Tween 80-Based Self-Assembled Mixed Micelles Boost Valsartan Transdermal Delivery
Abstract
:1. Introduction
2. Results
2.1. Formulation Factors
2.2. Characterization of the Mixed Micelle Formulations
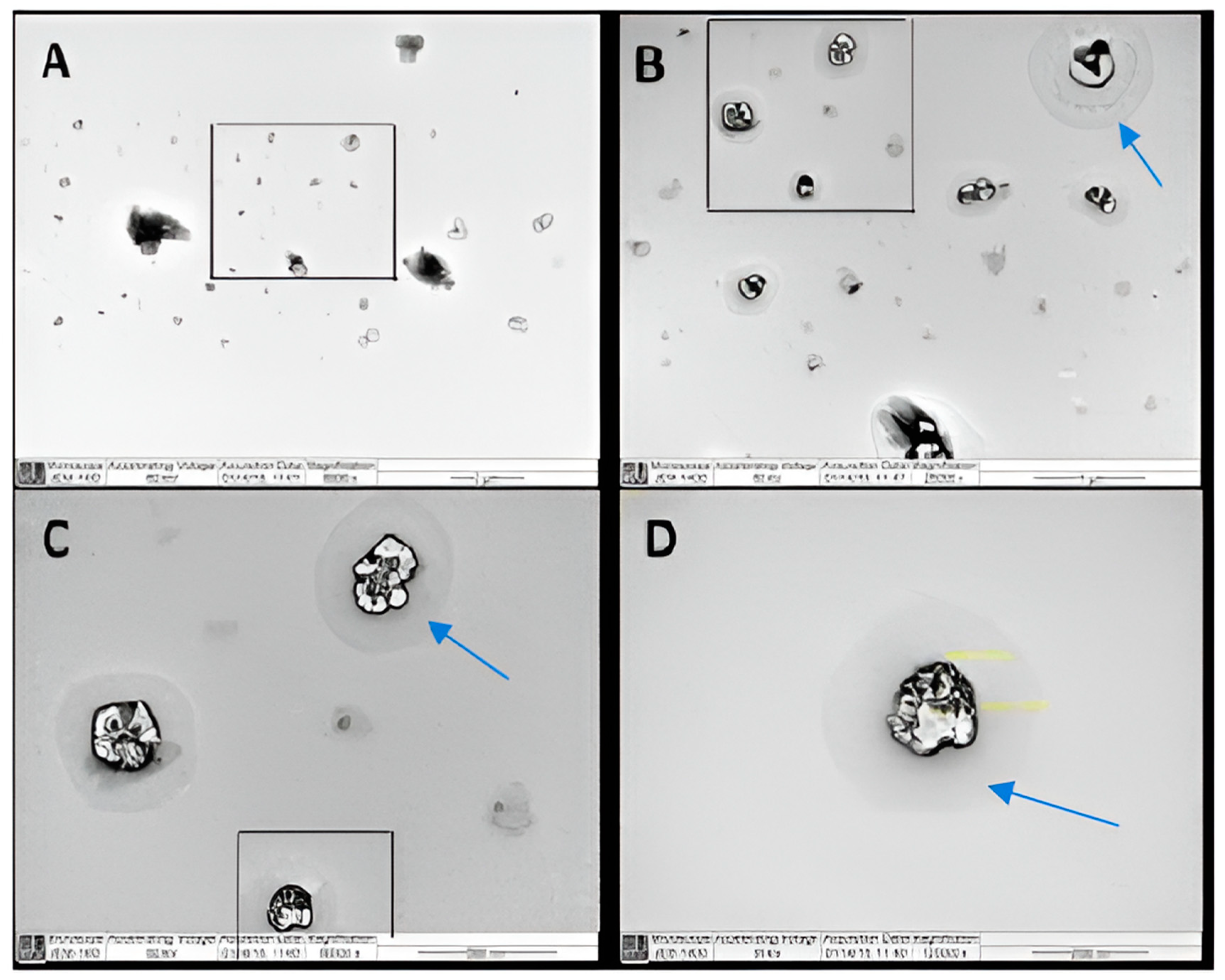
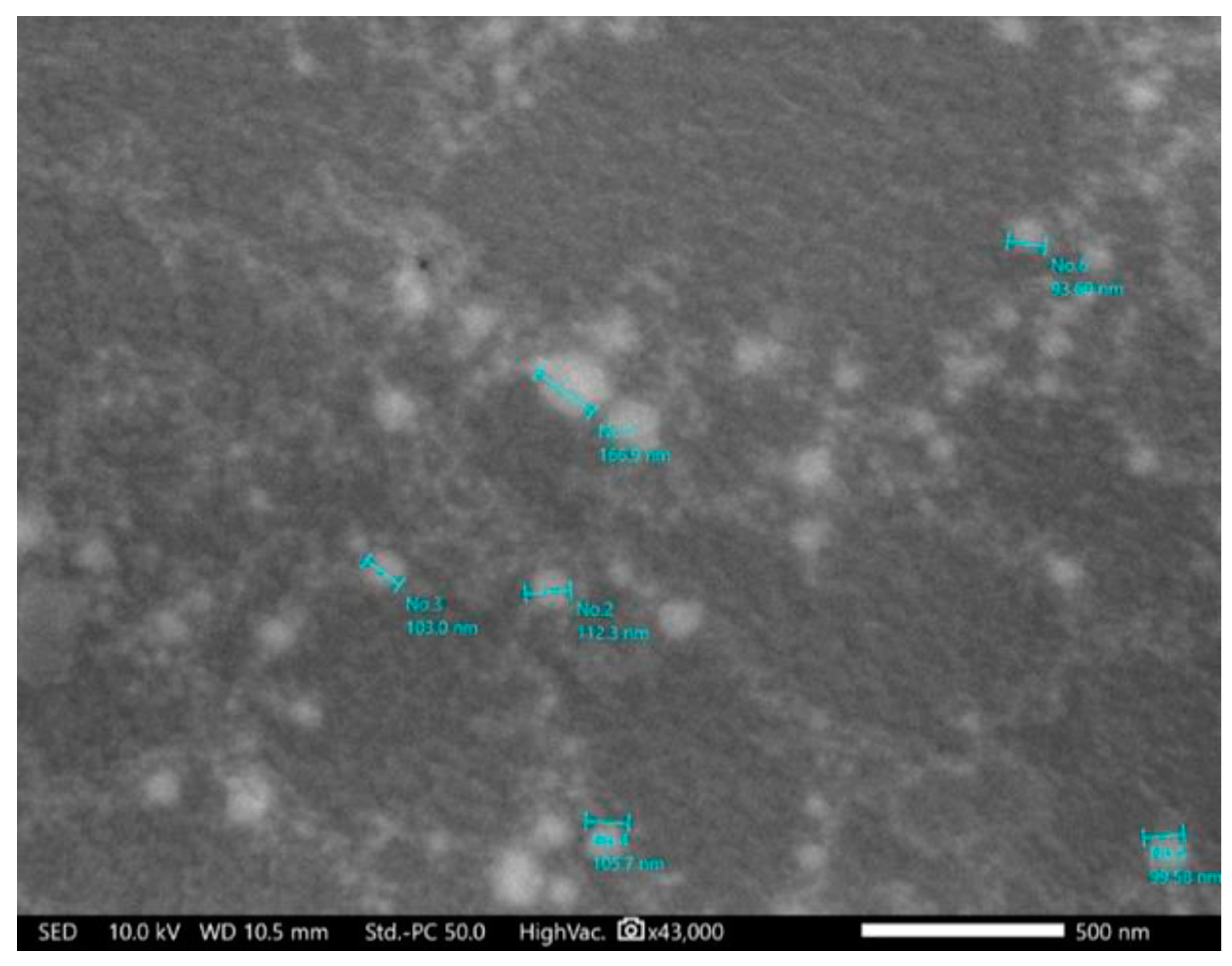
2.2.1. Particle Size, Polydispersity Index (PDI), Zeta Potential, and Structural Morphology
2.2.2. Drug Entrapment Efficiency (EE)
2.2.3. Validation of High-Performance Liquid Chromatography (HPLC) Method
2.2.4. In Vitro Release
2.2.5. In Vitro Skin Permeation Studies
3. Discussion
4. Materials and Methods
4.1. Materials
4.2. Preparation of Val-Loaded Mixed Micelles
4.2.1. The Micro-Phase Separation Method
4.2.2. The Thin-Film Hydration Method
4.2.3. Particle Size, PDI, and Zeta Potential
4.2.4. Drug EE
4.2.5. Particles Morphology
4.2.6. In Vitro Release Profile Study
4.2.7. Release Kinetic Analysis
4.3. In Vitro Skin Permeation Studies
Permeation Data Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- ClinCal.com. TheT 200 of 2020, Version 2022.08. Available online: https://clincalc.com/DrugStats/Top200Drugs.aspx (accessed on 23 October 2023).
- Dixit, A.R.; Rajput, S.J.; Patel, S.G. Preparation and bioavailability assessment of SMEDDS containing valsartan. AAPS PharmSciTech. 2010, 11, 314–321. [Google Scholar] [CrossRef] [PubMed]
- Ahad, A.; Aqil, M.; Kohli, K.; Sultana, Y.; Mujeeb, M.; Ali, A. Role of novel terpenes in transcutaneous permeation of valsartan: Effectiveness and mechanism of action. Drug Dev. Ind. Pharm. 2011, 37, 583–596. [Google Scholar] [CrossRef] [PubMed]
- Aqil, M.; Sultana, Y.; Ali, A. Matrix type transdermal drug delivery systems of metoprolol tartrate: In vitro characterization. Acta Pharm. 2003, 53, 119–125. [Google Scholar] [PubMed]
- Ahad, A.; Aqil, M.; Ali, A. Investigation of antihypertensive activity of carbopol valsartan transdermal gel containing 1,8-cineole. Int. J. Biol. Macromol. 2014, 64, 144–149. [Google Scholar] [CrossRef] [PubMed]
- Nishida, N.; Taniyama, K.; Sawabe, T.; Manome, Y. Development and evaluation of a monolithic drug-in-adhesive patch for valsartan. Int. J. Pharm. 2010, 402, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Ahad, A.; Aqil, M.; Ali, A. The application of anethole, menthone, and eugenol in transdermal penetration of valsartan: Enhancement and mechanistic investigation. Pharm. Biol. 2016, 54, 1042–1051. [Google Scholar] [CrossRef] [PubMed]
- Williams, A.C.; Barry, B.W. Penetration enhancers. Adv. Drug Deliv. Rev. 2004, 56, 603–618. [Google Scholar] [CrossRef] [PubMed]
- Morteza-Semnani, K.; Saeedi, M.; Akbari, J.; Eghbali, M.; Babaei, A.; Hashemi, S.M.H.; Nokhodchi, A. Development of a novel nanoemulgel formulation containing cumin essential oil as skin permeation enhancer. Drug Deliv. Transl. Res. 2022, 12, 1455–1465. [Google Scholar] [CrossRef]
- Thong, H.Y.; Zhai, H.; Maibach, H.I. Percutaneous penetration enhancers: An overview. Skin Pharmacol. Physiol. 2007, 20, 272–282. [Google Scholar] [CrossRef]
- Afouna, M.I.; Fincher, T.K.; Zaghloul, A.A.; Reddy, I.K. Effect of Azone upon the in vivo antiviral efficacy of cidofovir or acyclovir topical formulations in treatment/prevention of cutaneous HSV-1 infections and its correlation with skin target site free drug concentration in hairless mice. Int. J. Pharm. 2003, 253, 159–168. [Google Scholar] [CrossRef]
- Herman, A.; Herman, A.P. Essential oils and their constituents as skin penetration enhancer for transdermal drug delivery: A review. J. Pharm. Pharmacol. 2015, 67, 473–485. [Google Scholar] [CrossRef] [PubMed]
- Aungst, B.J. Structure/effect studies of fatty acid isomers as skin penetration enhancers and skin irritants. Pharm. Res. 1989, 6, 244–247. [Google Scholar] [CrossRef] [PubMed]
- Akbari, J.; Saeedi, M.; Farzin, D.; Morteza-Semnani, K.; Esmaili, Z. Transdermal absorption enhancing effect of the essential oil of Rosmarinus officinalis on percutaneous absorption of Na diclofenac from topical gel. Pharm. Biol. 2015, 53, 1442–1447. [Google Scholar] [CrossRef] [PubMed]
- Massadeh, S.; Omer, M.E.; Alterawi, A.; Ali, R.; Alanazi, F.H.; Almutairi, F.; Almotairi, W.; Alobaidi, F.F.; Alhelal, K.; Almutairi, M.S.; et al. Optimized polyethylene glycolylated polymer-lipid hybrid nanoparticles as a potential breast cancer treatment. Pharmaceutics 2020, 12, 666. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Pandey, V.K.; Tewari, R.P.; Agarwal, V. Nanoparticle based drug delivery system: Advantages and applications. Ind. J. Sci. Tech. 2011, 4, 177–184. [Google Scholar] [CrossRef]
- Cho, K.; Wang, X.; Nie, S.; Chen, Z.G.; Shin, D.M. Therapeutic nanoparticles for drug delivery in cancer. Clin. Cancer Res. 2008, 14, 1310–1316. [Google Scholar] [CrossRef] [PubMed]
- Yassin, A.; Alkatheri, A.; Sharma, R. Anticancer-loaded solid lipid nanoparticles: High potential advancement in chemotherapy. Dig. J. Nanomater. Bios. 2013, 8, 905–916. [Google Scholar]
- Husseini, G.A.; Pitt, W.G. Micelles and nanoparticles for ultrasonic drug and gene delivery. Adv. Drug Deliv. Rev. 2008, 60, 1137–1152. [Google Scholar] [CrossRef]
- Mao, Y.; Chen, X.; Xu, B.; Shen, Y.; Ye, Z.; Chaurasiya, B.; Liu, L.; Li, Y.; Xing, X.; Chen, D. Eprinomectin nanoemulgel for transdermal delivery against endoparasites and ectoparasites: Preparation, in vitro and in vivo evaluation. Drug Deliv. 2019, 26, 1104–1114. [Google Scholar] [CrossRef]
- Virani, A.; Puri, V.; Mohd, H.; Michniak-Kohn, B. Effect of penetration enhancers on transdermal delivery of oxcarbazepine, an antiepileptic drug using microemulsions. Pharmaceutics 2023, 15, 183. [Google Scholar] [CrossRef]
- Liu, D.; Ge, Y.; Tang, Y.; Yuan, Y.; Zhang, Q.; Li, R.; Xu, Q. Solid lipid nanoparticles for transdermal delivery of diclofenac sodium: Preparation, characterization and in vitro studies. J. Microencapsul. 2010, 27, 726–734. [Google Scholar] [CrossRef] [PubMed]
- Parra, A.; Jarak, I.; Santos, A.; Veiga, F.; Figueiras, A. Polymeric micelles: A promising pathway for dermal drug delivery. Materials 2021, 14, 7278. [Google Scholar] [CrossRef] [PubMed]
- Muzzalupo, R.; Tavano, L. Niosomal drug delivery for transdermal targeting: Recent advances. Res. Rep. Transdermal Drug Deliv. 2015, 4, 23–33. [Google Scholar] [CrossRef]
- Atanase, L.I. Micellar drug delivery systems based on natural biopolymers. Polymers 2021, 13, 477. [Google Scholar] [CrossRef] [PubMed]
- Hussein, Y.H.A.; Youssry, M. Polymeric micelles of biodegradable diblock copolymers: Enhanced encapsulation of hydrophobic drugs. Materials 2018, 11, 688. [Google Scholar] [CrossRef] [PubMed]
- Atanase, L.I.; Riess, G. Self-assembly of block and graft copolymers in organic solvents: An overview of recent advances. Polymers 2018, 10, 62. [Google Scholar] [CrossRef] [PubMed]
- Deng, C.; Jiang, Y.; Cheng, R.; Meng, F.; Zhong, Z. Biodegradable polymeric micelles for targeted and controlled anticancer drug delivery: Promises, progress and prospects. Nano Today 2012, 7, 467–480. [Google Scholar] [CrossRef]
- Rangel-Yagui, C.O.; Pessoa, A., Jr.; Tavares, L.C. Micellar solubilization of drugs. J. Pharm. Pharm. Sci. 2005, 8, 147–165. [Google Scholar]
- Mall, S.; Buckton, G.; Rawlins, D.A. Dissolution behaviour of sulphonamides into sodium dodecyl sulfate micelles: A thermodynamic approach. J. Pharm. Sci. 1996, 85, 75–78. [Google Scholar] [CrossRef]
- Aliabadi, H.M.; Lavasanifar, A. Polymeric micelles for drug delivery. Expert Opin. Drug Deliv. 2006, 3, 139–162. [Google Scholar] [CrossRef]
- Gothwal, A.; Khan, I.; Gupta, U. Polymeric micelles: Recent advancements in the delivery of anticancer drugs. Pharm. Res. 2016, 33, 18–39. [Google Scholar] [CrossRef] [PubMed]
- FitzGerald, P.A.; Chatjaroenporn, K.; Warr, G.G. Structure and composition of mixed micelles of polymerized and monomeric surfactants. J. Coll. Interface Sci. 2015, 449, 377–382. [Google Scholar] [CrossRef] [PubMed]
- Rupp, C.; Steckel, H.; Müller, B.W. Mixed micelle formation with phosphatidylcholines: The influence of surfactants with different molecule structures. Int. J. Pharm. 2010, 387, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Li, J.; Yu, H.; Wang, G.; Liu, W. Synthesis and characterization of a novel polydepsipeptide contained tri-block copolymer (mPEG-PLLA-PMMD) as self-assembly micelle delivery system for paclitaxel. Int. J. Pharm. 2012, 430, 282–291. [Google Scholar] [CrossRef] [PubMed]
- Yoo, H.S.; Park, T.G. Biodegradable polymeric micelles composed of doxorubicin conjugated PLGA-PEG block copolymer. J. Control. Release 2001, 70, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Zhang, W.; Gu, J.; Ren, Q.; Fan, Z.; Zhong, W.; Fang, X.; Sha, X. Enhanced antitumor efficacy by methotrexate conjugated Pluronic mixed micelles against KBv multidrug resistant cancer. Int. J. Pharm. 2013, 452, 421–433. [Google Scholar] [CrossRef] [PubMed]
- Opanasopit, P.; Yokoyama, M.; Watanabe, M.; Kawano, K.; Maitani, Y.; Okano, T. Block copolymer design for camptothecin incorporation into polymeric micelles for passive tumor targeting. Pharm. Res. 2004, 21, 2001–2008. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Huang, H.; Xia, Z.; Wei, Y.; Yao, N.; Zhang, L.; Yan, H.; Jia, X.; Zhang, Z. TPGS/phospholipids mixed micelles for delivery of icariside II to multidrug-resistant breast cancer. Integr. Cancer Ther. 2016, 15, 390–399. [Google Scholar] [CrossRef]
- Ould-Ouali, L.; Noppe, M.; Langlois, X.; Willems, B.; Te Riele, P.; Timmerman, P.; Brewster, M.E.; Ariën, A.; Préat, V. Self-assembling PEG-p(CL-co-TMC) copolymers for oral delivery of poorly water-soluble drugs: A case study with risperidone. J. Control. Release 2005, 102, 657–668. [Google Scholar] [CrossRef]
- Patil, S.; Choudhary, B.; Rathore, A.; Roy, K.; Mahadik, K. Enhanced oral bioavailability and anticancer activity of novel curcumin loaded mixed micelles in human lung cancer cells. Phytomedicine 2015, 22, 1103–1111. [Google Scholar] [CrossRef]
- Beg, S.; Swain, S.; Singh, H.P.; Patra, C.N.; Rao, M.E.B. Development, optimization, and characterization of solid self-nanoemulsifying drug delivery systems of valsartan using porous carriers. AAPS PharmSciTech. 2012, 13, 1416–1427. [Google Scholar] [CrossRef]
- Nekkanti, V.; Wang, J.; Betageri, G.V. Pharmacokinetic evaluation of improved oral bioavailability of solid valsartan: Proliposomes versus self-nanoemulsifying drug delivery system. AAPS PharmSciTech. 2016, 17, 851–860. [Google Scholar] [CrossRef] [PubMed]
- Yeom, D.W.; Chae, B.R.; Son, H.Y.; Kim, J.H.; Chae, J.S.; Song, S.H.; Oh, D.; Choi, Y.W. Enhanced oral bioavailability of valsartan using a polymer-based supersaturable self-microemulsifying drug delivery system. Int. J. Nanomed. 2017, 12, 3533–3545. [Google Scholar] [CrossRef] [PubMed]
- Aboud, H.M.; Mahmoud, M.O.; Abdeltawab Mohammed, M.; Shafiq Awad, M.; Sabry, D. Preparation and appraisal of self-assembled valsartan-loaded amalgamated Pluronic F127/Tween 80 polymeric micelles: Boosted cardioprotection via regulation of Mhrt/Nrf2 and Trx1 pathways in cisplatin-induced cardiotoxicity. J. Drug Target. 2020, 28, 282–299. [Google Scholar] [CrossRef] [PubMed]
- Chadha, R.; Bala, B.; Arora, P.; Jain, D.V.S.; Pissurlenkar, R.R.S.; Coutinho, E.C. Valsartan inclusion by methyl-β-cyclodextrin: Thermodynamics, molecular modeling, Tween 80 effect and evaluation. Carbohydr. Polym. 2014, 103, 300–309. [Google Scholar] [CrossRef] [PubMed]
- Bhosale, S.S.; Avachat, A.M. Design and development of ethosomal transdermal drug delivery system of valsartan with preclinical assessment in Wistar albino rats. J. Liposome Res. 2013, 23, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Ahad, A.; Aqil, M.; Kohli, K.; Sultana, Y.; Mujeeb, M. Enhanced transdermal delivery of an anti-hypertensive agent via nanoethosomes: Statistical optimization, characterization and pharmacokinetic assessment. Int. J. Pharm. 2013, 443, 26–38. [Google Scholar] [CrossRef]
- Ahad, A.; Aqil, M.; Kohli, K.; Sultana, Y.; Mujeeb, M. Design, formulation and optimization of valsartan transdermal gel containing iso-eucalyptol as novel permeation enhancer: Preclinical assessment of pharmacokinetics in Wistar albino rats. Expert Opin. Drug Deliv. 2014, 11, 1149–1162. [Google Scholar] [CrossRef]
- Kashanian, S.; Azandaryani, A.H.; Derakhshandeh, K. New surface-modified solid lipid nanoparticles using N-glutaryl phosphatidylethanolamine as the outer shell. Int. J. Nanomed. 2011, 6, 2393–2401. [Google Scholar]
- Thatipamula, R.; Palem, C.; Gannu, R.; Mudragada, S.; Yamsani, M. Formulation and in vitro characterization of domperidone loaded solid lipid nanoparticles and nanostructured lipid carriers. Daru J. Pharm. Sci. 2011, 19, 23–32. [Google Scholar]
- Verwey, E.J.W. Theory of the stability of lyophobic colloids. J. Phys. Coll. Chem. 1947, 51, 631–636. [Google Scholar] [CrossRef] [PubMed]
- Ding, B.; Ahmadi, S.H.; Babak, P.; Bryant, S.L.; Kantzas, A. On the stability of pickering and classical nanoemulsions: Theory and experiments. Langmuir 2023, 39, 6975–6991. [Google Scholar] [CrossRef] [PubMed]
- ICH Expert Working Group. Validation of Analytical Procedures–Text and Methodology; International Conference on Harmonization (ICH), Q2 (R1): Geneva, Switzerland, 2005. [Google Scholar]
- Ghumman, S.A.; Ijaz, A.; Noreen, S.; Aslam, A.; Kausar, R.; Irfan, A.; Latif, S.; Shazly, G.A.; Shah, P.A.; Rana, M.; et al. Formulation and characterization of curcumin niosomes: Antioxidant and cytotoxicity studies. Pharmaceuticals 2023, 16, 1406. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Q.; Zhang, B.; Wang, Y.; Liu, X.; Li, W.; Su, F.; Li, S. Self-assembled micelles prepared from poly(D,L-lactide-co-glycolide)-poly(ethylene glycol) block copolymers for sustained release of valsartan. Polym. Adv. Technol. 2021, 32, 1262–1271. [Google Scholar] [CrossRef]
- Goo, Y.T.; Park, S.Y.; Chae, B.R.; Yoon, H.Y.; Kim, C.H.; Choi, J.Y.; Song, S.H.; Choi, Y.W. Optimization of solid self-dispersing micelle for enhancing dissolution and oral bioavailability of valsartan using Box-Behnken design. Int. J. Pharm. 2020, 585, 119483. [Google Scholar] [CrossRef] [PubMed]
- Korsmeyer, R.W.; Gurny, R.; Doelker, E.; Buri, P.; Peppas, N.A. Mechanisms of solute release from porous hydrophilic polymers. Int. J. Pharm. 1983, 15, 25–35. [Google Scholar] [CrossRef]
- Peppas, N.A. Analysis of Fickian and non-Fickian drug release from polymers. Pharm. Acta Helv. 1985, 60, 110–111. [Google Scholar] [PubMed]
- Wang, H.; Chen, H. Study of the drug release kinetics in nanoscale micelle to micelle system. In Proceedings of the 2010 3rd International Nanoelectronics Conference (INEC), Hong Kong, China, 3–8 January 2010; pp. 1331–1332. [Google Scholar]
- Tao, L.; Chan, J.W.; Uhrich, K.E. Drug loading and release kinetics in polymeric micelles: Comparing dynamic versus unimolecular sugar-based micelles for controlled release. J. Bioact. Compat. Polym. 2016, 31, 227–241. [Google Scholar] [CrossRef]
- Akula, S.; Gurram, A.K.; Devireddy, S.R. Self-microemulsifying drug delivery systems: An attractive strategy for enhanced therapeutic profile. Int. Sch. Res. Notices 2014, 2014, 964051. [Google Scholar] [CrossRef]
- Alkilani, A.Z.; McCrudden, M.T.; Donnelly, R.F. Transdermal drug delivery: Innovative pharmaceutical developments based on disruption of the barrier properties of the stratum corneum. Pharmaceutics 2015, 7, 438–470. [Google Scholar] [CrossRef]
- Patel, P.V.; Patel, H.K.; Panchal, S.S.; Mehta, T.A. Self micro-emulsifying drug delivery system of tacrolimus: Formulation, in vitro evaluation and stability studies. Int. J. Pharm. Investig. 2013, 3, 95–104. [Google Scholar] [CrossRef] [PubMed]
- Seo, S.H.; Kim, E.; Joo, Y.; Lee, J.; Oh, K.T.; Hwang, S.J.; Choi, K.Y. A Mixed Micellar formulation for the transdermal delivery of an indirubin analog. Pharmaceutics 2020, 12, 175. [Google Scholar] [CrossRef] [PubMed]
- Liang, K.; Xu, K.; Bessarab, D.; Obaje, J.; Xu, C. Arbutin encapsulated micelles improved transdermal delivery and suppression of cellular melanin production. BMC Res. Notes 2016, 9, 254. [Google Scholar] [CrossRef] [PubMed]
- Omray, K. Enhanced transdermal delivery of diltiazem hydrochloride via reverse micellar transformation type liquid crystalline gel. Int. J. Pharm. Drug Anal. 2014, 2, 225–228. [Google Scholar]
- Lapteva, M.; Mondon, K.; Möller, M.; Gurny, R.; Kalia, Y.N. Polymeric micelle nanocarriers for the cutaneous delivery of tacrolimus: A targeted approach for the treatment of psoriasis. Mol. Pharm. 2014, 11, 2989–3001. [Google Scholar] [CrossRef] [PubMed]
- Khurana, B.; Arora, D.; Narang, R.K. QbD based exploration of resveratrol loaded polymeric micelles based carbomer gel for topical treatment of plaque psoriasis: In vitro, ex vivo and in vivo studies. J. Drug Deliv. Sci. Technol. 2020, 59, 101901. [Google Scholar] [CrossRef]
- Li, X.; Fan, R.; Wang, Y.; Wu, M.; Tong, A.; Shi, J.; Xiang, M.; Zhou, L.; Guo, G. In situ gel-forming dual drug delivery system for synergistic combination therapy of colorectal peritoneal carcinomatosis. RSC Adv. 2015, 5, 101494–101506. [Google Scholar] [CrossRef]
- Mendonça, P.V.; Matos, A.; Sousa, A.F.; Serra, A.C.; Simões, S.; Coelho, J.F.J. Increasing the bile acid sequestration performance of cationic hydrogels by using an advanced/controlled polymerization technique. Pharm. Res. 2017, 34, 1934–1943. [Google Scholar] [CrossRef]
- Chassaing, B.; Koren, O.; Goodrich, J.K.; Poole, A.C.; Srinivasan, S.; Ley, R.E.; Gewirtz, A.T. Dietary emulsifiers impact the mouse gut microbiota promoting colitis and metabolic syndrome. Nature 2015, 519, 92–96. [Google Scholar] [CrossRef]
- Ai, X.; Zhong, L.; Niu, H.; He, Z. Thin-film hydration preparation method and stability test of DOX-loaded disulfide-linked polyethylene glycol 5000-lysine-di-tocopherol succinate nanomicelles. Asian J. Pharm. Sci. 2014, 9, 244–250. [Google Scholar] [CrossRef]
- El Zaafarany, G.M.; Awad, G.A.; Holayel, S.M.; Mortada, N.D. Role of edge activators and surface charge in developing ultradeformable vesicles with enhanced skin delivery. Int. J. Pharm. 2010, 397, 164–172. [Google Scholar] [CrossRef] [PubMed]
- Xiong, D.; Wen, L.; Peng, S.; Xu, J.; Zhang, L. Reversible cross-linked mixed micelles for pH triggered swelling and redox triggered degradation for enhanced and controlled drug release. Pharmaceutics 2020, 12, 258. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Zhang, E.; Yang, J.; Cao, Z. Strategies to improve micelle stability for drug delivery. Nano Res. 2018, 11, 4985–4998. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Shi, Y.; Kim, J.Y.; Park, K.; Cheng, J.-X. Overcoming the barriers in micellar drug delivery: Loading efficiency, in vivo stability, and micelle–cell interaction. Expert Opin. Drug Deliv. 2010, 7, 49–62. [Google Scholar] [CrossRef] [PubMed]
- Hu, K.; Li, J.; Shen, Y.; Lu, W.; Gao, X.; Zhang, Q.; Jiang, X. Lactoferrin-conjugated PEG-PLA nanoparticles with improved brain delivery: In vitro and in vivo evaluations. J. Control. Release 2009, 134, 55–61. [Google Scholar] [CrossRef]
- Albekery, M.; Alharbi, K.; Alarifi, S.; Ahmad, D.; Omer, M.; Massadeh, S.; Yassin, A. Optimization of a nanostructured lipid carriers system for enhancing the biopharmaceutical properties of valsartan. Dig. J. Nanomater. Bios. 2017, 12, 381–389. [Google Scholar]
- Shakeel, F.; Baboota, S.; Ahuja, A.; Ali, J.; Aqil, M.; Shafiq, S. Nanoemulsions as vehicles for transdermal delivery of aceclofenac. Aaps Pharmscitech 2007, 8, 191. [Google Scholar] [CrossRef] [PubMed]
- Shakeel, F.; Haq, N.; Al-Dhfyan, A.; Alanazi, F.K.; Alsarra, I.A. Chemoprevention of skin cancer using low HLB surfactant nanoemulsion of 5-fluorouracil: A preliminary study. Drug Deliv. 2015, 22, 573–580. [Google Scholar] [CrossRef]
- El Maghraby, G.M. Transdermal delivery of hydrocortisone from eucalyptus oil microemulsion: Effects of cosurfactants. Int. J. Pharm. 2008, 355, 285–292. [Google Scholar] [CrossRef]
- Shakeel, F.; Ramadan, W.; Ahmed, M.A. Investigation of true nanoemulsions for transdermal potential of indomethacin: Characterization, rheological characteristics, and ex vivo skin permeation studies. J. Drug Target. 2009, 17, 435–441. [Google Scholar] [CrossRef]
- Shakeel, F.; Ramadan, W. Transdermal delivery of anticancer drug caffeine from water-in-oil nanoemulsions. Colloids Surf. B 2010, 75, 356–362. [Google Scholar] [CrossRef] [PubMed]




| Formulation | Val (mg) | Tween 80 (mg) | Span 80 (mg) | SDC (mg) | Method |
|---|---|---|---|---|---|
| F1 | 50 | 2000 | --- | 500 | Micro-phase separation (probe sonication) |
| F2 | 50 | 2000 | 500 | ---- | |
| F3 | 25 | 2000 | 500 | ---- | |
| F4 | 25 | 2000 | --- | 500 | |
| F5 | 50 | 2000 | 500 | --- | Thin-film hydration |
| F6 | 50 | 2000 | --- | 500 | |
| F7 | 25 | 2000 | 500 | --- | |
| F8 | 25 | 2000 | ---- | 500 |
| Formulation * | Particle Size (nm) | PDI | Zeta Potential (mV) | EE (%) |
|---|---|---|---|---|
| F1 | 107.6 ± 0.6 | 0.33 ± 0.01 | −0.11 ± 0.41 | 88.1 ± 4.4 |
| F2 | 137.0 ± 3.4 | 0.37 ± 0.02 | 3.74 ± 6.93 | 82.7 ± 3.3 |
| F3 | 112.7 ± 1.7 | 0.31 ± 0.01 | −0.67 ± 4.87 | 95.3 ± 5.7 |
| F4 | 117.7 ± 7.4 | 0.39 ± 0.03 | 0.92 ± 5.90 | 91.8 ± 4.1 |
| F5 | 140.4 ± 1.0 | 0.25 ± 0.00 | 0.26 ± 7.10 | 87.3 ± 4.4 |
| F6 | 191.7 ± 8.5 | 0.27 ± 0.05 | 5.93 ± 5.48 | 86.4 ± 3.1 |
| F7 | 112.6 ± 0.4 | 0.24 ± 0.01 | −4.93 ± 3.10 | 96.2 ± 6.7 |
| F8 | 119.7 ± 0.5 | 0.24 ± 0.02 | 3.85 ± 6.34 | 94.9 ± 2.8 |
| Formulation Code | Zero-Order | First-Order | Higuchi Diffusion | Hixson–Crowell | Peppas–Korsmeyer Exponent (n) |
|---|---|---|---|---|---|
| F1 | 0.947 | 0.979 | 0.993 | 0.970 | 0.409 |
| F2 | 0.948 | 0.987 | 0.995 | 0.977 | 0.385 |
| F3 | 0.935 | 0.965 | 0.990 | 0.956 | 0.399 |
| F4 | 0.945 | 0.977 | 0.994 | 0.968 | 0.423 |
| F5 | 0.854 | 0.912 | 0.935 | 0.894 | 0.418 |
| F6 | 0.937 | 0.970 | 0.990 | 0.961 | 0.407 |
| F7 | 0.965 | 0.986 | 0.996 | 0.980 | 0.524 |
| F8 | 0.962 | 0.991 | 0.997 | 0.984 | 0.438 |
| Formulation | JSS (µg/cm2/h) a | Kp (cm/h) a × 10−3 | Ef |
|---|---|---|---|
| Control b | 4.15 ± 0.37 | 0.83 ± 0.016 | - |
| F7 (Span/Tween micelles) | 68.84 ± 3.96 | 13.76 ± 0.064 | 16.57 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yassin, A.E.B.; Massadeh, S.; Alshwaimi, A.A.; Kittaneh, R.H.; Omer, M.E.; Ahmad, D.; Aodah, A.H.; Shakeel, F.; Halwani, M.; Alanazi, S.A.; et al. Tween 80-Based Self-Assembled Mixed Micelles Boost Valsartan Transdermal Delivery. Pharmaceuticals 2024, 17, 19. https://doi.org/10.3390/ph17010019
Yassin AEB, Massadeh S, Alshwaimi AA, Kittaneh RH, Omer ME, Ahmad D, Aodah AH, Shakeel F, Halwani M, Alanazi SA, et al. Tween 80-Based Self-Assembled Mixed Micelles Boost Valsartan Transdermal Delivery. Pharmaceuticals. 2024; 17(1):19. https://doi.org/10.3390/ph17010019
Chicago/Turabian StyleYassin, Alaa Eldeen B., Salam Massadeh, Abdullah A. Alshwaimi, Raslan H. Kittaneh, Mustafa E. Omer, Dilshad Ahmad, Al Hassan Aodah, Faiyaz Shakeel, Majed Halwani, Saleh A. Alanazi, and et al. 2024. "Tween 80-Based Self-Assembled Mixed Micelles Boost Valsartan Transdermal Delivery" Pharmaceuticals 17, no. 1: 19. https://doi.org/10.3390/ph17010019









