Pharmacology of P2X Receptors and Their Possible Therapeutic Potential in Obesity and Diabetes
Abstract
:1. Introduction
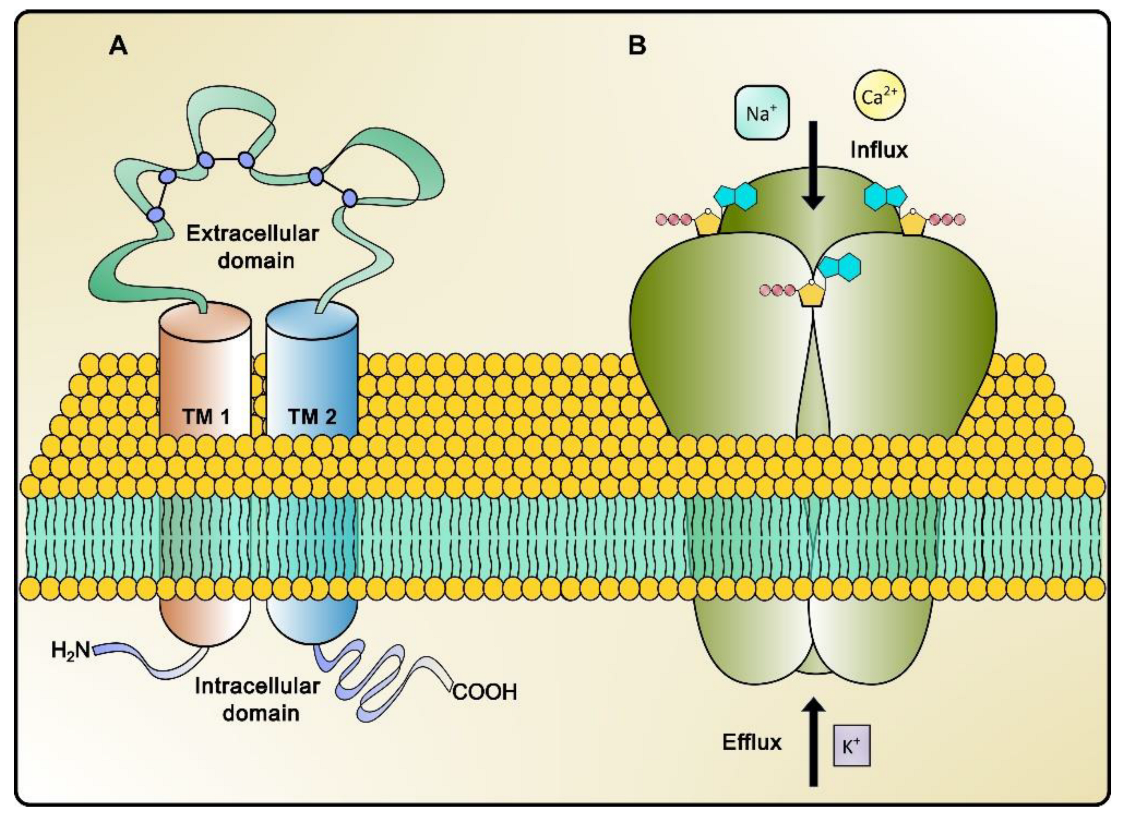
2. P2X Receptor Pharmacology
2.1. Molecular Characteristics
2.2. P2XR Agonists
2.3. P2XR Antagonists
2.3.1. P2X1R Antagonists
2.3.2. P2X2R Antagonists
2.3.3. P2X3R Antagonists
2.3.4. P2X4R Antagonists
2.3.5. P2X5R and P2X6R Antagonists
2.3.6. P2X7R Antagonists
3. Link between Obesity and Diabetes
4. Role P2XRs in Obesity and Diabetes
| Receptor | Tissue | Δ Gene or Protein Expression | Functional Consequence | References |
|---|---|---|---|---|
| P2X7 | Mice pancreatic β cells | Increased expression of P2X7 in an early stage of obesity and insulin resistance and decreased in later phases of T2D | IL-1Ra secretion and regulation of β cell mass and function | [9,104] |
| P2X7 | Adipose tissue | Increased protein and mRNA expression of P2X7 in metabolic syndrome patients | Modulated the release of inflammatory cytokines and attenuated adipogenesis | [98,102,105] |
| P2X7 | Lymphocyte T | Increased expression of P2X7 in patients with T2D | Associated with an increase in HbA1c and increased fasting plasma glucose level | [106,107] |
| P2X7 | Peripheral blood monocytes | Increased expression of P2X7 in patients with T2D | Associated with increased release of proinflammatory cytokines | [108] |
| P2X7 | Endothelial cells of aortas | No changes in P2X7 expression were reported in a rat model of T2D | Endothelial dysfunction in the aortas by activation of P2X7R | [109] |
| P2X7 | Human retinal pericytes | No changes in P2X7 expression were reported in an in vitro model of early diabetic retinopathy | Regulation of diameter of retinal microvessels and cell apoptosis | [63,110] |
| P2X4 | Hippocampal microglia | Decreased expression of P2X4R in a rat model of T2D | Associated with memory impairment | [111] |
| P2X4 | Satellite glial cells of DRG | Increased expression of P2X4R in a rat model of peripheral diabetic neuropathy | Activation of P2X4R-induced neuropathic mechanical hyperalgesia | [112] |
| P2X3 | DRG cells | Increased expression of P2X3R in diabetic rats | P2RX3 gene promoter DNA demethylation and enhanced interaction with p65 contribute to diabetic pain hypersensitivity | [113] |
| P2X2 and P2X7 | Colon tissue | Decreased expression of P2RX2 and P2RX7 mRNA in a murine T2D model | ND | [114] |
5. P2XRs in the Pathogenesis of Diabetic Complications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pereira, S.S.; Alvarez-Leite, J.I. Low-Grade Inflammation, Obesity, and Diabetes. Curr. Obes. Rep. 2014, 3, 422–431. [Google Scholar] [CrossRef] [PubMed]
- Klein, S.; Gastaldelli, A.; Yki-Jarvinen, H.; Scherer, P.E. Why does obesity cause diabetes? Cell Metab. 2022, 34, 11–20. [Google Scholar] [CrossRef]
- Jain, S.; Jacobson, K.A. Purinergic signaling in diabetes and metabolism. Biochem. Pharmacol. 2021, 187, 114393. [Google Scholar] [CrossRef] [PubMed]
- Ding, S.; Lund, P.K. Role of intestinal inflammation as an early event in obesity and insulin resistance. Curr. Opin. Clin. Nutr. Metab. Care 2011, 14, 328–333. [Google Scholar] [CrossRef] [PubMed]
- Duan, Y.; Zeng, L.; Zheng, C.; Song, B.; Li, F.; Kong, X.; Xu, K. Inflammatory Links Between High Fat Diets and Diseases. Front. Immunol. 2018, 9, 2649. [Google Scholar] [CrossRef] [PubMed]
- Antonioli, L.; Blandizzi, C.; Csoka, B.; Pacher, P.; Hasko, G. Adenosine signalling in diabetes mellitus-pathophysiology and therapeutic considerations. Nat. Rev. Endocrinol. 2015, 11, 228–241. [Google Scholar] [CrossRef]
- Junger, W.G. Immune cell regulation by autocrine purinergic signalling. Nat. Rev. Immunol. 2011, 11, 201–212. [Google Scholar] [CrossRef]
- Reichert, K.P.; Castro, M.F.V.; Assmann, C.E.; Bottari, N.B.; Miron, V.V.; Cardoso, A.; Stefanello, N.; Morsch, V.M.M.; Schetinger, M.R.C. Diabetes and hypertension: Pivotal involvement of purinergic signaling. Biomed. Pharmacother. 2021, 137, 111273. [Google Scholar] [CrossRef]
- Garcia-Jacobo, R.E.; Bergamin, L.S.; Vultaggio-Poma, V.; Thorstenberg, M.L.; Tarantini, M.; Garcia-Hernandez, M.H.; Di Virgilio, F. The Purinergic Landscape of Type 2 Diabetes Mellitus. Molecules 2022, 27, 1838. [Google Scholar] [CrossRef]
- Stefanello, N.; Schmatz, R.; Pereira, L.B.; Cardoso, A.M.; Passamonti, S.; Spanevello, R.M.; Thome, G.; de Oliveira, G.M.T.; Kist, L.W.; Bogo, M.R.; et al. Effects of chlorogenic acid, caffeine and coffee on components of the purinergic system of streptozotocin-induced diabetic rats. J. Nutr. Biochem. 2016, 38, 145–153. [Google Scholar] [CrossRef]
- Fotino, C.; Dal Ben, D.; Adinolfi, E. Emerging Roles of Purinergic Signaling in Diabetes. Med. Chem. 2018, 14, 428–438. [Google Scholar] [CrossRef]
- Reichert, K.P.; Schetinger, M.R.C.; Gutierres, J.M.; Pelinson, L.P.; Stefanello, N.; Dalenogare, D.P.; Baldissarelli, J.; Lopes, T.F.; Morsch, V.M. Lingonberry Extract Provides Neuroprotection by Regulating the Purinergic System and Reducing Oxidative Stress in Diabetic Rats. Mol. Nutr. Food Res. 2018, 62, e1800050. [Google Scholar] [CrossRef] [PubMed]
- North, R.A. P2X receptors. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2016, 371, 20150427. [Google Scholar] [CrossRef] [PubMed]
- Coddou, C.; Yan, Z.; Obsil, T.; Huidobro-Toro, J.P.; Stojilkovic, S.S. Activation and regulation of purinergic P2X receptor channels. Pharmacol. Rev. 2011, 63, 641–683. [Google Scholar] [CrossRef] [PubMed]
- Hattori, M.; Gouaux, E. Molecular mechanism of ATP binding and ion channel activation in P2X receptors. Nature 2012, 485, 207–212. [Google Scholar] [CrossRef] [PubMed]
- Zyma, M.; Pawliczak, R. Characteristics and the role of purinergic receptors in pathophysiology with focus on immune response. Int. Rev. Immunol. 2020, 39, 97–117. [Google Scholar] [CrossRef]
- Oken, A.C.; Krishnamurthy, I.; Savage, J.C.; Lisi, N.E.; Godsey, M.H.; Mansoor, S.E. Molecular Pharmacology of P2X Receptors: Exploring Druggable Domains Revealed by Structural Biology. Front. Pharmacol. 2022, 13, 925880. [Google Scholar] [CrossRef]
- Illes, P.; Muller, C.E.; Jacobson, K.A.; Grutter, T.; Nicke, A.; Fountain, S.J.; Kennedy, C.; Schmalzing, G.; Jarvis, M.F.; Stojilkovic, S.S.; et al. Update of P2X receptor properties and their pharmacology: IUPHAR Review 30. Br. J. Pharmacol. 2021, 178, 489–514. [Google Scholar] [CrossRef]
- Mansoor, S.E.; Lu, W.; Oosterheert, W.; Shekhar, M.; Tajkhorshid, E.; Gouaux, E. X-ray structures define human P2X(3) receptor gating cycle and antagonist action. Nature 2016, 538, 66–71. [Google Scholar] [CrossRef]
- Habermacher, C.; Dunning, K.; Chataigneau, T.; Grutter, T. Molecular structure and function of P2X receptors. Neuropharmacology 2016, 104, 18–30. [Google Scholar] [CrossRef]
- Bernier, L.P.; Ase, A.R.; Chevallier, S.; Blais, D.; Zhao, Q.; Boue-Grabot, E.; Logothetis, D.; Seguela, P. Phosphoinositides regulate P2X4 ATP-gated channels through direct interactions. J. Neurosci. 2008, 28, 12938–12945. [Google Scholar] [CrossRef] [PubMed]
- Karasawa, A.; Kawate, T. Structural basis for subtype-specific inhibition of the P2X7 receptor. eLife 2016, 5, e22153. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wang, Y.; Cui, W.W.; Huang, Y.; Yang, Y.; Liu, Y.; Zhao, W.S.; Cheng, X.Y.; Sun, W.S.; Cao, P.; et al. Druggable negative allosteric site of P2X3 receptors. Proc. Natl. Acad. Sci. USA 2018, 115, 4939–4944. [Google Scholar] [CrossRef] [PubMed]
- Lambertucci, C.; Dal Ben, D.; Buccioni, M.; Marucci, G.; Thomas, A.; Volpini, R. Medicinal chemistry of P2X receptors: Agonists and orthosteric antagonists. Curr. Med. Chem. 2015, 22, 915–928. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, K.A.; Muller, C.E. Medicinal chemistry of adenosine, P2Y and P2X receptors. Neuropharmacology 2016, 104, 31–49. [Google Scholar] [CrossRef]
- Bianchi, B.R.; Lynch, K.J.; Touma, E.; Niforatos, W.; Burgard, E.C.; Alexander, K.M.; Park, H.S.; Yu, H.; Metzger, R.; Kowaluk, E.; et al. Pharmacological characterization of recombinant human and rat P2X receptor subtypes. Eur. J. Pharmacol. 1999, 376, 127–138. [Google Scholar] [CrossRef]
- Wildman, S.S.; Brown, S.G.; King, B.F.; Burnstock, G. Selectivity of diadenosine polyphosphates for rat P2X receptor subunits. Eur. J. Pharmacol. 1999, 367, 119–123. [Google Scholar] [CrossRef]
- Wildman, S.S.; Brown, S.G.; Rahman, M.; Noel, C.A.; Churchill, L.; Burnstock, G.; Unwin, R.J.; King, B.F. Sensitization by extracellular Ca2+ of rat P2X(5) receptor and its pharmacological properties compared with rat P2X(1). Mol. Pharmacol. 2002, 62, 957–966. [Google Scholar] [CrossRef]
- Pintor, J.; King, B.F.; Miras-Portugal, M.T.; Burnstock, G. Selectivity and activity of adenine dinucleotides at recombinant P2X2 and P2Y1 purinoceptors. Br. J. Pharmacol. 1996, 119, 1006–1012. [Google Scholar] [CrossRef]
- Collo, G.; North, R.A.; Kawashima, E.; Merlo-Pich, E.; Neidhart, S.; Surprenant, A.; Buell, G. Cloning OF P2X5 and P2X6 receptors and the distribution and properties of an extended family of ATP-gated ion channels. J. Neurosci. 1996, 16, 2495–2507. [Google Scholar] [CrossRef]
- Surprenant, A.; Rassendren, F.; Kawashima, E.; North, R.A.; Buell, G. The cytolytic P2Z receptor for extracellular ATP identified as a P2X receptor (P2X7). Science 1996, 272, 735–738. [Google Scholar] [CrossRef] [PubMed]
- Chessell, I.P.; Simon, J.; Hibell, A.D.; Michel, A.D.; Barnard, E.A.; Humphrey, P.P. Cloning and functional characterisation of the mouse P2X7 receptor. FEBS Lett. 1998, 439, 26–30. [Google Scholar] [CrossRef] [PubMed]
- Abdelrahman, A.; Namasivayam, V.; Hinz, S.; Schiedel, A.C.; Kose, M.; Burton, M.; El-Tayeb, A.; Gillard, M.; Bajorath, J.; de Ryck, M.; et al. Characterization of P2X4 receptor agonists and antagonists by calcium influx and radioligand binding studies. Biochem. Pharmacol. 2017, 125, 41–54. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, K.A.; Jarvis, M.F.; Williams, M. Purine and pyrimidine (P2) receptors as drug targets. J. Med. Chem. 2002, 45, 4057–4093. [Google Scholar] [CrossRef]
- North, R.A.; Barnard, E.A. Nucleotide receptors. Curr. Opin. Neurobiol. 1997, 7, 346–357. [Google Scholar] [CrossRef]
- North, R.A.; Surprenant, A. Pharmacology of cloned P2X receptors. Annu. Rev. Pharmacol. Toxicol. 2000, 40, 563–580. [Google Scholar] [CrossRef]
- North, R.A.; Jarvis, M.F. P2X receptors as drug targets. Mol. Pharmacol. 2013, 83, 759–769. [Google Scholar] [CrossRef]
- Dal Ben, D.; Buccioni, M.; Lambertucci, C.; Marucci, G.; Spinaci, A.; Marchenkova, A.; Abdelrahman, A.; Nistri, A.; Muller, C.E.; Volpini, R. Investigation on 2′,3′-O-Substituted ATP Derivatives and Analogs as Novel P2X3 Receptor Antagonists. ACS Med. Chem. Lett. 2019, 10, 493–498. [Google Scholar] [CrossRef] [PubMed]
- Obrecht, A.S.; Urban, N.; Schaefer, M.; Rose, A.; Kless, A.; Meents, J.E.; Lampert, A.; Abdelrahman, A.; Muller, C.E.; Schmalzing, G.; et al. Identification of aurintricarboxylic acid as a potent allosteric antagonist of P2X1 and P2X3 receptors. Neuropharmacology 2019, 158, 107749. [Google Scholar] [CrossRef]
- Brown, S.G.; Kim, Y.C.; Kim, S.A.; Jacobson, K.A.; Burnstock, G.; King, B.F. Actions of a Series of PPADS Analogs at P2X(1) and P2X(3) Receptors. Drug Dev. Res. 2001, 53, 281–291. [Google Scholar] [CrossRef]
- Jarvis, M.F.; Burgard, E.C.; McGaraughty, S.; Honore, P.; Lynch, K.; Brennan, T.J.; Subieta, A.; Van Biesen, T.; Cartmell, J.; Bianchi, B.; et al. A-317491, a novel potent and selective non-nucleotide antagonist of P2X3 and P2X2/3 receptors, reduces chronic inflammatory and neuropathic pain in the rat. Proc. Natl. Acad. Sci. USA 2002, 99, 17179–17184. [Google Scholar] [CrossRef] [PubMed]
- Garceau, D.; Chauret, N. BLU-5937: A selective P2X3 antagonist with potent anti-tussive effect and no taste alteration. Pulm. Pharmacol. Ther. 2019, 56, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Morice, A.H.; Birring, S.S.; Smith, J.A.; McGarvey, L.P.; Schelfhout, J.; Martin Nguyen, A.; Xu, Z.J.; Wu, W.C.; Muccino, D.R.; Sher, M.R. Characterization of Patients with Refractory or Unexplained Chronic Cough Participating in a Phase 2 Clinical Trial of the P2X3-Receptor Antagonist Gefapixant. Lung 2021, 199, 121–129. [Google Scholar] [CrossRef]
- Garcia-Guzman, M.; Soto, F.; Gomez-Hernandez, J.M.; Lund, P.E.; Stuhmer, W. Characterization of recombinant human P2X4 receptor reveals pharmacological differences to the rat homologue. Mol. Pharmacol. 1997, 51, 109–118. [Google Scholar] [CrossRef]
- Hernandez-Olmos, V.; Abdelrahman, A.; El-Tayeb, A.; Freudendahl, D.; Weinhausen, S.; Muller, C.E. N-substituted phenoxazine and acridone derivatives: Structure-activity relationships of potent P2X4 receptor antagonists. J. Med. Chem. 2012, 55, 9576–9588. [Google Scholar] [CrossRef]
- Honore, P.; Donnelly-Roberts, D.; Namovic, M.T.; Hsieh, G.; Zhu, C.Z.; Mikusa, J.P.; Hernandez, G.; Zhong, C.; Gauvin, D.M.; Chandran, P.; et al. A-740003 [N-(1-[(cyanoimino)(5-quinolinylamino) methyl]amino-2,2-dimethylpropyl)-2-(3,4-dimethoxyphenyl)acetamide], a novel and selective P2X7 receptor antagonist, dose-dependently reduces neuropathic pain in the rat. J. Pharmacol. Exp. Ther. 2006, 319, 1376–1385. [Google Scholar] [CrossRef] [PubMed]
- Nelson, D.W.; Gregg, R.J.; Kort, M.E.; Perez-Medrano, A.; Voight, E.A.; Wang, Y.; Grayson, G.; Namovic, M.T.; Donnelly-Roberts, D.L.; Niforatos, W.; et al. Structure-activity relationship studies on a series of novel, substituted 1-benzyl-5-phenyltetrazole P2X7 antagonists. J. Med. Chem. 2006, 49, 3659–3666. [Google Scholar] [CrossRef]
- Donnelly-Roberts, D.L.; Namovic, M.T.; Han, P.; Jarvis, M.F. Mammalian P2X7 receptor pharmacology: Comparison of recombinant mouse, rat and human P2X7 receptors. Br. J. Pharmacol. 2009, 157, 1203–1214. [Google Scholar] [CrossRef]
- Donnelly-Roberts, D.L.; Namovic, M.T.; Surber, B.; Vaidyanathan, S.X.; Perez-Medrano, A.; Wang, Y.; Carroll, W.A.; Jarvis, M.F. [3H]A-804598 ([3H]2-cyano-1-[(1S)-1-phenylethyl]-3-quinolin-5-ylguanidine) is a novel, potent, and selective antagonist radioligand for P2X7 receptors. Neuropharmacology 2009, 56, 223–229. [Google Scholar] [CrossRef]
- Honore, P.; Donnelly-Roberts, D.; Namovic, M.; Zhong, C.; Wade, C.; Chandran, P.; Zhu, C.; Carroll, W.; Perez-Medrano, A.; Iwakura, Y.; et al. The antihyperalgesic activity of a selective P2X7 receptor antagonist, A-839977, is lost in IL-1alphabeta knockout mice. Behav. Brain Res. 2009, 204, 77–81. [Google Scholar] [CrossRef]
- Tian, M.; Abdelrahman, A.; Baqi, Y.; Fuentes, E.; Azazna, D.; Spanier, C.; Densborn, S.; Hinz, S.; Schmid, R.; Muller, C.E. Discovery and Structure Relationships of Salicylanilide Derivatives as Potent, Non-acidic P2X1 Receptor Antagonists. J. Med. Chem. 2020, 63, 6164–6178. [Google Scholar] [CrossRef] [PubMed]
- Rettinger, J.; Schmalzing, G.; Damer, S.; Muller, G.; Nickel, P.; Lambrecht, G. The suramin analogue NF279 is a novel and potent antagonist selective for the P2X(1) receptor. Neuropharmacology 2000, 39, 2044–2053. [Google Scholar] [CrossRef] [PubMed]
- Wolf, C.; Rosefort, C.; Fallah, G.; Kassack, M.U.; Hamacher, A.; Bodnar, M.; Wang, H.; Illes, P.; Kless, A.; Bahrenberg, G.; et al. Molecular determinants of potent P2X2 antagonism identified by functional analysis, mutagenesis, and homology docking. Mol. Pharmacol. 2011, 79, 649–661. [Google Scholar] [CrossRef] [PubMed]
- Baqi, Y.; Hausmann, R.; Rosefort, C.; Rettinger, J.; Schmalzing, G.; Muller, C.E. Discovery of potent competitive antagonists and positive modulators of the P2X2 receptor. J. Med. Chem. 2011, 54, 817–830. [Google Scholar] [CrossRef]
- Muller, C.E.; Namasivayam, V. Recommended tool compounds and drugs for blocking P2X and P2Y receptors. Purinergic Signal 2021, 17, 633–648. [Google Scholar] [CrossRef]
- Morice, A.H.; Kitt, M.M.; Ford, A.P.; Tershakovec, A.M.; Wu, W.C.; Brindle, K.; Thompson, R.; Thackray-Nocera, S.; Wright, C. The effect of gefapixant, a P2X3 antagonist, on cough reflex sensitivity: A randomised placebo-controlled study. Eur. Respir. J. 2019, 54, 1900439. [Google Scholar] [CrossRef]
- Spinaci, A.; Buccioni, M.; Dal Ben, D.; Marucci, G.; Volpini, R.; Lambertucci, C. P2X3 Receptor Ligands: Structural Features and Potential Therapeutic Applications. Front. Pharmacol. 2021, 12, 653561. [Google Scholar] [CrossRef]
- Matsumura, Y.; Yamashita, T.; Sasaki, A.; Nakata, E.; Kohno, K.; Masuda, T.; Tozaki-Saitoh, H.; Imai, T.; Kuraishi, Y.; Tsuda, M.; et al. A novel P2X4 receptor-selective antagonist produces anti-allodynic effect in a mouse model of herpetic pain. Sci. Rep. 2016, 6, 32461. [Google Scholar] [CrossRef]
- Inoue, K. Nociceptive signaling of P2X receptors in chronic pain states. Purinergic Signal 2021, 17, 41–47. [Google Scholar] [CrossRef]
- King, B.F. Rehabilitation of the P2X5 receptor: A re-evaluation of structure and function. Purinergic Signal 2023, 19, 421–439. [Google Scholar] [CrossRef]
- Robinson, L.E.; Murrell-Lagnado, R.D. The trafficking and targeting of P2X receptors. Front. Cell. Neurosci. 2013, 7, 233. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharya, A.; Wang, Q.; Ao, H.; Shoblock, J.R.; Lord, B.; Aluisio, L.; Fraser, I.; Nepomuceno, D.; Neff, R.A.; Welty, N.; et al. Pharmacological characterization of a novel centrally permeable P2X7 receptor antagonist: JNJ-47965567. Br. J. Pharmacol. 2013, 170, 624–640. [Google Scholar] [CrossRef] [PubMed]
- Platania, C.B.M.; Giurdanella, G.; Di Paola, L.; Leggio, G.M.; Drago, F.; Salomone, S.; Bucolo, C. P2X7 receptor antagonism: Implications in diabetic retinopathy. Biochem. Pharmacol. 2017, 138, 130–139. [Google Scholar] [CrossRef]
- de Heredia, F.P.; Gomez-Martinez, S.; Marcos, A. Obesity, inflammation and the immune system. Proc. Nutr. Soc. 2012, 71, 332–338. [Google Scholar] [CrossRef]
- Kennedy, A.; Martinez, K.; Chuang, C.C.; LaPoint, K.; McIntosh, M. Saturated fatty acid-mediated inflammation and insulin resistance in adipose tissue: Mechanisms of action and implications. J. Nutr. 2009, 139, 1–4. [Google Scholar] [CrossRef]
- Tchernof, A.; Despres, J.P. Pathophysiology of human visceral obesity: An update. Physiol. Rev. 2013, 93, 359–404. [Google Scholar] [CrossRef]
- Murphy, E.A.; Velazquez, K.T.; Herbert, K.M. Influence of high-fat diet on gut microbiota: A driving force for chronic disease risk. Curr. Opin. Clin. Nutr. Metab. Care 2015, 18, 515–520. [Google Scholar] [CrossRef] [PubMed]
- De Bandt, J.P.; Waligora-Dupriet, A.J.; Butel, M.J. Intestinal microbiota in inflammation and insulin resistance: Relevance to humans. Curr. Opin. Clin. Nutr. Metab. Care 2011, 14, 334–340. [Google Scholar] [CrossRef] [PubMed]
- Winer, D.A.; Luck, H.; Tsai, S.; Winer, S. The Intestinal Immune System in Obesity and Insulin Resistance. Cell Metab. 2016, 23, 413–426. [Google Scholar] [CrossRef]
- Zhang, X.; Zhang, G.; Zhang, H.; Karin, M.; Bai, H.; Cai, D. Hypothalamic IKKbeta/NF-kappaB and ER stress link overnutrition to energy imbalance and obesity. Cell 2008, 135, 61–73. [Google Scholar] [CrossRef]
- Cai, D.; Liu, T. Hypothalamic inflammation: A double-edged sword to nutritional diseases. Ann. N. Y. Acad. Sci. 2011, 1243, E1–E39. [Google Scholar] [CrossRef] [PubMed]
- Lumeng, C.N.; Saltiel, A.R. Inflammatory links between obesity and metabolic disease. J. Clin. Investig. 2011, 121, 2111–2117. [Google Scholar] [CrossRef] [PubMed]
- Bleau, C.; Karelis, A.D.; St-Pierre, D.H.; Lamontagne, L. Crosstalk between intestinal microbiota, adipose tissue and skeletal muscle as an early event in systemic low-grade inflammation and the development of obesity and diabetes. Diabetes Metab. Res. Rev. 2015, 31, 545–561. [Google Scholar] [CrossRef]
- Longo, M.; Zatterale, F.; Naderi, J.; Parrillo, L.; Formisano, P.; Raciti, G.A.; Beguinot, F.; Miele, C. Adipose Tissue Dysfunction as Determinant of Obesity-Associated Metabolic Complications. Int. J. Mol. Sci. 2019, 20, 2358. [Google Scholar] [CrossRef]
- Park, H.S.; Park, J.Y.; Yu, R. Relationship of obesity and visceral adiposity with serum concentrations of CRP, TNF-alpha and IL-6. Diabetes Res. Clin. Pract. 2005, 69, 29–35. [Google Scholar] [CrossRef]
- Ren, Y.; Zhao, H.; Yin, C.; Lan, X.; Wu, L.; Du, X.; Griffiths, H.R.; Gao, D. Adipokines, Hepatokines and Myokines: Focus on Their Role and Molecular Mechanisms in Adipose Tissue Inflammation. Front. Endocrinol. 2022, 13, 873699. [Google Scholar] [CrossRef]
- Ouchi, N.; Parker, J.L.; Lugus, J.J.; Walsh, K. Adipokines in inflammation and metabolic disease. Nat. Rev. Immunol. 2011, 11, 85–97. [Google Scholar] [CrossRef]
- Sell, H.; Eckel, J. Adipose tissue inflammation: Novel insight into the role of macrophages and lymphocytes. Curr. Opin. Clin. Nutr. Metab. Care 2010, 13, 366–370. [Google Scholar] [CrossRef] [PubMed]
- Puschel, G.P.; Klauder, J.; Henkel, J. Macrophages, Low-Grade Inflammation, Insulin Resistance and Hyperinsulinemia: A Mutual Ambiguous Relationship in the Development of Metabolic Diseases. J. Clin. Med. 2022, 11, 4358. [Google Scholar] [CrossRef]
- Yao, K.; Duan, Y.; Li, F.; Tan, B.; Hou, Y.; Wu, G.; Yin, Y. Leucine in Obesity: Therapeutic Prospects. Trends Pharmacol. Sci. 2016, 37, 714–727. [Google Scholar] [CrossRef]
- James, D.E.; Stockli, J.; Birnbaum, M.J. The aetiology and molecular landscape of insulin resistance. Nat. Rev. Mol. Cell Biol. 2021, 22, 751–771. [Google Scholar] [CrossRef] [PubMed]
- Boucher, J.; Kleinridders, A.; Kahn, C.R. Insulin receptor signaling in normal and insulin-resistant states. Cold Spring Harb. Perspect. Biol. 2014, 6, a009191. [Google Scholar] [CrossRef]
- Tanti, J.F.; Jager, J. Cellular mechanisms of insulin resistance: Role of stress-regulated serine kinases and insulin receptor substrates (IRS) serine phosphorylation. Curr. Opin. Pharmacol. 2009, 9, 753–762. [Google Scholar] [CrossRef]
- Yung, J.H.M.; Giacca, A. Role of c-Jun N-terminal Kinase (JNK) in Obesity and Type 2 Diabetes. Cells 2020, 9, 706. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Xu, S.; Zhang, X.; Yi, Z.; Cichello, S. Skeletal intramyocellular lipid metabolism and insulin resistance. Biophys. Rep. 2015, 1, 90–98. [Google Scholar] [CrossRef] [PubMed]
- Koves, T.R.; Ussher, J.R.; Noland, R.C.; Slentz, D.; Mosedale, M.; Ilkayeva, O.; Bain, J.; Stevens, R.; Dyck, J.R.; Newgard, C.B.; et al. Mitochondrial overload and incomplete fatty acid oxidation contribute to skeletal muscle insulin resistance. Cell Metab. 2008, 7, 45–56. [Google Scholar] [CrossRef]
- Eguchi, N.; Vaziri, N.D.; Dafoe, D.C.; Ichii, H. The Role of Oxidative Stress in Pancreatic beta Cell Dysfunction in Diabetes. Int. J. Mol. Sci. 2021, 22, 1509. [Google Scholar] [CrossRef]
- Novak, I.; Solini, A. P2X receptor-ion channels in the inflammatory response in adipose tissue and pancreas-potential triggers in onset of type 2 diabetes? Curr. Opin. Immunol. 2018, 52, 1–7. [Google Scholar] [CrossRef]
- Idzko, M.; Ferrari, D.; Eltzschig, H.K. Nucleotide signalling during inflammation. Nature 2014, 509, 310–317. [Google Scholar] [CrossRef]
- Vargas-Martinez, E.M.; Gomez-Coronado, K.S.; Espinosa-Luna, R.; Valdez-Morales, E.E.; Barrios-Garcia, T.; Barajas-Espinosa, A.; Ochoa-Cortes, F.; Montano, L.M.; Barajas-Lopez, C.; Guerrero-Alba, R. Functional expression of P2X1, P2X4 and P2X7 purinergic receptors in human monocyte-derived macrophages. Eur. J. Pharmacol. 2020, 888, 173460. [Google Scholar] [CrossRef]
- Sluyter, R.; Barden, J.A.; Wiley, J.S. Detection of P2X purinergic receptors on human B lymphocytes. Cell Tissue Res. 2001, 304, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Abramowski, P.; Ogrodowczyk, C.; Martin, R.; Pongs, O. A truncation variant of the cation channel P2RX5 is upregulated during T cell activation. PLoS ONE 2014, 9, e104692. [Google Scholar] [CrossRef] [PubMed]
- Cekic, C.; Linden, J. Purinergic regulation of the immune system. Nat. Rev. Immunol. 2016, 16, 177–192. [Google Scholar] [CrossRef] [PubMed]
- Gong, T.; Liu, L.; Jiang, W.; Zhou, R. DAMP-sensing receptors in sterile inflammation and inflammatory diseases. Nat. Rev. Immunol. 2020, 20, 95–112. [Google Scholar] [CrossRef] [PubMed]
- Karmakar, M.; Katsnelson, M.A.; Dubyak, G.R.; Pearlman, E. Neutrophil P2X7 receptors mediate NLRP3 inflammasome-dependent IL-1beta secretion in response to ATP. Nat. Commun. 2016, 7, 10555. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Z.F.; Wu, W.; Hu, H.B.; Li, Z.Y.; Zhong, M.; Zhang, L. P2X7 receptor as the regulator of T-cell function in intestinal barrier disruption. World J. Gastroenterol. 2022, 28, 5265–5279. [Google Scholar] [CrossRef]
- Di Virgilio, F.; Dal Ben, D.; Sarti, A.C.; Giuliani, A.L.; Falzoni, S. The P2X7 Receptor in Infection and Inflammation. Immunity 2017, 47, 15–31. [Google Scholar] [CrossRef]
- Madec, S.; Rossi, C.; Chiarugi, M.; Santini, E.; Salvati, A.; Ferrannini, E.; Solini, A. Adipocyte P2X7 receptors expression: A role in modulating inflammatory response in subjects with metabolic syndrome? Atherosclerosis 2011, 219, 552–558. [Google Scholar] [CrossRef]
- Beaucage, K.L.; Xiao, A.; Pollmann, S.I.; Grol, M.W.; Beach, R.J.; Holdsworth, D.W.; Sims, S.M.; Darling, M.R.; Dixon, S.J. Loss of P2X7 nucleotide receptor function leads to abnormal fat distribution in mice. Purinergic Signal 2014, 10, 291–304. [Google Scholar] [CrossRef]
- Perruzza, L.; Gargari, G.; Proietti, M.; Fosso, B.; D’Erchia, A.M.; Faliti, C.E.; Rezzonico-Jost, T.; Scribano, D.; Mauri, L.; Colombo, D.; et al. T Follicular Helper Cells Promote a Beneficial Gut Ecosystem for Host Metabolic Homeostasis by Sensing Microbiota-Derived Extracellular ATP. Cell Rep. 2017, 18, 2566–2575. [Google Scholar] [CrossRef]
- Perruzza, L.; Strati, F.; Gargari, G.; D’Erchia, A.M.; Fosso, B.; Pesole, G.; Guglielmetti, S.; Grassi, F. Enrichment of intestinal Lactobacillus by enhanced secretory IgA coating alters glucose homeostasis in P2rx7(-/-) mice. Sci. Rep. 2019, 9, 9315. [Google Scholar] [CrossRef] [PubMed]
- Gao, H.; Li, D.; Yang, P.; Zhao, L.; Wei, L.; Chen, Y.; Ruan, X.Z. Suppression of CD36 attenuates adipogenesis with a reduction of P2X7 expression in 3T3-L1 cells. Biochem. Biophys. Res. Commun. 2017, 491, 204–208. [Google Scholar] [CrossRef] [PubMed]
- Jacques-Silva, M.C.; Correa-Medina, M.; Cabrera, O.; Rodriguez-Diaz, R.; Makeeva, N.; Fachado, A.; Diez, J.; Berman, D.M.; Kenyon, N.S.; Ricordi, C.; et al. ATP-gated P2X3 receptors constitute a positive autocrine signal for insulin release in the human pancreatic beta cell. Proc. Natl. Acad. Sci. USA 2010, 107, 6465–6470. [Google Scholar] [CrossRef] [PubMed]
- Glas, R.; Sauter, N.S.; Schulthess, F.T.; Shu, L.; Oberholzer, J.; Maedler, K. Purinergic P2X7 receptors regulate secretion of interleukin-1 receptor antagonist and beta cell function and survival. Diabetologia 2009, 52, 1579–1588. [Google Scholar] [CrossRef]
- Li, J.; Gong, L.; Xu, Q. Purinergic 2X7 receptor is involved in adipogenesis and lipid degradation. Exp. Ther. Med. 2022, 23, 81. [Google Scholar] [CrossRef]
- Garcia-Hernandez, M.H.; Portales-Cervantes, L.; Cortez-Espinosa, N.; Vargas-Morales, J.M.; Fritche Salazar, J.F.; Rivera-Lopez, E.; Rodriguez-Rivera, J.G.; Quezada-Calvillo, R.; Portales-Perez, D.P. Expression and function of P2X(7) receptor and CD39/Entpd1 in patients with type 2 diabetes and their association with biochemical parameters. Cell Immunol. 2011, 269, 135–143. [Google Scholar] [CrossRef]
- Tezza, S.; Ben Nasr, M.; D’Addio, F.; Vergani, A.; Usuelli, V.; Falzoni, S.; Bassi, R.; Dellepiane, S.; Fotino, C.; Rossi, C.; et al. Islet-Derived eATP Fuels Autoreactive CD8+ T Cells and Facilitates the Onset of Type 1 Diabetes. Diabetes 2018, 67, 2038–2053. [Google Scholar] [CrossRef]
- Wu, H.; Nie, Y.; Xiong, H.; Liu, S.; Li, G.; Huang, A.; Guo, L.; Wang, S.; Xue, Y.; Wu, B.; et al. P2X7 Receptor Expression in Peripheral Blood Monocytes Is Correlated with Plasma C-Reactive Protein and Cytokine Levels in Patients With Type 2 Diabetes Mellitus: A Preliminary Report. Inflammation 2015, 38, 2076–2081. [Google Scholar] [CrossRef]
- Mahdi, A.; Jiao, T.; Tratsiakovich, Y.; Yang, J.; Ostenson, C.G.; Pernow, J.; Zhou, Z. Altered Purinergic Receptor Sensitivity in Type 2 Diabetes-Associated Endothelial Dysfunction and Up(4)A-Mediated Vascular Contraction. Int. J. Mol. Sci. 2018, 19, 3942. [Google Scholar] [CrossRef]
- Shibata, M.; Ishizaki, E.; Zhang, T.; Fukumoto, M.; Barajas-Espinosa, A.; Li, T.; Puro, D.G. Purinergic Vasotoxicity: Role of the Pore/Oxidant/K(ATP) Channel/Ca2+ Pathway in P2X(7)-Induced Cell Death in Retinal Capillaries. Vision 2018, 2, 25. [Google Scholar] [CrossRef]
- Zhang, P.A.; Sun, Q.; Li, Y.C.; Weng, R.X.; Wu, R.; Zhang, H.H.; Xu, G.Y. Overexpression of Purinergic P2X4 Receptors in Hippocampus Rescues Memory Impairment in Rats with Type 2 Diabetes. Neurosci. Bull. 2020, 36, 719–732. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, J.M.; Dos Santos, G.G.; Neves, A.F.; Athie, M.C.P.; Bonet, I.J.M.; Nishijima, C.M.; Farias, F.H.; Figueiredo, J.G.; Hernandez-Olmos, V.; Alshaibani, S.; et al. Diabetes-induced Neuropathic Mechanical Hyperalgesia Depends on P2X4 Receptor Activation in Dorsal Root Ganglia. Neuroscience 2019, 398, 158–170. [Google Scholar] [CrossRef]
- Zhang, H.H.; Hu, J.; Zhou, Y.L.; Qin, X.; Song, Z.Y.; Yang, P.P.; Hu, S.; Jiang, X.; Xu, G.Y. Promoted Interaction of Nuclear Factor-kappaB with Demethylated Purinergic P2X3 Receptor Gene Contributes to Neuropathic Pain in Rats with Diabetes. Diabetes 2015, 64, 4272–4284. [Google Scholar] [CrossRef]
- Cruz-Munoz, J.R.; Valdez-Morales, E.E.; Barajas-Espinosa, A.; Barrios-Garcia, T.; Linan-Rico, A.; Guerrero-Alba, R. Gene expression alterations of purinergic signaling components in obesity-associated intestinal low-grade inflammation in type 2 diabetes. Purinergic Signal 2024. [Google Scholar] [CrossRef]
- Tozzi, M.; Larsen, A.T.; Lange, S.C.; Giannuzzo, A.; Andersen, M.N.; Novak, I. The P2X7 receptor and pannexin-1 are involved in glucose-induced autocrine regulation in beta-cells. Sci. Rep. 2018, 8, 8926. [Google Scholar] [CrossRef] [PubMed]
- Vieira, F.S.; Nanini, H.F.; Takiya, C.M.; Coutinho-Silva, R. P2X7 receptor knockout prevents streptozotocin-induced type 1 diabetes in mice. Mol. Cell. Endocrinol. 2016, 419, 148–157. [Google Scholar] [CrossRef]
- Zhang, C.M.; Huang, X.; Lu, H.L.; Meng, X.M.; Song, N.N.; Chen, L.; Kim, Y.C.; Chen, J.; Xu, W.X. Diabetes-induced damage of gastric nitric oxide neurons mediated by P2X7R in diabetic mice. Eur. J. Pharmacol. 2019, 851, 151–160. [Google Scholar] [CrossRef]
- Burnstock, G.; Novak, I. Purinergic signalling and diabetes. Purinergic Signal 2013, 9, 307–324. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Sorop, O.; de Beer, V.J.; Heinonen, I.; Cheng, C.; Jan Danser, A.H.; Duncker, D.J.; Merkus, D. Altered purinergic signaling in uridine adenosine tetraphosphate-induced coronary relaxation in swine with metabolic derangement. Purinergic Signal 2017, 13, 319–329. [Google Scholar] [CrossRef]
- Zhou, Z.; Sun, C.; Tilley, S.L.; Mustafa, S.J. Mechanisms underlying uridine adenosine tetraphosphate-induced vascular contraction in mouse aorta: Role of thromboxane and purinergic receptors. Vascul Pharmacol. 2015, 73, 78–85. [Google Scholar] [CrossRef]
- Costa, G.; Pereira, T.; Neto, A.M.; Cristovao, A.J.; Ambrosio, A.F.; Santos, P.F. High glucose changes extracellular adenosine triphosphate levels in rat retinal cultures. J. Neurosci. Res. 2009, 87, 1375–1380. [Google Scholar] [CrossRef] [PubMed]
- Pereira Tde, O.; da Costa, G.N.; Santiago, A.R.; Ambrosio, A.F.; dos Santos, P.F. High glucose enhances intracellular Ca2+ responses triggered by purinergic stimulation in retinal neurons and microglia. Brain Res. 2010, 1316, 129–138. [Google Scholar] [CrossRef]
- Altmann, C.; Schmidt, M.H.H. The Role of Microglia in Diabetic Retinopathy: Inflammation, Microvasculature Defects and Neurodegeneration. Int. J. Mol. Sci. 2018, 19, 110. [Google Scholar] [CrossRef]
- Capiotti, K.M.; Siebel, A.M.; Kist, L.W.; Bogo, M.R.; Bonan, C.D.; Da Silva, R.S. Hyperglycemia alters E-NTPDases, ecto-5′-nucleotidase, and ectosolic and cytosolic adenosine deaminase activities and expression from encephala of adult zebrafish (Danio rerio). Purinergic Signal 2016, 12, 211–220. [Google Scholar] [CrossRef]
- Saez-Orellana, F.; Godoy, P.A.; Bastidas, C.Y.; Silva-Grecchi, T.; Guzman, L.; Aguayo, L.G.; Fuentealba, J. ATP leakage induces P2XR activation and contributes to acute synaptic excitotoxicity induced by soluble oligomers of beta-amyloid peptide in hippocampal neurons. Neuropharmacology 2016, 100, 116–123. [Google Scholar] [CrossRef]
- Burnstock, G. Purinergic Signalling: Therapeutic Developments. Front. Pharmacol. 2017, 8, 661. [Google Scholar]
- Christianson, J.A.; Riekhof, J.T.; Wright, D.E. Restorative effects of neurotrophin treatment on diabetes-induced cutaneous axon loss in mice. Exp. Neurol. 2003, 179, 188–199. [Google Scholar] [CrossRef]
- Calcutt, N.A. Diabetic neuropathy and neuropathic pain: A (con)fusion of pathogenic mechanisms? Pain 2020, 161 (Suppl. S1), S65–S86. [Google Scholar] [CrossRef] [PubMed]
- Recourt, K.; de Boer, P.; van der Ark, P.; Benes, H.; van Gerven, J.M.A.; Ceusters, M.; van Nueten, L.; Drevets, W.C.; Bhatacharya, A.; Browning, M.; et al. Characterization of the central nervous system penetrant and selective purine P2X7 receptor antagonist JNJ-54175446 in patients with major depressive disorder. Transl. Psychiatry 2023, 13, 266. [Google Scholar] [CrossRef]
- Fletcher, M.C. Selectivity of the P2X3 receptor antagonist Eliapixant, and its potential use in the treatment of endometriosis. Purinergic Signal 2022, 18, 1–3. [Google Scholar] [CrossRef]
- Ewerton, F.; Cruz, F.; Kapp, M.; Klein, S.; Roehm, P.; Chapple, C. Efficacy and Safety of Eliapixant in Overactive Bladder: The 12-Week, Randomised, Placebo-controlled Phase 2a OVADER Study. Eur. Urol. Focus 2024, 10, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Radi, G.; Campanti, A.; Diotallevi, F.; Martina, E.; Marani, A.; Offidani, A. A Systematic Review of Atopic Dermatitis: The Intriguing Journey Starting from Physiopathology to Treatment, from Laboratory Bench to Bedside. Biomedicines 2022, 10, 2700. [Google Scholar] [CrossRef] [PubMed]
- McGarvey, L.; Smith, J.A.; Morice, A.; Birring, S.S.; Chung, K.F.; Dicpinigaitis, P.V.; Niimi, A.; Benninger, M.S.; Sher, M.; Matsunaga, Y.; et al. A Randomized, Double-Blind, Placebo-Controlled, Parallel-Group Phase 2b Trial of P2X3 Receptor Antagonist Sivopixant for Refractory or Unexplained Chronic Cough. Lung 2023, 201, 25–35. [Google Scholar] [CrossRef]
- Ohishi, T.; Matsuyama, Y. Minodronate for the treatment of osteoporosis. Ther. Clin. Risk Manag. 2018, 14, 729–739. [Google Scholar] [CrossRef]
- Jacobson, K.A.; Giancotti, L.A.; Lauro, F.; Mufti, F.; Salvemini, D. Treatment of chronic neuropathic pain: Purine receptor modulation. Pain 2020, 161, 1425–1441. [Google Scholar] [CrossRef]
- Hagens, M.H.J.; Golla, S.S.V.; Janssen, B.; Vugts, D.J.; Beaino, W.; Windhorst, A.D.; O’Brien-Brown, J.; Kassiou, M.; Schuit, R.C.; Schwarte, L.A.; et al. The P2X(7) receptor tracer [(11)C]SMW139 as an in vivo marker of neuroinflammation in multiple sclerosis: A first-in man study. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 379–389. [Google Scholar] [CrossRef] [PubMed]
- Stock, T.C.; Bloom, B.J.; Wei, N.; Ishaq, S.; Park, W.; Wang, X.; Gupta, P.; Mebus, C.A. Efficacy and safety of CE-224,535, an antagonist of P2X7 receptor, in treatment of patients with rheumatoid arthritis inadequately controlled by methotrexate. J. Rheumatol. 2012, 39, 720–727. [Google Scholar] [CrossRef]
- Kivitz, A.; Ma, C.; Ahdieh, H.; Galer, B.S. A 2-week, multicenter, randomized, double-blind, placebo-controlled, dose-ranging, phase III trial comparing the efficacy of oxymorphone extended release and placebo in adults with pain associated with osteoarthritis of the hip or knee. Clin. Ther. 2006, 28, 352–364. [Google Scholar] [CrossRef]
- Arulkumaran, N.; Unwin, R.J.; Tam, F.W. A potential therapeutic role for P2X7 receptor (P2X7R) antagonists in the treatment of inflammatory diseases. Expert Opin. Investig. Drugs 2011, 20, 897–915. [Google Scholar] [CrossRef]
- Chrovian, C.C.; Soyode-Johnson, A.; Peterson, A.A.; Gelin, C.F.; Deng, X.; Dvorak, C.A.; Carruthers, N.I.; Lord, B.; Fraser, I.; Aluisio, L.; et al. A Dipolar Cycloaddition Reaction To Access 6-Methyl-4,5,6,7-tetrahydro-1H-[1,2,3]triazolo[4,5-c]pyridines Enables the Discovery Synthesis and Preclinical Profiling of a P2X7 Antagonist Clinical Candidate. J. Med. Chem. 2018, 61, 207–223. [Google Scholar] [CrossRef]

| Receptor | Compound | EC50 Value [μM] | References |
|---|---|---|---|
| P2X1 | ATP | 0.056 (h); 0.1–0.3 (r) | [26,27,28] |
| 2-MeS-ATP | 0.054 (h); 0.1 (r) | ||
| ATPγS | 2.3 (h); 0.59 (r) | ||
| α,β-MeATP | 0.2 (h); 3.2 (r) | ||
| β,γ-MeATP | 2.0 (h); 8.7 (r) | ||
| BzATP | 0.002 (h); 24.2 (r) | ||
| AP4A 1 | 0.182 (h) | ||
| AP6A | 0.6–0.72 (r) | ||
| CTP | 35.1 (r) | ||
| ADP | 30 (h) | ||
| P2X2 | ATP | 2.0–8.0 (h); 3.7 (r) | [27,29] |
| 2-MeATP | 1.0 (h); 1.5 (r) | ||
| ATPγS | 1.5 (r) | ||
| BzATP | 5.5 (h) | ||
| ADP | 100 (h) | ||
| AP4A | 15 (h) | ||
| P2X3 | ATP | 1.0 (h); 1.0 (r) | [26,27] |
| 2-MeS-ATP | 0.350 (h); 0.3 (r) | ||
| ATPγS | 0.690 (h) | ||
| α,β-MeATP | 0.740 (h); 1.0 (r) | ||
| β,γ-MeATP | 9.2 (r) | ||
| BzATP | 5.5 (h) | ||
| AP4A 1 | 0.80 (r); 15.0 (h) | ||
| AP5A1 | 1.3 (r) | ||
| AP6A | 1.6 (r) | ||
| P2X4 | ATP | 0.74 (h); 1.0–10 (r); 0.35 (m) | [26,30,31] |
| 2-MeS-ATP | 7.4–100 (r) | ||
| ATPγS | 2.3 (r) | ||
| β,γ-MeATP | 3–10 (r) | ||
| BzATP | 0.515 (h); 300 (r); 2.9 (m) | ||
| AP4A 1 | 1.0 (h) | ||
| P2X5 | ATP | 0.44–15.4 (r) | [28,30] |
| 2-MeS-ATP | 0.44–20 (r) | ||
| ATPγS | 0.29–9.3 (r) | ||
| α,β-MeATP | 1.1–100 (r) | ||
| β,γ-MeATP | 11.8 (r) | ||
| BzATP | 1.3 (r); 40 (h) | ||
| AP3A 1 | 5.4 (r) | ||
| ADP | 1.8 (r) | ||
| P2X6 | ATP | 12 (h); 1.0–10 (r) | [30] |
| 2-MeS-ATP | 9 (h); 0.6 (r) | ||
| ATPγS | 1.3 (r) | ||
| BzATP | 25 (r) | ||
| ADP | 11 (r) | ||
| P2X7 | ATP | 780 (h); 100 (r) | [26,31,32] |
| 2-MeS-ATP | 178 (h); 2000 – 4000 (m); 10 (r) | ||
| ATPγS | 138 (h) | ||
| α,β-MeATP | >300 (r) | ||
| BzATP | 52 (h); 5.0–500 (r) | ||
| ADP | >300 (r) |
| Receptor | Compound | IC50 Value [μM] | References |
|---|---|---|---|
| P2X1 | Suramin | 1.0 (h); 1.0–1.7 (r) | [26,28,39,40] |
| PPADS | 1.0 (h); 0.09–0.12 (r) | ||
| Reactive Blue 2 | 2.3 (r) | ||
| PPNDS | 14 (r) | ||
| TNP-ATP | 0.006 (h); 0.001 (r) | ||
| IP51 | 0.001–0.003 (r) | ||
| MRS2159 | 1.15 (h); 0.009 (r) | ||
| MRS2220 | 10.2 (r) | ||
| MRS2219 | 5.9 (r) | ||
| ATA | 0.008 (r) | ||
| P2X2 | Suramin | 10.4 (r) | [26,35] |
| PPADS | 1.2 (r) | ||
| NF023 | >50 (r) | ||
| Reactive Blue 2 | 0.360 (r) | ||
| TNP-ATP | 2 (h) | ||
| MRS 2179 | >10 (r) | ||
| IP51 | >30 (r) | ||
| MRS 2220 | >100 (r) | ||
| NF770 | 0.019 (h) | ||
| PSB-10211 | 0.09 (r) | ||
| PSB-1011 | 0.08 (r) | ||
| P2X3 | Suramin | 14.9 (h); 0.006–3.0 (r) | [26,40,41,42,43] |
| PPADS | 1.7 (h); 0.005–1.0 (r) | ||
| TNP-ATP | 0.9 (h) | ||
| MRS2179 | 13 (r) | ||
| IP5I | 2.8 (r) | ||
| MRS2220 | 58.3 (r) | ||
| A-317491 | 0.02–0.1 (h) | ||
| AF219-MK7264 | 0.03 (h) | ||
| RO-4 or AF-235 | 0.008 (h, r) | ||
| BAY1817080 | 0.008 (h) | ||
| BLU- 5937 | 0.025 (h) | ||
| P2X4 | Suramin | 100 (h); 500 (r) | [33,44,45] |
| PPADS | 30 (h); 200 (r) | ||
| NF023 | >100 (h) | ||
| Reactive Blue 2 | 128 (h) | ||
| TNP-ATP | 15.2 (h) | ||
| KN-62 | >100 (h) | ||
| MRS2220 | >100 (r) | ||
| 5-BDBD | 0.35–0.5 (h); 3.5 (r); 2.5 (m) | ||
| NP-1815-PX | 0.26 (h) | ||
| PSB-12054 | 0.19 (h) | ||
| PSB-12062 | 1.4 (h) | ||
| BX430 | 0.78 (h) | ||
| BAY-1797 | 0.11–0.23 (h, m, r) | ||
| PSB-15417 | 0.022–0.037 (r); 0.087 (m) | ||
| P2X5 | Suramin | 1.0–4.0 (r) | [28] |
| PPADS | 0.20–2 (r) | ||
| TNP-ATP | 0.45 (r) | ||
| Reactive Blue 2 | 18.5 (r) | ||
| IP5I | <30 (r) | ||
| P2X7 | Suramin | 300 (h); 300 (r) | [26,39,46,47,48,49,50] |
| PPADS | 62.2 (h); 50 (r) | ||
| MRS2179 | >30 (h) | ||
| A-438079 | 0.933 (h) | ||
| A-804598 | 0.010–0.021 (h, r, m) | ||
| A-740003 | 0.04–0.069 (h) | ||
| A-839977 | 0.02 (h); 0.042 (r); 0.150 (m) | ||
| AZ11645373 | 0.007–0.1(h) | ||
| CE224,543 | 0.002–0.013 (h) | ||
| GSK1482160 | 0.003 (h) | ||
| AZ9056 | 0.012 (h) | ||
| AZ10606120 | 0.0014–0.23 (h) | ||
| JNJ47965567 | 0.005–0.011 (h) | ||
| JNJ54232334 | 0.003 (h); 0.032 (r) | ||
| JNJ54140515 | 0.079 (r) | ||
| JNJ54175446 | 0.003 (h) | ||
| JNJ54173717 | 0.0016 (h) | ||
| JNJ42253442 | 0.020 (h) | ||
| JNJ64413739 | 0.015 (h) | ||
| GW791343 | 8.9 (h) |
| ID No./Drug Name | Target Receptor | Disease/Symptoms | Phase | Trial Status/Sponsor Name |
|---|---|---|---|---|
| NCT02502097/ Gefapixant (AF-219/MK-7269) | P2X3R antagonist | Idiopathic pulmonary fibrosis with persistent cough [57] | III | Completed/Afferent Pharmaceuticals, Inc., a subsidiary of Merck & Co., Inc. (Rahway, NJ, USA) |
| NCT04614246/ BAY-1817080 | P2X3R antagonist | Endometriosis with pelvic pain [130] | II | Terminated/Bayer (Leverkusen, Germany) |
| NCT04545580/ BAY-1817080 | P2X3R antagonist | Overactive bladder [131] | II | Completed/Bayer (Leverkusen, Germany) |
| NCT04693195/ BLU-5937 | P2X3R antagonist | Chronic pruritus associated with atopic dermatitis [132] | II | Completed/Bellus Health Inc.—a GSK company (London, UK) |
| NCT04110054/ S-600918 | P2X3R antagonist | Adults with refractory chronic cough [133] | II | Completed/Shionogi Inc. (Shuo-ku, Japan) |
| NCT05305183/ Minodronate | P2X2/3R antagonist | Osteoporosis; back pain in patients with osteoporosis [134] | III | Unknown/Shandong New Time Pharmaceutical Co., Ltd. (Linyi, China) |
| NC-2600 | P2X4R antagonist | Neuropathic pain [135] | I | Unknown/Nippon Chemiphar Co., Ltd. (Chiyoda-ku, Japan) |
| AK-1780 | P2X7R antagonist | Diabetic peripheral neuropathy/chronic pain [136] | II | Unknown/Eli Lilly and Company (Indianapolis, IN, USA) |
| NCT00628095/ CE-224535 | P2X7R antagonist | Rheumatoid arthritis in patients who have not totally improved with methotrexate [137] | II | Completed/Pfizer (New York, NY, USA) |
| NCT00418782/ CE-224535 | P2X7R antagonist | Osteoarthritis/chronic pain [138] | II | Terminated (lack of efficacy)/Pfizer (New York, NY, USA) |
| NCT00849134/ GSK1482160 | P2X7R antagonist | Inflammatory pain [139] | I | Completed/GlaxoSmithKline (London, UK) |
| NCT04116606/ JNJ-54175446 | P2X7R antagonist | Major depressive disorder [129] | II | Unknown/CCTU-Core (Cambridge, UK) |
| NCT05328297/ JNJ-55308942 | P2X7R antagonist | Bipolar depression [140] | II | Completed/Janssen Pharmaceutica N.V., Belgium (Beerse, Belgium) |
| NCT05620576/ LY3857210 | P2XR antagonist | Diabetic peripheral neuropathic pain | II | Completed/Eli Lilly and Company (Indianapolis, IN, USA) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cabral-García, G.A.; Cruz-Muñoz, J.R.; Valdez-Morales, E.E.; Barajas-Espinosa, A.; Liñán-Rico, A.; Guerrero-Alba, R. Pharmacology of P2X Receptors and Their Possible Therapeutic Potential in Obesity and Diabetes. Pharmaceuticals 2024, 17, 1291. https://doi.org/10.3390/ph17101291
Cabral-García GA, Cruz-Muñoz JR, Valdez-Morales EE, Barajas-Espinosa A, Liñán-Rico A, Guerrero-Alba R. Pharmacology of P2X Receptors and Their Possible Therapeutic Potential in Obesity and Diabetes. Pharmaceuticals. 2024; 17(10):1291. https://doi.org/10.3390/ph17101291
Chicago/Turabian StyleCabral-García, Guillermo A., José R. Cruz-Muñoz, Eduardo E. Valdez-Morales, Alma Barajas-Espinosa, Andrómeda Liñán-Rico, and Raquel Guerrero-Alba. 2024. "Pharmacology of P2X Receptors and Their Possible Therapeutic Potential in Obesity and Diabetes" Pharmaceuticals 17, no. 10: 1291. https://doi.org/10.3390/ph17101291







