The Effects of Green Tea Catechins in Hematological Malignancies
Abstract
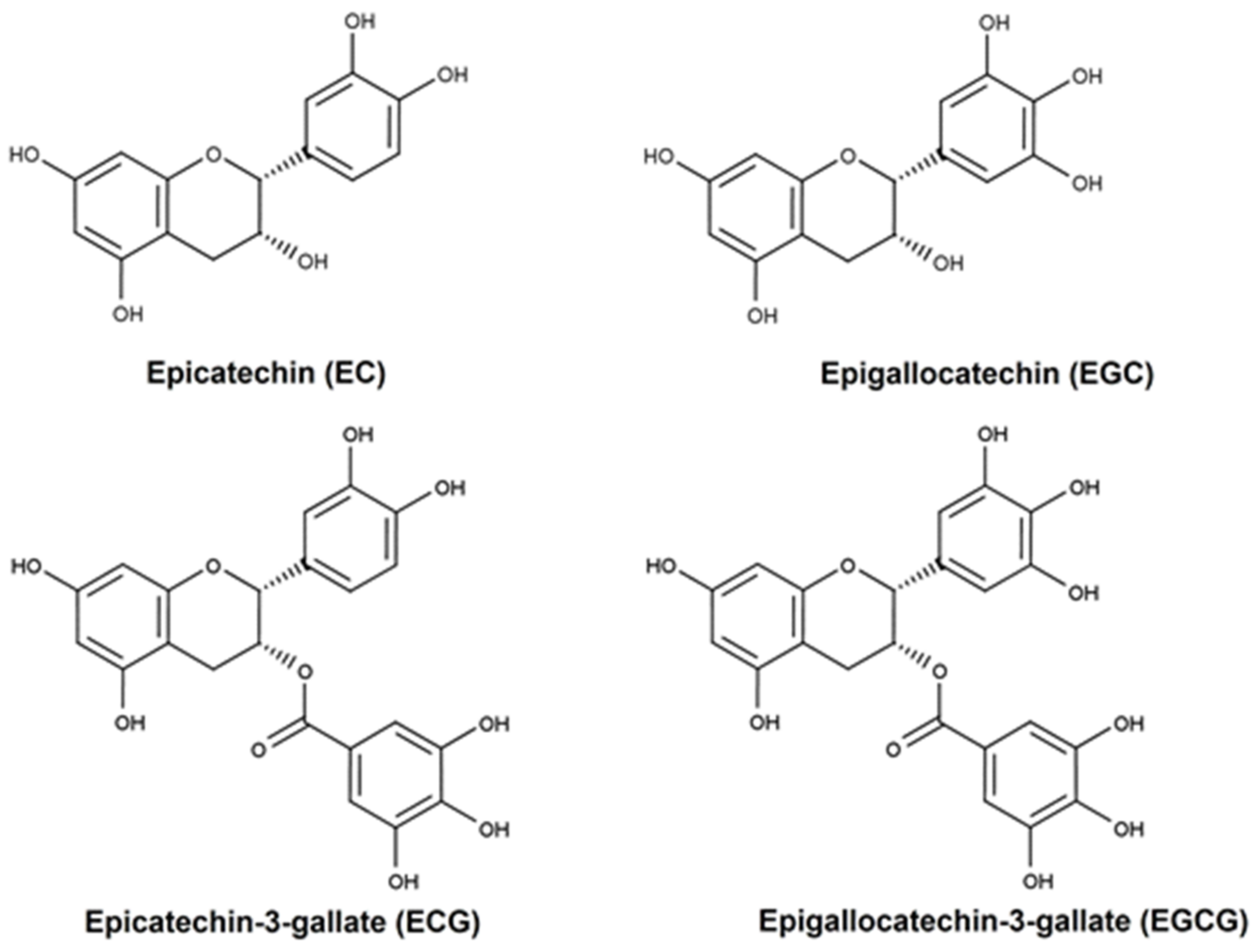
:1. Green Tea
2. Induction of Cell Death in Acute Leukemias by Green Tea Catechins
| Model | Compound/Component | Effect | Reference |
|---|---|---|---|
| In vitro | |||
| MOLT 4B | C, EC, ECG, EGC and EGCG 0.025–0.100 mM (3 days) | Inhibited the growth and apoptosis detected by DNA fragmentation and morphological change and inhibited the ornithine decarboxylase (ODC) activity (↓) | [36] |
| Leukemia blast cells from AML patients HEL | EGCG 0–100 nM (8–72 h) | Inhibited proliferation and the effects of TNFα or TPA (↓) and down modulated c-Kit (↓) | [15] |
| HL60 | Tea polyphenols 60–4000 µg/mL (5–48 h) | Induced apoptosis detected by internucleosomal DNA degradation, DNA ladder and apoptotic vehicles | [34] |
| U937 | EGCG 100–400 µM (16 h) | Induced apoptosis detected by formation of DNA ladder, chromatin condensation and apoptotic bodies | [48] |
| U937 | EGCG 100–400 µM (6–16 h) | Induced apoptosis (DNA fragmentation) | [49] |
| U937 JURKAT | EGCG IC50 = 26.0 µM (12 h) IC50 = 25.3 µM (12 h) | Inhibited cell growth (↓ ATP content), induction of apoptosis (morphological changes, chromosome condensation and DNA fragmentation ladder) | [46] |
| Peripheral blood T-lymphocytes of acute T-cell leukemia patient KODV | Tea (green tea polyphenols) EGCG 3-27 µg/mL (3 days) | Inhibited cell growth, induction of apoptosis (DNA fragmentation) and suppression of HTLV-1 pX mRNA | [44] |
| HL60 JURKAT K562 | EGC 50 µg/mL (2–24 h) | Induced apoptosis (DNA fragmentation and PARP cleavage) | [30] |
| U937 | EGCG 200 and 400 µM (0–16 h) | Induced apoptosis (formation of apoptotic bodies, DNA ladder formation, ↑ caspase 8 activity and interaction with Fas) | [23] |
| U937 | EGCG and GHF (high molecular weight fraction from green tea) EGCG—200 µM IC50 = 49 µM GHF 1.2 mg/mL IC50 = 0.61 mg/mL (20 h) | Induced apoptosis (formation of apoptotic bodies and DNA ladder formation) | [22] |
| HL60 | EGCG | Induced apoptosis (internucleosomal DNA fragmentation) and decreased activities of MnSOD and CuZnSOD | [32] |
| L1210 | EGCG 200 µM (24 h) | Induced apoptosis (DNA ladder) | [52] |
| NALM6 Health human lymphocytes | EGCG 10–100 µM (24 h) | Reduced viability by DNA damage and PAR formation (poly (APD-ribosyl) (↑)) | [37] |
| K562 V-79 | EGCG 50–500 µM (1–48 h) | Inhibited cell growth (↓ thymidine incorporation) and induction of apoptosis (chromatin condensation, nuclear and DNA fragmentation and ↑ caspase 3 and 8 activity) Protection of normal cells from genotoxic or carcinogenic assault | [47] |
| WEHI-3B JCS | EGCG 0–40 µM (48 h) IC50 = 16.8–31.0 µM | Inhibited proliferation (↓ thymidine incorporation), the ability to form colonies and induce apoptosis (formation of DNA ladder, condensed and fragmented nuclear structure) | [50] |
| JURKAT | EGCG and synthetic analogs of EGCG (with modification in the A-ring, C-ring or ester bond) 0–2.5 µM (0–24 h) | Induced apoptosis by inhibiting proteasomal activity (DNA fragmentation) Induced cycle arrest (↑ G1 population, ↑ sub-G1 DNA cell population) | [56] |
| JURKAT NIH/3T3 | EGCG and green tea extract 0–50 µM (0–48 h) | Induced apoptosis by inhibiting proteasomal chymotrypsin-like activity (↑ ubiquitinated proteins, PARP cleavage and caspase-3/-7 activation) | [38] |
| Primary chronic lymphocytic leukemia B-cells Human splenic B-cells | EGCG 0–40 µg/mL (24 h) | Induced apoptosis (caspase 3 activation, PARP cleavage); suppression of Bcl-2, XIAP and Mcl-1 (↓) and VEGF-R1 and VEGF-R2 phosphorylation (↓) | [43] |
| Primary chronic lymphocytic leukemia B-cells Human splenic B-cells | EGCG 3.12–25 µg/mL (24 h) | Induced apoptosis, inhibition of VEGF receptor activation, ↓ levels of serine p-STAT3 and ↓ Mcl-1 and XIAP | [42] |
| HL60 K652 | Green tea (GT)/EGCG 0–1000 µg/mL (24 h) IC50 HL60 GT = 375/EGCG = 60 K562 GT = 400/EGCG = 58 | Induced apoptosis (chromatin condensation, nuclear fragmentation, apoptotic bodies, cell shrinkage and ↓ thymidine incorporation in nuclear DNA) | [25] |
| HL60 K562 | EGCG 0–100 µg/mL (24 h) | Induced apoptosis (chromatin condensation, nuclear fragmentation, DNA fragmentation, caspase-3/-8 activation, ↓ Bcl-2 ↑ Bax) | [35] |
| UF-1 NB4 Fresh cells from patients with AML | EGCG 100 µM (0–24 h) IC50 = 50 µM | ROS production, induced apoptosis: mitochondrial dysfunction; release of cytocromo C; Bax ↑, Blc-2 and survivin ↓; caspase-3 ↑; PARP cleavage; DNA ladder. Induced cycle arrest—↑ G1 phase and ↓ S phase; ↑ expression of p21 and p27 | [26] |
| IM9, RPMI8226 and U266 HS-sultan Bone marrow samples from multiple myeloma | EC, ECG, EGC and EGCG 0–100 µmol/L (0–72 h) IC50 (EGCG) HS-sultan 17 µmol/L IM9 20 µmol/L | Induced apoptosis through ROS production (↑): mitochondrial dysfunction—loss of Δψm (↓); release of cytocromo C, Smac/DIABLO and AIF; Bax ↑, Blc-2 and Mcl-1↓; caspase-3 and -9 ↑; morphologic changes—condensed chromatin, nuclei fragmented and apoptotic bodies; and DNA ladder EGCG (10 µmol/L) + AS2O3 (2 µmol/L) intensified apoptosis and the production of ROS Induced cycle arrest—↑ G1 phase and ↓ S phase | [45] |
| U937 | EGCG 100 µM (8–24 h) GHF (high molecular weight fraction of green tea) 0.6 mg/mL (8–24 h) | Induced apoptosis (DNA fragmentation) GHF also induced cycle arrest (↑ G2/M, ↑ p21/Waf1 (mRNA and protein expression) | [28] |
| K562 | Green tea extract 100 mg/mL (0–24 h) | Induced apoptosis (chromatin condensation, nuclear fragmentation, DNA fragmentation, ↓ Bcl-2, ↑Bax and caspase-3/-8 activation) Induction of cycle arrest (↑ sub G1 peak, ↓DNA content of G1 phase) | [17] |
| K562 U937 Primary leukemic cells—CML and ALL (Ph+) Normal WBC | TRE—tea (Camellia sinensis var assamica) root extract 0–15 µg/mL | Induced apoptosis (↓ the rate of cellular DNA synthesis—↓ thymidine incorporation, DNA degradation, apoptotic bodies and membrane blebbing) Induced cell cycle arrest (↑ content of hypoploid DNA and ↓ content DNA in G0/G1 phases—U937 or ↓ cells in S or G2/M phases—K562) | [19] |
| RAJI | EGCG and synthetic analogs of EGCG (a para-amino group on the D-ring) 25 µM (4–24 h) | Induced apoptosis (caspase-3 activation, PARP cleavage) and inhibition of proteasome activity (accumulation of proteasome target protein, like Bax, Iκb-α and p27) | [11] |
| MPO-positive myeloid leukemia cell lines: HL60, KASUMI, NB4 and UF-1 MPO-negative myeloid leukemia cell lines: KG1, K652, THP-1 and U937 | EGCG 0–300 µM (30 min–48 h) | Induced apoptosis in MPO-sensitive leukemia cells through ROS production | [27] |
| HL60 K562 | EGCG and 5-AZA-CdR | Induced apoptosis through mitochondrial dysfunction—loss of Δψm (↓) and modulation of Bcl-xl (↓) and BAX | [57] |
| HTLV-I-positive ATL cell line: C91-PL HuT-102 HTLV-I-negative cell line: CEM JURKAT | EGCG 0-400 µM (0–96 h) IC50 (48 h) C91-PL= 310 µM HuT-102 = 350 µM CEM = 272 µM Jurkat = 378 µM | Induced apoptosis (DNA fragmentation, ↑ pre-G1 phase cells, ↑ p21, p53 and Bax, ↓ Bcl-2α, ↓ TGF-α—cytokine with proliferative activities, ↑ TGF-β2—anti-proliferative and apoptotic effects; DNA fragmentation) | [40] |
| HL60 undifferentiated | EGCG 50 µM (4 h) | Induced apoptosis detected through the formation of apoptotic bodies and DNA ladder | [29] |
| HL60 V79-4 | GTP 0–300 µg/mL (0–72 h) IC50 = 49.5 µg/mL (48 h) IC50 = 50.0 µg/mL (72 h) | Induction of apoptosis detected by nuclear fragmentation; Bcl-2 ↓; PARP cleavage (↑) and pro-caspase-3 ↓ Induced cycle arrest—↑ sub-G1 phase No cytotoxic effects in V79-4 with GTP (48 h) | [21] |
| HL60 V79-4 | EGCG and EGC 50 µM (24–48 h) EGCG IC50 = 60 µM (48 h) IC50 = 57.7 µM (72 h) EGC IC50 =107.7 µM (48 h) IC50 = 97.5 µM (72 h) | Induced apoptosis detected through nuclear fragmentation; Bcl-2; and pro-caspase-3 ↓ EGCG > EGC No cytotoxic effects in V79-4 with EGCG or EGC (48 h) | [20] |
| Primary AML blasts cells HL-60 NB4 | EGCG 0–40 µmol/L (24–36 h) IC50 = 21.5 µmol/L (24–36 h) IC50 = 30.5 µmol/L (24–36 h) | Induced apoptosis detected by ↑ of DAPK2 and the level of 67LR expression | [16] |
| NB4 NB4 R1 NB4 R2 Primary APL/leukemia cells | Catechins 0–400 µM (0–48 h) IC50 < 125 | Induced apoptosis through ROS production (↑): mitochondrial dysfunction—loss of Δψm; release cytocromo C; Blc-xL ↓; caspase-3, -8 and -9 ↑; PARP cleavage (↑); morphologic changes—condensed chromatin, nuclei fragmented and apoptotic bodies; and ↓ PML/RARα | [33] |
| NB4 | EGCG 0-40 µM (24 h) | Induced apoptosis through the SHP-1-p38αMAPK-Bax cascade (↑ Bax, SHP-1 (Src homology 1 domain-containing protein tyrosine phosphatase) expression and levels of phosphorylated (p)-p38α MAPK) | [18] |
| JURKAT | EGCG 0–100 µM (0–72 h) IC50 = 82.8 ± 3.1 µM 24 h 68.8 ± 4.0 µM 48 h 59.7 ± 4.8 µM 72 h | Induced apoptosis through Fas/Fas ligand activation: ↑ Fas expression and caspase-3 ↑ | [39] |
| K562 K652R KCL-22 BaF3/p210 BaF3/p210T3151 Primary bone marrow CML cells | EGCG 0–100 µmol/L (0–48 h) IC50 = 62.62 µmol/L K562 91.12 µmol/L K562R 53.76 µmol/L KCL-22 12.80 µmol/L BaF3/p210 29.82 µmol/L BaF3/p210T3151 | Induced apoptosis by regulating Bcr/Abl (degradation)-mediated JAK2/STAT3/AKT (↓) and p38-MAPK/JNK (↓) signaling pathways. Induced autophagy function (↑ Atg5 and LC3), as well as ↓ MMP (mitochondrial membrane potential), ↑ HSP60 (mitochondrial protein marker), histone H3 and AIF (apoptosis-inducing factor) | [51] |
| HL60 | EGCG 100 µM (5 days) IC50 = 190.4 ± 0.03 µM (5 days) | Induced apoptosis, ↓ AKT and ↑ CASP3, CASPP8, p21 and PTEN gene expression; ↓ ABCB1 and ABCC1 (genes of multi-drug resistance) | [24] |
| In vivo—Xenograft and systemics model | |||
| Murine myeloid leukemia WEHI-3B JCS cells pre incubated with EGGC in Balb/c mice (injected i.p.) | EGCG 40 µM (4 h) | Reduction in the tumorigenicity—↓ the leukemic cell growth | [50] |
| APL cells (UF-1) in Nod. Scid mice (xenografted) | EGCG 10 mM as the sole drink for 12 days | Reduction in tumor weight and inhibition of cell proliferation. During the treatment, the mice appeared healthy, and there was no change in the tissue organs | [26] |
| APL cells (NB4) in Nude mice (xenografted) | Catechins 10 mM as the sole drink for 21 days | Reduction in tumor weight and induction of apoptosis During the treatment, the mice appeared healthy, and there was no infiltration in any of the organs | [33] |
| APL cells (HL60) in NOD. CB17-Prkdcscid/J mice (xenografted) | GT 100 mg/kg as gavage | Reduction in tumor weight and induction of apoptosis (↑ cytochrome c ↓ Bcl-2, ↑ Bax and pJNK, ↑ caspase 3), cell cycle arrest (↓ CDK2 and cyclin A and ↑ p21) and autophagy (↑ LC3-II) | [54] |
| hCG-PML/RAR transgenic mice cells in NOD. CB17-Prkdcscid/J mice | GT 250 mg/kg/d intraperitoneally, for 5 days | Reduction in spleen weight and induction of apoptosis of blasts in spleen and bone marrow (↑ of caspase-3, -8 and -9) and ↓ CXCR4/HIF-1α pathway in response to ↓ ROS levels | [55] |
| hCG-PML/RAR transgenic mice cells in NOD. CB17-Prkdcscid/J mice | EGCG 25 mg/kg/d intraperitoneally, for 5 days | Reduction in spleen weight and induction of apoptosis of spleen cells by modulating Bax (↑), Bad (↑), Bcl-2 (↓) and c-Myc (↓) | [7] |
3. Pro-Oxidant or Antioxidants Effects of Green Tea Catechins
| Model | Compound/Component | Effect | Reference |
|---|---|---|---|
| In vitro | |||
| U937 | EGCG 400 µM (5–30 min) | Decreased levels of glutathione | [66] |
| HL60 | Catechins 1 µM (18 h) | Increased oxidative DNA damage augmenting the 8-oxodoG content | [67] |
| Jurkat | EGCG 12.5–50 µM (6 h) | Increased H2O2 levels | [68] |
| HL60 | EGCG 50 μM (1 h) | Decreased ROS levels, associated with an increase in apoptotic cells | [69] |
| UF-1 | EGCG 50 μM (3 h) | Increased ROS levels, loss of potential mitochondrial membrane | [26] |
| HS-Sultan RPMI8226 | EGCG 20 or 100 μM (1–4 h) | Increased ROS levels, loss of potential mitochondrial membrane, increased cytochrome c, Smac/DIABLO and AIF | [45] |
| Fresh myeloma cells from bone marrow from multiple myeloma patients | EGCG 20 μM (8 h) | Increased ROS levels associated with an increase in apoptotic cells | [45] |
| HL60 | EGCG 50 μM (24 h) | ROS production was blocked by antioxidants | [27] |
| Ramos | EGCG 40 or 80 μM (0.5–4 h) | Increased ROS levels, loss of mitochondrial transmembrane potential, increased release of cytochrome c to the cytosol | [70] |
| HL60 | EGCG 20 μM (1–2 h) | Increased ROS levels | [71] |
| HL60 | ECG 200 μM (2 h) | Inhibited chlorination of hypochlorous acid | [72] |
| JURKAT | EGCG 150 μM (1 h) | Increased depolarization on mitochondria | [74] |
| IM9 | EGCG 180 μM (9, 12 and 24 h) | Decreased protein levels of peroxiredoxin V | [73] |
| HPB-ALL | EGCG oxide 5, 10, 20, 40, 60 μM (12 h) | Inhibited proliferation associated with downregulation of Notch1 and Ki67 expression | [75] |
| NB4 | EGCG 12.5–50.0 μg/mL (2 h) | Increased ROS levels | [7] |
| In vivo—Xenograft and systemics model | |||
| hCG-PML/RAR transgenic mice cells in NOD. CB17-Prkdcscid/J mice | GT 250 mg/kg/d intraperitoneally, for 5 days | Increased intracellular ROS in Gr-1+ bone marrow cells and decreased intracellular ROS in CD34+ and CD117+ cells | [55] |
| hCG-PML/RAR transgenic mice cells in NOD. CB17-Prkdcscid/J mice | EGCG 25 mg/kg/d intraperitoneally, for 5 days | Increased ROS levels in bone marrow cells—CD34+, CD117+ and GR-1+ | [7] |
4. Epigenetics
4.1. DNA Methylation and Gene Regulation
4.2. Covalent Histone Modifications
5. Differentiation of Acute Promyelocytic Leukemia by Green Tea Catechins
6. Epidemiological Data and Clinical Trials with Green Tea
| Disease | Compound/Component | Effect | Reference |
|---|---|---|---|
| Prevention | |||
| AML Hospital-based case–control study (n = 111 cases and 439 controls) | Tea | Regular and high daily intake of tea reduced the risk of adult AML among males and females in New York | [112] |
| Leukemia Hospital-based case–control study (n = 107 cases and 110 orthopedic controls) | Green tea | The frequency, longer duration and higher quantity of green tea intake reduced the risk of ALL and CML/CLL in Southeast China | [119] |
| Leukemia Hospital-based matched case–control study (n = 107 cases and 110 inpatient controls) | Green tea | High consumption of green tea reduced the risk of adult leukemia | [120] |
| Leukemia Population-based case–control study (n = 252 cases and 637 controls) | Tea | The highest intake of tea, especially green tea, reduces the risk of leukemia in Southwestern Taiwan | [121] |
| AML NIH–AARP cohort (n = 338 cases and n = 491,163 people) | Tea | No association with consumption of tea and risk of leukemia in US | [115] |
| Childhood acute leukemia Population-based case–control study (n = 190 cases and 842 controls) | Tea | No association with consumption of tea and risk of leukemia in Southern Taiwan | [113] |
| Hematologic malignancies Population-based case–control study (n = 41,761) | Green tea | Green tea consumption reduces the risk of hematologic malignancies—lymphoid and myeloid neoplasms—in Japan | [116] |
| Leukemia Meta-analysis | Tea | High tea consumption reduces the risk of leukemia, indicating a protective role of tea against leukemia | [122] |
| De novo MDS Hospital-based case–control (n = 208 cases and 208 controls) | Tea | Regular and high intake of tea reduces the risk of MDS in China | [109] |
| Adult leukemia Hospital-based case–control (multicenter) (n = 442 cases and 442 outpatient controls) | Green tea | The regular daily intake of green tea reduces the risk of leukemia regardless of GSTM1 and GSTP1 polymorphic status in China | [[114] |
| AML and MDS Population-based cohort study (n = 95,807) | Green tea | No association between green tea consumption and the risk of MDS and AML in Japan | [110] |
| Adult leukemia Population-based cohort study (n = 651 cases and 1771 controls) | Tea | A protective effect of tea intake on the risk of AML in Italy | [117] |
| Hematologic neoplasm Community-based prospective study (n = 110,585 individuals) | Green tea | A protective effect of tea intake against hematologic neoplasm, specifically of AML and follicular lymphomas in Japan | [118] |
| Cancers Meta-analysis of observational studies. | Tea | The tea consumption was associated with a lower risk of cancer, like leukemia, showing a protective effect | [111] |
| Clinical trials | |||
| Patients with low-grade B-cells malignancies (n = 4) | Oral ingestion of products containing tea polyphenols by their own initiative | An objective clinical response | [124] |
| Asymptomatic Rai stage 0 to II CLL (phase I trial) (n = 33) | Polyphenon E—6 months 2000 mg twice per day | Reduction in absolute number of lymphocytes and lymphadenopathy in most patients | [125] |
| Asymptomatic Rai stage 0 to II CLL (phase II trial) (n = 42) | Polyphenon E—6 months 2000 mg twice per day | Reduction in absolute number of lymphocytes and lymphadenopathy in most patients | [126] |
| Patients with Rai stage 0 CLL (n = 12 per group) | Green tea extract—6 months four capsules/day for the first months and six capsules/day for the following 5 months (400 mg of green tea total concentrate per capsule) | Reduction in the absolute number of B-lymphocytes, circulating Treg cells and IL-10 and TGF-β serum levels | [127] |
| 48-year-old man with CLL (n = 1) | 1200 mg/day of EGCG | Patient achieved a complete clinical and molecular regression, 20 years after a diagnosis, without conventional therapy and using EGCG | [128] |
| Elderly acute myeloid leukemia patients with myelodysplasia-related changes (AML-MRCs) (n = 10) | Green tea extract—6 months (1000 mg/day—4 capsules/day) | Reduction in the immunosuppressive profile by ↓ Treg cells, CXCR4+ Treg cells and mRNA expression of TGF-β and IL4, and activation of cytotoxic phenotype by ↑ CD8+ T-cells, natural killer cells and classical monocytes in bone marrow and/or peripheral blood | [123] |
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CELL LINE | DISEASE/TYPE |
| BAF3/P210 | Human chronic myeloid leukemia |
| BAF3/P210T315L | Human chronic myeloid leukemia |
| C91-PL | Human T-lymphotropic virus 1 |
| CEM | Human acute T-lymphoblastic leukemia |
| HEL | Human acute myeloid leukemia |
| HL60 | Human acute myeloid leukemia |
| HPB-ALL | Human acute T-lymphoblastic leukemia |
| HS-SULTAN | Burkitt’s lymphoma cells |
| HUT-102 | Lymphoma |
| IMP9 | Human malignant B-cells |
| JURKAT | Humana acute T-cell leukemia |
| K562 | Human chronic myeloid leukemia |
| K652R | Human chronic myeloid leukemia resistant |
| KASUMI | Human acute myeloblastic leukemia |
| KCL-22 | Chronic myeloid leukemia |
| KG1 | Human acute myelogenous leukemia |
| L1210 | Mouse lymphocytic leukemia |
| MOLT 4B | Human lymphoid leukemia |
| NALM6 | Human acute lymphoblast leukemia |
| NB4 | Human promyelocytic leukemia with PML/RARα |
| NB4 R1 | Human promyelocytic leukemia with PML/RARα resistant to ATRA |
| NB4 R2 | Human promyelocytic leukemia with PML/RARα resistant to ATRA |
| NIH/3T3 | Mouse fibroblast |
| RAJI | Burkitt’s lymphoma cells |
| RAMOS | Burkitt’s lymphoma cells |
| RPMI-8226 | Chronic myeloid leukemia (human B-lymphocyte with plasmacytoma) |
| THP-1 | Human acute monocytic leukemia |
| U266 | Multiple myeloma (human B-lymphocyte with myeloma) |
| U937 | Human acute myeloid leukemia/ Human monocyte leukemia |
| UF-1 | Human promyelocytic leukemia with PML/RARα |
| V79-4 | Chinese hamster lung fibroblast cells |
| WEHI-3B JCS | Mouse myeloid leukemia |
| ↑ | Increase |
| ↓ | Decrease |
References
- Farhan, M. Green Tea Catechins: Nature’s Way of Preventing and Treating Cancer. Int. J. Mol. Sci. 2022, 23, 10713. [Google Scholar] [CrossRef] [PubMed]
- Kanwar, J.; Taskeen, M.; Mohammad, I.; Huo, C.; Chan, T.H.; Dou, Q.P. Recent Advances on Tea Polyphenols. Front. Biosci. 2012, E4, 111. [Google Scholar] [CrossRef] [PubMed]
- Parish, M.; Massoud, G.; Hazimeh, D.; Segars, J.; Islam, S. Green Tea in Reproductive Cancers: Could Treatment Be as Simple? Cancers 2023, 15, 862. [Google Scholar] [CrossRef]
- Trisha, A.T.; Shakil, M.H.; Talukdar, S.; Rovina, K.; Huda, N.; Zzaman, W. Tea Polyphenols and Their Preventive Measures against Cancer: Current Trends and Directions. Foods 2022, 11, 3349. [Google Scholar] [CrossRef]
- Yang, C.S.; Wang, X.; Lu, G.; Picinich, S.C. Cancer prevention by tea: Animal studies, molecular mechanisms and human relevance. Nat. Rev. Cancer 2009, 9, 429–439. [Google Scholar] [CrossRef] [Green Version]
- Tamfu, A.N.; Ceylan, O.; Kucukaydin, S.; Duru, M.E. HPLC-DAD phenolic profiles, antibiofilm, anti-quorum sensing and enzyme inhibitory potentials of Camellia sinensis (L.) O. Kuntze and Curcuma longa L. LWT 2020, 133, 110150. [Google Scholar] [CrossRef]
- Della Via, F.I.; Shiraishi, R.N.; Santos, I.; Ferro, K.P.; Salazar-Terreros, M.J.; Junior, G.C.F.; Rego, E.M.; Saad, S.T.O.; Torello, C.O. (–)-Epigallocatechin-3-gallate induces apoptosis and differentiation in leukaemia by targeting reactive oxygen species and PIN1. Sci. Rep. 2021, 11, 9103. [Google Scholar] [CrossRef]
- Forester, S.C.; Lambert, J.D. Antioxidant Effects of Green Tea. Mol. Nutr. Food Res. 2011, 55, 844. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.S.; Quon, M.J.; Kim, J.A. New Insights into the Mechanisms of Polyphenols beyond Antioxidant Properties; Lessons from the Green Tea Polyphenol, Epigallocatechin 3-Gallate. Redox Biol. 2014, 2, 187–195. [Google Scholar] [CrossRef] [Green Version]
- De Oliveira, M.R.; Nabavi, S.F.; Daglia, M.; Rastrelli, L.; Nabavi, S.M. Epigallocatechin Gallate and Mitochondria-A Story of Life and Death. Pharmacol. Res. 2016, 104, 70–85. [Google Scholar] [CrossRef]
- Osanai, K.; Landis-Piwowar, K.R.; Dou, Q.P.; Chan, T.H. A Para-Amino Substituent on the D-Ring of Green Tea Polyphenol Epigallocatechin-3-Gallate as a Novel Proteasome Inhibitor and Cancer Cell Apoptosis Inducer. Bioorg. Med. Chem. 2007, 15, 5076–5082. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carneiro, B.A.; El-Deiry, W.S. Targeting Apoptosis in Cancer Therapy. Nat. Rev. Clin. Oncol. 2020, 17, 395–417. [Google Scholar] [CrossRef]
- Pfeffer, C.M.; Singh, A.T.K. Apoptosis: A Target for Anticancer Therapy. Int. J. Mol. Sci. 2018, 19, 448. [Google Scholar] [CrossRef] [Green Version]
- Wong, R.S.Y. Apoptosis in Cancer: From Pathogenesis to Treatment. J. Exp. Clin. Cancer Res. 2011, 30, 87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Asano, Y.; Okamura, S.; Ogo, T.; Eto, T.; Otsuka, T.; Niho, Y. Effect of (-)-Epigallocatechin Gallate on Leukemic Blast Cells from Patients with Acute Myeloblastic Leukemia. Life Sci. 1996, 60, 135–142. [Google Scholar] [CrossRef]
- Britschgi, A.; Simon, H.U.; Tobler, A.; Fey, M.F.; Tschan, M.P. Epigallocatechin-3-Gallate Induces Cell Death in Acute Myeloid Leukaemia Cells and Supports All-Trans Retinoic Acid-Induced Neutrophil Differentiation via Death-Associated Protein Kinase 2. Br. J. Haematol. 2010, 149, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, S.; Kundu, T.; Dey, S.; Bhattacharya, R.K.; Siddiqi, M.; Roy, M. Tea-Induced Apoptosis in Human Leukemia K562 Cells as Assessed by Comet Formation. Asian Pac. J. Cancer Prev. 2006, 7, 201–207. [Google Scholar]
- Gan, L.; Zhong, L.; Shan, Z.; Xiao, C.; Xu, T.; Song, H.; Li, L.; Yang, R.; Liu, B. Epigallocatechin-3-Gallate Induces Apoptosis in Acute Promyelocytic Leukemia Cells via a SHP-1-P38α MAPK-Bax Cascade. Oncol. Lett. 2017, 14, 6314–6320. [Google Scholar] [CrossRef] [Green Version]
- Ghosh, P.; Besra, S.E.; Tripathi, G.; Mitra, S.; Vedasiromoni, J.R. Cytotoxic and Apoptogenic Effect of Tea (Camellia Sinensis Var. Assamica) Root Extract (TRE) and Two of Its Steroidal Saponins TS1 and TS2 on Human Leukemic Cell Lines K562 and U937 and on Cells of CML and ALL Patients. Leuk. Res. 2006, 30, 459–468. [Google Scholar] [CrossRef]
- Han, D.H.; Kim, J.H. Difference in Growth Suppression and Apoptosis Induction of EGCG and EGC on Human Promyelocytic Leukemia HL-60 Cells. Arch. Pharm. Res. 2009, 32, 543–547. [Google Scholar] [CrossRef]
- Han, D.H.; Jeong, J.H.; Kim, J.H. Anti-Proliferative and Apoptosis Induction Activity of Green Tea Polyphenols on Human Promyelocytic Leukemia HL-60 Cells. Anticancer. Res. 2009, 29, 1417–1421. [Google Scholar]
- Hayakawa, S.; Kimura, T.; Saeki, K.; Koyama, Y.; Aoyagi, Y.; Noro, T.; Nakamura, Y.; Isemura, M. Apoptosis-Inducing Activity of High Molecular Weight Fractions of Tea Extracts. Biosci. Biotechnol. Biochem. 2001, 65, 459–462. [Google Scholar] [CrossRef] [PubMed]
- Hayakawa, S.; Saeki, K.; Sazuka, M.; Suzuki, Y.; Shoji, Y.; Ohta, T.; Kaji, K.; Yuo, A.; Isemura, M. Apoptosis Induction by Epigallocatechin Gallate Involves Its Binding to Fas. Biochem. Biophys. Res. Commun. 2001, 285, 1102–1106. [Google Scholar] [CrossRef] [Green Version]
- Jokar, M.H.; Sedighi, S.; Moradzadeh, M. A Comparative Study of Anti-Leukemic Effects of Kaempferol and Epigallocatechin-3-Gallate (EGCG) on Human Leukemia HL-60 Cells. Avicenna J. Phytomed. 2021, 11, 314. [Google Scholar] [CrossRef] [PubMed]
- Kundu, T.; Bhattacharya, R.K.; Siddiqi, M.; Roy, M. Correlation of Apoptosis with Comet Formation Induced by Tea Polyphenols in Human Leukemia Cells. J. Environ. Pathol. Toxicol. Oncol. 2005, 24, 115–128. [Google Scholar] [CrossRef] [PubMed]
- Nakazato, T.; Ito, K.; Miyakawa, Y.; Kinjo, K.; Yamada, T.; Hozumi, N.; Ikeda, Y.; Kizaki, M. Catechin, a Green Tea Component, Rapidly Induces Apoptosis of Myeloid Leukemic Cells via Modulation of Reactive Oxygen Species Production in Vitro and Inhibits Tumor Growth in Vivo. Haematologica 2005, 90, 317–325. [Google Scholar]
- Nakazato, T.; Sagawa, M.; Yamato, K.; Xian, M.; Yamamoto, T.; Suematsu, M.; Ikeda, Y.; Kizaki, M. Myeloperoxidase Is a Key Regulator of Oxidative Stress-Mediated Apoptosis in Myeloid Leukemic Cells. Clin. Cancer Res. 2007, 13, 5436–5445. [Google Scholar] [CrossRef] [Green Version]
- Ohata, M.; Koyama, Y.; Suzuki, T.; Hayakawa, S.; Saeki, K.; Nakamura, Y.; Isemura, M. Effects of Tea Constituents on Cell Cycle Progression of Human Leukemia U937 Cells. Biomed. Res. 2005, 26, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Okada, N.; Tanabe, H.; Tazoe, H.; Ishigami, Y.; Fukutomi, R.; Yasui, K.; Isemura, M. Differentiation-Associated Alteration in Sensitivity to Apoptosis Induced by (-)-Epigallocatechin-3-O-Gallate in HL-60 Cells. Biomed. Res. 2009, 30, 201–206. [Google Scholar] [CrossRef] [Green Version]
- Smith, D.M.; Dou, Q.P. Green Tea Polyphenol Epigallocatechin Inhibits DNA Replication and Consequently Induces Leukemia Cell Apoptosis. Int. J. Mol. Med. 2001, 7, 645–652. [Google Scholar] [CrossRef]
- Henry, D.; Brumaire, S.; Hu, X. Involvement of PRb-E2F Pathway in Green Tea Extract-Induced Growth Inhibition of Human Myeloid Leukemia Cells. Leuk. Res. 2019, 77, 34–41. [Google Scholar] [CrossRef]
- Zhang, W.; Hashimoto, K.; Yu, G.Y.; Sakagami, H. Decline of Superoxide Dismutase Activity during Antioxidant-Induced Apoptosis in HL-60 Cells. Anticancer. Res. 2002, 22, 219–224. [Google Scholar] [PubMed]
- Zhang, L.; Chen, Q.S.; Xu, P.P.; Qian, Y.; Wang, A.H.; Xiao, D.; Zhao, Y.; Sheng, Y.; Wen, X.Q.; Zhao, W.L. Catechins Induced Acute Promyelocytic Leukemia Cell Apoptosis and Triggered PML-RARα Oncoprotein Degradation. J. Hematol. Oncol. 2014, 7, 75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, Y.; Cao, J.; Ma, H.; Liu, J. Apoptosis Induced by Tea Polyphenols in HL-60 Cells. Cancer Lett. 1997, 121, 163–167. [Google Scholar] [CrossRef] [PubMed]
- Kundu, T.; Dey, S.; Roy, M.; Siddiqi, M.; Bhattacharya, R.K. Induction of Apoptosis in Human Leukemia Cells by Black Tea and Its Polyphenol Theaflavin. Cancer Lett. 2005, 230, 111–121. [Google Scholar] [CrossRef]
- Achiwa, Y.; Hibasami, H.; Katsuzaki, H.; Imai, K.; Komiya, T. Inhibitory Effects of Persimmon (Diospyros Kaki) Extract and Related Polyphenol Compounds on Growth of Human Lymphoid Leukemia Cells. Biosci. Biotechnol. Biochem. 1997, 61, 1099–1101. [Google Scholar] [CrossRef]
- Bertram, B.; Bollow, U.; Rajaee-Behbahani, N.; Bürkle, A.; Schmezer, P. Induction of Poly(ADP-Ribosyl)Ation and DNA Damage in Human Peripheral Lymphocytes after Treatment with (−)-Epigallocatechin-Gallate. Mutat. Res. Genet. Toxicol. Environ. Mutagen. 2003, 534, 77–84. [Google Scholar] [CrossRef]
- Cheng, M.S.; Chen, D.; Ping, D.Q. Inhibition of Proteasome Activity by Various Fruits and Vegetables Is Associated with Cancer Cell Death. In Vivo 2004, 18, 73–80. [Google Scholar]
- Ghasemi-Pirbaluti, M.; Pourgheysari, B.; Shirzad, H.; Sourani, Z.; Beshkar, P. The Inhibitory Effect of Epigallocatechin Gallate on the Viability of T Lymphoblastic Leukemia Cells Is Associated with Increase of Caspase-3 Level and Fas Expression. Indian J. Hematol. Blood Transfus. 2018, 34, 253. [Google Scholar] [CrossRef]
- Harakeh, S.; Abu-El-Ardat, K.; Diab-Assaf, M.; Niedzwiecki, A.; El-Sabban, M.; Rath, M. Epigallocatechin-3-Gallate Induces Apoptosis and Cell Cycle Arrest in HTLV-1-Positive and -Negative Leukemia Cells. Med. Oncol. 2008, 25, 30–39. [Google Scholar] [CrossRef]
- Hibasami, H.; Achiwa, Y.; Fujikawa, T.; Komiya, T. Induction of Programmed Cell Death (Apoptosis) in Human Lymphoid Leukemia Cells by Catechin Compounds. Anticancer. Res. 1996, 16, 1943–1946. [Google Scholar] [PubMed]
- Lee, Y.K.; Shanafelt, T.D.; Bone, N.D.; Strege, A.K.; Jelinek, D.F.; Kay, N.E. VEGF Receptors on Chronic Lymphocytic Leukemia (CLL) B Cells Interact with STAT 1 and 3: Implication for Apoptosis Resistance. Leukemia 2005, 19, 513–523. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, Y.K.; Bone, N.D.; Strege, A.K.; Shanafelt, T.D.; Jelinek, D.F.; Kay, N.E. VEGF Receptor Phosphorylation Status and Apoptosis Is Modulated by a Green Tea Component, Epigallocatechin-3-Gallate (EGCG), in B-Cell Chronic Lymphocytic Leukemia. Blood 2004, 104, 788–794. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, H.C.; Yashiki, S.; Sonoda, J.; Lou, H.; Ghosh, S.K.; Byrnes, J.J.; Lema, C.; Fujiyoshi, T.; Karasuyama, M.; Sonoda, S. Green Tea Polyphenols Induce Apoptosis in Vitro in Peripheral Blood T Lymphocytes of Adult T-Cell Leukemia Patients. Jpn. J. Cancer Res. 2000, 91, 34–40. [Google Scholar] [CrossRef]
- Nakazato, T.; Ito, K.; Ikeda, Y.; Kizaki, M. Green Tea Component, Catechin, Induces Apoptosis of Human Malignant B Cells via Production of Reactive Oxygen Species. Clin. Cancer Res. 2005, 11, 6040–6049. [Google Scholar] [CrossRef] [Green Version]
- Pan, M.H.; Liang, Y.C.; Lin-Shiau, S.Y.; Zhu, N.Q.; Ho, C.T.; Lin, J.K. Induction of Apoptosis by the Oolong Tea Polyphenol Theasinensin A through Cytochrome c Release and Activation of Caspase-9 and Caspase-3 in Human U937 Cells. J. Agric. Food Chem. 2000, 48, 6337–6346. [Google Scholar] [CrossRef]
- Roy, M.; Chakrabarty, S.; Sinha, D.; Bhattacharya, R.K.; Siddiqi, M. Anticlastogenic, Antigenotoxic and Apoptotic Activity of Epigallocatechin Gallate: A Green Tea Polyphenol. Mutat. Res. 2003, 523–524, 33–41. [Google Scholar] [CrossRef]
- Saeki, K.; Sano, M.; Miyase, T.; Nakamura, Y.; Kara, Y.; Aoyagi, Y.; Isemura, M. Apoptosis-Inducing Activity of Polyphenol Compounds Derived from Tea Catechins in Human Histiolytic Lymphoma U937 Cells. Biosci. Biotechnol. Biochem. 1999, 63, 585–587. [Google Scholar] [CrossRef] [Green Version]
- Saeki, K.; Hayakawa, S.; Isemura, M.; Miyase, T. Importance of a Pyrogallol-Type Structure in Catechin Compounds for Apoptosis-Inducing Activity. Phytochemistry 2000, 53, 391–394. [Google Scholar] [CrossRef]
- Lung, H.L.; Ip, W.K.; Chen, Z.Y.; Mak, N.K.; Leung, K.N. Comparative Study of the Growth-Inhibitory and Apoptosis-Inducing Activities of Black Tea Theaflavins and Green Tea Catechin on Murine Myeloid Leukemia Cells. Int. J. Mol. Med. 2004, 13, 465–471. [Google Scholar] [CrossRef]
- Xiao, X.; Jiang, K.; Xu, Y.; Peng, H.; Wang, Z.; Liu, S.; Zhang, G. (-)-Epigallocatechin-3-Gallate Induces Cell Apoptosis in Chronic Myeloid Leukaemia by Regulating Bcr/Abl-Mediated P38-MAPK/JNK and JAK2/STAT3/AKT Signalling Pathways. Clin. Exp. Pharmacol. Physiol. 2019, 46, 126–136. [Google Scholar] [CrossRef]
- Kemberling, J.K.; Hampton, J.A.; Keck, R.W.; Gomez, M.A.; Selman, S.H. Inhibition of Bladder Tumor Growth by the Green Tea Derivative Epigallocatechin-3-Gallate. J. Urol. 2003, 170, 773–776. [Google Scholar] [CrossRef] [PubMed]
- Kizaki, M.; Xian, M.; Sagawa, M.; Ikeda, Y. Induction of Apoptosis via the Modulation of Reactive Oxygen Species (ROS) Production in the Treatment of Myeloid Leukemia. Curr. Pharm. Biotechnol. 2006, 7, 323–329. [Google Scholar] [CrossRef] [PubMed]
- Calgarotto, A.K.; Maso, V.; Junior, G.C.F.; Nowill, A.E.; Filho, P.L.; Vassallo, J.; Saad, S.T.O. Antitumor Activities of Quercetin and Green Tea in Xenografts of Human Leukemia HL60 Cells. Sci. Rep. 2018, 8, 3459. [Google Scholar] [CrossRef] [Green Version]
- Torello, C.O.; Shiraishi, R.N.; Della Via, F.I.; de Castro, T.C.L.; Longhini, A.L.; Santos, I.; Bombeiro, A.L.; Silva, C.L.A.; de Souza Queiroz, M.L.; Rego, E.M.; et al. Reactive Oxygen Species Production Triggers Green Tea-Induced Anti-Leukaemic Effects on Acute Promyelocytic Leukaemia Model. Cancer Lett. 2018, 414, 116–126. [Google Scholar] [CrossRef]
- Kazi, A.; Wang, Z.; Kumar, N.; Falsetti, S.C.; Chan, T.H.; Dou, Q.P. Structure-Activity Relationships of Synthetic Analogs of (-)-Epigallocatechin-3-Gallate as Proteasome Inhibitors. Anticancer. Res. 2004, 24, 943–954. [Google Scholar] [PubMed]
- Huang, Y.Y.; Xia, Y.; Guo, H.X.; Li, W.Y. [Effect of (-)-Epigallocatechin-3-Gallate and 5-AZA-CdR on Expression of X-Linked Inhibitor of Apoptosis Protein-Associated Factor 1 in Human Leukemia HL-60 and K562 Cells]. Nan Fang Yi Ke Da Xue Xue Bao J. South. Med. Univ. 2008, 28, 204–208. [Google Scholar]
- Aggarwal, V.; Tuli, H.S.; Varol, A.; Thakral, F.; Yerer, M.B.; Sak, K.; Varol, M.; Jain, A.; Khan, M.A.; Sethi, G. Role of Reactive Oxygen Species in Cancer Progression: Molecular Mechanisms and Recent Advancements. Biomolecules 2019, 9, 735. [Google Scholar] [CrossRef] [Green Version]
- Lambert, J.D.; Elias, R.J. The Antioxidant and Pro-Oxidant Activities of Green Tea Polyphenols: A Role in Cancer Prevention. Arch. Biochem. Biophys. 2010, 501, 65–72. [Google Scholar] [CrossRef] [Green Version]
- Yang, C.S.; Zhang, J. Studies on the Prevention of Cancer and Cardiometabolic Diseases by Tea: Issues on Mechanisms, Effective Doses, and Toxicities. J. Agric. Food Chem. 2019, 67, 5446–5456. [Google Scholar] [CrossRef]
- Peluso, I.; Serafini, M. Antioxidants from Black and Green Tea: From Dietary Modulation of Oxidative Stress to Pharmacological Mechanisms. Br. J. Pharmacol. 2017, 174, 1195–1208. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ho, C.T.; Chen, Q.; Shi, H.; Zhang, K.Q.; Rosen, R.T. Antioxidative Effect of Polyphenol Extract Prepared from Various Chinese Teas. Prev. Med. 1992, 21, 520–525. [Google Scholar] [CrossRef] [PubMed]
- Surh, Y.J. Molecular Mechanisms of Chemopreventive Effects of Selected Dietary and Medicinal Phenolic Substances. Mutat. Res. 1999, 428, 305–327. [Google Scholar] [CrossRef] [PubMed]
- Sang, S.; Lambert, J.D.; Ho, C.T.; Yang, C.S. The Chemistry and Biotransformation of Tea Constituents. Pharmacol. Res. 2011, 64, 87–99. [Google Scholar] [CrossRef]
- Wei, Y.; Chen, P.; Ling, T.; Wang, Y.; Dong, R.; Zhang, C.; Zhang, L.; Han, M.; Wang, D.; Wan, X.; et al. Certain (-)-Epigallocatechin-3-Gallate (EGCG) Auto-Oxidation Products (EAOPs) Retain the Cytotoxic Activities of EGCG. Food Chem. 2016, 204, 218–226. [Google Scholar] [CrossRef]
- Saeki, K.; Kobayashi, N.; Inazawa, Y.; Zhang, H.; Nishitoh, H.; Ichijo, H.; Saeki, K.; Isemura, M.; Yuo, A. Oxidation-Triggered c-Jun N-Terminal Kinase (JNK) and P38 Mitogen-Activated Protein (MAP) Kinase Pathways for Apoptosis in Human Leukaemic Cells Stimulated by Epigallocatechin-3-Gallate (EGCG): A Distinct Pathway from Those of Chemically Induced and Receptor-Mediated Apoptosis. Biochem. J. 2002, 368, 705–720. [Google Scholar] [CrossRef] [Green Version]
- Oikawa, S.; Furukawa, A.; Asada, H.; Hirakawa, K.; Kawanishi, S. Catechins Induce Oxidative Damage to Cellular and Isolated DNA through the Generation of Reactive Oxygen Species. Free Radic. Res. 2003, 37, 881–890. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa, H.; Hasumi, K.; Woo, J.T.; Nagai, K.; Wachi, M. Generation of Hydrogen Peroxide Primarily Contributes to the Induction of Fe(II)-Dependent Apoptosis in Jurkat Cells by (-)-Epigallocatechin Gallate. Carcinogenesis 2004, 25, 1567–1574. [Google Scholar] [CrossRef] [Green Version]
- Elbling, L.; Weiss, R.-M.; Teufelhofer, O.; Uhl, M.; Knasmueller, S.; Schulte-Hermann, R.; Berger, W.; Micksche, M. Green Tea Extract and (-)-Epigallocatechin-3-Gallate, the Major Tea Catechin, Exert Oxidant but Lack Antioxidant Activities. FASEB J. 2005, 19, 807–809. [Google Scholar] [CrossRef]
- Noda, C.; He, J.; Takano, T.; Tanaka, C.; Kondo, T.; Tohyama, K.; Yamamura, H.; Tohyama, Y. Induction of Apoptosis by Epigallocatechin-3-Gallate in Human Lymphoblastoid B Cells. Biochem. Biophys. Res. Commun. 2007, 362, 951–957. [Google Scholar] [CrossRef]
- Lee, T.C.; Cheng, I.C.; Shue, J.J.; Wang, T.C. Cytotoxicity of Arsenic Trioxide Is Enhanced by (-)-Epigallocatechin-3-Gallate via Suppression of Ferritin in Cancer Cells. Toxicol. Appl. Pharmacol. 2011, 250, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Kawai, Y.; Matsui, Y.; Kondo, H.; Morinaga, H.; Uchida, K.; Miyoshi, N.; Nakamura, Y.; Osawa, T. Galloylated Catechins as Potent Inhibitors of Hypochlorous Acid-Induced DNA Damage. Chem. Res. Toxicol. 2008, 21, 1407–1414. [Google Scholar] [CrossRef] [PubMed]
- Ren, L.; Yang, H.Y.; Choi, H.I.; Chung, K.J.; Yang, U.; Lee, I.K.; Kim, H.J.; Lee, D.S.; Park, B.J.; Lee, T.H. The Role of Peroxiredoxin V in (-)-Epigallocatechin 3-Gallate-Induced Multiple Myeloma Cell Death. Oncol. Res. 2011, 19, 391–398. [Google Scholar] [CrossRef] [PubMed]
- Tofolean, I.T.; Ganea, C.; Ionescu, D.; Filippi, A.; Garaiman, A.; Goicea, A.; Gaman, M.A.; Dimancea, A.; Baran, I. Cellular Determinants Involving Mitochondrial Dysfunction, Oxidative Stress and Apoptosis Correlate with the Synergic Cytotoxicity of Epigallocatechin-3-Gallate and Menadione in Human Leukemia Jurkat T Cells. Pharmacol. Res. 2016, 103, 300–317. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.N.; Wang, J.; Yang, H.N.; Zhang, B.L.; Zhang, P.; Sun, P.Y.; Zhang, N.; Wang, Y.; Sheng, J.; Wang, X.J.; et al. The Oxidation of (−)-Epigallocatechin-3-Gallate Inhibits T-Cell Acute Lymphoblastic Leukemia Cell Line HPB-ALL via the Regulation of Notch1 Expression. RSC Adv. 2020, 10, 1679–1684. [Google Scholar] [CrossRef]
- Lawrence, M.S.; Stojanov, P.; Mermel, C.H.; Robinson, J.T.; Garraway, L.A.; Golub, T.R.; Meyerson, M.; Gabriel, S.B.; Lander, E.S.; Getz, G. Discovery and Saturation Analysis of Cancer Genes across 21 Tumour Types. Nature 2014, 505, 495–501. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Herman, J.G.; Baylin, S.B. Gene Silencing in Cancer in Association with Promoter Hypermethylation. N. Engl. J. Med. 2003, 349, 2042–2054. [Google Scholar] [CrossRef]
- Portela, A.; Esteller, M. Epigenetic Modifications and Human Disease. Nat. Biotechnol. 2010, 28, 1057–1068. [Google Scholar] [CrossRef]
- Okano, M.; Bell, D.W.; Haber, D.A.; Li, E. DNA Methyltransferases Dnmt3a and Dnmt3b Are Essential for de Novo Methylation and Mammalian Development. Cell 1999, 99, 247–257. [Google Scholar] [CrossRef] [Green Version]
- Rasmussen, K.D.; Helin, K. Role of TET Enzymes in DNA Methylation, Development, and Cancer. Genes. Dev. 2016, 30, 733–750. [Google Scholar] [CrossRef] [Green Version]
- Hatziapostolou, M.; Iliopoulos, D. Epigenetic Aberrations during Oncogenesis. Cell Mol. Life Sci. 2011, 68, 1681–1702. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Odenike, O.; Rowley, J.D. Leukaemogenesis: More than Mutant Genes. Nat. Rev. Cancer 2010, 10, 23–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Galm, O.; Herman, J.G.; Baylin, S.B. The Fundamental Role of Epigenetics in Hematopoietic Malignancies. Blood Rev. 2006, 20, 1–13. [Google Scholar] [CrossRef]
- Jones, P.A.; Baylin, S.B. The Epigenomics of Cancer. Cell 2007, 128, 683. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ting, A.H.; McGarvey, K.M.; Baylin, S.B. The Cancer Epigenome—Components and Functional Correlates. Genes. Dev. 2006, 20, 3215–3231. [Google Scholar] [CrossRef] [Green Version]
- Mizuno, S.I.; Chijiwa, T.; Okamura, T.; Akashi, K.; Fukumaki, Y.; Niho, Y.; Sasaki, H. Expression of DNA Methyltransferases DNMT1, 3A, and 3B in Normal Hematopoiesis and in Acute and Chronic Myelogenous Leukemia. Blood 2001, 97, 1172–1179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haberland, M.; Montgomery, R.L.; Olson, E.N. The Many Roles of Histone Deacetylases in Development and Physiology: Implications for Disease and Therapy. Nat. Rev. Genet. 2009, 10, 32–42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Warrell, R.P.; He, L.Z.; Richon, V.; Calleja, E.; Pandolfi, P.P. Therapeutic Targeting of Transcription in Acute Promyelocytic Leukemia by Use of an Inhibitor of Histone Deacetylase. J. Natl. Cancer Inst. 1998, 90, 1621–1625. [Google Scholar] [CrossRef] [Green Version]
- Lin, R.J.; Evans, R.M. Acquisition of Oncogenic Potential by RAR Chimeras in Acute Promyelocytic Leukemia through Formation of Homodimers. Mol. Cell 2000, 5, 821–830. [Google Scholar] [CrossRef]
- Minucci, S.; Nervi, C.; Lo Coco, F.; Pelicci, P.G. Histone Deacetylases: A Common Molecular Target for Differentiation Treatment of Acute Myeloid Leukemias? Oncogene 2001, 20, 3110–3115. [Google Scholar] [CrossRef]
- Altucci, L.; Clarke, N.; Nebbioso, A.; Scognamiglio, A.; Gronemeyer, H. Acute Myeloid Leukemia: Therapeutic Impact of Epigenetic Drugs. Int. J. Biochem. Cell Biol. 2005, 37, 1752–1762. [Google Scholar] [CrossRef]
- Leone, G.; D’Alo, F.; Zardo, G.; Voso, M.; Nervi, C. Epigenetic Treatment of Myelodysplastic Syndromes and Acute Myeloid Leukemias. Curr. Med. Chem. 2008, 15, 1274–1287. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marks, P.A. Histone Deacetylase Inhibitors: A Chemical Genetics Approach to Understanding Cellular Functions. Biochim. Biophys. Acta 2010, 1799, 717–725. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Komashko, V.M.; Farnham, P.J. 5-Azacytidine Treatment Reorganizes Genomic Histone Modification Patterns. Epigenetics 2010, 5, 229–240. [Google Scholar] [CrossRef] [Green Version]
- Sporn, M.B.; Suh, N. Chemoprevention: An Essential Approach to Controlling Cancer. Nat. Rev. Cancer 2002, 2, 537–543. [Google Scholar] [CrossRef] [PubMed]
- Fang, M.Z.; Wang, Y.; Ai, N.; Hou, Z.; Sun, Y.; Lu, H.; Welsh, W.; Yang, C.S. Tea Polyphenol ()-Epigallocatechin-3-Gallate Inhibits DNA Methyltransferase and Reactivates Methylation-Silenced Genes in Cancer Cell Lines. Cancer Res. 2003, 63, 7563–7570. [Google Scholar]
- Won, J.L.; Shim, J.Y.; Zhu, B.T. Mechanisms for the Inhibition of DNA Methyltransferases by Tea Catechins and Bioflavonoids. Mol. Pharmacol. 2005, 68, 1018–1030. [Google Scholar] [CrossRef] [Green Version]
- Navarro-Perán, E.; Cabezas-Herrera, J.; del Campo, L.S.; Rodríguez-López, J.N. Effects of Folate Cycle Disruption by the Green Tea Polyphenol Epigallocatechin-3-Gallate. Int. J. Biochem. Cell Biol. 2007, 39, 2215–2225. [Google Scholar] [CrossRef]
- Balasubramanian, S.; Adhikary, G.; Eckert, R.L. The Bmi-1 Polycomb Protein Antagonizes the (-)-Epigallocatechin-3-Gallate-Dependent Suppression of Skin Cancer Cell Survival. Carcinogenesis 2010, 31, 496–503. [Google Scholar] [CrossRef] [Green Version]
- Choi, K.C.; Myung, G.J.; Lee, Y.H.; Joo, C.Y.; Seung, H.K.; Kang, H.B.; Kim, M.J.; Cha, J.H.; Young, J.K.; Woo, J.J.; et al. Epigallocatechin-3-Gallate, a Histone Acetyltransferase Inhibitor, Inhibits EBV-Induced B Lymphocyte Transformation via Suppression of RelA Acetylation. Cancer Res. 2009, 69, 583–592. [Google Scholar] [CrossRef] [Green Version]
- Nair, S.; Hebbar, V.; Shen, G.; Gopalakrishnan, A.; Khor, T.O.; Yu, S.; Xu, C.; Kong, A.N. Synergistic Effects of a Combination of Dietary Factors Sulforaphane and (-) Epigallocatechin-3-Gallate in HT-29 AP-1 Human Colon Carcinoma Cells. Pharm. Res. 2008, 25, 387–399. [Google Scholar] [CrossRef]
- Pandey, M.; Shukla, S.; Gupta, S. Promoter Demethylation and Chromatin Remodeling by Green Tea Polyphenols Leads to Re-Expression of GSTP1 in Human Prostate Cancer Cells. Int. J. Cancer 2010, 126, 2520–2533. [Google Scholar] [CrossRef] [Green Version]
- Borutinskaitė, V.; Virkšaitė, A.; Gudelytė, G.; Navakauskienė, R. Green Tea Polyphenol EGCG Causes Anti-Cancerous Epigenetic Modulations in Acute Promyelocytic Leukemia Cells. Leuk. Lymphoma 2018, 59, 469–478. [Google Scholar] [CrossRef]
- Alizadeh, M.; Nafari, A.; Safarzadeh, A.; Veiskarami, S.; Almasian, M.; Kiani, A.A. The Impact of EGCG and RG108 on SOCS1 Promoter DNA Methylation and Expression in U937 Leukemia Cells. Rep. Biochem. Mol. Biol. 2021, 10, 455–461. [Google Scholar] [CrossRef] [PubMed]
- Vitkeviciene, A.; Baksiene, S.; Borutinskaite, V.; Navakauskiene, R. Epigallocatechin-3-Gallate and BIX-01294 Have Different Impact on Epigenetics and Senescence Modulation in Acute and Chronic Myeloid Leukemia Cells. Eur. J. Pharmacol. 2018, 838, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Moradzadeh, M.; Roustazadeh, A.; Tabarraei, A.; Erfanian, S.; Sahebkar, A. Epigallocatechin-3-Gallate Enhances Differentiation of Acute Promyelocytic Leukemia Cells via Inhibition of PML-RARα and HDAC1. Phytother. Res. 2018, 32, 471–479. [Google Scholar] [CrossRef]
- Wei, S.; Kozono, S.; Kats, L.; Nechama, M.; Li, W.; Guarnerio, J.; Luo, M.; You, M.H.; Yao, Y.; Kondo, A.; et al. Active Pin1 Is a Key Target of All-Trans Retinoic Acid in Acute Promyelocytic Leukemia and Breast Cancer. Nat. Med. 2015, 21, 457–466. [Google Scholar] [CrossRef]
- Yao, S.; Zhong, L.; Chen, M.; Zhao, Y.; Li, L.; Liu, L.; Xu, T.; Xiao, C.; Gan, L.; Shan, Z.; et al. Epigallocatechin-3-Gallate Promotes All-Trans Retinoic Acid-Induced Maturation of Acute Promyelocytic Leukemia Cells via PTEN. Int. J. Oncol. 2017, 51, 899–906. [Google Scholar] [CrossRef] [Green Version]
- Liu, P.; Zhang, M.; Jin, J.; Holman, C.D.A.J. Tea Consumption Reduces the Risk of de Novo Myelodysplastic Syndromes. Leuk. Res. 2015, 39, 164–169. [Google Scholar] [CrossRef] [PubMed]
- Ugai, T.; Matsuo, K.; Sawada, N.; Iwasaki, M.; Yamaji, T.; Shimazu, T.; Goto, A.; Inoue, M.; Kanda, Y.; Tsugane, S. Coffee and Green Tea Consumption and Subsequent Risk of Acute Myeloid Leukemia and Myelodysplastic Syndromes in Japan. Int. J. Cancer 2018, 142, 1130–1138. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, T.L.; Jeong, G.H.; Yang, J.W.; Lee, K.H.; Kronbichler, A.; Van Der Vliet, H.J.; Grosso, G.; Galvano, F.; Aune, D.; Kim, J.Y.; et al. Tea Consumption and Risk of Cancer: An Umbrella Review and Meta-Analysis of Observational Studies. Adv. Nutr. 2020, 11, 1437–1452. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Moysich, K.B.; Baer, M.R.; Weiss, J.R.; Brasure, J.; Graham, S.; McCann, S.E. Intakes of Selected Food Groups and Beverages and Adult Acute Myeloid Leukemia. Leuk. Res. 2006, 30, 1507–1515. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.Y.; Hsu, Y.H.; Wu, M.T.; Pan, P.C.; Ho, C.K.; Su, L.; Xu, X.; Li, Y.; Christiani, D.C.; Chang, T.T.; et al. Cured Meat, Vegetables, and Bean-Curd Foods in Relation to Childhood Acute Leukemia Risk: A Population Based Case-Control Study. BMC Cancer 2009, 9, 15. [Google Scholar] [CrossRef] [Green Version]
- Liu, P.; Zhang, M.; Xie, X.; Jin, J.; Holman, C.D.J. Green Tea Consumption and Glutathione S-Transferases Genetic Polymorphisms on the Risk of Adult Leukemia. Eur. J. Nutr. 2017, 56, 603–612. [Google Scholar] [CrossRef]
- Ma, X.; Park, Y.; Mayne, S.T.; Wang, R.; Sinha, R.; Hollenbeck, A.R.; Schatzkin, A.; Cross, A.J. Diet, Lifestyle, and Acute Myeloid Leukemia in the NIH–AARP Cohort. Am. J. Epidemiol. 2010, 171, 312–322. [Google Scholar] [CrossRef] [Green Version]
- Naganuma, T.; Kuriyama, S.; Kakizaki, M.; Sone, T.; Nakaya, N.; Ohmori-Matsuda, K.; Hozawa, A.; Nishino, Y.; Tsuji, I. Green Tea Consumption and Hematologic Malignancies in JapanThe Ohsaki Study. Am. J. Epidemiol. 2009, 170, 730–738. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parodi, S.; Merlo, D.F.; Stagnaro, E. Coffee and Tea Consumption and Risk of Leukaemia in an Adult Population: A Reanalysis of the Italian Multicentre Case-Control Study. Cancer Epidemiol. 2017, 47, 81–87. [Google Scholar] [CrossRef]
- Takada, M.; Yamagishi, K.; Iso, H.; Tamakoshi, A. Green Tea Consumption and Risk of Hematologic Neoplasms: The Japan Collaborative Cohort Study for Evaluation of Cancer Risk (JACC Study). Cancer Causes Control 2019, 30, 1223–1230. [Google Scholar] [CrossRef]
- Zhang, M.; Zhao, X.; Zhang, X.; Holman, C.D.A.J. Possible Protective Effect of Green Tea Intake on Risk of Adult Leukaemia. Br. J. Cancer 2008, 98, 168–170. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.D.; Zhao, X.Y.; Zhang, M.; Liang, Y.; Xu, X.H.; D’Arcy, C.; Holman, J. A Case-Control Study on Green Tea Consumption and the Risk of Adult Leukemia. Zhonghua Liu Xing Bing. Xue Za Zhi 2008, 29, 290–293. [Google Scholar] [PubMed]
- Kuo, Y.C.; Yu, C.L.; Liu, C.Y.; Wang, S.F.; Pan, P.C.; Wu, M.T.; Ho, C.K.; Lo, Y.S.; Li, Y.; Christiani, D.C.; et al. A Population-Based, Case-Control Study of Green Tea Consumption and Leukemia Risk in Southwestern Taiwan. Cancer Causes Control 2009, 20, 57–65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhong, S.; Chen, Z.; Yu, X.; Chen, W.; Lv, M.; Ma, T.; Zhao, J. Tea Consumption and Leukemia Risk: A Meta-Analysis. Tumour Biol. 2014, 35, 5205–5212. [Google Scholar] [CrossRef] [PubMed]
- Calgarotto, A.K.; Longhini, A.L.; Pericole de Souza, F.V.; Duarte, A.S.S.; Ferro, K.P.; Santos, I.; Maso, V.; Olalla Saad, S.T.; Torello, C.O. Immunomodulatory Effect of Green Tea Treatment in Combination with Low-Dose Chemotherapy in Elderly Acute Myeloid Leukemia Patients with Myelodysplasia-Related Changes. Integr. Cancer Ther. 2021, 20. [Google Scholar] [CrossRef] [PubMed]
- Shanafelt, T.D.; Lee, Y.K.; Call, T.G.; Nowakowski, G.S.; Dingli, D.; Zent, C.S.; Kay, N.E. Clinical Effects of Oral Green Tea Extracts in Four Patients with Low Grade B-Cell Malignancies. Leuk. Res. 2006, 30, 707–712. [Google Scholar] [CrossRef]
- Shanafelt, T.D.; Call, T.G.; Zent, C.S.; LaPlant, B.; Bowen, D.A.; Roos, M.; Secreto, C.R.; Ghosh, A.K.; Kabat, B.F.; Lee, M.J.; et al. Phase I Trial of Daily Oral Polyphenon E in Patients with Asymptomatic Rai Stage 0 to II Chronic Lymphocytic Leukemia. J. Clin. Oncol. 2009, 27, 3808–3814. [Google Scholar] [CrossRef] [PubMed]
- Shanafelt, T.D.; Call, T.G.; Zent, C.S.; Leis, J.F.; Laplant, B.; Bowen, D.A.; Roos, M.; Laumann, K.; Ghosh, A.K.; Lesnick, C.; et al. Phase 2 Trial of Daily, Oral Polyphenon e in Patients with Asymptomatic, Rai Stage 0 to II Chronic Lymphocytic Leukemia. Cancer 2013, 119, 363–370. [Google Scholar] [CrossRef] [Green Version]
- D’Arena, G.; Simeon, V.; De Martino, L.; Statuto, T.; D’Auria, F.; Volpe, S.; Deaglio, S.; Maidecchi, A.; Mattoli, L.; Mercati, V.; et al. Regulatory T-Cell Modulation by Green Tea in Chronic Lymphocytic Leukemia. Int. J. Immunopathol. Pharmacol. 2013, 26, 117–125. [Google Scholar] [CrossRef]
- Lemanne, D.; Block, K.I.; Kressel, B.R.; Sukhatme, V.P.; White, J.D. A Case of Complete and Durable Molecular Remission of Chronic Lymphocytic Leukemia Following Treatment with Epigallocatechin-3-Gallate, an Extract of Green Tea. Cureus 2015, 7, e441. [Google Scholar] [CrossRef] [Green Version]
- Ullmann, U.; Haller, J.; Decourt, J.P.; Girault, N.; Girault, J.; Richard-Caudron, A.S.; Pineau, B.; Weber, P. A Single Ascending Dose Study of Epigallocatechin Gallate in Healthy Volunteers. J. Int. Med. Res. 2003, 31, 88–101. [Google Scholar] [CrossRef]
- Chow, H.H.S.; Hakim, I.A.; Vining, D.R.; Crowell, J.A.; Ranger-Moore, J.; Chew, W.M.; Celaya, C.A.; Rodney, S.R.; Hara, Y.; Alberts, D.S. Effects of Dosing Condition on the Oral Bioavailability of Green Tea Catechins after Single-Dose Administration of Polyphenon E in Healthy Individuals. Clin. Cancer Res. 2005, 11, 4627–4633. [Google Scholar] [CrossRef] [Green Version]
| Model | Compound/Component | Effect | Reference |
|---|---|---|---|
| In vitro | |||
| NB4 HL60 | EGCG 30–40 µM (6–96 h) | ↓ DNMT1, HDAC1, HDAC 2, G9a, H3K9me2, PCR2 and ↑ H4, H3K14 (p27, PCAF, c/EBPalfa, c/EBPe) and (EZH, SUZ12, EED) | [103] |
| U937 | EGCG 25 µM (12–72 h) | ↓ Promoter methylation SOCS1 | [104] |
| NB4 K562 | EGCG 30–40 µM (0–3 days) | ↓ DNMT1, H3K9me3 HP1alfa, EZH2, SUZ12 only NB4 cell line, no effect on K562 | [105] |
| NB4 HL60 | EGCG 0–100 µM (24–72 h) | ↓ HDAC1 | [106] |
| Model | Compound/Component | Effect | Reference |
|---|---|---|---|
| In vitro | |||
| HL60 NB4 | EGCG 0–40 µmol/L (24–36h) ATRA—1 µmol/L | Induction of neutrophil differentiation—↑ CD11b surface expression EGCG + ATRA—↑ CD11b and CD15 expression; ↑ CEBPE, CSF3R and DAPK2; and ↓ of undifferentiated promyelocytes and myelocytes | [16] |
| NB4 NB4 R1 NB4 R2 | Catechins 100–200 µM (12–24 h) | Induction of PML/RARα degradation | [33] |
| NB4 | EGCG 0–30 µM (72 h) ATRA—10 µM | Induction of PML-RARα degradation by inhibition of Pin1 (↓) | [107] |
| HL-60 NB4 | EGCG 0–100 µM (24–72 h) ATRA—10 µM | Induction of granulocytic maturation—morphological changes and ↑ NBT reduction ability; and degradation of PML/RARα (↓) and HDAC1 (↓) | [106] |
| HL60 NB4 THP-1 | EGCG 5–40 µM (48 h) ATRA 1 µM/mL | Induction of PML/RARα degradation (↓) and restored PML (↑) and PTEN (↑) function EGCG + ATRA—↑ PTEN, CD11b, CEBPE | [108] |
| NB4 | EGCG 12.5–20 µg/mL ATRA—1 µM | Induction of neutrophil differentiation—↑ of CD11b, CD14, CD15 and CD66 surface expression EGCG + ATRA—↑ CD15 expression | [7] |
| In vivo—Xenograft and systemics model | |||
| CTSG-PML-RARA transgenic mice cells in C57BL/6J mice | EGCG 12.50 mg/kg/d intraperitoneally for 21 days ATRA—5 mg | Induction of PML-RARα degradation in bone marrow cells and ↓ of spleen weight | [107] |
| hCG-PML/RAR transgenic mice cells in NOD. CB17-Prkdcscid/J mice | EGCG 25 mg/kg/d intraperitoneally, for 5 days | Induction of differentiation—↓ immature cells and undifferentiated promyelocytes in the bone marrow, ↑ mature myeloid cells, ↓ PIN1 and its substrates—cyclin D, NFκB, c-Myc and AKT and ↑ ROS; ↓ of spleen weight | [7] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Della Via, F.I.; Alvarez, M.C.; Basting, R.T.; Saad, S.T.O. The Effects of Green Tea Catechins in Hematological Malignancies. Pharmaceuticals 2023, 16, 1021. https://doi.org/10.3390/ph16071021
Della Via FI, Alvarez MC, Basting RT, Saad STO. The Effects of Green Tea Catechins in Hematological Malignancies. Pharmaceuticals. 2023; 16(7):1021. https://doi.org/10.3390/ph16071021
Chicago/Turabian StyleDella Via, Fernanda Isabel, Marisa Claudia Alvarez, Rosanna Tarkany Basting, and Sara Teresinha Olalla Saad. 2023. "The Effects of Green Tea Catechins in Hematological Malignancies" Pharmaceuticals 16, no. 7: 1021. https://doi.org/10.3390/ph16071021
APA StyleDella Via, F. I., Alvarez, M. C., Basting, R. T., & Saad, S. T. O. (2023). The Effects of Green Tea Catechins in Hematological Malignancies. Pharmaceuticals, 16(7), 1021. https://doi.org/10.3390/ph16071021






