Abstract
Medication therapy management by pharmaceutical care (MTM-PC) has been shown to improve the effectiveness of antihypertensive treatments. The aim was to answer the question: what are the MTM-PC models and their impact on hypertensive patients’ outcomes? This is a systematic review with meta-analysis. The search strategies were run on 27 September 2022 in the following databases: PubMed, EMBASE, Scopus, LILACs, Central Cochrane Library, Web of Science; and International Pharmaceutical Abstracts. The quality and bias risk was assessed by the Downs and Black instrument. Forty-one studies met the eligibility criteria and were included, Kappa = 0.86; 95% CI, 0.66–1.0; (p < 0.001). Twenty-seven studies (65.9%) had MTM-PC models outlined by the clinical team, showing as characteristics the mean of 10.0 ± 10.7 months of follow-up of hypertensive patients, with 7.7 ± 4.9 consultations. Instruments to assess the quality of life measured the enhancement by 13.4 ± 10.7% (p = 0.047). The findings of the meta-analysis show a mean reduction of −7.71 (95% CI, −10.93 to −4.48) and −3.66 (95% CI, −5.51 to −1.80), (p < 0.001) in mmHg systolic and diastolic pressures, respectively. Cardiovascular relative risk (RR) over ten years was 0.561 (95% CI, 0.422 to 0.742) and RR = 0.570 (95% CI, 0.431 to 0.750), considering homogeneous studies, I² = 0%. This study shows the prevalence of MTM-PC models outlined by the clinical team, in which there are differences according to the models in reducing blood pressure and cardiovascular risk over ten years with the improvement in quality of life.
1. Introduction
About 67% of deaths in the world (38 million) occur due to non-communicable chronic diseases (NCDs). A World Health Organization (WHO) projection presents the number of NCD deaths increasing each year, with an increase of three million more deaths every four years [1,2]. Among the NCDs, cardiovascular diseases (CVDs) stand out, which are responsible for 17.9 million annual deaths worldwide. Systemic arterial hypertension is of great importance among CVDs, as it is highly prevalent in the world population and can be considered an aggravating factor for other CVDs [3,4].
Hypertension affects approximately 45–67% of elderly individuals and 2–12% of children and adolescents worldwide. The prevalence in adult individuals is estimated at approximately 19–42.5% in emerging countries. Its severity is related to the impairment of target organs, such as kidneys, heart, and brain [1,3,5]. According to the WHO, hypertension is considered the main risk factor for the occurrence of other diseases of the circulatory system [2], as it is known that an increase of 10 mmHg in systolic blood pressure is capable of increasing by 25% the risk of developing CVDs, representing a risk association equal to 1.2 in observational studies [6,7].
Health technologies characterized as services capable of managing treatment preventively become contributory to the management of hypertensive patients with the promise of producing results of better effectiveness in blood pressure control and cardiovascular risk reduction [8,9]. Pharmaceutical care (PC) is a model of professional practice that constitutes a set of actions and services performed by the pharmaceutical professional, which considers the biopsychosocial sphere of the individual, family, and community, working along with the health team, focusing on the prevention and resolution of problems of health, further to the promotion, protection, damage prevention, and recovery of health, including not only the clinical assistance dimension but also the technical pedagogical dimension of health work. In this model of practice, the pharmacist assumes responsibility for managing people’s healthcare, which must be shared with the health team and the actions agreed upon with the patient/family [10,11,12].
PC works on adherence to medication, lifestyle changes, dietary sodium restriction, moderation of alcohol consumption, a balanced diet, weight reduction, regular physical activity, and smoking cessation, which are important changeable factors in the management of hypertension. In this way, PC develops a service capable of modifying those factors and providing care that improves the effectiveness and safety of the treatment—medication therapy management (MTM). Thus, MTM-PC is a health technology that is very important in enabling the aid of hypertension management regarding classic treatment with calcium channel blockers (CCB), angiotensin converting enzyme inhibitors (ACE inhibitors or ACE-I), angiotensin receptor blockers (ARBs), and diuretics, and is also related to treatment with new drugs [9,10].
The PC results related to MTM show that there is a positive clinical impact on the reduction in blood pressure and cardiovascular risk, but the impact of different models, as well as their results regarding the scenario in which it is inserted, are unknown in the literature [13,14]. Furthermore, in health management and planning, decision-making based on the highest possible degree of evidence is necessary [15,16,17]. Even if the PC produces good results for the treatment of hypertension, it is necessary to evaluate the existing MTM-PC models, their characteristics and the influence of the scenarios for their insertion in order to define a profile adjustable for each reality that generates results with greater precision, in order to incorporate this service as a feasible health technology for different realities of healthcare systems [8,18].
Decision-making processes in health are carried out either in a subjective way, which is more related to the previous conceptualizations of the decision maker and their subjectivity, or in a systematized way, which is more rational and is revealed to culminate in the most effective process. In the latter, it is essential to observe the sources of information as well as the origins of the results that will support decision-making [19]. The greater the robustness of the analysis on the source of information for decision-making, the greater the assertiveness of the decision. In addition, the highest degree of evidence must be considered. In view of the classifications of epidemiological studies, the satisfactory degree of evidence for assertive decision-making in health is at the top of Chiappelli’s pyramid, such as systematic review studies with meta-analysis. In this sense, a systematic review with meta-analysis and, mainly, meta-regression is capable of assigning better precision in the results to answer the review question and also to distinguish itself from other reviews. There are some reviews on this theme, but they are poor at describing different services and models of MTM-PC, as well as summarizing the characteristics of those models compared to their results [15].
This study was reasoned on the hypothesis that PC is a health technology to be incorporated into health systems to improve effectiveness in reducing blood pressure and cardiovascular risk in hypertensive patients, and its effects may differ and be measured in different models of MTM. In this context, the aim of this study was to generate evidence for the treatment effect on blood pressure and cardiovascular risk from different models of MTM by PC for hypertensive patients in the context of primary healthcare.
2. Results
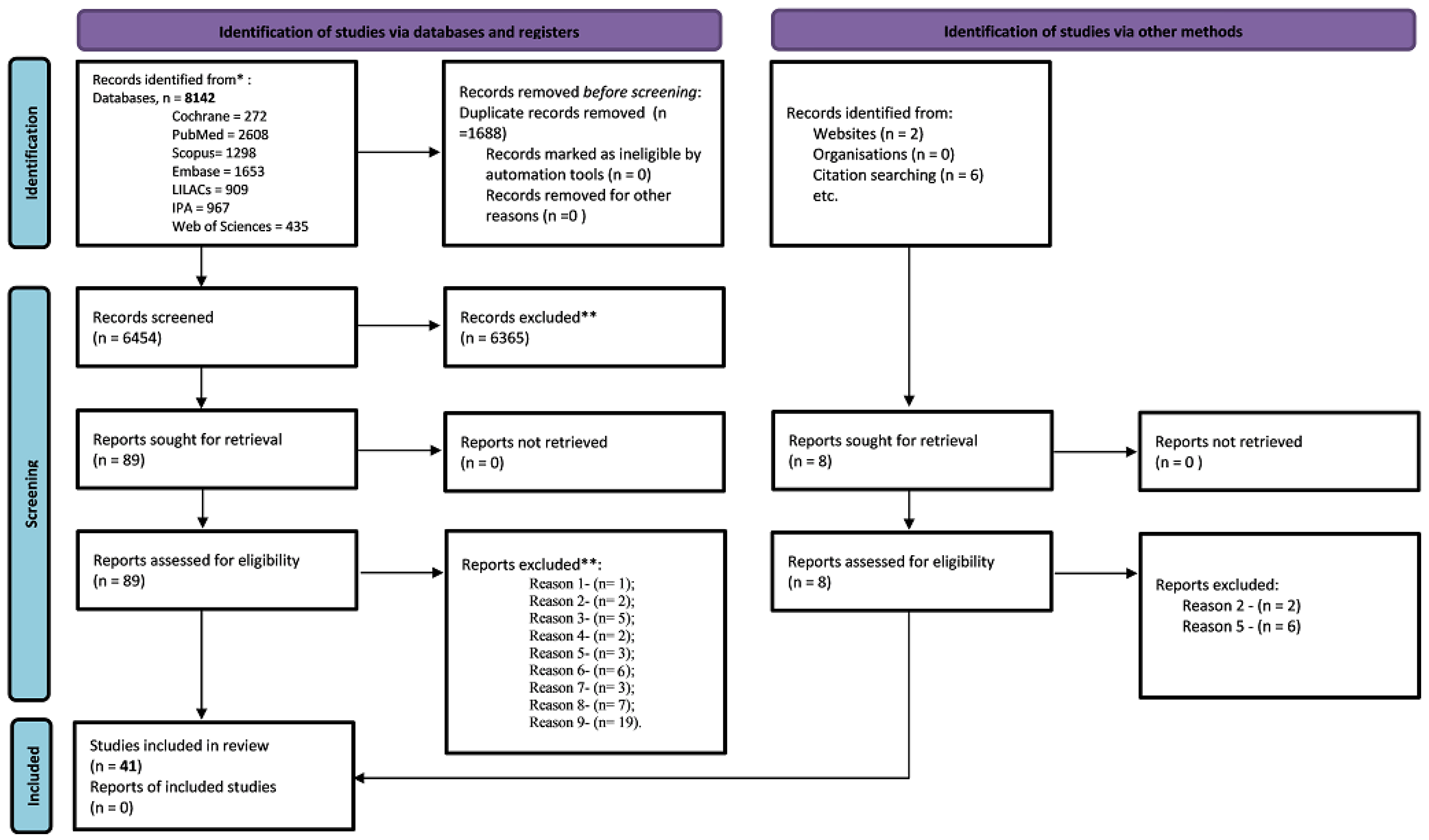
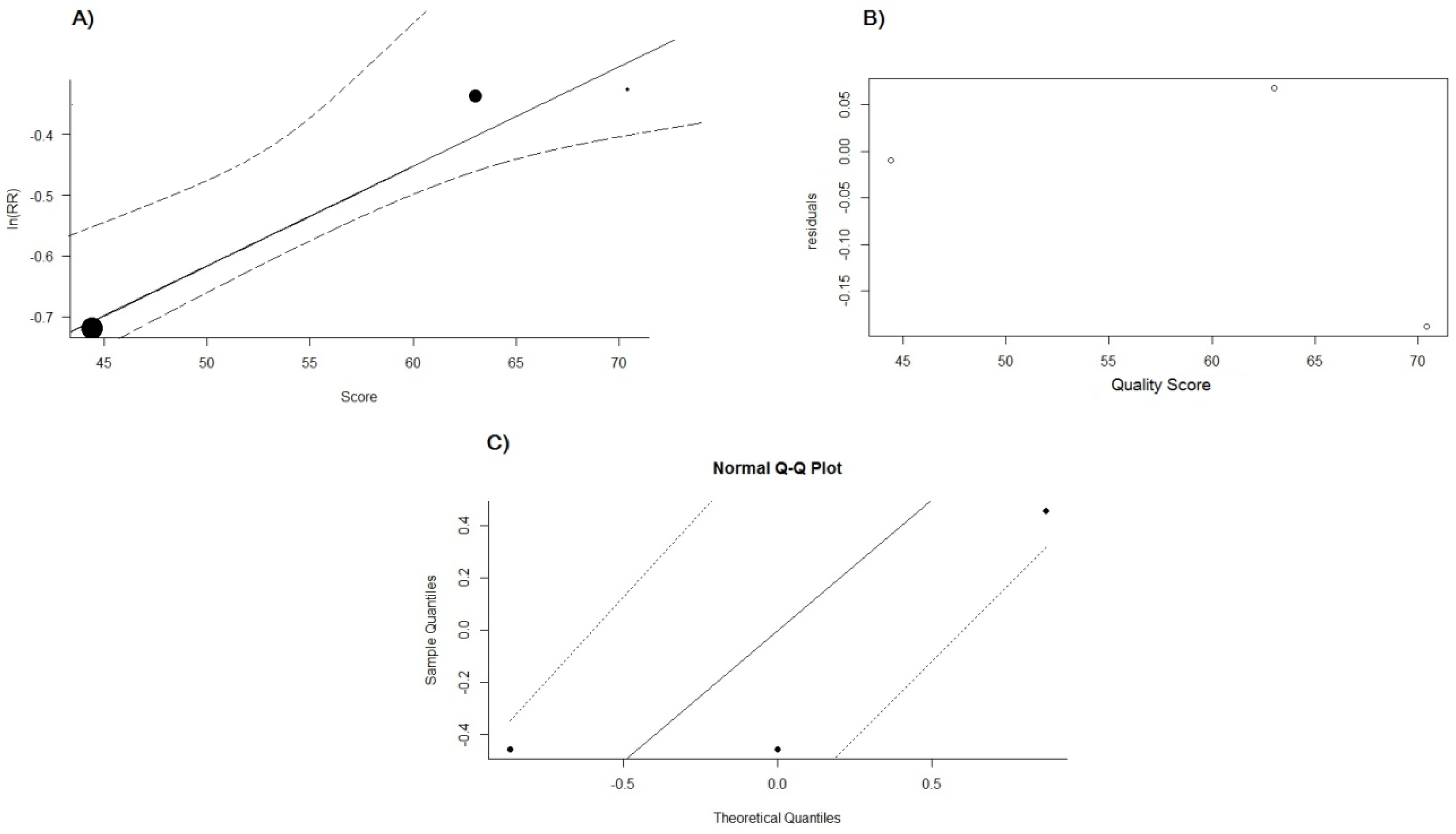
The initial search yielded 8142 records of which 89 articles underwent full-text evaluation, and 41 articles were selected and 48 were excluded (Table S1). Their selection was consistent with the researchers’ agreement [Kappa = 0.86; 95% CI, 0.66–1.0; (p < 0.001)]. It is noteworthy that in the search carried out in the grey literature, no study was found that met the inclusion criteria and mastery of the review after reading the full text (Figure 1).
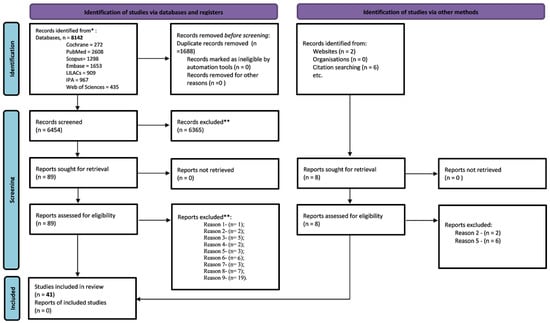
Figure 1.
Prisma flowchart for the search strategy and selection performed in the systematic review. Caption: * report of the number of records identified from each database or register searched; ** classification of exclusion for the studies: reason one—non-pharmaceutical interventions; reason two—evaluates the service and not outcomes; reason three—does not assess the outcomes of the review; reason four—the service is not suitable for review/intervention at a tertiary level; reason five—describes the results of the program; reason six—the methodology does not fit the review criteria; reason seven—there is not necessarily contact with the patient; reason eight—it is not necessarily a hypertensive patient; reason nine—clinical protocol, published abstract, case report, and review. Adapted from: Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. https://doi.org/10.1136/bmj.n71. For more information, available: http://www.prisma-statement.org/; accessed on 23 August 2022.
According to the 41 studies eligible for this systematic review, it was possible to report that the countries with more published studies within this theme are the USA with 17 (41.5%) and Brazil, 5 (12.2%). Among these studies, 25 (61.0%) are randomized controlled trials (RCTs); 3 (7.3%) are clinical trials without randomization; 10 (24.4%) represent clinical trials defined as quasi-experimental; 3 (7.3%) are observational studies; and 32 studies (78.1%) present sample calculation or at least report the number of patients eligible for the study. The mean duration of the studies is 18 ± 16.5 months and, 24 (58.5%), 9 (21.9%), and 15 (36.6%) studies feature randomization, blinding, and patient allocation concealment, respectively. The total number of patients in the intervention group is 4195 and in the control group 4978, with respective follow-up losses of 1338 and 913 (Table 1).

Table 1.
Identification and characteristics of the studies selected in the systematic review.
The quality of the studies was assessed and discriminated by the classification of Downs and Black [61]. The highest score achieved is 96.3 and the lowest is 22.2. The percentage of studies classified as having high evidence is 19.5% and with flawed evidence is 29.3% (Table 2).

Table 2.
Quality assessment of included studies in the systematic review.
In the qualitative evaluation of the MTM models from PC, it was possible to measure the mean of 10.0 ± 10.7 months of follow-up and a median of 6 months, with a minimum and maximum of 2–24 months. The mean of consultations is 7.7 ± 4.9 and the consultation time is 29.0 ± 8.0 min. The clinical scenario consists of 19 (44.2%) services developed in community pharmacies, 17 (39.5%) in healthcare facilities, and 7 (16.3%) in outpatient clinics. The most prevalent MTM models are those based on methods developed by the clinician themselves, an own model, 27 (65.9%); followed by the pharmacotherapy workup method 7 (17.1%); Dáder 5 (12.2%); and SOAP 1 (2.4%). Most MTM models have an educational/patient empowerment character, 34 (82.9%), and are structured with multidisciplinary support, even if it is just a pharmacist/physician, 26 (63.4%) (Table 3).

Table 3.
Evaluation of medication therapy management models by pharmaceutical care for hypertensive patients.
According to the total of 9173 patients, a profile could be defined whereby the mean age is 61.6 ± 6.6 and 61.9 ± 5.5 years for the intervention and control groups, respectively. In addition, there is a higher prevalence of male patients, with high education, and white skin color for both groups (Table 4).

Table 4.
Results of sociodemographic variables related to patients from studies included in the systematic review.
The number of patients with diabetes; smokers; and alcoholics is992 (30.6%) and 1236 (33.8%); 491 (21.2%) and 473 (22.1%); and 257 (19.5%) and 263 (21.7%) for the intervention and control/exposure groups, respectively. Most patients are level 1 and 2 obese, totaling 1740 (60.0%) in the intervention group, and 1424 (57.2%) in the control group. Among the previous history of diseases associated with hypertension, ischemic heart disease has the highest prevalence, with 227 (17.8%) and 255 (20.1%) patients for the intervention and control groups, respectively. It is noteworthy that out of the nine studies that evaluate the quality of life, 88% of them show that there was an improvement in the quality of life of hypertensive patients followed-up by the MTM-PC, which was measured by standard instruments to assess the quality of life. It is highlighted that the mean increase in the score of quality-of-life was 13.4 ± 10.7% (p = 0.047) (Table 5).

Table 5.
Clinical variables analysis comparing intervention and control/exposure groups from studies included in the systematic review.
The proportion of pressure control profile is 1673 (38.1%) and 2350 (63.3%) patients at the end of follow-up when compared the group with conventional care and the group with MTM by PC, respectively. The proportion of patients with total cholesterol, HDL, LDL, and triglycerides at satisfactory levels for both groups is 172 (32.7%) and 314 (59.6%) (p = 0.001); 200 (37.9%) and 206 (39.2%), (p = 0.650); 236 (44.9%) and 341 (64.8%), (p = 0.001); and 240 (45.5%) and 290 (55.0%), (p = 0.002), respectively (Table 5).
Regardless of the study design, there is a reduction in blood pressure when comparing the control/exposure and intervention groups. However, neither the study by Tobari et al. [59], a randomized clinical trial, or Erickson et al. [54], an observational study, have any evidence of improvement in blood pressure and the study by Robinson et al. [57], a non-randomized clinical trial, shows evidence of difference only for systolic pressure. Mean reductions in systolic (SBP) and diastolic blood pressure (DBP) are 6.8 and 3.7 for randomized clinical trials, 17.3 and 10.2 for non-randomized clinical trials, and 3.9 and 0.6 for observational studies, respectively (Table 6).

Table 6.
Evaluation of blood pressure values achieved from medication therapy management by pharmaceutical care for different types of studies.
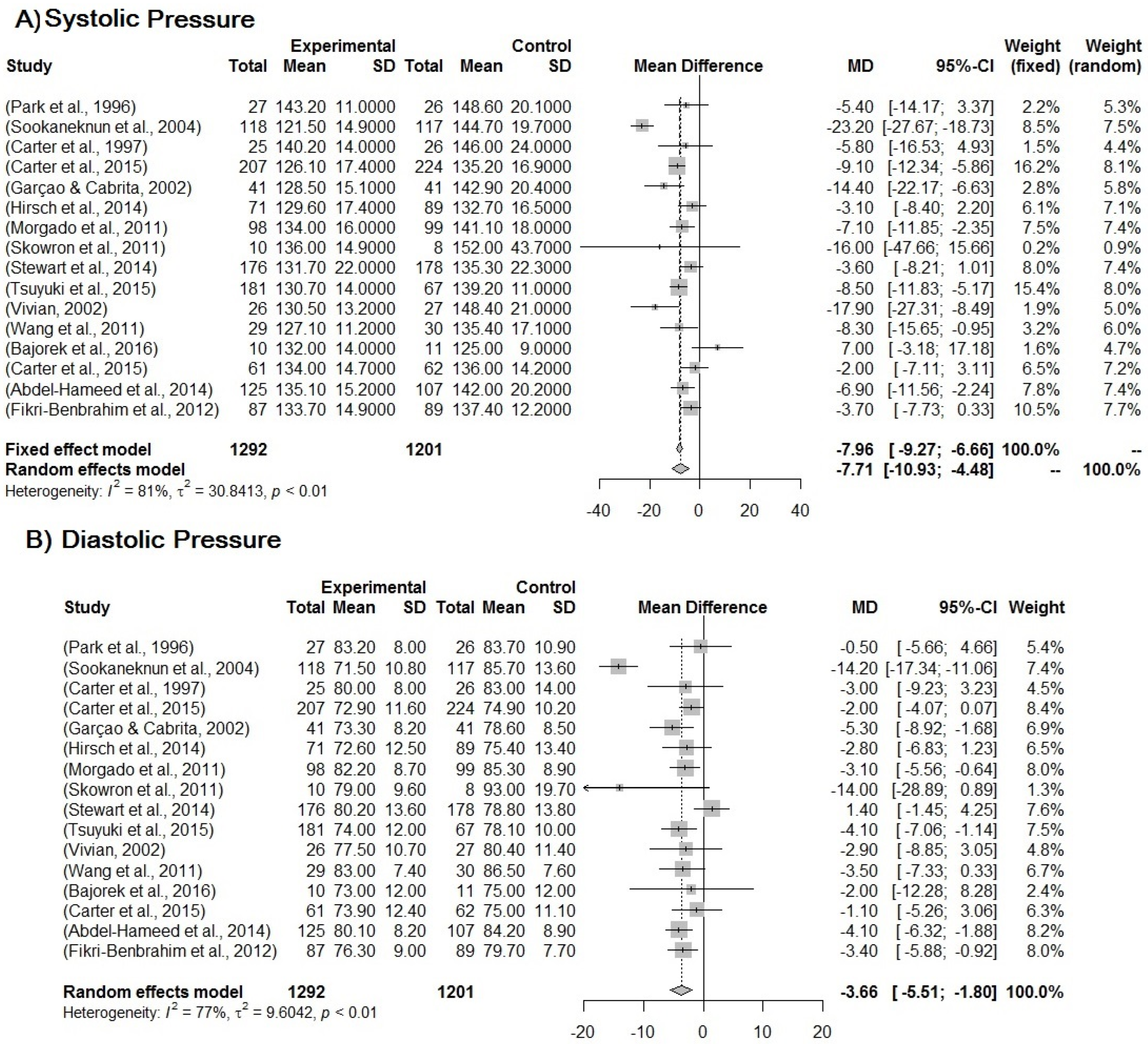
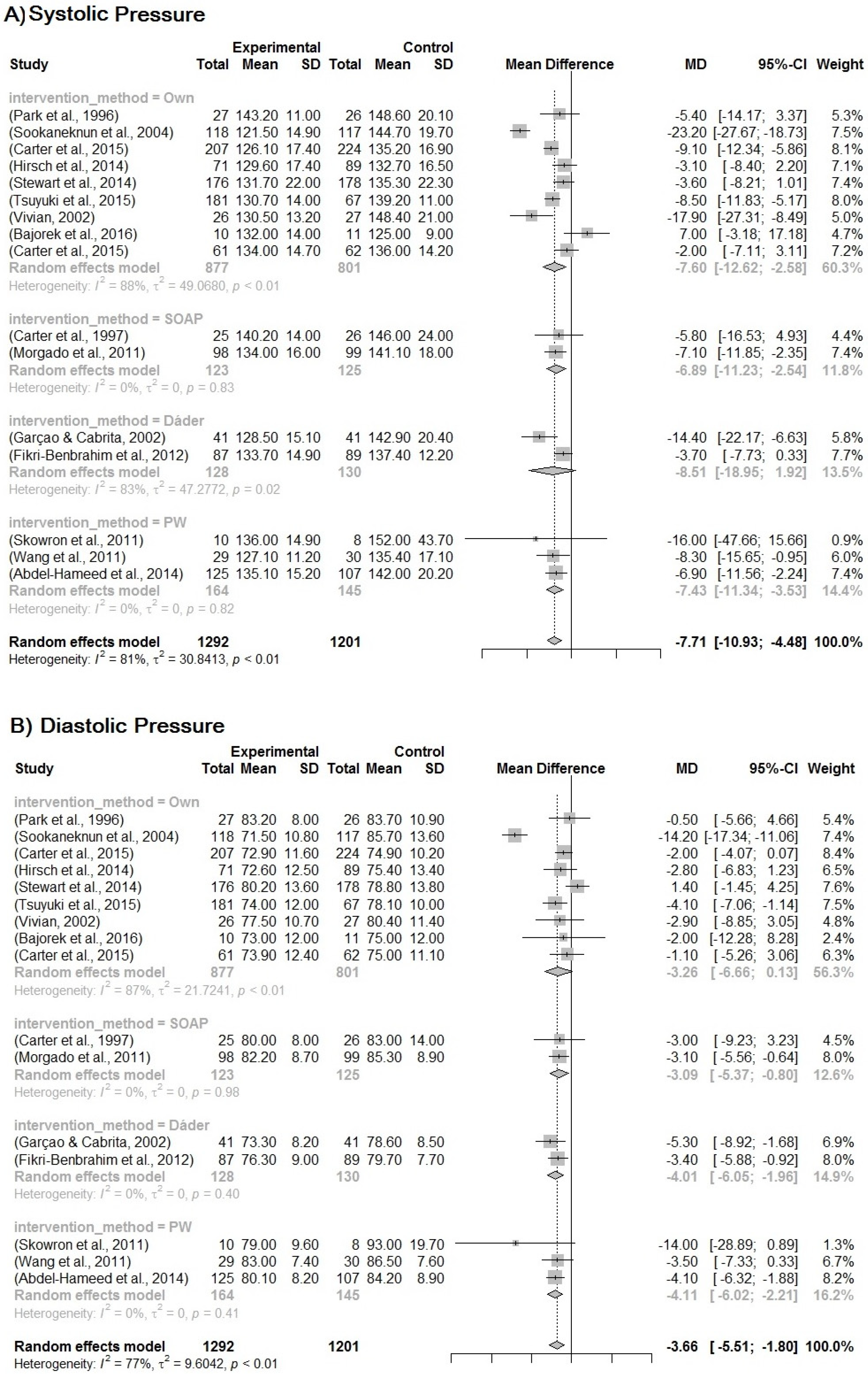
The randomized clinical trial studies with quality assessed as good-to-high evidence were selected to be included in the meta-analysis. The treatment effect of MTM-PC was analyzed firstly for blood pressure. The mean reduction in blood pressure in the intervention group compared to the control group is −7.71 (95% CI, −10.93 to −4.48) and −3.66 (95% CI, −5.51 to −1.80) (p < 0.001) for SBP and DBP, respectively. It is important to consider the random model for the results due to the high heterogeneity between the studies, which is 81% and 77% (Figure 2).
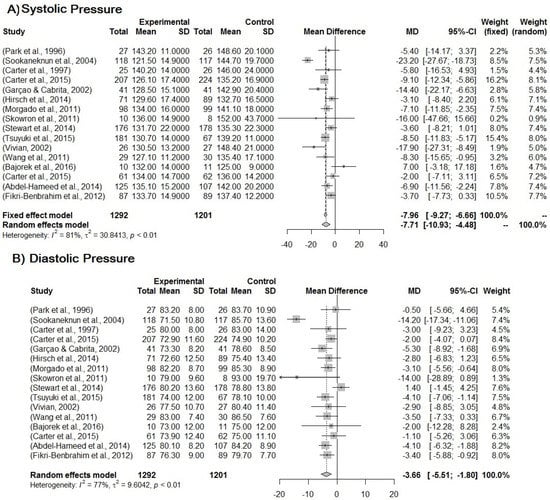
Figure 2.
(A) Forest plot for systemic blood pressure. (B) Forest plot for diastolic blood pressure. Forest plot of blood pressure reduction in the intervention group compared to the control group in relation to MTM by PC for the treatment of hypertension. Included studies: Park et al. [23]; Sookaneknun et al. [24]; Carter et al. [29]; Carter et al. [30]; Garçao, Cabrita [34]; Hirsch et al. [35]; Morgado, Rolo, Castelo-Branco [39]; Skowron, Polak, Brandys [42]; Stewart et al. [43]; Tsuyuki et al. [45]; Vivian [46]; Wang et al. [47]; Bajorek et al. [48]; Carter et al. [49]; Abdel-Hameed et al. [51]; Fikri-Benbrahim et al. [52].
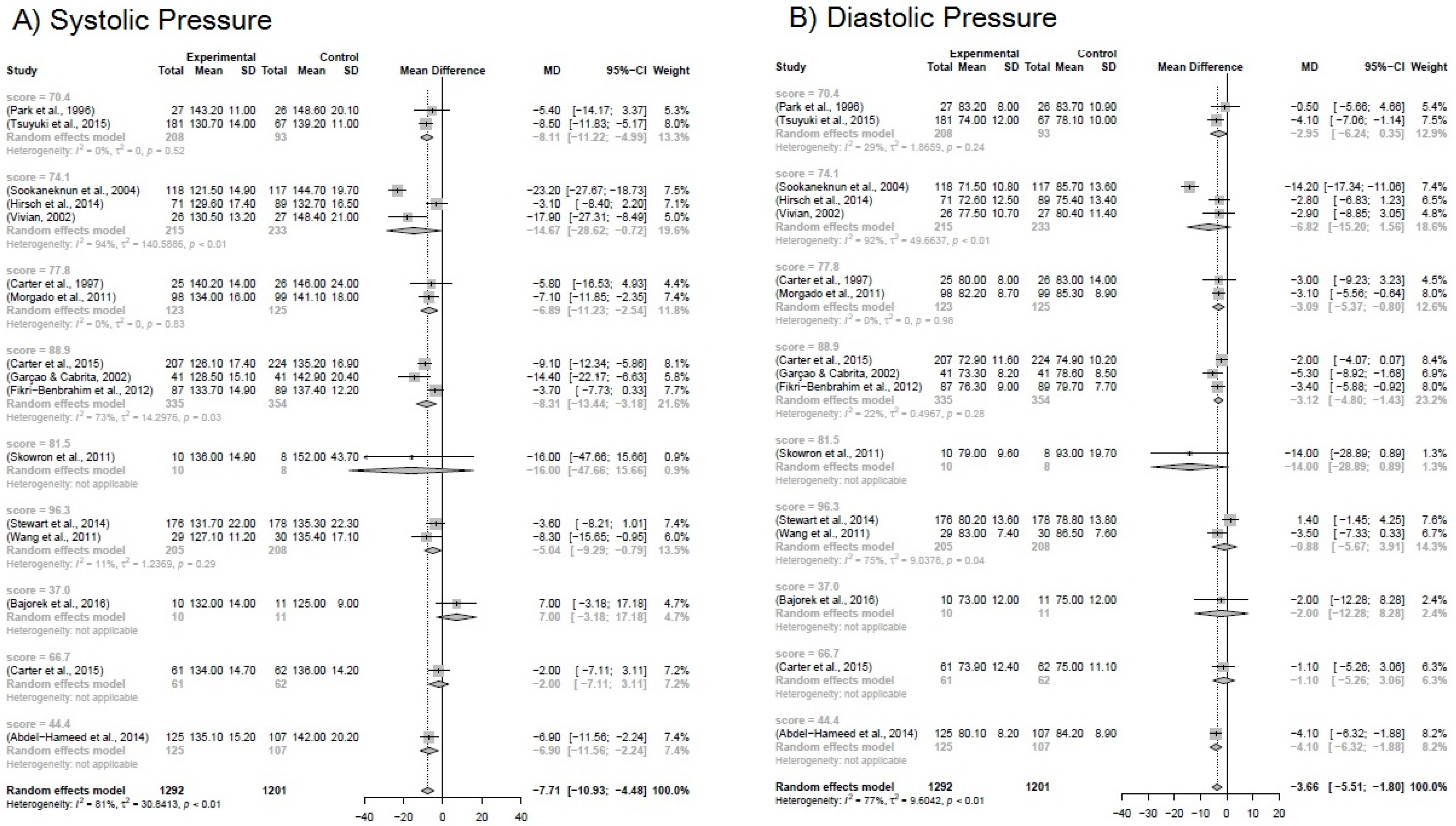
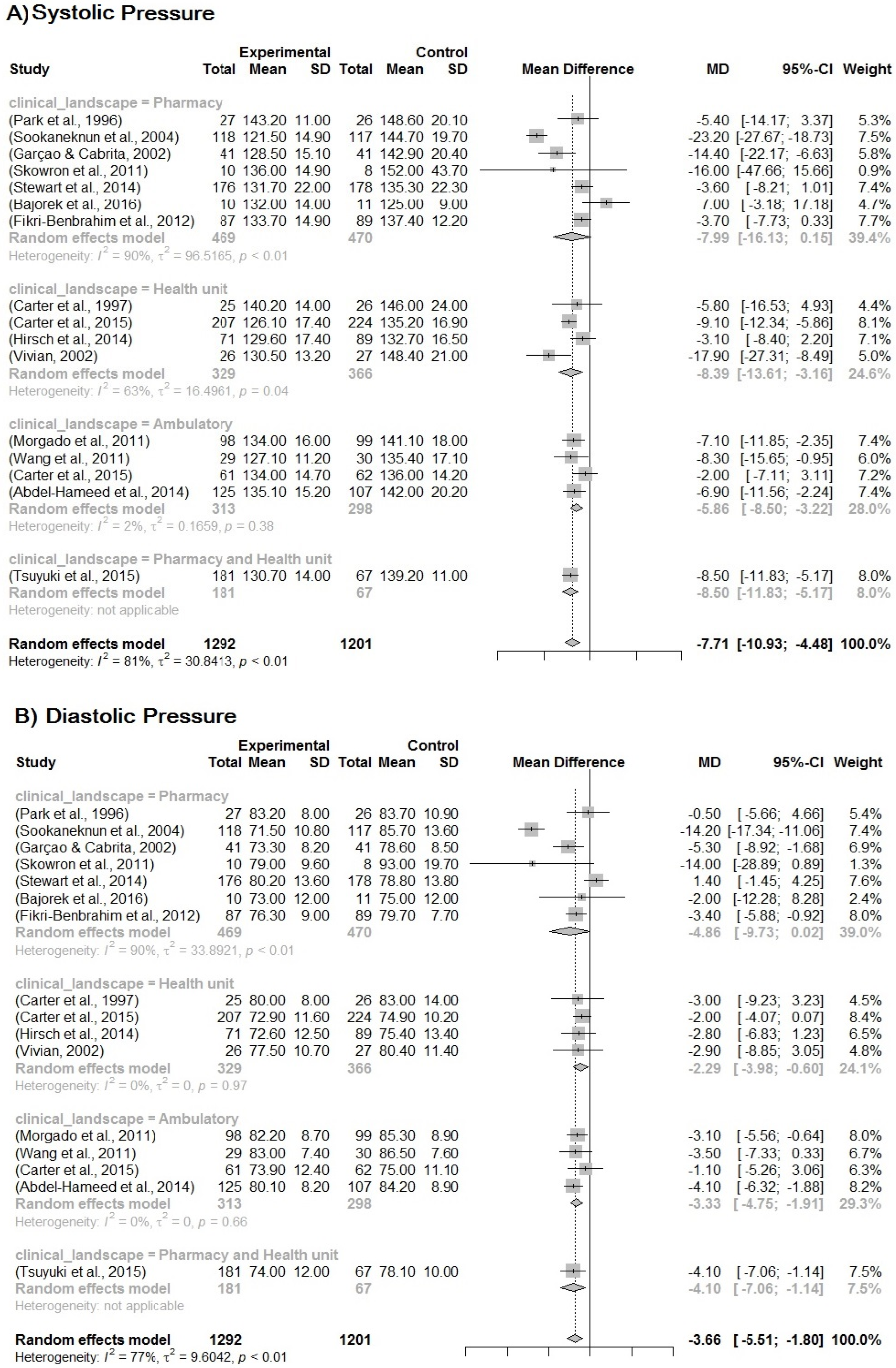
Due to the heterogeneity between the studies, a sub-analysis was performed based on the group of different variables: study quality score (0–100% according to the level of evidence); clinical setting (where the PC was developed, pharmacy, facilities, clinic); method for developing the MTM (own, Dáder, PW, SOAP). It is likely that if we removed the studies by Vivian et al. [46] and Skowron et al. [42], heterogeneity between studies may decrease, although in this case, the p-value is 0.0994. The same situation is represented for the other subgroup analyses, whose p-value is 0.6143 and 0.9916, for the clinical scenarios and the method, respectively. The results are shown in Figure 3, Figure 4 and Figure 5.
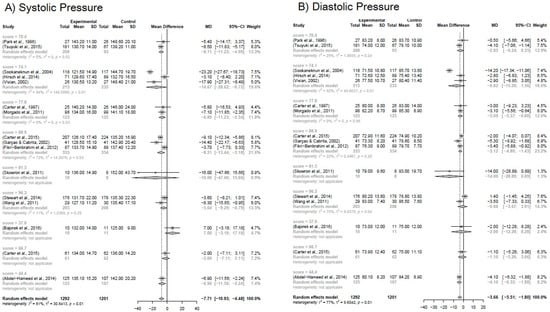
Figure 3.
(A) Forest plot for systemic blood pressure. (B) Forest plot for diastolic blood pressure. Forest plot of blood pressure reduction in the subgroup analysis for the study quality score. Included studies: Park et al. [23]; Tsuyuki et al. [45]; Sookaneknun et al. [24]; Hirsch et al. [35]; Vivian [46]; Carter et al. [29]; Morgado, Rolo, Castelo-Branco [39]; Carter et al. [30]; Garçao, Cabrita [34]; Fikri-Benbrahim et al. [52]; Skowron, Polak, Brandys [42]; Stewart et al. [43]; Wang et al. [47]; Bajorek et al. [48]; Carter et al. [49]; Abdel-Hameed et al. [51].
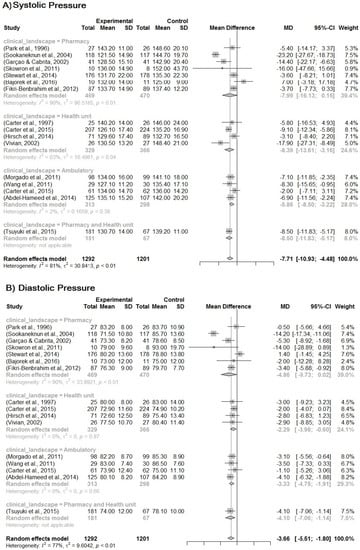
Figure 4.
(A) Forest plot for systemic blood pressure. (B) Forest plot for diastolic blood pressure Forest plot of blood pressure reduction in the subgroup analysis for the MTM-PC insertion scenario. Included studies: Park et al. [23]; Sookaneknun et al. [24]; Garçao, Cabrita [34]; Skowron, Polak, Brandys [42]; Stewart et al. [43]; Bajorek et al. [48]; Fikri-Benbrahim et al. [52]; Carter et al. [29]; Carter et al. [30]; Hirsch et al. [35]; Vivian [46]; Morgado, Rolo, Castelo-Branco [39]; Wang et al. [47]; Carter et al. [49]; Abdel-Hameed et al. [51]; Tsuyuki et al. [45].

Figure 5.
(A) Forest plot for systemic blood pressure. (B) Forest plot for diastolic blood pressure. Forest plot of blood pressure reduction in the subgroup analysis for the MTM-PC models. Included studies: Park et al. [23]; Sookaneknun et al. [24]; Carter et al. [30]; Hirsch et al. [35]; Stewart et al. [43]; Tsuyuki et al. [45]; Vivian [46]; Bajorek et al. [48]; Carter et al. [49]; Carter et al. [29]; Morgado, Rolo, Castelo-Branco [39]; Garçao, Cabrita [34]; Fikri-Benbrahim et al. [52]; Skowron, Polak, Brandys [42]; Wang et al. [47]; Abdel-Hameed et al. [51].
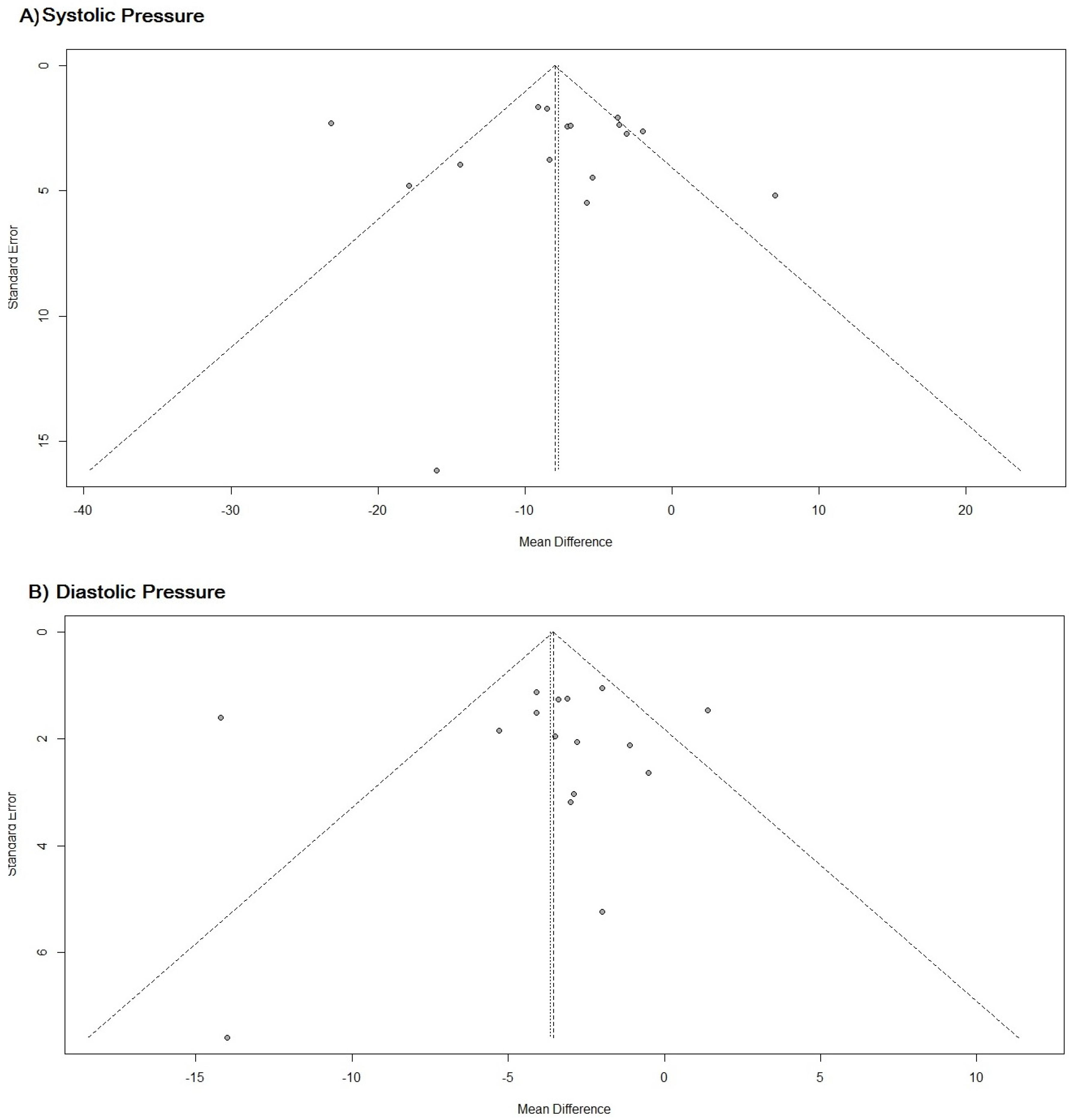
The funnel graph shows that there is considerable accuracy in the results of the studies and it also shows that there is no publication bias influencing the results, p-value = 0.8539 (Figure 6).
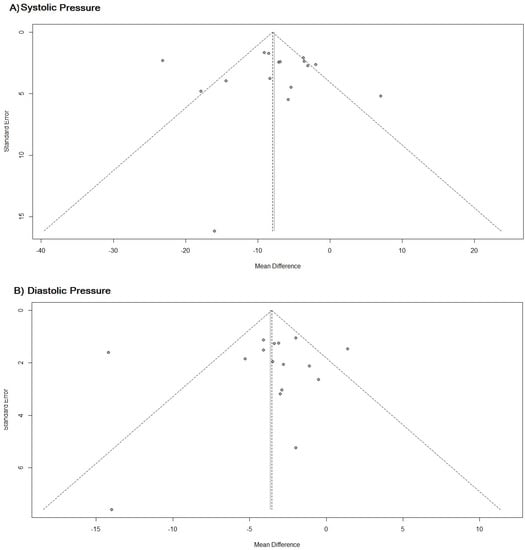
Figure 6.
(A) Funnel chart for systemic blood pressure. (B) Funnel plot for diastolic blood pressure. Funnel plot of studies on the impact of MTM by PC on blood pressure in hypertensive patients.
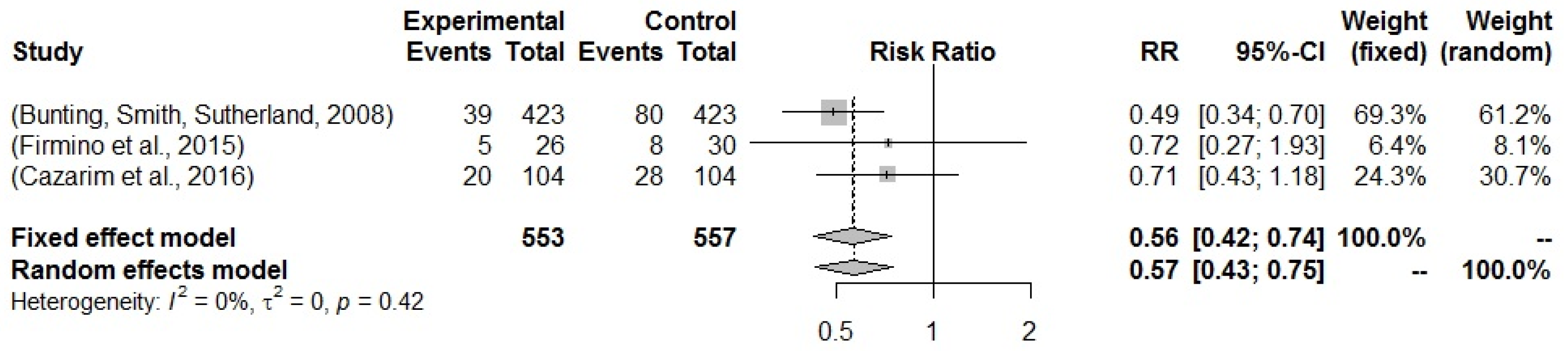
Relative risk was analyzed for cardiovascular risk over ten years, as measured by the ASCVD risk scale. It was only possible to calculate the risk in three studies. The results show that there is a reduction in the cardiovascular risk of hypertensive patients when there is MTM by PC for hypertensive patients. In this sense, the PC works as a protective factor when analyzed both by the fixed model and by the random model, relative risk (RR) = 0.561 (95% CI 0.422–0.742) and RR = 0.570 (95% CI 0.431–0.750). Although the studies can be considered homogeneous, I² = 0%, it makes no sense to state this possibility, due to the smaller number of studies for the calculation of “n” in the I² formula (Figure 7).
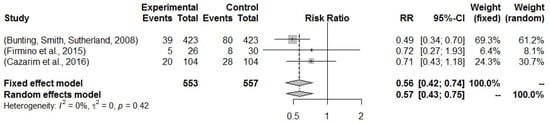
Figure 7.
Forest plot of studies for which it possible to assess the relative risk regarding the impact of MTM by PC on cardiovascular risk over ten years in hypertensive patients. Included studies: Bunting, Smith, Sutherland [21]; Firmino et al. [33]; Cazarim et al. [60].
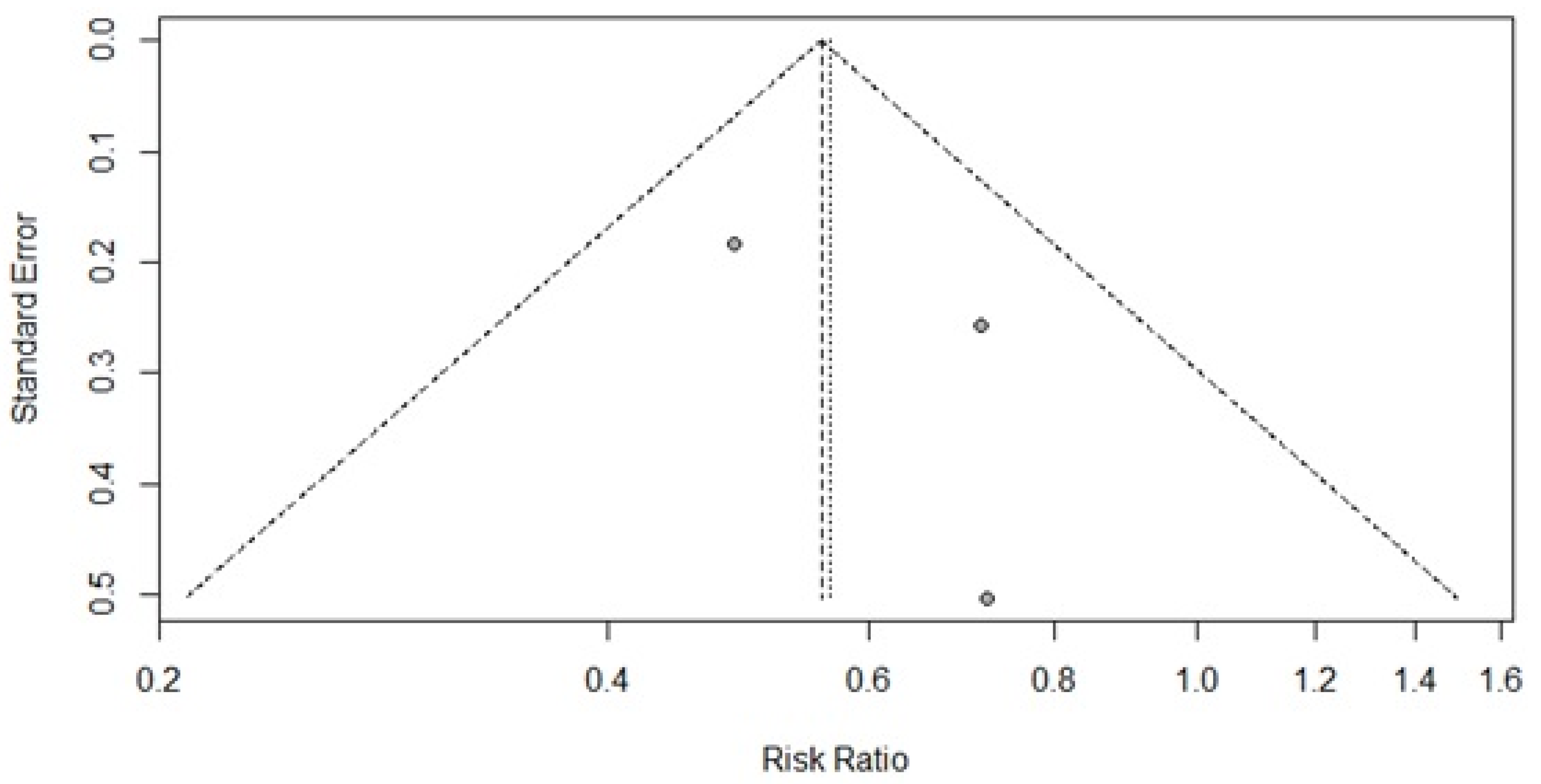
The funnel plot for analysis of cardiovascular risk shows that there is a lower possibility of publication bias; although there are few studies for this analysis, the tendency would be to increase the RR. However, there is no asymmetry to support a bias, p = 0.4949. It is noteworthy that more than 50% of the studies show good accuracy, greater than 30% (Figure 8).
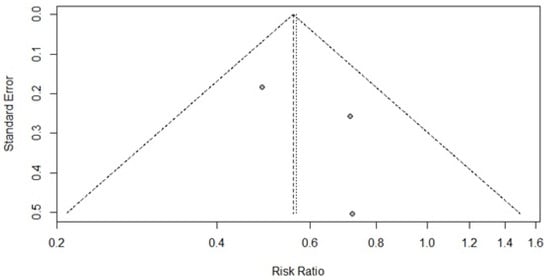
Figure 8.
Funnel plot of the studies that made it possible to assess the relative risk regarding the impact of MTM by PC on cardiovascular risk over ten years in hypertensive patients.
Data meta-regression was performed, as the quality scores of the studies may be associated with their results regarding cardiovascular risk over ten years. It is not possible to achieve a level of good evidence due to the number of studies, but meta-regression may suggest that the higher the study quality, the lower the protective impact of PC on cardiovascular risk, p = 0.2532 (Figure 9).
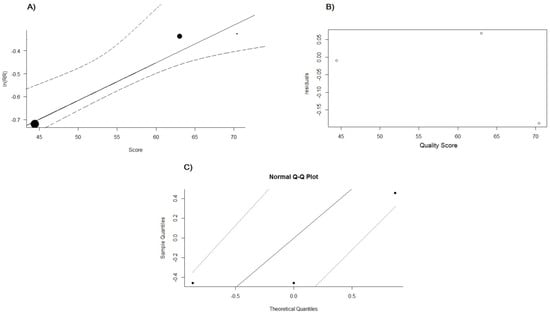
Figure 9.
(A) Meta-plot for cardiovascular risk and study quality score. (B) Meta-regression graph for cardiovascular risk and study quality score. (C) Normal Q–Q plot meta-regression for cardiovascular risk and study quality score. Meta-regression for mixed-effects models for cardiovascular risk and the quality score of studies referring to MTM by PC for hypertensive patients.
3. Discussion
The selection of studies for the review has a satisfactory agreement between the two researchers, classified as almost perfect, which shows that the review is consistent with its protocol regarding the robustness of the methods used for the inclusion of studies [62]. The quality evaluation of the included studies shows that the clinical trial studies have better scores than the observational studies in general, 70.7%, and the greatest number of studies included in the review have a score above 60 (0–100). The mean quality score is 70.8 ± 19.3 for randomized clinical trials, 52.7 ± 15.3 for non-randomized clinical trials, and 51.8 ± 19.3 for observational studies. However, studies with higher chances of bias, classified as poor or flawed evidence (51.2%), surpass the total number of studies with good and high evidence (48.8%). It is noteworthy that the better the quality of the study, the greater the chances of having better accuracy of the results, and this could be verified in this review, in which the types of studies with a higher level of evidence present positive results from MTM-PC [15,63].
Pharmaceutical interventions in the MTM process, either alone or in collaboration with other health professionals, are recognized to improve blood pressure control. However, pharmaceutical interventions can have a magnitude of differential effects on blood pressure ranging from very large, modest, to no effect. This fact can be determined by the heterogeneity of the MTM-PC models and in the methods of the study that evaluate that model [64]. It is noteworthy that this review shows that most MTM-PC models are developed by the pharmacist or clinical group, the own model grounded at default methods, maybe because they are better adapted to each reality.
Additionally, when analysing those studies that present poor results for blood pressure control compared to the others in this review, we find that there is no interference. In this case, it is noted that the studies by Bajorek et al. [48] and Modé et al. [55] present results in which MTM does not promote improvement in blood pressure values. The quality of studies that show improvement in blood pressure values was compared with the quality of these two studies. The adjusted value of the Mann–Whitney test, w = 7.00 (p= 0.036), shows that the quality of these two studies, measured by the Downs and Black [61] instrument, is lower than the other studies that show improvement in arterial blood pressure values.
It is noteworthy that there is evidence for homogeneity between the groups compared in this review regarding sociodemographic characteristics, as well as for the variables that cannot be modified by the intervention of the studies (staging of the degree of hypertension, presence of diabetes, smoking, alcoholism, obesity, body mass index, abdominal circumference, and history of diseases). Homogeneity between groups is an important factor for comparing them and obtaining the measure of the clinical effect of an intervention, which gives greater accuracy to the results of this review [65].
In addition, there is better pressure control of patients in MTM by PC, of which 25.2% more have blood pressure control and improvement in lipid profiles compared to the group with conventional health care. The importance of controlling blood pressure and improving the lipid profile directly infers in the management of hypertensive patients, both clinical regarding the reduction in cardiovascular risk, and managerial for improving the profile care in the sense to pass from emergency to a preventive scope and, consequently, to promote changes in the pharmacotherapy [60].
The meta-analysis of this study shows an RR less than 1 [0.56; 0.42–0.74, 95% CI] for the cardiovascular risk over ten years, which represents a protective character for hypertensives regarding the CP treatment effect [66]. The measure of effect is able to show the efficacy of MTM by PC equal to 44.0% (26.0–58.0, 95% CI), an important result when compared to other preventive interventions [67]. It is like that this result may have a strong association with pharmaceutical interventions related to drug-related problems, which have an impact on the effectiveness and safety of pharmacological treatment, with a consequence of improved adherence and lifestyle [68,69].
In addition, there is evidence for a mean reduction in systolic and diastolic pressures. These results are relevant, as a decrease of 5.7 mmHg is capable of reducing the absolute risk of acute myocardial infarction related to ischemic heart disease, stroke, and heart failure by 3.7 years, by 2.00%, 2.40%, and 2.20%, respectively. This study shows a reduction between 4.48 to 10.93 mmHg in systolic pressure and 1.80 to 5.51 mmHg in diastolic pressure. Consequently, it can impact on the absolute risk reduction over ten years, reaching 8.74% for health complications from hypertension and 1.13% for the reduction of morbidities associated with hypertension [70].
The subgroups’ analysis for quality of the studies, the clinical setting, and the follow-up models contribute to these results. The differences in the clinical scenario show that the community pharmacy presents a higher impact on blood pressure reduction, but these subgroups have the study of Bajorek et al. [48], which presents negative results for blood pressure. It could influence the confidence interval for this group. However, the other scenarios have evidence for reducing blood pressure. Although there are some differences among the models of MTM-PC on blood pressure, all models are shown to be efficient. There is evidence for own models to be able to cause the better mean difference in blood pressure, −7.60 [IC 95%, −12.62; −2.58] and −3.26 [IC 95%, −6.66; −0.13], followed by SOAP −6.89 [IC 95%, −11.23; −2.54] and −3.09 [IC 95%, −5.37; −0.80]. Additionally, the PW model has a good balance for reducing systolic and diastolic pressure, PW −7.43 [IC 95%, −11.34; 3.53] and −4.11 [IC 95%, −6.02; −2.21]. The Dáder model has a confidence interval passing by one, which means that it can have no good results for blood pressure, despite it presenting a better range for reducing blood pressure −8.51 [IC 95%, −18.95; 1.92] and −4.01 [IC 95%, −6.05; −1.96].
The results show that these subgroups do not influence the discrepancies in results between studies for blood pressure control, (p-value > 0.05). Thus, it is noted that the hypothesis that the different models of MTM by PC can influence, in a positive or negative result, does not apply [64]. Therefore, it is possible that MTM-PC models, which are not standard to the existing philosophy of PC and that are not adapted to the regional reality, cultural, and epidemiological characteristics, and to the needs of the health systems, are capable of providing discrepant and even ineffective results for reducing arterial blood pressure [71].
The result of the clinical impact of PC can have repercussions on the health system as a whole, since primary health care is recommended to be resolutive and preventive to improve the efficiency of the system. In this sense, it is noteworthy that MTM by PC is able to reduce hospital readmissions of hypertensive patients by an average of 30 days [72]. It is known that as the level of complexity of care increases, the cost per patient for the health system also increases. In this way, PC may be able to optimize resources and save costs in health systems, with the ability to improve the patient’s quality of life, as evidenced in the results of this review [73].
It is noteworthy that the results of this meta-analysis refer to hypertensive patients undergoing preventive care and follow-up in primary health care. Thus, the profile of the MTM models by PC can be delineated with the average number of eight consultations, with an average duration of 30 min among all consultations, with the first consultation taking the longest time from around 40 min to 1 h and 50 min, with a mean of ten months and median of six months of patient follow-up. In a direct cost analysis, it is shown that optimizing resources tends to be more cost-effective in six months of follow-up of patients with MTM by PC [70], which can cost USD 75 to increase in a unit the blood pressure control of hypertensive patients [74]. In the cost-effectiveness analysis of the MTM by PC for hypertensive patients, it is shown that the initial investment in the service is rewarded in outcomes and in return on investment even after three years of patient discharge, presenting the cost of USD 128.03 for improving by one unit the blood pressure of hypertensive patients [75].
In addition, it is highlighted in the profile of the MTM models developed in PC that community pharmacies and primary health units are the most prevalent scenarios for their insertion in the scope of primary health care. Additionally, added to the results of the MTM profile developed in the PC in this review, the important role of health education and the insertion of other PC services in its development in an interdisciplinary and collaborative way with other clinicians is highlighted, such as through pharmacotherapy review, medication reconciliation, therapeutic medication monitoring, and health condition management [71].
This study had some limitations. Several included studies had incomplete data for the cardiovascular risk calculating, and this fact made it difficult to measure the cardiovascular risk for different models and scenarios. If we tried to estimate the cardiovascular risk for different MTM-PC models and scenarios, we would need to perform another review, which certainly would completely change the aim of this review and not evaluate the influence of different models of MTM-PC and other important characteristics of their effects, since there are different instruments to calculate the cardiovascular risk, which must be considered when the calculation is ready in the study, and also there are different diseases that are applied to cardiovascular risk for their management [76,77].
The most important models for MTM-PC in this theme are identified in the included studies, but there are other models such as therapeutic outcomes monitoring (TOM), OLD CARTS, and others that are not identified. Actually, these methods are unhabitual by PC, and they are not very well incorporated into the clinical practice [71]. Consequently, it would not impact on the evidence level of the MTM-PC on hypertension management.
In fact, it is possible to refer to the fact that the MTM-PC can be an adjuvant health technology to new antihypertensive therapies when in the market clinical phase, most likely due to carrying out nonpharmacological lifestyle interventions along with antihypertensive drug therapies [78]. Consequently, it can aid to improve the numbers of poor blood pressure control, which are alarming, as only 10% on average have their blood pressure controlled in low-income and middle-income countries [79].
4. Materials and Methods
4.1. Review Question
This study is a systematic review with meta-analysis, which set off from the following review question: What MTM models in PC have been developed for hypertensive patients in primary care and what is their clinical impact in blood pressure and cardiovascular risk?
4.2. Register
This study had its protocol registered in the PROSPERO database, which makes this paper clearer regarding its production. It can be accessed at https://www.crd.york.ac.uk/prospero/, where ID registration is CRD42017079761. Accessed on 12 December 2022.
The review was designed for the following steps: a question based on the need for evidence; search strategies; deletion of duplicates; primary selection (reading the title and abstract); eligibility; secondary selection (reading the whole text); search in the grey literature, performed by manual search (search in the references of selected articles or indication of experts in the subject) and search in unofficial databases, Google® and clinical trials.gov; data extraction; assessment of the quality of studies; tabulation of results; primary analysis; and performance of meta-analysis. Consensus was established between two blinded researchers in the primary selection stage, and, when necessary, a third researcher intervened to support the inclusion or not of the study according to eligibility and inclusion and exclusion criteria established by the protocol. Eligibility aspects included reliability criteria based on the PRISMA checklist [80].
Search strategies were adjusted in English, Spanish, and Portuguese to four reference databases: PubMed, EMBASE, Scopus, and the Central Cochrane Library. As recommended by the Cochrane manual for systematic reviews, three databases considered local or multidisciplinary/specific to the topic were selected: LILACs, International Pharmaceutical Abstracts (IPA), and Web of Sciences. The descriptors were identified in the scientific dictionaries: Emtree thesaurus, Descriptors in Health Sciences (DeCS), and Medical Subject Headings (MeSH) for their specific databases. The Boolean operator “OR” was used for combining words into the same category and “AND” for combining inter-category [19]. The search was carried out on 27 September 2022. The grey literature search was carried out on 18 November 2022 (Table S2 and Item S1).
The outcomes category, “O” was not considered for this search strategy because it is not a gold standard comparator (placebo or drug, for example) and this could reduce the search sensitivity according to the Cochrane guideline; the outcomes were incorporated with the Boolean operator “OR” in the identification of the study population for the search [80]. A summary of the population (P), interventions (I)/exposition (E), comparators (C), outcomes (O), and study design (S) considered, following the PI(E)COS acronym for the search strategy, with no filters (Table 7).

Table 7.
Application of PI(E)COS acronym for the search strategy.
The studies were selected in the following order: title, abstract, and full-text reading. The selection was carried out using the Rayyan platform for systematic reviews, which is available for registration and, with free access. Data were tabulated in order to extract the general characteristics of the study, sociodemographic characteristics of the patient groups, and clinical and care characteristics, as well as the definitions of the MTM model developed in PC. To access the quality of the studies, the validated instrument by Downs and Black [61] was used, which comprises a checklist of 28 items, which allows for checking the general quality of observational studies and clinical trials, according to the following characteristics: qualities of general aspects of the study, internal and external validity, confounding biases, and the power of the analyses. This measurement is performed by a generated score [61].
The condition or domain of review was defined for the MTM models developed by PC in the context of primary health care, preventive or community care, performed for patients with non-secondary systemic arterial hypertension, and patients treated in the primary care scenario. In addition, it was necessary to judge whether the pharmacist carried out at least two consultations to monitor the patients in at least three months to characterize the clinical follow-up. In addition, it was imperative that the results presented by the study were exclusive to the pharmacist’s intervention, with the pharmacist being incorporated or not in a multidisciplinary team [10,60]. It is important that we have led our analysis to be different in some points of the published reviews on this theme, mainly to describe different services regarding its qualities, as well as the MTM-PC models and the scenarios in which the model is inserted. In this way, we summarize the characteristics of those models compared to their results.
Considerations about the studies eligible for the review were established, such as: considering the original articles to be language-free and considering the studies that sought to answer the question of the systematic review and that met the inclusion and eligibility criteria. It is noteworthy that clinical trials were analyzed in a separate group from other studies and divided into randomized and non-randomized. In addition, meta-analyses and systematic reviews were not included in the review results. Thus, this systematic review considered the following inclusion and exclusion criteria for the studies retrieved in the searches:
Inclusion: studies with adult patients, over 18 years old; outpatients or hypertensive patients seen in community pharmacies or primary/preventive care units; intervention performed based on MTM by PC; minimum of two consultations carried out by the pharmacist in the intervention group; the pharmacist should attend individually or to be a member of a multidisciplinary team, but in this case, the intervention should not depend on the team, but exclusively on the pharmacist; blood pressure assessment should be included as measured results.
Exclusion: studies that considered hypertensive pregnant women; patients with cognitive impairment; patients with moderate to severe chronic kidney disease; patients who were not receiving pharmacological treatment for systemic arterial hypertension; patients without a diagnosis of systemic arterial hypertension; narrative or integrative review studies, dissertations or theses, editorials, news, comments, letters to the editor, abstracts published in the annals of scientific journals or congresses, and guidelines; studies that developed MTM-PC without reviewing pharmacotherapy or pharmacotherapeutic follow-up or did not manage health conditions; studies that did not address MTM in its aspects as a service, on an individual basis, with the elaboration of a therapeutic plan, monitoring the results and with the systematic recording of the patient’s data; studies without a comparator for the results.
4.3. Analysis
The analysis of the results was performed using classical statistics. Thus, considering the significance level of 5% and test power equal to 80% [81]. For the classic inferential statistical analysis, MINITAB software version 18 was used. For the systematic review, before the moment of consensus between the two researchers, the agreement between them was analyzed by the Kappa coefficient, with a value above 0.70 being acceptable, otherwise, there would be a need to restructure a new search strategy.
The Mann–Whitney test was performed to assess the difference in quality scores between studies in which the MTM-PC presented favorable clinical results and those with unfavorable clinical results. The score from the Downs and Black instrument [61] was measured in percentages from 0 to 100%. The interpretation of the assessed scores was summarized as follows: up to 50% were considered flawed evidence or irrelevant studies; those between 50–69% were considered poor evidence; between 70–79% were considered good evidence; and 80–100% were considered with high scientific evidence [16,61].
R studio software was used to run the meta-analysis. The effect measure was measured in the meta-analysis by the difference between means for systolic and diastolic blood pressure and by the RR for cardiovascular risk over ten years. The results were diagrammed in a forest plot with the effect measure represented by the diamond. The evaluation of the inconsistency or heterogeneity of the studies was carried out by the I², represented by the percentage of heterogeneity, and analyzed by the p-value, which respected the significance level of 5%, thus, the reading of the p-value above 0.05 means rejecting the alternative hypothesis and assuming that the studies were homogeneous. However, a homogeneous result may show that there was some random variability in the results of the studies, whereas heterogeneous results represent variability due to inconsistency. The measurement of publication bias in the literature was evaluated using a funnel plot, in which, by diagramming the results, it was possible to verify where there was a tendency for publications for favoring some result. In this case, the better the distribution on the graph and the more homogeneous (symmetric), the smaller the bias [81].
5. Conclusions
Most of the studies included in this review have a quality score above 60% and almost half have a good-to-high evidence rating for the results. Among the MTM-PC models analyzed in this systematic review, most are from the USA. Own models, reasoned on standard models, emerge as the most prevalent. Sequentially, from the profile obtained from the MTM by the PC, it was noted that the average time for monitoring hypertensive patients is ten months, with an average of eight 30 min consultations, with the exception of the first consultation being longer, being approximately one hour and 30 min. It is not possible to calculate the average number of patients to be consulted by the pharmacist in the month because many models originate from epidemiological studies and do not refer to the feasibility regarding the capacity of consultation.
There is evidence for the mean reduction in blood pressure and also for better blood pressure control, consequently, there is a reduction in cardiovascular risk over ten years associated with the improvement in quality of life of hypertensive patients assisted in the MTM by PC, which can work as a protective factor to hypertension, presenting a good efficiency to avoid incidence of CVDs in hypertensive patients. Thus, the community pharmacy setting is important for the better reach of MTM-PC impact, but the ambulatory setting has better evidence for reducing blood pressure. Regarding different models, the own model of MTM-PC has the better impact and PW is the most balanced for reducing blood pressure. However, it is highlighted that further exploration is needed.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ph16060845/s1, Table S1: scientific studies/documents that were excluded from the systematic review; Table S2: Emtree terms for the search strategy in each database and; Item S1: search strategy combined for each database.
Author Contributions
Conceptualization, M.d.S.C.; methodology, M.d.S.C. and A.A.N.; software, M.d.S.C. and A.A.N.; validation, K.B. and A.A.N.; formal analysis, M.d.S.C.; investigation, M.d.S.C. and E.L.C.C.-C.; resources, A.A.N.; data curation, M.d.S.C. and E.L.C.C.-C.; writing—original draft preparation, M.d.S.C.; writing—review and editing, E.L.C.C.-C., A.A.N., K.B. and O.W.; visualization, M.d.S.C. and A.A.N.; supervision, O.W. and A.A.N.; project administration, A.A.N.; funding acquisition, A.A.N. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study due to the reason of this being a systematic review, in which the data were treated as secondary and published data.
Informed Consent Statement
It is not applicable due this study is a systematic review.
Data Availability Statement
Data are available upon request and provided by the corresponding author. The protocol of this systematic review was registered in the PROSPERO database and updated on 30 March 2023 [protocol number: is CRD42017079761]. Data can be viewed from the literature, since this is a systematic review; analyzed data can be requested from the corresponding author.
Acknowledgments
We would like to thank the Foundation for the Support of Teaching, Research and Service of the University Hospital (FAEPA), University Hospital of the Ribeirão Preto Medical School (HCFMRP)—University of São Paulo—USP, for supporting the publication of this study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Health Organization (WHO). World Health Statistics 2017: Monitoring Health for the SDGs, Sustainable Development Goals. 2017. Available online: https://goo.gl/ExTpjh (accessed on 26 December 2022).
- World Health Organization (WHO). Global Health Observatory Data Repository. Noncommunicable Diseases: Mortality. 2021. Available online: https://bityli.com/0Zyo3i (accessed on 27 December 2022).
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E., Jr.; Collins, K.J.; Himmelfarb, C.D.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. J. Am. Coll. Cardiol. 2018, 71, e127–e248. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Cardiovascular Diseases (CVDs). Media Centre: Fact Sheets. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 27 December 2022).
- Malta, D.C.; Stopa, S.R.; Szwarcwald, C.L.; Gomes, N.L.; Júnior, J.B.S.; Dos Reis, A.A.C. Surveillance and monitoring of major chronic diseases in Brazil—National Health Survey, 2013. Rev. Bras. Epidemiol. 2015, 18, 3–16. [Google Scholar] [CrossRef]
- Roush, G.; Fagard, R.; Salles, G.; Pierdomenico, S.; Reboldi, G.; Verdecchia, P.; Eguchi, K.; Kario, K.; Polónia, J.; De La Sierra, A.; et al. Prognostic impact of clinic, daytime, and nighttime systolic blood pressure in 9 cohorts of 13,843 patients with hypertension: Systematic review and meta-analysis. J. Am. Soc. Hypertens. 2014, 8, e59. [Google Scholar] [CrossRef]
- Luo, D.; Cheng, Y.; Zhang, H.; Ba, M.; Chen, P.; Li, H.; Chen, K.; Sha, W.; Zhang, C.; Chen, H. Association between high blood pressure and long term cardiovascular events in young adults: Systematic review and meta-analysis. BMJ 2020, 370, m3222. [Google Scholar] [CrossRef]
- Drummond, F.M.; Sculpher, M.J.; Torrance, G.W.; O’Brien, B.J.; Stoddart, G.L. Methods for the Economic Evaluation of Health Care Programmes, 4th ed.; Oxford University press: Oxford, UK, 2015; p. 429. [Google Scholar]
- Carey, R.M.; Muntner, P.; Bosworth, H.B.; Whelton, P.K. Prevention and Control of Hypertension: JACC Health Promotion Series. J. Am. Coll. Cardiol. 2018, 72, 1278–1293. [Google Scholar] [CrossRef]
- Strand, L.M.; Cipolle, R.J.; Morley, P.C.; Perrier, D.G. Levels of pharmaceutical care: A needs-based approach. Am. J. Hosp. Pharm. 1991, 48, 547–550. [Google Scholar] [CrossRef]
- Bektay, M.Y.; Sancar, M.; Al-Ezzı, S.A.A.; İzzettin, F.V. Time to change to improve health: Clinical pharmacy and pharmaceutical care education in Turkey. J. Ideas Health 2020, 3, 130–134. [Google Scholar] [CrossRef]
- Dreischulte, T.; Van-den-Bemt, B.; Steurbaut, S. European Society of Clinical Pharmacy definition of the term clinical pharmacy and its relationship to pharmaceutical care: A position paper. Int. J. Clin. Pharm. 2022, 44, 837–842. [Google Scholar] [CrossRef]
- Marupuru, S.; Roether, A.; Guimond, A.J.; Stanley, C.; Pesqueira, T.; Axon, D.R. A Systematic Review of Clinical Outcomes from Pharmacist Provided Medication Therapy Management (MTM) among Patients with Diabetes, Hypertension, or Dyslipidemia. Healthcare 2022, 10, 1207. [Google Scholar] [CrossRef]
- Ogungbe, O.; Cazabon, D.; Ajenikoko, A.; Jeemon, P.; Moran, A.E.; Commodore-Mensah, Y. Determining the frequency and level of task-sharing for hypertension management in LMICs: A systematic review and meta-analysis. EClinicalMedicine 2022, 47, 101388. [Google Scholar] [CrossRef]
- Chiappelli, F.; Brant, X.M.C.; Neagos, N.; Oluwadara, O.O.; Ramchandani, M.H. Evidence-Based Practice: Toward Optimizing Clinical Outcomes, 1st ed.; Springer: Berlin/Heidelberg, Germany, 2010; p. 294. [Google Scholar]
- Machado, M.; Bajcar, J.; Guzzo, G.C.; Einarson, T.R. Hypertenion: Sensitivity of patient outcomes to pharmacist interventions. Part II: Systematic review and meta-analysis in hypertension management. Ann. Pharmacother. 2007, 41, 1770–1781. [Google Scholar] [CrossRef]
- Luque, R.; Martínez-Martínez, F.; Martí, M.; Gastelurrutia, M.A.; Dago, A.; Andrés, J. Revisión sistemática de los estudios españoles sobre atención farmacéutica comunitaria en hipertensión arterial. Pharm. Care España 2014, 16, 193–202. [Google Scholar]
- Shrestha, S.; Shrestha, R.; Ahmed, A.; Sapkota, B.; Khatiwada, A.P.; Christopher, C.M.; Thapa, P.; Kc, B.; Blebil, A.Q.; Khanal, S.; et al. Impact of pharmacist services on economic, clinical, and humanistic outcome (ECHO) of South Asian patients: A systematic review. J. Pharm. Policy Pract. 2022, 15, 37. [Google Scholar] [CrossRef] [PubMed]
- Bazerman, M.H.; Moore, D. Processo Decisório, 8th ed.; Elsevier: Rio de Janeiro, Brazil, 2014; p. 312. [Google Scholar]
- Jamieson, L.H.; Scally, A.; Chrystyn, H. A randomised comparison of practice pharmacist-managed hypertension providing level 3 medication review versus usual care in general practice. J. Appl. Res. 2010, 7, 77–86. [Google Scholar]
- Bunting, B.A.; Smith, B.H.; Sutherland, S.E. The Asheville Project: Clinical and economic outcomes of a community-based long-term medication therapy management program for hypertension and dyslipidemia. J. Am. Pharm. Assoc. 2008, 48, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Erhun, W.O.; Agbani, E.O.; Bolaji, E.E. Positive benefits of a pharmacist-managed hypertension clinic in Nigeria. Public health 2005, 119, 792–798. [Google Scholar] [CrossRef]
- Park, J.J.; Kelly, P.; Carter, B.L.; Burgess, P.P. Comprehensive Pharmaceutical Care in the Chain Setting: Drug therapy monitoring and counseling by pharmacists contributed to improved blood pressure control in study patients. J. Am. Pharm. Assoc. 1996, 36, 443–451. [Google Scholar]
- Sookaneknun, P.; Richards, R.M.; Sanguansermsri, J.; Teerasut, C. Pharmacist involvement in primary care improves hypertensive patient clinical outcomes. Ann. Pharmacother. 2004, 38, 2023–2028. [Google Scholar] [CrossRef]
- Aguiar, P.M.; Balisa-Rocha, B.J.; Brito, G.C.; Lyra, D.P. Pharmaceutical care program for elderly patients with uncontrolled hypertension. J. Am. Pharm. Assoc. 2012, 52, 515–518. [Google Scholar] [CrossRef]
- Aguwa, C.N.; Ukwe, C.V.; Ekwunife, O.I. Effect of pharmaceutical care programme on blood pressure and quality of life in a Nigerian pharmacy. Pharm. World Sci. 2008, 30, 107–110. [Google Scholar] [CrossRef]
- Bex, S.D.; Boldt, A.S.; Needham, S.B.; Bolf, S.M.; Walston, C.M.; Ramsey, D.C.; Schmelz, A.N.; Zillich, A.J. Effectiveness of a hypertension care management program provided by clinical pharmacists for veterans. Pharmacotherapy 2011, 31, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Borenstein, J.E.; Graber, G.; Saltiel, E.; Wallace, J.; Ryu, S.; Jackson, A.; Deutsch, S.; Weingarten, S.R. Physician-pharmacist comanagement of hypertension: A randomized, comparative trial. Pharmacotherapy 2003, 23, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Carter, B.L.; Barnette, D.J.; Chrischilles, E.; Mazzotti, G.J.; Asali, Z.J. Evaluation of hypertensive patients after care provided by community pharmacists in a rural setting. Pharmacotherapy 1997, 17, 1274–1285. [Google Scholar]
- Carter, B.L.; Coffey, C.S.; Ardery, G.; Uribe, L.; Ecklund, D.; James, P.; Egan, B.; Vander Weg, M.; Chrischilles, E.; Vaughn, T. Cluster-randomized trial of a physician/pharmacist collaborative model to improve blood pressure control. Circ. Cardiovasc. Qual. Outcomes 2015, 8, 235–243. [Google Scholar] [CrossRef] [PubMed]
- Chabot, I.; Moisan, J.; Grégoire, J.P.; Milot, A. Pharmacist intervention program for control of hypertension. Ann. Pharmacother. 2003, 37, 1186–1193. [Google Scholar] [CrossRef]
- Júnior, D.P.L.; Marcellini, P.S.; Pelá, I.R. Effect of pharmaceutical care intervention on blood pressure of elderly outpatients with hypertension. Rev. Bras. Cienc. Farm. 2008, 44, 451–457. [Google Scholar] [CrossRef]
- Firmino, P.Y.; Vasconcelos, T.O.; Ferreira, C.C.; Moreira, L.M.; Romero, N.R.; Dias, L.A.; Queiroz, M.G.; Lopes, M.V.; Fonteles, M.M. Cardiovascular risk rate in hypertensive patients attended in primary health care units: The influence of pharmaceutical care. Braz. J. Pharm. Sci. 2015, 51, 617–627. [Google Scholar] [CrossRef]
- Garçao, J.A.; Cabrita, J. Evaluation of a pharmaceutical care program for hypertensive patients in rural Portugal. J. Am. Pharm. Assoc. 2002, 42, 858–864. [Google Scholar] [CrossRef]
- Hirsch, J.D.; Steers, N.; Adler, D.S.; Kuo, G.M.; Morello, C.M.; Lang, M.; Singh, M.; Wood, Y.; Kaplan, R.M.; Mangione, C.M. Primary care–based, pharmacist–physician collaborative medication-therapy management of hypertension: A randomized, pragmatic trial. Clin. Ther. 2014, 36, 1244–1254. [Google Scholar] [CrossRef]
- Hussain, T.; Franz, W.; Brown, E.; Kan, A.; Okoye, M.; Dietz, K.; Taylor, K.; Carson, K.A.; Halbert, J.; Dalcin, A.; et al. The role of care management as a population health intervention to address disparities and control hypertension: A quasi-experimental observational study. Ethn. Dis. 2016, 26, 285. [Google Scholar] [CrossRef]
- Kicklighter, C.E.; Nelson, K.M.; Humphries, T.L.; Delate, T. An evaluation of a clinical pharmacy-directed intervention on blood pressure control. Pharm. Pratic. 2006, 4, 110. [Google Scholar]
- Ortellado, G.L.; Bittner, M.R.; Chávez, H.; Pérez, S. Implementación de un Programa de Atención Farmacéutica en Farmacias Comunitarias para la detección de la Hipertensión Arterial y su Seguimiento Farmacoterapéutico. Lat. Am. J. Pharm. 2007, 26, 590–595. [Google Scholar]
- Morgado, M.; Rolo, S.; Castelo-Branco, M. Pharmacist intervention program to enhance hypertension control: A randomised controlled trial. Int. J. Clin. Pharm. 2011, 33, 132–140. [Google Scholar] [CrossRef] [PubMed]
- Parker, C.P.; Cunningham, C.L.; Carter, B.L.; Vander Weg, M.W.; Richardson, K.K.; Rosenthal, G.E. A Mixed-Method Approach to Evaluate a Pharmacist Intervention for Veterans with Hypertension. J. Clin. Hypertens. 2014, 16, 133–140. [Google Scholar] [CrossRef]
- Reid, F.; Murray, P.; Storrie, M. Implementation of a pharmacist-led clinic for hypertensive patients in primary care–a pilot study. Pharm. World Sci. 2005, 27, 202–207. [Google Scholar] [CrossRef]
- Skowron, A.; Polak, S.; Brandys, J. The impact of pharmaceutical care on patients with hypertension and their pharmacists. Pharm. Pract. 2011, 9, 110–115. [Google Scholar] [CrossRef]
- Stewart, K.; George, J.; Mc Namara, K.P.; Jackson, S.L.; Peterson, G.M.; Bereznicki, L.R.; Gee, P.R.; Hughes, J.D.; Bailey, M.J.; Hsueh, Y.S.; et al. A multifaceted pharmacist intervention to improve antihypertensive adherence: A cluster-randomized, controlled trial (HAPPy trial). J. Clin. Pharm. Ther. 2014, 39, 527–534. [Google Scholar] [CrossRef]
- Taylor, S.D.; Frazier, M.; Shimp, L.A.; Boyd, E.L. Implementing pharmaceutical care in an inner city pharmacy: Hypertension management and elderly African Americans. J. Aging Pharmacother. 2003, 13, 63–76. [Google Scholar] [CrossRef]
- Tsuyuki, R.T.; Houle, S.K.; Charrois, T.L.; Kolber, M.R.; Rosenthal, M.M.; Lewanczuk, R.; Campbell, N.R.; Cooney, D.; McAlister, F.A. A randomized trial of the effect of pharmacist prescribing on improving blood pressure in the community: The Alberta clinical trial in optimizing hypertension (RxACTION). Circulation 2015, 132, 93–100. [Google Scholar] [CrossRef]
- Vivian, E.M. Improving blood pressure control in a pharmacist-managed hypertension clinic. Pharmacotherapy 2002, 22, 1533–1540. [Google Scholar] [CrossRef]
- Wang, J.; Wu, J.; Yang, J.; Zhuang, Y.; Chen, J.; Qian, W.; Tian, J.; Chen, X.; She, D.; Peng, F. Effects of pharmaceutical care interventions on blood pressure and medication adherence of patients with primary hypertension in China. Clin. Res. Regul. Aff. 2011, 28, 1–6. [Google Scholar] [CrossRef]
- Bajorek, B.; Lemay, K.S.; Magin, P.; Roberts, C.; Krass, I.; Armour, C.L. Implementation and evaluation of a pharmacist-led hypertension management service in primary care: Outcomes and methodological challenges. Pharm. Pract. 2016, 14, 723. [Google Scholar] [CrossRef] [PubMed]
- Carter, B.L.; Vander Weg, M.W.; Parker, C.P.; Goedken, C.C.; Richardson, K.K.; Rosenthal, G.E. Sustained blood pressure control following discontinuation of a pharmacist intervention for Veterans. J. Clin. Hypert 2015, 17, 701–708. [Google Scholar] [CrossRef] [PubMed]
- Zillich, A.J.; Jaynes, H.A.; Bex, S.D.; Boldt, A.S.; Walston, C.M.; Ramsey, D.C.; Sutherland, J.M.; Bravata, D.M. Evaluation of pharmacist care for hypertension in the Veterans Affairs patient-centered medical home: A retrospective case-control study. Am. J. Med. 2015, 128, 539-e1. [Google Scholar] [CrossRef][Green Version]
- Abdel-Hameed, E.I.M.; Ali, Z.T.; Ghobary, M.A.F. Blood pressure control in hypertensive patients: Impact of an Egyptian pharmaceutical care model. J. Appl. Pharm. Sci. 2014, 4, 93–101. [Google Scholar]
- Fikri-Benbrahim, N.; Faus, M.J.; Martínez-Martínez, F.; González-Segura, A.D.; Sabater-Hernández, D. Effect of a pharmacist intervention in Spanish community pharmacies on blood pressure control in hypertensive patients. Am. J. Health-System Pharm. 2012, 69, 1311–1318. [Google Scholar] [CrossRef]
- Oparah, A.C.; Adje, D.U.; Enato, E.F. Outcomes of pharmaceutical care intervention to hypertensive patients in a Nigerian community pharmacy. Int. J. Pharm. Pract. 2006, 14, 115–122. [Google Scholar] [CrossRef]
- Erickson, S.R.; Slaughter, R.; Halapy, H. Pharmacists’ ability to influence outcomes of hypertension therapy. Pharmacotherapy 1997, 17, 140–147. [Google Scholar]
- Modé, C.L.; Lima, M.M.; Carnavalli, F.; Trindade, A.B.; Almeida, A.E.; Chin, C.M.; Santos, J.L. Atenção Farmacêutica em pacientes hipertensos: Um estudo piloto. Rev. Ciênc Farm. Básica Apl. 2015, 36, 35–41. [Google Scholar]
- Lee, V.W.; Yi, P.T.; Kong, K.W.; Chan, P.K.; Kwok, F.L. Impact of pharmacy outreach services on blood pressure management in the elderly community of Hong Kong. Geriatr. Gerontol. Int. 2013, 13, 175–181. [Google Scholar] [CrossRef]
- Robinson, J.D.; Segal, R.; Lopez, L.M.; Doty, R.E. Impact of a pharmaceutical care intervention on blood pressure control in a chain pharmacy practice. Ann. Pharmacother. 2010, 44, 88–96. [Google Scholar] [CrossRef] [PubMed]
- Hunt, J.S.; Siemienczuk, J.; Pape, G.; Rozenfeld, Y.; MacKay, J.; LeBlanc, B.H.; Touchette, D. A randomized controlled trial of team-based care: Impact of physician-pharmacist collaboration on uncontrolled hypertension. J. Gen. Intern. Med. 2008, 23, 1966–1972. [Google Scholar] [CrossRef] [PubMed]
- Tobari, H.; Arimoto, T.; Shimojo, N.; Yuhara, K.; Noda, H.; Yamagishi, K.; Iso, H. Physician–pharmacist cooperation program for blood pressure control in patients with hypertension: A randomized-controlled trial. Am. J. Hypertens. 2010, 23, 1144–1152. [Google Scholar] [CrossRef] [PubMed]
- Cazarim, M.S.; Freitas, O.; Penaforte, T.R.; Achcar, A.; Pereira, L.R.L. Impact Assessment of Pharmaceutical Care in the Management of Hypertension and Coronary Risk Factors after Discharge. PLoS ONE 2016, 11, e0155204. [Google Scholar] [CrossRef] [PubMed]
- Downs, S.H.; Black, N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J. Epidemiol. Community Health 1998, 52, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Portney, L.G. Foundations of Clinical Research: Applications to Evidence-Based Practice, 4th ed.; FA Davis: Philadelphia, PA, USA, 2020; p. 1298. [Google Scholar]
- Santschi, V.; Chiolero, A.; Colosimo, A.L.; Platt, R.W.; Taffé, P.; Burnier, M.; Burnand, B.; Paradis, G. Improving blood pressure control through pharmacist interventions: A meta-analysis of randomized controlled trials. J. Am. Hear. Assoc. 2014, 3, e000718. [Google Scholar] [CrossRef]
- Porzsolt, F.; Wiedemann, F.; Becker, S.I.; Rhoads, C.J. Inclusion and exclusion criteria and the problem of describing homogeneity of study populations in clinical trials. BMJ 2019, 24, 92–94. [Google Scholar] [CrossRef]
- Franco, L.J.; Passos, A.D.C. Fundamentos de Epidemiologia, 3rd ed.; Manole: Barueri, SP, Brazil, 2021; p. 421. [Google Scholar]
- Xia, T.L.; Huang, F.Y.; Peng, Y.; Huang, B.-T.; Pu, X.-B.; Yang, Y.; Chai, H.; Chen, M. Efficacy of different types of exercise-based cardiac rehabilitation on coronary heart disease: A network meta-analysis. J. Gen. Int. Med. 2018, 33, 2201–2209. [Google Scholar] [CrossRef]
- Aguiar, P.M.; Balisa-Rocha, B.J.; Brito, G.D.; Silva, W.B.; Machado, M.; Lyra, D.P., Jr. Pharmaceutical care in hypertensive patients: A systematic literature review. Res. Soc. Adm. Pharm. 2012, 8, 383–396. [Google Scholar] [CrossRef]
- Pessoa, L.D.; Borges, R.T.N.; Ribeiro, V.S.; Rios, C.C.; Bottacin, W.E.; de Fátima Bonetti, A.; de Souza, T.T.; Reis, W.C.T. Impacto do cuidado farmacêutico em pacientes com hipertensão arterial sistêmica. Braz. J. Dev. 2021, 7, 5849–5861. [Google Scholar] [CrossRef]
- Houle, S.K.; Chuck, A.W.; McAlister, F.A.; Tsuyuki, R.T. Effect of a Pharmacist-Managed Hypertension Program on Health System Costs: An Evaluation of the Study of Cardiovascular Risk Intervention by Pharmacists—Hypertension (SCRIP-HTN). Pharmacotherapy 2012, 32, 527–537. [Google Scholar] [CrossRef] [PubMed]
- Brazil—Federal Council of Pharmacy. Pharmaceutical Services Directly Aimed at the Patient, the Family and the Community: Contextualization and Conceptual Framework; Federal Council of Pharmacy: Brasília, DF, Brazil, 2016; p. 200. [Google Scholar]
- Feldman, J.D.; Otting, R.I.; Otting, C.M.; Witry, M.J. A community pharmacist–led service to facilitate care transitions and reduce hospital readmissions. JAPhA 2018, 58, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Brazil—Ministry of Health. Portaria n° 4.279 de 30 de Dezembro de 2010. Estabelece as Diretrizes para a Organização da Rede de Atenção à Saúde no Âmbito do Sistema Único de Saúde (SUS); Ministry of Health: Brasília, DF, Brazil, 2010. [Google Scholar]
- Polgreen, L.A.; Han, J.; Carter, B.L.; Ardery, G.P.; Coffey, C.S.; Chrischilles, E.; James, P.A. Cost-effectiveness of a physician–pharmacist collaboration intervention to improve blood pressure control. Hypertension 2015, 66, 1145–1151. [Google Scholar] [CrossRef]
- Cazarim, M.S.; Pereira, L.R.L. Cost-effectiveness analysis of pharmaceutical care for hypertensive patients from the perspective of the public health system in Brazil. PLoS ONE 2018, 13, e0193567. [Google Scholar] [CrossRef]
- Correr, C.J.; Otuki, M.F.; Soler, O. Assistência farmacêutica integrada ao processo de cuidado em saúde: Gestão clínica do medicamento. Rev. Pan-Amaz. Saúde 2011, 2, 41–49. [Google Scholar] [CrossRef]
- Assumpção, J.; Reis, S.L.; Batista, A.P.; Souza, L.F.A.; Reis, A.C.J.; Colacite, J. Pharmaceutical Care in Primary Care in Brazil compared to Spain and the United Kingdom–Literary review. Res. Soc. Dev. 2022, 11, e95111335029. [Google Scholar] [CrossRef]
- Curfman, G.; Bauchner, H.; Greenland, P. Treatment and control of hypertension in 2020: The need for substantial improvement. JAMA 2020, 324, 1166–1167. [Google Scholar] [CrossRef]
- Zhou, B.; Perel, P.; Mensah, G.A.; Ezzati, M. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat. Rev. Cardiol. 2021, 18, 785–802. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; John Wiley & Sons: Chichester, UK, 2019. [Google Scholar]
- Pagano, M.; Gauvreau, M. Princípios de Bioestatística, 2nd ed.; Cengage Learning: São Paulo, SP, Brazil, 2012; p. 506. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).