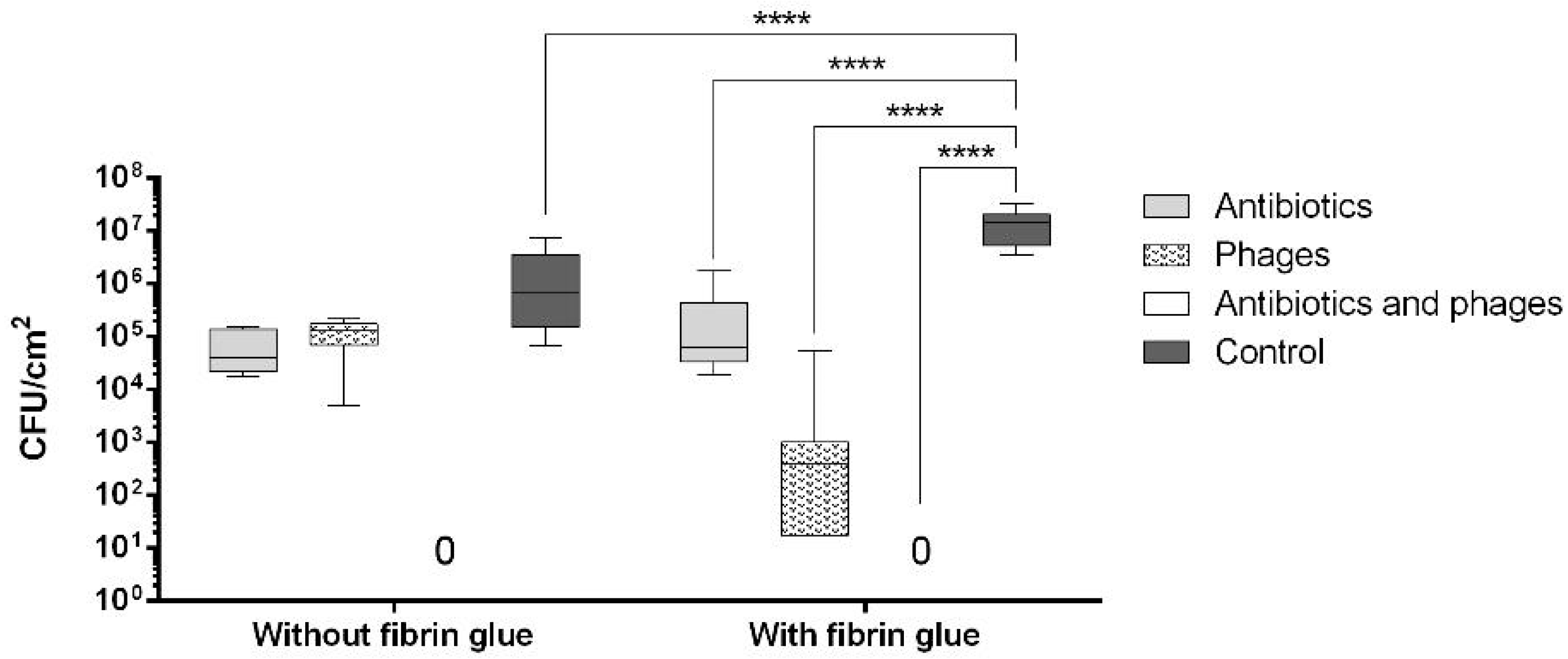
2.2. Antibacterial Loads of Graft Samples
2.2.1. Uncoated Grafts
2.2.2. Coated Grafts
2.3. Antibacterial Activity against Single Contamination
2.3.1. Activity against Staphylococcus aureus
2.3.2. Activity against Escherichia coli
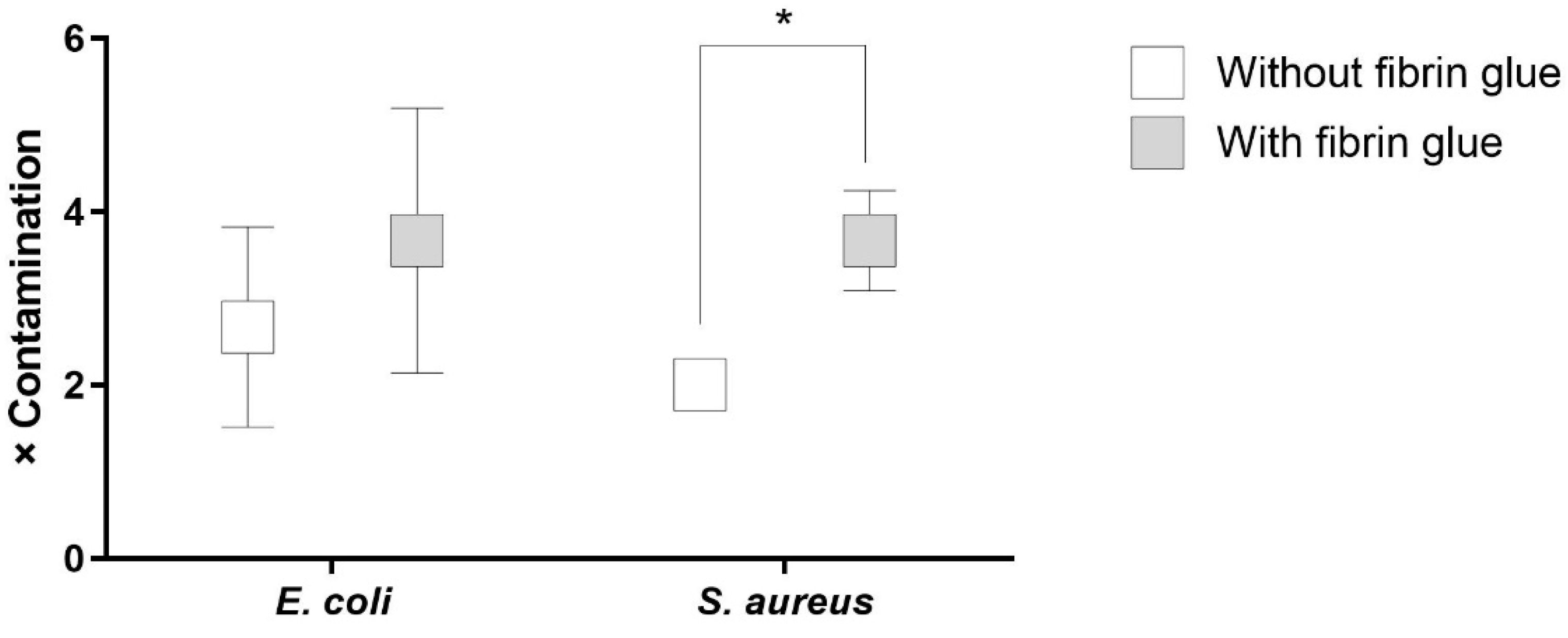
2.4. Antibacterial Activity against Recurrent Contamination
3. Discussion
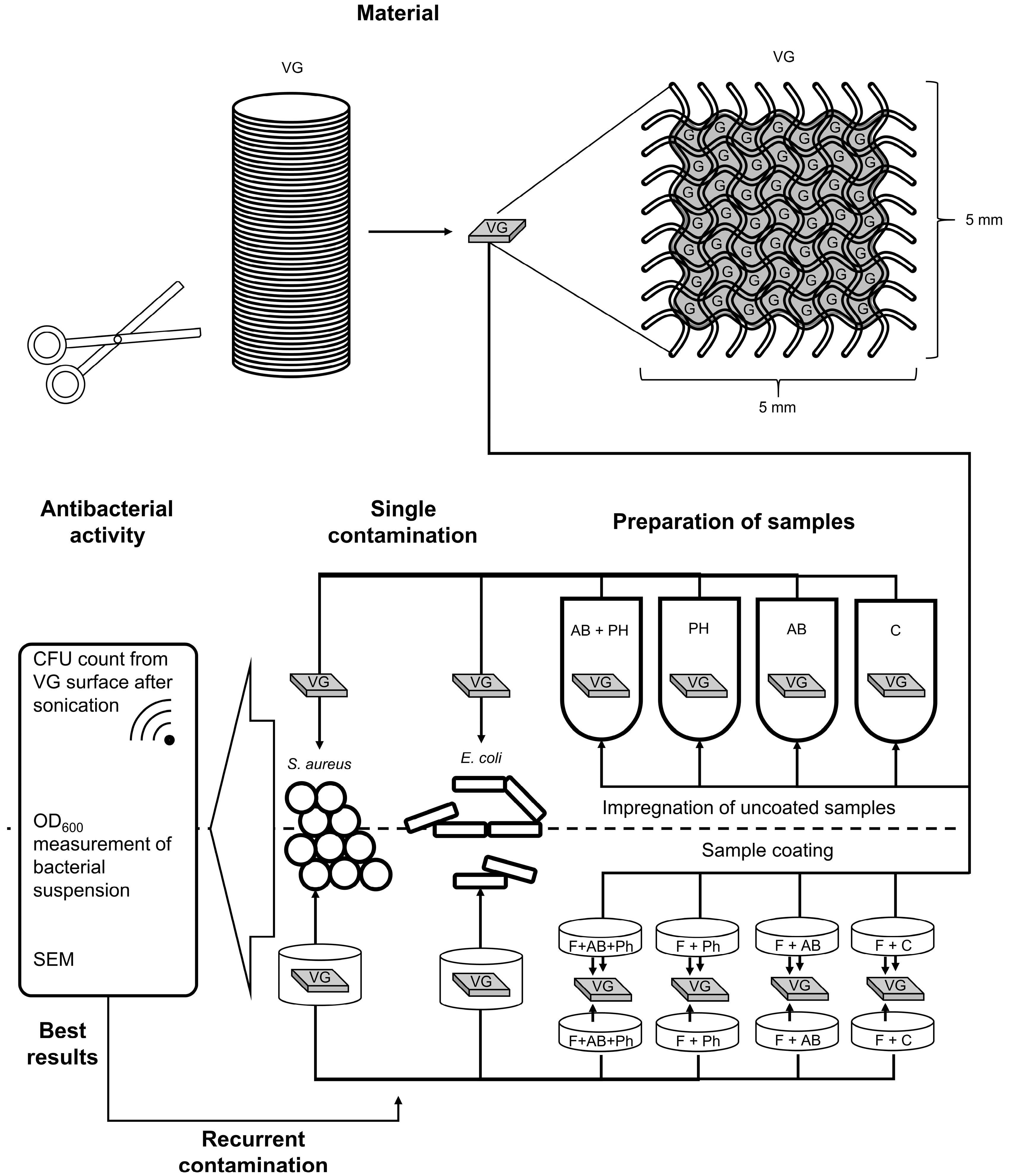
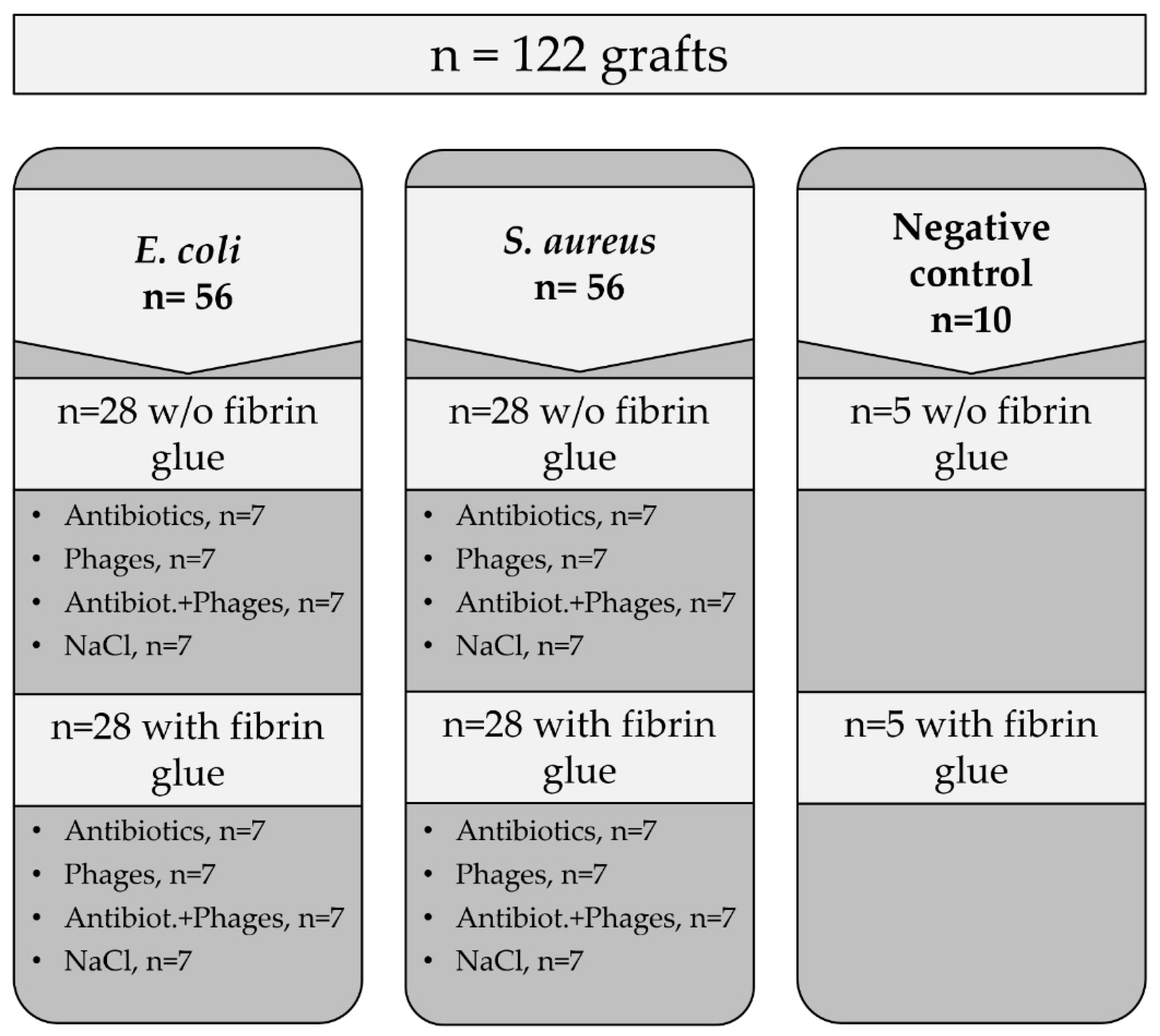
4. Materials and Methods
4.1. Materials
4.1.1. Antibiotic Agents
4.1.2. Bacterial Strains
4.1.3. Phage Strains
4.1.4. Vascular Graft
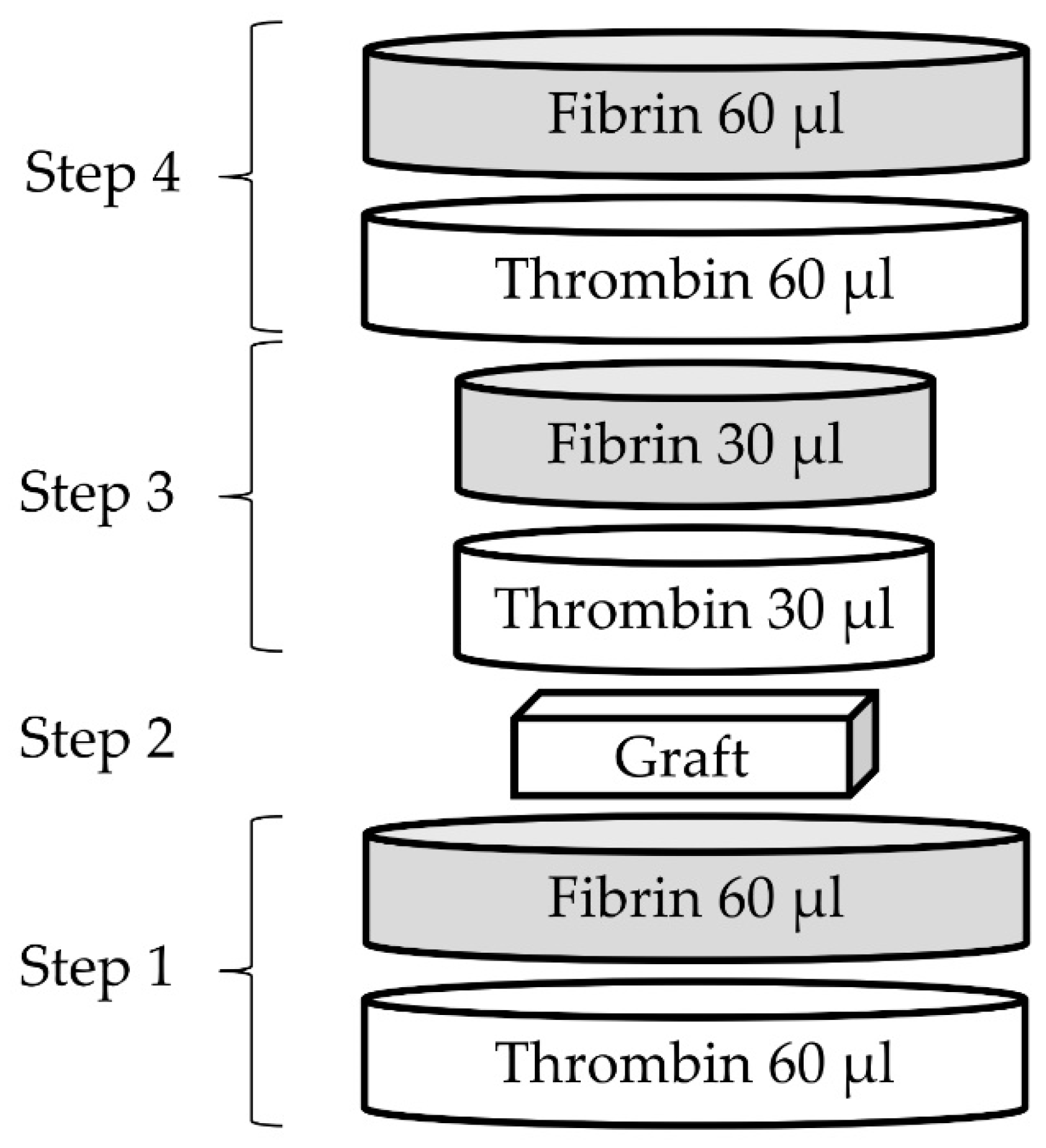
4.1.5. Fibrin Glue
4.2. Methods
4.2.1. Preparation of Working Antibacterial Solutions
4.2.2. Impregnation of Uncoated Samples
4.2.3. Preparation of Coated Samples
4.2.4. Processing of Samples—Antibacterial Activity against Single Contamination
4.2.5. Scanning Electron Microscopy
4.2.6. Processing of Samples—Antibacterial Activity against Recurrent Contamination
4.2.7. Sterility Test
4.2.8. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kuehn, C.; Graf, K.; Mashaqi, B.; Pichlmaier, M.A.; Heuer, W.; Hilfiker, A.; Stiesch, M.; Chaberny, I.; Haverich, A. Prevention of early vascular graft infection using regional antibiotic release. J. Surg. Res. 2010, 164, e185–e191. [Google Scholar] [CrossRef] [PubMed]
- Ruemke, S.; Rubalskii, E.; Mashaqi, B.; Burgwitz, K.; Haverich, A.; Salmoukas, C.; Kuehn, C. Evaluation of Gram-positive and Gram-negative bacterial adherence on four different vascular prosthetic grafts in vitro. Austin J. Surg. 2019, 6, 1200. [Google Scholar]
- Boot, W.; Schmid, T.; D’Este, M.; Guillaume, O.; Foster, A.; Decosterd, L.; Richards, R.G.; Eglin, D.; Zeiter, S.; Moriarty, T.F. A hyaluronic acid hydrogel loaded with gentamicin and vancomycin successfully eradicates chronic methicillin-resistant Staphylococcus aureus orthopedic infection in a sheep model. Antimicrob. Agents Chemother. 2021, 65, e01840-20. [Google Scholar] [CrossRef]
- Tello-Díaz, C.; Palau, M.; Muñoz, E.; Gomis, X.; Gavaldà, J.; Fernández-Hidalgo, N.; Bellmunt-Montoya, S. Methicillin-susceptible Staphylococcus aureus biofilm formation on vascular grafts: An in vitro study. Microbiol Spectr. 2023, 11, e0393122. [Google Scholar] [CrossRef] [PubMed]
- Ayrapetyan, M.; Williams, T.; Oliver, J.D. Relationship between the viable but nonculturable state and antibiotic persister cells. J. Bacteriol. 2018, 200, e00249-18. [Google Scholar] [CrossRef]
- Kutter, E.; Sulakvelidze, A. (Eds.) Bacteriophages: Biology and Applications; CRC Press: Boca Raton, FL, USA, 2005; p. 510. ISBN 0-8493-1336-8. [Google Scholar]
- Rubalskii, E.; Ruemke, S.; Salmoukas, C.; Boyle, E.C.; Warnecke, G.; Tudorache, I.; Shrestha, M.; Schmitto, J.D.; Martens, A.; Rojas, S.V.; et al. Bacteriophage therapy for critical infections related to cardiothoracic surgery. Antibiotics 2020, 9, 232. [Google Scholar] [CrossRef]
- Willy, C.; Bugert, J.J.; Classen, A.Y.; Deng, L.; Düchting, A.; Gross, J.; Hammerl, J.A.; Korf, I.H.E.; Kühn, C.; Lieberknecht-Jouy, S.; et al. Phage therapy in Germany-update 2023. Viruses 2023, 15, 588. [Google Scholar] [CrossRef]
- Hampton, H.G.; Watson, B.N.J.; Fineran, P.C. The arms race between bacteria and their phage foes. Nature 2020, 577, 327–336. [Google Scholar] [CrossRef]
- Heilmann, S.; Sneppen, K.; Krishna, S. Coexistence of phage and bacteria on the boundary of self-organized refuges. Proc. Natl. Acad. Sci. USA 2012, 109, 12828–12833. [Google Scholar] [CrossRef] [PubMed]
- Comeau, A.M.; Tétart, F.; Trojet, S.N.; Prère, M.F.; Krisch, H.M. Phage-Antibiotic Synergy (PAS): Beta-lactam and quinolone antibiotics stimulate virulent phage growth. PLoS ONE 2007, 2, e799. [Google Scholar] [CrossRef] [PubMed]
- Tagliaferri, T.L.; Jansen, M.; Horz, H.P. Fighting pathogenic bacteria on two fronts: Phages and antibiotics as combined strategy. Front. Cell. Infect. Microbiol. 2019, 9, 22. [Google Scholar] [CrossRef] [PubMed]
- Nakaminami, H.; Suzuki, Y.; Suzuki, R.; Saito, A.; Motomura, N.; Noguchi, N. In vitro antimicrobial activity of fibrin sealants containing antimicrobial agents. Surg. Infect. 2014, 15, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Mashaqi, B.; Marsch, G.; Shrestha, M.; Graf, K.; Stiesch, M.; Chaberny, I.F.; Haverich, A.; Kuehn, C. Antibiotic pretreatment of heart valve prostheses to prevent early prosthetic valve endocarditis. J. Heart Valve Dis. 2011, 20, 582–586. [Google Scholar]
- Rubalskii, E.; Ruemke, S.; Salmoukas, C.; Aleshkin, A.; Bochkareva, S.; Modin, E.; Mashaqi, B.; Boyle, E.C.; Boethig, D.; Rubalsky, M.; et al. Fibrin glue as a local drug-delivery system for bacteriophage PA5. Sci. Rep. 2019, 9, 2091. [Google Scholar] [CrossRef]
- Darouiche, R.O. Treatment of infections associated with surgical implants. New Engl. J. Med. 2004, 350, 1422–1429. [Google Scholar] [CrossRef]
- Wilson, W.R.; Bower, T.C.; Creager, M.A.; Amin-Hanjani, S.; O’Gara, P.T.; Lockhart, P.B.; Darouiche, R.O.; Ramlawi, B.; Derdeyn, C.P.; Bolger, A.F.; et al. American Heart Association Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease of the Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Surgery and Anesthesia; Council on Peripheral Vascular Disease; and Stroke Council. Vascular Graft Infections, Mycotic Aneurysms, and Endovascular Infections: A Scientific Statement From the American Heart Association. Circulation 2016, 134, e412–e460. [Google Scholar]
- Aleshkin, A.V.; Volozhantsev, N.V.; Svetoch, E.A.; Kiseleva, I.A.; Rubal’sky, E.O.; Afanas’ev, S.S.; Borzilov, A.I.; Zatevalov, A.M.; Vasil’ev, D.A.; Zolotukhin, S.N.; et al. Bacteriophages as probiotics: Phage-based probiotic dietary supplement in prophylaxis against foodborne infections. Infect. Dis. Infekt. Bolezn. 2016, 14, 31–40. [Google Scholar] [CrossRef]
- Aleshkin, A.V.; Rubalskii, E.O.; Volozhantsev, N.V.; Verevkin, V.V.; Svetoch, E.A.; Kiseleva, I.A.; Bochkareva, S.S.; Borisova, O.Y.; Popova, A.V.; Bogun, A.G.; et al. A small-scale experiment of using phage-based probiotic dietary supplement for prevention of E. coli traveler’s diarrhea. Bacteriophage 2015, 5, e1074329. [Google Scholar] [CrossRef]
- Schweizer, T.A.; Shambat, S.M.; Haunreiter, V.D.; Mestres, C.A.; Weber, A.; Maisano, F.; Zinkernagel, A.S.; Hasse, B. Polyester Vascular Graft Material and Risk for Intracavitary Thoracic Vascular Graft Infection. Emerg. Infect. Dis. 2020, 26, 2448–2452. [Google Scholar] [CrossRef]
- Pointner, R.; Kofler, J.; Offer, C.; Schwab, G. The kinetics of antibiotic release from a fibrin-clotting system: An animal experiment. In Fibrin Sealant in Operative Medicine; : Schlag, G., Redl, H., Eds.; Springer: Berlin, Heidelberg, 1986; pp. 194–198. [Google Scholar]
- Chan, B.K.; Turner, P.E.; Kim, S.; Mojibian, H.R.; Elefteriades, J.A.; Narayan, D. Phage treatment of an aortic graft infected with Pseudomonas aeruginosa. Evol. Med. Public Health. 2018, 2018, 60–66. [Google Scholar] [CrossRef]
- Junghans, S.; Rojas, S.V.; Skusa, R.; Püschel, A.; Grambow, E.; Kohlen, J.; Warnke, P.; Gummert, J.; Gross, J. Bacteriophages for the Treatment of Graft Infections in Cardiovascular Medicine. Antibiotics 2021, 10, 1446. [Google Scholar] [CrossRef]
- Grambow, E.; Junghans, S.; Kröger, J.C.; Reisinger, E.C.; Krause, B.J.; Groß, J. Treatment of an Infected TEVAR with Extra- and Endovascular Bacteriophage Application. EJVES Vasc. Forum. 2022, 56, 20–23. [Google Scholar] [CrossRef] [PubMed]
- Kebriaei, R.; Lev, K.L.; Shah, R.M.; Stamper, K.C.; Holger, D.J.; Morrisette, T.; Kunz Coyne, A.J.; Lehman, S.M.; Rybak, M.J. Eradication of biofilm-mediated methicillin-resistant Staphylococcus aureus infections in vitro: Bacteriophage-antibiotic combination. Microbiol. Spectr. 2022, 10, e0041122. [Google Scholar] [CrossRef]
- Lev, K.; Kunz Coyne, A.J.; Kebriaei, R.; Morrisette, T.; Stamper, K.; Holger, D.J.; Canfield, G.S.; Duerkop, B.A.; Arias, C.A.; Rybak, M.J. Evaluation of bacteriophage-antibiotic combination therapy for biofilm-embedded MDR Enterococcus faecium. Antibiotics 2022, 11, 392. [Google Scholar] [CrossRef]
- Manohar, P.; Madurantakam Royam, M.; Loh, B.; Bozdogan, B.; Nachimuthu, R.; Leptihn, S. Synergistic effects of phage-antibiotic combinations against Citrobacter amalonaticus. ACS Infect. Dis. 2022, 8, 59–65. [Google Scholar] [CrossRef]
- Landa, K.J.; Mossman, L.M.; Whitaker, R.J.; Rapti, Z.; Clifton, S.M. Phage-antibiotic synergy inhibited by temperate and chronic virus competition. Bull Math Biol. 2022, 84, 54. [Google Scholar] [CrossRef]
- Valente, L.G.; Federer, L.; Iten, M.; Grandgirard, D.; Leib, S.L.; Jakob, S.M.; Haenggi, M.; Cameron, D.R.; Que, Y.A.; Prazak, J. Searching for synergy: Combining systemic daptomycin treatment with localised phage therapy for the treatment of experimental pneumonia due to MRSA. BMC Res. Notes. 2021, 14, 381. [Google Scholar] [CrossRef] [PubMed]
- Van Nieuwenhuyse, B.; Galant, C.; Brichard, B.; Docquier, P.L.; Djebara, S.; Pirnay, J.P.; Van der Linden, D.; Merabishvili, M.; Chatzis, O. A Case of in situ phage therapy against Staphylococcus aureus in a bone allograft polymicrobial biofilm infection: Outcomes and phage-antibiotic interactions. Viruses 2021, 13, 1898. [Google Scholar] [CrossRef] [PubMed]
- Abedon, S.T. Phage-antibiotic combination treatments: Antagonistic impacts of antibiotics on the pharmacodynamics of phage therapy? Antibiotics 2019, 8, 182. [Google Scholar] [CrossRef]
- Ma, D.; Li, L.; Han, K.; Wang, L.; Cao, Y.; Zhou, Y.; Chen, H.; Wang, X. The antagonistic interactions between a polyvalent phage SaP7 and β-lactam antibiotics on combined therapies. Vet. Microbiol. 2022, 266, 109332. [Google Scholar] [CrossRef]
- Danis-Wlodarczyk, K.M.; Cai, A.; Chen, A.; Gittrich, M.R.; Sullivan, M.B.; Wozniak, D.J.; Abedon, S.T. Friends or Foes? Rapid determination of dissimilar colistin and ciprofloxacin antagonism of Pseudomonas aeruginosa phages. Pharmaceuticals 2021, 14, 1162. [Google Scholar] [CrossRef]
- Zuo, P.; Yu, P.; Alvarez, P.J.J. Aminoglycosides antagonize bacteriophage proliferation, attenuating phage suppression of bacterial growth, biofilm formation, and antibiotic resistance. Appl. Environ. Microbiol. 2021, 87, e0046821. [Google Scholar] [CrossRef]
- Gu Liu, C.; Green, S.I.; Min, L.; Clark, J.R.; Salazar, K.C.; Terwilliger, A.L.; Kaplan, H.B.; Trautner, B.W.; Ramig, R.F.; Maresso, A.W. Phage-antibiotic synergy is driven by a unique combination of antibacterial mechanism of action and stoichiometry. mBio 2020, 11, e01462-20. [Google Scholar] [CrossRef]
- Davies, J.; Gorini, L.; Davis, B.D. Misreading of RNA codewords induced by aminoglycoside antibiotics. Mol. Pharmacol. 1965, 1, 93–106. [Google Scholar]
- Misumi, M.; Nishimura, T.; Komai, T.; Tanaka, N. Interaction of kanamycin and related antibiotics with the large subunit of ribosomes and the inhibition of translocation. Biochem. Biophys. Res. Commun. 1978, 84, 358–365. [Google Scholar] [CrossRef]
- Cabañas, M.J.; Vázquez, D.; Modolell, J. Inhibition of ribosomal translocation by aminoglycoside antibiotics. Biochem. Biophys. Res. Commun. 1978, 83, 991–997. [Google Scholar] [CrossRef] [PubMed]
- Hirokawa, G.; Kiel, M.C.; Muto, A.; Selmer, M.; Raj, V.S.; Liljas, A.; Igarashi, K.; Kaji, H.; Kaji, A. Post-termination complex disassembly by ribosome recycling factor, a functional tRNA mimic. EMBO J. 2002, 21, 2272–2281. [Google Scholar] [CrossRef] [PubMed]
- Borovinskaya, M.; Pai, R.; Zhang, W.; Schuwirth, B.S.; Holton, J.M.; Hirokawa, G.; Kaji, H.; Kaji, A.; Cate, J.H. Structural basis for aminoglycoside inhibition of bacterial ribosome recycling. Nat. Struct. Mol. Biol. 2007, 14, 727–732. [Google Scholar] [CrossRef] [PubMed]
- Kever, L.; Hardy, A.; Luthe, T.; Hünnefeld, M.; Gätgens, C.; Milke, L.; Wiechert, J.; Wittmann, J.; Moraru, C.; Marienhagen, J.; et al. Aminoglycoside antibiotics inhibit phage infection by blocking an early step of the infection cycle. mBio 2022, 4, e0078322. [Google Scholar] [CrossRef]
- Kirby, A.E. Synergistic action of gentamicin and bacteriophage in a continuous culture population of Staphylococcus aureus. PLoS ONE 2012, 7, e51017. [Google Scholar] [CrossRef]
- Ali, H.M.H.; Abd, A.K.H.; Abdulameer, A.S.; Taha, R.N. Efficacy of bacteriophage–antibiotic combinations against Staphylococcus aureus infections: In vitro study. Int. J. Pharm. Sci. Rev. Res. 2015, 30, 186–189. [Google Scholar]
- Głowacka-Rutkowska, A.; Gozdek, A.; Empel, J.; Gawor, J.; Żuchniewicz, K.; Kozińska, A.; Dębski, J.; Gromadka, R.; Łobocka, M. The ability of lytic staphylococcal podovirus vB_SauP_phiAGO1.3 to coexist in equilibrium with its host facilitates the selection of host mutants of attenuated virulence but does not preclude the phage antistaphylococcal activity in a nematode infection model. Front. Microbiol. 2019, 9, 3227. [Google Scholar] [PubMed]
- McCallin, S.; Menzi, C.; Lassen, S.; Daraspe, J.; Oechslin, F.; Moreillon, P. Antibiotic exposure leads to reduced phage susceptibility in vancomycin intermediate Staphylococcus aureus (VISA). Antimicrob. Agents Chemother. 2022, e0224721. [Google Scholar] [CrossRef] [PubMed]
- Ramalhete, R.; Brown, R.; Blunn, G.; Skinner, J.; Coathup, M.; Graney, I.; Sanghani-Kerai, A. A novel antimicrobial coating to prevent periprosthetic joint infection. Bone Joint. Res. 2020, 9, 848–856. [Google Scholar] [CrossRef] [PubMed]
- Hyman, P.; Abedon, S.T. Bacteriophage host range and bacterial resistance. Adv. Appl. Microbiol. 2010, 70, 217–248. [Google Scholar] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ruemke, S.; Rubalskii, E.; Salmoukas, C.; Hermes, K.; Natanov, R.; Kaufeld, T.; Gryshkov, O.; Mutsenko, V.; Rubalsky, M.; Burgwitz, K.; et al. Combination of Bacteriophages and Antibiotics for Prevention of Vascular Graft Infections—An In Vitro Study. Pharmaceuticals 2023, 16, 744. https://doi.org/10.3390/ph16050744
Ruemke S, Rubalskii E, Salmoukas C, Hermes K, Natanov R, Kaufeld T, Gryshkov O, Mutsenko V, Rubalsky M, Burgwitz K, et al. Combination of Bacteriophages and Antibiotics for Prevention of Vascular Graft Infections—An In Vitro Study. Pharmaceuticals. 2023; 16(5):744. https://doi.org/10.3390/ph16050744
Chicago/Turabian StyleRuemke, Stefan, Evgenii Rubalskii, Christina Salmoukas, Kristina Hermes, Ruslan Natanov, Tim Kaufeld, Oleksandr Gryshkov, Vitalii Mutsenko, Maxim Rubalsky, Karin Burgwitz, and et al. 2023. "Combination of Bacteriophages and Antibiotics for Prevention of Vascular Graft Infections—An In Vitro Study" Pharmaceuticals 16, no. 5: 744. https://doi.org/10.3390/ph16050744




