The Benefits of Probiotics on Oral Health: Systematic Review of the Literature
Abstract
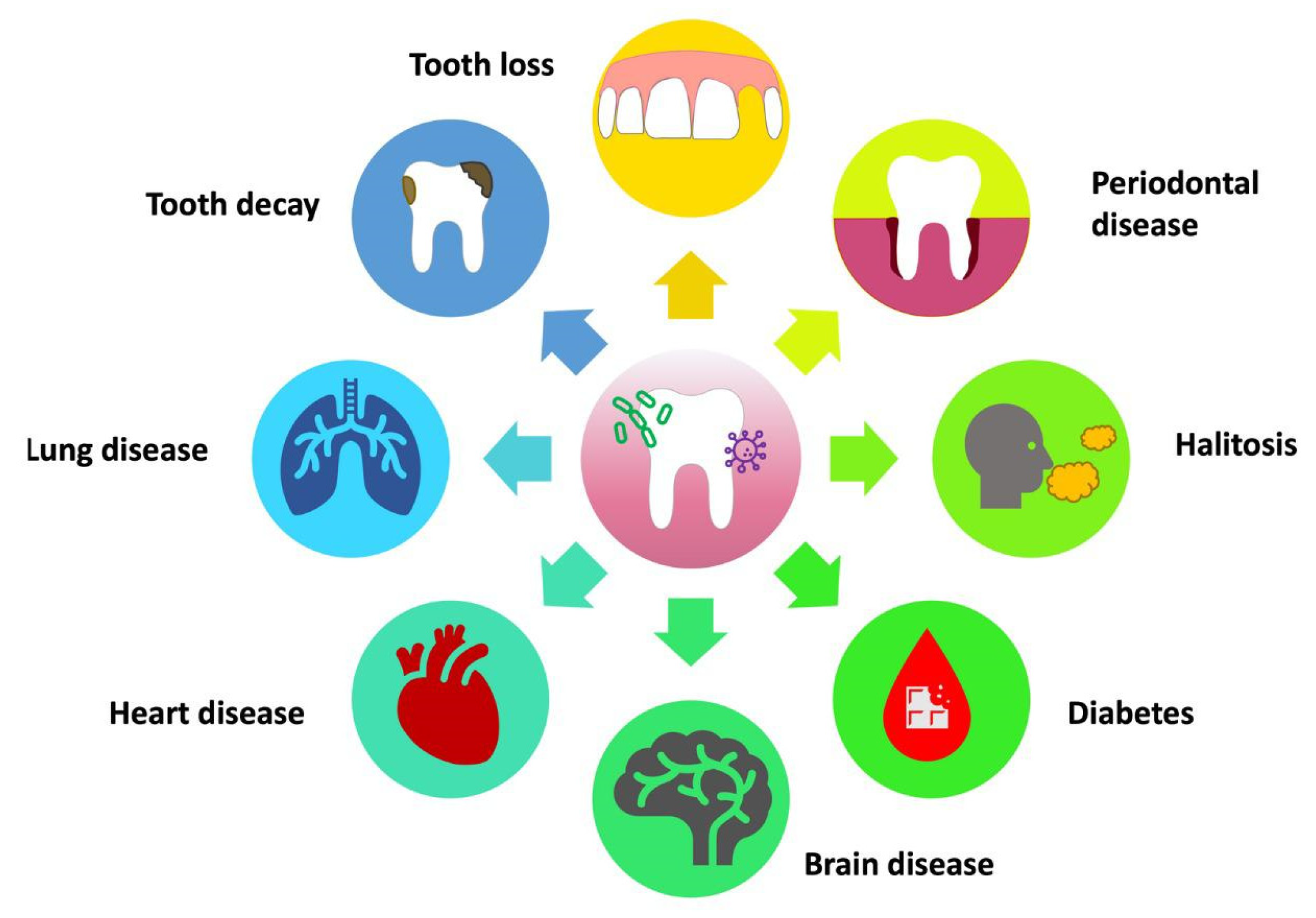
:1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Search Processing
2.3. Eligibility Criteria and Study Selection
2.4. Data Processing
2.5. Quality Assessment
2.6. PICOS Criteria
3. Results
Quality Assessment and Risk of Bias
4. Discussion
4.1. Caries and Associated Microbes
4.2. Periodontal Disease
4.3. Halitosis
4.4. Mucositis and Peri-Implantitis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| B. Bifidum | Bifidobacterium bifidum |
| B. Dentium | Bifidobacterium dentium |
| BEC | buccal epiteliale Cell adhesion |
| B. Longum | Bifidobacterium longum |
| CFU | Colony-forming units |
| CI | confidence interval |
| ECC | Early Childhood Caries |
| F. | Nucleatum Fusobacterium Nucleatum |
| GI | gingival index |
| GIT | Infant gastrointestinal tract |
| ICDAS II | International Caries Detection and Assessment System II |
| IL | interleukin |
| LAB | Lactic Acid bacteria |
| L. brevis CD2 | Lactobacillus brevis CD2 |
| L. paracasei | Lacticaseibacillus paracasei |
| L. plantarum | Lactobacillus plantarum |
| L. reuteri | Lactobacillus Reuteri |
| L. rhamnosus | Lacticaseibacillus rhamnosus |
| L. salivarius | Ligilactobacillus salivarius |
| MD | mechanical debridement |
| mPI | modified plaque index |
| mSBI | modified sulcus bleeding index |
| OHI-S index | Simplified Oral Hygiene Index |
| PBs | Probiotics |
| PI | plaque index |
| PiM | peri-implant mucositis |
| PPD | pocket probing depth |
| PD | probing depth |
| S. mutans | Streptococcus mutans |
| SRP | Scaling and root planing |
| TNF | tumor necrosis factor |
| W. cibaria | Weissella cibaria |
References
- Inchingolo, A.D.; Malcangi, G.; Semjonova, A.; Inchingolo, A.M.; Patano, A.; Coloccia, G.; Ceci, S.; Marinelli, G.; Di Pede, C.; Ciocia, A.M.; et al. Oralbiotica/Oralbiotics: The Impact of Oral Microbiota on Dental Health and Demineralization: A Systematic Review of the Literature. Children 2022, 9, 1014. [Google Scholar] [CrossRef] [PubMed]
- Ballini, A.; Santacroce, L.; Cantore, S.; Bottalico, L.; Dipalma, G.; Topi, S.; Saini, R.; De Vito, D.; Inchingolo, F. Probiotics Efficacy on Oxidative Stress Values in Inflammatory Bowel Disease: A Randomized Double-Blinded Placebo-Controlled Pilot Study. Endocr. Metab. Immune Disord Drug Targets 2019, 19, 373–381. [Google Scholar] [CrossRef]
- Signorini, L.; De Leonardis, F.; Santacroce, L.; Haxhirexha, K.; Topi, S.; Fumarola, L.; Dipalma, G.; Coscia, M.F.; Inchingolo, F. Probiotics May Modulate the Impact of Aging on Adults. J. Biol. Regul. Homeost Agents 2020, 34, 1601–1606. [Google Scholar] [CrossRef]
- Ballini, A.; Signorini, L.; Inchingolo, A.M.; Saini, R.; Gnoni, A.; Scacco, S.; Cantore, S.; Dipalma, G.; Inchingolo, F.; Santacroce, L. Probiotics May Improve Serum Folate Availability in Pregnant Women: A Pilot Study. Open Access Maced. J. Med. Sci. 2020, 8, 1124–1130. [Google Scholar] [CrossRef]
- Marrelli, M.; Tatullo, M.; Dipalma, G.; Inchingolo, F. Oral Infection by Staphylococcus Aureus in Patients Affected by White Sponge Nevus: A Description of Two Cases Occurred in the Same Family. Int. J. Med. Sci. 2012, 9, 47–50. [Google Scholar] [CrossRef] [PubMed]
- Dohan Ehrenfest, D.M.; Del Corso, M.; Inchingolo, F.; Sammartino, G.; Charrier, J.-B. Platelet-Rich Plasma (PRP) and Platelet-Rich Fibrin (PRF) in Human Cell Cultures: Growth Factor Release and Contradictory Results. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2010, 110, 418–421. [Google Scholar] [CrossRef] [PubMed]
- Santacroce, L.; Di Cosola, M.; Bottalico, L.; Topi, S.; Charitos, I.A.; Ballini, A.; Inchingolo, F.; Cazzolla, A.P.; Dipalma, G. Focus on HPV Infection and the Molecular Mechanisms of Oral Carcinogenesis. Viruses 2021, 13, 559. [Google Scholar] [CrossRef] [PubMed]
- Vermesan, D.; Inchingolo, F.; Patrascu, J.M.; Trocan, I.; Prejbeanu, R.; Florescu, S.; Damian, G.; Benagiano, V.; Abbinante, A.; Caprio, M.; et al. Anterior Cruciate Ligament Reconstruction and Determination of Tunnel Size and Graft Obliquity. Eur. Rev. Med. Pharmacol. Sci. 2015, 19, 357–364. [Google Scholar] [PubMed]
- Isacco, C.G.; Ballini, A.; De Vito, D.; Nguyen, K.C.D.; Cantore, S.; Bottalico, L.; Quagliuolo, L.; Boccellino, M.; Di Domenico, M.; Santacroce, L.; et al. Rebalancing the Oral Microbiota as an Efficient Tool in Endocrine, Metabolic and Immune Disorders. Endocr. Metab. Immune Disord Drug Targets 2021, 21, 777–784. [Google Scholar] [CrossRef]
- Contaldo, M.; Fusco, A.; Stiuso, P.; Lama, S.; Gravina, A.G.; Itro, A.; Federico, A.; Itro, A.; Dipalma, G.; Inchingolo, F.; et al. Oral Microbiota and Salivary Levels of Oral Pathogens in Gastro-Intestinal Diseases: Current Knowledge and Exploratory Study. Microorganisms 2021, 9, 1064. [Google Scholar] [CrossRef] [PubMed]
- Corriero, A.; Gadaleta, R.M.; Puntillo, F.; Inchingolo, F.; Moschetta, A.; Brienza, N. The Central Role of the Gut in Intensive Care. Critical. Care 2022, 26, 379. [Google Scholar] [CrossRef]
- Farias da Cruz, M.; Baraúna Magno, M.; Alves Jural, L.; Pimentel, T.C.; Masterson Tavares Pereira Ferreira, D.; Almeida Esmerino, E.; Luis Paiva Anciens Ramos, G.; Vicente Gomila, J.; Cristina Silva, M.; Cruz, A.G.d.; et al. Probiotics and Dairy Products in Dentistry: A Bibliometric and Critical Review of Randomized Clinical Trials. Food Res. Int. 2022, 157, 111228. [Google Scholar] [CrossRef] [PubMed]
- Signorini, L.; Ballini, A.; Arrigoni, R.; De Leonardis, F.; Saini, R.; Cantore, S.; De Vito, D.; Coscia, M.F.; Dipalma, G.; Santacroce, L.; et al. Evaluation of a Nutraceutical Product with Probiotics, Vitamin D, Plus Banaba Leaf Extracts (Lagerstroemia Speciosa) in Glycemic Control. Endocr. Metab. Immune Disord Drug Targets 2021, 21, 1356–1365. [Google Scholar] [CrossRef]
- Santacroce, L.; Inchingolo, F.; Topi, S.; Del Prete, R.; Di Cosola, M.; Charitos, I.A.; Montagnani, M. Potential Beneficial Role of Probiotics on the Outcome of COVID-19 Patients: An Evolving Perspective. Diabetes Metab. Syndr. Clin. Res. Rev. 2021, 15, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Minervini, G.; Franco, R.; Marrapodi, M.M.; Crimi, S.; Badnjević, A.; Cervino, G.; Bianchi, A.; Cicciù, M. Correlation between Temporomandibular Disorders (TMD) and Posture Evaluated Trough the Diagnostic Criteria for Temporomandibular Disorders (DC/TMD): A Systematic Review with Meta-Analysis. J. Clin. Med. 2023, 12, 2652. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.D.; Cazzolla, A.P.; Di Cosola, M.; Greco Lucchina, A.; Santacroce, L.; Charitos, I.A.; Topi, S.; Malcangi, G.; Hazballa, D.; Scarano, A.; et al. The Integumentary System and Its Microbiota between Health and Disease. J. Biol. Regul. Homeost Agents 2021, 35, 303–321. [Google Scholar] [CrossRef] [PubMed]
- Minervini, G.; Franco, R.; Marrapodi, M.M.; Fiorillo, L.; Cervino, G.; Cicciù, M. Prevalence of Temporomandibular Disorders (TMD) in Pregnancy: A Systematic Review with Meta-Analysis. J. Oral. Rehabil. 2023, 50, 627–634. [Google Scholar] [CrossRef]
- Progress in Oral Microbiome Related to Oral and Systemic Diseases: An Update - PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/34359364/ (accessed on 24 July 2023).
- Minervini, G.; Franco, R.; Marrapodi, M.M.; Fiorillo, L.; Cervino, G.; Cicciù, M. Economic Inequalities and Temporomandibular Disorders: A Systematic Review with Meta-Analysis. J. Oral. Rehabil. 2023, 50, 715–723. [Google Scholar] [CrossRef] [PubMed]
- Dipalma, G.; Inchingolo, A.D.; Inchingolo, F.; Charitos, I.A.; Di Cosola, M.; Cazzolla, A.P. Focus on the Cariogenic Process: Microbial and Biochemical Interactions with Teeth and Oral Environment. J. Biol. Regul. Homeost Agents 2021, 35. [Google Scholar] [CrossRef]
- Malcangi, G.; Patano, A.; Guglielmo, M.; Sardano, R.; Palmieri, G.; Di Pede, C.; de Ruvo, E.; Inchingolo, A.D.; Mancini, A.; Inchingolo, F.; et al. Precision Medicine in Oral Health and Diseases: A Systematic Review. J. Pers. Med. 2023, 13, 725. [Google Scholar] [CrossRef] [PubMed]
- Andersson, H.; Asp, N.-G.; Bruce, Å.; Roos, S.; Wadström, T.; Wold, A.E. Health Effects of Probiotics and Prebiotics A Literature Review on Human Studies. Food Nutr. Res. 2001, 45, 58–75. [Google Scholar] [CrossRef]
- Santacroce, L.; Sardaro, N.; Topi, S.; Pettini, F.; Bottalico, L.; Cantore, S.; Cascella, G.; Del Prete, R.; Dipalma, G.; Inchingolo, F. The Pivotal Role of Oral Microbiota in Health and Disease. J. Biol. Regul. Homeost Agents 2020, 34, 733–737. [Google Scholar] [CrossRef] [PubMed]
- Matsubara, V.H.; Bandara, H.M.H.N.; Mayer, M.P.A.; Samaranayake, L.P. Probiotics as Antifungals in Mucosal Candidiasis. Clin Infect Dis. 2016, 62, 1143–1153. [Google Scholar] [CrossRef]
- Di Cosola, M.; Cazzolla, A.P.; Charitos, I.A.; Ballini, A.; Inchingolo, F.; Santacroce, L. Candida Albicans and Oral Carcinogenesis. A Brief Review. JoF 2021, 7, 476. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.D.; Malcangi, G.; Inchingolo, A.M.; Piras, F.; Settanni, V.; Garofoli, G.; Palmieri, G.; Ceci, S.; Patano, A.; De Leonardis, N.; et al. Benefits and Implications of Resveratrol Supplementation on Microbiota Modulations: A Systematic Review of the Literature. IJMS 2022, 23, 4027. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Rath, G.K.; Chaudhary, S.P.; Thakar, A.; Mohanti, B.K.; Bahadur, S. Lactobacillus Brevis CD2 Lozenges Reduce Radiation- and Chemotherapy-Induced Mucositis in Patients with Head and Neck Cancer: A Randomized Double-Blind Placebo-Controlled Study. Eur. J. Cancer 2012, 48, 875–881. [Google Scholar] [CrossRef] [PubMed]
- Borsani, E.; Bonazza, V.; Buffoli, B.; Nocini, P.F.; Albanese, M.; Zotti, F.; Inchingolo, F.; Rezzani, R.; Rodella, L.F. Beneficial Effects of Concentrated Growth Factors and Resveratrol on Human Osteoblasts In Vitro Treated with Bisphosphonates. BioMed Res. Int. 2018, 2018, 1–13. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Inchingolo, A.M.; Malcangi, G.; Avantario, P.; Azzollini, D.; Buongiorno, S.; Viapiano, F.; Campanelli, M.; Ciocia, A.M.; De Leonardis, N.; et al. Effects of Resveratrol, Curcumin and Quercetin Supplementation on Bone Metabolism—A Systematic Review. Nutrients 2022, 14, 3519. [Google Scholar] [CrossRef] [PubMed]
- Hasslöf, P.; Granqvist, L.; Stecksén-Blicks, C.; Twetman, S. Prevention of Recurrent Childhood Caries with Probiotic Supplements: A Randomized Controlled Trial with a 12-Month Follow-Up. Probiotics Antimicrob. Proteins 2022. [Google Scholar] [CrossRef] [PubMed]
- Effects of Probiotic Bacterium Weissella Cibaria CMU on Periodontal Health and Microbiota: A Randomised, Double-Blind, Placebo-Controlled Trial - PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/32878603/ (accessed on 12 July 2023).
- Effect of Probiotic Bacteria in Composition of Children’s Saliva - PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/30716917/ (accessed on 12 July 2023).
- Invernici, M.M.; Furlaneto, F.A.C.; Salvador, S.L.; Ouwehand, A.C.; Salminen, S.; Mantziari, A.; Vinderola, G.; Ervolino, E.; Santana, S.I.; Silva, P.H.F.; et al. Bifidobacterium Animalis Subsp Lactis HN019 Presents Antimicrobial Potential against Periodontopathogens and Modulates the Immunological Response of Oral Mucosa in Periodontitis Patients. PLoS One 2020, 15, e0238425. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.-S.; Kim, M.; Nam, S.-H.; Kang, M.-S.; Lee, S.-A. Effects of Oral Probiotics on Subjective Halitosis, Oral Health, and Psychosocial Health of College Students: A Randomized, Double-Blind, Placebo-Controlled Study. Int. J. Environ. Res. Public Health 2021, 18, 1143. [Google Scholar] [CrossRef]
- Staszczyk, M.; Jamka-Kasprzyk, M.; Kościelniak, D.; Cienkosz-Stepańczak, B.; Krzyściak, W.; Jurczak, A. Effect of a Short-Term Intervention with Lactobacillus Salivarius Probiotic on Early Childhood Caries-An Open Label Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2022, 19, 12447. [Google Scholar] [CrossRef]
- Laleman, I.; Pauwels, M.; Quirynen, M.; Teughels, W. The Usage of a Lactobacilli Probiotic in the Non-Surgical Therapy of Peri-Implantitis: A Randomized Pilot Study. Clin. Oral. Implants Res. 2020, 31, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Santana, S.I.; Silva, P.H.F.; Salvador, S.L.; Casarin, R.C.V.; Furlaneto, F.A.C.; Messora, M.R. Adjuvant Use of Multispecies Probiotic in the Treatment of Peri-Implant Mucositis: A Randomized Controlled Trial. J. Clin. Periodontol. 2022, 49, 828–839. [Google Scholar] [CrossRef] [PubMed]
- Comparative Evaluation of the Antimicrobial Effects of Probiotic Milk and Probiotic Powder on the Salivary Streptococcus Mutans Counts and the Plaque Scores in Children Aged 3-6 Years: A Randomized Controlled Trial - PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/35302301/ (accessed on 12 July 2023).
- Role of Probiotics and Synbiotics on Inhibiting Streptococcus Mutans Level in Saliva of Children: A Randomized Controlled Trial - PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/34810344/ (accessed on 12 July 2023).
- A Dual-Strain Lactobacilli Reuteri Probiotic Improves the Treatment of Residual Pockets: A Randomized Controlled Clinical Trial - PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/31520543/ (accessed on 12 July 2023).
- Schlagenhauf, U.; Rehder, J.; Gelbrich, G.; Jockel-Schneider, Y. Consumption of Lactobacillus Reuteri-Containing Lozenges Improves Periodontal Health in Navy Sailors at Sea: A Randomized Controlled Trial. J. Periodontol. 2020, 91, 1328–1338. [Google Scholar] [CrossRef]
- Qamar, Z.; Alghamdi, A.M.S.; Haydarah, N.K.B.; Balateef, A.A.; Alamoudi, A.A.; Abumismar, M.A.; Shivakumar, S.; Cicciù, M.; Minervini, G. Impact of Temporomandibular Disorders on Oral Health-related Quality of Life: A Systematic Review and Meta-analysis. J. Oral Rehabil. 2023. [Google Scholar] [CrossRef] [PubMed]
- Rapone, B.; Ferrara, E.; Santacroce, L.; Topi, S.; Gnoni, A.; Dipalma, G.; Mancini, A.; Di Domenico, M.; Tartaglia, G.M.; Scarano, A.; et al. The Gaseous Ozone Therapy as a Promising Antiseptic Adjuvant of Periodontal Treatment: A Randomized Controlled Clinical Trial. Int. J. Environ. Res. Public Health 2022, 19, 985. [Google Scholar] [CrossRef] [PubMed]
- Minervini, G.; Franco, R.; Marrapodi, M.M.; Ronsivalle, V.; Shapira, I.; Cicciù, M. Prevalence of Temporomandibular Disorders in Subjects Affected by Parkinson Disease: A Systematic Review and Metanalysis. J. Oral Rehabil. 2023. [Google Scholar] [CrossRef]
- Adina, S.; Dipalma, G.; Bordea, I.R.; Lucaciu, O.; Feurdean, C.; Inchingolo, A.D.; Septimiu, R.; Malcangi, G.; Cantore, S.; Martin, D.; et al. Orthopedic Joint Stability Influences Growth and Maxillary Development: Clinical Aspects. J. Biol. Regul. Homeost Agents 2020, 34, 747–756. [Google Scholar] [CrossRef]
- Inchingolo, F.; Martelli, F.S.; Gargiulo Isacco, C.; Borsani, E.; Cantore, S.; Corcioli, F.; Boddi, A.; Nguyễn, K.C.D.; De Vito, D.; Aityan, S.K.; et al. Chronic Periodontitis and Immunity, Towards the Implementation of a Personalized Medicine: A Translational Research on Gene Single Nucleotide Polymorphisms (SNPs) Linked to Chronic Oral Dysbiosis in 96 Caucasian Patients. Biomedicines 2020, 8, 115. [Google Scholar] [CrossRef] [PubMed]



| Criteria | Application in the Present Study |
|---|---|
| Population | Both children and adults |
| Intervention | Use of PBs to improve oral health |
| Comparisons | Comparing effect of use of PBs on different oral pathologies |
| Outcomes | Efficacy in preventing caries, periodontal disease, halitosis, mucositis, and periimplantitis |
| Study design | Clinical Trials. |
| Authors | Type of Study | Object | Study Design and Timeline | Results | Number of Participants | nn |
|---|---|---|---|---|---|---|
| Duraisamy et al., 2021 [39] | Randomized controlled trial | After 15 days of daily consumption of probiotic and synbiotic curd, this study seeks to determine how well PBs and synbiotics inhibit the level of S. mutans in children’s saliva. | 40 children aged 6–12 received probiotic and synbiotic curd for 15 days, saliva samples collected, and S. mutans levels estimated. | Both groups showed significant decrease in salivary S. mutans counts, with probiotic group showing higher growth inhibition. | ||
| Sarmento et al., 2019 [32] | Clinical study | Evaluate the impact of petit-suisse cheese added with PBs on the salivary microbiota of children | Administration of cheese fortified with L. casei for 28 days and subsequent evaluation of saliva | The probiotic microorganisms that can be carried by the petit-suisse cheese have been developed, offering a potential substitute for reducing potentially harmful microbiota in the mouth | ||
| Janiani et al., 2022 [38] | Randomized controlled trial | To investigate the impact of a brief intake of probiotic milk on children’s plaque scores and salivary number of S. mutans | Administration of PBs for one week to 34 children aged 3 to 6 years, final comparison with control group | There was a very important reduction in S. mutans in saliva with karyostatic effect after probiotic intake, but no known long-term effects | 34 | |
| Invernici et al., 2020 [33] | Randomized clinical trial | Evaluate the effects of Bifidobacterium animalis subsp. lactis HN019 on clinical periodontal parameters, immunocompetence, and saliva immunological properties. | Scaling and root planing (SRP) was performed on thirty patients, and they were observed at the beginning, at 30, and at 90 days. Probiotic lozenges were administered to the participants for 30 days in either the Test or Control groups. | The probiotic B. lactis HN019 may enhance the results of non-surgical periodontal therapy | 30 | |
| Lee et al., 2021 [34] | Randomized, Double-Blind, Placebo-Controlled Study | The purpose of this research was to determine how taking tablets of the oral probiotic Weissella cibaria (W. cibaria) affected psychosocial indicators and halitosis. | Random selection was used to place the participants in either the experimental or control groups. Depending on which group they belonged to, they consumed W. cibaria CMU or a placebo just before going to sleep every day for eight weeks. | For eight weeks, taking the oral probiotic could be a helpful nursing intervention for halitosis reduction and quality-of-life enhancement in relation to oral health | 100 | |
| Staszczyk et al., 2022 [35] | Open Label Randomized Controlled Trial | Determine if chewing tablets containing thermally inactivated L. salivarius decreased the 12-month caries increase relative to the control group after two weeks of daily ingestion. | A study involving 140 healthy children aged 3–6 with or without ECC was conducted. The primary end measure was the 1-year increase in dental caries incidence and prevalence, while secondary outcomes included cavitated and apparent dentinal caries and dental plaque buildup | The probiotic group’s initial and end mean OHI-S scores did not significantly differ from one another. In conclusion, consistent short-term consumption of PBs may slow the onset of caries. | 140 | |
| Laleman et al., 2020 [40] | Randomized controlled clinical trial | To investigate the supplemental impact of a probiotic Lactobacillus reuteri strain on the re-instrumentation of residual pockets. | 39 periodontitis patients underwent re-instrumentation, probiotic or placebo drops administered, and lozenges for 12 weeks. Examined probing pocket depth, recession, bleeding on probing, and plaque levels | Probiotic lozenges significantly reduced overall PPD after 24 weeks, especially in intermediate and deep pockets, with fewer surgically necessary sites and pockets. The group reduced thickness from 4 mm to 3 mm at 24 weeks. | 39 | |
| Santana et al., 2022 [37] | Randomized controlled trial | Check the effects of a multispecies probiotic supplemented with mechanical debridement (MD) on changes in BOP in edentulous patients with peri-implant mucositis (PiM). The supplement contains Lactobacillus rhamnosus HN001TM, Lactobacillus paracasei Lpc-37®, and Bifidobacterium animalis subsp. lactis HN019TM. | Patients were randomly assigned to probiotic test or placebo control groups. MD and topical gel applications were applied twice daily for 12 weeks. Clinical and immunological measurements were taken at baseline, 12, and 24 weeks. Statistical analysis was used. | 36 | ||
| Laleman et al., 2019 [36] | Randomized pilot study | Analyze the clinical and microbiological advantages of a dual-strain probiotic of L. reuteri for the non-surgical treatment of first peri-implantitis. | Patients with peri-implantitis underwent full-mouth prophylaxis and cleaned sites. Study lozenges and drops were applied to peri-implantitis areas, with probiotics and placebos given. Implant-level variables, bleeding, PPD, full-mouth bleeding, plaque scores, and subgingival, tongue, and saliva samples were analyzed for microbes. | statistically significant difference. After 12 and 24 weeks, clinical measures showed significant decreases. The probiotic group experienced a greater decline in plaque levels at implant level, while the probiotic group had a larger reduction in full-mouth BOP sites. No measurable microbiological changes were observed. | 10 | |
| Schlagenhauf et al., 2020 [41] | Randomized controlled trial | The purpose of this trial was to establish if the regular consumption of L. reuteri PBs can help periodontal health and oral health in navy sailors. | A 42-day study involved 72 healthy sailors in two groups: the test group, who consumed probiotic strains of L. reuteri twice daily, and the placebo group, who received no PBs. Primary outcome was bone marrow opacity. | Probiotic L. reuteri strains consumption significantly improved test group scores at 14 and 42 days, proving a practical and easy method for maintaining periodontal health and oral care. | 72 | |
| Kang et al., 2020 [31] | Randomized, double-blind, placebo-controlled trial | The aim of this study was to evaluate the effects of W. cibaria CMU (oraCMU)on periodontal health and oral microbiota | 92 adults (20–39 years old) without periodontitis underwent dental scaling and root planing and were randomized to either the probiotic or placebo groups. When taken once daily for eight weeks, the 800 mg probiotic tablet delivered 1.0 108 CFU/g of W. cibaria CMU (oraCMU). BOP, PD, GI, plaque index (PI), and microbiota in the gingival sulcus were all examined as periodontal clinical parameters. | Over an 8-week period, BOP improved more in the probiotic group. During the intervention, no discernible inter-group differences in PD, GI, or PI were found. The probiotic group was found to have fewer oral bacteria. At 8 weeks, there was a significant difference between the two groups in the levels of Fusobacterium nucleatum (F. Nucleatum) and Staphylococcus aureus. For patients with periodontitis, CMU enhances BOP and the oral environment. | 92 | |
| Hasslof et al., 2022 [30] | Randomized controlled trial | To assess the impact of drops containing probiotic bacteria on dental caries recurrence in preschoolers | 38 preschoolers were enrolled after receiving extensive restorative care while sedated or under general anesthesia, and they were monitored again at 6 and 12 months. Parents of kids in the test group were told to put 5 drops of two strains of L. reuteri in their children’s mouths at bedtime each day. | There were no notable variations between the groups. | 38 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Inchingolo, F.; Inchingolo, A.M.; Malcangi, G.; De Leonardis, N.; Sardano, R.; Pezzolla, C.; de Ruvo, E.; Di Venere, D.; Palermo, A.; Inchingolo, A.D.; et al. The Benefits of Probiotics on Oral Health: Systematic Review of the Literature. Pharmaceuticals 2023, 16, 1313. https://doi.org/10.3390/ph16091313
Inchingolo F, Inchingolo AM, Malcangi G, De Leonardis N, Sardano R, Pezzolla C, de Ruvo E, Di Venere D, Palermo A, Inchingolo AD, et al. The Benefits of Probiotics on Oral Health: Systematic Review of the Literature. Pharmaceuticals. 2023; 16(9):1313. https://doi.org/10.3390/ph16091313
Chicago/Turabian StyleInchingolo, Francesco, Angelo Michele Inchingolo, Giuseppina Malcangi, Nicole De Leonardis, Roberta Sardano, Carmela Pezzolla, Elisabetta de Ruvo, Daniela Di Venere, Andrea Palermo, Alessio Danilo Inchingolo, and et al. 2023. "The Benefits of Probiotics on Oral Health: Systematic Review of the Literature" Pharmaceuticals 16, no. 9: 1313. https://doi.org/10.3390/ph16091313
APA StyleInchingolo, F., Inchingolo, A. M., Malcangi, G., De Leonardis, N., Sardano, R., Pezzolla, C., de Ruvo, E., Di Venere, D., Palermo, A., Inchingolo, A. D., Corriero, A., & Dipalma, G. (2023). The Benefits of Probiotics on Oral Health: Systematic Review of the Literature. Pharmaceuticals, 16(9), 1313. https://doi.org/10.3390/ph16091313













